Abstract
Introduction and importance
Unicystic ameloblastomas are less aggressive than solid (multicystic) variant, unfortunately this subtypes mimics clinically and radiographically more gentle lesions: like odontogenic cysts, so are misdiagnosed unless a histological study is carried out. Moreover, it is clinically silent and normally discovered accidentally.
Case presentation
60-year-old male patient, suffering from a pain and swelling located in the left maxillary region; the patient came with double vision and that was the main compliment.
Radiographs showed uniocular radiolucent lesion in the left sinus that contained an impacted third molar. Patient asked for minimal aggressive surgical intervention, and a curettage was preformed along with third impacted molar extraction.
Final diagnosis was obtained from histological study, the result was intraluminal unicystic ameloblastoma plexiform subtype.
Healing went eventually, patient recovered double vision in one month period and six years follow up showed no recurrence.
Clinical discussion
Unicystic ameloblastoma is a rare odontogenic lesion, with clinical, radiographic and gross features of jaw cysts. The lesion histologically shows typical ameloblastomatous epithelium lining part of the cyst cavity with or without and/or mural tumor growth. Unicystic ameloblastoma usually presents in posterior mandibular ramus region, while it is rare and atypical in posterior maxillary region.
Unicystic ameloblastomas with orbital invasion cases are 4 worldwide and this case reports represents the first case in the Middle East.
Conclusion
Thorough examination is recommended when unilocular radiolucency of the jaw is detected. Likewise, orbital surgeons are highly advised to take into account the biological behaviors of maxillary odontogenic tumors.
Keywords: Unicystic ameloblastoma, Odontogenic lesion, Orbital
Highlights
-
•
Maxillary unicystic ameloblastoma is a rare case.
-
•
Orbital involvement is extremely rare.
-
•
Accurate diagnosis, treatment plan and specialties cooperation are important to achieve recovery.
-
•
Radiographic and clinical appearance may cause misdiagnosis and later a treatment failure or recurrence.
1. Introduction
Although ameloblastoma is the most common odontogenic tumor, representing approximately 11 to 18 % of all odontogenic tumor [1] and although its diagnosis normally is not a big challenge for any well trained oral pathologist, still some rare cases are really challenging.
Following WHO classification of head and neck tumors, ameloblastoma is sub classified into either: solid or multicystic (75–86 % of all cases) or less frequent unicystic [2]. It affects mandible four times more than the maxilla [2]. The cystic ameloblastoma normally develops in early age males, mostly in the second and third decade.
Generally, unicystic ameloblastoma cases are less aggressive than the conventional solid (multicystic) variant and it still subdivided into three subtypes, namely: luminal, intraluminal and mural [3]. Unfortunately this subtypes mimics clinically and on radiographs more gentle lesions such as odontogenic cysts [3]. For that they are misdiagnosed unless a histological study is carried out. Moreover, it is clinically silent and normally discovered accidentally [4].
The case we are presenting here is extremely rare from several aspects: patient age, maxillary involvement and its clinical manifestations, which was written according to scare criteria [5].
2. Presentation of case
60-year-old male patient, suffering from a pain and swelling located in left maxillary region; the patient came with double vision (diplopia) he was seeing two images of a single thing and he could not move his eyes in a harmonious manner and that was the main complaint.
It is very rare to see double vision with cystic lesions and tumors in the jaw.
The initial clinical evaluation showed a swelling that extends from the left maxillary second molar. ct.scan (Fig. 1) and (Fig. 2) showed a corticated unilocular radiolucent lesion of 30 × 40 × 50 mm in biggest dimensions. It was in contact with the roots of the upper-second molar. Moreover, radiographs showed that the radiolucency includes an impacted tooth.
Fig. 1.
ct.scan (coronal) showing left maxillary unicystic lesion.
Fig. 2.
ct.scan (axial) demonstrating a large well-defined radiolucent expansile unilocular lesion and impacted third molar inside it.
The patient underwent surgery namely enucleation: a procedure that included surgical curettage of the lesion and extraction of the impacted third molar that exists inside the lesion by the surgeon as one unit. This step was followed by utilizing the electric scalpel onto the cystic cavity to destroy any rests of epithelial cells by the rounded head of the electric scalpel.
The histopathological examination of the lesion revealed and confirmed the unicystic ameloblastoma, a type known as intraluminal plexiform (Fig. 3).
Fig. 3.
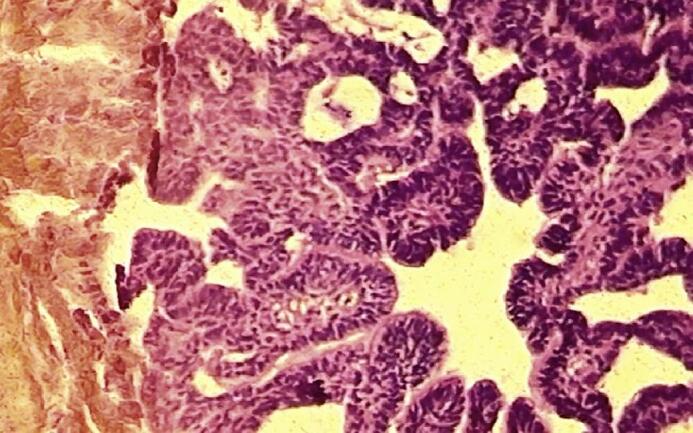
Plexiform unicystic ameloplastoma (40×).
No recurrence was observed in the span of 6 years following treatment by ophthalmologist follow up. Recovery of double vision was achieved within 1 month after surgical intervention (Fig. 4). Panoramic imaging after 6 years disclosed no existence of cystic lesion at any criteria (Fig. 5). The eye exhibited diplopia, presumably originating from the cystic pressure inside the maxillary sinus (Fig. 6). It is identified to affect the floor of the orbit, without immediate invasion against it. Orbital surgeons resorted to performing surgery to the eye muscular tissues after paresis of the sixth ocular nerve; our patient refused the surgery upon his request.
Fig. 4.
Double vision is absent after 6 years of follow up.
Fig. 5.

Panoramic radiograph after 6 year of surgery and follow up.
Fig. 6.
Double vision is still after 1 week of surgery.
The patient keeps at a well-being status, free from tumor recurrence even after 6 years from the treatment. In addition, no surgical procedures whatsoever have been required in the muscular tissues surrounding the eye and follow up by his surgeon and ophthalmologist.
3. Discussion
In this case report, we reiterate discussing surgical management of unicystic ameloblastoma (UA) of the maxilla and double vision. Unicystic ameloblastoma located in the maxillary region has rarely been documented. It is considered as neoplasm demonstrating aggressive local behavior with invasion without the occurrence of distant metastasis. Maxillary spongy architecture, accompanying both the thin and fragile maxilla osseous structure, helps to facilitate easy infiltration of neighboring vital and important structures, such as cranium and orbit [6].
Our study is the first of its type since it is a maxillo-unicystic ameloblastoma case, in which the tumor invaded the orbit. This concern with the entirety of studies at the Middle East regional level, where merely 23 well-documented cases regarding orbital involvement have been reported in the world literature on ameloblastoma. Besides, only 4 publications covering the area of research, unicystic ameloblastoma, abide the literature on ophthalmology [4,7]. Ours is the first case study to report complete recovery after one month of surgical interference against ameloblastomic lesions, under the second category named as Unicystic. This is revealed in (Table 1).
Table 1.
Maxillary unicystic ameloblastoma case reports.
| Serial no. | Year | Author name | Case report/retrospective/prospective | Sex | Age (average) year | Extra maxillary extension | histopathology | treatment | Follow up (years) | Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2020 | El Sayed et al. [8] | Case | F | 3.5 | Orbital nasal | Mural | Maxillectomy | 1 | No |
| 2 | 1985 | Weiss et al. [7] | Case | M | 72 | Intracranial, orbit | Mural | Maxillectomy & radiotherapy | N/A | No |
| 3 | 1993 | Thompson et al. [9] | Case | F | 7 | None | Mural | Limited resection (enucleation) | 6 | Yes: 6 years |
| 2 | 2010 | Pitak-Arnnop et al. [10] | Case | M | 19 | Nasal wall | Unicystic ameloblastoma | Enucleation with curettage | 5 | No |
F: female, M: male, N/A: not applicable.
The whole histopathological ameloblastomous categories have been shown. At the microscopic level, the unicystic abnormality is diagnosed via the presence of a distinct single cystic depth, cavity. This is necessitated to be lined with two entities: the odontogenic ameloblastomatous epithelium as well as fibrous stroma. Occasionally it exhibits patterns of intraluminal plexiform nature. Ackerman classified UA into 3 categories according to the microscopic appearance of lesions [1]: Luminal: fibrous cystic wall is not infiltrated by tumor, intraluminal: epithelial proliferation without any infiltration of connective tissue wall, and mural: invasive islands of ameloblastomatous epithelium in the connective tissue wall not involving the entire epithelium.
Nonetheless, mural ameloblastoma, has been found out in the literature to claim itself as the most aggressive – at the local level – with a high recurrence probability; such reappearance owes its presence to its invasive nature [9,10]. Given that a thorough histopathological analysis was realized, our patient belonged to the second subtype.
Attaining the ultimate surgical approach to address this tumor has always been a controversial method, particularly for those patients in their 20s and 30s, adding to the basic consideration of treatment decision during the initial diagnosis. Opinions diverge between conservative management, such as limited resection, enucleation, curettage, opposing extensive surgical interference, presented as the radical re-sectioning, known medically as maxillectomy [11].
Ameloblastoma originating in the maxillary region has been found throughout the majority of research to be extremely rare. However, it is highly associated with ophthalmologic defects. Conversely, our investigation recommends a multifaceted scheme of treatment to reach the most preferable outcomes of whatever medical treatment is decided upon. This holds true for functional as well as cosmetic concerns. Practitioners in the fields of otolaryngology and ophthalmology are advised to focus on maxillary ameloblastoma once to the patient is displays ophthalmologic symptoms with a history of such rare tumor. When the patient is subject to treatment under the mode of conservative surgery, they are suggested to be evaluated for a long follow-up period. Contrastively, a mere recurrence of UA in the maxilla region invites pervasive treatment, such as that of radical re-sectioning as a more adequate scheme of medical interference.
4. Conclusion
Close monitoring and thorough examination are recommended when unilocular radiolucency of the jaw is detected. Likewise, orbital surgeons are highly advised to take into account the biological behaviors of maxillary odontogenic tumors. Accordingly, minute management considerations inside the clinic settings are extremely recommended prior to administering any type of surgical interference.
Consent
Written informed consent was obtained from the patient's for publication of this case report and accompanying images, for the necessity of showing the eyes the patient was informed on this particular point and his acceptance was added to the written informed consent. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Patient perspective
Patient was rather satisfied with the entire surgical procedure and overall treatment.
Ethical approval
Ethical approval was waived by the authors institution (Damascus University).
Funding
N/A. No external source of funding.
Guarantor
Prof. Dr. Nabil Kochaji.
Research registration number
No research was made, no registry is needed.
CRediT authorship contribution statement
Prof. Dr. Nabil Kochaji: pathological study, paper writing and literature review.
Dr. Raqi barber: primary surgeon, literature review, paper writing and patient follow-up.
Prof. Dr. Charif Barakat, Dr. Maher Assaf literature review.
Declaration of competing interest
Authors have no conflicts of interest.
Acknowledgements
None.
References
- 1.Siar C.H., Lau S.H., Ng K.H. Ameloblastoma of the jaws: a retrospectiveanalysis of 340 cases in a Malaysian population. J. Oral Maxillofac. Surg. 2012;70:608–615. doi: 10.1016/j.joms.2011.02.039. [DOI] [PubMed] [Google Scholar]
- 2.Thompson L. World Health Organization classification of tumours: pathologyand genetics of head and neck tumours. Ear Nose Throat J. 2006;85(2):74. [PubMed] [Google Scholar]
- 3.Philipsen H.P., Reichard P.A., Unicystic ameloblastoma. A review of 193 cases from literature. Oral Oncol. 1998;34:317–325. doi: 10.1016/s1368-8375(98)00012-8. [DOI] [PubMed] [Google Scholar]
- 4.Agani Z., Hamiti-Krasniqi V., Recica J., Loxha M.P., Kurshumliu F., Rexhepi A. Maxillary unicystic ameloblastoma: a case report. BMC Res. Notes. 2016;18:469. doi: 10.1186/s13104-016-2260-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., et al. The SCARE 2020 guideline: updating consensus surgical Case REport (SCARE) guidelines. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Zwahlen R.A., Grätz K.W. Maxillary ameloblastomas: a review of the literature and of a 15-year database. J. Craniomaxillofac. Surg. 2002;30(5):273–279. doi: 10.1016/s1010-5182(02)90317-3. (PMID: 12377199) [DOI] [PubMed] [Google Scholar]
- 7.Weiss J.S., Bressler S.B., Jacobs E.F., Jr., Shapiro J., Weber A., Albert D.M. Maxillary ameloblastoma with orbital invasion. A clinicopathologic study. Ophthalmology. 1985;92(5):710–713. doi: 10.1016/s0161-6420(85)33977-5. (PMID: 4011147) [DOI] [PubMed] [Google Scholar]
- 8.El Sayed M., Touny M., Ibrahim N., Al-Azzawi Z. A rare case of huge maxillary ameloblastoma in a 3.5 years old girl. Int. J. Surg. Case Rep. 2020;72:448–453. doi: 10.1016/j.ijscr.2020.06.027. (PMID: 32698263) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson I.O., Ferreira R., van Wyk C.W. Recurrent unicystic ameloblastoma of the maxilla. Br. J. Oral Maxillofac. Surg. 1993;31(3):180–182. doi: 10.1016/0266-4356(93)90121-c. (PMID: 8512914) [DOI] [PubMed] [Google Scholar]
- 10.Pitak-Arnnop P., Chaine A., Dhanuthai K., Bertrand J.C., Bertolus C. Unicystic ameloblastoma of the maxillary sinus: pitfalls of diagnosis and management. Hippokratia. 2010;14(3):217–220. (PMID: 20981175) [PMC free article] [PubMed] [Google Scholar]
- 11.Meshram M., Sagarka L., Dhuvad J., Anchlia S., Vyas S., Shah H. Conservative management of unicystic ameloblastoma in young patients: a prospective single-center trial and review of literature. J. Maxillofac. Oral Surg. 2017;16(3):333–341. doi: 10.1007/s12663-016-0987-2. (PMID: 28717292) [DOI] [PMC free article] [PubMed] [Google Scholar]






