Abstract
Introduction
Patellar instability can arise from a traumatic event with anatomical predisposing factors increasing the risk of dislocation. Accurate diagnosis is required to initiate appropriate treatment. We aimed to evaluate the patella apprehension test (PAT) as a method to diagnose patellar instability.
Methods
The PRISMA diagnostic test accuracy checklist was followed. The review protocol was registered on PROSPERO with registration number CRD42022357898. Electronic databases, currently registered studies, conference proceedings and the reference lists of included studies were searched. A narrative synthesis evaluated the validity of the PAT as a method of diagnosing patellar instability.
Results
A total of 4867 records were screened in the initial search. Of these, 34 articles satisfied the inclusion criteria, assessing 1139 knees of 1046 patients. The PAT was found to have a high sensitivity and specificity. Its intra and inter-rater reliability was highly variable among studies. Studies reporting patellar instability correction following surgery also found a decrease in the number of patients exhibiting a positive PAT.
Conclusion
Current evidence suggests that the PAT has a high sensitivity and specificity. The intra- and inter-rater validities of the PAT are widely variable due to its subjective nature. Thus, though the PAT can be used to provide a provisional clinical diagnosis of patellar instability, formal functional assessment and imaging should be performed to confirm the diagnosis. Further research should explore the association between a positive PAT and anatomical parameters. In addition, studies comparing the accuracy of the PAT and radiological investigations should be performed.
Keywords: Patella apprehension test, Patellar instability, Systematic review
Abbreviations
- PAT
patella apprehension test
- MPFL:
medial patellofemoral ligament
- CT
computerized tomography
- EFORT
European federation of national associations of Orthopaedics and traumatology
- AQUA
anatomical quality assessment
- MPFLR
medial patellofemoral ligament reconstruction
- MPAT
modified version of the patella apprehension test
- RDPAT
reversed dynamic patella apprehension test
- TT-TG
tibial tuberosity – tibial groove
- TT – PCL
tibial tuberosity – posterior cruciate ligament
- VAS
visual analogue scale
- BPII 2.0
Banff Patellofemoral Instability Score 2.0
1. Introduction
Patellar instability can lead to patellar dislocation, which accounts for 2–3% of injuries of the knee joint.1 Its incidence is 6 in every 100,000 patients per year.2 This can lead to femoral condyle contusion, knee effusion, and rupture of the medial patellofemoral ligament (MPFL).1,3 The latter can result in tearing of the medial retinaculum.1 Recurrent dislocations occur in 15%–44% of patients who experience an initial patellar dislocation.4 In addition, 58% of patients note limitations when carrying out strenuous activity six months after the injury. Other symptoms include severe knee pain, swelling, and the inability to run.5
The PAT is used in clinical practice to diagnose patella instability. It was first described by Ferrari et al., who performed the PAT with the patient standing.6 The test is considered positive if the patient reports apprehension or instability during internal rotation of the torso. However, in current clinical practice, the PAT is more commonly performed with the patient lying supine. Firm pressure is applied to the medial border of the patella in an extended and relaxed knee. A positive finding occurs when the patient expresses apprehension that the patella will dislocate,7 with instability or discomfort being reported.8 A correct identification of patellar instability is required to initiate any of the appropriate treatment strategies. These range from conservative approaches like closed reduction and rehabilitation, to surgical interventions like lateral retinacular release and osteotomy.7
Adequate identification of patellar instability through physical examination is required, since radiological studies may be insensitive in the non-acute setting. Radiographs and computerized tomography (CT) scans are static, and may not help visualize a dislocated patella.9 The PAT is widely used in clinical practice. Considering this, its validity should be formally assessed to determine whether its common use is justified. A previous review, conducted in 2008, revealed the validity of the PAT was unclear.10 Articles published since the previous study were therefore evaluated to determine an accurate and updated assessment of the validity of the PAT. The aim of this systematic review was therefore to determine whether the PAT is a valid way of diagnosing patellar instability.
2. Methods
We aimed to determine whether the PAT is a valid way of diagnosing patellar instability. The PRISMA diagnostic test accuracy checklist was followed.11 The protocol for this review was registered on PROSPERO with registration number CRD42022357898.
2.1. Study eligibility
Study eligibility was determined by following the pre-specified criteria. All studies reporting on results of the PAT both before and after intervention (conservative or surgical) were included, as well as those assessing its validity or reliability. Papers not reporting original data such as literature or systematic reviews were excluded, along with case reports, animal studies, cadaveric studies and letters to the editor. Studies describing theoretical models, studies not reporting on PAT outcomes, and studies in which the PAT was not performed pre- and post-operatively were also excluded. There were no language or publication status constraints.
2.2. Search strategy and data extraction
We searched the following electronic databases from their inception to 06/09/2022: MEDLINE, Embase, CINAHL, the Cochrane Library, PEDro, and AMED. Study registries, including the ISRCTN registry, the UK National Research Register Archive, the WHO International Clinical Trials Registry Platform, OpenSIGLE, and the National Institute for Health Research Portfolio were reviewed. Conference proceedings from the European federation of national associations of Orthopaedics and traumatology (EFORT), British Orthopaedic Association and British Trauma Society were searched. The reference lists of included studies were also searched.
Database search was conducted independently by three reviewers. Reviewers screened records independently. Disagreements regarding study eligibility were solved by discussion. The first search was first conducted on 17/11/2021, and repeated on 06/09/2022. The search strategy is attached (Appendix A). Data extraction was conducted by the first author.
2.3. Methodological appraisal
Two reviewers independently evaluated the level of evidence and risk of bias of each study. The level of evidence of the studies presented was determined with the Oxford CEBM: Levels of Evidence.12 The Cochrane Collaboration's tool for Non-Randomized Studies was used to perform a risk of bias assessment for non-randomized interventional studies.13 The IHE case series quality appraisal checklist was used to assess risk of bias in interventional case series.14 The AQUA tool was used to assess risk of bias in non-interventional anatomical studies.15
2.4. Data synthesis strategy
Quantitative pooled analysis was prevented by the heterogeneity of the data in terms of interventions performed, outcomes evaluated, and approach to the PAT. Therefore, a narrative synthesis was performed. Number of patients and knees, follow-up duration, mean patient age. and degree of patellar instability were extracted. In addition, intervention performed, stability scores, pre- and post-operative PAT (positive or negative), and stability outcomes were presented in Table 2.
Table 2.
Stability and PAT outcomes following different surgical interventions.
| Study | Intervention | Pre-operative patella stability score | Post-operative patella stability score | Pre-operative PAT | Post-operative PAT | Stability outcomes |
|---|---|---|---|---|---|---|
| Malecki et al., 201628 | Group 1: MPFL reconstruction Group 2: Combination of: retinacular plasty, vastus medialis advancement, and Roux-Goldthwait procedure |
NR | Group 1: Kujala score: 90.8 Lysholm score: 89.8 Group 2: Kujala score: 85 Lysholm score: 84.2 |
All patients had a positive PAT pre-operatively | 6 patients in group 1 (19%) and 6 in group 2 (18%) noted a positive PAT | Group 1: 3 dislocations noted Group 2: 4 dislocations noted |
| Leite et al., 202132 | Tibial tubercle osteotomy with concomitant distalization and MPFL reconstruction | Kujala score: 52 | Kujala score: 77 | All patients had a positive PAT pre-operatively | All patients had a negative PAT pre-operatively | J-sign improved in 30 cases (97%). One case (3%) of recurrent instability was reported |
| Sadigursky et al., 201733 | MPFL and medial patellotibial ligament reconstruction | Kujala score: 42.57 Lysholm score: 33.71 |
Kujala score: 88.57 Lysholm score: 87.71 |
All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | J-sign was noted in 6 patients pre-operatively (85.7%), compared to 1 post-operatively (14.3%) |
| Akgün et al., 201020 | Fulkerson osteotomy | NR | Kujala score: 82.6 | All patients had a positive PAT pre-operatively | PAT was negative in 14 knees (82.4%), and positive in three (17.6%) | Subluxation was noted in 2 knees (11.8%). Patellar tilt and subluxation were corrected in all but two knees. |
| Wang et al., 201049 | Group 1 (MPFLR): 28 Group 2 (MPFLR and vastus medialis advancement): 41 |
Kujala score: Group 1: 51.3 Group 2: 53.7 |
Kujala score: Group 1: 79.9 Group 2: 83.9 |
All patients had a positive PAT pre-operatively | Group 1: 20 had a negative PAT (71.4%) Group 2: 38 had a negative PAT (92.7%) |
Recurrent dislocation was not reported in any patient post-operatively |
| Torkaman et al., 201535 | MPFLR | Kujala score: 59.8 | Kujala score: 88.6 | All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | NR |
| Xu and Zhao, 201121 | Arthroscopic medial retinaculum plication | Kujala score: 66.7 Lysholm score: 52.6 |
Kujala score: 76.6 Lysholm score: 70.7 |
All patients had a positive PAT pre-operatively. | At 2 years follow-up, 12 demonstrated a positive PAT (42.9%). | Six patients suffered from redislocation (21.4%), and 23 patients experienced patella instability (82.1%). |
| Ma et al., 201216 | Group 1: Medial capsule reefing Group 2: Medial patellar retinaculum plasty |
Kujala score: Group 1: 52.3 Group 2: 53.5 |
Kujala score: Group 1: 78.1 Group 2: 82.2 |
All patients had a positive PAT pre-operatively | Group 1: 20 patients had a negative PAT (68.9%) Group 2: 30 patients had a negative PAT (93.8%) |
Medial retinacular plasty was better than medial capsule reefing in decreasing the rate of patellar dislocation |
| Fink et al., 201436 | MPFLR | Kujala score: NR Lysholm score: 69.5 |
Kujala score: 89.2 Lysholm score: 88.1 |
All patients had a positive PAT pre-operatively | Fifteen patients had a negative PAT (88.2%) | No dislocation during the follow-up period |
| Song et al., 201437 | MPFLR | Kujala score: 52.6 Lysholm score: 49.2 |
Kujala score: 90.9 Lysholm score: 90.9 |
All patients had a positive PAT pre-operatively | Nineteen patients had a negative PAT (95%) | No patient experience a redislocation |
| Ellera Gomes et al., 200438 | MPFLR | NR | NR | All patients had a positive PAT pre-operatively | Fifteen patients had a negative PAT (93.8%) | Patellar tracking was normal in 14 knees (87.5%) |
| Ntagiopoulos et al., 201339 | Sulcus-deepening trochleoplasty | Kujala score: 59 | Kujala score: 87 | PAT was positive in 30 knees (96.7%) | PAT was positive in 6 knees (19.4%) PAT was negative in 25 knees (80.6%) |
No recurrence was observed |
| Beckert et al., 201640 | Lateral patellofemoral ligament reconstruction | NR | NR | All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No recurrence of patellar instability was observed |
| Calanna et al., 201641 | MPFLR | Kujala score: 65.2 Lysholm score: 64.3 |
Kujala score: 94.7 Lysholm score: 94.7 |
PAT was positive in 17 patients (89%) | PAT was positive in 2 cases (11%) | No recurrence of patellar dislocation was reported |
| Fadel and Hosni, 202027 | MPFLR | Kujala score: 69.5 | Kujala score: 94.8 | All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No recurrence of patellar dislocation was reported |
| Yang et al., 201723 | MPFLR | NR | NR | All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No recurrence of patellar dislocation was reported |
| Watanabe et al., 200819 | Group 1: MPFLR Group 2: MPFLR + tibial tubercle transfer |
Lysholm score: Group 1: 70 Group 2: 72 |
Lysholm score: Group 1: 92 Group 2: 90 |
Group 1: 28 had a positive PAT (97%) Group 2: 11 had a positive PAT (92%) |
Group 1: 6 had a positive PAT (21%) Group 2: 4 had a positive PAT (31%) |
NR |
| Elbarbary et al., 202042 | MPFLR | Tegner-Lysholm score: 63 | Tegner-Lysholm score: 89.2 | All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No redislocations were reported |
| Kang et al., 201443 | MPFLR | Kujala score: 52.4 Lysholm score: 51.8 |
Kujala score: 90.9 Lysholm score: 91.7 |
All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No redislocations were reported |
| Niu et al., 201726 | MPFLR | Kujala score: 58.9 Lysholm score: 53.3 |
Kujala score: 92 Lysholm score: 91.6 |
All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No redislocations were reported |
| Chen et al., 201522 | Tibial tubercle internal rotation | Kujala score: 56.9 Lysholm score: 51.6 |
Kujala score: 89.0 Lysholm score: 89.0 |
All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No redislocations were reported |
| Li et al., 201817 | Lateral retinacular release and MPFLR | Lysholm score: 68.3 | Lysholm score: 92.9 | All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No redislocations were reported |
| Camathias et al., 201644 | Trochleoplasty | Kujala score: 71 | Kujala score: 92 | Positive PAT in 41 knees (82%) | Positive PAT in 8 knees (16%) | One patella dislocated post-operatively (2%) |
| Mochizuki et al., 201918 | MPFLR | Kujala score: 50.9 | Kujala score: 93.7 | All patients had a positive PAT pre-operatively | One patient had a positive PAT (4.2%) | No redislocations were reported |
| Mahmoud et al., 202145 | MPFLR | Lysholm score: 59 | Lysholm score: 80.2 | All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No redislocations were reported |
| Kumahashi et al., 201646 | MPFLR | Kujala score: 72.2 Lysholm score: 67.8 |
Kujala score: 96.4 Lysholm score: 96.2 |
All patients had a positive PAT pre-operatively | One patient had a positive PAT post-operatively (5.9%) | No redislocations were reported |
| Kumahashi et al., 201229 | MPFLR | Kujala score: 67.4 Lysholm score: 64.4 |
Kujala score: 95.4 Lysholm score: 96.0 |
All patients had a positive PAT pre-operatively | All patients had a negative PAT post-operatively | No redislocations were reported |
| Schöttle et al. 200547 | MPFLR | Kujala score: 53.3 | Kujala score: 85.7 | Fourteen knees had a positive PAT (93%) | Three knees remained with a positive PAT (20%) | 86.7% reported to recurrent instability |
| Kita et al., 201248 | MPFLR | Kujala score: 73 | Kujala score: 95 | All patients had a positive PAT pre-operatively | 22 knees had a negative PAT (88%) | Patellar maltracking was corrected in all patients |
3. Results
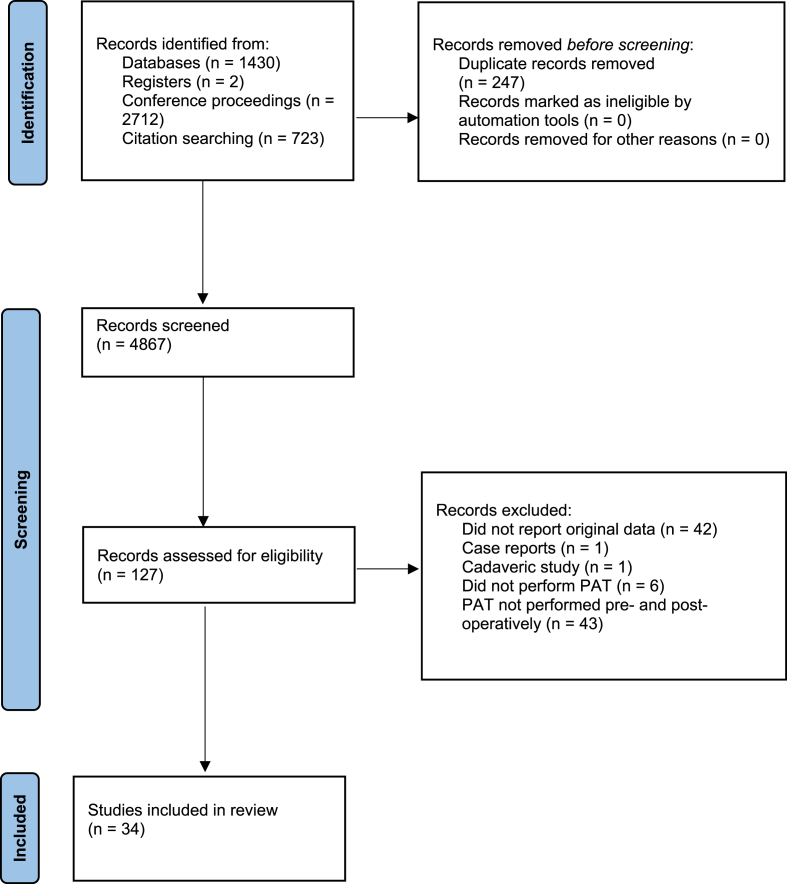
A total of 4867 records were screened, with 127 potentially eligible articles identified (Fig. 1). Ninety-three articles were excluded based on the pre-specified exclusion criteria. Thirty-four studies were included, evaluating 1139 knees of 1046 patients. Table 1 depicts subjects’ baseline characteristics. Thirty studies reported on patients with recurrent patellar instability (2 or more episodes). In two studies it was unclear whether patellar instability was recurrent or acute.16,17 Ahmad et al. used the PAT to diagnose instability in patients for which this was suspected.9 Mochizuki et al. did not report outcomes separately for patients with first time and recurrent patellar dislocations.18
Fig. 1.
PRISMA diagram depicting the study collection process.
Table 1.
Level of evidence, risk of bias, and baseline characteristics of studies included.
| Study | Study design, level of evidence | Risk of bias | Number of patients (males, females) | Number of knees | Mean patient age (years) | Follow-up duration |
|---|---|---|---|---|---|---|
| Malecki et al., 201628 | Case control, 3 | Some concerns | 56 (12, 44) | Group 1: 32 | 14 | 5.6 years |
| Group 2: 33 | ||||||
| Leite et al., 202132 | Case series, 4 | Some concerns | 25 (3, 22) | 31 | 28.7 | 2.62 years |
| Sadigursky et al., 201733 | Case series, 4 | Some concerns | 7 (4, 3) | 7 | 11.28 | 1 year |
| Akgün et al., 201020 | Case series, 4 | NFT | 16 (11, 5) | 17 | 25 | 2.6 years |
| Ahmad et al., 20099 | Non-interventional anatomical study, 2b | Low | 51 (24, 27) | 51 | 24.2 | NA |
| Hiemstra et al., 202131 | Case series, 4 | Some concerns | 38 (11, 27) | 76 | 24.7 | NA |
| Zimmermann et al., 201930 | Non-interventional anatomical study, 2b | Low | RDPAT: 78 (35, 43) | 113 | RDPAT: 22 | NA |
| Control: 35 (16, 19) | Control: 31 | |||||
| Wang et al., 201034 | Case series, 4 | Some concerns | Group 1: 28 (10, 18) | 69 | Group 1: 29 | 3.5 years |
| Group 2: 41 (20, 21) | Group 2: 31 | |||||
| Torkaman et al., 201535 | Case series, 4 | Some concerns | 15 (6, 9) | 15 | 26.5 | 1 year |
| Xu and Zhao, 201121 | Case series, 4 | NFT | 28 (5, 23) | 28 | 14.7 | 4.8 years |
| Ma et al., 201216 | Cohort study, 2b | Some concerns | Group 1: 29 (13, 16) | Group 1: 29 | Group 1: 13 | 50 months |
| Group 2: 32 (12, 20) | Group 2: 32 | Group 2: 14 | ||||
| Fink et al., 201436 | Case series, 4 | Some concerns | 17 (7, 10) | 17 | 21.5 | 12 months |
| Smith et al., 201225 | Case series, 4 | Low | 5 (0, 5) | 10 | 26.6 | NA |
| Song et al., 201437 | Case series, 4 | Some concerns | 20 (10, 10) | 20 | 21 | 34.5 months |
| Ellera Gomes et al., 200438 | Case series, 4 | Some concerns | 15 (4, 11) | 16 | 26.7 | 5 years |
| Ntagiopoulos et al., 201339 | Case series, 4 | Some concerns | 27 (14, 13) | 31 | 21 | 7 years |
| Beckert et al., 201640 | Case series, 4 | Some concerns | 17 | 19 (18, 1) | 29.5 | 2 years |
| Calanna et al., 201641 | Case series, 4 | Some concerns | 19 (12, 7) | 19 | 25.5 | 22 months |
| Fadel and Hosni, 202027 | Case series, 4 | Low | 34 (5, 29) | 34 | 19.4 | 28.7 months |
| Yang et al., 201723 | Case series, 4 | NFT | 12 | 12 | NR | 16.4 months |
| Watanabe et al., 200819 | Case series, 4 | NFT | 40 | Group 1: 29 | NR | 4.3 years |
| Group 2: 13 | ||||||
| Elbarbary et al., 202042 | Case series, 4 | Some concerns | 7 (2, 5) | 7 | 23.7 | 18.8 months |
| Kang et al., 201443 | Case series, 4 | Some concerns | 45 (18, 27) | 45 | 26.6 | 33.7 months |
| Niu et al., 201726 | Case series, 4 | Low | 30 (10, 20) | 30 | 25 | 4 years |
| Chen et al., 201522 | Case series, 4 | NFT | 28 (4, 24) | 28 | 21.8 | 41.8 months |
| Li et al., 201817 | Case series, 4 | NFT | 28 (6, 22) | 32 | 21 | 6 months |
| Camathias et al., 201644 | Case series, 4 | Some concerns | 44 (14, 30) | 50 | 15.6 | 2 years |
| Mochizuki et al., 201918 | Case series, 4 | Some concerns | 24 (6, 18) | 24 | 25.4 | 2 years |
| Mahmoud et al., 202145 | Case series, 4 | Some concerns | 10 | 10 | 26 | 19.4 months |
| Kumahashi et al., 201646 | Cohort study, 2b | Some concerns | 15 (3, 12) | 17 | 22 | 45 months |
| Hiemstra et al., 202124 | Case series, 4 | High | 89 | 98 | NR | 2 years |
| Kumahashi et al., 201229 | Case series, 4 | Some concerns | 5 (2, 3) | 5 | 13.6 | 27.8 months |
| Schöttle et al. 200547 | Case series, 4 | Some concerns | 12 (4, 8) | 15 | 30.1 | 47 months |
| Kita et al., 201248 | Case series, 4 | Some concerns | 24 (6, 18) | 25 | 22.7 | 13.2 months |
3.1. Study quality assessment
The findings of the study quality assessment are presented in Table 1. Of the 34 studies included, 29 were case series. These carry a low level of evidence of 4. Risk of bias of six case series could not be assessed due to these being non-full text studies.17,19, 20, 21, 22, 23 Risk of bias was deemed high in one case series due to missing details of patient demographics.24 Only three case series carried a low risk of bias.25, 26, 27 There were some concerns regarding the risk of bias in the remaining 19 case series due to their retrospective nature and being performed in a single center.
Five non-randomized comparative studies were included. These comprised a case control study and four cohort studies. The case control study28 and two cohort studies16,29 carried some concerns regarding their risk of bias due to lack of blinding of assessors.28 Two cohort studies carried a low risk of bias.9,30 Overall, the majority of studies included in this review exhibited methodological limitations in terms of study design and risk of bias (Table 1).
3.2. The PAT as a measure of post-operative patella stability
A total of 29 studies utilized the PAT to assess pre- and post-operative patellar stability. Intervention, stability scores, pre- and post-operative PAT and stability outcomes are presented in Table 2. Symptom scores used in the studies included are detailed in Appendix B. Medial patellofemoral ligament reconstruction (MPFLR) comprised the majority of surgical interventions. None of the 29 studies analyzed the relationship between PAT outcomes and patient demographics, anatomical or radiological characteristics. No study reported outcomes in patients with and without a positive PAT separately.
All studies reporting on stability scores reported an improvement from baseline, and a decrease in patients with patellar instability post-operatively. All studies reported a reduction in patients with a positive PAT following surgery aimed at correcting patellar instability. Thirteen studies reported that every patient exhibiting a positive PAT pre-operatively communicated a negative PAT post-operatively. Of the eleven studies which did not, percentage of patients with a positive PAT post-operatively ranged from 4.2% to 42.9%. Five studies reported a high percentage of patients with a positive PAT pre-operatively, instead of the entire population (range: 82%–97%). Number of patients with a positive PAT post-operatively decreased in all of these five studies (range: 11%–21%).
3.3. The reliability, validity, and accuracy of the PAT
Ahmad et al. described a new version of the PAT (MPAT) on 51 knees.9 The patella is laterally translated while the patient lies supine. The knee is then flexed to 90° and brought back to extension. For the second part, the knee is flexed to 90°, and then extended fully while translating the patella medially. For the MPAT to be considered positive, apprehension must occur during part 1, but not part 2. The MPAT was performed pre-operatively and during knee examination under anaesthesia in 51 patients. The MPAT during examination under anaesthesia was considered the gold standard to diagnose patellar instability. For the detection of patellar instability, the pre-operative MPAT had an accuracy of 94.1%, 100% sensitivity, 88.4% specificity, a negative predictive value of 100%, and a positive predictive value of 89.2%,
Hiemstra et al. measured the inter-rater reliability of the PAT in 38 patients with patellofemoral instability.31 Knees were assessed bilaterally by two orthopedic surgeons. The PAT demonstrated fair to substantial reliability (intraclass correlation coefficient was 0.30 for left knees, and 0.65 for right knees). Both surgeons agreed on the PAT status in 27 right knees (71.1%), and 28 left knees (73.7%), indicating moderate to substantial agreement. In addition, evaluation of the PAT in terms of reactions to the test (including verbal, withdrawal, reflex, and physiological) demonstrated good consistency between the two examiners.
Smith et al. assessed the intra- and inter-rater reliability of the PAT.25 Five patients were assessed by five consultant Orthopaedic surgeons. The lateral PAT at 0° and 30° demonstrated fair intra-rater reliability (Kappa statistic 0.32 and 0.27, respectively), whereas the medial PAT at 30° knee flexion demonstrated moderate intra-rater reliability (Kappa statistic 0.50). There was slight inter-rater reliability of the PAT at full knee extension (Kappa statistic 0.19), and no inter-rater reliability for the medial and lateral PAT at 30° (Kappa statistic −0.19 and −0.01, respectively).
Zimmermann et al. performed the reversed dynamic PAT (RDPAT) in 78 subjects with recurrent patellar dislocations, and in 35 controls.30 During the RDPAT, the patient lies supine, and the knee is brought to extension from 120°, while the patella is translated laterally. The RDPAT is considered positive if apprehension occurs. Seventy-four subjects with recurrent dislocations (94.9%) had a positive RDPAT, whereas 30 control patients (85.7%) had a negative RDPAT. Its specificity was 88.2%, sensitivity 93.7%, negative predictive value was 85.7%, while positive predictive values was 94.9%. Intra- and inter-rater reliability of the RDPAT were 0.85 and 0.84, respectively. In addition, the correlation of a positive RDPAT with patellar instability risk factors was calculated. A positive RDPAT correlated significantly with trochlear dysplasia (p = 0.018) and valgus deformity (p = 0.011). A positive RDPAT did not demonstrate significant correlation with tibial tuberosity – tibial groove (TT – TG) or TT – posterior cruciate ligament (TT – PCL) distances, nor patellar height (p > 0.05).
Hiemstra et al. performed MPFLR in 89 patients to assess the reliability of the PAT.24 Apprehension as rated by patient and surgeon were rated on a visual analogue scale (VAS). This was performed at 0° and 30° knee flexion. This was assessed by a single surgeon and his/her patients. Pre-operatively, 81 (91%) and 84 (94.4%) had a positive PAT at 0° and 30° degrees of flexion. This changed to 39 (43.8%) and 36 (40.4%), respectively. The Banff Patellofemoral Instability Score 2.0 (BPII 2.0) improved from a mean of 27.6 before the operation to 74.3 after it. Three subjects experienced a patellar dislocation postoperatively. The surgeon-rated and patient-rated PAT score on the VAS decreased from 5.30 and 6.80 pre-operatively to 1.87 and 2.36, respectively, at 0° knee flexion. At 30°, these decreased from 5.16 and 6.82 pre-operatively to 1.95 and 2.00 as rated by the surgeon and patients, respectively. Pre-operatively, the inter-rater reliability between the surgeon and patients was moderate at 0° (r = 0.60) and weak at 30° (r = 0.42). Post-operatively, there was strong inter-rater reliability in extension (r = 0.74) and 30° flexion (r = 0.73). There was a statistically significant negative correlation between patient-rated apprehension in the VAS and the BPII 2.0 score at 0° knee flexion (r = −0.35, P = 0.001), with less residual apprehension correlating with higher BPII 2.0 scores. This was not the case for 30° of flexion (r = −0.20, P = 0.054). There was no correlation between postoperative patient-rated apprehension in the VAS with ligamentous laxity, patella alta, trochlear dysplasia, WARPS-STAID classification, or age at first dislocation.
4. Discussion
A previous systematic review revealed the validity of the PAT was unclear.10 This review included studies published since, providing further insight on the validity of this test. Current evidence suggests that the PAT is a valid test to provide a provisional clinical diagnosis of patellar instability. Two studies found it had a high sensitivity, specificity, positive and negative predictive values.9,30 However, these comprised a total of 164 patients. Further study evaluating the accuracy of the PAT are required to ascertain its validity. There is conflicting evidence regarding the intra and inter-rater reliability of the PAT. Four studies assessed these, with results varying widely. Hiemstra et al. found fair to substantial inter-rater reliability,31 Zimmermann et al. found strong intra- and inter-rater reliability,30 whereas Hiemstra et al. found weak to moderate inter-rater reliability pre-operatively, and a strong reliability post-operatively.24 In addition, Smith et al. demonstrated fair to moderate intra-rater reliability pre-operatively, and none to slight inter-rater reliability post-operatively.25 Such variability in results can be attributed to differing sample sizes and approaches to performing the PAT. In addition, the PAT is a subjective test, with its results depending heavily on the assessor. This could explain discrepancies in findings between individuals. Therefore, the inter-rater and intra-rater reliability of the PAT are likely to widely vary. Considering this, though the PAT can be used to provide a provisional clinical diagnosis of patellar instability, the PAT alone cannot be used to confirm the diagnosis of recurrent patellar instability. Multiple tests and investigations are required to do so, including functional assessment with validated scoring tools and imaging.
It is not possible to reliably establish if there is an association between a positive PAT and radiological or anatomical features with current evidence. This is because, of the 34 included studies, only two reported on these parameters, and had discrepancies in terms of factors evaluated and findings.24,30 There are insufficient studies exploring the association between a positive PAT and anatomical features. Further research exploring radiological/anatomical features of a positive PAT is required.
Twenty-nine studies utilized the PAT to assess pre- and post-operative patellar stability. All studies reported an increase in stability scores from baseline, and a reduction in subjects exhibiting patellar instability post-operatively. Every study reported a reduced number of subjects communicating a positive PAT post-operatively. This suggests that the PAT is a valid method of assessing patellar stability, since the PAT was negative following surgery aimed at correcting instability. However, no studies reported outcomes separately in patients with and without a positive PAT. In addition, no direct numerical correlation between PAT and stability scores was established, which decreases the validity of this conclusion.
This review identified areas of further research that could further the understanding of the validity of the PAT. Firstly, there is insufficient stratification of outcomes according to anatomical parameters and patient demographics. Exploring the relationship between risk factors for patellar dislocation and PAT outcomes could help determine with more certainty whether this test is a valid method of diagnosing patellar instability. Secondly, no studies comparing the accuracy of the PAT and radiological investigations were identified. The PAT is cheaper given the lack of equipment requirements, and renders an immediate outcome. This is in contrast to imaging, which requires a trained practitioner to perform and evaluate the test, and takes a longer time to convey results. Further research comparing the PAT and radiological investigations could help determine which is a more cost-effective way of diagnosing patellar instability.
Current evidence has limitations that must be improved upon to more reliably ascertain the validity of the PAT. Firstly, there is a lack of a standardized approach to performing the PAT in current literature. It is possible a study's results could be affected if a different variation of the PAT were performed. Furthermore, the lack of a standardized approach to the PAT hinders the generalization of this review's results, since they may not be applicable to all versions of the test. Secondly, no study reported outcomes in patients with and without a positive PAT separately. Therefore, there is a lack of a direct numerical correlation of the PAT to patella stability. This hinders the claim that the PAT is a valid way of assessing patella stability, and impedes the performance of meta-analyses on the subject, which limits the review process. Thirdly, no studies compared the pre-op and post-op sensitivity of the PAT, and only two studies reported the exact point at follow-up in which the PAT was assessed (at one year post-op).35,36 Further study should aim to evaluate these parameters to ascertain whether the PAT is valid both before and after surgery, and to establish the point during follow-up in which the PAT can be reliably used. Finally, the majority of studies included carried a low level of evidence and concerns regarding their risk of bias. This must be taken into consideration when evaluating any conclusions drawn.
5. Conclusion
Current evidence suggests that the PAT has a high sensitivity and specificity. The intra- and inter-rater validities of the PAT are widely variable due to its subjective nature. Considering this, though the PAT can be used to provide a provisional diagnosis of patellar instability, the PAT alone cannot be used to confirm the diagnosis of recurrent patellar instability. Multiple tests and investigations are required to do so, including functional assessment with validated scoring tools and imaging. Further research should explore the association between a positive PAT and anatomical parameters under imaging. In addition, studies comparing the accuracy of the PAT and radiological investigations should be performed. The reliability of any conclusions drawn are hindered by limitations of current evidence. These include lack of a standardized approach to performing the PAT, not reporting surgical outcomes according to whether the test result was positive, and the lack of a comparison of PAT validity before and after surgery.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Informed consent
Not applicable.
Institutional ethical committee approval
Not applicable.
Author statement
Diego Agustín Abelleyra Lastoria: Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – Original draft preparation, Literature search, Data extraction, Risk of Bias Assessment Bethany Kenny: Investigation, Methodology, Literature Search, Risk of Bias Assessment Sara Dardak: Conceptualization, Investigation, Methodology, Literature search Charlotte Brookes: Conceptualization, Investigation, Methodology, Literature search Caroline Hing: Conceptualization, Methodology, Project Administration, Supervision, Writing – Review and Editing.
Declaration of competing interest
None.
Acknowledgement
None.
Appendix A. search strategy
-
1.
Patell*.tw,kf.
-
2.
Patella/
-
3.
Patellofemoral joint/
-
4.
Knee*.tw,kf.
-
5.
Knee joint/
-
6.
1 or 2 or 3 or 4 or 5
-
7.
(dislocat* or sublux* or instability).tw,kf.
-
8.
Joint Dislocations/
-
9.
Joint Instability/
-
10.
Knee dislocation/
-
11.
Knee Injuries/
-
12.
7 or 8 or 9 or 10 or 11
-
13.
(apprehension and test).af.
-
14.
*Physical Examination/
-
15.
13 or 14
-
16.
6 and 12 and 15
Appendix B. scoring systems mentioned in this review
Tegner-Lysholm/Lysholm score50
| Parameter | Score |
|---|---|
| Modified Lysholm limp (5 points) | None = 5. Slightly or periodically = 3. Severe or constant = 0. |
| Support (5 points) | None = 5. Limp = 2. Weight-bearing impossible = 0. |
| Locking (15 points) | No locking or crepitation sensation = 15. “Catching” sensation but no locking sensation = 10. Occasional locking = 6. Frequently = 2. Locked joint on examination = 0. |
| Instability (25 points) | Has never presented buckling = 25. Rarely during sports activities or other exertion = 20. Frequently during sports activities or other exertion = 15. Occasionally in daily living activities = 10. Frequently in daily living activities = 5. With every step = 0. |
| Pain (25 points) | None = 25. Inconstant and slight during severe exertion = 20. Marked during severe exertion = 15. Marked on or after walking 2 km or more = 10. Marked on or after walking less than 2 km = 5. Constant = 0. |
| Joint effusion/swelling (10 points) | None = 10. On severe exertion = 6. On slight exertion = 2. Constant = 0. |
| Stair climbing (10 points) | No problem = 10. Slightly impaired = 6. Step by step (one stair at a time) = 2. Impossible = 0. |
| Squatting (5 points) | No problem = 5. Slightly impaired = 4. Up to 90° = 2. Impossible = 0. |
| Total score is out of 100 (100 being the highest possible score): | |
| Excellent: 91-100 | |
| Good: 84-90 | |
| Fair: 65-83 | |
| Poor: ≤64 | |
Kujala score51
| Parameter | Score |
|---|---|
| Limp (5 points) | None = 5. Slightly or periodically = 3. Constant = 0. |
| Support (5 points) | Full support without pain = 5. Painful = 3. Weight-bearing impossible = 0. |
| Walking (5 points) | Unlimited = 5. More than 2 km = 3. 1–2 km = 2. Unable = 0. |
| Stairs (10 points) | No difficulty = 10. Slight pain when descending = 8. Pain both when descending and ascending = 5. Unable = 0. |
| Squatting (5 points) | No difficulty = 5. Repeated squatting painful = 4. Painful each time = 3. Possible with partial weight bearing = 2. Unable = 0. |
| Running (10 points) | No difficulty = 10. Pain after more than 2 km = 8. Slight pain from start = 6. Severe pain = 3. Unable = 0. |
| Jumping (10 points) | No difficulty = 10. Slight difficulty = 7. Constant pain = 2. Unable = 0. |
| Prolonged sitting with the knees flexed (10 points) | No difficulty = 10. Pain after exercise = 8. Constant pain = 6. Pain forces to extend knees temporarily = 4. Unable = 0. |
| Pain (10 points) | None = 10. Slight and occasional (8). Interferes with sleep = 6. Occasionally severe = 3. Constant and severe = 0. |
| Swelling (10 points) | None = 10. After severe exertion = 8. After daily activities = 6. Every evening = 4. Constant = 0. |
| Abnormal painful patellar movements (10 points) | None = 10. Occasionally in sports activities = 6. Occasionally in daily activities = 4. At least one documented dislocation = 2 points. More than two dislocations = 0. |
| Atrophy of thigh (5 points) | None = 5. Slight = 3. Severe = 0. |
| Flexion deficiency (5 points) | None = 5. Slight = 3. Severe = 0. |
| Total score is out of 100 (100 being the highest possible score). | |
References
- 1.Petri M., Ettinger M., Stuebig T., et al. Current concepts for patellar dislocation. Arch Traum Res. 2015;4(3) doi: 10.5812/atr.29301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krebs C., Tranovich M., Andrews K., Ebraheim N. The medial patellofemoral ligament: review of the literature. J Orthop. 2018;15(2):596–599. doi: 10.1016/j.jor.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirsch M.D., Fitzgerald S.W., Friedman H., Rogers L.F. Transient lateral patellar dislocation: diagnosis with MR imaging. Am J Roentgenol. 1993;161:109–113. doi: 10.2214/ajr.161.1.8517287. [DOI] [PubMed] [Google Scholar]
- 4.Neel P.J., Khan N., Fithian D.C. A treatment algorithm for primary patellar dislocations. Sport Health. 2011;3(2):170–174. doi: 10.1177/1941738111399237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atkin D.M., Fithian D.C., Marangi K.S., Stone M.L., Dobson B.E., Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 Months of injury. Am J Sports Med. 2000;28(4):472–479. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari D.A., Ferrari J.D., Coumas J. Posterolateral instability of the knee. J Bone Joint Surg Br. 1994;76(2):187–192. [PubMed] [Google Scholar]
- 7.Cosgarea A.J., Browne J.A., Kim T.K., McFarland E.G. Evaluation and management of the unstable patella. Physiother Sport. 2002;30(10):33–40. doi: 10.3810/psm.2002.10.492. [DOI] [PubMed] [Google Scholar]
- 8.Heyworth B.E., Carroll K.M., Dawson C.K., Gill T.J. Open lateral retinacular closure surgery for treatment of anterolateral knee pain and disability after arthroscopic lateral retinacular disease. Am J Sports Med. 2012;40(2):376–382. doi: 10.1177/0363546511428600. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad C.S., McCarthy M., Gomez J.A., Shubin Stein B.E. The moving patellar apprehension test for lateral patellar instability. Am J Sports Med. 2009;37(4):791–796. doi: 10.1177/0363546508328113. [DOI] [PubMed] [Google Scholar]
- 10.Smith T.O., Davies L., O'Driscoll M.L., Donell S.T. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15(4):255–262. doi: 10.1016/j.knee.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Jean-Paul Salameh, Bossuyt Patrick M., McGrath Trevor A., Thombs Brett D., Hyde Christopher J. BMJ; 2020. Macaskill Petra et al. Preferred reporting items for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): explanation, elaboration, and checklist. [DOI] [PubMed] [Google Scholar]
- 12.Centre for Evidence-Based Medicine Oxford centre for evidence-based medicine: levels of evidence. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. 2020 March 2009.
- 13.Sterne J.A.C., Hernán M.A., Reeves B.C., et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355 doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Institute of Health Economics Case series studies quality appraisal checklist. https://www.ihe.ca/research-programs/rmd/cssqac/cssqac-about. 2014
- 15.Henry B.M., Tomaszewski K.A., Ramakrishnan P.K., et al. Development of the anatomical quality assessment (AQUA) tool for the quality assessment of anatomical studies included in meta-analyses and systematic reviews. Clin Anat. 2016;30:6–13. doi: 10.1002/ca.22799. [DOI] [PubMed] [Google Scholar]
- 16.Ma L.F., Wang C.H., Chen B.C., et al. Medial patellar retinaculum plasty versus medial capsule reefing for patellar dislocation in children and adolescents. Arch Orthop Trauma Surg. 2012;132:1773–1780. doi: 10.1007/s00402-012-1598-0. [DOI] [PubMed] [Google Scholar]
- 17.Li X., Fu Z., Lu C. Arthroscopic treatment for patellar dislocation with lateral retinacular release combined with medial patellofemoral ligament reconstruction. Chin J Reparative Reconstr Surg. 2018;32(2):169–173. doi: 10.7507/1002-1892.201711050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mochizuki Y., Kaneko T., Kawahara K., Toyoda S., Ikegami H., Musha Y. A 2-year follow-up of isolated medial patellofemoral ligament reconstruction by using soft suture anchor and adjustable cortical fixation system. J Orthop. 2019;16(4):356–360. doi: 10.1016/j.jor.2019.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watanabe T., Muneta T., Ikeda H., Tateishi T., Sekiya I. Visual analog scale assessment after medial patellofemoral ligament reconstruction: with or without tibial tubercle transfer. J Orthop Sci. 2008;13(1):32–38. doi: 10.1007/s00776-007-1196-0. [DOI] [PubMed] [Google Scholar]
- 20.Akgün U., Nuran R., Karahan M. Modified Fulkerson osteotomy in recurrent patellofemoral dislocations. Acta Orthop Traumatol Turcica. 2010;44(1):27–35. doi: 10.3944/AOTT.2010.2143. [DOI] [PubMed] [Google Scholar]
- 21.Xu C., Zhao J. Treatment of recurrent patellar dislocation with arthroscopic medial retinaculum plication in adolescents. Chin J Reparative Reconstr Surg. 2011;25(8):931–936. [PubMed] [Google Scholar]
- 22.Chen H., Zhao D., Zhang J., Yang Z., Wu Z., Xie J. Role of tibial tubercle internal rotation to treat recurrent patellar dislocation associated with trochlear dysplasia. Chin J Reparative Reconstr Surg. 2015;29(1):31–34. [PubMed] [Google Scholar]
- 23.Yang D., Liu X., Yu H., et al. Double bundle medial patellofemoral ligament reconstruction with anterior half tendon of peroneus longus and lateral retinacular release in treatment of recurrent patellar dislocation: a report of 12 cases and literature review. J Jilin Univ - Med Ed. 2017;43(6):1248–1252. doi: 10.13481/j.1671-587x.20170633. [DOI] [Google Scholar]
- 24.Hiemstra L.A., Kerslake S., Lafave M.R. Patellar apprehension is reduced in most but not all patients after successful patellar stabilization. Am J Sports Med. 2021;49(4):975–981. doi: 10.1177/0363546520988731. [DOI] [PubMed] [Google Scholar]
- 25.Smith T.O., Clark A., Neda S., et al. The intra- and inter-observer reliability of the physical examination methods used to assess patients with patellofemoral joint instability. Knee. 2012;19(4):404–410. doi: 10.1016/j.knee.2011.06.002. 1016/j.knee.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Niu J., Qi Q., Fu K., Duan G., Liu C., Wang F. Medial patellofemoral ligament reconstruction with semi-patellar tunnel fixation: surgical technique and mid-term follow-up. Med Sci Mon Int Med J Exp Clin Res. 2017;23:5870–5875. doi: 10.12659/MSM.905583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fadel M.E., Hosni Y. Medial patellofemoral ligament reconstruction using a central strip of the quadriceps tendon in patients with recurrent patellar instability: a prospective case series. Current orthopaedic practice. 2020;31(4) [Google Scholar]
- 28.Malecki K., Fabis J., Flont P., Lipczyk Z., Niedzielski K. Preliminary results of two surgical techniques in the treatment of recurrent patellar dislocation: medial patellofemoral ligament reconstruction versus combined technique of vastus medialis advancement, capsular plasty and Roux-Goldthwait procedure in treatment of recurrent patellar dislocation. Int Orthop. 2016;40(9):1869–1874. doi: 10.1007/s00264-016-3119-1. [DOI] [PubMed] [Google Scholar]
- 29.Kumahashi N., Kuwaya S., Tadenuma T., Kadowaki M., Uchio Y. A “sandwich” method of reconstruction of the medial patellofemoral ligament using a titanium interference screw for patellar instability in skeletally immature patients. Arch Orthop Trauma Surg. 2012;132(8):1077–1083. doi: 10.1007/s00402-012-1516-5. [DOI] [PubMed] [Google Scholar]
- 30.Zimmermann F., Liebensteiner M.C., Balcarek P. The reversed dynamic patellar apprehension test mimics anatomical complexity in lateral patellar instability. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):604–610. doi: 10.1007/s00167-018-5198-6. [DOI] [PubMed] [Google Scholar]
- 31.Hiemstra L.A., O'Brien C.L., Lafave M.R., Kerslake S. Common physical examination tests for patellofemoral instability demonstrate weak inter-rater reliability. Arthrosc Sports Med Rehabil. 2021;3(3) doi: 10.1016/j.asmr.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leite C.B.G., Santos T.P., Giglio P.N., Pécora J.R., Camanho G.L., Gobbi R.G. Tibial tubercle osteotomy with distalization is a safe and effective procedure for patients with patella alta and patellar instability. Orthop J Sports Med. 2021;9(1) doi: 10.1177/2325967120975101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sadigursky D., Cortizo Garcia L., Armede M., Rodrigues de Oliveira L., Fernandes Carneiro R.J., Oliveira Colavolpe P. Medial patellofemoral ligament and medial patellotibial ligament reconstruction in children: preliminary results. Rev Bras Ortop. 2017;52(4):417–422. doi: 10.1016/j.rboe.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang F., Kang H.J., Chen B.C., Chen W., Su Y.L., Zhang Y.Z. Combination of medial patellofemoral ligament reconstruction with vastus medialis advancement for chronic patellar dislocation. Chin Med J. 2010;123(21):3024–3029. [PubMed] [Google Scholar]
- 35.Torkaman A., Monshizadeh S., Shabanpour M. Medial patellofemoral ligament (MPFL) reconstruction surgery in Iranian patients with recurrent patellar dislocation: report of three years experiences. Biomedical and pharmacology journal. 2015;8(1):165–170. doi: 10.13005/bpj/595. [DOI] [Google Scholar]
- 36.Fink C., Veselko M., Herbort M., Hoser C. MPFL reconstruction using a quadriceps tendon graft☆ Part 2: operative technique and short term clinical results. Knee. 2014;21(2014):1175–1179. doi: 10.1016/j.knee.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 37.Song S.Y., Kim I.S., Chang H.G., Shin J.H., Kim H.J., Seo Y.J. Anatomic medial patellofemoral ligament reconstruction using patellar suture anchor fixation for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2431–2437. doi: 10.1007/s00167-013-2730-6. [DOI] [PubMed] [Google Scholar]
- 38.Ellera Gomes J.L., Marczyk Stigler, de César P.C., Jungblut C.F. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004;20(2):147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 39.Ntagiopoulos P.G., Byn P., Dejour D. Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41(5):998–1004. doi: 10.1177/0363546513482302. [DOI] [PubMed] [Google Scholar]
- 40.Beckert M., Crebs D., Nieto M., Gao Y., Albright J. Lateral patellofemoral ligament reconstruction to restore functional capacity in patients previously undergoing lateral retinacular release. World J Clin Cases. 2016;4(8):202–206. doi: 10.12998/wjcc.v4.i8.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Calanna F., Pulici L., Carimati G., Quaglia A., Volpi P. Medial patello-femoral ligament (MPFL) reconstruction using suture anchors fixation: preliminary results. Muscles Ligaments Tendons J. 2016;6(1):64–70. doi: 10.11138/mltj/2016.6.1.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elbarbary A.N., Badr I.T., Fotoh D.S. Medial patellofemoral ligament reconstruction using a partial-thickness quadriceps tendon graft: short-term clinical outcome retrospective case series. Current Orthopaedic Practice. 2020;31(3):258–262. doi: 10.1097/BCO.0000000000000867. [DOI] [Google Scholar]
- 43.Kang H.J., Cao J.H., Pan S., Wang X.J., Yu D.H., Zheng Z.M. The horizontal Y-shaped graft with respective graft tension angles in anatomical two-bundle medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2445–2451. doi: 10.1007/s00167-014-3005-6. [DOI] [PubMed] [Google Scholar]
- 44.Camathias C., Studer K., Kiapour A., Rutz E., Vavken P. Trochleoplasty as a solitary treatment for recurrent patellar dislocation results in good clinical outcome in adolescents. Am J Sports Med. 2016;44(11):2855–2863. doi: 10.1177/0363546516652894. [DOI] [PubMed] [Google Scholar]
- 45.Mahmoud A.N., Ebied W.F., Bassiony A., Gameel S. All aperture fixation technique of anatomical medial patellofemoral ligament (MPFL) reconstruction with semitendinosus double loop graft: a retrospective case series. Current Orthopaedic Practice. 2021;32(3) doi: 10.1097/BCO.0000000000000981. 256-60. [DOI] [Google Scholar]
- 46.Kumahashi N., Kuwata S., Takuwa H., Egusa N., Uchio Y. Longitudinal change of medial and lateral patellar stiffness after reconstruction of the medial patellofemoral ligament for patients with recurrent patellar dislocation. J Bone Joint Surg. 2016;98(7):576–583. doi: 10.2106/JBJS.15.00605. [DOI] [PubMed] [Google Scholar]
- 47.Schöttle P.B., Fucentese S.F., Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 48.Kita K., Horibe S., Toritsuka Y., et al. Effects of medial patellofemoral ligament reconstruction on patellar tracking. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):829–837. doi: 10.1007/s00167-011-1609-7. [DOI] [PubMed] [Google Scholar]
- 49.Wang C.H., Ma L.F., Zhou J.W., et al. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. 2013;37(4):617–624. doi: 10.1007/s00264-013-1788-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tegner Y., Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 51.Kujala U.M., Jaakkola L.H., Koskinen S.K., Taimela S., Hurme M., Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–163. doi: 10.1016/S0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]