Abstract
Background:
In the US, sexual and gender minority (SGM) individuals continue to experience health inequities, and nursing curricula content and nursing faculty with SGM health expertise in the US remain limited. Addressing health disparities begins with the preparation of future nurses—US nursing faculty must be supported to meet these growing needs.
Purpose:
To describe, appraise, and synthesize research from 2000-2020 on US nursing faculty knowledge, awareness, inclusion, and perceived importance of SGM health content.
Method:
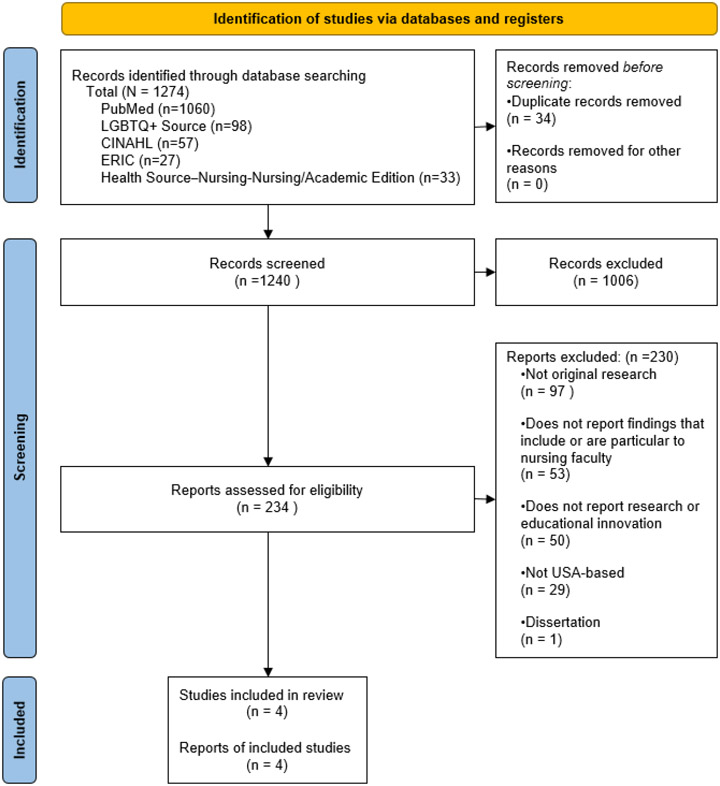
Following PRISMA 2020 guidelines, we registered a systematic review and appraisal protocol in PROSPERO, and then executed the protocol and synthesized the literature.
Findings:
Only four cross-sectional, descriptive empirical articles fit the a priori inclusion criteria. The studies were of moderate quality at best and often relied on unvalidated or older measures. In general, the studies focused on examining characteristics of nursing programs, faculty comfort with content, faculty perceptions of content importance, and hours dedicated to content.
Discussion:
Since the close of the review, new commentaries and editorials expanding the call for change in the US were published—the time for commentary has passed. We found an empirical evidence base surrounding US nursing faculty and SGM health much more limited than expected. It remains unclear whether US nursing faculty are adequately prepared to educate future nurses about SGM health issues—and an unprepared healthcare workforce is yet another barrier to SGM health equity. The evidence base supporting US nursing faculty development desperately needs more studies using rigorous methodologies.
Keywords: Sexual and Gender Minorities, Nursing Education, Faculty, Curriculum, Equity, Health Disparities
Introduction
Sexual or gender minority (SGM) is a universal umbrella term used in the clinical and research domains to describe populations, including but not limited to lesbian, gay, bisexual, transgender, genderqueer, and Two-spirit persons. When compared with cisgender and heterosexual persons, SGM populations experience increased stigma related health disparities and a greater burden of mental health issues, substance use, chronic diseases (e.g. HIV, diabetes), and certain malignancies (Agénor, 2015; Caceres et al., 2020; Cochran et al., 2016; Committee on Understanding the Well-Being of Sexual and Gender Diverse Populations et al., 2020; Fish, 2022; Meyer et al., 2017; Moore et al., 2021; Streed et al., 2021). Data show that these disparities contribute to decreased healthcare access and utilization, in part because of fear of negative attitudes of healthcare providers, including nurses (Felner et al., 2018; Macapagal et al., 2016; White Hughto et al., 2016). With SGM individuals now comprising 7.1% of the US population (an estimated 23.5 million individuals based on 2020 US Census results) the US health system is at a critical turning point requiring the preparation and implementation of SGM-inclusive policies and practices (Jones, 2022; Vespa et al., 2020). The nursing profession must rise to meet the growing need for a professional nursing workforce that is prepared to deliver compassionate SGM-inclusive care across all care settings, at all levels of practice and through inclusive education, research, policy, and advocacy (Hughes et al., 2022).
The 2010 report The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding produced by the National Academies of Science, Engineering, and Medicine [NASEM] (né Institute of Medicine) identified LGBT Health as an area of great need for further study and development in US healthcare. The need for attention to SGM care again was highlighted by NASEM in their 2020 report Understanding the Well-Being of LGBTQI+ Populations (Committee on Understanding the Well-Being of Sexual and Gender Diverse Populations et al., 2020; Institute of Medicine, 2011). LGBT population health was included as a distinct topic area in the US Department of Health and Human Services Healthy People 2020 and 2030 programs (Healthy People 2020 ∣, n.d.; Healthy People 2030 ∣ Health.Gov, n.d.). Yet in the context of both repeated calls from respected institutions and persistent, long-established health disparities among SGM populations, there has been limited focus on the health and well-being of SGM populations within the bodies that govern the education, licensure, credentialing, and accreditation of nurses and schools of nursing in the US. However, broad statements endorsing underserved and population-based health have been made. Specifically, the Future of Nursing 2020-2030 report calls for a nursing education evolution that includes addressing health equity through competencies for varied populations and diverse backgrounds (National Academies of Sciences, Engineering, and Medicine, 2021). Also, the American Association of Colleges of Nursing (AACN)’s new Essentials aims to integrate diversity, equity, and inclusion throughout all of the domains and learning experiences across curricula in order to be integrated across all spheres of care (AACN, 2021). Specifically, the AACN Essentials aim to support “nursing workforce development to prepare graduates who contribute to the improvement of access and care quality for underrepresented and medically underserved populations (p. 5)” (AACN, 2021). As seen in these examples, governing entities continuously fail to provide any comprehensive guidance on how to support the faculty who are in the classrooms and labs and clinical rotations preparing future nurses. Thus, nursing has been slow to advance any broad priorities in this area (Hughes et al., 2022).
It is also well documented that nursing lags behind other healthcare professions in addressing SGM health disparities (Burton et al., 2021; De Guzman et al., 2018; Harrell & Sasser, 2018; Ray King et al., 2021). As the largest segment of the healthcare workforce and the most trusted profession for two decades, nursing has a mandate to take a leading role in providing high quality care for SGM individuals, families, and communities in order to lessen the burden of SGM health inequities. Although the inclusion of care for diverse populations is a large focus of the Future of Nursing 2020-2030 report, the 2021 American Association of Colleges of Nursing (AACN) Essentials do not identify ‘diversity, equity, and inclusion’ as one of the 10 domains of the professional nursing practice framework. Rather ‘diversity, equity, and inclusion’ are listed as a core concept. While AACN states the core concepts are “not of ‘lesser importance’[sic] than a domain,” (AACN, 2021, p.12) this categorization misses an important opportunity to center ‘diversity, equity, and inclusion’ as essential to professional practice nursing by codifying standards for curricular commitment to the area.
To our knowledge, this is the first systematic review to examine US nursing faculty perceptions, attitudes, and behaviors related to SGM health content and its inclusion in the curricula of US schools of nursing. The purpose of this systematic review of literature was to gather, describe, appraise, and synthesize research literature from the past 20 years regarding the knowledge, awareness, inclusion, and perceived importance of content related to SGM health among nursing faculty in the US. This systematic review was guided by five specific research questions:
RQ1) How much SGM health and wellbeing content is included in nursing curricula?
RQ2) To what extent are competencies for SGM health promotion and wellbeing among nursing faculty addressed in the scientific literature?
RQ3) What SGM health and wellbeing knowledge, attitudes, and competency outcomes describing nursing faculty are measured in the scientific literature?
RQ4) What are the best practices for education of nursing faculty regarding inclusion of SGM health topics in nursing curricula?
RQ5) What are the barriers and facilitators for incorporating SGM health into nursing faculty professional development?
Of our initial five research questions only two (RQ1 & RQ3) were addressed in any way, and the others (RQ2, RQ4, & RQ5) remain open questions that need to be answered. There were several other important areas of inquiry that these reports addressed that do have direct relevance to our review’s purpose which also provide important context related to the state of nursing science related to this important topic.
Methods
Search Strategy and Selection of Articles
We developed and registered a systematic review search protocol on Prospero, CRD42020201475 (Nursing Faculty Education for LGBTQ+ Health: An Integrative Review, n.d.). We executed the protocol and conducted electronic searches spanning January 2000 through June 4, 2020 using the following databases: PubMed, LGBT Health, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Education Resources Information Center (ERIC), and Health Source-Nursing Nursing/Academic Edition on June 4, 2020. Search terms included three categories of terms: nursing, education, and sexual and gender minority. For a full formatted list of search terms by database please refer to the supplemental file. Inclusion criteria were: 1) English language peer-reviewed original research articles, 2) studies conducted in the US, and 3) results include perceptions or attitudes of nursing faculty/academic nursing leadership [OR] characteristics of nursing curricula (e.g., evaluation/description of gaps, knowledge/content, skills, attitudes/beliefs) related to LGBTQ+ health and well-being, [OR] barriers and facilitators to integrating SGM curricular content. To ensure that we were only including data-based, peer reviewed scientific publications with a complete record of methods and measures for evaluation our exclusion criteria were: 1) literature reviews, dissertations, theses, or DNP projects, 2) grey literature (e.g., white papers, government documents), and 3) abstracts.
From the very outset of protocol development, our team made the specific choice to focus only on the US literature because the environment within US higher education is demonstrably different from the environments in other countries (e.g., “Don’t say gay” legislation proposed in several US states). Additionally, US schools of nursing are overseen by certifying bodies that are US-specific making the preparedness of US faculties particularly relevant to informing those bodies’ policies and guidelines.
Each title and abstract was screened for inclusion by two independent reviewers on the Covidence Systematic Review platform (www.covidence.org). Conflicts were resolved by a third reviewer. Articles meeting eligibility criteria underwent a full-text review by two independent reviewers. Any disagreement regarding inclusion was resolved by a third reviewer and any uncertainty about a given article was resolved by lead investigators (authors Moore and Coleman).
Data Extraction, Analysis, and Synthesis
Data extraction was completed by five team members using a standardized data extraction tool developed for this review by the research team. Data extraction from each article included: study aims, research questions, hypotheses, sample characteristics (e.g. demographic characteristics), nursing role descriptors for samples (e.g., faculty, deans, directors), inclusion criteria, exclusion criteria, independent variable concepts, dependent variable concepts, items or measures specific to SGM populations beyond those demographic measures (e.g., measure of SGM health and well-being knowledge), descriptions of interventions, study findings, limitations, and additional information relevant to the systematic review research questions.
Following data extraction, a quality audit of 25% of the records was completed by a second reviewer. Extraction quality was measured using a Likert-type rating scale from 100%-0%, with an a-priori minimum threshold of 75% overall agreement. Any article extraction that had a quality level rated at less than 75% would have been completely redone followed by another quality audit. Those with less than 100% quality were revised to correct missing or incompleteness and then reviewed by one of the lead authors (Moore or Coleman). The extraction quality for this review was rated at 100%, indicating that the second reviewer assessed the data extracted to be an accurate representation of the article.
To enable us to make the most of the small yet very heterogenous set of articles in our sample we utilized narrative review approach strategies for preliminary synthesis development and exploration of relationships among and between studies allowing comparison and evaluation of the articles both individually and collectively (Popay et al., 2006).
Risk of Bias and Quality Assessment
Two reviewers independently conducted quality and bias appraisal of the articles using an augmented version of the Mixed Methods Appraisal Tool (MMAT) Version 2018 (Hong et al., 2019). Based on a comparison of the MMAT with previous reviews examining key elements in tools for risk of bias/quality assessment (Katrak et al., 2004; Ma et al., 2020) the investigative team incorporated themes and items from other established appraisal tools to address important missing factors. All of the items included in the 2018 version of the MMAT were included with some questions enhanced to better capture concerns of quality and bias in qualitative, quantitative nonrandomized, and quantitative descriptive studies. Items related to these types of studies were improved by revising the criteria from the MMAT to incorporate key concepts from three other quality and bias appraisal tools. Specific items changed and the source of changes are described below. To better assess for quality and bias within qualitative studies we incorporated portions of the Joanna Briggs Institute’s Critical Appraisal Checklist for Qualitative Research (JBICACQR, Lockwood et al., 2020). Specifically, MMAT 2018 version criteria 1.5 was revised to include coherence with ‘conclusion’ to improve alignment of the item with JBICACQR item 10, and we also added JBICACQR items 6-9 to the criteria for qualitative study appraisal. To better evaluate the quality and risk of bias in quantitative nonrandomized and descriptive studies we adapted items 3.1 and 4.2 to include language related to ‘specified and defined’ study populations based on criteria 2 of the NIH Study Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (Study Quality Assessment Tools ∣ NHLBI, NIH, n.d.; https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). From the same assessment tool we added criteria 5, related to sample size justification, to those criteria for quantitative nonrandomized and quantitative descriptive studies. We also added a ‘does not apply’ option to the possible ratings for all of the criteria.
Quality and risk of bias appraisals were conducted by four team members with each study being reviewed by two reviewers. Any discrepancies were resolved in video conference meetings among the reviewers. Any discrepancies that remained unresolved following the video conference were adjudicated by the first author.
Percentage of Reports Meeting Criteria.
The MMAT developers do not recommend scoring studies based on criteria ratings (Hong et al., 2019). We did, however, calculate a figure reflecting the ‘percentage of reports meeting criteria’ in the interest of identifying trends in quality among included studies The ‘percentage of reports meeting criteria’ was calculated for each criteria by: 1) Identifying the number of studies for which the criterion was applicable by subtracting the count of those studies for which the criterion was rated ‘does not apply’ by two reviewers from the total sample; 2) Calculating the number of studies that met each criterion; this is a count of those articles with a rating of ‘Yes’ with any articles rated as either ‘No’ or ‘Can’t Tell’ left uncounted; and 3) Dividing the number of studies meeting the criterion by the total number to which the criterion is applicable and multiplying the dividend by 100 to result in percentage of reports meeting criteria.
Findings
Search results are shown in the PRISMA 2020 Flow Diagram (see Figure 1). There were n = 230 articles excluded during full-text review with the majority of those being excluded because they did not report original research (n = 97). The final sample consisted of 4 study reports meeting all inclusion criteria.
Figure 1.
Prisma Flow Diagram
Description of Studies Reviewed
General characteristics of the articles are included in Table 1. All studies included a nurse author and were published between 2013 and 2017 in nursing education-focused journals. Three of the four (Cornelius et al., 2017; Sirota, 2013; Walsh & Hendrickson, 2015) were published in the same journal. All four articles reported research that used cross-sectional, descriptive survey methods with data collected from among faculty, deans, and nursing program directors. One study (Sirota, 2013) specifically focused on nursing faculty attitudes towards lesbian and gay people. Another focused on Texas nursing faculty attitudes towards transgender individuals and their health (Walsh & Hendrickson, 2015). The third focused on inclusion of SGM content in curricula of North Carolina nursing programs (Cornelius et al., 2017). The fourth focused on inclusion of SGM-related content in nursing curricula (Aaberg, 2016).
Table 1.
Design Characteristics of Reviewed Studies
| Authors | Aaberg (2016) | Cornelius, Enwaana, Alston, & Baldwin (2017) | Sirota (2013) | Walsh & Hendrickson (2015) |
|---|---|---|---|---|
| Recruitment, Population, Data Collection Method | Email recruitment Purposive selection of 300 individual faculty identified from the websites of AACN accredited baccalaureate nursing programs with a minimum of 2 faculty invited from each state in the US Internet Survey (SurveyMonkey) |
Mailed Survey with one reminder 4-weeks later Deans and directors from nursing education programs listed on the North Carolina Board of Nursing website were invited to participate Paper Survey Instrument |
Email recruitment 6,766 individuals invited to participate representing all faculty listed on the websites of CCNE accredited colleges of nursing Internet Survey (SurveyMonkey |
Email recruitment 111 individuals listed as contacts for the Texas Board of Nursing approved professional nursing education programs were invited to participate Internet Survey (SurveyMonkey) |
| Purpose/Aims | To determine how many BSN programs required human sexuality content, the number of hours dedicated, the type of content, and to assess educators’ beliefs about the need for this content. | To identify how LGBT health-related content was integrated into North Carolina schools of nursing curricula and the presence of relevant policies | To describe the attitudes of educators about homosexuality and associated sociodemographic factors . | To identify transgender-related content in nursing curricula |
| Sample Characteristics | N = 44 individual faculty participated There were no characteristic data reported about either respondents or schools |
N=41 Deans and directors of North Carolina nursing programs: Diploma programs n = 2; Associate Degree in Nursing programs n = 27; Bachelor of Science in Nursing programs n = 12 |
N=1,116 individual faculty | N=21 schools of nursing in Texas responded N = 11 completed the entire survey. |
Quality Assessment.
The included reports were of lower quality than would be ideal (see Table 2). In all, clear research questions were provided and reported data collection appeared to be appropriate for the research questions. Only one paper (Sirota, 2013) addressed representativeness of their sample. All four of the studies’ samples are subject to sampling bias limiting the generalizability of their findings. Matters related to SGM health are often associated with strong feelings which may influence survey respondents to either make a point or to be socially desirable. Other potential threats to validity among the included studies include the use of non-validated or older measures with limited to no reliability information.
Table 2.
Individual and Aggregate Quality Assessment of Reviewed Studies
| Aaberg (2016) | Cornelius, Enwaana, Alston, & Baldwin (2017) | Sirota (2013) | Walsh & Hendrickson (2015) | Reports Meeting Criteria |
|
|---|---|---|---|---|---|
| Are there clear research questions? * | Yes | Yes | Yes | Yes | 100% |
| Do the collected data allow to address the research questions? * | Yes | Yes | Yes | Yes | 100% |
| Is the sampling strategy relevant to address the research question? | Yes | Undetermined | Yes | Yes | 75% |
| Was the study population clearly specified and defined, and is the sample representative of the target population? | Undetermined | Undetermined | Yes | No | 25% |
| Was a sample size justification, power description, or variance and effect estimates provided? | Yes | No | Yes | No | 50% |
| Are the measurements appropriate? | No | Yes | Yes | Yes | 75% |
| Is the risk of nonresponse bias low? | No | Undetermined | Undetermined | No | 0% |
| Is the statistical analysis appropriate to answer the research question? | No | Undetermined | Yes | Yes | 50% |
Note:
Initial screening questions included in MMAT
Theoretical Grounding.
Three of the articles did not specify a theoretical framework used to inform the study design, measurement, or analytical choices for their studies. One (Sirota, 2013) identified the Theory of Planned Behavior as the guiding framework for their study of nursing faculty attitudes.
Sampling, Recruitment, and Responsiveness.
The sampling frames for each of the studies was unique; two focused on schools of nursing within single US states, Texas (Walsh & Hendrickson, 2015) and North Carolina (Cornelius et al., 2017). The other two studies recruited samples from nation-wide samples of nursing faculty based on the schools’ status of: accreditation by the Commission on Collegiate Nursing Education (CCNE) (Sirota, 2013) or membership in AACN (Aaberg, 2016). The two state-specific studies used their state Board of Nursing websites to identify the accredited programs in the state. Walsh & Hendrickson (2015) emailed the contacts of record for 111 schools of nursing with Texas Board of Nursing approval. There were 21 responses to the survey resulting in an 18.9% response rate. Cornelius et al. (2017) directly solicited participation from 70 deans and heads of nursing programs of accredited schools listed on the North Carolina Board of Nursing website. They had 41 surveys returned for a 58.6% response rate. Of the remaining studies, Sirota (2013) identified their population as nursing faculty listed on CCNE accredited schools of nursing websites. They sent 6,766 invitations and had an 18.9% response rate (n = 1,282). Aaberg (2016) reported that their sampling frame consisted of faculty of nursing at AACN member schools further specifying their recruitment focused on ‘individuals who would be knowledgeable about the curriculum of their nursing program’ (p. 15). They report a 14.67% response rate with 44 of 300 responding. Three studies recruited participants by email (Aaberg, 2016; Sirota, 2013; Walsh & Hendrickson, 2015) and one mailed recruitment materials to deans and program heads (Cornelius et al., 2017).
Each of the studies included faculty in pre-licensure programs, but only one reported results by nursing education program type (Cornelius et al., 2017). Sirota (2013) included faculty from baccalaureate, master’s, doctoral (PhD and DNP), and post-graduate nurse practitioner certificate programs, however, the results were not stratified by program type. Across all studies the level of reporting varied with some reporting outcomes at the program level while others reported outcomes at the individual faculty member level. Key findings from the reviewed reports are summarized in Table 3, and then further discussed in the context of the research questions.
Table 3.
Findings of Importance from included reports
| Concept | Aaberg (2016) | Cornelius, Enwaana, Alston, & Baldwin (2017) | Sirota (2013) | Walsh & Hendrickson (2015) |
|---|---|---|---|---|
| Perceived preparedness for teaching SGM-related Content | Not Reported | Not Reported | 56.6% faculty reported feeling not at all prepared to teach homosexuality-related content | Not Reported |
| Appropriateness/Importance of LGBT content for Nursing Curriculum. | 32 (86.5%) agree that LGBT Sexual Health is appropriate for nursing curriculum | Not Reported | 78.6% of faculty rated teaching nursing students about sexual minorities as very important to extremely important | Not Reported |
| Time spent on LGBT/SGM content | 0.59 hrs average spent on LGBT sexual health 29 of 39 (74%) reported <1 hr of LGBT sexual health content 11 (28%), reported 0 hrs of LGBT sexual health content |
32 of 41 (78%) reported <5 hrs of LGBT content. 7 of 41 (17%) reported 6 to 10 hrs of LGBT content 1 (2%) reported 11 to 15 hrs of LGBT content |
Not Reported | 1.63 hrs average LGBT content 4 of 15 (26%) reported 0 hrs of LGBT content 0 schools report >4 hrs LGBT content |
| Courses where SGM-related content is taught | Maternal-Newborn 18.5% Medical-Surgical Nursing 46.1% Health Promotion 15.4% Other courses 37% |
Fundamentals of Nursing 37% Health Assessment 32% Health Diversity 27% Medical-Surgical Nursing 24% Psychiatric Nursing 22% Maternal-Child Nursing 17% LGBT Health 2% |
Not Reported | Not Reported |
| Additional Findings | 16% of faculty indicated that graduates of their program are prepared to address sexuality issues with clients. | 85% of respondents reported that their schools did not have any policies regarding students caring for LGBT patients. | ATLG scores indicated mostly positive attitudes towards homosexuality (M =47.2, SD=27.7). 22% indicated much more negative views (ATLG > 99) | >47.6% of schools address ‘transgender or transsexual [sic] individuals’ and 57% report teaching gender identity concepts |
Measures of SGM Health and Wellbeing Knowledge, Attitudes, and Competency Outcomes among Nursing Faculty (RQ3).
Three studies (Aaberg, 2016; Sirota, 2013; Walsh & Hendrickson, 2015) collected data using the internet survey platform SurveyMonkey© and the fourth used a paper and pencil survey (Cornelius et al., 2017). Three used open ended questions in their surveys (Aaberg, 2016; Cornelius et al., 2017; Walsh & Hendrickson, 2015). One study (Aaberg, 2016) conducted qualitative ‘content analysis’ of open-ended responses and reported thematic content as counts and percentages. Only one study (Sirota, 2013) used an established measure of attitudes related to SGM populations. Sirota’s survey had two parts, the first was the Attitudes Towards Lesbians and Gays (ATLG) instrument. The ATLG by Herek from 1994 includes 20 items with response options on a 9-point Likert-type scale; half of the items focus on gay men and half on lesbian women. Higher scores indicated more negative attitudes. Sirota collected information about the nursing faculty participants’ perceptions of their own preparedness to deliver SGM content. None of the included studies identified any nursing faculty competencies for SGM health promotion and wellbeing (RQ 2).
Measures of SGM Health and Wellbeing Content Included in Nursing Curricula (RQ1).
Three studies used author-developed surveys or survey items related to SGM-related content in nursing curricula. Only two reports included the majority of the items included in the surveys (Aaberg, 2016; Walsh & Hendrickson, 2015). Aaberg (2016) reported that their survey had both content and face validity per review by two experts in nursing education and sexuality education; however, only one item was related to LGBT-specific nursing education. Walsh & Hendrickson (2015) developed a survey based on published literature and other sources of information about transgender care, including informal communication with transgender individuals. The survey included 10 yes/no items and two open-ended questions focused on number of classroom hours of LGBT education, and ways to incorporate transgender education. Cornelius et al. (2017) indicated that they developed their 10-item survey based on a review of the literature. The survey consisted of eight Likert-type items (1-not relevant to 4-highly relevant) about curriculum and LGBT health content, another asked what courses included LGBT content, and the last was an open-ended question regarding school policies prohibiting nursing students from caring for LGBT patients in clinicals.
Sexual and Gender Minority Content-related Outcomes Reported.
None of the included reports addressed best practices for nursing faculty education related to inclusion of SGM health content in curricula (RQ4), nor did any of the reports identify barriers and facilitators for incorporating SGM health into nursing faculty professional development (RQ5). The reviewed publications did report several SGM content-related outcomes not included in the initial research questions yet very relevant to describing the current state of the science related to US nursing faculty’s knowledge, awareness, inclusion, and perceived importance of SGM health content. Three reports included measures of SGM health content inclusion among nursing curricula by examining the number of hours in curricula focused on SGM content (Aaberg, 2016; Cornelius et al., 2017; Walsh & Hendrickson, 2015), and two reports also included lists of courses including the SGM health-related content (Aaberg, 2016; Cornelius et al., 2017). There were two reports with results related to nursing faculty’s attitudes towards and perceptions of the relevance, importance, and appropriateness of SGM content for nursing students (Aaberg, 2016; Sirota, 2013). Cornelius also collected information related to school policies regarding students’ caring for LGBT patients.
Barriers and Facilitators to Inclusion of Sexual and Gender Minority Content in Nursing Curricula.
None of the included articles identified facilitators for inclusion of SGM content in nursing curricula. However, three of the four papers in this study collected data about barriers to inclusion of SGM content in the curriculum (see Table 4; Aaberg, 2016; Sirota, 2013; Walsh & Hendrickson, 2015). The most common barriers included the lack of SGM content on the NCLEX (Aaberg, 2016; Walsh & Hendrickson, 2015), the lack of appropriate materials or curricula related to SGM content (Sirota, 2013; Walsh & Hendrickson, 2015), and discomfort with the subject matter (Aaberg, 2016; Sirota, 2013).
Table 4.
Sexual and Gender Minority Content Integration Barriers Identified in Studies
| Not on NCLEXa,c |
| Lacking appropriate curricula and teaching materialsb, c |
| Discomfort with subject mattera, b |
| Time constraintsa |
| Lower priority compared with other curricular contenta |
| Perceived as unimportanta |
| Lack of fundinga |
Notes: Superscript letters indicate source report:
Discussion and Recommendations
A search and screen of 20 years of scientific literature to describe the state of the current empirical evidence related to US nursing faculty’s perceptions of SGM-related content and inclusion of SGM-related content in nursing curricula resulted in a sample of only four descriptive studies. While reporting data collected from 62 schools of nursing and 1,157 individual nursing faculty members across the US, these studies had very low response rates introducing increased risks of bias related to the sample which also limits their generalizability. The limited number of studies underscores the fact that there has been minimal research conducted related to the inclusion of information regarding the care of SGM patients in nursing curricula. Many passionate voices both in and out of nursing have been working to advance this cause, however the systems and organizational changes needed will be even more challenging without data to drive them. In addition to the fact that RQ2, RQ4, and RQ5 were left unaddressed, we identified three major gaps among the reviewed reports: 1) none included representative samples; 2) the studies mostly relied on author-developed, self-report measures, and the one validated instrument used (ATLG, Herek, 1994) is over 25 years old and only asks questions related to gay men and lesbians using arguably outdated language that does not fit the current understanding of SGM populations; and 3) none of the studies reported interventions supporting faculty development or incorporating SGM-related information in curriculum. To improve our understanding of potential barriers to inclusive curricula, and shape the future of SGM health and well-being-related nursing education the work done to further develop the evidence base must seek to overcome these three gaps. In addition to these identified gaps, scientific literature from other professions and some nursing research published since the close of this review provide us with important insights to consider when identifying opportunities for future research, interventions, and policy to ensure meaningful and evidence-based changes for the future of nursing.
Strategies for Integrating SGM Content in Other Health Profession Curricula.
Other healthcare professions had already begun addressing the need for integrating SGM content when we began this systematic review, and since the completion of our search other health professions have continued to publish new guidance for integrating SGM curricular content. One of the most impressive leaps forward in healthcare professions is the mandated inclusion of SGM-specific curricular content in physician assistant programs (Rolls et al., 2022). While not mandated at this time, medicine has increased their focus on SGM health inclusion through research such as pilot studies(Najor et al., 2020; Ufomata et al., 2018) or through policy initiatives including curricular content guidance (Hollenbach et al., 2014). There are also published recommendations for SGM-integrative curricular development for pharmacy schools (Llayton & Caldas, 2020).
Nursing knowledge and practice being unique from other healthcare professions, nurses would be best served by assessing and when appropriate adapting extant curricular interventions, tools, and other innovations. While we continue to work to fit our own needs there is room for the development of nursing-specific tools and interventions to prepare faculty to confidently and compassionately teach SGM-related content across programs and specialty areas. Some key options and approaches include integrating SGM health content into both didactic and clinical courses through a range of opportunities: simulations of real world encounters and exemplars; discussions of appropriate and therapeutic communication strategies when addressing SGM individuals and their chosen families in multiple settings (e.g. home, hospital, community); opportunities for nursing students to make critical linkages between theoretical content and clinical practice surrounding intersections of SGM identity and physical and mental health; and emphasizing the implications of identity for nursing assessment and nursing intervention development (Llayton & Caldas, 2020).
Recent Increases in Published Calls Advocating for Inclusive Nursing Curricula.
When our literature search was completed there were no evidence-based recommendations for inclusion of SGM content in nursing curricula. There have been several recent publications originating from both in and outside the US focusing on addressing health care needs of SGM individuals (Avery-Desmarais et al., 2021; Burkey et al., 2021; Burton et al., 2021; Eickhoff, 2021; Englund et al., 2020; Lauderdale et al., 2020; McCann & Brown, 2020; Morris et al., 2019; Sefolosha et al., 2021; Thangthaeng et al., 2022; Traister, 2020). Several of these publications provide further commentary on the growing needs within the nursing profession for attention to SGM health and well-being from various perspectives (e.g. nursing research [Thangthaeng et al.], BSN curricula [Englund et al.], graduate nursing education [Lauderdale et al.], inclusion and support of minority doctoral nursing students [Avery-Desmarais et al.]).Increased awareness is valuable, but we must move beyond commentaries and descriptive cross-sectional convenience samples, incorporating more sophisticated designs with purposeful and meaningful sampling approaches.
Emerging Tools for Supporting Integrating SGM Content in Nursing Curricula.
Another important area of ongoing development is identifying and testing frameworks and interventions for understanding, including, and even evaluating SGM-inclusive nursing curricular content. A Canada-based group has published work surrounding the development of an online nursing educational toolkit for sexual orientation and gender identity (Luctkar-Flude et al., 2020; Ziegler et al., 2021). These types of tools could be the basis for similar tools though adaptation may be key to ensure that they are addressing student and faculty needs in the US which may differ from other countries due to healthcare system structures, laws related to SGM-related healthcare (e.g. policies limiting access to affirming care for trans and gender diverse populations), and social climates.
Schools of nursing must assess their curricula, identify and implement evidence based-plans for content inclusion, and codify a systematic process to incorporate best practices for providing SGM healthcare. While not a panacea, tools for assessment of curricular inclusivity (e.g. Tool for Assessing LGBTQI+ Health Training (Sherman et al., 2022)]) may provide a valuable lens for programs to begin understanding the curricular areas that need further development. Even nursing programs with more inclusive curricula must monitor and adjust their approaches to ensure students receive the very best preparation for the realities of nursing practice in a diverse world. For example, Ercan-§ahin & Aslan (2020) explored undergraduate nursing students’ perceptions about how to include LGBTQ content into curriculum using qualitative methods. Students reported that it is essential for schools of nursing to promulgate knowledge acquisition and implement best practices when providing nursing care to SGM populations. Including SGM content in undergraduate nursing curricula will support graduates in developing scaffolding for comprehensive, affirming nursing care of SGM populations (McCann & Brown, 2020; Ray King et al., 2021; Sherman et al., 2022)
Anticipating Potential Pitfalls and Challenges to LGBTQIA+ Content Integration.
Proactively preventing obstacles from deterring the progression of developing SGM-inclusive curricula is imperative for success, and as such, the barriers to inclusion highlighted previously (see Table 4) are important considerations for programs seeking to implement curricular changes. Nursing program directors, deans, and faculty must consider critical questions early on in this process, including: How do schools determine how attitudes, biases, and or beliefs about SGM individuals are addressed?; How do schools’ or community clinical partners’ policies work to eliminate rather than perpetuate systemic inequity and biases?; and Where are the SGM-content expertise gaps in knowledge and practice experience of faculty? Several studies in our review reported that a major barrier for inclusion of content about SGM health and well-being is faculty feeling unprepared to deliver the content. To be effective, nursing faculty must believe in and speak up about the importance of SGM-related content and they must also be confident in their ability to integrate such content into curricula. Occasional guest lectures by SGM nursing experts will not adequately address the needs of future nurses. Beyond the limited initiatives towards inclusion of SGM health and well-being among nursing professional organizations, many nursing faculties in the US remain less than optimally diversified and in general are not representative of the nation with respect to gender identity, sexual orientation, race, and ethnicity.
Next Steps and Recommendations.
The 2021 AACN Essentials guide nursing programs to intentionally incorporate understanding intersections of social characteristics (e.g. race, age, gender identity, sexual orientation) as important for high quality, holistic nursing care (AACN, 2021). As such, nursing programs must ensure their curricular choices not only include such material, but that they challenge existing paradigms, and work in direct opposition to systemic biases from the institutional to the individual level. Failure to comprehensively address these issues will result in significant failure in reaching the 2021 AACN Essentials’ overarching goals. Although the spirit of inclusiveness may be represented in many documents, the absence of sexual- and gender-identity-specific language signals passive acceptance of non-inclusive practices among schools of nursing, faculty, practicing nurses, professional organizations, and healthcare systems. Nursing cannot afford to continue tilting towards inclusivity with general statements slowly evolving across successive editions of guidelines and standards. Rather, we must take bold action at all levels and use specific language acknowledging that delivery of high quality inclusive and affirming care of SGM people as essential competencies for all nurses. Further, it must be acknowledged that no matter how well intentioned, the adoption of inclusive and affirming standards and practices is ineffective without accountability through action-directed outcomes of nursing education’s regulatory bodies.
The provision of compassionate, inclusive, and affirming care for all individuals requires that healthcare education have a strong evidence-base that extends beyond the content of textbooks(De Guzman et al., 2018; Ray King et al., 2021). To adequately prepare a nursing workforce to address SGM-related health disparities nursing faculty must be well-prepared, empathetic, compassionate, and enthusiastic about teaching students about SGM health. Additionally, deans, directors, and faculty of nursing programs must explicitly frame inclusive curriculum as essential to professional nursing practice. As is sadly the case with many areas of research regarding equity and inclusion in healthcare, faculty preparation for delivery of SGM health and well-being content as well as inclusion of the content in general remain largely under-described and unexplored, thus open to innovation and exploration. Results from our review underscore the need to build the evidence base to inform development of interventions, tools, and tool kits for faculty and students to better provide the high-quality care SGM folks deserve. Progressing beyond the status quo is imperative for nursing to advance health equity. Nurses are leaders regardless of their areas of expertise, and nurses must respond to this growing, under acknowledged need.
Conclusion
This first of its kind, review of original nursing research related to faculty attitudes and perceptions with regard to SGM health content inclusion in nursing curricula highlights the exigent need for further study to better equip nursing faculty to educate nursing students at all levels with regard to care of SGM populations. A nation-wide effort is needed with input drawn from experts, practitioners, community members, stakeholders, students, and faculty. Coalitions that span boundaries and industries would be ideal for the development of a national strategy for systematic dissemination of best practices for meaningful inclusion of SGM content into nursing curricula across the US. To address critical inequities in health and healthcare it is imperative that nurses be prepared to care for diverse communities. Accrediting bodies must provide specific and intentionally inclusive guidelines for developing a more intentionally inclusive and affirming nursing profession. The exclusion of explicit content regarding SGM individuals and their health is not acceptable and must be rectified. Relegating content about the health of vulnerable populations to guest speakers and “special population highlights” in textbooks or course content is tokenizing and may identify such content as inferior in importance. If only similar time, energy, and resources as those being put into preparing nursing faculties for competency-based evaluation were focused on preparing nursing faculty to educate students to better serve marginalized populations, we would likely see the type of change needed.
Supplementary Material
Highlights-.
First systematic review of nursing faculty perceptions and curricular inclusion of LGBTQ+ content in US nursing programs
Despite numerous calls for nursing education to address the issue the evidence base is small and limited to descriptive empirical literature.
Measurement is an area of great need in this area with most studies using investigator developed surveys or dated instruments.
The nursing profession must invest the same amount of energy in inclusive curriculum as it is in competency-based education.
US nursing faculty deserve evidence-based SGM health education preparedness programs.
Footnotes
CREDIT Statement
SEM, CLC, and AS were involved in the conceptualization, methodology, validation, analysis, investigation, resources, data curation, writing, revising, editing, supervising, and administration; TH was involved in the conceptualization, writing, revising, and editing; CD was involved in the conceptualization, methodology, writing, revising, and editing; SKS and KB were involved in the conceptualization, methodology, writing, revising, supervising, and editing; JC and KC were involved in the validation, formal analysis, investigation, data curation, writing, revising, and editing of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aaberg V (2016). The state of sexuality education in baccalaureate nursing programs. Nurse Education Today, 44, 14–19. 10.1016/j.nedt.2016.05.009 [DOI] [PubMed] [Google Scholar]
- Agénor M (2015). What Are the Numbers? The Epidemiology of Cancer by Sexual Orientation and Gender Identity. In Boehmer U& Elk R (Eds.), Cancer and the LGBT Community: Unique Perspectives from Risk to Survivorship (pp. 117–140). Springer International Publishing. 10.1007/978-3-319-15057-4_8 [DOI] [Google Scholar]
- American Association of Colleges of Nursing. (2021). The Essentials: Core Competencies for Professional Nursing Education. https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf
- Avery-Desmarais SL, Hunter Revell SM, & McCurry MK (2021). A theoretical framework to promote minority PhD and DNP student success in nursing education. Journal of Professional Nursing, 37(6), 1149–1153. 10.1016/j.profnurs.2021.10.002 [DOI] [PubMed] [Google Scholar]
- Burkey DF, Fetty A, & Watson-Huffer K (2021). Infusing LGBTQ cultural competency into nursing curriculum. Nurse Education Today, 96, 104642. 10.1016/j.nedt.2020.104642 [DOI] [PubMed] [Google Scholar]
- Burton CW, Nolasco K, & Holmes D (2021). Queering nursing curricula: Understanding and increasing attention to LGBTQIA+ health needs. Journal of Professional Nursing, 37(1), 101–107. 10.1016/j.profnurs.2020.07.003 [DOI] [PubMed] [Google Scholar]
- Caceres BA, Streed Carl G, Corliss Heather L, Lloyd-Jones Donald M, Matthews Phoenix A, Monica Mukherjee, Tonia Poteat, Nicole Rosendale, Ross Leanna M, & null null. (2020). Assessing and Addressing Cardiovascular Health in LGBTQ Adults: A Scientific Statement From the American Heart Association. Circulation, 142(19), e321–e332. 10.1161/CIR.0000000000000914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Björkenstam C, & Mays VM (2016). Sexual Orientation and All-Cause Mortality Among US Adults Aged 18 to 59 Years, 2001-2011. American Journal of Public Health, 106(5), 918–920. 10.2105/AJPH.2016.303052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Understanding the Well-Being of Sexual and Gender Diverse Populations, Committee on Population, Division of Behavioral and Social Sciences and Education, & National Academies of Sciences, Engineering, and Medicine. (2020). Understanding the Well-Being of LGBTQI+ Populations (Patterson CJ, Sepdlveda M-J, & White J, Eds.; p. 25877). National Academies Press. 10.17226/25877 [DOI] [Google Scholar]
- Cornelius JB, Enweana I, Alston CK, & Baldwin DM (2017). Examination of Lesbian, Gay, Bisexual, and Transgender Health Care Content in North Carolina Schools of Nursing. Journal of Nursing Education, 56(4), 223–226. 10.3928/01484834-20170323-06 [DOI] [PubMed] [Google Scholar]
- De Guzman FLM, Moukoulou LNN, Scott LD, & Zerwic JJ (2018). LGBT inclusivity in health assessment textbooks. Journal of Professional Nursing, 34(6), 483–487. 10.1016/j.profnurs.2018.03.001 [DOI] [PubMed] [Google Scholar]
- Eickhoff C (2021). Identifying Gaps in LGBTQ Health Education in Baccalaureate Undergraduate Nursing Programs. Journal of Nursing Education, 60(10), 552–558. 10.3928/01484834-20210729-01 [DOI] [PubMed] [Google Scholar]
- Englund H, Basler J, & Meine K (2020). Nursing Education and Inclusion of LGBTQ Topics: Making Strides or Falling Short? Nurse Educator, 45(4), 182–184. 10.1097/NNE.0000000000000749 [DOI] [PubMed] [Google Scholar]
- Ercan-§ahin N, & Aslan F (2020). Nursing students’ perspectives on the inclusion of course content on lesbian, gay, bisexual, and transgender health in the nursing curriculum: A descriptive qualitative study. Nursing & Health Sciences, 22(3), 822–829. 10.1111/nhs.12742 [DOI] [PubMed] [Google Scholar]
- Felner JK, Dudley TD, & Ramirez-Valles J (2018). “Anywhere but here": Querying spatial stigma as a social determinant of health among youth of color accessing LGBTQ services in Chicago’s Boystown. Social Science & Medicine, 213, 181–189. 10.1016/j.socscimed.2018.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN (2022). Health disparities affecting LGBTQ+ populations. Communications Medicine, 2(1), Article 1. 10.1038/s43856-022-00128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell BR, & Sasser JT (2018). Sexual and gender minority health: Nursing’s overdue coming out. International Journal of Nursing Studies, 79, A1–A4. 10.1016/j.ijnurstu.2017.12.002 [DOI] [PubMed] [Google Scholar]
- Healthy People 2020. ∣. (n.d.). Retrieved May 8, 2022, from https://www.healthypeople.gov/2020/
- Healthy People 2030. ∣ health.gov. (n.d.). Retrieved May 8, 2022, from https://health.gov/healthypeople?_ga=2.254129416.1812327314.1651940200-1468598934.1651940200
- Herek GM (1994). Assessing Heterosexuals’ Attitudes toward Lesbians and Gay Men: A Review of Empirical Research with the ATLG Scale. In Lesbian and Gay Psychology: Theory, Research, and Clinical Applications (pp. 206–228). SAGE Publications, Inc. 10.4135/9781483326757 [DOI] [Google Scholar]
- Hollenbach AD, Eckstrand KL, & Dreger A (Eds.). (2014). Implementing Curricular and Institutional Climate Changes to Improve Health Care for Individuals Who Are LGBT, Gender Nonconforming, or Born with DSD. AAMC. https://store.aamc.org/downloadable/download/sample/sample_id/129/ [Google Scholar]
- Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, & Vedel I (2019). Improving the content validity of the mixed methods appraisal tool: A modified e-Delphi study. Journal of Clinical Epidemiology, 111, 49–59.e1. 10.1016/j.jclinepi.2019.03.008 [DOI] [PubMed] [Google Scholar]
- Hughes TL, Jackman K, Dorsen C, Arslanian-Engoren C, Ghazal L, Christenberry-deceased T, Coleman C, Mackin M, Moore SE, Mukerjee R, Sherman A, Smith S, & Walker R (2022). How can the nursing profession help reduce sexual and gender minority related health disparities: Recommendations from the national nursing LGBTQ health summit. Nursing Outlook. 10.1016/j.outlook.2022.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2011). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. National Academies Press (US). 10.17226/13128 [DOI] [PubMed] [Google Scholar]
- Jones J (2022, February 17). LGBT Identification in U.S. Ticks Up to 7.1%. Gallup.Com. https://news.gallup.com/poll/389792/lgbt-identification-ticks-up.aspx
- Katrak P, Bialocerkowski AE, Massy-Westropp N, Kumar VS, & Grimmer KA (2004). A systematic review of the content of critical appraisal tools. BMC Medical Research Methodology, 4(1), 22. 10.1186/1471-2288-4-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale JL, Fogel SC, Schorn MN, & Dietrich MS (2020). Perceptions of Sexual and Gender Minority Content in Graduate Nursing Curricula. Nursing Education Perspectives, 41(6), 334–339. 10.1097/01.NEP.0000000000000663 [DOI] [PubMed] [Google Scholar]
- Llayton CK, & Caldas LM (2020). Strategies for inclusion of lesbian, gay, bisexual, transgender, queer, intersex, and asexual (LGBTQIA+) education throughout pharmacy school curricula. Pharmacy Practice, 18(1), 1862. 10.18549/PharmPract.2020.1.1862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockwood C, Porritt K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, Loveday H, Carrier J, & Stannard D (2020). Chapter 2: Systematic reviews of qualitative evidence—JBI Manual for Evidence Synthesis—JBI Global Wiki. In Aromataris E & Munn Z (Eds.), JBI Manual for Evidence Synthesis. 10.46658/JBIMES-20-03 [DOI] [Google Scholar]
- Luctkar -Flude Marian, Tyerman J, Ziegler E, Carroll B, Shortall C, Chumbley L, & Tregunno D (2020). Developing a Sexual Orientation and Gender Identity Nursing Education Toolkit. The Journal of Continuing Education in Nursing, 51(9), 412–419. 10.3928/00220124-20200812-06 [DOI] [PubMed] [Google Scholar]
- Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, & Zeng X-T (2020). Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Military Medical Research, 7(1), 7. 10.1186/s40779-020-00238-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macapagal K, Bhatia R, & Greene GJ (2016). Differences in Healthcare Access, Use, and Experiences Within a Community Sample of Racially Diverse Lesbian, Gay, Bisexual, Transgender, and Questioning Emerging Adults. LGBT Health, 3(6), 434–442. 10.1089/lgbt.2015.0124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann E, & Brown M (2020). The needs of LGBTI+ people within student nurse education programmes: A new conceptualisation. Nurse Education in Practice, 47, 102828. 10.1016/j.nepr.2020.102828 [DOI] [PubMed] [Google Scholar]
- Meyer IH, Brown TNT, Herman JL, Reisner SL, & Bockting WO (2017). Demographic Characteristics and Health Status of Transgender Adults in Select US Regions: Behavioral Risk Factor Surveillance System, 2014. American Journal of Public Health, 107(4), 582–589. 10.2105/AJPH.2016.303648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SE, Wierenga KL, Prince DM, Gillani B, & Mintz LJ (2021). Disproportionate Impact of the COVID-19 Pandemic on Perceived Social Support, Mental Health and Somatic Symptoms in Sexual and Gender Minority Populations. Journal of Homosexuality, 68(4), 577–591. 10.1080/00918369.2020.1868184 [DOI] [PubMed] [Google Scholar]
- Morris M, Cooper RL, Ramesh A, Tabatabai M, Arcury TA, Shinn M, Im W, Juarez P, & Matthews-Juarez P (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: A systematic review. BMC Medical Education, 19(1), 325. 10.1186/s12909-019-1727-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najor AJ, Kling JM, Imhof RL, Sussman JD, Nippoldt TB, & Davidge-Pitts CJ (2020). Transgender Health Care Curriculum Development: A Dual-Site Medical School Campus Pilot. Health Equity, 4(1), 102–113. 10.1089/heq.2019.0106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nursing Faculty Education for LGBTQ+ Health: An Integrative Review. (n.d.). Retrieved December 4, 2020, from https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=201475
- Popay J, Roberts HM, Sowden A, Petticrew M, Arai L, Rodgers M, & Britten N (2006). Guidance on the conduct of narrative synthesis in sytematic reviews. Institute for Health Research. [Google Scholar]
- Ray King K, Fuselier L, & Sirvisetty H (2021). LGBTQIA+ invisibility in nursing anatomy/physiology textbooks. Journal of Professional Nursing, 37(5), 816–827. 10.1016/j.profnurs.2021.06.004 [DOI] [PubMed] [Google Scholar]
- Rolls J, Showstark M, Jones Q, Bruessow D, & Kluznik J (2022). Promising Practices in Sexual Orientation and Gender Identity Curriculum Inclusion. The Journal of Physician Assistant Education, 33(4), 346–351. 10.1097/JPA.0000000000000475 [DOI] [PubMed] [Google Scholar]
- Sefolosha A, van Wyk N, & van der Wath A (2021). Reframing Personal and Professional Values: A Substantive Theory of Facilitating Lesbian, Gay, Bisexual, Transgender and Intersex Youth-Inclusive Primary Health Care by Nurses. Journal of Homosexuality, 68(8), 1298–1319. 10.1080/00918369.2019.1696106 [DOI] [PubMed] [Google Scholar]
- Sherman ADF, Klepper M, Claxton A, Deng A, Ling C, Mollenkopf NL, & Bower K (2022). Development and psychometric properties of the tool for assessing LGBTQI+ health training (TALHT) in pre-licensure nursing curricula. Nurse Education Today, 110, 105255. 10.1016/j.nedt.2021.105255 [DOI] [PubMed] [Google Scholar]
- Sirota T (2013). Attitudes Among Nurse Educators Toward Homosexuality. Journal of Nursing Education, 52(4), 219–227. 10.3928/01484834-20130320-01 [DOI] [PubMed] [Google Scholar]
- Streed CG, Beach LB, Caceres BA, Dowshen NL, Moreau KL, Mukherjee M, Poteat T, Radix A, Reisner SL, Singh V, & null, null. (2021). Assessing and Addressing Cardiovascular Health in People Who Are Transgender and Gender Diverse: A Scientific Statement From the American Heart Association. Circulation, 144(6), e136–e148. 10.1161/CIR.0000000000001003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Study Quality Assessment Tools ∣ NHLBI, NIH. (n.d.). Retrieved December 14, 2022, from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Thangthaeng N, Hillard MA, Cayford M, Barrett S, Ducar D, & Larkin ME (2022). Promoting a gender-affirming environment in research: Implications for research nurses. Journal of Research in Nursing, 27(1–2), 157–165. 10.1177/17449871211068647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traister T (2020). Improving LGBTQ Cultural Competence of RNs Through Education. Journal of Continuing Education in Nursing, 51(8), 359–366. 10.3928/00220124-20200716-05 [DOI] [PubMed] [Google Scholar]
- Ufomata E, Eckstrand KL, Hasley P, Jeong K, Rubio D, & Spagnoletti C (2018). Comprehensive Internal Medicine Residency Curriculum on Primary Care of Patients Who Identify as LGBT. LGBT Health, 5(6), 375–380. 10.1089/lgbt.2017.0173 [DOI] [PubMed] [Google Scholar]
- Vespa J, Medina L, & Armstrong DM (2020). Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports, 1–15. [Google Scholar]
- Walsh D, & Hendrickson SG (2015). Focusing on the “T” in LGBT: An Online Survey of Related Content in Texas Nursing Programs. Journal of Nursing Education, 54(6), 347–351. 10.3928/01484834-20150515-07 [DOI] [PubMed] [Google Scholar]
- White Hughto JM, Murchison GR, Clark K, Pachankis JE, & Reisner SL (2016). Geographic and Individual Differences in Healthcare Access for U.S. Transgender Adults: A Multilevel Analysis. LGBT Health, 3(6), 424–433. 10.1089/lgbt.2016.0044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler E, Luctkar-Flude M, Carroll B, Tyerman J, Chumbley L, & Shortall C (2021). Development of an online educational toolkit for sexual orientation and gender identity minority nursing care. Revista Latino-Americana de Enfermagem, 29, e3470. 10.1590/1518-8345.4712.3470 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.