Abstract
Background
As the focal point of epidemic prevention and control, the mental health of COVID-19 patients cannot be ignored. Online Mindfulness-Based Stress Reduction (MBSR) allows for the provision of conveniently accessible, effective and low-cost interventions on a large scale. We aim to evaluate the effectiveness of an online MBSR intervention in alleviating anxiety and depression among asymptomatic/mild patients limited by COVID-19-related restrictions.
Methods
Fifty-eight patients treated in Sanya Fangcang hospital were randomly allocated to either to the experimental group (n = 29) following daily, for 5 days, an online-based mindfulness intervention or to the control group (n = 29). Patients from both groups underwent online questionnaires including assessment of anxiety and depression status at pre- and post-tests using Self-rating Anxiety Scale and Self-Rating Depression Scale.
Results
After the online-based MBSR program, the anxiety and depression scores of the patients in the MBSR group decreased significantly in comparison to the scores of those in the control group (respectively η2 = 0.175, η2 = 0.215, p < 0.001). And the proportion of severe anxiety and depression patients in the MBSR group decreased to 0% which lower than the control group, and the proportion of light anxiety and depression patients was significantly more than that in the control group after the MBSR intervention.
Conclusion
The online-based MBSR intervention appears to be an effective way of alleviating anxiety and depression symptoms among COVID-19 patients with associated quarantine in Fangcang hospital. Given the seriousness of mental health threat that could be posed by this ongoing pandemic, our study provides a new idea and method for cost-effective and time-efficient interventions in the future of epidemic prevention and control.
Keywords: COVID-19 patients, online mindfulness, psychological intervention, anxiety, depression
Introduction
Coronavirus disease 2019 (COVID-19) has spread globally since being reported in late December 2019 from the Chinese province of Hubei, and new COVID-19 cases continue to climb worldwide.1 Since then, the virus has expanded to the point where it is considered to be a pandemic, with 659,108,952 cases of infection and 6,684,756 documented fatalities globally as of this writing.2 Currently, a variety of mutant strains of this extremely contagious virus have emerged, with Omicron variant being one of the most common variants.3 Because of its high transmissibility and its potential to infect those previously vaccinated, the uncertainty of COVID-19 presents a serious challenge to public health again.4,5
Alongside physical health hazards, the COVID-19 caused severe mental trauma among general populations.6 To date, the psychological implications of the COVID-19 epidemic are rapidly being recognized as a public health hazard, and the most frequently reported are depression and anxiety.7 A recent meta-analysis containing 31 studies reported that the pooled prevalence of depression and anxiety in COVID-19 patients was 45% and 47% respectively.8 It has been proposed that COVID-19 patients suffer a higher psychological impact of the outbreak than psychiatric patients and healthy controls.9 The psychological impact of the COVID-19 epidemic has affected every country across different continents, whether developed or developing.10,11 The need for health information, some demographic characteristics (such as age, gender, education), preexisting mood disorders and clinical symptoms (such as fever and myalgia) are all influential factors.9,11–14 Various preventive and control measures such as lockdown at different levels have been implemented in different countries in order to combat the spread of COVID-19. On one hand, the government’s response was beneficial to the public’s mental health since it gave the public a sense of security.15 But from another perspective, prolonged lockdowns and restriction (including home isolation and centralized isolation in Fangcang hospitals) measures also impose a psychological burden. A previous study of 307 patients admitted to Wuhan Fangcang hospitals in the early stage of the epidemic, showed the prevalence of anxiety and depressive symptoms were 18.6% and 13.4%, respectively. Patients’ anxiety and depression ratings were greater than Chinese norms, indicating that COVID-19 patients admitted to Fangcang hospitals had more severe levels of anxiety and depressive symptoms than the general public.16 In addition, previous studies also have shown that social isolation had a significant detrimental psychological influence on locals, leading to negative moods like depression, stress, and anxiety.17 A variety of research has demonstrated that in the first weeks of lockdown, the prevalence of depression and anxiety among the general population in various European and Asian countries was higher than that reported before.18,19 With the recent advancements in epidemic prevention and control, and considering the constant mutation of the virus and the uncertain impact, the isolation and restricted environments imposed by COVID-19 pandemic may still be continued. Additionally, it has been about two years since the outbreak of the COVID-19 pandemic, but the frequency of negative mood in the post-COVID-19 era remains unknown. Therefore, it is very necessary to make timely psychological evaluation and appropriate intervention for COVID-19 patients who are troubled by social isolation and considered as high-risk group.
To this purpose, we tested in this study a non-pharmacological self-management solution named Mindfulness-Based Stress Reduction (MBSR), which can be used as prevention or treatment strategy in a Web-based intervention format. MBSR is a widely used mindfulness-based intervention that incorporates a variety of mindfulness practices aimed at pain alleviation or stress reduction,20–22 and teaches individuals to observe situations and thoughts in a nonjudgmental, nonreactive, and accepting manner.23 According to prior theoretical and empirical evidence, mindfulness practices may aid in the cessation of negative rumination associated to COVID-19 by promoting cognitive behavior.24–27 MBSR can be conducted in clinical and non-clinical settings and be practiced face-to-face or online through smartphone application or audio recording.21,23 In the current COVID-19 pandemic period, such online psychological support interventions are taken into consideration because of their contactless nature and the ease of implementation. There are studies which proposed that online-based MBSR has helped to better manage during social isolation in university students,28,29 healthy workers of isolation ward30 or home quarantined people.24 However, the participants in the previous studies were mostly non-infected quarantined individuals, without disease burden that also had an impact on the mental health. Currently, a growing number of people with infection are either being isolated at homes or in Fangcang hospitals for treating until recovery. Nevertheless, evidence-based interventions aimed at patients who suffer from psychological problems as a result of the COVID-19-related isolation are yet insufficient. The online MBSR intervention can be applied in everyday clinical practice, even able to be generalizability to home-based care, if the efficiency was confirmed, therefore decreasing the obstacle for accessible and low-threshold mental healthcare.
Materials and Methods
Procedure and Participants
A randomized-controlled trial was used to design this study in order to determine the effects of online MBSR program on status of anxiety and depression in asymptomatic/mild patients treated in Fangcang hospitals. Since patients with asymptomatic or mild COVID symptoms are generally treated in Fangcang hospitals, patients with more severe COVID symptoms such as lung infection are hospitalized in large general hospitals. Therefore, all participants in our present study were asymptomatic/mild COVID-19 patients. A dedicated survey was prepared to collect demographic and epidemiological variables, anxiety and depression status using Questionnaire Star program before and after the intervention. Questionnaires were distributed and collected from August to October 2022 in Sanya Fangcang shelter hospital (Hainan, China). To fill in the questionnaire, participants were invited to scan a QR code through their smartphone and answer the online questionnaire. The aims and procedures of this study were explained in the questionnaire and the consent was obtained from each patient when completing the questionnaire. The settings on the questionnaire (such as the needed questions and the scope restrictions) provided control over the questionnaire and prevented participants from selecting answers at random or rushing to finish the survey. And patients were assisted in completing the questionnaires by the trained medical and nursing staff of the Fangcang hospital to ensure the accuracy and reliability of the questionnaires.
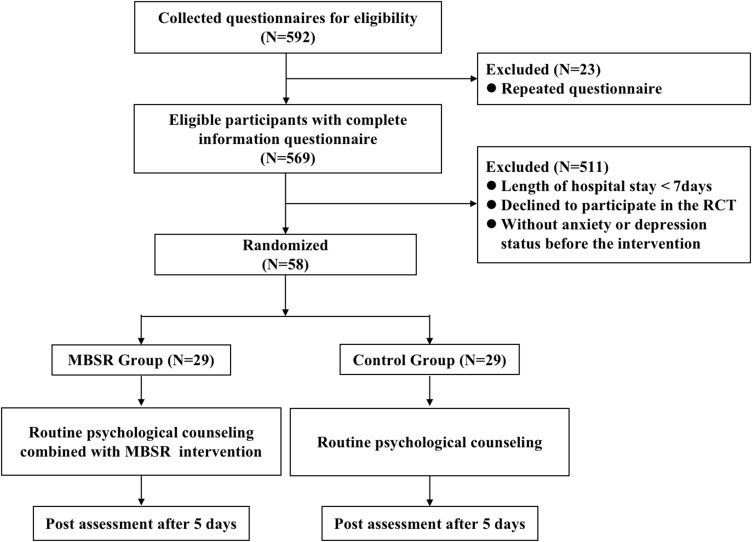
In the present study, 569 patients completed the pre-intervention questionnaires after excluding duplicate questionnaires based on our checks of the participants IP addresses. In the next step, we further excluded patients with a stay of less than 7 days because their length of stay did not meet the time required for a complete intervention, and patients who refuse to participate the trail entry, as well as those whose pre-intervention questionnaire results showed absence of anxiety and depression. Finally, 58 patients were assessed for eligibility. Complete results (pre- and post-test) were obtained for 29 patients in the MBSR group and 29 in the control group. The flow diagram of the trial is presented in Figure 1.
Figure 1.
Flow diagram of study participants.
Randomization and Blinding
A randomization number created by a separate statistician was used to assign the participants at random, the number of random seeds is set as “20,220,909”, and software SPSS was used. Patients who were qualified in our study were ranked by random number size and categorized into two equal groups of 29 patients each. Blinding was carried out at the analysis stage as patient, psychologist and outcome assessor (research staff) blinding was not possible due to the nature of the procedure of intervention.
Intervention
For ethical concerns as well as to control the effects of receiving online MBSR interventions, patients in the control group were given conventional psychological counseling, while patients in the experimental group (MBSR group) accepted a daily online mindfulness practice session on the basis of conventional psychological counseling. Conventional psychological counseling included confronting the epidemic, accepting emotions, scientific protection, improving communication, and reducing intake of negative information. An audio-video mindfulness designed by experts was produced to guide patients through relaxation techniques incorporating mindfulness meditation, breathing exercises, body scanning and progressive muscle relaxation.31,32 The content was selected from the traditional MBSR exercise, which may have been shorter in duration compared to the traditional protocol because of the limited length of hospitalization, and the content did not cover all of it.20,33 However, our protocol focused on the components that were most relevant to the issues that patients isolated in the Fangcang hospitals faced during the studied COVID-19 period. Before the intervention, the patients of MBSR group were provided with a full explanation of mindfulness practice by trained psychometrists, and each exercise was trained for five minutes to ensure that the patients could perform each exercise. And an instruction manual was provided to patients post-training. All eligible patients received conventional psychological counseling and the training of online MBSR intervention in the psychological consulting room of the Fangcang hospital to guarantee patient blinding—patients were blinded to the group allocations and were unaware of the other interventions were. The mindfulness practice was performed in 30 minutes per session, 2 sessions daily (before nap and nightfall) for 5 days. Participants were asked to record their personal experience per day via Wechat. The detailed contents of the mindfulness practice were reported in Supplementary Table 1.
Assessment
All participants underwent online questionnaires including assessment of anxiety and depression status at the beginning (pre-tests) and the end (post-tests) of the study. The pre- and post-tests for both the control and experimental groups were phased throughout the two days preceding and after the online-based MBSR. The anxiety and depression status of the patients were assessed by the Self-rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) scores, respectively. Both scales contain 20 items reflecting subjective feelings of anxiety or depression, and each item was divided into four levels of scores according to the frequency of symptoms, which were recorded as 1 to 4, respectively. The 20 questions’ combined scores were multiplied by 1.25, and the resultant integer score served as a standard score and categorized as: 25–49, no anxiety; 50–59, light anxiety; 60–69, moderate anxiety; 70–100, severe anxiety; 25–52, no depression; 53–62, light depression; 63–72, moderate depression; 73–100, severe depression.34
In addition, we also collected data about patient sociodemographic characteristics before the intervention (pre-tests), including age, sex, ethnicity, education, marriage and work-related nature. The age of the patients was divided into 4 biologically relevant groups: under 20, 20–39, 40–59, and 60 years and older. The ethnicity of a subject was classified as either Han or minority. Marital status was divided as married or not (including single, divorced, widowed, or other). Educational attainment was trichotomized as junior high school and below, senior high school, and college and above. The occupation types were classified into the following three categories: mental labor, light and moderate physical labor, and heavy physical labor. Smoking status, alcohol drinking status and daily exercise assessment were also collected at the same time. Smoking status and alcohol drinking status are classified into two categories: current and former or never. Regular physical exercise was defined as more than 3 times weekly with each time lasting at least 30 minutes. The presence of chronic disease (hypertension, diabetes, and coronary heart disease) was also recorded.
Ethical Considerations
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Biomedical Ethics Committee of Chinese PLA general hospital. Moreover, before commencing, the trail was registered with ClinicalTrials.gov (ChiCTR2200063502).
Statistical Analysis
A target sample size of 29 patients in each group was estimated to provide 80% power at an α level of 0.05 (2-sided) to detect a difference between groups in the change in anxiety and depression scores. This was based on a previous study that showed a significant difference of the SAS and SDS scores (4.65 and 2.89, respectively) after 12 sessions of mindfulness-based online intervention among undergraduate students during times of COVID-19.35 The frequencies, percentages, means, and standard deviations are the forms in which descriptive statistics are presented. The intergroup comparisons of the categorical variables were conducted using the Chi-squared test. Pairwise comparisons between the three groups were also performed using Chi-squared tests. Groups were compared using Student’s t-test corrected for small sample size. Independent-samples t-test will be used for comparisons among MBSR and control groups, while paired t-tests will be used for within-group comparisons. Effect sizes for ANOVA were analyzed when appropriate using eta-squared (η2). We conducted subgroup analyses based on the unbalanced variables found before intervention. Statistical analyses were performed using SPSS Statistics version 24.0 (IBM Corporation, Armonk, NY, United States) and the level of statistical significance was accepted as p < 0.05.
Results
Patient Characteristic
The demographic characteristics of the patients are listed in Table 1. Of the 58 patients, the age was mostly concentrated in the middle-aged (37.9%) and young groups (43.1%), of which light and moderate physical workers accounted for a relatively high proportion (74.1%). Most patients were Han (93.1%) and married (70.7%). Patients with junior high school education and below accounted for 48.3%, followed by senior high school level (37.9%), and college and above (13.8%). The proportions of current smokers and drinkers among the patients were 24.1% and 22.4%, respectively. And patients with regular physical exercise were high of 65.5%. Moreover, a low proportion of patients with chronic disease (including hypertension, diabetes, and coronary heart disease). We found no significant differences in basic characteristic data between the MBSR and control groups, except for sex (p = 0.004) and drinking status (p = 0.028).
Table 1.
Characteristics of the Participants
| Variables | MBSR Group (N=29) | Control Group (N=29) | P-value |
|---|---|---|---|
| Age (year), n (%) | 0.264 | ||
| <20 | 2 (6.9) | 2 (6.9) | |
| 20–39 | 9(31.0) | 16(55.2) | |
| 40–59 | 13(44.8) | 9(31.0) | |
| ≥60 | 5(17.2) | 2(6.9) | |
| Sex, n (%) | 0.004 | ||
| Male | 10(34.5) | 21(72.4) | |
| Female | 19(65.5) | 8(27.6) | |
| Ethnicity, n (%) | 1.000 | ||
| Han | 27(93.1) | 27(93.1) | |
| Non-Han | 2(6.9) | 2(6.9) | |
| Education degree, n (%) | 0.850 | ||
| Junior high school and below | 15(51.7) | 13(44.8) | |
| Senior high school | 10(34.5) | 12(41.4) | |
| College and above | 4(13.8) | 4(13.8) | |
| Marital Status, n (%) | 0.387 | ||
| Married | 22(75.9) | 19(65.5) | |
| Nonmarried (single, divorced, widowed, or other) | 7(24.1) | 10(34.5) | |
| Work-related nature, n (%) | 0.520 | ||
| Mental labor | 6(20.7) | 8(27.6) | |
| Light and moderate physical labor | 22(75.9) | 21(72.4) | |
| Heavy physical labor | 1(3.4) | 0(0.0) | |
| Smoker, n (%) | 4(13.8) | 10(34.5) | 0.066 |
| Drinker, n (%) | 3(10.3) | 10(34.5) | 0.028 |
| Regular physical exercise, n (%) | 17(58.6) | 21(72.4) | 0.269 |
| Previous medical history | |||
| Hypertension, n (%) | 4(13.8) | 1(3.4) | 0.160 |
| Diabetes, n (%) | 0(0.0) | 0(0.0) | - |
| Coronary heart disease, n (%) | 0(0.0) | 1(3.4) | 0.313 |
Effects of Online MBSR Intervention
Table 2 shows the comparison results of the mean pretest-posttest anxiety and depression scores of the patients in the MBSR and control groups. For anxiety scores, the mean scores were higher in patients of the MBSR group compared with control group (55.73 ± 13.04 vs 44.78 ± 7.87). However, there was no significant difference between the two groups after the intervention. Of note, the MBSR group scores being lower than the control group despite not having been found to be statistically significant. Additionally, the effect size of the two groups after the intervention differed. The mean scores of the patients significantly decreased after the MBSR intervention in the MBSR group (p < 0.001), while no significant reduction was observed from pre to post in the control group. For depression scores, there was a significant difference between MBSR and control groups before and after the intervention, with the MBSR group scores being higher than the control group at pre-test (65.00 ± 7.34 vs 59.87 ± 6.34) and the results were reversed at post-test (41.16 ± 14.76 vs 52.80 ± 13.44). Results showed that both groups demonstrated reduction in the depression scores, but the reduction was more pronounced in the MBSR group.
Table 2.
Group Scores of the Anxiety and Depression at Pre- and Post-Tests
| Pre-Test | Post-Test | t-test | ||
|---|---|---|---|---|
| t | P-value | |||
| Anxiety score | ||||
| MBSR group | 55.73±13.04 | 40.13±8.63 | 4.412 | <0.001 |
| Control group | 44.78±7.87 | 42.28±8.79 | 1.786 | 0.085 |
| t | 3.870 | −0.942 | ||
| P-value | <0.001 | 0.350 | ||
| Depression score | ||||
| MBSR group | 65.00±7.34 | 41.16±14.76 | 6.607 | <0.001 |
| Control group | 59.87±6.34 | 52.80±13.44 | 3.052 | 0.005 |
| t | 2.847 | −3.139 | ||
| P-value | 0.006 | 0.003 | ||
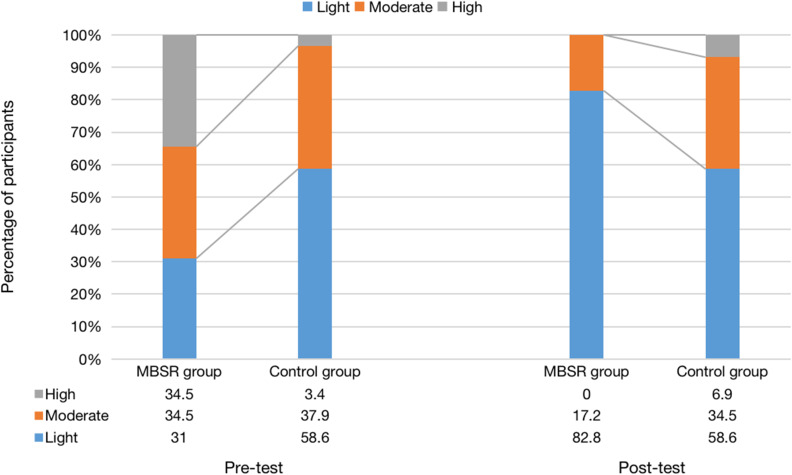
In addition, it was determined that the change score (∆difference) between the mean anxiety and depression scores was shown to be statistically significant in favor of the MBSR group (p < 0.001). The eta-squared values discovered in the study suggested a large effect size of the MBSR intervention on the anxiety and depression scores of the patients (respectively η2 = 0.175, η2 = 0.215) (Table 3). Moreover, we further conducted an additional analysis to investigate the change of the severity of anxiety and depression symptoms from pre to post. We found that the differences in the distribution across different severity levels were statistically significant before the intervention, showing that there were more severe degrees and fewer light degrees in the MBSR group. However, the differences in the distribution cease to be statistically significant after the intervention, with the proportion of severe patients in the MBSR group decreased to 0%, and the proportion of light was significantly more than that in the control group. (A post hoc pairwise comparison of the proportion of light level showed a statistically significant difference) (Figure 2).
Table 3.
Comparison of the Anxiety and Depression Scores Differences of the MBSR and Control Groups
| Difference | t | P-value | η² | |
|---|---|---|---|---|
| Anxiety score | ||||
| MBSR group | 13.75(−1.25–37.50) | 3.445 | 0.001 | 0.175 |
| Control group | 0.00(−1.25–5.63) | |||
| Depression score | ||||
| MBSR group | 21.25(6.25–44.38) | 3.911 | <0.001 | 0.215 |
| Control group | 6.25(−3.13–15.00) |
Figure 2.
The distribution of participants in the different levels for both the MBSR and control groups at pre- and post-tests.
Because sex and drinking status were unbalanced between the two groups at pre-test, we performed exploratory subgroup analysis stratified by sex and drinking status (Supplement Figures 1 and 2). The results of all the subgroup analysis are consistent with the results of the main analysis.
Discussion
The primary objective of the current research was to assess the effectiveness of a brief online-based mindfulness intervention in countering the anxiety and depression status in asymptomatic/mild patients treated in Fangcang hospitals. The findings of this study demonstrated that, in comparison to the scores of those in the control group, the anxiety and depression scores of the patients in the MBSR group considerably decreased following the implementation of the MBSR program.
In the relevant literature, several studies have identified the high levels of anxiety and depression in patients who were diagnosed with COVID-19.8 The mitigation measures for COVID-19 patients like social distancing, isolation in hospital or at home were encouraged or mandated in various countries. The harmful effects of COVID-19 restrictions on mental health were highlighted by the previous work that those who were quarantined and self-isolated for two weeks showed high levels of stress and anxiety.18 On one hand, hospital isolation such as Fangcang hospital reduces access and support from family, friends and social support system. On the other hand, home isolation constitutes a stressful situation due to the concern and fear of a potentially serious infection for the family members, which results in worsening the anxiety and depression status among patients. These evidence in the psychological domain support the urgent need to develop preventive and interventional ways to deal with the increased psychological suffering during the pandemic.
A wide variety of psychological interventions have been studied within the context of reducing anxiety and depression levels for patients in the face of the COVID-19 pandemic, including face-to-face36,37 and internet-based psychological interventions.38,39 Related studies indicated that most of the interventions have achieved positive effect on the improvement of psychological conditions of patients with COVID-19.36–39 However, continuously tense epidemic situation and increasing number of infections have restricted extensive face-to-face psychological interventions for patients who are isolated in hospital or at home. In this situation, using an online intervention could offer a safe, affordable and convenient tool for protecting patients from the undesirable psychological damages of the isolation and infection.
Mindfulness is a nonpharmacologic mind-body therapy initially introduced by Kabat-Zinn to the medical profession in the MBSR Program.40 MBSR is an approach to stress management that is supported by research and teaches people how to intentionally regulate their attention.41 Over recent decades, MBSR has been reported to be beneficial in the treatment of many physical and mental health problems.42–44 Moreover, attempts have been made to integrate traditional mindfulness training with internet, and evaluate the feasibility and effectiveness of this intervention approach in different types of populations during the outbreak.45 In a randomized-controlled trial performed in 84 pregnant women diagnosed with COVID-19, it was observed that after the MBSR intervention, participants’ levels of prenatal distress, anxiety and childbirth fear in the trained group significantly decreased in comparison to the levels of those in the control group.46 In addition, a study in Italy involving 108 residents who underwent an Internet delivered MBSR designed as an eight-week session during the initial stages of lockdown found that MBSR may be useful for helping individuals with emotion regulation and mental health support.47 Another study conducted among 96 university students showed that online-based mindfulness practice could alleviate stress, anxiety and depressive symptoms during the COVID-19 period after the intervention.28 However, the subjects of the above studies did not suffer from the double psychological burden of being infected with the disease, and most studies focused on the early stage of epidemic. Considering that patients are at higher risk of psychological stress in isolation, the additional stress of infection with COVID-19 can increase their vulnerability. Unfortunately, evidence about the efficacy of online-based MBSR interventions on COVID-19 patients in the post-COVID-19 era is still insufficient. Two previous studies with randomized controlled trial designs indicated a significant decrease in the levels of anxiety, depression, and stress in the experimental group through the internet-based psychological support, compared to the control group.38,39 Consistent with these findings, our results confirmed the expected benefits of online-based MBSR on the improvement of anxiety and depressive states. Findings in our study revealed that after the online-based MBSR intervention, the decrease in the MBSR group is higher than that in the control group, and the difference (∆difference) is statistically significant, both for the score of anxiety and depression. On one hand, the detailed content of online-based MBSR intervention in our study is simple to implement and promote mental health in a feasible and effective manner, and its effectiveness was achieved in the short time, without the complex and comprehensive intervention approach used in the previous studies. On the other hand, our study extends previous research in this area, because it evaluated the effects of online-based mindfulness to alleviate patients’ anxiety and depressive symptoms in the post-COVID-19 era, and provide feasible solutions for mitigating epidemic-related mental health impacts during the period of epidemic prevention and control in the further.
Although the current isolation policy has become more relaxed worldwide, home isolation is still required after infection for consideration of the health impacts on oneself and on others. And public health facility such as Fangcang hospital remains as the primary isolation and treatment site for those with centralized isolation needs. Offering therapies that will be accessible to everyone is a crucial goal in the promotion of mental health in the post-COVID-19 era. Currently, the availability of smartphones and online services allows patients in isolation to access timely psychological help from professionals if needed. Thus, online psychological interventions were considered as cost-effective and time-efficient methods.38,45 In addition, the online-based and audio-guided MBSR intervention in our study resulted in a rapid improvement on anxiety and depression states of isolated patients, indicating its applicability. We believe that the standardized application of the web-based MBSR programs could offer appropriate prescriptions to others with psychologically unstable states due to this ongoing pandemic (or any future similar crisis).
To our knowledge, this study is the first to confirm the positive effect of online-based MBSR intervention on patients treated in Fangcang hospitals, and provide further evidence to support its promotion in the post-COVID-19 era. However, there are a few limitations to the current study. Firstly, we did not measure the long-term effects of online-based MBSR on patients. Indeed, the adherence to the intervention was highly encouraging, and despite the relatively short period of practice in our trial, beneficial psychological effects on anxiety and depression were seen. Secondly, although we randomly allocated the patients into two groups, their demographic characteristics were not fully balanced between the groups at the baseline. Nevertheless, the results remain consistent and robust in our subgroup analyses. Thirdly, there is lack of data of assessment of the efficacy of mindfulness because of some technical reasons. Recent advances in technology have facilitated the use of functional neuroimaging to evaluate the efficacy of mindfulness, which offers significant promise for clinical applications of a series of mindfulness-based therapies.48 Lastly, the pandemic context also constrained our sample size. Population-based research with larger samples need to be conducted in the future. On the basis of larger sample size, future research should concentrate on identifying patient subgroups which might benefit from the intervention the most in order to effectively utilize resources, customize therapies, and obtain the most possible benefit. The results of this study, together with the limitations noted above, suggest directions for future research in this area.
Conclusion
Overall, our findings indicate that we provided a cost-effective and time-efficient method to relieves anxiety, depression, and other negative emotions through online-based MBSR program in the post-COVID-19 era. The speed at which COVID-19 might spread was accelerated by new virus mutations, and increasing COVID-19 patients and heightened psychological symptoms have become common. Low-threshold mental health assistance, such as the online-based MBSR program, may be able to fill the gap in the provision of interventions for the general population during times of public contact restrictions and disease distress, thereby reducing the negative impacts of this public health crisis.
Acknowledgments
We appreciate the dedication of all nursing, medical, and health-care personnel in caring for the patients in this study.
Funding Statement
The study was supported by the Major Science and Technology Project in Hainan Province of China (No. ZDKJ2019012), National Natural Science Foundation of China (82173589, 82173590), Capital’s Funds for Health improvement and research (2022-2G-5031), National Key R&D Program of China (2022YFC2503605), Joint logistics support force military theoretical scientific research project (JJ2021A06-B018).
Data Sharing Statement
The database of the current study is not publicly available.
Informed Consent
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Biomedical Ethics Committee of Chinese PLA general hospital. Moreover, before commencing, the trail was registered with ClinicalTrials.gov (ChiCTR2200063502).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Yazaki S, Yoshida T, Kojima Y, et al. Difference in SARS-CoV-2 antibody status between patients with cancer and health care workers during the COVID-19 pandemic in Japan. JAMA Oncol. 2021;7(8):1141–1148. doi: 10.1001/jamaoncol.2021.2159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available from: https://covid19.who.int/. Accessed January 10, 2023.
- 3.Cai W, Yang Z, Liang J, et al. How fast and how well the Omicron epidemic was curtailed. A Guangzhou experience to share. Front Public Health. 2022;10:979063. doi: 10.3389/fpubh.2022.979063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tzitzi E, Pyrpasopoulou A, Kalmoukos P, et al. Casivirimab/Imdevimab effect on COVID-19 outcome and reinfection in a real-world SARS-COV-2 variant transition period setting. Monoclon Antib Immunodiagn Immunother. 2023;42:48–50. doi: 10.1089/mab.2022.0033 [DOI] [PubMed] [Google Scholar]
- 5.Aleem A, Akbar Samad AB, Slenker AK. Emerging variants of SARS-CoV-2 and novel therapeutics against Coronavirus (COVID-19). In: StatPearls. Treasure Island: StatPearls Publishing LLC; 2022. [PubMed] [Google Scholar]
- 6.Salanti G, Peter N, Tonia T, et al. The impact of the COVID-19 pandemic and associated control measures on the mental health of the general population: a systematic review and dose-response meta-analysis. Ann Intern Med. 2022;175(11):1560–1571. doi: 10.7326/M22-1507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly M, Robinson E. Depression and anxiety during COVID-19. Lancet. 2022;399(10324):518. doi: 10.1016/S0140-6736(22)00187-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deng J, Zhou F, Hou W, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. 2021;1486(1):90–111. doi: 10.1111/nyas.14506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hao F, Tam W, Hu X, et al. A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID-19 inpatients in isolation facilities. Transl Psychiatry. 2020;10(1):355. doi: 10.1038/s41398-020-01039-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang C, Chudzicka-Czupała A, Tee ML, et al. A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans, Asians and Europeans. Sci Rep. 2021;11(1):6481. doi: 10.1038/s41598-021-85943-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C, Tee M, Roy AE, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS One. 2021;16(2):e0246824. doi: 10.1371/journal.pone.0246824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ceban F, Nogo D, Carvalho IP, et al. Association between mood disorders and risk of COVID-19 infection, hospitalization, and death: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(10):1079–1091. doi: 10.1001/jamapsychiatry.2021.1818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chudzicka-Czupała A, Chiang SK, Grabowski D, et al. Predictors of psychological distress across three time periods during the COVID-19 pandemic in Poland. Int J Environ Res Public Health. 2022;19(22):15405. doi: 10.3390/ijerph192215405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lau SS, Ho cc, Pang RC, et al. Measurement of burnout during the prolonged pandemic in the Chinese zero-COVID context: COVID-19 burnout views scale. Front Public Health. 2022;10:1039450. doi: 10.3389/fpubh.2022.1039450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee Y, Lui LMW, Chen-Li D, et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J Affect Disord. 2021;290:364–377. doi: 10.1016/j.jad.2021.04.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dai LL, Wang X, Jiang TC, et al. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. PLoS One. 2020;15(8):e0238416. doi: 10.1371/journal.pone.0238416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921. doi: 10.12659/MSM.923921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021;51(2):201–211. doi: 10.1017/S0033291721000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. doi: 10.1016/0163-8343(82)90026-3 [DOI] [PubMed] [Google Scholar]
- 21.Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Altern Complement Med. 2009;15(5):593–600. doi: 10.1089/acm.2008.0495 [DOI] [PubMed] [Google Scholar]
- 22.Anheyer D, Haller H, Barth J, Lauche R, Dobos G, Cramer H. Mindfulness-based stress reduction for treating low back pain: a systematic review and meta-analysis. Ann Intern Med. 2017;166(11):799–807. doi: 10.7326/M16-1997 [DOI] [PubMed] [Google Scholar]
- 23.Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res. 2015;78(6):519–528. doi: 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- 24.Zhang H, Zhang A, Liu C, Xiao J, Wang K. A brief online mindfulness-based group intervention for psychological distress among Chinese residents during COVID-19: a pilot randomized controlled trial. Mindfulness. 2021;12(6):1502–1512. doi: 10.1007/s12671-021-01618-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y, Xue J, Huang Y. A meta-analysis: internet mindfulness-based interventions for stress management in the general population. Medicine. 2020;99(28):e20493. doi: 10.1097/MD.0000000000020493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spijkerman MP, Pots WT, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2016;45:102–114. doi: 10.1016/j.cpr.2016.03.009 [DOI] [PubMed] [Google Scholar]
- 27.Kladnitski N, Smith J, Allen A, Andrews G, Newby JM. Online mindfulness-enhanced cognitive behavioural therapy for anxiety and depression: outcomes of a pilot trial. Internet Interv. 2018;13:41–50. doi: 10.1016/j.invent.2018.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Devillers-Réolon L, Mascret N, Sleimen-Malkoun R. Online mindfulness intervention, mental health and attentional abilities: a randomized controlled trial in university students during COVID-19 lockdown. Front Psychol. 2022;13:889807. doi: 10.3389/fpsyg.2022.889807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simonsson O, Bazin O, Fisher SD, Goldberg SB. Effects of an eight-week, online mindfulness program on anxiety and depression in university students during COVID-19: a randomized controlled trial. Psychiatry Res. 2021;305:114222. doi: 10.1016/j.psychres.2021.114222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dincer B, Inangil D. The effect of emotional freedom techniques on nurses’ stress, anxiety, and burnout levels during the COVID-19 pandemic: a randomized controlled trial. Explore. 2021;17(2):109–114. doi: 10.1016/j.explore.2020.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hathiramani S, Pettengell R, Moir H, Younis A. Relaxation and exercise in lymphoma survivors (REIL study): a randomised clinical trial protocol. BMC Sports Sci Med Rehabil. 2019;11:17. doi: 10.1186/s13102-019-0127-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kersemaekers WM, Vreeling K, Verweij H, et al. Effectiveness and feasibility of a mindful leadership course for medical specialists: a pilot study. BMC Med Educ. 2020;20(1):34. doi: 10.1186/s12909-020-1948-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: effects on well-being. J Clin Psychol. 2008;64(7):840–862. doi: 10.1002/jclp.20491 [DOI] [PubMed] [Google Scholar]
- 34.Long FJ, Chen H, Wang YF, et al. Research on the effect of health care integration on patients’ negative emotions and satisfaction with lung cancer nursing activities. World J Clin Cases. 2020;8(18):4059–4066. doi: 10.12998/wjcc.v8.i18.4059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alvarado-García PAA, Soto-Vásquez MR, Rosales-Cerquín LE. Mindfulness-based online intervention for mental health during times of COVID-19. Indian J Psychiatry. 2022;64(3):264–268. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_642_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li J, Li X, Jiang J, et al. The effect of cognitive behavioral therapy on depression, anxiety, and stress in patients with COVID-19: a randomized controlled trial. Front Psychiatry. 2020;11:580827. doi: 10.3389/fpsyt.2020.580827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. 2020;39:101132. doi: 10.1016/j.ctcp.2020.101132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shaygan M, Yazdani Z, Valibeygi A. The effect of online multimedia psychoeducational interventions on the resilience and perceived stress of hospitalized patients with COVID-19: a pilot cluster randomized parallel-controlled trial. BMC Psychiatry. 2021;21(1):93. doi: 10.1186/s12888-021-03085-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wei N, Huang BC, Lu SJ, et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J Zhejiang Univ Sci B. 2020;21(5):400–404. doi: 10.1631/jzus.B2010013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paulson S, Davidson R, Jha A, Kabat-Zinn J. Becoming conscious: the science of mindfulness. Ann N Y Acad Sci. 2013;1303:87–104. doi: 10.1111/nyas.12203 [DOI] [PubMed] [Google Scholar]
- 41.Weingartner LA, Sawning S, Shaw MA, Klein JB. Compassion cultivation training promotes medical student wellness and enhanced clinical care. BMC Med Educ. 2019;19(1):139. doi: 10.1186/s12909-019-1546-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- 43.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78(2):169–183. doi: 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carlson LE. Mindfulness-based interventions for physical conditions: a narrative review evaluating levels of evidence. ISRN Psychiatry. 2012;2012:651583. doi: 10.5402/2012/651583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yeun Y-R, Kim S-D. Psychological effects of online-based mindfulness programs during the COVID-19 pandemic: a systematic review of randomized controlled trials. Int J Environ Res Public Health. 2022;19(3):1624. doi: 10.3390/ijerph19031624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Güney E, Cengizhan S, Karataş Okyay E, Bal Z, Uçar T. Effect of the mindfulness-based stress reduction program on stress, anxiety, and childbirth fear in pregnant women diagnosed with COVID-19. Complement Ther Clin Pract. 2022;47:101566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Borghi S, Nisticò A, Marano G, Janiri L, Sani G, Mazza M. Beneficial effects of a program of Mindfulness by remote during COVID-19 lockdown. Eur Rev Med Pharmacol Sci. 2022;26(15):5562–5567. [DOI] [PubMed] [Google Scholar]
- 48.Yu J, Ang KK, Choo CC, Ho CS, Ho R, So RQ. prefrontal cortical activation while doing mindfulness task: a pilot functional near-infrared spectroscopy study. Annu Int Conf IEEE Eng Med Biol Soc. 2020;2020:2905–2908. [DOI] [PubMed] [Google Scholar]