Summary
Background
Pacific Island Countries (PICs) face unique challenges in providing surgical care. We assessed the surgical care capacity of five PICs to inform the development of National Surgical, Obstetric and Anaesthesia Plans (NSOAP).
Methods
We conducted a cross-sectional survey of 26 facilities in Fiji, Tonga, Vanuatu, Cook Islands, and Palau using the World Health Organization - Program in Global Surgery and Social Change Surgical Assessment Tool.
Findings
Eight referral and 18 first-level hospitals containing 39 functioning operating theatres, 41 post-anaesthesia care beds, and 44 intensive care unit beds served a population of 1,321,000 across the five countries. Most facilities had uninterrupted access to electricity, water, internet, and oxygen. However, CT was only available in 2/8 referral hospitals, MRI in 1/8, and timely blood transfusions in 4/8. The surgical, obstetric, and anaesthetist specialist density per 100,000 people was the highest in Palau (49.7), followed by Cook Islands (22.9), Tonga (9.9), Fiji (7.1), and Vanuatu (5.0). There were four radiologists and 3.5 pathologists across the five countries. Surgical volume per 100,000 people was the lowest in Vanuatu (860), followed by Fiji (2,247), Tonga (2,864), Cook Islands (6,747), and Palau (8,606). The in-hospital peri-operative mortality rate (POMR) was prospectively monitored in Tonga and Cook Islands but retrospectively measured in other countries. POMR was below 1% in all five countries.
Interpretation
Whilst PICs share common challenges in providing specialised tertiary services, there is substantial diversity between the countries. Strategies to strengthen surgical systems should incorporate both local contextualisation within each PIC and regional collaboration between PICs.
Funding
None.
Keywords: Global surgery, Pacific Island Countries, Health system strengthening, National surgical planning
Research in context.
Evidence before this study
The Lancet Commission on Global Surgery (LCoGS) highlighted barriers to safe, affordable, and timely surgical, obstetric, and anaesthesia care globally. However, the evidence on surgical care capacity in the Pacific region remains limited. Furthermore, Pacific Island Countries (PICs) face unique challenges in providing essential and emergency surgical care.
We searched academic databases (PubMed, Web of Science, and Global Health) and the grey literature using the keywords ‘Pacific Island’, individual PIC names, and surgical, obstetric, anaesthesia, and trauma care (‘surgical procedure’, ‘operating room’, ‘anaesthesia’, ‘maternal health’, ‘trauma’) for original publications between January 1, 1990 and June 1, 2022 (S1).
Previous studies demonstrated the burden of a range of surgically treated conditions in PICs, including maternal and neonatal conditions, infectious diseases, non-communicable diseases, and traumatic injuries. We found that comprehensive surgical care capacity assessments have only been performed in four PICs: Vanuatu, the Solomon Islands, Samoa and Papua New Guinea. There has only been one cross-national assessment of surgical care in the Pacific region; however, this was limited to the LCoGS indicators and did not include a comprehensive assessment of surgical care capacity.
Added value of this study
This is the first cross-national surgical capacity assessment in Pacific Island Countries. This study analysed the current status, barriers, and opportunities for strengthening surgical systems in five PICs: Fiji, Vanuatu, Tonga, Cook Islands, and Palau. We found that all countries shared common challenges in providing surgical care in first-level hospitals, providing specialised technologically complex services, and adhering to quality assurance processes. However, there is also substantial diversity in surgical care capacity between countries.
Unlike many previous surgical care capacity assessments, our study was co-designed with the Ministry of Health and closely integrated with the policy process of developing National Surgical, Obstetric, and Anaesthesia Plans (NSOAP) in each country.
Implications of all the available evidence
This study identified health system constraints in each country to formulate locally tailored interventions for surgical care system strengthening. There is no one-size-fits-all solution. We recommend conducting comprehensive surgical capacity assessments to identify critical constraints in surgical care capacity in each country in order to develop locally tailored solutions. In addition to policy development by individual countries, regional collaboration could address shared challenges in quality assurance processes, the nursing workforce, and the provision of specialised services.
Introduction
Surgical, obstetric, and anaesthesia (SOA) care is required to treat a third of the global disease burden.1 The World Health Assembly resolution 68.15 recognised emergency and essential surgical care as indispensable to universal health coverage (UHC).2 In 2019, Pacific Health Ministers, at their 13th meeting, championed a Pacific-specific approach to advancing the safe and affordable surgery agenda as a critical component of UHC and the Pacific Healthy Islands Vision, including the development and implementation of National Surgical, Obstetric and Anaesthesia Plans (NSOAPs).3
An NSOAP aims to provide a system-based and coordinated roadmap towards surgical system strengthening.4 NSOAPs shift the focus from externally led programs that temporarily plug gaps towards long-term health system strengthening.5 This builds on Pacific Island Countries’ (PIC) experience in country-led strategic planning. Five PICs: Fiji, Vanuatu, Tonga, Palau, and Cook Islands, commenced NSOAP development in 2020.6
PICs face common barriers to surgical care, including their small populations, geographic dispersion, small-scale economies, distance from the global economy, and vulnerability to external shocks.7 However, they also have considerable diversity in size, population, income status, and health outcomes.7 Previous literature has detailed the burden of diseases requiring SOA care in the Pacific region, highlighting the need to address maternal mortality rates, trauma, complications of non-communicable diseases such as diabetes, and infectious disease sequelae such as cervical cancer and rheumatic heart disease.8, 9, 10, 11
The collection of the Lancet Commission on Global Surgery (LCoGS) indicators in 13 PICs in 2016 demonstrated challenges in surgical care access, specialist workforce, surgical volume, and financial risk protection (Table 1).12 Strengthening health systems requires an understanding of health system building blocks, the interactions between them, and critical points of constraints and bottlenecks through health system assessments.5 Comprehensive surgical care capacity assessments have been conducted in Vanuatu, Samoa, Solomon Islands, and Papua New Guinea.13, 14, 15, 16 However, little is known about surgical and anaesthesia care capacity in other PICs. While surgical care capacity assessments have been widely conducted in other regions,17 cross-country comparisons within a region have not often been made. The Pacific region has a long history of regional collaboration to address common health challenges.7 Surgical care capacity assessments led by external researchers without integration with national policy processes could lead to a distant academic gaze without generating proximal policy solutions.18
Table 1.
| Indicator | 2030 target | Fiji | Vanuatu | Tonga | Cook Islands |
|---|---|---|---|---|---|
| 1. Access to timely essential surgery – the percentage of the population that can access, within 2 h, a facility capable of providing bellwether procedures (Caesarean section, laparotomy, and open fracture management) | 80% | 67% | 44% | 85% | 88% |
| 2. Specialist surgical workforce density – number of surgical, anaesthesia, and obstetric specialists per 100,000 people | 20 | 5.8 | 3.2 | 14 | 22 |
| 3. Surgical volume - procedures performed in an operating theatre per 100,000 population per year | 5000 | 1490 | 1277 | 5061 | 6758 |
| 4. Peri-operative mortality - all-cause death rate before discharge in patients who have undergone a procedure in an operating theatre | Monitored | Not monitored | Not monitored | Monitored | Not monitored |
| 5. Percentage risk of catastrophic out-of-pocket expenditureb on surgical care | 0% | 21% | 14% | 8% | NA |
| 6. Percentage risk of impoverishment due to out-of-pocket expenditurec on surgical care | 0% | 24% | 37% | 16% | NA |
NA: not available.
The LCoGS indicators were collected in four out of five countries included in this study in 2016: Fiji, Vanuatu, Tonga, and the Cook Islands. The LCoGS indicators in Palau were not collected as a part of the 2016 study.12
Catastrophic expenditure is defined as direct out-of-pocket payments of greater than 40% of household income net of subsistence needs.1
Impoverishing expenditure is defined as being pushed into poverty or being pushed further into poverty by out-of-pocket payments.1
This study aimed to assess the capacity to provide essential SOA care in Fiji, Vanuatu, Tonga, Cook Islands, and Palau to inform policy development and strategic planning as a part of the NSOAP process. In addition, we performed an exploratory analysis of factors associated with surgical volume across all facilities in the five countries.
Methods
Study design
We conducted a cross-sectional survey of surgical care capacity in the five PICs developing NSOAPs. Here, we report the quantitative component of this mixed-method assessment in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.19
Study setting
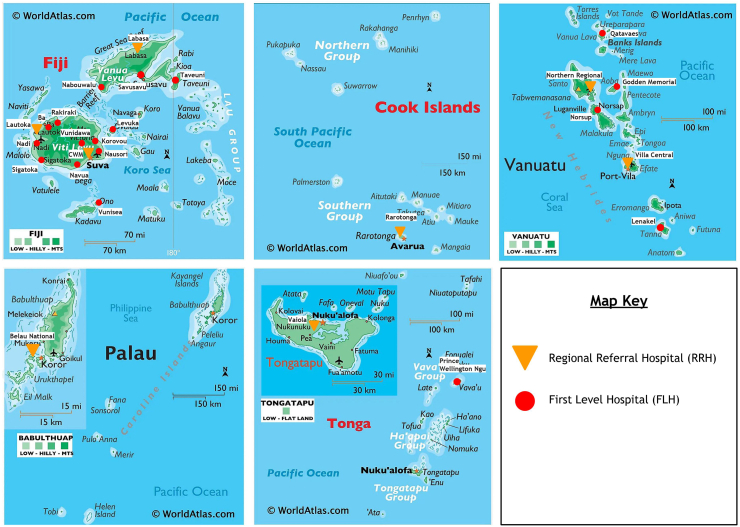
Table 2 summarises the socio-economic characteristics of the five participating PICs and demonstrates substantial diversity in population, income levels, and geography. While the population is largely concentrated on the small main islands of some countries (Tonga, Cook Islands, and Palau), Fiji and Vanuatu have larger islands with a mountainous interior and more dispersed populations across archipelagos. Fig. 1 displays the geographic location and distribution of the included health facilities in each PIC.
Table 2.
Socio-economic characteristics of Fiji, Vanuatu, Tonga, Palau, and Cook Islands.20, 21, 22, 23, 24, 25, 26
| Country | Population | Land area/Sea area (km2) | Geography | Income classification | Year of Inde-Pendencea | GDP per capita (USD) (2020) | CHE as % GDP (2019) | HDI (2019) | LE (2021) |
|---|---|---|---|---|---|---|---|---|---|
| Fiji | 884,887 | 18,270/1,282,978 | Two main islands with 87% of the population, mountainous interior | Upper-middle | 1970 | 5086 | 3.8 | 0.743 | 68 |
| Vanuatu | 300,019 | 12,190/663,251 | Archipelago with 55% of the population on the two most populous islands | Low-middle | 1980 | 2920 | 3.4 | 0.609 | 71 |
| Tonga | 100,651 | 720/659,558 | One main island with 74% of the population | Upper-middle | 1970 | 4625 | 5.0 | 0.725 | 71 |
| Palau | 18,092 | 459/603,978 | One main island with 70% of the population | Upper-middle | 1994 | 14,244 | 15.2 | 0.826 | 69 |
| Cook Islands | 17,459 | 240/1,960,027 | One main island with 74% of the population | Upper-middle | 1965 | 16,135 | 3.4 | 0.789 | 77 (2020) |
CHE: current health expenditure; GDP: gross domestic product; HDI: human development index; LE: life expectancy.
Fiji, Vanuatu, and Tonga are Member States of the Commonwealth of Nations. Palau is in a compact of free association with the USA. Cook Islands is a self-governing state in free association with New Zealand.
Fig. 1.
Location of the included health facilities in Fiji, Vanuatu, Tonga, Palau, and Cook Islands. Map source: worldatlas.com.27
Health services in all five countries are predominantly delivered through the public system. The private sector plays a minimal role, except in Fiji, where private health expenditure constitutes a third of total health expenditure.28,29 All five countries have tiered health systems, consisting of health centres, first-level hospitals, and referral hospitals. First-level or district hospitals are defined by the World Health Organization (WHO) as being responsible for a well-defined population in a clearly delineated administrative area.30 It typically provides 24-h clinical service of a generalised nature.31 Referral hospitals provide more specialised clinical care to patients referred from a lower level.32 Tertiary and quaternary care is supplemented by overseas medical referrals and visiting specialists.7
Participants
We included all referral and first-level hospitals in the public system. We excluded health centres and nursing stations not designated to provide surgical care, facilities with a catchment population of <10,000, and private facilities.
Data collection
Data were collected through facility visits between June 2020 to February 2021 using a validated Surgical Assessment Tool (SAT) developed by the Program in Global Surgery and Social Change (PGSSC) at Harvard Medical School and the WHO through a systematic review and the Delphi consensus process.33 It contains 169 items on surgical care inputs (access to care, infrastructure, workforce, information management, finance), outputs (service volume), and outcomes (peri-operative mortality rate) based on the WHO Health Systems Building Blocks Framework (S2).
Access to care was assessed using health providers’ estimate of the proportion of patients able to access the health facility within 2 h. The availability of utility (electricity, running water, internet, oxygen), equipment, consumables, and medication was measured using a 6-point scale: 100%, 76–99%, 51–75%, 26–50%, 1–25%, and 0% of the time (S2). Surgical volume was collected over a 12-month period preceding the data collection date. In-hospital peri-operative mortality rate (POMR) was collected by reviewing the admission to discharge record.
The Ministry of Health of each study country initiated contact with each health facility and obtained consent to conduct the facility assessment. After receiving training on the SAT, a senior medical provider at each facility administered the tool. Data were collected through hospital walk-throughs, review of operative logbooks, admission, and outpatient records, direct observation of consumable and medication availability, and interviews with the hospital staff.
Data analysis
For the descriptive analysis, data were categorised by country and by facility level: referral hospital (national and provincial) and first-level hospital. Summary statistics were planned for each country and facility level, including the number of admissions, hospital beds, functioning operating room (ORs), post anaesthesia care unit (PACU) beds, intensive care unit (ICU) beds, and anaesthetic machines; the availability of utility, blood, diagnostics, medication, equipment, and consumables; the number of specialist and non-specialist providers, supporting staff, and surgical volume. Availability scores for utility, blood, radiology, laboratory, medication, equipment and supplies were calculated from the sum of individual item availability in each category on the WHO-PGSSC SAT in line with previous literature (where 100% = 5, 76–99% = 4, 51–75% = 3, 26–50% = 2, 1–25% = 1, and 0% = 0). In accordance with previous literature, we categorised equipment and consumables into anaesthetic equipment, surgical equipment, and consumables (S2).34,35 Descriptive comparisons were made without statistical inference.
Three of the six LCoGS indicators outlined in Table 1 were calculated at a national level, including the SOA specialist density per 100,000 people, surgical volume per 100,000 people, and in-hospital POMR.1
In addition to the descriptive analysis, we conducted an exploratory regression analysis to assess factors associated with facility-level surgical volume. Surgical volume at each facility over a 12-month period was the dependent variable. Independent variables included the number of hospital beds, functioning ORs, PACU beds, anaesthetic machines, SOA specialists, nurses, midwives and the composite availability scores of medications, equipment, consumables, utility, radiology, laboratory, and blood transfusions at each facility. A correlation matrix was used to assess collinearity. Colinear independent variables were additively combined. Variables with a univariate p-value <0.1 were selected as covariates in the multivariate model. Robust linear regression was used due to the small sample size and the presence of outliers with substantial variation in surgical volume between facilities. Statistical significance was defined as p < 0.05. Data analyses were conducted using R Studio version 4.2.
Any missing or unclear data fields were validated with submitters by email or phone. As a part of the NSOAP process, the result of the data analysis was shared with stakeholders through policy briefs and national stakeholder consultation meetings for co-interpretation and triangulation.
Ethical consideration
Ethics approval was granted by the Harvard Longwood Campus Institutional Review Board (IRB21-122) and the Ministry of Health ethics committee in each study country.
Role of the funding source
No funding received.
Results
Among the 27 eligible facilities across the five countries, one first-level hospital in Fiji was excluded due to non-response after multiple contact. 26 facilities were included in the final study. They comprised eight referral hospitals, which encompassed five national referral hospitals and three provincial referral hospitals in the larger study countries (Fiji and Vanuatu), and 18 first-level hospitals. They served a total population of 1,321,000 across the five study countries.
Access to care
Due to geographical variation, the catchment population of first-level hospitals had a wide range between 10,000 and 100,000 people. Providers reported that more than 76% of the population could access all facilities in Cook Islands, Tonga, and Palau within 2 h. However, less than 76% of the population was estimated to have timely access within 2 h to 6/16 hospitals in Fiji and 6/6 hospitals in Vanuatu. Timely access was achieved where the population is concentrated on a few small main islands. However, it can be more challenging when the population is dispersed across an archipelago or larger islands with a mountainous interior. Three private hospitals provide elective surgical care in Fiji, all located in urban areas.
Infrastructure
Beds and space
Table 3 displays the catchment population and the number of admissions, inpatient hospital beds, ORs, PACU beds, and ICU beds across health facility levels in the five countries. A total of 39 functioning ORs, 41 PACU beds, and 44 ICU beds served a population of 1,321,000 across the five countries. Comparing across health facility levels, ORs, PACU and ICU beds and anaesthetic machines were concentrated in referral hospitals.
Table 3.
Catchment population, admissions, and infrastructure of surveyed health facilities in Fiji, Vanuatu, Tonga, Palau, and Cook Islands.
| Country | Facility | Catchment population | Admissions per year | Inpatient hospital beds | Functional ORs | Functional ORs per 100,000 people | PACU beds | PACU beds per 100,000 people | ICU beds | Anaesthetic machines |
|---|---|---|---|---|---|---|---|---|---|---|
| Fiji | RH #1 | 415,932 | 24,475 | 458 | 5 | 14 | 16 | 9 | ||
| RH #2 | 337,041 | 15,980 | 339 | 3 | 3 | 11 | 4 | |||
| RH #3 | 131,914 | 11,300 | 170 | 3 | 4 | 3 | 5 | |||
| FL #1 | 27,895 | 1000 | 20 | 1 | 0 | 0 | 0 | |||
| FL #2 | 22,649 | 352 | 12 | 1 | 1 | 0 | 0 | |||
| FL #3 | 17,769 | 500 | 22 | 1 | 0 | 0 | 1 | |||
| FL #4 | 94,088 | 0 | 0 | 0 | 0 | 0 | 1 | |||
| FL #5 | 75,838 | 3550 | 86 | 1 | 0 | 0 | 2 | |||
| FL #6 | 72,582 | 1200 | 50 | 0 | 0 | 0 | 0 | |||
| FL #7 | 58,940 | 4200 | 56 | 1 | 2 | 0 | 1 | |||
| FL #8 | 30,416 | 1500 | 29 | 1 | 0 | 0 | 1 | |||
| FL #9 | 33,660 | 2844 | 56 | 1 | 0 | 0 | 1 | |||
| FL #10 | 16,787 | 1132 | 33 | 1 | 0 | 0 | 1 | |||
| FL #11 | 15,489 | 828 | 26 | 1 | 2 | 0 | 1 | |||
| FL #12 | 15,657 | 215 | 32 | 1 | 1 | 0 | 1 | |||
| FL #13 | 10,869 | 480 | 22 | 1 | 0 | 0 | 0 | |||
| National | 884,887 | 69,556 | 1399 | 22 | 2.49 | 27 | 3.05 | 30 | 28 | |
| Vanuatu | RH #1 | 103,987 | 6700 | 163 | 2 | 3 | 2 | 2 | ||
| RH #2 | 608,84 | 4105 | 80 | 3 | 2 | 1 | 2 | |||
| FL #1 | 45,714 | 2152 | 37 | 1 | 0 | 0 | 0 | |||
| FL #2 | 35,607 | 400 | 28 | 1 | 0 | 0 | 0 | |||
| FL #3 | 42,499 | 790 | 50 | 2 | 0 | 0 | 1 | |||
| FL #4 | 11,330 | 70 | 10 | 0 | 0 | 0 | 0 | |||
| National | 300,019 | 14,217 | 368 | 9 | 3.00 | 5 | 1.67 | 3 | 5 | |
| Tonga | RH #1 | 86,913 | 8888 | 200 | 3 | 4 | 4 | 3 | ||
| FL #1 | 13,738 | 1715 | 60 | 1 | 2 | 0 | 0 | |||
| National | 100,651 | 10,603 | 260 | 4 | 3.97 | 6 | 5.96 | 4 | 3 | |
| Palau | RH #1/national | 18,092 | 1887 | 80 | 2 | 11.05 | 1 | 5.53 | 4 | 3 |
| Cook Islands | RH #1/national | 17,459 | 4567 | 88 | 2 | 11.46 | 2 | 11.46 | 3 | 2 |
FL: first-level hospital; ICU: intensive care unit; OR: operating room; PACU: post anaesthesia care unit; RH: referral hospital.
Comparing between countries, there was more infrastructure constraint in terms of OR and PACU space in Fiji and Vanuatu compared to Tonga, Cook Islands and Palau. The number of ORs and PACUs per 100,000 people was the lowest in Fiji and Vanuatu, followed by Tonga, Palau, and Cook Islands.
Utility, diagnostics, blood
Uninterrupted access to electricity, running water, internet, oxygen, X-ray, USS, and laboratory tests was available in all referral hospitals in Tonga, Cook Islands, Palau and Fiji (Table 4). Most first-level hospitals had consistent access to electricity, water, internet, and oxygen. However, less than 50% of first-level hospitals in Fiji and Vanuatu had access to X-ray, biochemistry, and urinalysis. Ultrasound was available in more facilities than X-ray. Stakeholders reported X-ray availability to be limited by technician and radiographer availability, whereas ultrasound could be utilised by medical staff at the point of care when required.
Table 4.
Utility, blood, radiology, and laboratory test availability.a
| Country | Hospital level | Utility |
Timely Blood Accessb | Radiology |
Laboratory |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Electricity | Running water | Internet | Oxygen | X-ray | USS | CT | CBC | UEC | Urine | |||
| Fiji | RH | 3/3 | 3/3 | 3/3 | 3/3 | 2/3 | 3/3 | 3/3 | 1/3 | 3/3 | 3/3 | 3/3 |
| FL | 12/13 | 13/13 | 10/13 | 12/13 | 4/13 | 6/13 | 12/13 | 0/13 | 9/13 | 3/13 | 5/13 | |
| Vanuatu | RH | 2/2 | 2/2 | 2/2 | 1/2 | 0/2 | 1/2 | 2/2 | 0/2 | 1/2 | 2/2 | 2/2 |
| FL | 4/4 | 3/4 | 2/4 | 3/4 | 0/4 | 1/4 | 1/4 | 0/4 | 1/4 | 0/4 | 1/4 | |
| Tonga | RH | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 |
| FL | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 0/1 | 1/1 | 1/1 | 1/1 | |
| Palau | RH | 1/1 | 1/1 | 1/1 | 1/1 | 0/1 | 1/1 | 1/1 | 0/1 | 1/1 | 1/1 | 1/1 |
| Cook Island | RH | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 1/1 | 0/1 | 1/1 | 1/1 | 1/1 |
CT: computerised tomography; FL: first-level hospital; RH: referral hospital.
Utility, blood transfusions or diagnostic tests are deemed unavailable at a facility when it is available for less than 75% of the time.
Defined as red blood cell transfusion within 2 h (S1).
Complex equipment, such as CT and MRI for cross-sectional imaging, was not readily available. CT was present in two out of five countries and two out of eight referral hospitals; MRI was only present in one referral hospital in one country. They were not available in first-level hospitals.
There was very poor availability of blood across both referral and first-level hospitals in all five countries. Timely access to red blood cell transfusion within 2 h was consistently available in only 4/8 referral hospitals and 5/18 first-level hospitals across all five countries (Table 4).
Equipment and supplies
There was generally good availability of equipment, consumables, and medications in referral hospitals across all five countries and poorer availability in first-level hospitals in Fiji and Vanuatu.
Comparing referral hospitals across countries, the composite availability scores for anaesthetic and surgical equipment and supplies were lower in Vanuatu and Fiji than in Tonga, Palau, and Cook Islands (Table S4). The medication availability score was lower in the referral hospital in Palau compared to the referral hospitals in other countries, possibly due to the impact of the COVID-19 pandemic on supply chains (Table S4).
Workforce
The SOA specialist density per 100,000 people was the highest in Palau (49.7), followed by Cook Islands (22.9), Tonga (9.9), Fiji (7.1), and Vanuatu (5.0) (Table 5). The two least populated countries with the highest income per capita, Palau and Cook Islands, met the Lancet Commission SOA specialist density target of 20 per 100,000. However, the number of anaesthetists/anaesthesiologists in both Palau and Cook Islands was one. This highlights that workforce isolation remains a significant workforce issue in both countries despite meeting the SOA specialist density target.
Table 5.
Surgical, obstetric, and anaesthesia (SOA) workforce.
| Country |
Fiji |
Vanuatu |
Tonga |
Palau |
Cook Islands |
|||
|---|---|---|---|---|---|---|---|---|
| Hospital level | RH | FL | RH | FL | RH | FL | RH | RH |
| Surgeons | 25 | 0 | 7 | 0 | 5 | 0 | 5 | 1 |
| Obstetricians & Gynaecologists | 21 | 0 | 5 | 0 | 3 | 0 | 3 | 2 |
| Anaesthetists/anaesthesiologists | 17 | 0 | 3 | 0 | 2 | 0 | 1 | 1 |
| Non-physicians providing surgery | 0 | 0 | 4 | 5 | 0 | 0 | 0 | 0 |
| Non-physicians providing caesarean sections | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Non-physicians providing anaesthesia | 3 | 0 | 6 | 3 | 1 | 0 | 2 | 0 |
| Midwives | 98 | 115 | 33 | 17 | 11 | 5 | 5 | 10 |
| Surgical Nurses | 169 | 34 | 39 | 18 | 23 | 2 | 13 | NA |
| Pharmacists | 33 | 14 | 7 | 1 | 6 | 3 | 3 | 1 |
| Biomedical Technicians | 15 | 2 | 0.25a | 0 | 1 | 2 | 2 | 1 |
| Radiologists | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| Pathologists | 2 | 0 | 1 | 0 | 0.5a | 0 | 0 | 0 |
| National total SOA number | 63 | 15 | 10 | 9 | 4 | |||
| National SOA Density (Per 100,000) | 7.1 | 5.0 | 9.9 | 49.7 | 22.9 | |||
FL: first-level hospital; NA: not available; RH: referral hospital; SOA: surgical, obstetric, and anaesthesia.
Part-time personnel was counted based on their full-time equivalent.
Compared to the LCoGS indicator collected in 2016, the SOA specialist density in 2020 and 2021 had improved in Vanuatu (3.2 to 5.0), Fiji (5.8 to 7.1), Cook Islands (22–22.9) but decreased in Tonga (14–9.9).12
Comparing across hospital levels, all SOA specialists were concentrated in referral hospitals, with no SOA specialists present in first-level hospitals. Surgical nurses were concentrated in referral hospitals; however, midwives were more evenly distributed between referral and first-level hospitals.
Task-shifting was practised in limited settings across the five countries. Non-physicians provided anaesthesia in Fiji, Vanuatu, Tonga, and Cook Islands. In Vanuatu, non-physician nurse practitioners provided primary-level surgical procedures, such as incision and drainage, circumcision and suturing of lacerations.
The number of supporting workforce, such as biomedical technicians, radiologists, and pathologists, was low across all five countries. There were four radiologists and 3.5 pathologists across Tonga, Vanuatu, and Fiji, with no radiologists and pathologists in Cook Islands and Palau.
Service delivery
Surgical volume per 100,000 population was the lowest in Vanuatu, followed by Fiji, Tonga, Cook Islands, and Palau (Table 6). Palau and Cook Islands met the LCoGS surgical volume target of 5000 per 100,000 people. Since 2016, the surgical volume has increased in Fiji (1490 –> 2247), remained static in Cook Islands (6758 –> 6747), and decreased in Vanuatu (1277 –> 860) and Tonga (5061 –> 2864).
Table 6.
Service volume, quality, and safety.
| Country | Service volume |
Quality & safety |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Facility level | Total number of surgeries | Laparo-tomies | C/S | Open fracture management | Surgical volume per 100,000 | C/S rate (%) | POMR (%) | WHO Checklist use 100% of the time | |
| Fiji | RH | 19,628 | 768 | 3416 | 996 | 17.5% | 0/3 | ||
| FL | 259 | 2 | 23 | 0 | 0.4% | 1/13 | |||
| National | 19,887 | 770 | 3439 | 996 | 2247 | 13.2% | 0.3% | 1/16 | |
| Vanuatu | RH | 2556 | 150 | 319 | 279 | 6.0% | 0/2 | ||
| FL | 25 | 0 | 3 | 0 | 0.2% | 0/4 | |||
| National | 2581 | 150 | 322 | 279 | 860 | 4.7% | 0.2% | 0/6 | |
| Tonga | RH | 2633 | 57 | 239 | 73 | 11.2% | 0/1 | ||
| FL | 250 | 9 | 19 | 10 | 8.1% | 1/1 | |||
| National | 2883 | 66 | 258 | 73 | 2864 | 10.9% | 0.2% | 1/2 | |
| Palau | RH/National | 1557 | 48 | 66 | 10 | 8606 | 12.2% | 0.3% | 0/1 |
| Cook Islands | RH/National | 1178 | 35 | 40 | 89 | 6747 | 12.5% | 0.0% | 1/1 |
C/S: Caesarean section; FL: first-level hospital; POMR: peri-operative mortality rate; RH: referral hospital; WHO: World Health Organization.
Most surgeries were performed in referral hospitals, with very few performed in first-level hospitals. Tertiary-level procedures comprised less than 1% of all procedures performed across all five countries.
As the proxy marker of quality and safety, POMR was less than 1% in all countries. The Caesarean section (C/S) rate was between the standard of 10–15% set by the WHO in Fiji, Tonga, Palau, and Cook Islands. However, it was well below this target in Vanuatu (4.7%), indicating inadequate access to operative obstetric care. The WHO Surgical Safety Checklist was only used 100% of the time in 1/8 referral hospitals and 2/18 first-level hospitals.
Information management
All hospitals had personnel in charge of maintaining patient health records. Both paper and electronic patient records were used. POMR and other post-operative outcomes (e.g. deep vein thrombosis, surgical site infection) were prospectively monitored 100% of the time in Tonga and Cook Islands. They were never prospectively monitored in Palau, while monitoring in Fiji and Vanuatu was variable (Table S5).
Referral hospitals in Tonga, Cook Islands, Vanuatu, and Fiji held more than ten mortality and morbidity meetings in a year. The number of mortality and morbidity meetings was variable in other hospitals (Table S5).
Regression
A composite variable was created for space (sum of the number of ORs and PACUs) and equipment and supply availability (sum of the availability scores of anaesthetic and surgical equipment and supplies) to address collinearity. On univariate analysis, surgical volume was significantly associated with the number of SOA specialists (β = 293.1, p < 0.001), nurses (β = 94.6, p < 0.001), midwives (β = 199.2, p < 0.001), surgical beds (β = 83.6, p < 0.001), the number of ORs and PACUs (β = 549.4, p < 0.001), anaesthetic machines (β = 1061.4, p < 0.001), the composite equipment and supplies availability (β = 19.9, p = 0.046), medication availability (β = 94.8, p = 0.003), and radiology availability (β = 402.8, p < 0.001) (Table S6). Surgical volume was not significantly associated with the availability of utility, laboratory, and blood transfusion.
In the final multivariate regression model, operative volume was significantly associated with the number of nurses and the combined number of ORs and PACUs after controlling for the number of SOA specialists, midwives, beds, and anaesthetic machines, and the availability of equipment and supplies, medications, radiology, and laboratory (Table S7). This model predicted 97% of the variability in surgical volume in all facilities across the five PICs.
Discussion
In this paper, we reported the result of surgical capacity assessment in five PICs: Fiji, Vanuatu, Tonga, Palau, and Cook Islands. Across all five countries, surgical care capacity was concentrated in referral hospitals with low capacity to deliver surgical services in first-level hospitals. All countries shared challenges in providing specialised, technologically complex services, such as CT/MRI, blood bank, pathology, biomedical engineering, and tertiary-level procedures.
There was diversity as well as commonalities between the five PICs. Two out of five countries, Cook Islands and Palau, met the LCoGS SOA specialist workforce and surgical volume targets. Tonga met the surgical volume target in 2016 but fell short of it in 2020. Whilst workforce appeared to be the main capacity constraint in Tonga, Vanuatu and Fiji faced limitations in infrastructure as well as workforce.
The POMR in all countries was less than 1%; however, POMR was only prospectively monitored in Tonga and Cook Islands. There is an opportunity to make substantial improvements to quality assurance processes through prospectively monitoring POMR and using the WHO Surgical Safety Checklist 100% of the time. The importance of the non-specialist workforce and infrastructure was highlighted, with the number of nurses, and the number of ORs and PACUs were found to be significantly associated with surgical volume across all facilities.
Within the Pacific region, previous surgical capacity assessments had been conducted in the Solomon Islands, Papua New Guinea, Vanuatu and Samoa.13, 14, 15, 16 These studies have also documented the challenges PICs face in accessing specialised services due to their small size and distance from the global market.
Our findings could be explained by the diversity between countries in income status, geography, and affiliation with high-income countries (HICs). Palau and Cook Islands are HICs in free association with the United States and New Zealand, respectively. They met the LCoGS SOA specialist workforce density and surgical volume targets. However, due to their small population, they still face the challenge of workforce isolation. In Tonga, Palau, and Cook Islands, where the population is concentrated on small main islands, timely access to facilities was more readily achievable. However, Fiji and Vanuatu face more significant challenges in timely access due to their geography. Notably, Fiji has a lower SOA specialist workforce density and surgical volume compared to Tonga despite having a higher GDP per capita, possibly due to lower health expenditure as a percentage of GDP.
The LCoGS indicators were collected in four study countries except for Palau in 2016.12 From 2016 to 2020, the LCoGS workforce density indicators improved in Fiji, Vanuatu, and Cook Islands. This is likely due to the ongoing postgraduate regional specialist training program, which has been reported to substantially contribute to workforce retention and development throughout the Pacific region.36 Surgical volume improved in Fiji from 2016 to 2020, likely due to workforce development and outreach from referral to first-level hospitals. However, SOA workforce density and surgical volume decreased in Tonga from 2016 to 2020. This was attributed to a decrease in the number of anaesthetists reported by local stakeholders in data triangulation.
Predictors of surgical volume identified by previous studies include the number of SOA specialists in Uganda, and the number of full-time equivalent surgical providers and infrastructure score in Liberia.35,37 Our study highlighted that OR and PACU space and the number of nurses were significantly correlated with surgical volume across the five PICs. Health systems are complex, adaptive systems with dynamic interactions between their components.38,39 The proper functioning of health systems to produce outputs, such as surgical volume, requires careful alignment and coordination between inputs, such as space, equipment, and workforce.5 The regression analysis could shed light on areas of capacity constraints limiting surgical volume in particular settings. Whilst the LCoGS indicators focused on SOA specialist workforce density, the importance of an adequate nursing workforce must not be forgotten. Previous regression models of surgical volume did not include nurses and midwives as independent variables.35,37 This must be rectified in future studies.
The strength of this study is that it provides a cross-country regional comparison of surgical care capacity, which can be invaluable for benchmarking and policymaking. Multi-national surgical capacity assessments have seldom been undertaken in the past.40,41 Where they have been performed, some studies only included referral hospitals.40
Unlike previous surgical care capacity assessments, this study was closely integrated with national policy development. As a part of the NSOAP process, the data has been co-interpreted and triangulated by the Ministries of Health in each country through regular priority-setting meetings with a broad group of local stakeholders. We believe this helped reduce the ‘foreign gaze’ and biased data interpretation that may occur from studies written by external HIC researchers.18
There are several limitations to this study. Firstly, the data had been collected by providers at each hospital rather than an external team due to COVID-19 travel restrictions. There could be variations in data collection methods despite the provision of training. Secondly, data were only collected from public facilities. The SOA specialist density and surgical volume were underestimated in Fiji, where the private sector plays a more substantial role than the other four countries. Thirdly, the limitations of surgical care assessment tools have been well documented in the literature. The other three LCoGS indicators on timely access and financial risk protection could not be calculated from data collected using the facility assessment tool and require further in-depth study. Only health system inputs and outputs are assessed. The process by which inputs interact to produce outputs, and outcomes of surgical care in terms of safety and quality were not adequately assessed.42,43 Fourthly, our regression was merely an exploratory analysis to highlight the potential areas of capacity constraint limiting surgical volume among the included facilities. Further in-depth exploration through future dynamic modelling studies is warranted. The regression should be triangulated with descriptive data, qualitative data, and the lived experience of local providers in policymaking.5 Lastly, despite closer integration with NSOAP policy development and co-interpretation by in-country practitioners, a degree of ‘foreign gaze’ is still present. We recommend future surgical care capacity assessments be led by in-country researchers.
In terms of policy implications, this study has highlighted the importance of cross-country regional comparisons for identifying health system strengths and limitations to aid policymaking. Interventions to strengthen surgical systems must be tailored to country-specific health system capacity constraints and opportunities.5 Many global surgery initiatives focus on workforce development. Whilst workforce is the main challenge in Tonga, Palau, and Cook Islands, infrastructure was constrained in Fiji and Vanuatu. There is no one-size-fits-all solution. We recommend undertaking the NSOAP development process to identify critical constraints in surgical care capacity in each country and develop locally tailored solutions. While the result of our regression could inspire others to heed attention to the nursing workforce, we recommend other countries and regions conduct their own regression analysis to identify capacity constraints in their specific context.
As well as forward planning by individual countries, regional-level collaboration provides an opportunity to address the common challenges of the nursing workforce, quality assurance processes, and the provision of specialised services, such as tertiary procedures, biomedical engineering, blood bank, and complex diagnostics.
Several countries have highlighted expanding surgical services to first-level hospitals as a policy priority. The designation of first-level hospitals varies widely around the world, with the population served ranging from 10,000 to 1 million.32 Due to the unique geographic context of the Pacific, the population served by first-level hospitals is often much smaller, between a few thousand to 100,000, compared to several hundred thousand in other countries. Expecting all first-level hospitals in the Pacific to provide essential and emergency surgery is unrealistic and could lead to unfair, deficit-based portrayals of surgical care capacity. Instead, policy attention should be placed on identifying select key first-level hospitals in larger districts to upgrade with surgical care capacity.
We have several recommendations for conducting surgical care capacity assessments in future research. Firstly, a review found the method of conducting surgical care capacity assessments to vary widely.17 We have developed a manual to accompany the WHO-PGSSC SAT and would recommend the publication of a standardised manual with wider stakeholder consultation and validation in the future. Secondly, specialists from referral hospitals often conduct outreach services to first-level hospitals in the Pacific region. The SOA specialist workforce and equipment from referral hospitals are shared with first-level hospitals and contribute to the surgical volume in both facility levels. The mobility and fluidity of surgical care infrastructure and workforce across facility levels need to be better incorporated into future surgical capacity assessments.
Conclusion
Our study found that PICs share common and yet diverse challenges in surgical care capacity that can be unique compared to other regions of the world. Solutions to improve surgical care capacity in PICs must be tailored to the health system context of individual countries. Surgical care capacity assessments must be closely integrated with policy development to formulate coordinated, system-based strategies to strengthen surgical systems. In addition to policy development by individual countries, regional collaboration could help address common challenges in providing specialised services and augmenting the nursing workforce. Beyond developing surgical care capacity, attention must be paid to surgical care outcomes, quality, and safety.
Contributors
KM, BK, VT, IW, JT, JH, MT, BL, NM, LM, and KBP conceptualized the study and developed its methodology. JT, RP, LU, JH, DT, YYM, MT, BL, NM, RXQ, and MXL undertook program administration. JT, RP, DT, JH, ML, and NM collected and curated the data. RXQ, GZ, and MXL analysed and visualised the data. All authors contributed to data interpretation and triangulation. RXQ, GZ, and MXL compiled the first draft of the manuscript. All authors critically reviewed and edited subsequent drafts of the manuscript. All authors read and approved the final manuscript.
Data sharing statement
The study protocol and data collection tool are available as supplementary material. The dataset collected by this study is not publicly available due to restrictions in the ethics approval. However, it may be available through communication to the corresponding author and agreement by all co-authors on reasonable request.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Consent for publication
All authors approved the final version of the manuscript submitted for publication.
Declaration of interests
The authors declare no competing interest.
Acknowledgements
We would like to thank Zachary G. Fowler, Hugo Flores, Asinamai Ndai, and Sultan Uz Zaman for their assistance in facilitating the data collection.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100830.
Appendix A. Supplementary data
References
- 1.Meara J.G., Leather A.J.M., Hagander L., et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 2.WHO . World Health Organization; Geneva, Switzerland: 2015. WHA 68.15: strengthening emergency and essential surgical care and anaesthesia as a component of universal health coverage. [DOI] [PubMed] [Google Scholar]
- 3.WHO . World Health Organization; 2019. Outcomes of the thirteenth Pacific health Ministers meeting. Tahiti, French polynesia. [Google Scholar]
- 4.Sonderman K.A., Citron I., Mukhopadhyay S., et al. Framework for developing a national surgical, obstetric and anaesthesia plan. BJS Open. 2019;3(5):722–732. doi: 10.1002/bjs5.50190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chee G., Pielemeier N., Lion A., Connor C. Why differentiating between health system support and health system strengthening is needed. Int J Health Plann Manag. 2013;28(1):85–94. doi: 10.1002/hpm.2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watters D.A., Tangi V., Guest G.D., McCaig E., Maoate K. Advocacy for global surgery: a Pacific perspective. ANZ J Surg. 2020;90(10):2084–2089. doi: 10.1111/ans.15972. [DOI] [PubMed] [Google Scholar]
- 7.Sarfati D., Dyer R., Sam F.A.L., et al. Cancer control in the Pacific: big challenges facing small island states. Lancet Oncol. 2019;20(9):e475–e492. doi: 10.1016/S1470-2045(19)30400-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kool B., Raj N., Wainiqolo I., Kafoa B., McCaig E., Ameratunga S. Hospitalised and fatal head injuries in Viti Levu, Fiji: findings from an island-wide trauma registry (TRIP 4) Neuroepidemiology. 2012;38(3):179–185. doi: 10.1159/000337261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Obel J., Souares Y., Hoy D., et al. A systematic review of cervical cancer incidence and mortality in the Pacific Region. Asian Pac J Cancer Prev. 2014;15(21):9433–9437. doi: 10.7314/apjcp.2014.15.21.9433. [DOI] [PubMed] [Google Scholar]
- 10.Parks T., Kado J., Miller A.E., et al. Rheumatic heart disease-attributable mortality at ages 5-69 Years in Fiji: a five-year, national, population-based record-linkage cohort study. PLoS Neglected Trop Dis. 2015;9(9) doi: 10.1371/journal.pntd.0004033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bythell M., Fong J., Vuadreu R. Maternal mortality in Fiji 2008-2012. Fiji J Public Health. 2014;3:32–37. [Google Scholar]
- 12.Guest G.D., McLeod E., Perry W.R.G., et al. Collecting data for global surgical indicators: a collaborative approach in the Pacific Region. BMJ Glob Health. 2017;2(4) doi: 10.1136/bmjgh-2017-000376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Young S., Perry W.R.G., Leodoro B., et al. Challenges and opportunities in the provision of surgical care in Vanuatu: a mixed methods analysis. World J Surg. 2016;40(8):1865–1873. doi: 10.1007/s00268-016-3535-9. [DOI] [PubMed] [Google Scholar]
- 14.Natuzzi E.S., Kushner A., Jagilly R., et al. Surgical care in the Solomon Islands: a road map for universal surgical care delivery. World J Surg. 2011;35(6):1183–1193. doi: 10.1007/s00268-011-1097-4. [DOI] [PubMed] [Google Scholar]
- 15.Comery B., Perry W.R.G., Young S., et al. Delivery of surgical care in Samoa: perspectives on capacity, barriers and opportunities by local providers. ANZ J Surg. 2020;90(10):1910–1914. doi: 10.1111/ans.15295. [DOI] [PubMed] [Google Scholar]
- 16.Martin J., Tau G., Cherian M.N., et al. Survey of the capacity for essential surgery and anaesthesia services in Papua New Guinea. BMJ Open. 2015;5(12) doi: 10.1136/bmjopen-2015-009841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blair K.J., Paladino L., Shaw P.L., Shapiro M.B., Nwomeh B.C., Swaroop M. Surgical and trauma care in low- and middle-income countries: a review of capacity assessments. J Surg Res. 2017;210:139–151. doi: 10.1016/j.jss.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 18.Abimbola S. The foreign gaze: authorship in academic global health. BMJ Glob Health. 2019;4(5) doi: 10.1136/bmjgh-2019-002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 20.World Bank World Bank open data [internet] https://data.worldbank.org/ World Bank Open Data. [cited 2022 Oct 29]. Available from:
- 21.Fiji Bureau of Statistics . 2018. 2017 Population and housing census release 1. Suva, Fiji. [Google Scholar]
- 22.World Health Organization Global health expenditure database [internet] https://apps.who.int/nha/database/Select/Indicators/en [cited 2022 Oct 29]. Available from:
- 23.Te Marae Ora . Te Marae Ora Cook Islands Ministry of Health; Rarotonga, Cook Islands: 2020. National health information bulletin 2019-2020. [Google Scholar]
- 24.Tonga Statistics Department . Nuku’alofa; Tonga: 2017. Tonga 2016 census of population and housing volume 1: basic tables and administrative report. [Google Scholar]
- 25.National Statistics Office . Vanuatu National Statistics Office; Port Vila, Vanuatu: 2021. National population and housing census 2020. Basic Tables Report vol. 1. [Google Scholar]
- 26.Sea Around Us Fisheries, ecosystems and biodiversity: exclusive economic zone (EEZ) [internet] http://www.seaaroundus.org/data/#/eez [cited 2023 May 9]. Available from:
- 27.World Atlas World Atlas [Internet] https://www.worldatlas.com/ [cited 2022 Oct 29]. Available from:
- 28.Roberts G., Wayne I., Tuiketei T., et al. The World Health Organization; Geneva, Switzerland: 2011. The Fiji islands health system review. [Google Scholar]
- 29.Asante A.D., Irava W., Limwattananon S., et al. Financing for universal health coverage in small island states: evidence from the Fiji Islands. BMJ Glob Health. 2017;2(2) doi: 10.1136/bmjgh-2016-000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO . World Health Organization; 2009. Definitions of health-care settings and other related terms. WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. [PubMed] [Google Scholar]
- 31.Global Initiative for Children’s Surgery Optimal resources for children's surgical care: executive summary. World J Surg. 2019;43(4):978–980. doi: 10.1007/s00268-018-04888-7. [DOI] [PubMed] [Google Scholar]
- 32.Debas H.T., Donkor P., Gawande A., Jamison D.T., Kruk M.E., Mock C.N., editors. Essential surgery: disease control priorities. World Bank; Washington (DC): 2015. Third Edition (Volume 1) [PubMed] [Google Scholar]
- 33.Lin Y., Raykar N.P., Saluja S., et al. Identifying essential components of surgical care delivery through quality improvement: an updated surgical assessment tool. Int J Surg. 2020;82:103–107. doi: 10.1016/j.ijsu.2020.08.002. [DOI] [PubMed] [Google Scholar]
- 34.Roa L., Moeller E., Fowler Z., et al. Assessment of surgical capacity in Chiapas, Mexico: a cross-sectional study of the public and private sector. BMJ Open. 2021;11(7) doi: 10.1136/bmjopen-2020-044160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adde H.A., van Duinen A.J., Oghogho M.D., et al. Impact of surgical infrastructure and personnel on volume and availability of essential surgical procedures in Liberia. BJS Open. 2020;4:1246–1255. doi: 10.1002/bjs5.50349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Watters D.A., McCaig E., Nagra S., Kevau I. Surgical training programmes in the South Pacific, Papua New Guinea and Timor leste. Br J Surg. 2019;106(2):e53–e61. doi: 10.1002/bjs.11057. [DOI] [PubMed] [Google Scholar]
- 37.Albutt K., Punchak M., Kayima P., Namanya D.B., Shrime M.G. Operative volume and surgical case distribution in Uganda's public sector: a stratified randomized evaluation of nationwide surgical capacity. BMC Health Serv Res. 2019;19(1):104. doi: 10.1186/s12913-019-3920-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Verguet S., Feldhaus I., Jiang Kwete X., et al. Health system modelling research: towards a whole-health-system perspective for identifying good value for money investments in health system strengthening. BMJ Glob Health. 2019;4(2) doi: 10.1136/bmjgh-2018-001311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Adam T., de Savigny D. Systems thinking for strengthening health systems in LMICs: need for a paradigm shift. Health Pol Plann. 2012;27(Suppl 4):1–3. doi: 10.1093/heapol/czs084. [DOI] [PubMed] [Google Scholar]
- 40.Epiu I., Tindimwebwa J.V.B., Mijumbi C., et al. Challenges of anesthesia in low- and middle-income countries: a cross-sectional survey of access to safe obstetric anesthesia in east africa. Anesth Analg. 2017;124(1):290–299. doi: 10.1213/ANE.0000000000001690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gajewski J., Pittalis C., Lavy C., et al. Anesthesia capacity of district-level hospitals in Malawi, Tanzania, and Zambia: a mixed-methods study. Anesth Analg. 2020;130(4) doi: 10.1213/ANE.0000000000004363. http://pubmed.ncbi.nlm.nih.gov/31453870/ [cited 2021 Oct 23] Available from: [DOI] [PubMed] [Google Scholar]
- 42.Stewart B.T., Gyedu A., Gaskill C., et al. Exploring the relationship between surgical capacity and output in Ghana: current capacity assessments may not tell the whole story. World J Surg. 2018;42(10):3065–3074. doi: 10.1007/s00268-018-4589-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frenk J. The global health system: strengthening national health systems as the next step for global progress. PLoS Med. 2010;7(1) doi: 10.1371/journal.pmed.1000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.