Abstract
Background
Nursing home quality of care is a persistent challenge, with recent reports calling for increased reforms to improve quality and safety. Less is known about the clinical approaches currently used and the barriers perceived by skilled nursing facilities (SNFs) to provide care for their short-stay residents.
Methods
We conducted a nationally representative survey of SNFs from October 2020 to May 2021 to understand their care delivery approaches and perceived barriers. Our primary outcomes were the reported number of 23 separate care delivery approaches and the reported number of 12 separate barriers to reduce spending or improve care for SNF short-stay residents. We also performed stratified analyses by facility participation in bundled payments and other SNF characteristics.
Results
We received 377 responses from 693 SNFs contacted (response rate = 54%). SNFs reported an average of 16.8 care delivery approaches and an average of 5.0 barriers. While there were some differences observed by SNF characteristics, such as by bundled payments participation or ownership type, there were common care delivery approaches and barriers shared by most facilities. Care management practices, including reviewing the patient census and medication reconciliation on discharge, were the most common delivery approaches reported. SNFs were less likely to ensure completion of a follow-up appointment with a primary care provider or track repeat emergency room visits. Issues concerning staffing, such as staff turnover and/or burnout, and lack of resources to provide patients social support, mental health and substance use services, were the most cited barriers to care delivery.
Conclusions
Nationally, SNFs implemented a wide array of care delivery approaches, but challenges with staffing and limited resources to address patients’ social and mental health needs were dominant. Individual SNFs may have limited ability to address these key barriers, so involvement of many stakeholders across the entire health care system may be necessary.
Keywords: post-acute care, care delivery approaches, barriers to care
INTRODUCTION
Concerns about the quality of care in skilled nursing facilities (SNFs) have persisted for decades, with National Academies of Sciences, Engineering, and Medicine (NASEM) reports in 1986 and 2022 calling for major policy reforms, including better regulation and greater oversight.1,2 Recently, President Biden’s 2022 nursing home quality improvement plan proposed reforms to improve the quality and safety of nursing homes and increase the accountability and transparency of the quality of care provided.3 Although there is ongoing controversy about how to best measure quality of care in nursing homes,4 studies have shown that patients who receive care in nursing homes with lower quality scores (e.g. Medicare “star” ratings), lower staffing levels, or more health inspection deficiencies were more likely to be re-hospitalized within 30-days of discharge.5 In contrast, patients receiving care from SNFs with higher quality ratings spent more time at home in the 30 and 90 days after SNF discharge.6
There have been many recent public and private initiatives to improve SNF quality,7,8 but few have made significant or reproducible progress. Perhaps the most prominent federal effort has been the bundled payments for care improvement (BPCI) program, which created incentives for hospitals and SNFs to better coordinate their services and redesign care delivery through a global payment covering the initial SNF stay and all subsequent care during the 90 days following SNF admission.9,10 Episode payment for SNFs has been associated with a decrease in costs for patients with total joint replacement and patients with other conditions who are frail, but no change in health outcomes.11,12
To design effective policy, it is important to understand the clinical approaches that SNFs pursue to deliver high quality care and the barriers they face in achieving quality improvement. However, little is known about the clinical approaches now commonly used by SNFs or the barriers and difficulties faced in providing care during the patient stay and post-discharge. To address this evidence gap, we conducted a national survey of SNF administrators to understand how SNFs have adopted care practices and perceive barriers to providing high quality care for their short-stay residents. We also stratified our sample to compare the care delivery approaches and barriers by SNFs that did and did not participate in BPCI.
METHODS
Survey Administration
We conducted a nationally representative survey on post-acute care delivery in SNFs. The intent of the survey was to ascertain information on the different clinical care delivery approaches used by SNFs nationally and the barriers they perceive in improving quality and lowering the cost of care. As initially designed, the survey focused on whether participation in payment reform models, such as BPCI, were associated with care redesign. We stratified our random sample to include similar numbers of SNFs that did (N = 345) and did not (N = 348) participate in BPCI. However, the COVID-19 pandemic interrupted the timeline of the originally planned survey and BPCI is only one of many factors that may influence care redesign. As a result, our analysis of the survey results focuses on overall effects, with survey weighting used to derive nationally representative estimates. The survey was designed by researchers at the Harvard T.H. Chan School of Public Health (HSPH) and Washington University in St. Louis and conducted October 15, 2020 to May 16, 2021. This study was approved as exempt by HSPH’s Institutional Review Board.
At each SNF, the administrator, executive director, or other administrative individual most knowledgeable about the clinical approaches of the facility was invited to complete a voluntary survey. SNFs were contacted by a survey firm via a sequential mixed mode approach by mail, web, and telephone. SNFs were sent an initial personalized pre-notification form by the study principal investigators explaining the study and sponsorship, as well as a link to the online version of the survey. After the pre-notification letter, a $100 check was sent along with a second invitation to provide a financial incentive for participation. The purpose of the $100 incentive was to increase the likelihood of response from the individual completing the survey (e.g., Executive Director, Nurse Administrator; not for the facility itself) and was based on literature surveying physicians on the effective amount to increase participation in surveys.13 A follow-up campaign included email, telephone, and mailed reminders.
Survey Instrument Design
The survey question domains were informed by a literature review, discussions with members of an expert advisory panel, and exploratory interviews with administrative directors of SNFs in multiple states. Feedback on the initial draft of the survey was obtained through cognitive interviews with 10 SNF administrators to ensure the questions captured the clinical approaches and barriers consistent with our intent. After incorporating input from the cognitive interviews, the survey was formally pre-tested with 40 SNF administrators randomly selected from the sampling frame to refine the content and question wording, as well as limit the potential for missing data because of questions that were misunderstood or unanswerable. The final survey consisted of 17 multi-component questions within seven modules (respondent and care settings, participation in alternative payment methods, clinical approaches, barriers and context, quality, relationships with other institutions, and adapting to the patient driven payment model); the entire survey instrument is available in Supplementary Survey S1. Although the survey instrument asked about clinical care “redesign,” we use the term “approaches” to describe these items more broadly in this manuscript. Results from these modules were grouped into categories of “care delivery approaches” and “barriers” for the purposes of this analysis.
Study Outcomes and Measures
We focused on two key outcomes: the reported number of 23 possible approaches to reduce spending or improve care reported for short-stay residents (e.g., use of a discharge check list, patient experience surveys) and the reported number of 12 possible barriers to reduce spending or improve care for short-stay residents (e.g., inadequate mental health services, lack of staff buy-in for changes) (Table S1). The number of care delivery approaches used or barriers faced was determined by taking the sum of answers saying “yes, this is currently in use or exists” or “yes, this poses a barrier to reducing spending or improving care” to survey questions for each outcome, respectively. Although each of the approaches and barriers were complex and not necessarily interchangeable, measuring these sums enabled us to summarize the scope of currently available tools and challenges faced by SNFs across the whole sample. We also examined differences by facility characteristics, including BPCI participation, ownership type, chain membership, quality rating, and share of minority patients.
Study Covariates
The information collected by SNF survey respondents was supplemented by facility-level covariates gathered from the 2021 Centers for Medicare and Medicaid Services’ Nursing Home Care Compare Data,14 the 2019 Long-Term Care: Facts on Care in the US (LTCFocus) from Brown University,15 2018 SNF Medicare claims data16 and the 2018 Minimum Data Set (MDS) 3.0.17 The following characteristics were obtained from the Nursing Home Care Compare data: the total number of beds, whether the facility was part of a chain, whether the facility was part of a continuing care retirement community,18 total nurse staffing hours per resident per day, overall quality rating (categorized into 1-2 stars, 3 stars, 4-5 stars), and ownership type (for-profit, non-profit, government-owned). From LTCFocus, we obtained the share of residents whose primary support was Medicaid. Medicare claims data were used to obtain information on the share of residents who were non-white and the mean number of residents. We calculated the share of residents with cognitive impairment, based on the cognitive function scale (low, moderate, or severe cognitive impairment) using the MDS. Urbanization was determined based on the National Center for Health Statistics’ Urban-Rural classification Scheme for U.S. counties (categorized into large metro, small/medium metro, micropolitan/non-core).19 From our survey, we also collected characteristics such as accountable care organization (ACO) participation and whether a SNF was connected with an assisted living facility.
Statistical Analyses
The survey was designed to capture differences in care redesign approaches associated with payment reform participation, so the sample was weighted to account for the stratified sampling design by BPCI and non-BPCI facilities, as well as non-response bias based on a series of facility-level characteristics (percent female, percent minority, number of residents, chain membership, ownership type) and population-level measures (metropolitan status, U.S census region, mean household income, percentage of Medicare Advantage penetration, and the hospital referral region’s Herfindahl-Hirschman Index based on SNF location).
We calculated average counts of the outcomes and tested for differences across groups using t-tests for continuous variables and chi-square tests for categorical variables. We estimated average counts of the number of care delivery approaches and barriers reported by surveyed SNFs using Poisson regression models with robust standard errors, controlling for the facility-level characteristics above. Statistical tests were performed on the set of non-missing data (there were 40 facilities, 10.61%, with any missing data). In additional sensitivity analyses, we examined differences in outcomes using multiple imputation with 10 imputed datasets to replace the missing values using the MI commands in Stata.20 All analyses were performed with Stata version 17.0 and RStudio 1.4.1103. A p value of 0.05 or less was considered statistically significant. However, given the use of multiple comparisons, we regard our findings as preliminary.
RESULTS
We contacted 698 SNFs by mail and telephone. This included 5 cases where the mailing was returned as undeliverable at least once and the facility had a non-working telephone number, no answer, or busy signal during all call attempts. In total, the sample was comprised of 693 SNFs (348 BPCI, 345 non-BPCI), with 377 completing the survey for a 54% response rate (377/693). The response rate was 51% among BPCI SNFs (179/348) and 57% among non-BPCI SNFs (198/345). 83% of survey respondents were either the SNF Administrator (67.37%) or Executive Director (15.65%) of the facility (Table S2). There were some differences between SNFs which responded to our survey compared to all other SNFs in the U.S. For example, SNF respondents were more likely to be for-profit (77% vs. 70%, p=0.01) and located in a large metropolitan area (47% vs. 41%, p=0.01) (Table 1). Survey respondents also had more federally certified beds (115 vs. 106, p=0.05), but there were not statistically significant differences in the number of residents or quality rating of the facility. There were not many differences observed between contacted SNFs who did and did not respond to the survey, except for minor differences in geographic location, with respondents more likely to be in the West (16% vs. 9%, p=0.04). (Table S3).
Table 1.
Characteristics of SNF Survey Respondents and All Other SNFs (Table)
| Variables | All SNFs | SNF Survey Respondents |
All Other SNFs |
|
|---|---|---|---|---|
| % or mean | % or mean | % or mean | p-value | |
| N of SNFs | 15,266 | 377 | 14,889 | |
| Ownership status | ||||
| Not for profit | 23.2% | 18.7% | 23.3% | 0.04 |
| Government | 6.2% | 4.3% | 6.3% | 0.11 |
| For profit | 70.6% | 77.1% | 70.4% | 0.01 |
| Urban | ||||
| large metro | 40.9% | 47.3% | 40.7% | 0.01 |
| medium/small metro | 30.5% | 29.5% | 30.5% | 0.69 |
| micropolitan/non-core | 28.7% | 23.2% | 28.8% | 0.02 |
| Number of residents | 95.8 | 103.1 | 95.6 | 0.13 |
| Number of federally certified beds | 106.4 | 115.2 | 106.2 | 0.05 |
| SNF in chain | 57.9% | 62.2% | 57.8% | 0.09 |
| SNF hospital based | 3.9% | 3.2% | 3.8% | 0.51 |
| Region | ||||
| West | 15.1% | 19.5% | 15.0% | 0.02 |
| Northeast | 18.4% | 21.9% | 18.3% | 0.08 |
| Midwest | 32.8% | 30.8% | 32.8% | 0.40 |
| South | 33.7% | 27.8% | 33.9% | 0.01 |
| Overall quality rating | 3.2 | 3.2 | 3.2 | 0.92 |
Note: Pearson chi-square tests performed for ownership status, urban location, chain membership, hospital-based, and region. T-tests performed for number of residents, number of federally certified beds, and overall quality rating.
Care delivery approaches and barriers to reduce spending or improve care delivery
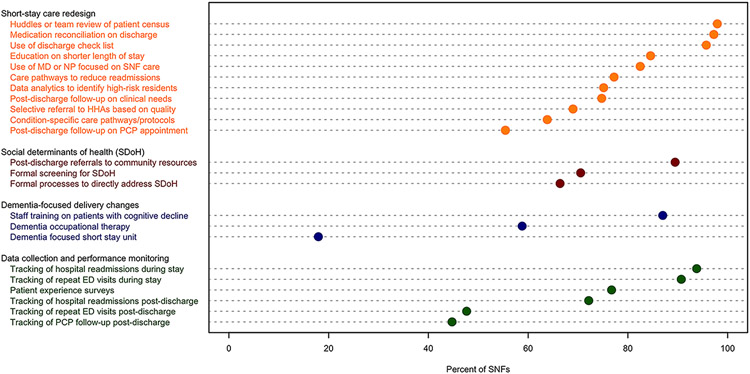
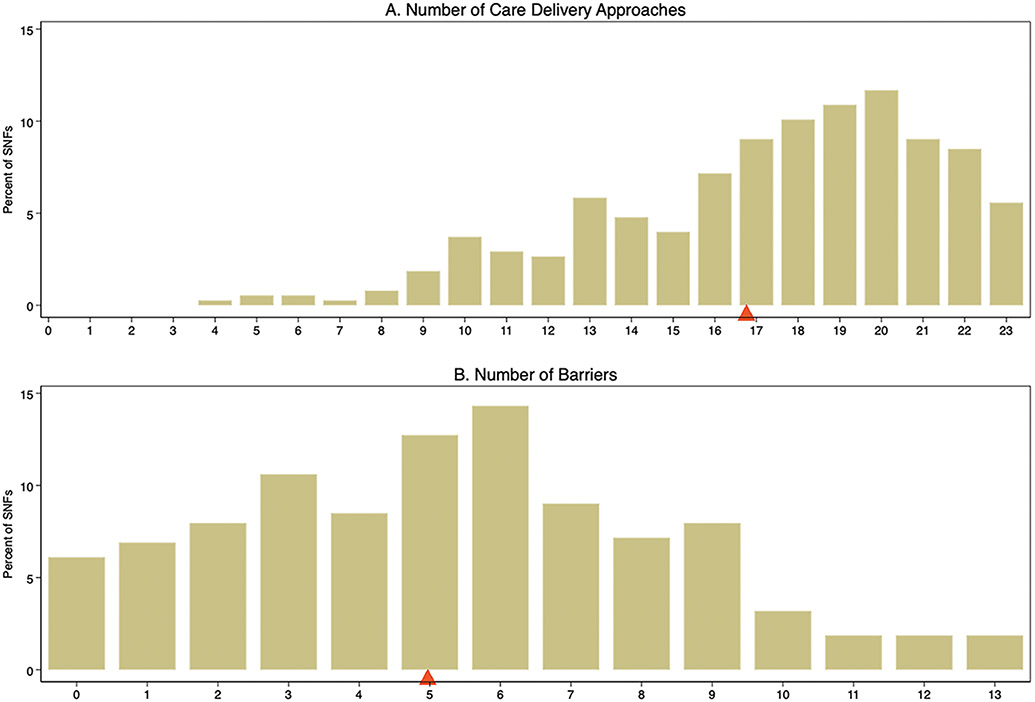
All SNFs (100%, n=377) reported at least four of 23 approaches to reduce spending or improve care delivery for their short-stay residents, with an average of 16.8 approaches (standard deviation [SD]: 4.2) reported (Figure 1, Table S1). The most prevalent types of care approaches were implemented nearly universally, including huddles or regular reviews of the patient census as a team (97%, n=365), medication reconciliation on discharge (97%, n=364), and use of a discharge check list (96%, n=361) (Figure 2, Table S1). The use of services specifically targeting residents with dementia, such as a specific physical unit for short-stay residents with dementia or enhanced occupational therapy (e.g., kitchen simulation environment) were less frequently reported (18%, n=71 and 59%, n=222 respectively). Post-discharge from a SNF activities, such as following-up to confirm an appointment was completed with the patient’s primary care physician (45%, n=178) and following repeat emergency room visits (48%, n=201) were also less commonly reported approaches used by SNFs. In adjusted analyses of SNF delivery approaches, for-profit governance was associated with a higher average number of care delivery approaches (p=0.01) while a higher share of minority patients (p=0.02) or more reported total nurse staffing hours per resident per day (p<0.001) were associated with a decrease in the average number of care delivery approaches reported (Table S4 and Table S5).
Figure 1. Distribution of the number of care delivery approaches and barriers reported by SNF survey respondents.
Note: Red triangles denote weighted average estimates for each group. The average number of care delivery approaches was 16.8. The average number of barriers was 5.0.
Figure 2. Types of care delivery approaches reported by SNF survey respondents.
Note: For care redesign, social determinants of health, and dementia-focused delivery approaches, participants were provided a list of initiatives that SNFs might pursue. They were asked to indicate whether each tool or approach was used by their SNF for short-stay residents. For data collection and performance monitoring, participants were asked if the performance indicators were collected and monitored. ED is emergency department. EHR is electronic health record. PCP is primary care physician. HHA is home health agency.
The vast majority (94%, n=354) of SNFs reported at least one barrier to reducing spending or improving care delivery for their short-stay residents, with an average of 5.0 barriers (SD: 3.1) reported (Figure 1, Table S1). The most common barrier experienced by three-fourths of the sample was staff turnover and/or burnout (74%, n=289) (Figure 3). Factors related to a patient’s post-discharge care, such as difficulty with residents’ lack of social support (e.g., living alone) (66%, n=267) and inadequate availability or accessibility of mental health services (65%, n=238) were also common concerns. Few SNFs expressed difficulties with their relationships with other institutions, as the least common barrier reported by SNFs was difficulty forging effective affiliations with home health agencies (12%, n=46) or hospitals (15%, n=60). In adjusted analyses (Table S4 and S5), not adopting alternative payment models (p=0.02), chain membership (p=0.01), and serving more minority residents (p=0.03) were associated with fewer barriers reported.
Figure 3. Types of barriers reported by SNF survey respondents (Figure).
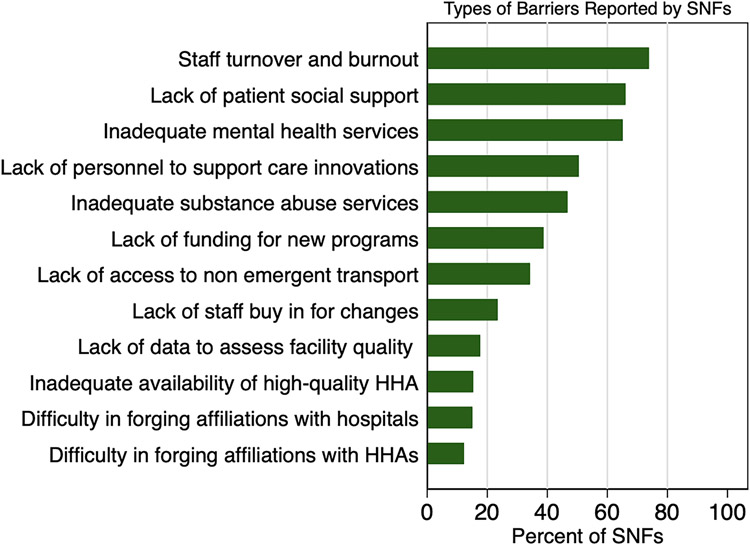
Note: Participants were asked if each item posed a barrier to reducing spending or improving care. HHA is home health agency.
Differences in care delivery approaches and barriers by facility characteristics
We also examined the types of care delivery approaches and barriers by participation in BPCI and SNF characteristics (Table S6-S8). There were a few differences in the prevalence of individual items (Table S6). BPCI facilities were more likely to report the use of condition-specific care pathways/protocols (79% vs. 63%, p=0.001) and care pathways to reduce admissions (91% vs. 76%, p<0.001), use of a medical doctor or nurse practitioner focused on SNF care (94% vs. 82%, p<0.001), and tracking of hospital readmissions or repeat ED visits both during and post-discharge compared to non-BPCI facilities. BPCI facilities also reported increased barriers for some items compared to non-BPCI facilities, including lack of access to non-emergent transport (47% vs. 33%, p=0.01) and lack of staff buy-in for changes (35% vs. 23%, p=0.01)
There were differences in the use of some approaches and barriers by profit status and chain membership (Table S7). For-profit facilities were more likely to report using condition-specific care pathways or protocols for SNF care (72% for-profit vs. 45% non-profit, p<0.001) and use of data analytics to identify high-risk patients (81% vs. 63%, p=0.01). For-profit facilities were also more likely to report lack of staff buy-in for changes as a barrier (29% vs 13%, p=0.01). There were other differences in approaches and barriers experienced in facilities by chain membership. Chain membership was associated with greater use of tools such as education on shorter length of stay (90% chain vs. 78% non-chain, p=0.01) and using care pathways to reduce readmissions (83% vs 69%, p=0.03). Members of chains were also less likely to report funding for new programs (30% vs. 50%, p<0.001) and lack of data to assess facility quality (9% vs 28%, p<0.001) as barriers compared to non-chain members.
There were fewer differences observed by overall quality rating or share of minority patients served (Table S8). There were no statistically significant differences in the implementation of care delivery approaches by star rating, but there were some differences in the barriers experienced. Lower quality rated facilities were more likely to experience greater difficulty with inadequate mental health services (p=0.01), inadequate substance abuse services (p=0.04), and lack of staff buy-in for changes (p=0.04). Facilities serving a higher share of racial minority patients were less likely to use huddles for team review of patient census (p=0.03), track repeat ED visits post-discharge (p=0.03), or use selective referral to HHAs based on quality (p<0.001).
We also compared the facility-level shares of residents with cognitive impairment for facilities which did and did not report using each of the dementia-focused care delivery approaches (Table S9). On average, facilities with the dementia-focused approaches had larger shares of patients with severe impairment based on the cognitive function scale (CFS) and smaller shares of patients with low or moderate CFS compared to facilities without the dementia tools. Facilities which reported having a dementia-focused short-stay unit were more likely to have a larger share of patients with severe CFS (4.29%) compared to those which did not have the specialty unit (3.90%).
DISCUSSION
In this nationally representative survey of SNFs, we found that 100% of SNFs implemented 4 or more care delivery approaches and nearly all SNFs experienced one or more barriers in care delivery for their short-stay residents. Fewer SNFs implemented tools likely requiring higher investment, like dementia-focused short-stay units. While there was some variation observed by SNF characteristics, there were more common themes than stark differences across types of facilities, such as the high number of respondents reporting barriers to staffing and access to outside resources like mental health.
It is concerning that the least common care delivery approaches reported by SNFs were services to meet the care needs of patients with dementia. Although over 30% of short-stay patients are diagnosed with Alzheimer’s disease and other forms of dementia,21 only 60% of surveyed facilities were capable of providing enhanced occupational therapy for these patients and less than 20% had a specific physical unit for short-stay residents with dementia. Previous work has found that facilities with dementia special care units had improved quality of care, including reduced inappropriate antipsychotic use, physical restraints, pressure ulcers, and hospitalizations.22 This suggests that expanding dementia-focused units may be an evidence-based opportunity for quality improvement.
One question raised by the results is how the implementation of these delivery care approaches can be so widespread among SNFs in our sample, given the relatively static variation in overall quality scores observed. A simple explanation could be that the correlation between SNF directors’ report of the use of a delivery approach and its actual implementation is weak, as the act of identifying an implementation is not fully indicative of its quality. It could also be the case that composite nature of the star ratings calculations, which include a number of dimensions aside from quality, do not closely reflect advances in care delivery. Another possibility is that common care delivery approaches are not enough to systematically improve quality on dimensions that matter for patients, like staffing and coordination across settings of care. Despite observed variation by SNF characteristics such as profit or private equity ownership and other factors,23,24 we found that the care delivery approaches adopted by SNFs were not systematically correlated with markers of quality and were common in both high- and low-rated facilities by Medicare star ratings. These findings suggest that pushing individual delivery reforms to SNFs may provide little systematic change without addressing other barriers. We also found that few followed whether patients had subsequent emergency room visits or primary care physician follow-up visits post-discharge from the SNF. CMS’ quality measures currently only capture events during the nursing home stay, such as the percentage of short-stay residents re-hospitalized after the nursing home admission.25 Including post-discharge follow-up measures could be a useful addition to standard SNF quality measures to understand patient outcomes throughout the continuum of care.
It is not surprising that most respondents reported staff turnover or burnout as a common barrier to improving care. Even before the pandemic, the average nursing home turned over its entire staff every year.26 Staff turnover has been associated with more rehospitalizations,27 use of physical restraints,28 and increased probability of an infection control citation during a nursing home inspection.29 It is unclear how much ability SNFs have to address the staffing crisis given labor market turmoil, changes in immigration policy (given the high percentage of immigrants in the SNF labor force), and changing payment models. The 2022 NASEM report on nursing home quality highlighted underinvestment in nurse staffing as a major issue, as low salaries and few benefits alongside inadequate training reduced the desirability of working in a nursing home.2 There have been state-led initiatives, such as a program launched by state officials in Minnesota, to recruit, train, and deploy new certified nurse assistants.30 These programs are designed to alleviate concerns about the nursing home workforce, however, further efforts are needed to provide job training and nurse development to bolster the workforce. Our survey confirms that staffing is a priority for enabling SNFs to improve quality, and further policy efforts to improve job satisfaction and increase staff retention are necessary.
The majority of SNFs also lacked resources to address patient social support as well as the availability and accessibility of mental health and substance use services. Although policymakers have recently shown willingness to strengthen the system capacity of behavioral health providers and connect individuals with care options,31 there has been less focus on the specific needs of the geriatric population who most commonly use SNFs. These are issues that would be very difficult for SNFs to address themselves because they involve provider workforce and social safety net challenges outside their facilities. This highlights how closely challenges in the SNF industry are intertwined with nationwide policy struggles in health care in other domains.
This study had several limitations. First, differences may exist between the SNFs which responded to the survey and the total sample of SNFs which were invited to complete the survey, as weighting does not fully eliminate non-response bias. There could also be concerns about social desirability bias, as survey respondents may have felt pressured to report responses that were positive and socially acceptable. Second, although the survey was designed and piloted before the COVID-19 pandemic, administration occurred during the pandemic. Because of this, SNF respondents likely experienced additional barriers and underwent concurrent practice changes unrelated to the Medicare payment model the survey was designed to assess. Third, this was an observational study using cross-sectional data, so we were not able to assess causal relationships between SNF characteristics and the care delivery approaches and barriers they reported. Fourth, the survey measures SNF administrator perspectives on delivery of care and barriers rather than measures that are completely objective. Finally, our results focus on summarizing the aggregate number of care delivery approaches and barriers reported by SNFs. If a facility leader responded that an item was not a meaningful barrier to care redesign, we were unable to assess if that indicated they felt that the item was not important, or that it was important and they had successfully overcome it.
Conclusions
In a national survey of SNF leadership, we found that SNFs implemented a wide array of care delivery approaches internally, but challenges with staffing, mental health access, and limited resources to address patients’ social determinants of health remain prevalent. Solutions to these challenges will require policy change alongside practice change as individual SNFs have limited ability to address many key barriers by themselves, so involvement of many stakeholders across the entire health care system will be necessary.
Supplementary Material
Key Points:
Most, but not all, surveyed SNFs utilized common care management practices
Few SNFs were specially equipped to care for patients with dementia or follow their patients’ entire continuum of care, such as follow-up activities post-discharge from the facility
SNFs also reported staff turnover and lack of resources for patient social support as important barriers preventing them from improving their care delivery
Why does this paper matter?
Policy change, alongside facility-level practice change, will be required for SNFs to address the needs of their short-stay residents.
ACKNOWLEDGMENTS
Sponsor's Role
The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Disclosures:
This work was supported by grants K23 AG058806 (Barnett) and R01 AG060935 from the National Institute on Aging of the National Institutes of Health (Epstein, Grabowski, Orav, and Joynt Maddox). Dr. Barnett receives compensation as an expert witness through Greylock McKinnon Associates.
Footnotes
Conflicts of Interest
The authors have no conflicts.
REFERENCES
- 1.Institute of Medicine (US) Committee on Nursing Home Regulation. Improving the Quality of Care in Nursing Homes [Internet]. Washington (DC): National Academies Press (US); 1986. [cited 2022 Apr 26]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK217556/ [PubMed] [Google Scholar]
- 2.Committee on the Quality of Care in Nursing Homes, Board on Health Care Services, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. The National Imperative to Improve Nursing Home Quality: Honoring Our Commitment to Residents, Families, and Staff [Internet]. Washington, D.C.: National Academies Press; 2022. [cited 2022 May 9]. Available from: https://www.nap.edu/catalog/26526 [PubMed] [Google Scholar]
- 3.FACT SHEET: Protecting Seniors by Improving Safety and Quality of Care in the Nation’s Nursing Homes [Internet]. White House. 2022. [cited 2022 Apr 26];Available from: https://www.whitehouse.gov/briefing-room/statements-releases/2022/02/28/fact-sheet-protecting-seniors-and-people-with-disabilities-by-improving-safety-and-quality-of-care-in-the-nations-nursing-homes/ [Google Scholar]
- 4.Konetzka RT. The Challenges of Improving Nursing Home Quality. JAMA Netw Open 2020;3(1):e1920231. [DOI] [PubMed] [Google Scholar]
- 5.Thomas KS, Rahman M, Mor V, Intrator O. Influence of hospital and nursing home quality on hospital readmissions. Am J Manag Care 2014;20(11):e523–531. [PMC free article] [PubMed] [Google Scholar]
- 6.Simning A, Orth J, Temkin-Greener H, Li Y. Patients discharged from higher-quality skilled nursing facilities spend more days at home. Health Serv Res 2021;56(1):102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huckfeldt PJ, Kane RL, Yang Z, et al. Degree of Implementation of the Interventions to Reduce Acute Care Transfers (INTERACT) Quality Improvement Program Associated with Number of Hospitalizations. J Am Geriatr Soc 2018;66(9):1830–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kane RL, Huckfeldt P, Tappen R, et al. Effects of an Intervention to Reduce Hospitalizations From Nursing Homes: A Randomized Implementation Trial of the INTERACT Program. JAMA Intern Med 2017;177(9):1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.U.S. Centers for Medicare & Medicaid Services. Bundled Payments for Care Improvement (BPCI) Initiative: General Information ∣ CMS Innovation Center [Internet]. 2022. [cited 2022 Apr 8];Available from: https://innovation.cms.gov/innovation-models/bundled-payments
- 10.The Lewin Group, Inc. CMS Bundled Payments for Care Improvement Advanced Model: Third Evaluation Report. 2022;89. [Google Scholar]
- 11.Barnett ML, Joynt Maddox KE, Orav EJ, Grabowski DC, Epstein AM. Association of Skilled Nursing Facility Participation in a Bundled Payment Model With Institutional Spending for Joint Replacement Surgery. JAMA 2020;324(18):1869–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joynt Maddox KE, Barnett ML, Orav EJ, Zheng J, Grabowski DC, Epstein AM. Savings and outcomes under Medicare’s bundled payments initiative for skilled nursing facilities. J Am Geriatr Soc 2021;69(12):3422–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dykema J, Stevenson J, Day B, Sellers SL, Bonham VL. Effects of Incentives and Prenotification on Response Rates and Costs in a National Web Survey of Physicians. Eval Health Prof 2011;34(4):434–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Centers for Medicare & Medicaid Services. Provider Data Catalog [Internet]. CMS. [cited 2022 Apr 29];Available from: https://data.cms.gov/provider-data/dataset/4pq5-n9py [Google Scholar]
- 15.LTCFocus Public Use Data sponsored by the National Institute on Aging (P01AG027296) through a cooperative agreement with the Brown University School of Public Health. LTCFocus [Internet]. LTCFocus. [cited 2022 Apr 29];Available from: https://ltcfocus.org [Google Scholar]
- 16.ResDAC. Skilled Nursing Facility (Fee-for-Service) [Internet]. Res. Data Assist. Cent [cited 2022 Apr 29];Available from: https://requests.resdac.org/cms-data/files/snf-ffs [Google Scholar]
- 17.Long Term Care Minimum Data Set (MDS) 3.0 ∣ ResDAC [Internet]. [cited 2022 Apr 21];Available from: https://resdac.org/cms-data/files/mds-30 [Google Scholar]
- 18.What Is a CCRC (Continuing Care Retirement Community)? ∣ U.S. News [Internet]. [cited 2022 Jul 3];Available from: https://health.usnews.com/senior-care/caregiving/articles/continuing-care-retirement-communities#expert-sources [Google Scholar]
- 19.U.S. Department for Health and Human Services. 2013 NCHS Urban-rural Classification Scheme for Counties. 2014. [PubMed]
- 20.Stata Multiple-Imputation Reference Manual [Internet]. [cited 2022 Apr 26];Available from: https://www.stata.com/manuals/mi.pdf
- 21.Burke RE, Xu Y, Ritter AZ. Outcomes of post-acute care in skilled nursing facilities in Medicare beneficiaries with and without a diagnosis of dementia. J Am Geriatr Soc 2021;69(10):2899–907. [DOI] [PubMed] [Google Scholar]
- 22.Joyce NR, McGuire TG, Bartels SJ, Mitchell SL, Grabowski DC. The Impact of Dementia Special Care Units on Quality of Care: An Instrumental Variables Analysis. Health Serv Res 2018;53(5):3657–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braun RT, Jung H-Y, Casalino LP, Myslinski Z, Unruh MA. Association of Private Equity Investment in US Nursing Homes With the Quality and Cost of Care for Long-Stay Residents. JAMA Health Forum 2021;2(11):e213817–e213817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hillmer MP, Wodchis WP, Gill SS, Anderson GM, Rochon PA. Nursing home profit status and quality of care: is there any evidence of an association? Med Care Res Rev MCRR 2005;62(2):139–66. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Medicare & Medicaid Services. Quality Measures ∣ CMS [Internet]. Cent. Medicare Medicaid Serv. 2022. [cited 2022 Dec 23];Available from: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/nursinghomequalityinits/nhqiqualitymeasures [Google Scholar]
- 26.Gandhi A, Yu H, Grabowski DC. High Nursing Staff Turnover In Nursing Homes Offers Important Quality Information. Health Aff Proj Hope 2021;40(3):384–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomas KS, Mor V, Tyler DA, Hyer K. The Relationships Among Licensed Nurse Turnover, Retention, and Rehospitalization of Nursing Home Residents. The Gerontologist 2013;53(2):211–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Med Care 2005;43(6):616–26. [DOI] [PubMed] [Google Scholar]
- 29.Loomer L, Grabowski DC, Yu H, Gandhi A. Association between nursing home staff turnover and infection control citations. Health Serv Res 2022;57(2):322–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kellerman Jenna. 1000+ New CNAs: State Launches New Pipeline Initiative to Help Alleviate Workforce Concerns ∣ LeadingAge Minnesota [Internet]. Lead. Age Minn 2021. [cited 2022 Dec 23];Available from: https://www.leadingagemn.org/news/1000-new-cnas-state-launches-new-pipeline-initiative-to-help-alleviate-workforce-concerns [Google Scholar]
- 31.FACT SHEET: President Biden to Announce Strategy to Address Our National Mental Health Crisis, As Part of Unity Agenda in his First State of the Union [Internet]. White House. 2022. [cited 2022 May 15];Available from: https://www.whitehouse.gov/briefing-room/statements-releases/2022/03/01/fact-sheet-president-biden-to-announce-strategy-to-address-our-national-mental-health-crisis-as-part-of-unity-agenda-in-his-first-state-of-the-union/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.