Summary
Harmful algal blooms (HABs) are increasing across many locations globally. Toxins from HABs can be incorporated into aerosols and transported inland, where subsequent exposure and inhalation can induce adverse health effects. However, the relationship between HAB aerosols and health outcomes remains unclear despite the potential for population-level exposures. In this review, we synthesized the current state of knowledge and identified evidence gaps in the relationship between HAB aerosols and human health. Aerosols from Karenia brevis, Ostreopsis sp., and cyanobacteria were linked with respiratory outcomes. However, most works did not directly measure aerosol or toxin concentrations and instead relied on proxy metrics of exposure, such as cell concentrations in nearby waterbodies. Furthermore, the number of studies with epidemiological designs was limited. Significant uncertainties remain regarding the health effects of other HAB species; threshold dose and the dose–response relationship; effects of concurrent exposures to mixtures of toxins and other aerosol sources, such as microplastics and metals; the impact of long-term exposures; and disparities in exposures and associated health effects across potentially vulnerable subpopulations. Additional studies employing multifaceted exposure assessment methods and leveraging large health databases could address such gaps and improve our understanding of the public health burden of HABs.
Keywords: Harmful algal blooms, Aerosols, Human health, Climate change
Introduction
Harmful algal blooms (HABs) are diverse phenomena consisting of rapid and exponential expansions and accumulation of microalgal populations, such as cyanobacteria, diatoms, and dinoflagellates, in aquatic ecosystems.1 Blooms can range from small, short-lived (days to weeks) patches to very large blooms that can cover areas spanning thousands of square kilometres and last from a few months to multiple years. The frequency, duration, severity, and geographical extent of harmful algal blooms across freshwater, estuarine, and marine ecosystems are increasing across many locations globally.2,3 These shifting patterns and distributions are driven primarily by climate change and anthropogenic nutrient loading.4 Climate change is leading to warming waters, more extreme wet/dry cycles, and acidification, leading to favourable conditions for the rapid proliferation of many HAB species.5 Excess nutrients from large-scale agriculture, industrialization, urbanization, and population growth can further lead to altered composition of nutrients and timing that create conditions that are ideal for blooms.6
The economic impacts of HABs on fishing and aquaculture, drinking water treatment and availability, livestock, and property values are substantial.7 HABs also pose a significant threat to public health as many HAB species can produce secondary metabolites, including potent toxins, that adversely impact many different human organ systems. The most well-understood and described routes of exposure to HABs and associated health effects include direct dermal contact leading to multiple symptoms such as rash and irritation, as well as ingestion of contaminated water or seafood resulting in gastrointestinal and neurotoxic effects.8 Under certain environmental conditions, toxins generated from HABs may become airborne, and subsequent inhalation of the generated aerosols can induce adverse health effects. The public health burden of HAB aerosols is likely to be considerable. One study estimated that approximately 15% of global asthma cases are attributable to the inhalation of aerosolized HAB toxins in coastal regions,9 while another work found that the 2012 red tide blooms in Florida were linked with approximately 11,000 hospital admissions and 4000 emergency department visits.10 This potential association between HAB aerosols and health outcomes remains unclear despite the potential for ubiquitous exposures for populations living near or downwind of HABs, occupations that interact directly with HABs (e.g., lifeguards), or recreational users in bodies of water with HABs.
Prior reviews have focused on the health effects of a single HAB species,11,12 or provided a broader overview of the array of symptoms associated with different HAB exposure pathways.8 In this review, we describe the mechanisms of exposure to aerosolized HAB toxins and the associated health effects. We first conducted a title and abstract review on articles identified through PubMed and then summarized those that investigated health outcomes with HAB aerosols as a potential source of exposure. We then summarized the mechanisms by which HAB toxins can be aerosolized, transported, and inhaled, in addition to the current methods for exposure assessment of HABs and aerosols. Finally, we synthesized the current state of knowledge and identified evidence gaps.
Mechanisms of aerosolization, transport, and exposure for HAB toxins
Aerosolization
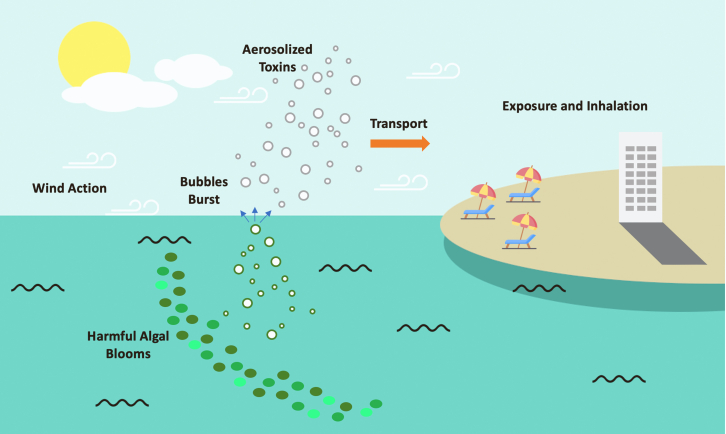
In this section, we briefly summarize the mechanisms by which toxins from HABs can be aerosolized, transported, and inhaled (Fig. 1). Toxins from microalgae/bacteria suspended at the water surface from HABs can be emitted to the atmosphere by aerosolization. The primary mechanism of aerosolization from blooms is via the formation of spray aerosols (SA) in marine (sea spray aerosol; SSA),13,14 freshwater (lake spray aerosol; LSA),15,16 or estuarine environments.17 SAs are formed when wind-driven wave action entrains plumes of air bubbles beneath the water followed by bubbles bursting at the air-water interface, ejecting water droplets into the atmosphere that can contain organic material from cells or whole cells themselves.18, 19, 20 Elevated concentrations of biomass during HAB conditions result in a greater proportion of the SA mass composed of biological material along with shifting of the size distributions.15 The properties of bubbles leading to aerosolization significantly differ between marine SSA and freshwater LSA, with bubbles formed in freshwater much larger than in seawater.21 The larger bubbles, combined with different aquatic chemistry for marine and freshwater systems, lead to dramatically different aerosol concentrations, particle size distributions, and aerosol chemical composition.22 For example, ambient LSA number concentrations are about one-third that of SSA and have a chemical composition composed primarily of calcium carbonate and organic carbon. Studies on freshwater and estuarine SA generation and HAB toxin aerosolization remain relatively limited compared to marine environments.
Fig. 1.
Diagram depicting the mechanisms of aerosolization, transport, and exposure to harmful algal bloom toxins.
The mechanisms by which HAB toxins become incorporated into aerosols are dependent on species and environmental conditions. Brevetoxins, which are hydrophobic toxins produced by K. brevis, are mainly released into the water column through cell lysis due to physical forces, especially towards the end of the blooms.12 Toxins from cyanobacteria, on the other hand, are not usually released from cell lysis due to shear stress or turbulence but are released during cell senescence, exposure to heightened salinity, or from lysis from viral activity.23 These extracellular toxins are then enriched at the air-water interface of the bubbles generated by wave action and water turbulence.12 Toxin concentration levels in aerosols may be significantly higher than in the water due to bubble scavenging, with one work finding that aerosols can contain levels of brevotoxin that are 20–50 times greater than in seawater,24 while another study found 78- to 1769-fold enrichment of phycotoxins in SAs.25 The aerosols generated from seawater and freshwater cover a wide size range important for inhalation exposure. Analyses of the particle size distribution of air samples collected during red tides showed that the generated aerosols were mainly coarse particles, which deposit mainly in the upper respiratory tract, with a small percentage (2–6%) that would travel to tracheobronchial and alveolar regions.24,26 An analysis of aerosols and multiple HAB toxins (brevetoxin, okadaic acid, pectenotoxin-2, domoic acid, tetrodotoxin, saxitoxin, ciguatoxin, and ω-Conotoxin) off the coast of China found that the particles were predominantly coarse, and deposition efficiency was found in the head airway region (74.06%–75.76%), followed by the alveolar (16.14%–17.40%) and tracheobronchial (8.24%–8.69%) regions.27 An experimental study found that an increase in cyanoHAB activity enhanced aerosol production in the ultrafine size range (da < 100 nm) and accumulation modes (100–1000 nm),28 which can penetrate deeper into the respiratory tract than fine and coarse aerosols. The size of aerosols further varies as a function of distance from HAB locations. Inland microalgae and cyanobacteria frequently occurred in particles not exceeding a diameter of 3.3 μm, while over the sea bioaerosol particles had a diameter of >3.3 μm, as smaller particles are likely to be transported further inland via wind.29
Transport
The transport of SA in the environment is dependent primarily on the aerodynamic diameter and meteorology. Wave action can produce SSA that can be transported up to 1000 km via wind.30 Prior measurements of LSA concentrations have observed LSA transported >30 km inland,31 while modelling has shown that freshwater aerosol production contributes significantly to particle number concentrations over the Great Lakes region and significantly impacts atmospheric chemistry over the lakes.32 The maximum distance travelled by aerosolized toxins could be transported depends on the stability of the compound in question under a range of environmental conditions and remains unclear due to the difficulty of measuring some toxins and scarce direct measurement data. During the Florida red tide, brevetoxins produced by Karenia brevis were detected in the aerosol samples as far as 4.2 km from the beach of origin,33 while during cyanobacteria HAB events, microcystin in atmospheric particles could be transported many kilometres inland without degradation as it is a very stable compound.23 Bioaerosols collected over the Baltic Sea, as well as hundreds of meters inland, harboured cyanobacteria and other related microalgae species.28 Multiple HAB toxins have been detected at a sampling site that was 25 km away from the coast in Qingdao, China.27 Aerosolized toxins may also persist along the shore, where blooms tend to accumulate.23
Inhalation
After transport onshore by wind, aerosolized HAB toxins are deposited mostly in the upper respiratory tract. Brevetoxins were detected in the nasal-pharyngeal swabs of individuals (n = 129) exposed to red tide events.34 After recreational activities in a small lake with a cyanobacterial bloom, low levels of microcystins were detected in water and air samples, but blood levels were below the level of detection (n = 97).35 In a study of children and adults (n = 81) who had gone to two California lakes, microcystin levels before and after recreational activities were measured in plasma and nasal swab specimens, with elevated concentrations in nasal specimens but not in plasma.36 An examination of MC levels in the nasal mucosa of participants (n = 125) during a cyanobacterial bloom of cyanobacteria Microcystis aeruginosa found that 95% had concentrations of MC above the limit of detection, with significantly elevated MC concentrations among individuals with direct contact with impacted waters compared to those with no recent contact.37 In this work, nasal concentrations of MC were found to vary by time and location of exposure to HAB, with the highest levels observed during periods when concentrations in the surrounding waters peaked. In contrast, there was no statistical difference in detected levels between bloom and non-bloom seasons as well as residential proximity to a body of water in a study (n = 29) in cyanotoxins levels in the upper airways and central airway were detected using PCR, suggesting that exposure could be more ubiquitous across both time and space, including locations that are not nearby waterbodies.38 The studies that have examined cyanotoxin in the blood did not detect concentrations above detectable limits,34,35,38 suggesting that the toxins may not cross the blood-air barrier or that the HAB toxins may transform into other metabolites that have not been identified thus far.23
Climate change, HABs, and human health
Intergovernmental Panel on Climate Change's (IPCC) Special Report on the Ocean and Cryosphere in a Changing Climate (SROCC) in 2019 directly linked HABs to climate change, stating with high confidence that “harmful algal blooms display range expansion and increased frequency in coastal areas since the 1980s in response to both climatic and non-climatic drivers such as increased riverine nutrients run-off.”39 However, the extent to which climate change is intensifying HABs remains unclear. Warming is linked to shifts in the composition of microorganisms and the promotion of rapidly proliferating HABs.2 Studies have shown that progressively warming waters have resulted in regions with increasing frequencies and intensities of HABs, resulting in HAB extents that may be moving towards higher latitudes.2,4 Acidification with increasing CO2 levels in the water may be further promoting growth rates of HABs, whereas non-harmful algae did not demonstrate this trend.40 Altered precipitation patterns and the frequency of extreme weather events are further impacting the delivery of nutrients into aquatic ecosystems.41 Accelerating eutrophication can lead to algal blooms and subsequent loss of dissolved oxygen, furthering a change in ecosystem states that pose major threats to both aquatic ecosystems and human health. While regional analyses have reported increasing trends, the global trends are less clear. Analysis of the recent 30-year (1990–2019) database from the Harmful Algae Event Database and Ocean Biodiversity Information System (HAEDAT) shows an increasing trend in all HAB events.1 However, these trends are not uniformly consistent across regions and may be due in part to increased awareness, monitoring, and reporting.42 Freshwater HABs and their toxins are transported along a connected network of estuarine and coastal water sources, requiring multiregional assessments and solutions.43
Predicting how HABs will respond to climate change is challenging as this will vary significantly across species, interactive effects of stressors that impact growth, and adaptation. The effects of warming and acidification on toxin production are also unclear, with species-specific responses reported.44 Studies may disagree on the magnitude or even the direction of the growth rate response of HAB genera to climate change perturbations such as CO2.45 Overall, the effects of climate change on toxin production – and thus the associated health impacts-remain uncertain, as the relationship between temperature and HAB toxicity is complex and highly dependent on a variety of contributing factors including nutrient and light status as well as species composition, which may further differ geographically.
Overview of current exposure assessment and surveillance methods
Direct sampling of waters via vessels and collecting samples from buoys and moored automated collection devices are the most common and traditional approaches for assessing HAB composition and size.46 Within the collected samples, cells are identified and characterized with microscopy, diagnostic photopigments, and nucleic acid techniques. Toxins are thereafter extracted and then analysed. However, this process is expensive and time intensive, and the personnel and equipment may not be available to collect sufficient data with the needed spatial and temporal scales needed to fully characterize bloom occurrences, size, duration, and toxin production rates. Reconstruction of HAB events is thus frequently based on the best available data, which are often limited and not definitive. Furthermore, HAB events may occur in regions without available resources for sampling and analysis.
Ambient measurements are needed to accurately quantify HAB toxin aerosolization, as toxin production by HABs and aerosolization is highly variable across time and space, species, and environmental conditions. Concentration levels of aerosols and toxins-and associated health impacts-cannot be easily predicted from the physical size or composition of a HAB.28 However, the measurement of bioaerosols and toxins in the atmospheric air is difficult and complex. Physiochemical parameters can greatly impact aerosolization efficiency, leading to different relative amounts of toxins in the aerosol phase compared to the water.28 As there are no standards for ways samples are collected, stored, or analysed, similar techniques used to study microorganisms in the air or particulate matter (PM) are applied. The most common approach for sampling aerosols is using a filter sampler, cascade impactor, or impinger. Filter samplers pull flow through a filter (e.g., quartz fibre) and generally collect most aerosols below the size of a pre-selector (typically a cyclone with a PM2.5 or PM10 size cut).28 Cascade impactors use inertial impaction and collect multiple size-fractionated samples onto substrates (e.g., aluminium or glass fibre filters), which then provide information on size-resolved aerosol composition.47 For both filter samples and cascade impactors, the resulting samples are extracted prior to analysis, often by liquid chromatography coupled to tandem mass spectrometry (LC/MS/MS). Impingers collect directly into the water,48 avoiding the extraction step, but are at generally lower flow and collect less aerosol material. Previous works used enzyme linked immunosorbent assays (ELISA) to detect HAB toxins in the sampled particulate matter.26,27 ELISA kits provide total HAB toxin concentration, but there are >300 congeners with different amino acids or other molecular modifications whose prevalence connects to bloom conditions.49 These congeners have different toxicity and bioavailability,50 which makes connecting total toxin concentrations to exposure and health outcomes challenging. Recent research has used LC/MS/MS to quantify specific congeners,51 as well as identify new congeners.52
Recently, there have been significant advances in instruments that are available to detect cell abundance automatically and remotely. These instruments take advantage of either unique morphologies, genetic or chemical signatures targeted by molecular probes or imaging technology that can take pictures of cells in rapid succession. There also have been significant advances in satellite remote sensing allowing environmental managers and government agencies to detect and manage HABs.53,54 Satellite remote sensing provides spatiotemporal coverage that instruments and surveys are unable to achieve.55 Remote sensing can leverage specific optical signals related to HABs, such as chlorophyll a and other diagnostic photopigments, for developing algorithms for HAB detection. For example, a recent analysis of 2.91 million Landsat satellite images from 1982 to 2019 across 88 lakes across 6 continents found an increase of locations that experienced algal blooms, with the most pronounced increases in Asia and Africa.56 The major limitations of satellite images are that they cannot be used to measure toxin concentration levels or identify HAB types and that they can only provide information for the surface layer. Nevertheless, satellite images could be utilized in conjunction with collected samples for the prediction and mapping of HAB toxin concentration levels. Recent efforts have expanded using drones to sample air57 and water48 over HABs. Citizen science, such as the incorporation of data from social media and sensors, offers an additional approach to monitor and/or characterize HABs or supplement ongoing tracking efforts.58 Municipal requests for information or services (311 calls) could serve as an additional surveillance tool as they were associated with cyanobacterial algal blooms and waterborne microcystin-LR concentrations in Cape Coral, Florida.59
Human health effects and mechanisms
We conducted a title and abstract review on articles identified through PubMed and summarized studies that 1) examine respiratory outcomes in relation to HAB exposure, as aerosol inhalation is the most likely route of exposure, and/or 2) investigate HAB as a potential mechanism of exposure. We found that most studies were limited to those examining K. brevis, Ostreopsis sp., and cyanobacteria, and we summarize the findings below, as well as in Table 1, Table 2, Table 3, Table 4.
Table 1.
Summaries of studies on Karenia brevis aerosols and health (n = 15).
| Author and year | Location | Exposure assessment method | Population and study period | measured outcome | Findings summary |
|---|---|---|---|---|---|
| Backer 2003 | Sarasota and Jacksonville, Florida, USA | Seawater samples were collected twice per day to measure the concentrations of K.brevis cells and brevetoxins. To obtain spatial brevetoxin distribution over the beach and surrounding areas, six high-volume air samplers were placed. Brevetoxin analyses were performed by High Performance Liquid Chromatography (HPLC). Exposure was then categorized into three levels according to K. brevis cells or brevetoxin concentrations: low/no exposure, moderate exposure, and high. |
129 adults (≥18 years) who spent time (10 min to ∼8 h; average of 71 min) on beaches in Sarasota or Jacksonville during February and October 1999. | Pre- and post-beach visits. Spirometry test values: peak expiratory flow (PEF); forced expiratory volume in 1s (FEV1); forced vital capacity (FVC); and the ratio of FEV1 to forced vital capacity (FEV1/FVC). Upper respiratory symptoms (eye and throat irritation, nasal congestion, cough), lower respiratory symptoms (chest tightness; wheezing; shortness of breath), and other symptoms (itchy skin; headaches; and others) as measured by questionnaires. The nasal–pharyngeal swabs were collected to compare the inflammatory response, as measured by the relative percentages of neutrophils vs. chronic inflammatory cells (e.g., macrophages, lymphocytes, plasma cells). |
After exposure to aerosolized brevetoxins during red tide events, participants experienced upper and lower respiratory irritation. Those with high or medium exposure reported more symptoms than low/no exposure participants. An increase in inflammation (mostly acute and sub-acute in nature) in the nose and/or throat swab sample was observed in 49% and 39% of participants sampled on high and moderate exposure days, respectively. No significant changes in pulmonary function were reported. |
| Backer 2005 | Sarasota and Manatee, Florida, USA | For cell counts, water samples were collected three times per each day from the surf zone adjacent to the study high-volume air sampler locations. To assess lifeguard exposure to brevetoxins in the air, samples were collected using high-volume air samplers and personal breathing zone samplers. Brevetoxins from the environmental and personal air samplers were analysed via liquid chromatography-mass spectrometry (LC-MS) and enzyme-linked immunosorbent assay (ELISA). |
28 healthy lifeguards (≥18 years) who are occupationally exposed to red tide toxins during daily work activities. Unexposed period: May 2002, January 2003; exposed period: September 2001, March 2003. |
Spirometry and symptoms before and after 8-hr shifts during an unexposed period and again during an exposure period. Spirometry tests: FVC; FEV1; FEV1/FVC percentage; FEF25–75%; and PEF. Upper respiratory symptoms (eye and throat irritation, nasal congestion, cough), lower respiratory symptoms (chest tightness; wheezing; shortness of breath), and other symptoms (itchy skin; headache; and other) measured by questionnaires. |
Brevetoxin concentration levels displayed spatial and temporal variability. Compared with unexposed periods, the group of lifeguards reported upper respiratory symptoms and headache during the periods of aerosolized brevetoxin exposure but did not report lower respiratory symptoms. No impact of exposure on pulmonary function, with or without mild exercise, was reported. |
| Fleming 2005 | Sarasota, Florida, USA | For cell counts, water samples were collected three times per each day from the surf zone adjacent to the study high-volume air sampler locations. Samples were collected using high-volume air samplers equipped to capture aerosol particles by size, and personal breathing zone samplers. Concentrations of brevetoxins on portions of the samplers, as well as the nasal and throat swabs, were analysed by LC-MS and ELISA. |
59 persons (≥12 years) with physician-diagnosed asthma. The use of asthma medications within 12 h before going to the beach was used as a surrogate for asthma severity. Unexposed period: January 2003; exposed period: March 2003. |
Spirometry test values before and after 1 h exposure: FVC; FEV1; FEV1/FVC percentage; FEF25–75%; and PEF. Respiratory symptoms (cough; wheezing; shortness of breath; chest tightness), and other symptoms (throat irritation; nasal congestion; eye irritation; headache; itchy skin; and diarrhoea) measured by questionnaires. The nose and throat swabs taken pre- and post- beach trips were analysed for neutrophils and chronic inflammatory cells, protein transudation, amount of fibrin, and percentage of reactive epithelial cells |
Participants were significantly more likely to report respiratory symptoms and report respiratory impairment after Florida red tide exposure. Participants demonstrated small but statistically significant decreases in FEV1 FEF25–75%, and PEF; stronger effects were seen among those regularly using asthma medications. Increased but not statistically significant levels for inflammation were seen. |
| Kirkpatrick 2006 | Sarasota, Florida, USA | The red tide cell count data were provided by the Phytoplankton Ecology Program at Mote Marine Laboratory, Sarasota, FL. This program routinely monitors a minimum of two shore locations on its campus. Water samples are analysed weekly during non-bloom conditions and daily during blooms; blooms are defined as when cell counts are over 100,000 cells/L. | Emergency room (ER) visits between two time periods; October 1–December 31, 2001 (red tide period) and October 1–December 31, 2002 (non-red tide period) in Sarasota, FL. | Using the ICD-9 codes (460–519), diagnoses were categorized as pneumonia, bronchitis, asthma, upper airway disease, or all other primary diagnoses. | A significant increase in the rate of annual ER admissions were found for respiratory diseases (pneumonia – by 31%, bronchitis – 56%, asthma – 44%, and upper airway disease – 64%) during the 2001 red tide exposure period vs. the 2002 non-red tide period in the coastal areas. No increases were seen in the non-coastal areas. |
| Milian 2007 | Sarasota, Florida, USA | Six high volume air samplers collecting brevetoxin levels and particle size were placed on the beach in the same area where study participants walked for 1 h. Near shore water samples were collected 3 times per day and evaluated for cell counts and brevetoxin concentrations. Every participant carried a personal air sampler during their beach walk to determine an individualized aerosol dose. Brevetoxin analyses for all environmental monitoring were performed by HPLC and by ELISA. |
97 persons (≥12 years) with physician-diagnosed asthma (unexposed period: March 2003 and, March 2005; exposed period: January 2003, May 2004 October 2004). | Respiratory symptoms (e.g., eye and/or throat irritation; nasal congestion; cough; wheeze; chest tightness; and shortness of breath) and other symptoms designed to identify people who over-report symptoms (e.g., headache; itchy skin and/or diarrhoea), as well as the use of asthma medications, were recorded before and after each 1-h beach walk. The participants further categorized and scored their symptom intensity. |
Inhalation of aerosolized brevetoxins during exposure events resulted in statistically significant increases in the respiratory symptom intensity scores; both coastal and inland residents both reacted significantly, suggesting that location of residence does not modify the observed relationships. Asthmatics who use medications reported fewer changes in respiratory symptom intensity compared with non-medicated asthmatics when exposed to aerosolized brevetoxins. |
| Fleming 2007 | Sarasota, Florida, USA | Water samples were collected twice daily and analysed for K. brevis cell counts and for brevetoxin using both the ELISA and LC-MS analyses. To sample air for toxin and particulate size, three types of samplers were used: high-volume air samplers; high volume air with impactors to capture aerosol particles by size; and personal breathing zone monitors. |
97 persons (≥12 years) with physician-diagnosed asthma (unexposed period: March 2003 and, March 2005; exposed period: January 2003, May 2004 October 2004). | Respiratory (cough, wheezing, shortness of breath, chest tightness); other (throat irritation, nasal congestion, eye irritation, headache, itchy skin, diarrhoea) symptoms. Spirometry test values pre- and post-beach visit (FVC; FEV1; FEV1/FVC percentage; FEF25–75%; and PEF.) The use of asthma medications within 12 h before going to the beach was used as a surrogate for increased asthma severity. |
Participants were significantly more likely to report respiratory symptoms after brevetoxin aerosol exposure than before exposure. Participants demonstrated small, but statistically significant, decreases in FEV1, FEF25–75%, and PEF after brevetoxin exposures, particularly among those participants regularly using asthma medications. |
| Fleming 2009 | Sarasota, Florida, USA | Water samples were collected twice daily and analysed for K. brevis cell counts and for brevetoxin using both the ELISA and LC-MS analyses. To sample air for toxin and particulate size, three types of samplers were used: high-volume air samplers; high volume air with impactors to capture aerosol particles by size; and personal breathing zone monitors. |
87 persons (≥12 years) with physician-diagnosed asthma. Florida red tide exposure periods in March 2005 and September 2006. |
Respiratory (cough, wheezing, shortness of breath, chest tightness); other (throat irritation, nasal congestion, eye irritation, headache, itchy skin, diarrhoea) symptoms. Spirometry test values pre- and post-beach visit (FVC; FEV1; FEV1/FVC percentage; FEF25–75%; and PEF.) The use of asthma medications within 12 h before going to the beach was used as a surrogate for increased asthma severity. |
After 1-hr of exposure to low concentrations of brevetoxin aerosols, asthmatics had statistically significant increases in self-reported respiratory symptoms and total symptom scores. Pulmonary function changes were not observed. Symptoms increased significantly in those not using asthma medication and those living inland. |
| Hoagland 2009 | Sarasota, Florida, USA |
In situ K. brevis cell counts in the ocean served as a proxy for aerosolized brevetoxin concentrations. Water samples were collected at two Sarasota Bay locations and analysed weekly during non-bloom conditions and daily during blooms. The in situ cell count was averaged from the two stations. |
The total number of daily emergency department (ED) visits for respiratory diagnoses (October 2001–September 2006) | Hospital emergency department visits (2001–2006) at Sarasota Memorial Hospital for total of all four respiratory diseases (pneumonia, bronchitis, asthma, upper airway disease UAD) and a combination of UAD and bronchitis. | The statistical models showed that the number of emergency department visits for respiratory ailments was positively associated with 1-week lagged K. brevis cell counts after adjustment for confounders (e.g., temperature, Flu season, pollen counts, tourist visits). The models estimated the marginal costs of illness for respiratory ED visits associated with blooms to be ranging from $0.5 to $4 million, depending on the bloom severity. |
| Kirkpatrick 2010 | Sarasota, Florida, USA | The red tide cell count data were provided by the Phytoplankton Ecology Program at Mote Marine Laboratory, Sarasota, FL. This program routinely monitors a minimum of two shore locations on its campus. Water samples are analysed weekly during non-bloom conditions and daily during blooms | The total number of emergency room (ER) admissions during the Florida red tide bloom period was during the fall of 2001 (September 1–December 31, 2001), and the non-bloom period during the fall of 2002 (September 1–December 31, 2002). The number of ER admissions was similar (21,308 in 2001 vs. 22,270 in 2002). |
ER admission diagnosis with the ICD-9 codes for gastrointestinal (GI) diseases (530–579). Further classification for selected outcomes most consistent with exposure to brevetoxins: gastritis, duodenitis, and non-infectious enteritis and colitis (acute, chronic, unspecified, and other) (ICD 535.0–537.9 and 557.0–558.0). |
ER admissions rates (adjusted for age) were not significantly different between the 2 years for all GI diseases (RR = 1.01; 95% CI: 0.92–1.10). ER admissions rates for the selected gastrointestinal diagnoses (RR = 1.40; 95% CI: 1.06–1.84) were significantly different for the Florida red tide bloom period compared to the no red tide period. No significant difference between the 2 time periods for the ER admission rates for all other gastrointestinal diagnoses (1.04; 0.94–1.16). |
| Bean 2011 | Sarasota, Florida, USA | Participants spent ≥1 h at the beach with field/personal environmental monitoring. Each participant had at least evaluation during an active bloom (exposure period) and during a period without a bloom (non-exposure period) each. Measures of red tide toxins were through monitoring (cell counts for K. brevis > 100,000 cells/L in the sampled water), brevetoxins detected via ELISA, and/or LCMS in both water and air. |
125 asthmatic participants (self-reported diagnosis by a physician; ≥12 years old; smoked for ≤10 years; able to walk ≥30 min on the beach; resident of the Sarasota, Florida for ≥6 months) in a cohort of asthmatics over 7 years. 38 participants with 1 exposure study (Group 1) were compared to 36 who participated in ≥4 studies (Group 2). |
Pre- and post-exposure pulmonary functions measured by spirometry (the pre-exposure percent predicted values for FEV1, PEF, and FEF25–75%). A respiratory symptom intensity score – mild (1), moderate (2), and severe (3). |
There were no significant changes in the pulmonary functions associated with exposure over a 7-year period among the participants who participated in ≥4 exposure evaluations, indicating that living in areas with occasional K. brevis blooms do not exhibit long-term respiratory effects from repeated, intermittent exposures to brevetoxin aerosols. |
| Kirkpatrick 2011 | Sarasota, Florida, USA | Water samples were collected twice daily at Siesta Key beach during the main beach study and throughout the 5 days follow-up study. The water samples were analysed for K. brevis cell counts and for brevetoxin concentrations, using brevetoxin ELISA and LC–MS analyses. During the primary beach study, air samples for toxin and aerosol particle size were collected using two types of high-volume samplers and a personal sampler of the subjects' breathing zones. |
52 participants (≥12 years) with self-report of physician-diagnosed asthma and who agreed to do study activities over 5 additional days after the day of their initial 1 h beach exposure. | The spirometry values included the peak expiratory flow (PEF). Respiratory symptoms established as relevant to brevetoxin exposure in past studies (cough, wheeze, throat irritation, shortness of breath, chest tightness, nasal congestion, eye irritation, and headache) were asked before and after spending 1 h on the beach, as well as in the follow-up interviews and symptom diaries. Categorized as severe asthmatics vs. controlled asthmatics based on the use of asthma medications within 12 h before going to the beach. |
Asthmatics may continue to experience increased symptoms and suppressed respiratory function suppression for several days after 1 h of exposure to the brevetoxin aerosols. After exposure during an active bloom, subjects had elevated mean symptoms which did not return to the pre-exposure baseline for at least 4 days. The PEF measurements decreased after the initial beach exposure, with a subsequent additional delayed effect within 24 h, and continued to be suppressed after 5 days. Most pronounced effects were seen in severe asthmatics and those living inland. |
| Hoagland 2014 | 6 counties in Southwest Florida, USA | Two measures of red tides: (1) opportunistic water sampling of the number of K. brevis cells per litre of seawater within 15 km of the coast collected once blooms were known to occur; and (2) the closures of individual shellfish harvesting areas to mitigate illnesses resulting from the consumption of contaminated shellfish. | Monthly emergency department (ED) data 2005–2009 and monthly hospital inpatient data from 1999 to 2009 in older (≥55 years) patients | Diseases of the respiratory system (ICD-9 codes 460.0–519.2) and diseases of the digestive system (520.0–579.9) using a time-series model using monthly data at the county level | Adverse respiratory and digestive health effects were significantly associated with increases in two measures of red tides. Annual costs of illness ranged from $60,000 to $700,000, potentially exceeding $1 million per year for severe red tide blooms |
| Diaz 2019 | 6 counties in Southwest Florida, USA | Measures of red tide blooms were compiled using counts of K. brevis cells obtained through opportunistic water sampling efforts along the Gulf coast during the study period. These included all K. brevis counts greater than 103 cell counts/L within 15 km of waters of the counties. As sampling was not consistent across space and time, the maximum cell count in a month and county was used to represent bloom severity. |
Emergency department (ED) visits in older (≥55 years) patients between 2005 and 2009 | Headache (ICD-9 784.0) as a primary diagnosis | Significant increases in ED visits for headaches as the primary diagnosis were observed during coastal K. brevis blooms |
| Abdullah 2022 | 5 counties in Southwest Florida, USA | A surrogate variable for aerosolized brevetoxin was developed, which generated an estimate of exposure derived from K. brevis cell counts in coastal waters in relation to the participants' home location. | Data on past medical history and medical symptoms were collected from n = 258 participants enrolled between June 2019 and August 2021; n = 70 were seen twice. | Upper respiratory tract symptoms (coughing, sneezing, sore throat, nasal congestion); neurological (headaches and dizziness); and systemic outcomes (fever, chills, nausea). | A linear dose-dependent relationship between the magnitude of K. brevis blooms and upper respiratory tract symptoms was seen. Linear dose–response relationship between exposure and neurotoxin shellfish poisoning-like symptoms (weakness, headaches, dizziness, muscle pain, stiff neck, metallic taste); no impact of seafood consumption on this relationship, suggesting that brevetoxin aerosols can induce these symptoms. |
| Stumpf 2022 | Sarasota and Manatee Counties, Florida, USA | Monthly and annual bloom severity indices (BSI) derived from the historical cell count observations along the southwest Florida shoreline. | Beach Conditions Reporting System (BCRS) provided respiratory irritation reports based on the intensity of the coughing as routinely reported by volunteers. Eight beach sites in Sarasota and Manatee Counties, Florida; August 2006–January 2019 |
Respiratory irritation conditions reported once or twice daily by the volunteers were used to determine the respiratory measure falling into the 4 categories (none, slight, moderate, high) for each beach site. A monthly respiratory irritation index (RI) was developed using the sum of days with respiratory irritation observations across the eight beach sites over a month divided by the number of sites and the number of days for a given month. |
The seasonality of RI mirrors that of the BSI with a peak in the fall, decreasing in winter and lowest frequency in the spring. RI generally corresponded with BSI, but discrepancies were observed. The onshore wind anomalies were related to such discrepancies between the monthly BSI and RI, indicating their influence in predicting respiratory irritation due to blooms. |
Table 2.
Summaries of studies on Ostreopsis sp. aerosols and health (n = 6/8).
| Author | Location | Exposure assessment method | Population and study period | Measured outcome | Findings summary |
|---|---|---|---|---|---|
| Galitelli 2006 | Coasts of Bari, Italy | Unusual proliferations of the Ostreopsis genus (more than 1 million cells/L) occurred during summers of 2003 and 2004. | 28 patients (9 men, 18 women, and 1 child; mean age, 38.6 years; range, 10–68 years) were identified with symptoms occurring during recreational or working activities on the beach. | Rhinorrhoea; dry or mildly productive cough; fever; bronchoconstriction with mild dyspnoea and wheezing; conjunctivitis | The most common symptom was rhinorrhoea (100% of patients); cough (43%); fever (14%); and bronchoconstriction with mild dyspnoea and wheezes (43%). Conjunctivitis was also observed (11%). No hospitalization was required; some symptoms ceased within a few hours of exposure. Cough, fever, dyspnoea, and wheezing lasted up to 24 h. There was no relationship between symptoms and exposure duration or activities. |
| Bresciani 2007 & Durando 2007 | Genova and La Spezia, Italy | After symptoms were reported, local environmental protection staff analysed air and water samples to exclude the presence of chemical pollution. After Ostreopsis was suspected as the causative agent, sea water from around five beaches were sampled for analysis during and after the outbreak; high densities of Ostreopsis ovata were detected. The analysis of water, plankton and macrophyte samples showed the presence of ‘putative palytoxin’. |
Summers of 2005 and 2006 | A case definition was constructed: presence at the seaside with an ongoing Ostreopsis ovata algal bloom; seeking medical care in a hospital emergency department; and presenting with at least two of the following symptoms: cough, dyspnoea, sore throat, rhinorrhoea, fever ≥38 °C, headache, lacrimation, nausea/vomiting and dermatitis. Patients who met the case definition were asked to provide detailed demographics, symptoms, time-activity, and baseline health data. |
During the summer of 2015 in Genoa, a total of 209 patients (mean age 35.9 ± 20.1 years, range 1–89 years) met the case definition. Mean onset of symptoms was 4 h 33 min (median 7 h, range 30 min–23 h) after the beginning of exposure. For most, the symptoms stopped. Overall, 43 patients seeking medical help at the emergency departments needed hospitalization. The most frequent symptoms were fever (63.6%), sore throat (50.2%), cough (40.2%), and dyspnoea (38.8%). Samples for laboratory analysis were available during the acute phase in 82 patients (39.2%). Of these patients, 46.3% had leucocytosis, and 40.2% had neutrophilia. No other significant divergence from normal laboratory values (transaminases, gamma-glutamyl transpeptidase, creatinine and sedimentation rate) was found. All electrocardiogram and chest X-ray tests were negative. None of the examined risk variables regarding time activity patterns (e.g., distance from the sea, length of stay on the beach), demographics, or comorbidities were associated with hospitalization. During the following summer, along with new Ostreopsis algal blooms, 19 cases matching the above described case definition were identified by the surveillance network in both cities of Genoa and La Spezia. thought that only a few of these were caused by inhalation of aerosolised O. ovata fragments. |
| Vila 2008 | Sant Andreu de Llavaneres, Catalonia, Spain | Seawater was sampled and cells were counted using microscope | 62 people were interviewed for symptoms during outbreak; summer 2004. | Rhinorrhoea, nose irritation, throat irritation, coughing, expectoration, eye irritation, and migraine | The main symptoms were rhinorrhea (74.2%), nose irritation (66.1%), throat irritation (62.9%), coughing (59.7%), expectoration (51.6%), eye irritation (41.4%) and migraine (40.3%). The estimated period between exposure and symptoms was around 3 h, and the symptoms persisted for around 45 h. Symptoms increased during evenings. |
| Tichadou 2010 | French Mediterranean coast | The French Mediterranean Ostreopsis Surveillance Network operates on an active basis during the blooming period from June 15 to September 15, which provides environmental monitoring by visual observation and testing of water samples; and a health vigilance system to detect suspected cases arising from direct contact or inhalation of contaminated water. | Between 2006 and 2009, nine blooms were observed, five of which led to 47 patients presenting symptoms. | Symptoms reported by affected, which included mild skin, mucosal, and/or respiratory irritations. | Ostreopsis blooms induce skin and respiratory disorders when human beings are exposed to saltwater with a high concentration of algal cells. Severe cases with prolonged exposures reported general flu-like symptoms, including headache, joint pain, vertigo, fever, fatigue, and diarrheal. Symptoms regressed without treatment within 12–72 h. |
| Illoul 2012 | Beaches in Western area of Algiers Wilaya, Algeria | In July 2009, 9 samples were taken few days after the toxic event from five beaches. At 14 beaches, at least one monthly water sample was taken at each beach between August 2009 to February 2011 and cell abundance was measured using microscopy. To estimate the abundances of epiphytic Ostreopsis cells, macroalgae samples (red, brown and green algae) were occasionally taken in select beaches. To identify the Ostreopsis species, molecular analyses via PCR amplification were attempted on different water samples collected during a former summer sampling in 2008 and during the 2009 and 2010 blooms. |
Approximately 300 patients reported symptoms during July 2009 | Human respiratory intoxication episode registered during July 2009 in five beaches of the western area of Algiers Wilaya. Fever, rhinitis, conjunctivitis, cough and skin irritations were the most common clinical symptoms observed. |
Relatively high levels of Ostreopsis were detected in the first samples taken a few days after the human intoxication event (19 and 22 of July 2009). Otherwise, Ostreopsis was also detected with abundances ranging from with period ranges from July to December 2009 and from April 2010 to January 2011. These values were generally lower than past values reported in the Northern Mediterranean. When macroalgae were sampled, Ostreopsis was also detected. |
| Vila 2016 | Sant Andreu de Llavaneres, Catalonia, Spain | Water samples were taken at very shallow (about 20–50 cm) depths. Samples for the estimations of epiphytic Ostreopsis were collected from the macroalgae mat. Cell numbers in the water column and the mat were estimated from the samples via microscopy. |
16 staff of a nearby indoor-outdoor restaurant directly exposed to marine aerosols at least 8 h daily from June to December 2013. | Ostreopsis-related symptoms reported by the cohort (e.g., eye irritation, nose irritation, rhinorrhoea, and general malaise) as measured by a questionnaire. | Throughout the bloom (June–October 2013), 81% of the human cohort experienced at least one Ostreopsis-related symptom. Symptoms lasted no longer than 3–4 days. The health effects were greatest in early August when the bloom transitioned from the exponential growth phase to the stationary phase. Negligible symptoms were reported from August to mid-October, which is the stationary period with persistently high cell concentrations. The O. cf. ovata epiphytic and planktonic cell populations exhibited similar patterns, with a peak in early August, then a stationary period from August to mid-October, and then a decrease. |
| Berdalet 2022 | Sant Andreu de Llavaneres, Catalonia, Spain | Same sampling methods as Vila et al., 2016. Samples were taken once or twice per week in July and August, twice per month in June, September and October, and monthly in November and December. Additional samples were collected when necessary in the fall. |
Restaurant staff and the nearby residents were invited to participate in epidemiological surveys. Between 5 and 29 surveys were answered each year. |
Ostreopsis-related symptoms reported by the cohort grouped by organ systems (general, otorhinolaryngologic, ophthalmologic; digestive; respiratory; dermatologic; and cardiac) as measured by a daily questionnaire. | Over the 6 years, the prevalence rate of the symptoms varied over time – between 3.1% and 13.1% for malaise, 2.6% and 45.9% for runny nose, 2.3% and 9.7% for sore eyes, 0%–13.6% for headaches, and 0%–45.9% for nose irritation. Temporal patterns of reported health symptoms were observed, with highest rates coinciding with the early stationary phase of the blooms. |
| Chomeret 2022 | Several beaches on the French Basque coast | Water samples and macroalgae samples were taken at beaches with reported cases. Observation and counts of cells were done by light microscopy and by fluorescence. Species were isolated and identified via sequencing and phylogenetic analysis. Toxins were screened for the presence of toxins (PLTX and related analogues) using LC-MS/MS analysis. |
About 10 cases of respiratory symptoms in September 2020 were first reported by swimmers and beach visitors. In 2021, following an unusual outbreak of Ostreopsis in some of the beaches, 674 confirmed cases were reported. |
Beach users reported various respiratory and cutaneous symptoms (e.g., difficulty breathing, irritations, headaches, dry cough, nose irritation, eye irritation and/or dermatitis, and general malaise) after direct contact with water and/or after inhalation of aerosols. | The symptoms disappeared within 2 days without a need to medicate when people moved away from the area concerned by the Ostreopsis bloom. Detection of presence of both O. cf. siamensis and O. cf. ovata, establishing the French Basque coast as a new Northern distribution limit. The presence of ovatoxins in the collected and cultivated samples confirmed toxicity and identified O. cf. ovata as the producer. |
Table 3.
Summaries of studies on cyanobacteria aerosols and health (n = 8).
| Author | Location | Exposure assessment method | Population and study period | Measured outcome | Findings summary |
|---|---|---|---|---|---|
| Stewart 2006a | Southern Queensland and the Myall Lakes area of New South Wales, Australia; Northeast and central Florida, USA | Water samples for phytoplankton and cyanotoxin analysis were collected by a modified grab sample method. Faecal coliforms were also sampled. Total phytoplankton analyses, cell identification and enumeration, and analyses for various cyanotoxins were conducted. Cyanobacterial cell surface area was used as the main exposure variable of interest. |
1331 study participants (n = 216 in Florida) comprised of adults and children engaging in recreational activities in enclosed waters (e.g., not marine waters) with cyanobacteria. | Reported symptoms were categorized as ear, eye, gastrointestinal, respiratory (difficulty breathing; dry cough; productive cough; runny nose; unusual sneezing; sore throat; wheezy breathing), cutaneous, fever, and the combined “any symptom” (any of the above). Symptoms were rated none, mild, and moderate/severe. | Respiratory symptoms were 2.1 (95% CI: 1.1–4.0) times more likely to be reported by subjects in the high-exposure group than the low-exposure group. Any symptoms were 1.7 (95%CI: 1.0–2.8) times more likely to be reported by subjects in the high-exposure group than the low-exposure group. Most reported respiratory symptoms were in the ‘mild’ category. |
| Backer 2008 | Unspecified lakes, USA | Air and water samples were taken and cell densities and microcystin concentrations were measured. Microcystin concentration levels in blood samples were also measured via ELISA. |
97 participants recruited from a lake with an ongoing Microcystis aeruginosa bloom, and another 7 from a nearby bloom-free lake for 3 days in August of 2006. Demographic information and symptoms were measured. | Respiratory (sore throat; congestion; cough; throat irritation; eye irritation; other), dermatologic (itchy skin, red skin, hives, skin irritation, rash, other); other (earache, agitation, headache, abdominal pain, diarrhoea) symptoms 7 days before study, before study activities, after study activities, and 7–10 days after study activities were recorded. | Low levels of microcystin were detected in both water and aerosol samples. No significant differences appeared in the symptom frequency between the exposed and control groups 1 week before, immediately before/after recreational activities, and after the study period. Results are somewhat suggestive that symptoms may occur a few days after initial exposure to microcystin aerosols. |
| Backer 2010 | Two lakes in Siskiyou County, California, USA | Air and water samples were taken and cell densities and microcystin concentrations were measured | August 2007 | Respiratory (sore throat; congestion; cough; throat irritation; eye irritation; other), dermatologic (itchy skin, red skin, hives, skin irritation, rash, other); other (earache, agitation, headache, abdominal pain, diarrhea) symptoms 7 days before study, before study activities, after study activities, and 7–10 days after study activities | No significant changes in symptoms were observed after exposure. |
| Hilborn 2014 | US States participating in the CDC surveillance system (Florida, Iowa, Maryland, Massachusetts, New York, Oregon, South Carolina, Virginia, Washington, and Wisconsin). | Human health data and water sampling results voluntarily reported to CDC's Waterborne Disease and Outbreak Surveillance System (WBDOSS) via the National Outbreak Reporting System (NORS) and the Harmful Algal Bloom-Related Illness Surveillance System (HABISS) for 2009–2010. | During 2009–2010 in the United States, 11 outbreaks (3 in NY; 6 in OH; 2 in WA) associated with recreational activities at freshwater lakes that affected at least 61 persons. 8 outbreak investigations included the evaluation of cyanotoxins, with 4 evaluating multiple cyanotoxins; 3 identified cyanobacteria, while 2 identified potentially toxic cyanobacteria without quantification. |
Gastrointestinal, general, dermatologic, eye/ear, neurologic, respiratory symptoms | Out of 58 persons with available data, seven (12%) visited an emergency department and 34 (59%) visited a health-care provider. 66% of persons were aged ≤19 years, suggesting that children might be at higher risk for HAB-related health effects. |
| Levesque 2014 | Quebec province, Canada | Daily surface water samples and cyanobacterial cells were counted and identified. Dissolved microcystin was measured in filtered water samples. |
267 families consisting of 466 subjects living near three lakes filled out questionnaires and journals of daily symptoms and contact (full or limited contact, location, and duration) with water | Eye, ear, respiratory, gastrointestinal, skin, muscle pain, headaches, mouth ulcers | Only gastrointestinal symptoms were significantly associated with recreational contact with lakes and higher cyanobacteria concentrations |
| Figgatt 2017 | New York state, USA | New York State Department of Environmental Conservation (NYSDEC) evaluated bodies of water for HABs in response to reports of possible HABs from the public, staff, and lake associations. HABs were confirmed by laboratory tests. Public health workers received training and surveillance tools, which included outreach material to public to encourage reporting suspected exposures. When an HAB was identified, other surveillance activities were conducted, such as monitoring of hospital data; providing education material to healthcare providers and veterinarians; and coordination with poison control centres. |
16 (out of 62) New York counties were selected for participation in the pilot surveillance system based on interest and likelihood of HABs. During June to September 2015, HAB-associated human and animal illnesses reported by local health departments (LHD) were collected. |
Each HAB illness report was investigated using a questionnaire given by either the LHD or NYSDOH and assessed using the CDC case definitions. Case definitions take into consideration information such as environmental/visual evidence of an HAB; confirmation via toxin-detecting test strips or laboratory confirmation; and clinical evidence of HAB exposure. |
In this pilot cyanobacteria HAB-associated illness surveillance system in 16 counties, 51 human and canine HAB-associated illnesses were reported, including 32 human and 3 canine cases that met the CDC case definition. The pilot surveillance during a 4-month period suggest that HAB-associated illnesses might be more common than previously reported. Commonly reported symptoms included: skin problems; respiratory; gastrointestinal; other symptoms (e.g., chills, muscle aches, watery eyes); fatigue/general weakness; and sore throat. |
| Wu 2021 | Greater Boston area, Massachusetts, USA | Satellite-derived cyanobacteria cell concentrations were estimated in the source of drinking water for the Greater Boston area. 300-m resolution imageries from the MEdium Resolution Imaging Spectrometer (MERIS) were processed. |
Patients who visited the emergency rooms of approximately 70 Massachusetts hospitals for gastrointestinal, respiratory, and dermal illnesses during 2008–2011. | Daily counts of hospital emergency room visit for gastrointestinal (ICD-9: 001–009.9, 558.9, 787.91, 787.01, and 787.03); respiratory (460, 461, 465.9, 493, 786.2, 786.05, and 786.07); and dermal illnesses (782.1, 136.9, 686.9, 692, and 691.8) from approximately 70 Massachusetts hospitals. | Time-series models adjusting for confounding effects (day of the week, ambient ozone concentration, average mean ambient temperature, school days, and holidays) showed that there were no significant associations between cyanobacteria concentrations and daily visits for gastrointestinal illness. There was a significant positive association between satellite-derived cyanobacteria abundance and visits for respiratory illnesses at the 2-day lag. Associations at all other lags were not significant. Visits for dermal illnesses were not significantly associated with the level of cyanobacteria concentrations. |
| Lee 2022 | South Korea | Chlorophyll-a (chl-a) concentrations during HAB seasons in 2005–2017 obtained from 939 locations, from a Korean governmental agency conducting monitoring of cyanobacterial cell counts, geosmin, and chl-a concentrations during HAB seasons. Annual average chl-a concentrations, as a proxy for blooms, per location were used for analysis. A secondary pilot study was conducted to sample and confirm the presence of microcystins and BMAA in water and air samples downstream of a large river (Nakdong River). |
Annual number of neurodegenerative diseases (NDs) between 2005 and 2017. | Three neurodegenerative disease outcomes including motor neuron disease (ICD-10 code G12.2), Alzheimer's disease (G30.0), and Parkinson's disease (G20). | The increase in the chl-a concentrations showed significantly positive correlations with the same-year annual incidence rate of motor neuron disease, Alzheimer's disease, and Parkinson's disease, separately. For Parkinson's disease, a positive correlation was found for the HAB measures with lags of 1, 2, and 3 years. For motor neuron disease and Alzheimer's disease, a positive correlation was found for the HAB measures for the previous year. |
Table 4.
Summaries of studies on non-specified HAB aerosols and health (n = 3).
| Author and year | Location | Exposure assessment method | Population and study period | Measured outcome | Findings summary |
|---|---|---|---|---|---|
| Lavery 2021a | USA | ICD-9 and ICD-10 codes for HAB exposure | IBM MarketScan Research Databases, which contain de-identified healthcare claims data for individuals with commercial insurance and some Medicaid beneficiaries. Databases between January 2009 and April 2019 |
ICD-9 and ICD-10 health diagnostic codes that were associated with HAB exposure. Most frequent outcomes included cough, allergy, other malaise and fatigue, headache, routine general medical examination, shortness of breath, hypertension, acute pharyngitis, and acute upper respiratory infection. |
380 records in the Commercial database and 178 records in the Medicaid database were identified. The most common ICD health code was for respiratory events. A large peak in HAB exposure code and respiratory events coincided with red tide event in the Gulf of Mexico High counts of respiratory events were also seen in East North Central region consisting of states by the Great Lakes, potentially coinciding with cyanobacterial HABs. Few records for neurological events such as headaches and dizziness (11.8%); eye or skin irritation (10.9%); or gastrointestinal events (5.7%). |
| Lavery 2021b | USA | ICD-9 and ICD-10 codes for HAB exposure; chief complaint text | National Syndromic Surveillance Program (NSSP) for HAB exposure–associated administrative discharge diagnosis codes and chief complaint text terms related to HAB exposure January 1, 2017–December 31, 2019. |
Emergency department visits associated with HAB exposure | n = 321 harmful algal bloom–associated ED visits were identified, with ED visits increasing in summers. Among these visits, 106 (33%) were identified through ICD-10 codes only; the addition of chief complaint text key terms to the query identified an additional 215 (67%) visits. Primary syndrome categories among the ED visits were respiratory (41.4%); gastrointestinal (13.7%); neurologic (10.3%); and dermatologic (8.4%). |
| Roberts 2020 | 18 states in USA that adapted the One Health Harmful Algal Bloom System (OHHABS) | Data reported to OHHABS included 421 HAB events. HAB events reported to CDC are classified based on standard definitions:
|
A total of 389 human cases of illness, with 341 (88%) classified as probable, and at least 413 animal illnesses were reported between 2016 and 2018. | Reported symptoms (e.g., gastrointestinal, generalized, dermatologic, neurologic) were recorded, as well as time to onset for a subset of cases. | Data reported to OHHABS by 18 states for 2016–2018 included 421 harmful algal bloom events, 389 cases of human illness, and 413 cases of animal illness. Laboratory testing for 372 (88%) HAB events was performed. Toxin texts were done for 308 reports of HAB events (83%), which frequently identified microcystins (94%), followed by anatoxin-a (10%) and saxitoxin (6%). 11% identified multiple toxins. The majority of HAB events occurred during May–October (98%), peaking in July (27%). The majority (89%) of the exposures involved fresh water. Most of HAB events were classified as confirmed (88%), while the majority of human illnesses were classified as probable (87%), and animal illnesses as suspected (81%). Most frequent symptoms were (67%); generalized (43%); dermatologic (27%); or ear, nose, or throat-related (16%) symptoms. Time to onset of initial signs or symptoms was available for 124 persons who had a one-time exposure and ranged from 1 min to 8 days. No mortality cases were reported. |
Karenia brevis
Among the marine HAB species, health effects associated with aerosolized K. brevis toxins are perhaps the most well-characterized. K. brevis is a dinoflagellate native to the waters of the Gulf of Mexico and the Caribbean and close relatives have been detected in Europe, Australia, and Japan.42 K. brevis blooms, known as “red tide,” are frequently observed on coastlines and beaches during the late summer and fall. These species produce brevetoxin, which is a neurotoxin that activates sodium channels and releases acetylcholine and other neurotransmitters from autonomic nerve endings, thereby producing lower airway smooth muscle contraction (Pierce).60
Past studies in Florida during K. brevis blooms have demonstrated that aerosolized brevetoxins can induce respiratory symptoms including cough, bronchoconstriction, and shortness of breath, with symptoms occurring as soon as 1 h after exposure. Recreational beachgoers (n = 129) were measured before and after a visit to the beach, and exposure to high levels of brevetoxin aerosols was associated with observed increases in upper and lower respiratory tract symptoms; some inflammatory responses were also seen.34 In follow-up work, healthy lifeguards (n = 28) were measured before and after their work shift, with observed changes in their self-reported respiratory symptoms, including nasal congestion, throat irritation, and coughing (Backer).61 Neither study reported significant changes in pulmonary function among the study participants. A series of panel studies in Florida further examined whether exposures to brevetoxin-containing aerosols especially impact asthmatics. After 1 h of aerosolized brevetoxin exposure at the beach with symptom data and spirometry data collected before and after, a significant increase in self-reported respiratory symptoms and a decrease in pulmonary function were observed.62, 63, 64, 65 In a follow-up study of 52 asthmatics, there were no significant changes in symptoms or pulmonary function either acutely or over 5 days of follow-up during non-exposure periods.66 After the beach exposure during an active Florida red tide, asthmatics continued to experience increased symptoms and respiratory function suppression for several days. Linear dose–response relationships between estimated exposure to aerosolized K. brevis and both upper respiratory tract and neurological outcomes were also observed among southwest Florida residents (n = 258).67 Counts and intensity of respiratory outcomes, namely cough and sneezes, were used to create a respiratory irritation index. This index generally coincided with the size and intensity of blooms, which in turn was measured by an index on bloom severity based on detailed spatiotemporal data on K. brevis cell counts.68 These studies suggest that upper respiratory symptoms are reported even in healthy populations at high enough cell counts, and asthmatics may be at heightened risk.
A single work examined the potential long-term health effects of K. brevis aerosol exposure. Respiratory health effects of repeated exposure to aerosolized brevetoxins were assessed in a cohort of asthmatics (n = 125) over 7 years, with at least one evaluation each conducted during a K. brevis bloom period as well as during a non-bloom period.69 Assessments of pulmonary function and respiratory symptoms were conducted before and after 1 h of brevetoxin exposure at the beach. In a subgroup of participants (n = 36) that participated in at least 4 exposure evaluations, initial exposure to K. brevis was not significantly associated with subsequent pre-exposure measures of standardized percent predicted pulmonary function. The findings suggest that for asthmatics with controlled asthma, living in areas with K. brevis blooms does not have a potential long-term respiratory effect from intermittent exposure to aerosolized brevetoxins. However, certain subpopulations (less controlled asthmatics and those who lived inland) appeared to show longitudinal changes in pulmonary function.
Multiple studies have utilized hospital records to study the association between K. brevis and health outcomes. Increased emergency room admissions for respiratory diseases (pneumonia, bronchitis, and asthma) were observed during active Florida red tides, particularly for coastal residents.70 The number of respiratory-specific ED diagnoses between 2001 and 2006 in Sarasota, Florida was associated with K. brevis cell counts in nearby oceans in the previous week, after adjusting for temperatures, influenza outbreaks, high pollen counts, and tourist visits.71 This study design incorporating a 1-week lag accounted for the hypothesized route and timing of exposure by considering the delay between HAB occurrence, the release of toxins from the water after cell lysis, aerosolization, and finally inhalation. In a study across six southwest coastal counties in Florida, K. brevis blooms were associated with increases in the number of emergency department visits and hospital inpatient admissions for both respiratory and digestive illnesses among those aged 55 or older.72 Increased visits to hospital emergency departments due to headaches73 and gastrointestinal illness74 during K. brevis blooms have also been reported previously, with inhalation hypothesized as one of the possible routes of exposure.
Ostreopsis sp.
Ostreopsis species Ostreopsis ovata and Ostreopsis siamensis in the Mediterranean produce ovatoxins, which are similar to palytoxins (PTX), one of the most potent marine toxins that act as vasoconstrictors.75 Multiple events of respiratory symptoms and dermal irritation on beaches after exposure to sea spray during microalgal blooms of Ostreopsis have been reported. Respiratory symptoms were first reported in August 2003 and September 2004 in Bari, Italy, where people exposed to aerosols (n = 28) via recreational activities on the beach or work reported rhinorrhea, cough, fever, and bronchoconstriction with mild dyspnea and wheezes.76 Another event in August 2004 near Barcelona, Spain similarly resulted in respiratory symptoms and headaches among those who were exposed (n = 62).77 In 2005, respiratory symptoms and fever were observed in (n = 209) people who inhaled Ostreoposis aerosols in Genoa, Italy.78,79 In Algeria, more than three hundred cases of human respiratory symptoms were reported across several beaches, with fever, rhinitis, conjunctivitis, cough, and skin irritations as the most common clinical symptoms observed.80 In these events, most of the symptoms disappeared within a few hours without specific medication when people moved away from the affected area, although some required hospitalization. A surveillance study described 9 blooms across the French Mediterranean coast between 2006 and 2009, including 5 blooms where patients (n = 47) reported mild respiratory, skin, and mucosal irritations.81 During summer blooms of unidentified Ostreopsis species on the French Basque coast in 2020 and 2021, people (n = 674) reported irritations and respiratory symptoms after direct contact with water and/or inhalation of marine aerosols. Sampling was carried out and the presence of ovatoxins was confirmed in the collected samples. Ostreoposis was first reported in this region, suggesting an expansion of the geographic extent of Ostreopsis blooms and associated impacts.82 In a cohort of restaurant workers (n = 16) working nearby an Ostreopsis bloom in Catalonia, Spain, with prolonged exposures to blooms (e.g., at least 8 h daily from June to October), 81% reported at least one symptom, with symptoms usually not lasting more than 3–4 days.83 In a follow-up study at the same location with additional participants and years of surveys, reports of respiratory symptoms, along with other range of symptoms (e.g., digestive to dermatologic outcomes), were observed.84 Temporal trends in the number of symptoms reported were observed in these two works, with the highest health outcomes observed between the exponential phase and early stationary phase of the blooms. Studies on Ostreopsis aerosols and associated health outcomes have been primarily limited to case reports describing symptoms with limited exposure assessment methods.
Cyanobacteria
Cyanobacteria are oxygen-producing bacteria that obtain energy via photosynthesis and convert carbon dioxide into biomass; notable genera include Cylindrospermopsis, Microcystis, and Dolichospermum.5 Under certain environmental conditions, they can form very dense blooms in aquatic environments and dominate the phytoplankton populations.85 Cyanobacterial blooms can cause major water quality issues, increase turbidity, and deplete oxygen, which can lead to hypoxic and anoxic conditions that can cause the deaths of aquatic life.86 Cyanobacteria produce a variety of bioactive compounds and cyanotoxins that adversely affect human and animal health. Hepatotoxins, such as microcystins (MC) and nodularin, and neurotoxins, such as anatoxin-a, anatoxin-a(s), and β-N-methylamino-L-alanine (BMAA) are globally the most prevalent cyanotoxins.87 Exposure to MC is linked with inflammation in airway epithelial cells.88 Cyanobacteria HABs (cyanoHABs) are expanding globally in duration, frequency, and extent across freshwater, estuarine, and marine ecosystems,86 posing a rising threat to public health.
The evidence regarding the association between cyanoHABs and health is limited and mixed to date. A prospective cohort study (n = 1331) across Queensland and New South Wales, Australia, and Florida, U.S found that low-severity respiratory symptoms were significantly higher to be reported among subjects exposed to high levels of total cyanobacteria compared to low exposures during recreational activities (Stewart)89; other symptoms (ear, eye, gastrointestinal, dermal, fever) were not elevated. Cyanobacterial cell surface area from collected water samples was used as the main exposure variable of interest. Recreational activities at lakes and exposure to microcystins during cyanoHAB events were not associated with symptoms.35,36 Among residents living near three lakes in Canada with cyanoHABs, mild respiratory symptoms were reported but no significant associations with contact with water bodies were found.90 A recent study estimated potential exposures to cyanobacteria cell concentrations using remote sensing data in the Greater Boston area, Massachusetts, and found significant associations between cyanobacteria and increased cases of respiratory illness-related emergency room visits, but not with gastrointestinal or dermal symptoms.91 State- and national-level surveillance systems have been recently leveraged to track cyanoHABs and associated health impacts,92,93 with findings suggesting that the population-level health impacts of HABs have been underestimated previously. Multiple cyanotoxins were detected in several of the HAB outbreaks.
There is also some evidence suggestive of an association between cyanoHAB aerosols and neurological outcomes.54 Chlorophyll-a levels along lakes and rivers, used as a proxy for cyanoHABs, were positively associated with annual incidence rates of neurodegenerative diseases in South Korea.94 As a secondary analysis, the study authors also conducted a pilot sampling study at a large river and found cyanotoxins in both water and air samples, implicating inhalation as one of the potential pathways of exposure. Chronic exposure to the cyanotoxin BMAA has been linked as a significant risk factor for developing amyotrophic lateral sclerosis (ALS), with the hypothesis that aerosolization may play a significant role.95,96
Unspecified/other
Here we summarize the studies that did not specify the HAB genera. An analysis of a US health claims dataset from commercial insurance and Medicaid identified records (n = 558) that used the ICD-9/10 codes for HAB exposure.97 Respiratory illness was the most commonly reported among these records using HAB exposure codes, and these events tended to coincide with major HAB events, such as occurrences of red tides in the Gulf of Mexico region. The same authors also analysed emergency department visit data from the CDC National Syndromic Surveillance Program for HAB exposure-related diagnosis codes and chief complaint text terms, identifying n = 321 HAB-associated ED visits. HAB exposures were documented infrequently with diagnosis codes, and 67% of the visits were identified through querying chief complaint text.98 These two reports suggest that using only ICD codes for exposure may be limited in capturing the full extent of health outcomes, but also highlight the potential of national-level health datasets for monitoring of HABs. CDC One Health Harmful Algal Bloom System (OHHABS) was launched in 2016 as a surveillance system to inform efforts to prevent human and animal illnesses associated with harmful algal bloom events.99 Between 2016 and 2018, 18 states reported 421 HAB events and 389 cases of human illness, and 413 cases of animal illness. Gastrointestinal or generalized illness signs were the most frequently reported, but other symptoms, including respiratory, were also common.
Conclusions
Overall, we found that the number of studies linking HAB aerosols and health outcomes, mainly respiratory symptoms along with some evidence of neurological and gastrointestinal outcomes, is growing, but the strength of current evidence remains hampered by limited exposure assessment methods and a lack of robust epidemiological study designs. Evidence suggests that large segments of the population could be at risk for acute and chronic exposures as aerosolized toxins have been detected tens of kilometres away from the source. Health effects could be observed at low doses in some works. The disease burden associated with exposure to HABs is likely to be underestimated and underexamined as suggested by recent analyses of syndromic surveillance data and national-level electronic health databases. The increasing proliferation of HABs resulting from climate change and eutrophication across many locations around the world could result in a corresponding rise in aerosolized toxins and adverse health impacts. Growing populations and tourism near bodies of water and coasts will further increase the number of people at risk. Despite the potential risk to public health, there are no inhalation standards for HABs from the World Health Organization, Center for Disease Control, or the U.S. Environmental Protection Agency. Additional studies addressing the identified knowledge gaps are needed to provide the evidence needed for informing policy standards that can better protect populations under a changing climate.
Outstanding questions
Studies that examined mechanisms of aerosolization, as well as the health effects of HAB aerosols, were limited in terms of genera and geography, with prior works restricted to K. brevis in Florida, US, Ostreopsis sp. on Mediterranean coasts, and cyanobacteria. Most studies utilized limited exposure assessment methods and lacked direct measurement of aerosol concentrations and composition, instead utilizing proxy metrics such as HAB cell counts in nearby bodies of water. However, water cell abundance and toxin concentrations are not consistently correlated with aerosol toxin concentration levels,100 which are highly variable and dependent on a host of other factors, such as the phase of the bloom, temperature, wind, and nutrients. In addition, these studies focused on one type of HAB and toxin at a given time, although aerosols contain multiple toxins, each with concentration levels that are highly variable over space and time.27 Potentially synergistic effects of concurrent exposure to multiple toxins and other components in the aerosols (e.g., microplastics and heavy metals), along with gaseous pollutants (e.g., hydrogen sulphide) that could be emitted with decaying biomass,101 remain unexplored. Multiple routes of exposure are also often involved, but their respective contributions to observed adverse health outcomes are also unclear. Findings from many animal studies further suggest that toxic effects from exposure to aerosolized toxins could occur at lower doses than that for ingestion,28 but there is minimal evidence on the threshold doses and dose–response relationships. Deploying more robust aerosol sampling protocols, developing biomarkers for exposure, and employing multiple exposure assessment approaches simultaneously could help to address these knowledge gaps. In terms of study design, most works were either case reports or anecdotal evidence that examined acute exposure during recreational activities, and epidemiological analyses were very limited. Studies examining long-term exposures and health effects are especially lacking despite the potential for prolonged exposure for populations living nearby waterbodies. Furthermore, investigations primarily relied on self-reported activities and symptoms, which may be subject to potential bias. As symptoms of exposure are often generic and nonspecific, HAB-associated health impacts are also likely to be underestimated. Although a few of the prior studies examined asthmatics as a potentially vulnerable population, evidence on other potential risk factors such as age, socioeconomic factors, and other chronic diseases is significantly lacking. Finally, the impacts of climate change on HAB toxin generation and patterns of exposure remain unclear. Additional studies leveraging large cohorts and health datasets with information on individual-level risk factors, in conjunction with the application of multifaceted exposure assessment methods, are needed for assessing population-level disease burdens and disparities associated with HAB exposures.
Search selection and strategy.
We searched PubMed and Google Scholar for papers published before December 31st, 2022, for research articles related to HABs and health using the search terms (“harmful algal blooms” OR “HAB” OR “HABs” OR “cyanobacteria” OR “red tide” OR “Karenina” OR “Ostreopsis”) AND (“particles” OR “particulate matter” OR “aerosols” OR “aerosolization” OR “inhalation” OR “exposure”) AND (“health” OR “human health” OR “surveillance” OR “hospitalization” OR “emergency” OR “respiratory” OR “asthma” OR “gastrointestinal” OR “neurological”) in English. Our team reviewed the title and abstracts for inclusion. We also reviewed the reference lists of eligible texts to find additional papers (Fig. 2).
Fig. 2.
Flow diagram for inclusion of studies in the review (n = 34).
Contributors
C.C.L.-conceptualization, investigation, writing-original draft. J.Y.-investigation, resources, writing - review & editing. K.R.-investigation, writing - review & editing. L.B.G.-methodology, writing - review & editing. A.P.A.-investigation, writing- original draft. S.H.- methodology, writing - review & editing. M.L.B.-methodology, writing - original draft. All authors have read and approved the final version.
Data sharing statement
Not applicable.
Declaration of interests
C.C.L.-grants from the Robert Wood Johnson Foundation (RWJF) and the University of Arizona Health Sciences. J.Y., S.H. and K.R. have no declarations of interest. LBG-grants from the National Institutes of Health (NIH); American Lung Association; Southern California National Institute for Occupational Safety & Health Education Center; Centers for Disease Control and Prevention; royalties or licenses from Up-to-Date and Wolters Kluwer; consulting fees Nemours Foundation; leadership or fiduciary role in American Lung Association of Arizona (unpaid) and Arizona Asthma Coalition (unpaid); receipt of equipment, materials, drugs, medical writing, gifts, or other services from Thayer Medical Corporation. A.P.A.-grants from the National Science Foundation (NSF), National Oceanic and Atmospheric Administration (NOAA), NIH, and Sloan Foundation; patents pending on instrument for determining aerosol acidity. M.L.B.-grants from the U.S. Environmental Protection Agency (EPA), NIH, High Tide Foundation, Yale Climate Change and Health Center, RWJF, Environmental Defense Fund, Health Effects Institute, Wellcome Trust; consulting fees from EPA and Clinique; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Boston University, Korea University, Organization of Teratology Information Specialists, University of Pennsylvania, Duke University, University of Texas, Data4Justice, NIH, Health Canada, PAC-10, UKRI, AXA Research Fund Fellowship, Harvard University, University of Montana, IOP Publishing; support for attending meetings and/or travel from Boston University, Harvard University, University of Illinois at Champaign, University of Texas, EPA, UPenn; participation on a data safety monitoring board or advisory board from US EPA Clean Air Scientific Advisory Board, National Academies Panels and Committees, Member of Lancet Countdown, Fifth National Climate Assessment NCAS, Johns Hopkins University, World Health Organization Global Air Pollution and Health Technical Advisory Group.
Acknowledgements
This research was supported by the University of Arizona Health Sciences Career Development Award. Research reported in this publication was also supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD012769. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders did not have any role in the paper design, data collection, data analysis, interpretation, or writing of the paper.
References
- 1.Anderson D.M., Fensin E., Gobler C.J., et al. Marine harmful algal blooms (HABs) in the United States: history, current status and future trends. Harmful Algae. 2021;102 doi: 10.1016/j.hal.2021.101975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gobler C.J., Doherty O.M., Hattenrath-Lehmann T.K., Griffith A.W., Kang Y., Litaker R.W. Ocean warming since 1982 has expanded the niche of toxic algal blooms in the North Atlantic and North Pacific oceans. Proc Natl Acad Sci U S A. 2017;114(19):4975–4980. doi: 10.1073/pnas.1619575114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wells M.L., Karlson B., Wulff A., et al. Future HAB science: directions and challenges in a changing climate. Harmful Algae. 2020;91 doi: 10.1016/j.hal.2019.101632. [DOI] [PubMed] [Google Scholar]
- 4.Griffith A.W., Gobler C.J. Harmful algal blooms: a climate change co-stressor in marine and freshwater ecosystems. Harmful Algae. 2020;91 doi: 10.1016/j.hal.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 5.O'Neil J.M., Davis T.W., Burford M.A., Gobler C.J. The rise of harmful cyanobacteria blooms: the potential roles of eutrophication and climate change. Harmful Algae. 2012;14:313–334. [Google Scholar]
- 6.Glibert P.M., Burford M.A. Globally changing nutrient loads and harmful algal blooms: recent advances, new paradigms, and continuing challenges. Oceanography. 2017;30(1):58–69. [Google Scholar]
- 7.Adams C.M., Larkin S.L., Hoagland P., Sancewich B. Harmful algal blooms: a compendium desk reference. 2018. Assessing the economic consequences of harmful algal blooms: a summary of existing literature, research methods, data, and information gaps; pp. 337–354. [Google Scholar]
- 8.Young N., Sharpe R.A., Barciela R., et al. Marine harmful algal blooms and human health: a systematic scoping review. Harmful Algae. 2020;98 doi: 10.1016/j.hal.2020.101901. [DOI] [PubMed] [Google Scholar]
- 9.Walsh J.J., Lenes J.M., Weisberg R.H., et al. More surprises in the global greenhouse: human health impacts from recent toxic marine aerosol formations, due to centennial alterations of world-wide coastal food webs. Mar Pollut Bull. 2017;116(1-2):9–40. doi: 10.1016/j.marpolbul.2016.12.053. [DOI] [PubMed] [Google Scholar]
- 10.Limaye V.S., Max W., Constible J., Knowlton K. Estimating the health-related costs of 10 climate-sensitive US events during 2012. Geohealth. 2019;3(9):245–265. doi: 10.1029/2019GH000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fleming L.E., Kirkpatrick B., Backer L.C., et al. Review of Florida red tide and human health effects. Harmful Algae. 2011;10(2):224–233. doi: 10.1016/j.hal.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel S.S., Lovko V.J., Lockey R.F. Red tide: overview and clinical manifestations. J Allergy Clin Immunol Pract. 2020;8(4):1219–1223. doi: 10.1016/j.jaip.2019.10.030. [DOI] [PubMed] [Google Scholar]
- 13.Lewis E.R., Schwartz S.E. American Geophysical Union; 2004. Sea salt aerosol production: mechanisms, methods, measurements, and models. [Google Scholar]
- 14.De Leeuw G., Andreas E.L., Anguelova M.D., et al. Production flux of sea spray aerosol. Rev Geophys. 2011;49(2) [Google Scholar]
- 15.May N.W., Olson N.E., Panas M., et al. Aerosol emissions from great lakes harmful algal blooms. Environ Sci Technol. 2018;52(2):397–405. doi: 10.1021/acs.est.7b03609. [DOI] [PubMed] [Google Scholar]
- 16.Axson J.L., May N.W., Colon-Bernal I.D., Pratt K.A., Ault A.P. Lake spray aerosol: a chemical signature from individual ambient particles. Environ Sci Technol. 2016;50(18):9835–9845. doi: 10.1021/acs.est.6b01661. [DOI] [PubMed] [Google Scholar]
- 17.Plaas H.E., Paerl R.W., Baumann K., et al. Harmful cyanobacterial aerosolization dynamics in the airshed of a eutrophic estuary. Sci Total Environ. 2022;852 doi: 10.1016/j.scitotenv.2022.158383. [DOI] [PubMed] [Google Scholar]
- 18.Ault A.P., Zhao D., Ebben C.J., et al. Raman microspectroscopy and vibrational sum frequency generation spectroscopy as probes of the bulk and surface compositions of size-resolved sea spray aerosol particles. Phys Chem Chem Phys. 2013;15(17):6206–6214. doi: 10.1039/c3cp43899f. [DOI] [PubMed] [Google Scholar]
- 19.Ault A.P., Moffet R.C., Baltrusaitis J., et al. Size-dependent changes in sea spray aerosol composition and properties with different seawater conditions. Environ Sci Technol. 2013;47(11):5603–5612. doi: 10.1021/es400416g. [DOI] [PubMed] [Google Scholar]
- 20.Patterson J.P., Collins D.B., Michaud J.M., et al. Sea spray aerosol structure and composition using cryogenic transmission electron microscopy. ACS Cent Sci. 2016;2(1):40–47. doi: 10.1021/acscentsci.5b00344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cartmill J.W., Su M.Y. Bubble size distribution under saltwater and freshwater breaking waves. Dynam Atmos Oceans. 1993;20(1-2):25–31. [Google Scholar]
- 22.May N.W., Axson J.L., Watson A., Pratt K.A., Ault A.P. Lake spray aerosol generation: a method for producing representative particles from freshwater wave breaking. Atmos Meas Tech. 2016;9(9):4311–4325. [Google Scholar]
- 23.Plaas H.E., Paerl H.W. Toxic cyanobacteria: a growing threat to water and air quality. Environ Sci Technol. 2020;55(1):44–64. doi: 10.1021/acs.est.0c06653. [DOI] [PubMed] [Google Scholar]
- 24.Pierce R.H., Henry M.S., Blum P.C., et al. Brevetoxin composition in water and marine aerosol along a Florida beach: assessing potential human exposure to marine biotoxins. Harmful Algae. 2005;4(6):965–972. [Google Scholar]
- 25.Van Acker E., Huysman S., De Rijcke M., et al. Phycotoxin-enriched sea spray aerosols: methods, mechanisms, and human exposure. Environ Sci Technol. 2021;55(9):6184–6196. doi: 10.1021/acs.est.1c00995. [DOI] [PubMed] [Google Scholar]
- 26.Cheng Y.S., Zhou Y., Irvin C.M., et al. Characterization of marine aerosol for assessment of human exposure to brevetoxins. Environ Health Perspect. 2005;113(5):638–643. doi: 10.1289/ehp.7496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu S., Zhou X., Hu P., et al. Inhalable particle-bound marine biotoxins in a coastal atmosphere: concentration levels, influencing factors and health risks. J Hazard Mater. 2022;434 doi: 10.1016/j.jhazmat.2022.128925. [DOI] [PubMed] [Google Scholar]
- 28.Olson N.E., Cooke M.E., Shi J.H., Birbeck J.A., Westrick J.A., Ault A.P. Harmful algal bloom toxins in aerosol generated from inland lake water. Environ Sci Technol. 2020;54(8):4769–4780. doi: 10.1021/acs.est.9b07727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewandowska A.U., Śliwińska-Wilczewska S., Woźniczka D. Identification of cyanobacteria and microalgae in aerosols of various sizes in the air over the Southern Baltic Sea. Mar Pollut Bull. 2017;125(1-2):30–38. doi: 10.1016/j.marpolbul.2017.07.064. [DOI] [PubMed] [Google Scholar]
- 30.Bondy A.L., Wang B., Laskin A., et al. Inland sea spray aerosol transport and incomplete chloride depletion: varying degrees of reactive processing observed during SOAS. Environ Sci Technol. 2017;51(17):9533–9542. doi: 10.1021/acs.est.7b02085. [DOI] [PubMed] [Google Scholar]
- 31.May N.W., Gunsch M.J., Olson N.E., et al. Unexpected contributions of sea spray and lake spray aerosol to inland particulate matter. Environ Sci Technol Lett. 2018;5(7):405–412. [Google Scholar]
- 32.Chung S., Basarab B., VanReken T. Regional impacts of ultrafine particle emissions from the surface of the Great Lakes. Atmos Chem Phys. 2011;11(24):12601–12615. [Google Scholar]
- 33.Kirkpatrick B., Pierce R., Cheng Y.S., et al. Inland transport of aerosolized Florida red tide toxins. Harmful Algae. 2010;9(2):186–189. doi: 10.1016/j.hal.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Backer L.C., Fleming L.E., Rowan A., et al. Recreational exposure to aerosolized brevetoxins during Florida red tide events. Harmful Algae. 2003;2(1):19–28. [Google Scholar]
- 35.Backer L.C., Carmichael W., Kirkpatrick B., et al. Recreational exposure to low concentrations of microcystins during an algal bloom in a small lake. Mar Drugs. 2008;6(2):389–406. doi: 10.3390/md20080018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Backer L.C., McNeel S.V., Barber T., et al. Recreational exposure to microcystins during algal blooms in two California lakes. Toxicon. 2010;55(5):909–921. doi: 10.1016/j.toxicon.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Schaefer A.M., Yrastorza L., Stockley N., et al. Exposure to microcystin among coastal residents during a cyanobacteria bloom in Florida. Harmful Algae. 2020;92 doi: 10.1016/j.hal.2020.101769. [DOI] [PubMed] [Google Scholar]
- 38.Facciponte D.N., Bough M.W., Seidler D., et al. Identifying aerosolized cyanobacteria in the human respiratory tract: a proposed mechanism for cyanotoxin-associated diseases. Sci Total Environ. 2018;645:1003–1013. doi: 10.1016/j.scitotenv.2018.07.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pörtner H.-O., Roberts D.C., Masson-Delmotte V., et al. IPCC special report on the ocean and cryosphere in a changing climate. 2019. The ocean and cryosphere in a changing climate. 1155. [Google Scholar]
- 40.Brandenburg K.M., Velthuis M., Van de Waal D.B. Meta-analysis reveals enhanced growth of marine harmful algae from temperate regions with warming and elevated CO2 levels. Global Change Biol. 2019;25(8):2607–2618. doi: 10.1111/gcb.14678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coffey R., Paul M.J., Stamp J., Hamilton A., Johnson T. A review of water quality responses to air temperature and precipitation changes 2: nutrients, algal blooms, sediment, pathogens. J Am Water Resour Assoc. 2019;55(4):844–868. doi: 10.1111/1752-1688.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hallegraeff G.M., Anderson D.M., Belin C., et al. Perceived global increase in algal blooms is attributable to intensified monitoring and emerging bloom impacts. Commun Earth Environ. 2021;2(1):117. doi: 10.1038/s43247-021-00178-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zepernick B.N., Wilhelm S.W., Bullerjahn G.S., Paerl H.W. Climate change and the aquatic continuum: a cyanobacterial comeback story. Environ Microbiol Rep. 2023;15(1):3–12. doi: 10.1111/1758-2229.13122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Raven J.A., Gobler C.J., Hansen P.J. Dynamic CO2 and pH levels in coastal, estuarine, and inland waters: theoretical and observed effects on harmful algal blooms. Harmful Algae. 2020;91 doi: 10.1016/j.hal.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 45.Wells M.L., Trainer V.L., Smayda T.J., et al. Harmful algal blooms and climate change: learning from the past and present to forecast the future. Harmful Algae. 2015;49:68–93. doi: 10.1016/j.hal.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glibert P.M., Pitcher G.C., Bernard S., Li M. Global ecology and oceanography of harmful algal blooms. 2018. Advancements and continuing challenges of emerging technologies and tools for detecting harmful algal blooms, their antecedent conditions and toxins, and applications in predictive models; pp. 339–357. [Google Scholar]
- 47.Marple V.A., Rubow K.L., Behm S.M. A microorifice uniform deposit impactor (MOUDI): description, calibration, and use. Aerosol Sci Technol. 1991;14(4):434–446. [Google Scholar]
- 48.Hanlon R., Jacquemin S.J., Birbeck J.A., et al. Drone-based water sampling and characterization of three freshwater harmful algal blooms in the United States. Front Remote Sens. 2022;3:80. [Google Scholar]
- 49.Birbeck J.A., Westrick J.A., O'Neill G.M., Spies B., Szlag D.C. Comparative analysis of microcystin prevalence in Michigan lakes by online concentration LC/MS/MS and ELISA. Toxins. 2019;11(1):13. doi: 10.3390/toxins11010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Puddick J., Prinsep M.R., Wood S.A., Cary S.C., Hamilton D.P. Modulation of microcystin congener abundance following nitrogen depletion of a microcystis batch culture. Aquat Ecol. 2016;50:235–246. [Google Scholar]
- 51.Ortiz X., Korenkova E., Jobst K.J., MacPherson K.A., Reiner E.J. A high throughput targeted and non-targeted method for the analysis of microcystins and anatoxin-A using on-line solid phase extraction coupled to liquid chromatography–quadrupole time-of-flight high resolution mass spectrometry. Anal Bioanal Chem. 2017;409:4959–4969. doi: 10.1007/s00216-017-0437-0. [DOI] [PubMed] [Google Scholar]
- 52.Teta R., Della Sala G., Glukhov E., et al. Combined LC–MS/MS and molecular networking approach reveals new cyanotoxins from the 2014 cyanobacterial bloom in Green Lake, Seattle. Environ Sci Technol. 2015;49(24):14301–14310. doi: 10.1021/acs.est.5b04415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stroming S., Robertson M., Mabee B., Kuwayama Y., Schaeffer B. Quantifying the human health benefits of using satellite information to detect cyanobacterial harmful algal blooms and manage recreational advisories in US Lakes. Geohealth. 2020;4(9) doi: 10.1029/2020GH000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schaeffer B.A., Urquhart E., Coffer M., et al. Satellites quantify the spatial extent of cyanobacterial blooms across the United States at multiple scales. Ecol Indicat. 2022;140 doi: 10.1016/j.ecolind.2022.108990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhao Y., Liu D., Wei X. Monitoring cyanobacterial harmful algal blooms at high spatiotemporal resolution by fusing Landsat and MODIS imagery. Environ Adv. 2020;2 [Google Scholar]
- 56.Ho J.C., Michalak A.M., Pahlevan N. Widespread global increase in intense lake phytoplankton blooms since the 1980s. Nature. 2019;574(7780):667–670. doi: 10.1038/s41586-019-1648-7. [DOI] [PubMed] [Google Scholar]
- 57.Bilyeu L., Bloomfield B., Hanlon R., et al. Drone-based particle monitoring above two harmful algal blooms (HABs) in the USA. Environ Sci Atmos. 2022;2(6):1351–1363. [Google Scholar]
- 58.Mishra D.R., Kumar A., Ramaswamy L., et al. CyanoTRACKER: a cloud-based integrated multi-platform architecture for global observation of cyanobacterial harmful algal blooms. Harmful Algae. 2020;96 doi: 10.1016/j.hal.2020.101828. [DOI] [PubMed] [Google Scholar]
- 59.Uejio C.K., Gonsoroski E., Sherchan S.P., et al. Harmful algal bloom-related 311 calls, Cape Coral, Florida 2018–2019. J Water Health. 2022;20(3):531–538. doi: 10.2166/wh.2022.257. [DOI] [PubMed] [Google Scholar]
- 60.Pierce R., Henry M., Blum P., et al. Brevetoxin concentrations in marine aerosol: human exposure levels during a Karenia brevis harmful algal bloom. Bull Environ Contam Toxicol. 2003;70(1):161. doi: 10.1007/s00128-002-0170-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Backer L.C., Kirkpatrick B., Fleming L.E., et al. Occupational exposure to aerosolized brevetoxins during Florida red tide events: effects on a healthy worker population. Environ Health Perspect. 2005;113(5):644–649. doi: 10.1289/ehp.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Milian A., Nierenberg K., Fleming L.E., et al. Reported respiratory symptom intensity in asthmatics during exposure to aerosolized Florida red tide toxins. J Asthma. 2007;44(7):583–587. doi: 10.1080/02770900701539251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fleming L.E., Bean J.A., Kirkpatrick B., et al. Exposure and effect assessment of aerosolized red tide toxins (brevetoxins) and asthma. Environ Health Perspect. 2009;117(7):1095–1100. doi: 10.1289/ehp.0900673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fleming L.E., Kirkpatrick B., Backer L.C., et al. Initial evaluation of the effects of aerosolized Florida red tide toxins (brevetoxins) in persons with asthma. Environ Health Perspect. 2005;113(5):650–657. doi: 10.1289/ehp.7500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fleming L.E., Kirkpatrick B., Backer L.C., et al. Aerosolized red-tide toxins (brevetoxins) and asthma. Chest. 2007;131(1):187–194. doi: 10.1378/chest.06-1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kirkpatrick B., Fleming L.E., Bean J.A., et al. Aerosolized red tide toxins (brevetoxins) and asthma: continued health effects after 1 h beach exposure. Harmful Algae. 2011;10(2):138–143. doi: 10.1016/j.hal.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abdullah L., Ferguson S., Niedospial D., et al. Exposure-response relationship between K. brevis blooms and reporting of upper respiratory and neurotoxin-associated symptoms. Harmful Algae. 2022;117 doi: 10.1016/j.hal.2022.102286. [DOI] [PubMed] [Google Scholar]
- 68.Stumpf R.P., Li Y., Kirkpatrick B., et al. Quantifying Karenia brevis bloom severity and respiratory irritation impact along the shoreline of Southwest Florida. PLoS One. 2022;17(1) doi: 10.1371/journal.pone.0260755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bean J.A., Fleming L.E., Kirkpatrick B., et al. Florida red tide toxins (brevetoxins) and longitudinal respiratory effects in asthmatics. Harmful Algae. 2011;10(6):744–748. doi: 10.1016/j.hal.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kirkpatrick B., Fleming L.E., Backer L.C., et al. Environmental exposures to Florida red tides: effects on emergency room respiratory diagnoses admissions. Harmful Algae. 2006;5(5):526–533. doi: 10.1016/j.hal.2005.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hoagland P., Jin D., Beet A., et al. The human health effects of Florida red tide (FRT) blooms: an expanded analysis. Environ Int. 2014;68:144–153. doi: 10.1016/j.envint.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 72.Hoagland P., Jin D., Polansky L.Y., et al. The costs of respiratory illnesses arising from Florida Gulf Coast Karenia brevis blooms. Environ Health Perspect. 2009;117(8):1239–1243. doi: 10.1289/ehp.0900645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Diaz R.E., Friedman M.A., Jin D., et al. Neurological illnesses associated with Florida red tide (Karenia brevis) blooms. Harmful Algae. 2019;82:73–81. doi: 10.1016/j.hal.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kirkpatrick B., Bean J.A., Fleming L.E., et al. Gastrointestinal emergency room admissions and Florida red tide blooms. Harmful Algae. 2010;9(1):82–86. doi: 10.1016/j.hal.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ciminiello P., Dell'Aversano C., Iacovo E.D., et al. First finding of Ostreopsis cf. ovata toxins in marine aerosols. Environ Sci Technol. 2014;48(6):3532–3540. doi: 10.1021/es405617d. [DOI] [PubMed] [Google Scholar]
- 76.Gallitelli M., Ungaro N., Addante L.M., Procacci V., Silver N.G., Sabbà C. Respiratory illness as a reaction to tropical algal blooms occurring in a temperate climate. JAMA. 2005;293(21):2595–2600. doi: 10.1001/jama.293.21.2599-c. [DOI] [PubMed] [Google Scholar]
- 77.Vila M., Masó M., Sampedro N., Illoul H., Arin L., Garcés E., et al., editors. Proceedings of the 12th international conference on harmful algae. International Society for the Study of Harmful Algae and Intergovernmental…; 2008. The genus Ostreopsis in recreational waters of the Catalan Coast and Balearic Islands (NW Mediterranean Sea): is this the origin of human respiratory difficulties. [Google Scholar]
- 78.Brescianini C., Grillo C., Melchiorre N., et al. Ostreopsis ovata algal blooms affecting human health in Genova, Italy, 2005 and 2006. Euro Surveill. 2006;11(9) doi: 10.2807/esw.11.36.03040-en. Weekly releases (1997–2007) [DOI] [PubMed] [Google Scholar]
- 79.Durando P., Ansaldi F., Oreste P., et al. Ostreopsis ovata and human health: epidemiological and clinical features of respiratory syndrome outbreaks from a two-year syndromic surveillance, 2005-06, in north-west Italy. Euro Surveill. 2007;12(6) doi: 10.2807/esw.12.23.03212-en. Weekly releases (1997–2007) [DOI] [PubMed] [Google Scholar]
- 80.Illoul H., Hernández F.R., Vila M., et al. The genus Ostreopsis along the Algerian coastal waters (SW Mediterranean Sea) associated with a human respiratory intoxication episode. Cryptogam Algol. 2012;33(2):209–216. [Google Scholar]
- 81.Tichadou L., Glaizal M., Armengaud A., et al. Health impact of unicellular algae of the Ostreopsis genus blooms in the Mediterranean sea: experience of the French Mediterranean coast surveillance network from 2006 to 2009. Clin Toxicol. 2010;48(8):839–844. doi: 10.3109/15563650.2010.513687. [DOI] [PubMed] [Google Scholar]
- 82.Chomérat N., Antajan E., Auby I., et al. First characterization of Ostreopsis cf. ovata (Dinophyceae) and detection of ovatoxins during a multispecific and toxic Ostreopsis bloom on French Atlantic Coast. Mar Drugs. 2022;20(7):461. doi: 10.3390/md20070461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vila M., Abós-Herràndiz R., Isern-Fontanet J., Àlvarez J., Berdalet E. Establishing the link between Ostreopsis cf. ovata blooms and human health impacts using ecology and epidemiology. Sci Mar. 2016;80(S1):107–115. [Google Scholar]
- 84.Berdalet E., Pavaux A.-S., Abós-Herràndiz R., et al. Environmental, human health and socioeconomic impacts of Ostreopsis spp. blooms in the NW Mediterranean. Harmful Algae. 2022;119 doi: 10.1016/j.hal.2022.102320. [DOI] [PubMed] [Google Scholar]
- 85.Huisman J., Codd G.A., Paerl H.W., Ibelings B.W., Verspagen J.M., Visser P.M. Cyanobacterial blooms. Nat Rev Microbiol. 2018;16(8):471–483. doi: 10.1038/s41579-018-0040-1. [DOI] [PubMed] [Google Scholar]
- 86.Paerl H.W., Otten T.G., Kudela R. ACS Publications; 2018. Mitigating the expansion of harmful algal blooms across the freshwater-to-marine continuum. [DOI] [PubMed] [Google Scholar]
- 87.Metcalf J., Banack S., Wessel R., et al. Toxin analysis of freshwater cyanobacterial and marine harmful algal blooms on the west coast of Florida and implications for estuarine environments. Neurotox Res. 2021;39(1):27–35. doi: 10.1007/s12640-020-00248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Breidenbach J.D., French B.W., Gordon T.T., et al. Microcystin-LR aerosol induces inflammatory responses in healthy human primary airway epithelium. Environ Int. 2022;169 doi: 10.1016/j.envint.2022.107531. [DOI] [PubMed] [Google Scholar]
- 89.Stewart I., Webb P.M., Schluter P.J., et al. Epidemiology of recreational exposure to freshwater cyanobacteria–an international prospective cohort study. BMC Public Health. 2006;6:1–11. doi: 10.1186/1471-2458-6-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lévesque B., Gervais M.-C., Chevalier P., et al. Prospective study of acute health effects in relation to exposure to cyanobacteria. Sci Total Environ. 2014;466:397–403. doi: 10.1016/j.scitotenv.2013.07.045. [DOI] [PubMed] [Google Scholar]
- 91.Wu J., Hilborn E.D., Schaeffer B.A., et al. Acute health effects associated with satellite-determined cyanobacterial blooms in a drinking water source in Massachusetts. Environ Health. 2021;20:1–13. doi: 10.1186/s12940-021-00755-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hilborn E.D., Roberts V.A., Backer L., et al. Algal bloom–associated disease outbreaks among users of freshwater lakes—United States, 2009–2010. Morb Mortal Wkly Rep. 2014;63(1):11. [PMC free article] [PubMed] [Google Scholar]
- 93.Figgatt M., Hyde J., Dziewulski D., et al. Harmful algal bloom–associated illnesses in humans and dogs identified through a pilot surveillance system—New York, 2015. Morb Mortal Wkly Rep. 2017;66(43):1182–1184. doi: 10.15585/mmwr.mm6643a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lee S., Choi B., Kim S.J., Kim J., Kang D., Lee J. Relationship between freshwater harmful algal blooms and neurodegenerative disease incidence rates in South Korea. Environ Health. 2022;21(1):1–11. doi: 10.1186/s12940-022-00935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Stommel E.W., Field N.C., Caller T.A. Aerosolization of cyanobacteria as a risk factor for amyotrophic lateral sclerosis. Med Hypotheses. 2013;80(2):142–145. doi: 10.1016/j.mehy.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 96.Torbick N., Ziniti B., Stommel E., et al. Assessing cyanobacterial harmful algal blooms as risk factors for amyotrophic lateral sclerosis. Neurotox Res. 2018;33:199–212. doi: 10.1007/s12640-017-9740-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lavery A., Backer L., Daniel J. Evaluation of electronic health records to monitor illness from harmful algal bloom exposure in the United States. J Environ Health. 2021;839:8–14. [PMC free article] [PubMed] [Google Scholar]
- 98.Lavery A.M., Backer L.C., Roberts V.A., DeVies J., Daniel J. Evaluation of syndromic surveillance data for studying harmful algal bloom-associated illnesses—United States, 2017–2019. Morb Mortal Wkly Rep. 2021;70(35):1191. doi: 10.15585/mmwr.mm7035a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Roberts V.A., Vigar M., Backer L., et al. Surveillance for harmful algal bloom events and associated human and animal illnesses—one health harmful algal bloom system, United States, 2016–2018. Morb Mortal Wkly Rep. 2020;69(50):1889. doi: 10.15585/mmwr.mm6950a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Medina-Pérez N.I., Dall'Osto M., Decesari S., Paglione M., Moyano E., Berdalet E. Aerosol toxins emitted by harmful algal blooms susceptible to complex Air–Sea interactions. Environ Sci Technol. 2020;55(1):468–477. doi: 10.1021/acs.est.0c05795. [DOI] [PubMed] [Google Scholar]
- 101.Resiere D., Valentino R., Nevière R., et al. Sargassum seaweed on Caribbean islands: an international public health concern. Lancet. 2018;392(10165):2691. doi: 10.1016/S0140-6736(18)32777-6. [DOI] [PubMed] [Google Scholar]