Abstract
Introduction:
Beverage taxes are associated with declines in sugar-sweetened beverage (SSB) sales and consumption, but few studies have evaluated associations of these taxes with health outcomes. This study analyzed changes in dental decay after implementation of the Philadelphia sweetened beverage tax.
Methods:
Electronic dental record data were obtained on 83,260 patients living in Philadelphia and control areas from 2014–2019. Difference-in-differences (DD) analyses compared the number of new Decayed, Missing, and Filled Teeth (DMFTnew) and new Decayed, Missing, and Filled Surfaces (DMFSnew) before (January 2014–December 2016) and after (January 2019–December 2019) tax implementation in Philadelphia and control patients. Analyses were conducted in older children/adults (≥15 years) and younger children (<15 years). Subgroup analyses stratified by Medicaid status. Analyses were conducted in 2022.
Results:
DMFTnew did not change post-tax in Philadelphia in panel analyses of older children/adults (DD=−0.02, 95% CI: −0.08, 0.03) or in younger children (DD=0.07, 95% CI: −0.08, 0.23). There were similarly no post-tax changes in DMFSnew. However, in cross-sectional samples of patients on Medicaid, DMFTnew was lower post-tax in older children/adults (DD=−0.18, 95% CI: −0.34, −0.03; −22% decline) and younger children (DD=−0.22, 95% CI: −0.46, 0.01; −30% decline), with similar results for DMFSnew.
Conclusions:
The Philadelphia beverage tax was not associated with reduced tooth decay in the general population, but it was associated with reduced tooth decay in adults and children on Medicaid, suggesting potential health benefits for low-income populations.
INTRODUCTION
Several countries and U.S. localities have implemented sweetened beverage excise taxes to raise revenue and curb sugar-sweetened beverage (SSB) consumption, which is associated with chronic disease,1,2 including tooth decay.3 These taxes have produced large changes in behavior. A recent meta-analysis found that beverage taxes were associated with a mean 15% decrease in SSB sales, with similar declines observed in studies of SSB consumption.4,5 Given that 49% of U.S. adults and 63% of U.S. youth drink SSBs daily, with higher consumption among low-income households,6–9 beverage taxes may improve health outcomes, including oral health.
Dental caries are one of the most common diseases, with a prevalence of 46% in youth and 91% in adults in the U.S.10,11 The prevalence of untreated caries in these groups is 13% and 27%, respectively, with higher prevalence in lower-income populations.10,12 Untreated caries are associated with pain, infection, and poor school attendance and performance,10,13–15 and emerging evidence suggests that tooth loss, which is often caused by long-term decay, is associated with cardiovascular disease.16,17 Beverage taxes may mitigate tooth decay through reduced SSB consumption, especially among lower-income populations given their relatively higher consumption.8,9 These benefits have been suggested in simulation studies18–20 and observed in an evaluation of Mexico’s beverage tax, which found posttax reductions in the number of teeth treated for caries.21 However, no study has examined associations of U.S. beverage taxes with oral health outcomes.
This study examined changes in tooth decay after implementation of the Philadelphia beverage tax on January 1, 2017.22 Large quasi-experimental evaluations of this 1.5 cent-per-oz tax, which applies to SSBs and artificially-sweetened beverages, have observed 22–35% declines in SSB purchases after accounting for increased beverage purchases outside of the city (i.e., tax avoidance),23,24 and an approximate 15% decline in SSB consumption.5 This study used difference-in-differences analyses of electronic dental records (EDR) to examine changes in tooth decay measures in Philadelphia residents versus residents of control areas.
METHODS
Study sample
EDR data with procedures from January 1, 2014 to October 28, 2021 were obtained from 51 University of Pennsylvania School of Dental Medicine clinics in Philadelphia and nearby suburbs. The clinics treat residents of Pennsylvania, New Jersey, Delaware, and Maryland. The data included procedures performed, procedure dates, specific teeth and tooth surfaces that were treated, as well as patient age, gender, insurance type, and residential zip code, which identified patients living in Philadelphia (intervention) or outside Philadelphia (control).
There were 1,215,036 procedures performed across all clinics over the study period. Procedures from 2017–2018 were excluded (n=317,423) because the authors hypothesized that the tax would require 2 years to affect dental health outcomes. Procedures performed in 2020–2021 were excluded (n=264,089) because patients may have changed their health behaviors or dental care utilization during the COVID-19 pandemic. Patients living in Delaware (n=15,183 procedures) or Maryland (n=1,772 procedures) were excluded because these states’ Medicaid policies did not cover dental procedures over the study period, whereas Medicaid in Pennsylvania and New Jersey did.25 Additionally, patients who lived in both Philadelphia and a control area at different points of the study were excluded (n=50,054 procedures) because they would have been exposed to both treatment conditions. After applying these criteria and removing 91 patients with missing data on age, gender, or zip code (n=305 procedures), the analytic sample included 83,260 patients (n=604,895 procedures). The majority (59%) of control patients lived in a county bordering Philadelphia (Bucks, Delaware, or Montgomery in PA; Camden or Burlington in NJ).
Analyses were conducted in repeated cross-sections of older children/adults (≥15 years; n=67,077) and younger children (<15 years; n=17,403); some patients were in both groups if they turned 15 during the study. Fifteen years was used as the cutoff because that is when most people have all their permanent teeth and when the University of Pennsylvania dental clinics transition children to the adult clinics. Longitudinal analyses were additionally conducted using panels of individuals with data in both the pre- (2014–2016) and posttax (2019) periods. Older children/adults in the panel (n=11,756) were ≥15 years from 2014–2019 and younger children in the panel (n=2,950) were <15 years from 2014–2019. All outcomes were aggregated at the patient-quarter level, which ensured enough time points to evaluate pretax trends.
Measures
Tooth decay was measured with two indices. First, the Decayed, Missing, and Filled Teeth (DMFT) index was calculated by summing the total number of decayed, missing, and filled teeth for each patient at each time point, based on EDR procedures (Appendix Table 1 lists procedures that were included and excluded in tooth decay calculations). DMFT counts all teeth that were ever treated, except third molars, and can only increase over time.26 The Decayed, Missing, and Filled Surfaces (DMFS) index was also calculated, which captures the total number of treated surfaces except incisal surfaces (i.e., the biting edge) on each tooth (up to 4 on incisors and canines and up to 5 on premolars and molars),26 providing greater detail on the level of decay. Similarly, this index can only increase over time. Analyses included only treatments on permanent teeth in older children/adults and treatments on both permanent and primary teeth in younger children.
The two primary outcomes were number of new teeth treated (DMFTnew) and number of new surfaces treated (DMFSnew). This was calculated by summing all newly treated teeth/surfaces at each time point for each patient. This approach assumed that the teeth/surfaces that were treated during the study had not been previously treated before study initiation in 2014, though they could have been treated in prior unobservable years. For patients with only 1 visit, DMFTnew and DMFSnew equaled the total DMFT and DMFS, respectively, from that visit. DMFTnew and DMFSnew were calculated before excluding the 2017–2018 data from analysis to ensure any treatments in 2019 accounted for 2017–2018 treatments.
The 2015 Social Deprivation Index (SDI) score of each patient’s residential zip code was calculated. This score is a composite measure of 7 demographic characteristics to quantify neighborhood socioeconomic status (SES)27,28 and ranges from 0 (least deprivation) to 100 (most deprivation). For participants who moved zip codes during the study, the median SDI score over follow-up was calculated. Patients were also classified by whether they were ever on Medicaid during the study as a marker of lower SES (e.g., Medicaid is available to adults in Pennsylvania and New Jersey with incomes <138% of the federal poverty level29). For panel members only, the total number of pretax non-treatment visits (i.e., well visits) was used as a measure of pretax dental care utilization.
Statistical analysis
Difference-in-differences analyses required pretax parallel trends in outcomes between Philadelphia and control patients.30 Because the unadjusted pretax trends were not parallel in several analyses, inverse probability of treatment weights (IPTW) were created to adjust for variables that were imbalanced between the 2 groups and that could influence outcome trends31 (age, gender, SDI score, Medicaid status and, for panel only, number of pretax non-treatment visits). The Appendix provides details on IPTW construction. IPTWs were truncated at the 95th percentile to reduce the influence of extreme weights. After weighting with IPTWs, the pretax trends were reassessed using a model for each outcome with terms for group (Philadelphia versus control), time (continuous quarter), and a group-by-time interaction. Pretax parallel trends were observed upon evaluation of the group-by-time interaction term and upon visual inspection (see Appendix).
Posttax changes in DMFTnew and DMFSnew in Philadelphia versus control were estimated using generalized estimating equations clustered at the patient level with robust empirical standard errors and weighted by IPTWs. The models specified a negative binomial distribution (i.e., for over-dispersed count outcomes) and included terms for group, period (pre versus post), and a group-by-period interaction, which estimated the difference-in-differences (DD). Absolute changes are reported from models with an identity link and percent changes from models with a log link (see Appendix). The main analyses examined DMFTnew and DMFSnew separately in the adult and child panels, as well as in the adult and child cross-sectional samples. Subgroup analyses were conducted by gender (men/women and boy/girl) because previous studies have observed posttax differences in health outcomes by gender.32 Analyses also stratified by Medicaid status (ever/never on Medicaid). Stratified analyses were not conducted in the panels due to small sample sizes.
Several sensitivity analyses were conducted. First, patient-months were analyzed (versus patient-quarters) to determine robustness using different aggregations of time. Second, IPTWs were truncated at the 99th percentile (versus 95th), which led to better covariate balance between groups but resulted in more extreme weights. Third, New Jersey residents were excluded because New Jersey’s Medicaid program included extensive dental benefits, whereas Pennsylvania’s program only offered limited benefits.25 Fourth, analyses adjusted for season. Fifth, in child cross-sectional analyses, Medicaid status was included in the regression model (versus in IPTW) because the Medicaid distribution differed over time between groups even after weighting. Sixth, analyses stratified by current Medicaid status (versus ever-/never-Medicaid in the main subgroup analyses). Seventh, analyses used 14- and 16-year cutoffs between older children/adults and younger children (versus 15 years). Eighth, Philadelphia residents who lived in zip codes on the city border, and could therefore more easily avoid the tax, were excluded. Lastly, models included city-specific trends in case there were undetected violations of the parallel trends assumption.
Analyses used SAS version 9.4 (Cary, NC) and calculated two-sided 95% confidence intervals (CI). This study was approved by the University of Pennsylvania institutional review board.
RESULTS
In the panel datasets, before applying IPTW, Philadelphia patients were more likely to have ever had Medicaid (older children/adults: 21% Philadelphia versus 7% control; younger children: 71% versus 28%) and live in neighborhoods with greater deprivation (older children/adults: mean [SD] SDI score of 77.7 [20.0] in Philadelphia versus 23.8 [24.1] in control; younger children: 87.1 [13.3] versus 27.0 [28.2]), with minor differences for other characteristics (Table 1). Approximately 7% of older children/adults (n=766) and 3% of younger children (n=85) were New Jersey residents; all other patients were from Pennsylvania. IPTW improved covariate balance, though some differences persisted in SDI score and Medicaid status. These same overall patterns were observed in the cross-sectional sample. However, applying IPTW made pretax trends much more similar between groups compared to the unweighted analyses for both samples (see Appendix). After weighting, characteristics of the cross-sectional samples were generally similar in each year except for Medicaid status, which increased in both groups over time (Appendix Table 2). Among ever-Medicaid patients, the covariate distributions over time were similar between Philadelphia and control (Appendix Table 3).
Table 1.
Characteristics of panel and cross-sectional samples before and after inverse probability of treatment weightinga
| Older children/adults | Younger children | |||||||
|---|---|---|---|---|---|---|---|---|
| Before weighting | After weighting | Before weighting | After weighting | |||||
| Characteristicb | Philadelphia | Control | Philadelphia | Control | Philadelphia | Control | Philadelphia | Control |
| Panel | ||||||||
| N | 7,043 | 4,713 | 7,043 | 4,713 | 2,088 | 862 | 2,088 | 862 |
| Age at baseline, years | 45.1 (17.2) | 49.3 (16.0) | 46.3 (17.4) | 48.7 (16.0) | 4.1 (2.8) | 4.6 (2.7) | 4.1 (2.8) | 4.6 (2.7) |
| Gender | ||||||||
| Female | 62% | 57% | 61 % | 59 % | 48% | 49% | 48% | 50% |
| Male | 38% | 43% | 39% | 41% | 52% | 51% | 52% | 50% |
| Other | <1% | 0% | <1% | 0% | -- | -- | -- | -- |
| %Ever Medicaid | 21% | 7% | 19% | 12% | 71% | 28% | 67% | 45% |
| Zip code SDI score | 77.7 (20.0) | 23.8 (24.1) | 69.7 (23.9) | 41.2 (32.0) | 87.1 (13.3) | 27.0 (28.2) | 83.6 (17.0) | 52.7 (35.6) |
| Number of pre-tax non-treatment visits | 4.2 (2.5) | 4.7 (2.4) | 4.3 (2.5) | 4.6 (2.4) | 3.3 (2.1) | 4.0 (2.2) | 3.4 (2.1) | 3.9 (2.2) |
| Cross-section | ||||||||
| N | 44,093 | 22,978 | 44,093 | 22,978 | 11,853 | 5,550 | 11,853 | 5,550 |
| Age, years | 40.9 (17.9) | 46.2 (18.4) | 41.8 (18.2) | 44.2 (18.0) | 7.7 (3.7) | 8.0 (3.8) | 7.6 (3.8) | 8.1 (3.8) |
| Gender | ||||||||
| Female | 58% | 55% | 57% | 56% | 48% | 48% | 48% | 47% |
| Male | 42% | 45% | 43% | 44% | 52% | 52% | 52% | 53% |
| Other | 0% | <1% | <1% | <1% | <1% | <1% | <1% | <1% |
| %Ever Medicaid | 29% | 21% | 26% | 22% | 69% | 34% | 65% | 54% |
| Zip code SDI score | 81.4 (18.7) | 30.6 (27.5) | 74.0 (23.3) | 55.4 (33.1) | 87.3 (13.0) | 34.1 (30.2) | 82.2 (18.3) | 64.9 (32.6) |
Inverse probability of treatment weights accounted for all listed covariates and were truncated at the 95th percentile.
Mean (SD) or %
The mean (SD) pretax DMFTnew in the Philadelphia panel was 0.51 (1.15) in older children/adults and 0.49 (1.39) in younger children after applying IPTW (Table 2). The mean pretax DMFTnew was ~50% higher among ever-Medicaid patients versus never-Medicaid patients (older children/adults: 0.87 [1.86] versus 0.56 [1.26]; younger children: 0.66 [1.64] versus 0.42 [1.36]). The mean (SD) pretax DMFSnew in the Philadelphia panel was 1.35 (3.46) in older children/adults and 1.48 (5.08) in younger children, with 60–75% higher values among ever-Medicaid versus never-Medicaid patients.
Table 2.
Difference-in-differences in number of new treatments (DMFTnew) and surfaces (DMFSnew) after Philadelphia beverage tax implementation
| Pre-tax Mean (SD)a | Post-tax Mean (SD)a | ||||
|---|---|---|---|---|---|
| Outcome | Philadelphia | Control | Philadelphia | Control | Difference-in-differences (95% CI)b |
| Older children/adults | |||||
| DMFTnew | |||||
| Panel | 0.51 (1.15) | 0.49 (1.14) | 0.28 (0.79) | 0.31 (0.93) | −0.02 (−0.08, 0.03) |
| Cross-section | 0.62 (1.40) | 0.64 (1.48) | 0.46 (1.20) | 0.55 (1.45) | −0.05 (−0.11, 0.01) |
| Cross-section, ever-Medicaid | 0.87 (1.86) | 0.77 (1.71) | 0.65 (1.48) | 0.72 (1.76) | −0.18 (−0.34, −0.03) |
| Cross-section, never-Medicaid | 0.56 (1.26) | 0.62 (1.43) | 0.40 (1.08) | 0.49 (1.33) | −0.02 (−0.08, 0.03) |
| DMFSnew | |||||
| Panel | 1.35 (3.46) | 1.35 (3.29) | 0.91 (2.72) | 1.03 (3.44) | −0.06 (−0.29, 0.17) |
| Cross-section | 1.76 (4.66) | 1.91 (5.16) | 1.38 (4.13) | 1.73 (5.26) | −0.11 (−0.37, 0.14) |
| Cross-section, ever-Medicaid | 2.69 (6.86) | 2.46 (6.30) | 2.02 (5.34) | 2.36 (6.91) | −0.64 (−1.27, −0.01) |
| Cross-section, never-Medicaid | 1.54 (3.93) | 1.79 (4.90) | 1.16 (3.60) | 1.53 (4.66) | 0.00 (−0.23, 0.22) |
| Younger children | |||||
| DMFTnew | |||||
| Panel | 0.49 (1.39) | 0.52 (1.56) | 0.32 (0.94) | 0.31 (0.93) | 0.07 (−0.08, 0.23) |
| Cross-section | 0.56 (1.53) | 0.76 (1.99) | 0.41 (1.20) | 0.77 (2.21) | −0.16 (−0.33, 0.02) |
| Cross-section, ever-Medicaid | 0.66 (1.64) | 0.89 (2.15) | 0.49 (1.29) | 0.94 (2.45) | −0.22 (−0.46, 0.01) |
| Cross-section, never-Medicaid | 0.42 (1.36) | 0.63 (1.82) | 0.27 (1.01) | 0.49 (1.62) | 0.04 (−0.15, 0.22) |
| DMFSnew | |||||
| Panel | 1.48 (5.08) | 1.63 (6.02) | 0.99 (3.44) | 0.94 (3.45) | 0.43 (−0.22, 1.09) |
| Cross-section | 1.66 (5.69) | 2.57 (7.91) | 1.31 (4.55) | 2.91 (9.43) | −0.70 (−1.49, 0.09) |
| Cross-section, ever-Medicaid | 1.96 (5.99) | 3.04 (8.56) | 1.56 (4.92) | 3.66 (10.65) | −1.03 (−2.05, −0.01) |
| Cross-section, never-Medicaid | 1.23 (5.25) | 2.10 (7.16) | 0.88 (3.85) | 1.68 (6.52) | 0.30 (−0.59, 1.18) |
Note: Boldface indicates statistical significance (p<0.05).
Weighted by inverse probability of treatment weights.
Difference-in-differences models were fit with generalized estimating equations weighted by inverse probability of treatment weights with variables for group (Philadelphia=1, control=0), period (pre-tax=0, post-tax=1), and a group
period interaction, which estimated the difference-in-differences.
In the older child/adult panel, there were no differences-in-differences in DMFTnew (DD=−0.02, 95% CI: −0.08, 0.03) or DMFSnew (DD=−0.06, 95% CI: −0.29, 0.17) in Philadelphia versus control (Table 2; Figure 1; graphs of difference between cities in Appendix Figure 1), with similar findings in the cross-sectional sample (DMFTnew: DD=−0.05, 95% CI: −0.11, 0.01; DMFSnew: DD=−0.11, 95% CI: −0.37, 0.14). There were, however, differences-in-differences among ever-Medicaid older children/adults (DMFTnew: DD=−0.18, 95% CI: −0.34, −0.03; DMFSnew: DD=−0.64, 95% CI: −1.27, −0.01) (Table 2; Appendix Figure 2). This translated to a decline of −21.7% (95% CI: −36.5, −3.4) for DMFTnew and −24.1% (95% CI: −41.7, −1.2) for DMFSnew. There were no associations among never-Medicaid patients or when stratifying by gender (Appendix Table 4). Results were similar in all sensitivity analyses but were stronger for DMFTnew in the panel and cross-sectional sample when removing Philadelphia patients living in zip codes on the city border (e.g., panel: DD=−0.06, 95% CI: −0.12, 0.00) (Appendix Table 5). Truncating weights at the 99th percentile improved covariate balance (Appendix Table 6).
Figure 1. Difference-in-differences in dental outcomes among adults after Philadelphia beverage tax implementation.
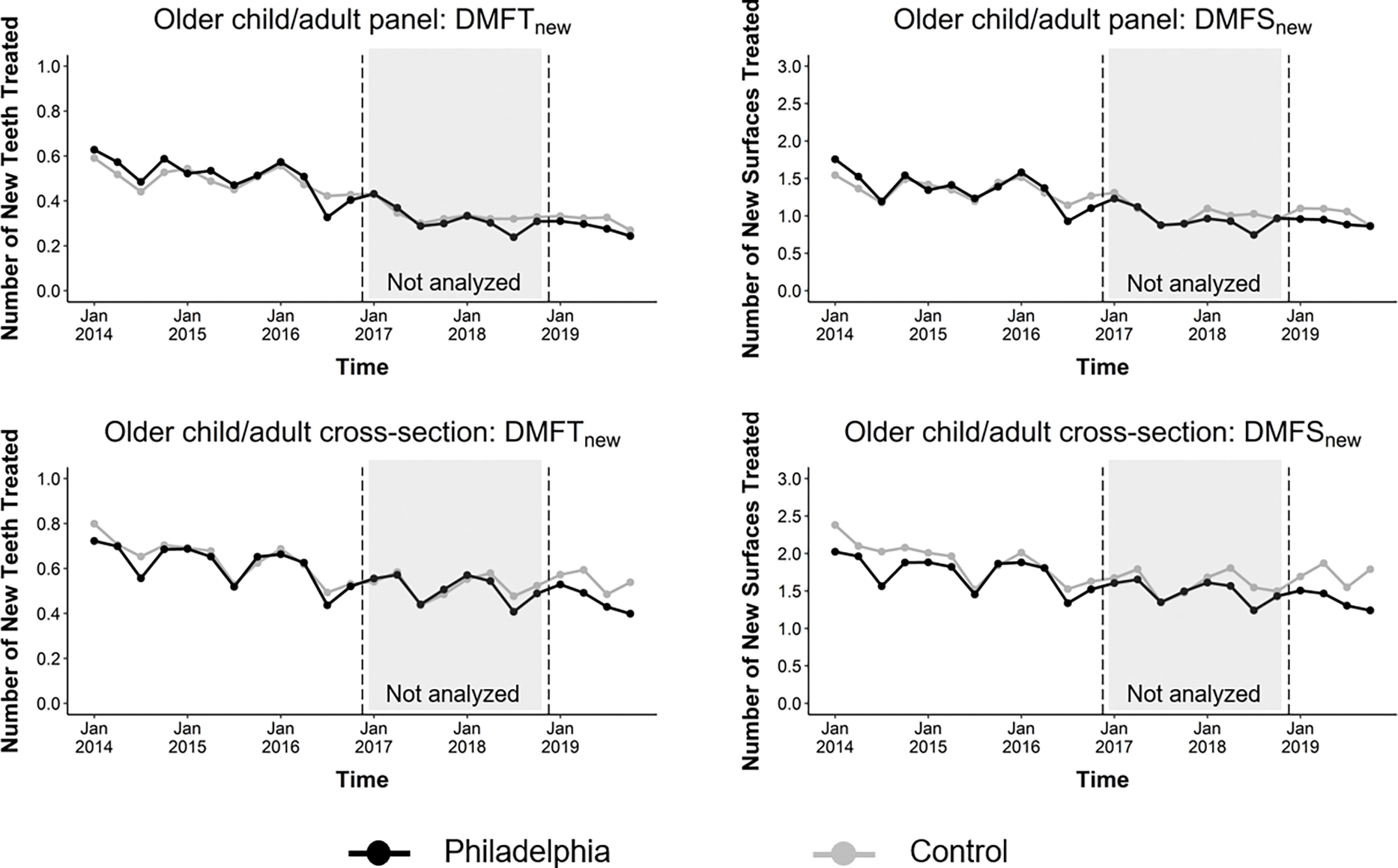
The graphs show mean changes in DMFTnew and DMFSnew among Philadelphia (black) and control (grey) adult patients in the panel and cross-sectional samples.
There were no difference-in-differences in tooth decay in the younger child panel (DMFTnew: DD=0.07, 95% CI: −0.08, 0.23; DMFSnew: DD=0.43, 95% CI: −0.22, 1.09). The cross-sectional analysis revealed larger (though not statistically significant) differences-in-differences (DMFTnew: DD=−0.16, 95% CI: −0.33, 0.02; DMFSnew: DD=−0.70, 95% CI: −1.49, 0.09) (Table 2; Figure 2; graphs of difference between cities in Appendix Figure 3). Similar to results in older children/adults, among younger children ever on Medicaid, there was a difference-in-differences of −0.22 (95% CI: −0.46, 0.01) DMFTnew and −1.03 (95% CI: −2.05, −0.01) DMFSnew, translating to declines of −30.1% (95% CI: −46.8, −8.0) and −34.1% (95% CI: −52.3, −8.9), respectively (Table 2; Appendix Figure 4). There were no associations among never-Medicaid younger children or when stratifying by gender (Appendix Table 4). Results were generally similar in sensitivity analyses (Appendix Table 7), though the main results were slightly attenuated when adjusting for Medicaid in the regression models (versus in IPTW). Truncating weights at the 99th percentile improved covariate balance (Appendix Table 5).
Figure 2. Difference-in-differences in dental outcomes among children after Philadelphia beverage tax implementation.
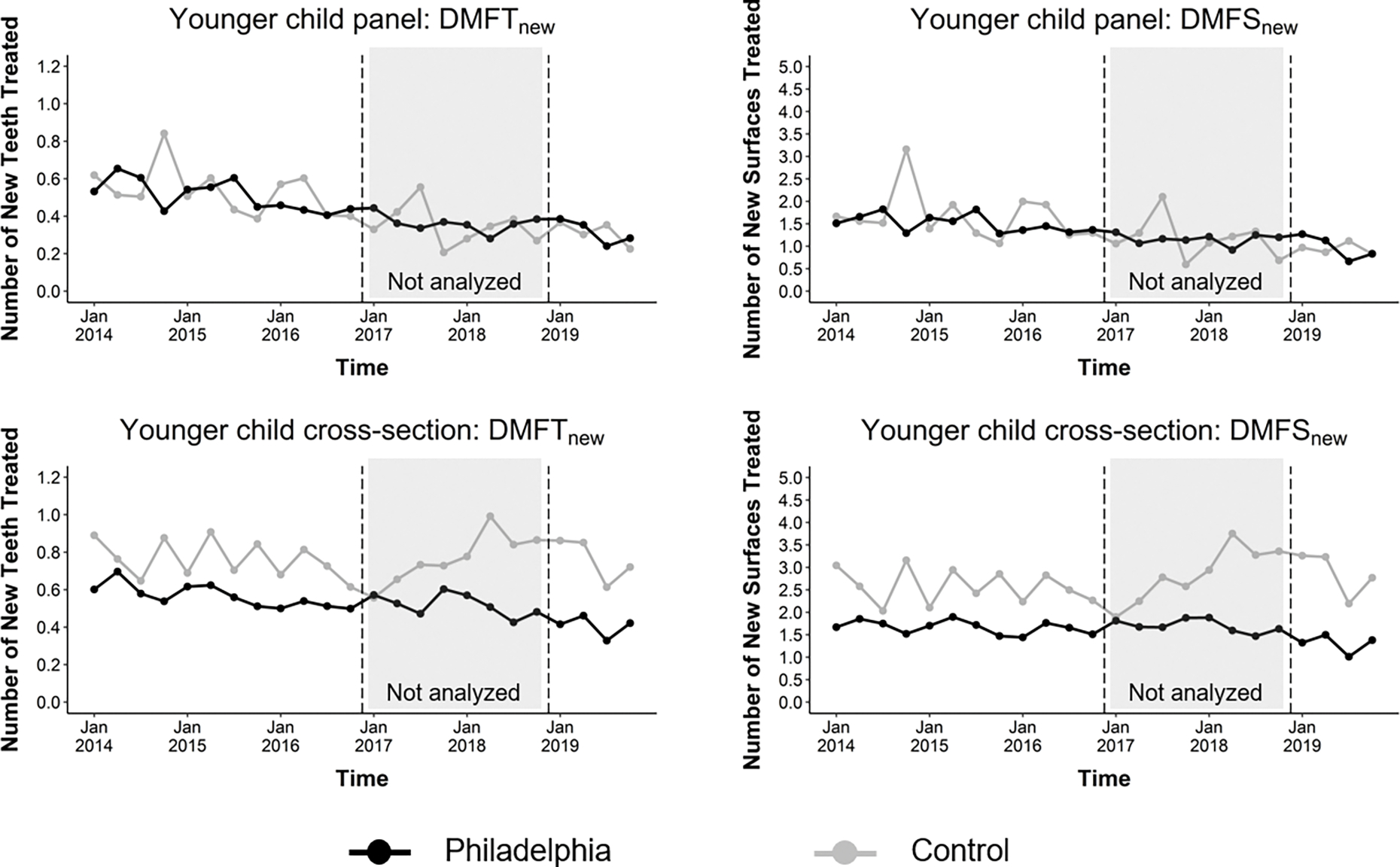
The graphs show mean changes in DMFTnew and DMFSnew among Philadelphia (black) and control (grey) child patients in the panel and cross-sectional samples.
DISCUSSION
Although no overall associations were observed between the Philadelphia beverage tax and tooth decay measures, the tax was on average associated with 22–24% (older children/adults) and 30–34% (younger children) reductions in tooth decay measures among those ever on Medicaid, which is available only to lower-income households. In Philadelphia, 21% of older children/adults and 56% of younger children are enrolled in Medicaid,33 and income-related disparities in oral health are well established.34,35 In this study, the mean pretax tooth decay outcomes were approximately 50–75% higher among ever-Medicaid patients than never-Medicaid patients. The beverage tax may thus increase dental health equity given that improvements were only observed within the lower-income group.
These results are consistent with sweetened beverage tax simulation studies that projected posttax reductions in dental caries and treatment costs, particularly among low-income populations.18–20 Similar results were also observed in an evaluation of Mexico’s tax,21 which found posttax reductions in oral health outpatient visits, 0.31 fewer DMFT in children (6–19 years), and 0.57 fewer DMFT in adults (≥20 years). These larger effects may be because Mexico simultaneously passed an 8% tax on nonessential energy-dense foods,36 which likely also contributed to dental health improvements. These taxes affected the entire country and so could not easily be avoided with cross-border shopping. Additionally, Mexico had higher per capita baseline SSB consumption and prevalence of untreated caries than the U.S.21 The present study’s findings among ever-Medicaid patients were in the same overall direction but with lower magnitude. Gracner et al., which is one of the only other studies to analyze health outcomes after tax implementation, observed a 1.3% reduction in overweight or obesity prevalence in girls per 10% increase in SSB prices following Mexico’s sweetened beverage tax.32 Additional research examining associations between beverage taxes and dental and nutrition-related health outcomes, particularly among lower-income populations, is needed.
The observed dental health improvements in the ever-Medicaid patients may be explained by greater posttax reductions in SSB intake in this population, who may be more sensitive to price increases than higher-income groups because higher prices represent a larger proportion of their income. Similar percent declines in SSB intake across lower and higher income groups could produce larger health effects in lower-income groups because they are likely to have greater baseline SSB intake and tooth decay.8,9 Some,37–39 but not all24,40 previous studies have observed stronger posttax reductions in sales among lower-income groups, though most U.S. studies have not stratified by income.4 Other nutrition policies, such as the 2010 Healthy, Hunger-Free Kids Act, have also been more strongly associated with improved health outcomes (e.g., reduced obesity prevalence) among lower SES versus higher SES populations,41,42 perhaps owing to baseline disparities in diet and health. The present study’s results were robust to stratifying by time-varying Medicaid status (versus ever-Medicaid status) and when excluding patients from New Jersey, which has slightly different Medicaid eligibility requirements than Pennsylvania. Additionally, although the cross-sectional analyses could be biased if the Medicaid population changed differently over time between groups, the sample was similar on all measured covariates over time between groups after applying IPTW.
Limitations
This study has several limitations. First, there may be measurement error of DMFTnew and DMFSnew because EDRs were not available before 2014 and some teeth/surfaces that were counted as newly treated may have been previously treated. Moreover, procedure codes do not directly reflect decay. In addition, some dental providers were students, who might be more prone to errors when documenting dental decay, but we would not expect such errors to vary by study group. Second, there may have been treatment contamination if patients who lived in one study group frequently consumed beverages purchased in the other (e.g., if patients lived in a control area but worked in Philadelphia). This could have attenuated associations in the overall sample; when excluding Philadelphia patients living in border zip codes (who may have more easily avoided the tax), we observed slightly stronger DMFTnew results in adults. The public health effects of beverage taxes therefore might increase if they were implemented at a state or national level to limit tax avoidance. Third, IPTW did not achieve balance on all covariates, but pretax parallel trends were observed for all analyses after weighting, satisfying the difference-in-differences requirement. Truncating weights at the 99th percentile (versus 95th) produced better covariate balance and overall similar results. Another potential limitation is the modest sample size of the panel data, which may have prevented detection of small associations in the overall sample. Additionally, outcomes from 2020 and later were excluded because of COVID-19-related changes in dental care utilization, which further limited the sample size. Recent evidence indicates that the pandemic was associated with increases in SSB consumption among families experiencing financial hardship45 and declines in children’s oral health,43,44 suggesting a need for future research on the post-pandemic effects of beverage taxes. Lastly, stratified analyses were not possible in the panel data given the smaller sample sizes, though those analyses would have been less vulnerable to changing sample composition than the cross-sectional analyses.
CONCLUSIONS
This study of dental records from 83,260 patients found reduced tooth decay measures in adults and children on Medicaid 3 years after implementation of the Philadelphia beverage tax, though no changes were observed in the general population. These findings suggest potential health benefits of the tax among low-income populations. More studies examining the association between sweetened beverage taxes and other health outcomes are needed.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Susan Schlussler for help with data collection.
Funding sources:
This study was supported by R01 DK123624 from NIDDK (PIs: CAR and LAG). The funders did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of interest statement: No conflicts of interest have been reported by the authors this paper.
Financial disclosures statement: No financial disclosures have been reported by the authors of this paper.
CREDIT STATEMENT
Joshua Petimar: methodology, software, formal analysis, data curation, writing – original draft, writing – review & editing, visualization; Laura A. Gibson: conceptualization, methodology, supervision, funding acquisition, writing – review and editing; Mark S. Wolff: methodology, writing – review and editing; Nandita Mitra: methodology, writing – review and editing; Patricia Corby: methodology, writing – review and editing; Gary Hettinger: methodology, validation, writing – review and editing; Emily F. Gregory: funding acquisition, writing – review and editing; Emma Edmondson: funding acquisition, writing – review and editing; Jason P. Block: funding acquisition, writing – review and editing; Christina A. Roberto: conceptualization, methodology, supervision, funding acquisition, writing – review and editing
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Malik VS, Hu FB. The role of sugar-sweetened beverages in the global epidemics of obesity and chronic diseases. Nat Rev Endocrinol. 2022;18(4):205–218. doi: 10.1038/s41574-021-00627-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2012;346:e7492. doi: 10.1136/bmj.e7492 [DOI] [PubMed] [Google Scholar]
- 3.Chi DL, Scott JM. Added Sugar and Dental Caries in Children: A Scientific Update and Future Steps. Dent Clin North Am. 2019;63(1):17–33. doi: 10.1016/j.cden.2018.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andreyeva T, Marple K, Marinello S, Moore TE, Powell LM. Outcomes Following Taxation of Sugar-Sweetened Beverages: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022;5(6):e2215276. doi: 10.1001/jamanetworkopen.2022.15276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edmondson EK, Roberto CA, Gregory EF, Mitra N, Virudachalam S. Association of a Sweetened Beverage Tax With Soda Consumption in High School Students. JAMA Pediatr. 2021;175(12):1261–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened Beverage Consumption Among U.S. Adults, 2011–2014. NCHS data brief. 2017;(270):1–8. [PubMed] [Google Scholar]
- 7.Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened Beverage Consumption Among U.S. Youth, 2011–2014. NCHS data brief. 2017;(271):1–8. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Get the facts: sugar-sweetened beverages and consumption. Published online 2022. Accessed August 11, 2022. https://www.cdc.gov/nutrition/data-statistics/sugar-sweetened-beverages-intake.html
- 9.Vercammen KA, Moran AJ, Soto MJ, Kennedy-Shaffer L, Bleich SN. Decreasing Trends in Heavy Sugar-Sweetened Beverage Consumption in the United States, 2003 to 2016. J Acad Nutr Diet. 2020;120(12):1974–1985.e5. doi: 10.1016/j.jand.2020.07.012 [DOI] [PubMed] [Google Scholar]
- 10.Fleming E, Afful J. Prevalence of Total and Untreated Dental Caries Among Youth: United States, 2015–2016. National Center for Health Statistics; 2018. [PubMed] [Google Scholar]
- 11.Dye BA, Thornton-Evans G, Li X, Iafolla TJ. Dental Caries and Tooth Loss in Adults in the United States, 2011–2012. National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 12.Williams S, Wei L, Griffin SO, Thornton-Evans G. Untreated caries among US working-aged adults and association with reporting need for oral health care. J Am Dent Assoc. 2021;152(1):55–64. doi: 10.1016/j.adaj.2020.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012;102(9):1729–1734. doi: 10.2105/AJPH.2011.300478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jackson SL, Vann WF, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heilmann A, Tsakos G, Watt RG. Oral Health Over the Life Course. In: A Life Course Perspective on Health Trajectories and Transitions. Springer; Cham; 2015:39–59. [Google Scholar]
- 16.Cheng F, Zhang M, Wang Q, et al. Tooth loss and risk of cardiovascular disease and stroke: A dose-response meta analysis of prospective cohort studies. PLoS One. 2018;13(3):e0194563. doi: 10.1371/journal.pone.0194563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu K, Yu W, Li Y, et al. Association between tooth loss and hypertension: A systematic review and meta-analysis. J Dent. Published online June 2, 2022:104178. doi: 10.1016/j.jdent.2022.104178 [DOI] [PubMed] [Google Scholar]
- 18.Schwendicke F, Thomson WM, Broadbent JM, Stolpe M. Effects of Taxing Sugar-Sweetened Beverages on Caries and Treatment Costs. J Dent Res. 2016;95(12):1327–1332. doi: 10.1177/0022034516660278 [DOI] [PubMed] [Google Scholar]
- 19.Jevdjevic M, Trescher AL, Rovers M, Listl S. The caries-related cost and effects of a tax on sugar-sweetened beverages. Public Health. 2019;169:125–132. doi: 10.1016/j.puhe.2019.02.010 [DOI] [PubMed] [Google Scholar]
- 20.Sowa PM, Birch S. The effects of a sugar-sweetened beverage tax: moving beyond dental health outcomes and service utilisation. Health Econ Policy Law. Published online August 2, 2022:1–15. doi: 10.1017/S1744133122000147 [DOI] [PubMed] [Google Scholar]
- 21.Hernández-F M, Cantoral A, Colchero MA. Taxes to Unhealthy Food and Beverages and Oral Health in Mexico: An Observational Study. Caries Res. 2021;55(3):183–192. doi: 10.1159/000515223 [DOI] [PubMed] [Google Scholar]
- 22.City of Philadelphia Sugar-Sweetened Beverage Tax. Chapter 19–4100 of the Philadelphia Code. Bill No. 160176. [Google Scholar]
- 23.Petimar J, Gibson LA, Yan J, et al. Sustained Impact of the Philadelphia Beverage Tax on Beverage Prices and Sales Over 2 Years. Am J Prev Med. 2022;62(6):921–929. doi: 10.1016/j.amepre.2021.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seiler S, Tuchman A, Yao S. The impact of soda taxes: pass-through, tax avoidance, and nutritional effects. J Mark Res. 2020;58(1):22–49. [Google Scholar]
- 25.Center for Health Care Strategies, Inc. Medicaid Adult Dental Benefits: An Overview; 2019. Accessed January 18, 2023. https://www.chcs.org/media/Adult-Oral-Health-Fact-Sheet_091519.pdf
- 26.Shulman JD, Cappelli DP. Epidemiology of Dental Caries. In: Prevention in Clinical Oral Health Care. Mosby Elsevier; 2008:2–13. [Google Scholar]
- 27.Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013;48(2 Pt 1):539–559. doi: 10.1111/j.1475-6773.2012.01449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robert Graham Center. Social Deprivation Index (SDI). Published online 2021. Accessed June 24, 2022. https://www.graham-center.org/maps-data-tools/social-deprivation-index.html
- 29.Kaiser Family Foundation. Medicaid/CHIP Eligibility Limits. Published online 2022. Accessed July 5, 2022. https://www.kff.org/state-category/medicaid-chip/medicaidchip-eligibility-limits/
- 30.Wing C, Simon K, Bello-Gomez RA. Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annu Rev Public Health. 2018;39:453–469. doi: 10.1146/annurev-publhealth-040617-013507 [DOI] [PubMed] [Google Scholar]
- 31.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. doi: 10.1002/sim.6607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gracner T, Marquez-Padilla F, Hernandez-Cortes D. Changes in Weight-Related Outcomes Among Adolescents Following Consumer Price Increases of Taxed Sugar-Sweetened Beverages. JAMA Pediatr. 2022;176(2):150–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.City of Philadelphia Department of Public Health. Staying Healthy: Access to Primary Care in Philadelphia. Published online 2018. Accessed July 5, 2021. https://www.phila.gov/media/20181109113640/2018-PrimaryCareReportFINAL.pdf
- 34.Gupta N, Vujicic M, Yarbrough C, Harrison B. Disparities in untreated caries among children and adults in the U.S., 2011–2014. BMC Oral Health. 2018;18(1):30. doi: 10.1186/s12903-018-0493-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moss ME, Luo H, Rosinger AY, Jacobs MM, Kaur R. High sugar intake from sugar-sweetened beverages is associated with prevalence of untreated decay in US adults: NHANES 2013–2016. Comm Dent Oral Epid. 2022;50(6):579–588. doi: 10.1111/cdoe.12725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Batis C, Rivera JA, Popkin BM, Taillie LS. First-Year Evaluation of Mexico’s Tax on Nonessential Energy-Dense Foods: An Observational Study. PLoS Med. 2016;13(7):e1002057. doi: 10.1371/journal.pmed.1002057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bleich SN, Dunn CG, Soto MJ, et al. Association of a Sweetened Beverage Tax With Purchases of Beverages and High-Sugar Foods at Independent Stores in Philadelphia. JAMA Netw Open. 2021;4(6):e2113527. doi: 10.1001/jamanetworkopen.2021.13527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. In Mexico, Evidence Of Sustained Consumer Response Two Years After Implementing A Sugar-Sweetened Beverage Tax. Health Aff (Milwood). 2017;36(3):564–571. doi: 10.1377/hlthaff.2016.1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colchero MA, Molina M, Guerrero-López CM. After Mexico Implemented a Tax, Purchases of Sugar-Sweetened Beverages Decreased and Water Increased: Difference by Place of Residence, Household Composition, and Income Level. J Nutr. 2017;147(8):1552–1557. doi: 10.3945/jn.117.251892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cawley J, Frisvold D, Hill A, Jones D. The impact of the Philadelphia beverage tax on purchases and consumption by adults and children. J Health Econ. 2019;67:102225. doi: 10.1016/j.jhealeco.2019.102225 [DOI] [PubMed] [Google Scholar]
- 41.Kenney EL, Barrett JL, Bleich SN, Ward ZJ, Cradock AL, Gortmaker SL. Impact Of The Healthy, Hunger-Free Kids Act On Obesity Trends. Health Aff (Millwood). 2020;39(7):1122–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Richardson AS, Weden MM, Cabreros I, Datar A. Association of the Healthy, Hunger-Free Kids Act of 2010 With Body Mass Trajectories of Children in Low-Income Families. JAMA Netw Open. 2022;5(5):e2210480. doi: 10.1001/jamanetworkopen.2022.10480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lyu W, Wehby GL. Effects of the COVID-19 pandemic on children’s oral health and oral health care use. J Am Dent Assoc. 2022;153(8):787–796.e2. doi: 10.1016/j.adaj.2022.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matsuyama Y, Isumi A, Doi S, Fujiwara T. Impacts of the COVID-19 pandemic exposure on child dental caries: Difference-in-differences analysis. Caries Res. Published online November 28, 2022. doi: 10.1159/000528006 [DOI] [PubMed] [Google Scholar]
- 45.Pulvera R, Altman E, Avina L, Thompson H, Schillinger D, Madsen K. Pandemic-related financial hardship and disparities in sugar-sweetened beverage consumption and purchasing among San Francisco Bay Area residents during COVID-19. Prev Med Rep. 2022;26:101759. doi: 10.1016/j.pmedr.2022.101759 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


