Key Teaching Points.
-
•
Electrical cardioversion can lead to a loss of stimulation in patients with a leadless pacemaker system.
-
•
Safety precautions for the management of bradycardia or asystole must be taken before performing cardioversion.
-
•
Further investigation of the described case and its potential ramifications for other patients is necessary.
Introduction
Leadless cardiac pacemakers were introduced as a novel approach to treat bradyarrhythmias, overcoming the risk of lead- and pocket-associated complications of transvenous pacemakers.1, 2, 3 Recently, a system with an accelerometer capable of detecting mechanical atrial activity has been introduced, offering the opportunity for atrioventricular (AV) synchronous pacing.4, 5, 6 Owing to their intracardiac position, leadless cardiac pacemakers are inevitably in the path of electrical current during treatment with external cardioversion. This might increase the risk for damage to the implanted device. To our knowledge, this is the first case report of pacemaker dysfunction of a leadless cardiac pacemaker after external cardioversion.
Case report
History
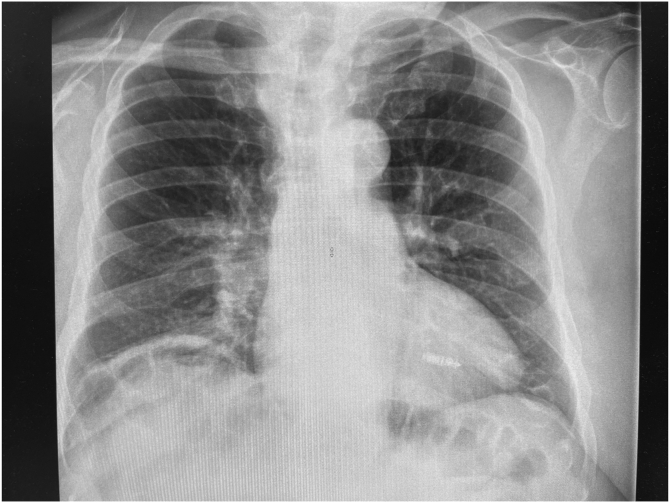
A 76-year-old man with symptomatic atrial fibrillation was referred to our outpatient arrhythmia clinic for external cardioversion. Twenty-one months prior, a transcatheter pacing system (TPS) was implanted owing to complete AV block and recurring bacteremia (Streptococcus equinus), avoiding future risk of lead- or pocket-related infections (Micra™ AV; Medtronic, Inc, Minneapolis, MN). A chest radiograph showing the device location is displayed in Figure 1. Relevant preexisting comorbidities were coronary artery disease, history of transcatheter aortic valve replacement owing to severe aortic stenosis, WHO grade III obesity (body mass index 43 kg/m2), arterial hypertension, type II diabetes, and obstructive sleep apnea. Transthoracic echocardiography showed a normal left ventricular ejection fraction without additional pathologies. Medication included apixaban and a 6-fold combination of antihypertensive agents.
Figure 1.
Chest radiograph showing the leadless pacemaker located in the right ventricular septal position.
Treatment and course
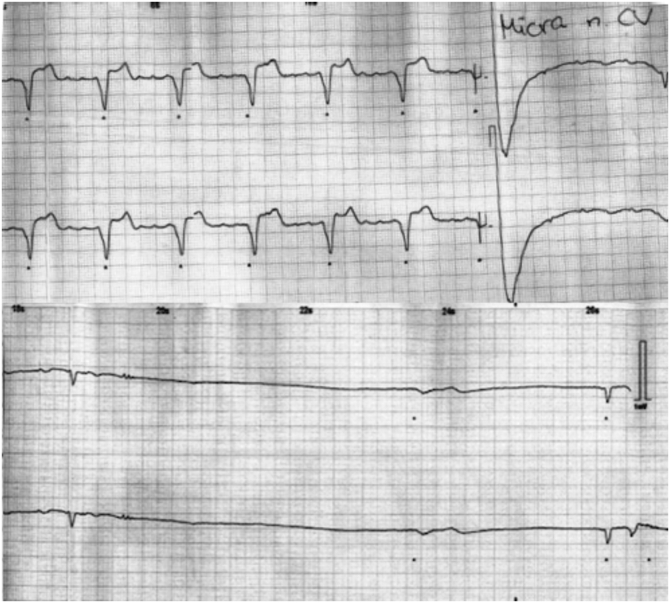
The initial electrocardiogram showed atrial fibrillation with permanent pacemaker stimulation (60 beats per minute [bpm]) in the patient with complete AV block. The TPS had been programmed to VVIR mode to avoid inadequate triggering during the arrhythmia. Sedation with propofol (230 mg fractionated) and exclusion of intracardiac thrombi via transesophageal echocardiography was performed before cardioversion. A first cardioversion attempt (200 J, biphasic, synchronized) was made using defibrillator patches in an anterior-lateral position. This impulse showed no effect. Therefore, the second cardioversion attempt (200 J, biphasic, synchronized) was performed via defibrillator paddles with a high contact pressure. The paddles were positioned in the anterior-lateral position. After delivery of the second impulse, the arrhythmia was terminated and loss of pacemaker stimulation was observed, leading to severe bradycardia (<20 bpm) in the pacemaker-dependent patient (Figure 2). Transcutaneous pacing was established. Few seconds later, pacemaker stimulation recommenced with a regular rate of 60 bpm. Directly after cardioversion, transient sinus arrest was observed but resolved spontaneously. The total duration of pacemaker dysfunction was estimated at 20 seconds. A device interrogation directly after the incident showed a reduced sensing, but no signs of damage or dysfunction (Table 1). After cardioversion, normal sinus rhythm with a very low A4 signal was recorded, which is likely owing to atrial cardiomyopathy. Therefore, AV synchronous pacing could not be ensured, and the pacemaker was kept in VVIR mode.
Figure 2.
Continuous electrocardiogram tracings during cardioversion. Tracing 1 (top) shows a macroreentrant atrial tachycardia with permanent ventricular pacing. On the right side, the shock artefact is visible. Tracing 2 (bottom) displays a loss of pacemaker stimulation, leading to severe bradycardia.
Table 1.
Technical device data of the leadless pacemaker system (Micra AV; Medtronic, Inc) periprocedurally and at follow-up
| Variable | Before cardioversion | After cardioversion | At 6-week follow-up |
|---|---|---|---|
| Programmed mode | VVIR | VVIR | VVIR |
| Battery voltage (V) | 3.01 | 3.01 | 3.01 |
| Sensing (mV) | 14.2 | 4.5 | 17.3 |
| Stimulation threshold (V) | 0.38 | 0.38 | 0.38 |
| Impulse duration (ms) | 0.24 | 0.24 | 0.24 |
| Impedance (Ω) | 640 | 580 | 590 |
Six weeks after cardioversion, a follow-up device interrogation was performed. All technical device parameters showed stable measurements and sensing had improved to a value comparable to the status before cardioversion. There were no signs of damage or dysfunction.
Given the transient nature of sinus arrest after cardioversion and the history of lead-associated complications, we deliberately decided against the implementation of atrial-based pacing in this case.
Discussion
Electrical cardioversion is a standard treatment for the restoration of sinus rhythm in patients with symptomatic atrial arrhythmias. So far, data concerning the safety of cardioversion and defibrillation in patients with TPS is scarce. In the few cases described so far, electrical cardioversion of patients with a TPS7,8 did not result in device dysfunction, even with energies as high as 360 J.7 Generally, 2 mechanisms could have led to device dysfunction: (1) a sensing defect resulting in oversensing and inadequate inhibition of the pacemaker system; and (2) the system’s inability to pace effectively (exit block). An exit block after cardioversion might occur owing to a rise in pacing thresholds or lead dislocation. The leadless pacemaker system does not have a capacitor, and thus capacitor saturation after cardioversion is not a possible mechanism in this case.
The alternating sensing might be a result of the cardioversion, indicating a potential sensing problem as the reason for the device dysfunction. However, it could also be explained by the sensing of different ectopic ventricular beats in this patient without sufficient intrinsic heart rhythm. Also, a transient exit block cannot be ruled out, as the pacing artefacts are extremely small during pacing and might not be discernible in the electrocardiogram recording of bradycardia (Figure 2).
Both cases published so far cover the cardioversion/defibrillation of leadless pacemakers without AV synchrony. We are not aware of any reports about cardioversions of systems with AV synchrony. Differences in the leadless pacemaker models could render the latter more susceptible to dysfunction by electrical current. The manufacturer was consulted but is not aware of a higher risk for this specific model.
Filipovic and colleagues7 reported a case of external cardioversion with defibrillator patches in the anterior-posterior position. Four shocks were required for successful cardioversion. There is conflicting evidence regarding the optimal patch position for cardioversion of atrial arrhythmias.9, 10, 11, 12 If the patches are placed anterior-posteriorly, a left parasternal position is recommended for the anterior patch.9 For the anterior-lateral variant, the anterior patch is placed in a right-parasternal position.9 In this special case, choosing a left-parasternal patch position would have placed the anterior patch in direct proximity to the leadless pacemaker system. Therefore, we deliberately opted for the anterior-lateral patch placement, which allowed us to use the right-parasternal position with more distance to the pacemaker. A possible influence of the patch position cannot be ruled out, but we are not aware of any data or recommendations supporting the anterior-posterior over the anterior-lateral position regarding periprocedural safety. It is our opinion that a leadless pacemaker system will inevitably be in the path of the electrical current regardless of the patch position. In the case reported here, defibrillator paddles were used, while Filipovic and colleagues used defibrillator patches. The high contact pressure applied through paddles might have an influence on the effective intracardiac current. However, Filipovic and colleagues applied more shocks with higher energy. Therefore, we consider this explanation to be unlikely.
To our knowledge, this is the first report of a device dysfunction of a TPS after external cardioversion. So far, the reason for this dysfunction remains unclear. Further investigation and a high level of vigilance is necessary for cardioversion of patients with leadless pacemakers.
Conclusion
External cardioversion can cause transient device dysfunction in patients with a TPS. Safety precautions for the management of bradycardia or asystole must be taken before performing external cardioversion. Until further investigations have been performed, caution is advised in the cardiac application of electrical impulses in patients with TPS.
Footnotes
Funding Sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures: Dr Fluschnik received a grant from Biotronik and speaker fees from Abbott and Medtronic, all outside this submitted work. Dr Tönnis received speaker fees from Medtronic and proctoring fees from Boston Scientific, all outside this submitted work. Dr Würger, Dr Nies, and Dr Nikorowitsch report no conflicts of interest.
References
- 1.Tjong F.V., Reddy V.Y. Permanent leadless cardiac pacemaker therapy: a comprehensive review. Circulation. 2017;135:1458–1470. doi: 10.1161/CIRCULATIONAHA.116.025037. [DOI] [PubMed] [Google Scholar]
- 2.Cantillon D.J., Dukkipati S.R., Ip J.H., et al. Comparative study of acute and mid-term complications with leadless and transvenous cardiac pacemakers. Heart Rhythm. 2018;15:1023–1030. doi: 10.1016/j.hrthm.2018.04.022. [DOI] [PubMed] [Google Scholar]
- 3.El-Chami M.F., Bockstedt L., Longacre C., et al. Leadless vs. transvenous single-chamber ventricular pacing in the Micra CED study: 2-year follow-up. Eur Heart J. 2022;43:1207–1215. doi: 10.1093/eurheartj/ehab767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitacchione G., Schiavone M., Gasperetti A., Viecca M., Curnis A., Forleo G.B. Atrioventricular synchronous leadless pacemaker: state of art and broadened indications. Rev Cardiovasc Med. 2021;22:395–401. doi: 10.31083/j.rcm2202045. [DOI] [PubMed] [Google Scholar]
- 5.Steinwender C., Khelae S.K., Garweg C., et al. Atrioventricular synchronous pacing using a leadless ventricular pacemaker: results from the MARVEL 2 study. JACC Clin Electrophysiol. 2020;6:94–106. doi: 10.1016/j.jacep.2019.10.017. [DOI] [PubMed] [Google Scholar]
- 6.Chinitz L., Ritter P., Khelae S.K., et al. Accelerometer-based atrioventricular synchronous pacing with a ventricular leadless pacemaker: results from the Micra atrioventricular feasibility studies. Heart Rhythm. 2018;15:1363–1371. doi: 10.1016/j.hrthm.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Filipovic K., Bellmann B., Luker J., Steven D., Sultan A. External electrical cardioversion of persistent atrial fibrillation in a patient with a Micra Transcatheter Pacing System. Indian Pacing Electrophysiol J. 2018;18:44–46. doi: 10.1016/j.ipej.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venier S., Jacon P., Defaye P. Direct electrical shock on a leadless pacemaker. J Interv Card Electrophysiol. 2017;49:39. doi: 10.1007/s10840-017-0230-1. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt A.S., Lauridsen K.G., Moller D.S., et al. Anterior-lateral versus anterior-posterior electrode position for cardioverting atrial fibrillation. Circulation. 2021;144:1995–2003. doi: 10.1161/CIRCULATIONAHA.121.056301. [DOI] [PubMed] [Google Scholar]
- 10.Motawea K.R., Mostafa M.R., Aboelenein M., et al. Anteriolateral versus anterior-posterior electrodes in external cardioversion of atrial fibrillation: a systematic review and meta-analysis of clinical trials. Clin Cardiol. 2023;46:359–375. doi: 10.1002/clc.23987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eid M., Abu Jazar D., Medhekar A., et al. Anterior-posterior versus anterior-lateral electrodes position for electrical cardioversion of atrial fibrillation: a meta-analysis of randomized controlled trials. Int J Cardiol Heart Vasc. 2022;43 doi: 10.1016/j.ijcha.2022.101129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirchhof P., Eckardt L., Loh P., et al. Anterior-posterior versus anterior-lateral electrode positions for external cardioversion of atrial fibrillation: a randomised trial. Lancet. 2002;360:1275–1279. doi: 10.1016/s0140-6736(02)11315-8. [DOI] [PubMed] [Google Scholar]