Summary
Background
Health facility-level factors play a crucial role in women's access to and use of caesarean section (CS) services, but lacks relevant evidence. The study aimed to understand the effects of health facility-level factors on CS delivery in Bangladesh.
Methods
The 2017–18 Bangladesh Demographic and Health Survey (2017–18 BDHS) and the 2017 Bangladesh Health Facility Survey (2017 BHFS) were linked and analysed in this study. The sample comprised of 4954 women gave at least one live birth within three years preceding the survey. The outcome variable was delivery through CS (yes, no) and the explanatory variables were health facility-level, individual-level, household-level, and community-level factors. Moran's I and Getis-Ord General G statistic were used to identify the hotspots of delivery through CS. Mixed-effect multilevel logistic regression was used to examine the association of the outcome variable with explanatory variables.
Findings
Around 33% of women in Bangladesh underwent CS in their most recent pregnancies. The hotspots of delivery through CS are located primarily in Rajshahi, Dhaka, and Khulna divisions. The likelihood of delivered through CS increased with the rising scores of the management (Adjusted Odds Ratio (AOR), 1.83; 95% CI 1.04–2.07) and infrastructure (AOR, 3.14; 95% CI 1.40–5.12) of the nearest health facility. The readiness of health facilities to provide comprehensive obstetric care was significantly associated with an increased likelihood of delivery through CS (AOR, 2.18; 95% CI 1.15–3.28). These relationships were strong for private than non-government and government health facilities.
Interpretation
The proximity of comprehensive obstetric care facilities to women's residences and their readiness to provide services play critical roles in the access to and use of CS in Bangladesh. The findings highlight the importance of necessary healthcare personnel, including midwives, availability of government hospitals where undue CS are avoided, and awareness-building programmes about the adverse effects of CS delivery.
Funding
None.
Keywords: Caesarean delivery, Health facility-level factors, Spatial variation of caesarean section, Multilevel logistics regression, Bangladesh
Research in context.
Evidence before this study
Available research in Bangladesh and other low-income and middle-income countries (LMICs) have focused mainly on population-level factors associated with caesarean section (CS) delivery, such as women's age, education, occupation, husband's education, occupation, number of children ever born, wealth quintile, places of residence and place of region. Evidence suggests that facility-level factors play a crucial role in determining the prevalence of CS delivery. However, there has been little high-quality and population-based evidence in LMICs on the association between health facility-level factors and CS delivery, and none from Bangladesh and other Asian countries.
Added value of this study
The current study provides an understanding of the association between health facility-level factors and CS delivery. Some of the health facility-level factors that are found positively associated with CS delivery include improved management, infrastructure, and healthcare facility readiness for comprehensive obstetric care.
Implications of all the available evidence
The findings of this study and other available evidence provide a picture of the current CS delivery and its determinants in Bangladesh. The study also provides a strong justification for ensuring proper accountability of the healthcare providers who unnecessarily induce CS delivery.
Introduction
Caesarean section (CS) is usually performed to manage emergency obstetric complications and ensure the best possible health outcomes for mothers and newborns.1 Although the optimal rate of CS remains unknown in many settings,2 the World Health Organization suggests it should be between 10 and 15%.2,3 Globally, the prevalence of delivery through CS, including medically avoidable CS, has started to increase by several folds since the mid-1980s and continues to climb.3 The number of delivery through CS was 16 million in 2000 (12.1% of all live births) and within twenty years, it rose to 29.7 million (21.1% of all live births in 2021). A further challenge is inequities in the availability of and accessibility to CS across the countries.4 The delivery rates via CS are alarmingly high in many low-income and middle-income countries (LMICs), including Latin America and the Caribbean (42.8%) and Eastern Asia (33.7%).4 Although the CS delivery rate is lower in many Sub-Saharan African countries (9% or below),5 the rates are significantly different in urban and rural areas. For example, the findings of a spatial analysis conducted in Ethiopia show that the delivery through CS rate is more than 20% in urban Ethiopia and less than 5% in rural and regional Ethiopia,6 indicating a double burden of CS—the unmet need of CS coupled with its overuse.7,8 A massive rise of unnecessary delivery through CS coupled with unavailability to those for whom it is a medical necessity (triple burden) has become a global public health concern.9
The higher rate of delivery through CS is associated with maternal morbidity (severe postpartum complications including infection or heavy bleeding) and mortality.2 Evidence suggests that the adverse outcomes associated with CS births will continue to increase over the coming decades, with the global average of CS climbing to 29% by 2030.5 The outcomes would become even worse for some regions, including Eastern Asia (63%), Latin America and the Caribbean (54%), and Western Asia (50%).4
The percentage of delivery through CS in Bangladesh was only 4% in 2004.10 Like many LMICs, Bangladesh observed a rapid surge in the CS birth rate and the percentage increased nearly eightfold within a decade. Currently, Bangladesh has one of the highest rates of CS delivery in the world (31% in 2016), equivalent to around 1.48 million CS births per annum.1 A significant proportion of these CS deliveries (>65%) was unnecessary and avoidable.1 A further 7.5% of women (n = 300,000), who needed a CS, were deprived of accessing the service due to associated higher expenses.1 The average cost of delivery through CS in Bangladesh is US$ 612, two times higher than the average monthly income of the Bangladesh population and many times higher than average income of the low-earning groups.11 Between 2016 and 2018, the rate of medically unnecessary CS climbed to 51%, an alarming increase within a short period.1 This growth rate and the double burden of CS delivery are associated mainly with poor regulations, particularly in the private sector, where over 80% of the overall CS is performed.1
Increased delivery rate through CS is multifaceted and interconnected5,12 and health facilities play a major role.13 However, the extent to which the health facilities influence performing1 CS remains unknown in Bangladesh and many other LMICs due to a lack of evidence. Most research studies conducted in LMICs, including Bangladesh have focused mainly on population-level factors associated with CS delivery, such as women's age, education, occupation, wealth quintile, and places of residence.8,13, 14, 15, 16, 17, 18, 19, 20, 21, 22 Although health facility-level factors play a crucial role in determining the prevalence of CS births,13 these studies did not consider the health facility-level factors. Therefore, not considering health facility-level factors in the previous studies might have overestimated or underestimated the true effects sizes.17 Moreover, evidence of spatial variation to indicate areas where delivery through CS is relatively high or low is rare in the context of Bangladesh. As a result, it is often a challenge for policymakers in Bangladesh to develop effective policies and programmes to rationalise the appropriate use of CS delivery. This study aimed to determine the clusters of CS use, and their locations and to identify the effects of health facility-level factors on CS delivery in the context of Bangladesh.
Methods
Study design
In this cross-sectional study, the population-level and health facility-level data were extracted from the 2017–18 Bangladesh Demographic and Health Survey (2017–18 BDHS) and the 2017 Bangladesh Health Facility Survey (2017 BHFS), respectively. We merged both data using their GPS (global positioning system) point locations and administrative boundary linkage methods. Details of this method can be found elsewhere,23 and detailed sampling procedures are available in the survey reports.24,25 Briefly, both surveys were conducted as part of the Demographic and Health Survey Program. The National Institute of Population Research and Training conducted these surveys at the field level, and the Ministry of Health and Family Welfare (MOHFW) of Bangladesh provided supervision.24
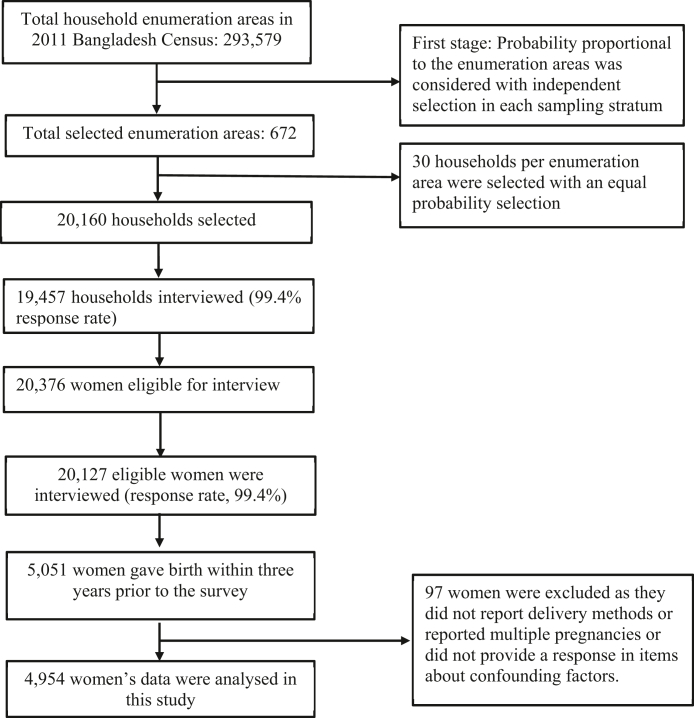
The 2017–18 BDHS collected a nationally representative sample using the multistage random sampling methods. At the first stage of sampling, the survey selected 675 Enumeration Areas (EAs, clusters) from the list of 293,579 EAs used by the Bangladesh Bureau of Statistics in the 2011 National Population Census. Of these EAs, data collection was undertaken in 672 EAs. Prior to data collection, a household listing operation was conducted. This was then used to select a fixed number of 30 households from each selected EAs through probability proportional to the unit size. A total of 20,160 households were selected, of which the data collection was undertaken in 19,457, with over a 96% inclusion rate. There were 20,376 eligible women aged 15–49 years, who were usual residents of or lived in those households the night before the date of the survey. Of those eligible women, data were collected from 20,127 women with a response rate of 98.8%.
The 2017 BHFS offers data on the availability of health facilities and the range of services provided by those facilities in Bangladesh.25 The survey used a list of 19,811 registered health facilities generated by the MOHFW. A shortlist of 1600 health facilities was generated, of which 1524 health facilities were finally included. The selection was made following the census of the district health facilities (DHF), mother and child welfare centres (MCWC) and stratified random sampling of healthcare facilities run by the government (health facility which is operated by the government and accessible to all with no or a very few costs), private (health facility which is operated by any person or partnership or agency where the initial target is to make a profit), and non-governmental (health facility which is non-profit and operated by any voluntary citizen group or international organization) organizations. The reasons for using the census of the DHF (n = 62) and MCWC (n = 91) were their limited number and vital role in providing reproductive healthcare services, including CS delivery.
Sample
We analysed data collected from 4954 women selected from 672 EAs included in the BDHS 2017/18 (Fig. 1). The criteria used for inclusion in this study were at least one live birth within three years preceding the survey and response to the questions on delivery through CS. Women who reported giving birth to multiple pregnancies were excluded from the analysis, as they were at higher risk of facing pregnancy complications and thereby resulting in CS deliveries.26,27 We did not involve patients or the public in our work.
Fig. 1.
Sampling strategy of the 2017/18 BDHS and sample selection procedure.
Outcome variable
The outcome variable was delivery through CS. The relevant data were collected by asking women “Was (NAME of the most recent child they gave birth in the preceding three years) delivered by caesarean, that is, did they cut your belly open to take the baby?”. Responses were coded as 1 for delivery through CS and 0 for not delivery through CS.
Explanatory variables
The explanatory variables were selected based on a rapid literature review of papers published in the LMICs context. Online databases including PubMed, CINHAL, Web of Science, Embase, and Google Scholar were searched with the relevant keywords for the period January 2000–July 2021. Of the factors identified from the literature search, those were available in our dataset were then classified as health facility-level, individual-level, household-level, and community-level factors.
The health facility-level variables were general service readiness (consisting of management and infrastructure of health facilities), the availability and readiness to provide comprehensive obstetric care, and the regional level average on-road distance from women's homes to the nearest health facilities providing comprehensive emergency obstetric care. The scores for the availability of comprehensive obstetric care services at the healthcare facilities were created using seven variables: parenteral administration of antibiotics, parenteral administration of uterotonic drugs, parenteral administration of anticonvulsants, assisted vaginal delivery, manual removal of retained products, neonatal resuscitation, and blood transfusion. Comprehensive obstetric care readiness scores were computed using nine dichotomous variables, which were the following: staff trained in delivery and newborn care; anaesthesia equipment; resuscitation table or neonatal resuscitation kit; oxygen; spinal needle; blood typing; crossmatch testing; blood supply sufficiency, and caesarean section set. The scores for these two indicators were generated using the principal component analysis.28 Finally, the availability and the readiness scores were used to measure the preparedness of facilities to provide comprehensive obstetric care services.
The average on-road distance was calculated in two stages. In the first stage, women's household clusters of the nearest health facilities that provide comprehensive emergency obstetric care were identified. In the second stage, road communication system data in Bangladesh were used and the average on-road distance was computed separately for eight administrative divisions. We used divisional distance instead of distance for each woman's household cluster from health facilities. This means that not all nearest CS-providing health facilities in a cluster were included because data for only a section of CS-providing private healthcare facilities were available. However, BHFS included all government facilities that provide CS services. The computation procedures can be found elsewhere.29
The individual-level variables were: respondents' age at last birth, educational attainment, employment status, and the number of children ever given birth. The household-level variables were: husbands' educational attainment, occupation, and household wealth quintile. We categorised husbands’ occupations based on common jobs identified in previous studies in Bangladesh.30,31 The BDHS generated the wealth quintile variable using the principal component analysis of data on household assets. The detailed computational procedure of this variable can be found in the BDHS survey report.24 The community-level factors variables were the place of residence and region of residence.
Statistical analysis
Descriptive statistics were used to summarise the characteristics of the respondents. The global Moran's I statistic was used to assess the variation of delivery through CS across divisions. The Getis-Ord General G statistic was used to measure the degree of clustering of delivery through CS. Multilevel logistic regression was used to assess the associations of CS delivery with health facility-level factors and adjusted for the individual-level, household-level, and community-level factors. We used multilevel regression because BDHS data are hierarchically structured, individuals are nested within households and households are nested within clusters.24,25 The variables included in the multilevel models were selected in two stages. We first ran univariable regression and selected the independent variables that were significant at p < 0.20 level. In the second stage, the multicollinearity of the selected variables was checked before including them in the models. If evidence of multicollinearity was found (if Variance Inflation Factor (VIF) > 10), the relevant variable was deleted, and the model was re-run. We followed the progressive model building technique to develop four different models. Model 1 was the null model where no covariate was adjusted. Model 2 was the health facility level model, which was adjusted with the relevant variables at the health facility level. Model 3 was the extension of Model 2, in which individual- and household-level factors were included. Finally, Model 4 was adjusted for health facility-level, individual-level, household-level, and community-level variables. Results were reported as Adjusted Odds Ratios (AOR) with 95% CI. The Intra-Class Correlation (ICC), VIF, Akaike information criterion (AIC) and Bayesian information criterion (BIC) for each model were recorded and compared to indicate the best model. The ICC was calculated by dividing the between-clusters-variance of delivery through CS (random intercept variance) with the total variance of delivery through CS (sum of between-clusters-variance and within-cluster (residual) variance of delivery through CS). Statistical package R and ArcGIS version 10.6.1 (ESRI. ArcGIS Desktop: Release 10. Redlands, CA: Environmental Systems Research Institute. 2011) were used for all statistical analyses.
Ethical considerations
We analysed de-identified publicly available data from two nationally representative surveys. Both the surveys received ethical approvals from the Demographic and Health Survey and the Government of Bangladesh. No additional ethical approval was required to conduct this study.
Role of the funding source
We did not receive any funding for this study.
Results
Socio-economic characteristics of the respondents
Table 1 presents the socio-demographic characteristics of the study participants. Of the 4954 study participants, 71% were between 20 and 34 years old. Nearly half of the participants had completed secondary education (49%), and an additional 17% had completed higher education. Nearly one-third had one to two children at the time of performing CS operation. Around 73% of women resided in rural areas and over 75% of women had four years or more intervals between their two most recent successive live births.
Table 1.
Socio-demographic characteristics of the respondents.
| Overall+ % (95% CI) |
Delivered through caesarean section++ % (95% CI) |
|
|---|---|---|
| Women's age at birth of the last child | ||
| ≤19 years | 25.10 (23.74–26.52) | 29.69 (26.75–32.80) |
| 20–34 years | 70.68 (69.21–72.11) | 34.70 (32.51–36.96) |
| ≥35 years | 4.21 (3.66–4.85) | 29.29 (23.18–36.24) |
| Women's educational attainment | ||
| No formal education | 6.31 (5.48–7.25) | 17.26 (12.88–22.74) |
| Primary | 27.65 (25.87–29.50) | 18.12 (15.70–20.82) |
| Secondary | 49.00 (47.18–50.83) | 34.48 (32.11–36.94) |
| Higher | 17.03 (15.57–18.61) | 59.98 (56.08–63.76) |
| Women's employment status | ||
| Employed | 37.26 (35.13–39.45) | 25.33 (22.89–27.94) |
| Not employed | 62.74 (60.55–64.87) | 37.90 (35.53–40.33) |
| Husbands' educational attainment | ||
| No formal education | 13.65 (12.26–15.17) | 17.48 (14.34–21.15) |
| Primary | 33.67 (31.96–35.42) | 22.38 (19.83–25.15) |
| Secondary | 34.04 (32.29–35.73) | 35.80 (32.92–38.79) |
| Higher | 18.37 (16.89–19.95) | 60.62 (56.81–64.30) |
| Husbands' occupation | ||
| Agriculture worker | 19.14 (17.54–20.85) | 21.01 (17.83–24.58) |
| Physical worker | 52.32 (50.42–54.21) | 31.53 (29.19–33.95) |
| Services | 5.73 (4.99–6.56) | 67.35 (61.10–73.03) |
| Business | 20.39 (18.96–21.90) | 39.85 (36.32–43.49) |
| Other | 0.21 (0.11–0.42) | 28.58 (7.34–66.91) |
| Parity | ||
| 1–2 children | 71.06 (69.47–72.61) | 38.13 (36.01–40.28) |
| >2 children | 28.94 (27.39–30.53) | 21.16 (18.65–23.91) |
| Intervals between the two most recent live births | ||
| ≤2 years | 6.76 (5.99–7.62) | 23.96 (19.14–29.56) |
| 3–4 years | 17.83 (16.65–19.07) | 23.85 (20.54–27.50) |
| >4 years | 75.42 (73.97–76.81) | 36.26 (34.16–38.41) |
| Family types | ||
| Nuclear family | 31.33 (29.66–33.05) | 35.06 (32.21–38.03) |
| Joint family | 68.67 (66.95–70.34) | 32.37 (30.21–34.61) |
| Household wealth status | ||
| Poorest | 20.65 (18.61–22.84) | 13.14 (10.77–15.94) |
| Poorer | 20.53 (19.03–22.12) | 22.58 (19.51–25.98) |
| Middle | 19.18 (17.66–20.81) | 31.42 (27.94–35.13) |
| Richer | 20.15 (18.41–22.01) | 38.92 (35.37–42.59) |
| Richest | 19.48 (17.58–21.54) | 61.56 (57.98–65.02) |
| Place of residence | ||
| Urban | 26.81 (25.13–28.55) | 44.24 (41.15–47.39) |
| Rural | 73.19 (71.45–74.87) | 29.18 (26.88–31.58) |
| Region of residence | ||
| Barishal | 5.71 (5.15–6.33) | 24.81 (20.19–29.96) |
| Chattogram | 21.13 (19.48–22.88) | 26.68 (22.51–31.31) |
| Dhaka | 25.60 (23.88–27.40) | 43.11 (38.52–47.81) |
| Khulna | 9.20 (8.34–10.14) | 43.51 (38.17–49.00) |
| Mymensingh | 8.54 (7.69–9.49) | 26.33 (22.16–30.96) |
| Rajshahi | 11.63 (10.39–13.00) | 35.73 (30.47–41.36) |
| Rangpur | 10.59 (9.54–11.74) | 27.77 (22.49–33.75) |
| Sylhet | 7.60 (6.75–8.54) | 23.40 (18.68–28.90) |
Note: Overall sample: 4954, Caesarean section use sample: 1642, +Column percentage, ++Row percentage.
Distribution of delivery through CS across women's socio-demographic characteristics
Over 33% of women underwent CS during their last deliveries (Table 1). Most of the women were 20–34 years old (34.70%) and received higher education (59.98%). Delivery through CS was higher among unemployed women (38%) and those who had 1–2 children at the time of CS delivery operation (38%). Higher rates of delivery through CS was found among women living in urban areas (44%) and resided in Dhaka (43%) and Khulna (44%) divisions. The division-wise variations in CS use were significant (p < 0.001, results not shown) (Supplementary Figure S1).
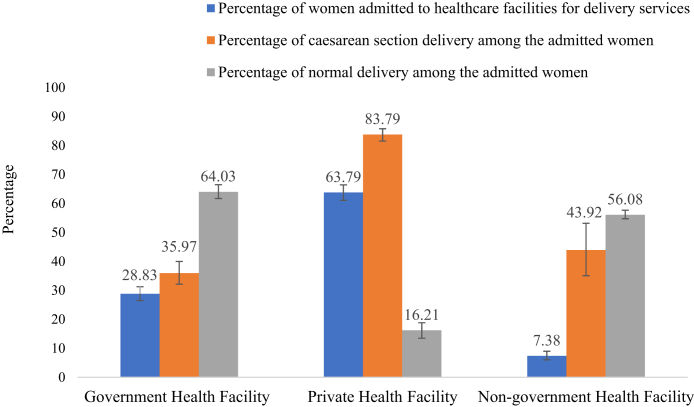
The division-wise distribution of healthcare facilities included in the 2017 BHFS is presented in Supplementary Table S1. The average score of comprehensive obstetric care service availability for health facilities was 77, higher for the private health facilities (score = 86) than non-government health facilities (score = 76) and government health facilities (score = 69) (results not shown in the table). The rate of delivery through CS was significantly different across government, private and non-government health facilities (Fig. 2, p < 0.01, results not shown, Supplementary Figure S2). Around two-thirds of women having facility-based delivery were admitted to private health facilities, and nearly 84% of them underwent CS. On the contrary, around 36% of women who had been admitted to government health facilities underwent CS.
Fig. 2.
Distribution of women from Bangladesh who underwent caesarean section across different types of health facilities.
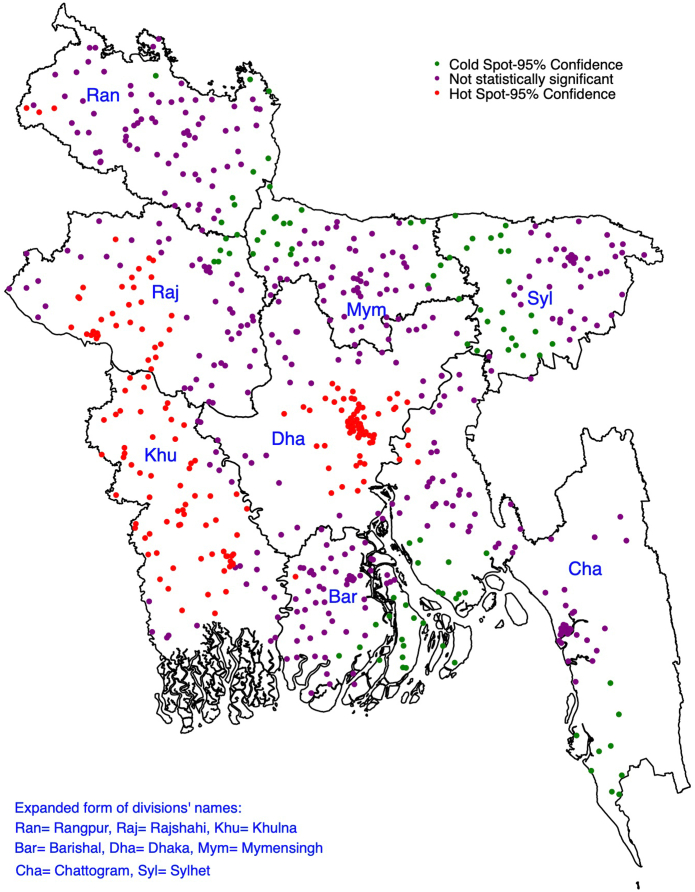
The spatial clustering of the delivery through caesarean section in Bangladesh
We found statistically significant positive spatial autocorrelation of delivery through CS in Bangladesh (Global Moran's I = 0.437, z = 69.586, p < 0.001). The Getis-Ord General G statistics revealed the presence of high clustering (z-score = 6.78, p < 0.001). The hot spots, areas with a high-level of delivery through CS, were mainly located in Dhaka, Rajshahi, and Khulna divisions (Fig. 3). The cold spots, areas with low-level of delivery through CS, were located mainly in Rangpur, Mymensingh, Sylhet, and Chattogram divisions.
Fig. 3.
Spatial clustering of the delivery through caesarean section in Bangladesh.
Model selection
The associations of delivery through CS with health facility-, individual-, household-, and community-level factors were assessed using multilevel logistic regression models. We developed four different models with different sets of confounders at the health facility-level, individual-level, household-level, and community-level. AIC, BIC, and ICC values of the models were compared and the preferred model was the one that had the smallest AIC, BIC, and ICC values (Table 2). According to these markers, Model 4 (which included health facility-, individual-, household-, and community-level variables) fitted the data better than the other models. The ICC value for the null model (Model 1) suggested around 22% variation in CS delivery across the clusters. However, this variation was reduced to only 5% once health facility-, individual-, household-, and community-level factors were included in the final model. Around 12% of this reduction occurred once health facility-level factors were included in the null model.
Table 2.
Multilevel logistic regression models assessing the relationship of delivery through caesarean section with health facility-, individual-, household-, and community-level factors (N = 4954).
| Characteristics | Null model | Health facility-level model, AOR (95% CI) | Health facility-, individual- and household-level model, AOR (95% CI) | Health facility-, individual-, household-, and community-level model, AOR (95% CI) |
|---|---|---|---|---|
| General health service readiness | ||||
| Health facility management system | 1.18 (0.98–1.36) | 1.16 (0.96–1.40) | 1.13 (0.91–1.42) | |
| Health facility infrastructure | 1.88 (1.08–2.18)∗∗ | 1.83 (1.05–2.08)∗∗ | 1.83 (1.04–2.07)∗∗ | |
| Comprehensive obstetric care availability in health facility | 3.17 (1.20–5.20)∗ | 3.13 (1.34–5.13)∗ | 3.14 (1.40–5.12)∗ | |
| Health facility readiness to provide comprehensive obstetric care | 2.76 (2.14–3.18)∗∗ | 2.24 (1.14–3.28)∗∗ | 2.18 (1.15–3.28)∗∗ | |
| Average distance to the nearest health facility | 0.84 (0.78–0.98)∗∗ | 0.78 (0.44–0.98)∗∗ | 0.72 (0.42–0.94)∗∗ | |
| Women's age | ||||
| ≤19 (ref) | 1.00 | 1.00 | ||
| 20–34 | 1.44 (1.20–1.71)∗∗ | 1.44 (1.21–1.72)∗∗ | ||
| ≥35 | 1.81 (1.20–2.73)∗∗ | 1.75 (1.16–2.64)∗∗ | ||
| Women's educational attainment | ||||
| No education (Ref) | 1.00 | 1.00 | ||
| Primary | 0.95 (0.65–1.38) | 0.94 (0.65–1.38) | ||
| Secondary | 1.42 (0.98–2.08) | 1.40 (0.96–2.05) | ||
| Higher | 2.12 (1.39–3.23)∗∗ | 2.11 (1.38–3.22)∗∗ | ||
| Women's employment status | ||||
| Not employed (ref) | 1.00 | 1.00 | ||
| Employed | 0.74 (0.63–0.86)∗∗ | 0.69 (0.58–0.80)∗∗ | ||
| Husbands' educational attainment | ||||
| No formal education (ref) | 1.00 | 1.00 | ||
| Primary | 1.07 (0.82–1.39) | 1.08 (0.83–1.41) | ||
| Secondary | 1.32 (1.01–1.74)∗ | 1.35 (1.03–1.77)∗ | ||
| Higher | 2.04 (1.47–2.83)∗∗ | 1.98 (1.42–2.75)∗∗ | ||
| Husbands' occupation status | ||||
| Agricultural worker (ref) | 1.00 | 1.00 | ||
| Physical worker | 1.09 (0.88–1.35) | 1.13 (0.91–1.39) | ||
| Services | 1.52 (1.05–2.21)∗ | 1.59 (1.10–2.30) | ||
| Business | 1.12 (0.88–1.43) | 1.17 (0.92–1.49) | ||
| Other | 0.53 (0.09–3.28) | 0.57 (0.09–3.49) | ||
| Total children ever born | ||||
| 1–2 (ref) | 1.00 | 1.00 | ||
| >2 | 0.64 (0.53–0.79)∗∗ | 0.67 (0.56–0.82)∗∗ | ||
| Intervals between the two most recent live births | ||||
| ≤2 years | 1.00 | 1.00 | ||
| 3–4 years | 1.11 (0.78–1.56) | 1.10 (0.78–1.55) | ||
| >4 years | 1.67 (1.23–2.27)∗∗ | 1.57 (1.15–2.14)∗∗ | ||
| Family types | ||||
| Nuclear (ref) | 1.00 | 1.00 | ||
| Joint | 0.90 (0.77–1.05) | 0.94 (0.80–1.10) | ||
| Household wealth status | ||||
| Richest (ref) | 2.37 (1.88–2.99)∗∗ | 1.00 | ||
| Richer | 1.12 (0.90–1.39) | 2.43 (1.90–3.11)∗∗ | ||
| Middle | 1.00 | 1.13 (0.91–1.41) | ||
| Poorer | 0.76 (0.60–0.95)∗∗ | 0.75 (0.60–0.95)∗∗ | ||
| Poorest | 0.48 (0.37–0.63)∗∗ | 0.49 (0.38–0.64)∗∗ | ||
| Type of residential place | ||||
| Urban (ref) | 1.00 | |||
| Rural | 1.00 (0.83–1.21) | |||
| Region of residence | ||||
| Barishal (ref) | 1.00 | |||
| Chattogram | 0.75 (0.54–1.05) | |||
| Dhaka | 1.40 (1.01–1.95)∗ | |||
| Khulna | 1.93 (1.37–2.72)∗∗ | |||
| Mymensingh | 1.19 (0.84–1.69) | |||
| Rajshahi | 1.64 (1.16–2.32)∗∗ | |||
| Rangpur | 1.35 (0.95–1.91) | |||
| Sylhet | 0.86 (0.60–1.22) | |||
| Random effects (Measures of variation for short birth interval) | ||||
| Community level variance (SE) | 0.91 (0.11)∗∗ | 0.59 (0.06)∗∗ | 0.51 (0.07)∗∗ | 0.42 (0.06)∗∗ |
| ICC | 0.216 | 0.095 | 0.073 | 0.050 |
| PCV | Reference | 35.16% | 43.95% | 53.85% |
| Median odds ratio | 2.48 | 1.75 | 1.63 | 1.44 |
| Model fit statistics | ||||
| AIC | 6126.08 | 5244.86 | 5208.38 | 4436.93 |
| BIC | 6139.11 | 5394.19 | 5409.66 | 4564.98 |
Note: Model 1 is the null model, a baseline model without any determinant variables. Model 2 is adjusted for health facility-level factors. Model 3 is adjusted for health facility-, individual- and household-level factors. Model 4 is adjusted for health facility-, individual-, household- and community-level factors. AIC: Akaike's Information Criteria, BIC: Bayesian Information Criteria, PCV: Percentage Change in Variance. ∗∗p < 0.01, ∗p < 0.05.
Factors associated with caesarean section use in Bangladesh
After adjusting for all factors in the final model, health facility-level factors were identified as the most important predictors of delivery through CS (Table 2). Likelihoods of delivery through CS increased with the increasing scores in health facility infrastructure (AOR, 1.83, 95% CI, 1.04–2.07), availability of emergency obstetric care in the health facility (AOR, 3.14, 95% CI, 1.40–5.12), and readiness to provide such services (AOR, 2.18, 95% CI, 1.15–3.28). At the participants' level, women's increasing age, higher educational attainment, more than four-year intervals between the two most recent successive pregnancies, and husbands' secondary or higher educational attainment were associated with the higher likelihoods of delivery through CS. Women's engagement to formal work (compared to the unemployed women) and having more than two children (compared to 1–2 children) were protectively associated with delivery through CS. The likelihoods of delivery through CS were lower among women of poorer and poorest household wealth quintiles than women of middle-wealth quintiles. On the contrary, the likelihood of delivery through CS was higher among women in the richer-wealth quintile.
In addition to the overall effects of health facility-level factors, their differences were further explored across types of health facilities: government, private, and non-government (Table 3). We found the effects of health facility-level factors on delivery through CS were different across the types of health facilities. For every unit increase in scores of managements of the nearest health facility, likelihoods of delivery through CS among women increased approximately 2.56 times (95% CI, 1.88–4.20) and 1.13 times (95% CI, 1.01–1.64) in private health facilities and non-government health facilities, respectively. Similarly, for every unit increase in infrastructure score of the nearest health facility, the AORs of delivery through CS among women increase up to 1.94 times, with the highest effect for private health facilities. The higher the score of the availability of comprehensive obstetric care services in the nearest private health facilities, the greater the likelihood of (AOR, 3.19; 95% CI, 1.45–4.13) increased delivery through CS among women. The corresponding AORs were 1.21 (95% CI, 1.02–3.25) and 1.27 (95% CI, 1.03–1.63) for the availability scores in governmental and non-governmental health facilities, respectively. Women accessing private health facilities that have better readiness to provide comprehensive obstetric care were 3.06 times (95% CI, 1.34–4.13) more likely to perform delivery through CS. For the government and non-governmental health facilities, the corresponding AORs were 1.38 (95% CI, 1.13–1.98) and 2.06 (95% CI, 1.14–3.26), respectively.
Table 3.
Multilevel logistics regression assessing the relationship of delivery through caesarean section and characteristics of the health facilities.
| Health facility characteristics | Caesarean section use, AOR (95% CI) |
||
|---|---|---|---|
| Government health facility | Private health facility | Non-government health facility | |
| General health service readiness | |||
| Health facility management system | 1.06 (0.80–1.98) | 2.56 (1.88–4.20)∗∗ | 1.13 (1.01–1.64)∗∗ |
| Health facility infrastructure | 1.42 (1.02–1.84)∗ | 1.94 (1.07–2.24)∗∗ | 1.80 (1.03–2.13)∗∗ |
| Comprehensive obstetric care availability in health facility | 1.21 (1.02–3.25)∗ | 3.19 (1.45–4.13)∗∗ | 1.27 (1.03–1.63)∗∗ |
| Health facility readiness to provide comprehensive obstetric care | 1.38 (1.13–1.98)∗∗ | 3.06 (1.34–4.13)∗∗ | 2.06 (1.14–3.26)∗∗ |
Note: All three models were adjusted for women's age, educational attainment, employment status, number of children ever given birth, intervals between the most recent two births, family types, household wealth quintile, place of residence and administrative region, husbands' educational attainment, and occupation. ∗∗p < 0.01, ∗p < 0.05.
Discussion
Our findings suggest that over 33% of women in Bangladesh underwent CS with a considerable regional variation. The hotspots of CS delivery were primarily located in urban areas of Dhaka, Khulna, and Rajshahi divisions. In contrast, cold spots were located in parts of Chattogram, Barishal, and Sylhet divisions. The likelihood of women undergoing CS significantly increased with the increased scores of the nearest health facilities in terms of management, infrastructure, availability and readiness to deliver comprehensive obstetric care. To ensure the robustness of our study findings, we adjusted for a range of potential confounders and used advanced statistical modelling. Also, to our knowledge, analysis of linked data of the health facility survey and the population-level survey to examine clusters of CS use in the context of LMICs is scarce.
Previous studies in Bangladesh that used the data collected in 2016 or earlier reported a lower national rate of CS delivery (<24%) than our observed rate (33%).11,15,18 However, these percentages were higher than the recommended CS delivery rate (5–15%).32 It is concerning that the CS delivery rates in some divisions were even higher than the national average. According to a Save the Children Bangladesh report, there was a 51% increase in CS delivery between 2016 and 2017, indicating a rapid rise.4,33 Another previous study reported CS delivery rate was as high as 50% among women who delivered their most recent babies in urban health facilities25 and the remaining 50% had homebirth, and a significant percentage of the latter group could not access CS services, although for some of them access to CS services was deemed necessary.17 This malpractice is difficult to overcome without the active cooperation of the healthcare facilities, ethical use of such lifesaving clinical procedures, and strict regulations against the unnecessary use of CS.34
In Bangladesh, CS is available in all three types of health facilities: governmental, private, and non-governmental with a uniform guideline to perform CS delivery when it is required for medical reasons.1,35 Like other studies, we found that CS delivery was higher in urban settings and particularly in private health facilities.35,36 The reasons, as the literature suggests, are manifold and include (i) proximity (located close to communities), (ii) improved management and infrastructure and (iii) readiness to provide comprehensive obstetric care.35,37 Our findings confirm these multidimensional factors regarding private facilities and are consistent with the findings of a study conducted in Ethiopia.6 Private facilities are often blamed for inefficient quality control, poor ethical standards, and profit motives.37 While profit motives and associated ethical standards of private facilities are understandable, the reasons for the poor quality of services remain unclear. However, it is likely that their better infrastructures and readiness for services together with strong profit motives led to the surge in CS delivery rate in urban areas across the country.13 In addition, around 36% of women who were admitted to public health facilities reported to have had CS deliveries. Such a relatively higher rate of CS delivery in public facilities might be attributed to complicated delivery referrals from private and non-governmental facilities, as often public facilities are the key referral centres to manage complicated delivery cases.13,38,39 Further research is needed to identify the precise reasons for this.
Evidence suggests that the rapid increase in facility-based CS delivery, particularly in LMICs like Bangladesh, to a large extent, is associated with the preference of health professionals and/or pregnant women.8,35,38 Despite having no medical emergencies, some health professionals are known to prefer performing CS for their personal and organizational benefits, such as financial incentives and organizational profits. Other reasons for preferring CS include lack of trained supporting staff (such as midwives), saving time for other emergency cases, etc.2,8,12, 13, 14,35,40 Government healthcare facilities often have a shortage of trained healthcare providers for obstetric care and/or the available healthcare providers are primarily engaged in handling complicated cases that are referred from private and non-governmental health facilities.13 Moreover, skilled healthcare providers are mostly unavailable during after-hours in the subdistrict- and union-level health facilities.18 As a result, many women are referred to district-level government hospitals or private hospitals and where they ultimately receive CS. Excessive demand for CS delivery services and crowdedness in district-level government health facilities also influence admission to private health facilities where the rate of CS is relatively high.1 Therefore, strengthening the emergency obstetric services at the government healthcare facilities and making them more available at the community level are likely to reduce unnecessary CS delivery services induced by private facilities. Increasing the number of midwives in health facilities may reduce unnecessary CS delivery. Currently, there is a shortage of trained midwives in Bangladesh, with only 1200 midwives countrywide.41 Furthermore, many pregnant women, particularly urban-educated women, are sometimes motivated by their health professionals to choose CS delivery as the preferred method to avoid the pain of normal delivery and the impact of vaginal delivery on physical appearances and sexual functionality.42, 43, 44 Evidence-informed counselling services for pregnant women on their birth preferences need to be implemented to empower women to make informed decisions regarding their childbirths.
The findings of our study indicates that both population-level and health facility-level factors contribute to the rise in CS delivery in Bangladesh. Like other studies in LMICs, women of a relatively high age-group (aged > 30) and who had longer birth intervals in the most recent two live births were more likely to undergo CS than others.45,46 These characteristics were associated with an increased risk of complications during pregnancy and delivery, which might have motivated some women to prefer CS delivery to normal vaginal delivery.45,46 It is also reasonable that women who gave few live births are more likely to use CS, as more than two CS operations are not recommended due to the additional risks involved.47 Our findings also suggest that having more years of formal education leads to a greater likelihood of delivery through CS among women. This observation is understandable, as education is connected with a range of other factors that can lead to using CS, including women's agency for decision-making and perceived safety.48 Also, educated women are more likely to be aware of their existing medical conditions e.g., obesity, diabetes and hypertension.13 Our findings showed that women who were employed in the formal sector were less likely to undergo CS. However, it is difficult to justify the underlying reasons for this. Further research on women's perspectives in choosing CS over vaginal childbirth is required to develop a better understanding in this regard.
This study revealed the hotspots of delivery through CS are mostly located in the Rajshahi, Khulna and Dhaka divisions, where the rates of CS births are more than 43%. Previous studies in Bangladesh also reported similar rates in these three divisions.11,17,18 It is reasonable to have a relatively higher rate of CS delivery in the Dhaka division, the capital city, where delivery through CS has always been high. One possible explanation for the relatively higher rates of CS delivery in Rajshahi and Khulna is the availability of CS-providing healthcare facilities in these locations. Further research is needed to identify the significant factors that influence relatively higher CS rates in those divisions.
This study has several strengths and limitations. To our knowledge, this is the first study in the context of Bangladesh and other LMICs that explored the hotspots and cold spots of CS delivery and determined the effects of health facility- and population-level factors.14,17,18,40 A comprehensive list of explanatory variables was considered in this study and these were selected carefully through a literature review of the published papers and included in the models through proper model-building techniques. They were summarised in three broad themes, i.e. health facility-level, community-level, household-level and individual-level factors, as per the socio-ecological model of health. However, many other factors, such as existing chronic conditions, complications during pregnancy, and gravidity, are important predictors of undergoing CS. Therefore, it is important to adjust them in the model. However, we could not do that because of the lack of relevant data in the survey we analysed. Another major limitation of this study is that the data we used were from cross-sectional surveys; therefore, the variables considered in the analyses were different time events. For instance, all variables considered were recorded for the time of the survey conducted, whereas CS delivery occurred within three years prior to the survey. Because of these time variations in recording relevant information, the findings are correlational only, not casual.
In addition, to protect the privacy of the participants, the BDHS displaced the cluster location up to 5 km for the urban sample and 2 km for the rural sample. For a further 2% of the sample, the cluster locations were displaced up to 10 km. Thus, the cluster locations we showed on the map were slightly different from the actual locations. However, during displacing, BDHS ensured that the displaced locations were placed within the same administrative boundary. Hence, the findings reported in this study are valid for administrative divisions and, therefore, can be used for developing divisional-level policies and programs. Also, BHFS had included only the government-registered private health facilities, which we included in this study. Moreover, health facility readiness scores were generated based on the availability of equipment for CS delivery and their useable status and health facility capacity scores to provide services. However, the availability of equipment does not always indicate their functionality, particularly in LMICs, where equipment may not be used for many reasons, including lack of workforce and other logistic supports. This is particularly true for health facilities located in rural and remote areas. The survey did not have any data to determine the functionality of the equipment available. Similarly, data on the availability of full-time anaesthetic consultants (associated with obstetrics and gynaecology) and registered nurses/midwives were not available in the survey. We, therefore, could not adjust for these factors in the analyses. In this study, however, we considered CS-performing health facilities only that were located in the urban and semi-urban areas. Therefore, the findings of this study are still valid and provide an important understanding of the effects of health facility readiness on performing CS delivery. Apart from multiple births, some other factors such as breech pregnancies, previous CS, preterm birth, eclampsia and other obstetric complications are risk factors for performing CS. However, we could not consider these factors because data were not available. Also, in some countries, health insurance coverage was found to be an important predictor of performing CS delivery, but we could not include this variable in our analysis due to data unavailability in the dataset we used. Since health insurance is rare in Bangladesh, we can assume that its impact is unlikely to be substantial. It is possible that a small subset of CS delivery was attributed to a lack of skilled health professionals such as midwives. However, we could not examine this as no information was available in the dataset. Finally, CS is a life-saving procedure when it is performed in medical necessity. Profit motives of some health care facilities and providers increased its undue use. It is critical to know the reasons for its use to understand the extent and nature of CS delivery and its predictors. However, these information were also not available in the datasets.
This study found that 33% of women underwent CS in Bangladesh with a significant variation across divisions. The hotspots of CS delivery were located mainly in the Rajshahi, Dhaka and Khulna divisions, where the prevalence of CS delivery was more than 43% (higher than the national average rate of CS delivery). Health facility-level factors, including improved healthcare facility management and infrastructure and availability and readiness of providing comprehensive obstetric care, are significantly associated with increased delivery through CS. These relationships were strong for private health facilities, where more than 80% of CS delivery was performed. Higher maternal age and more than four-year intervals between the two most recent pregnancies were associated with an increased likelihood of CS delivery. Besides, women who were employed or had more than two children were less likely to undergo CS delivery. The likelihood of undergoing CS increased with longer years of education as well as improved wealth status. Ensuring the availability of skilled healthcare providers including midwives at public healthcare facilities to perform normal vaginal birth and strict government-level monitoring on reasons for performing each CS are recommended. Programmes to create awareness among women on their childbirth options and associated consequences are required to help women make informed decisions regarding choosing CS over normal vaginal births. It is also crucial to know the perspectives of healthcare providers performing CS in public and private facilities that will assist in designing effective policies to reduce avoidable CS. Active participation of health professionals performing CS and pregnant women in decision-making based on scientific evidence can contribute to reducing avoidable CS in Bangladesh.
Contributors
Khan MN designed the study, performed the data analysis, and wrote the first draft of this manuscript. Islam MM and Akter S critically reviewed and edited the previous versions of this manuscript. All authors approved this final version of the manuscript.
Data sharing statement
The datasets used and analysed in this study are available from the Measure DHS website: https://dhsprogram.com/data/available-datasets.cfm.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
None.
Acknowledgment
The authors thank the MEASURE DHS for granting access to the 2017/18 BDHS and 2017 BHFS data.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100153.
Appendix A. Supplementary data
References
- 1.Khan M.N., Kabir M.A., Shariff A.A., Rahman M.M. Too many yet too few caesarean section deliveries in Bangladesh: evidence from Bangladesh demographic and health surveys data. PLoS Global Public Health. 2022;2(2) doi: 10.1371/journal.pgph.0000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Betran A., Torloni M.R., Zhang J., et al. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–670. doi: 10.1111/1471-0528.13526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ye J., Zhang J., Mikolajczyk R., Torloni M.R., Gülmezoglu A., Betran A. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG. 2016;123(5):745–753. doi: 10.1111/1471-0528.13592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Betran A.P., Ye J., Moller A.-B., Souza J.P., Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Global Health. 2021;6(6) doi: 10.1136/bmjgh-2021-005671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boerma T., Ronsmans C., Melesse D.Y., et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–1348. doi: 10.1016/S0140-6736(18)31928-7. [DOI] [PubMed] [Google Scholar]
- 6.Tegegne T.K., Chojenta C., Getachew T., Smith R., Loxton D. Caesarean delivery use in Ethiopia: a spatial and hierarchical Bayesian analysis. PLoS One. 2021;75(12) doi: 10.1371/journal.pone.0277885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Betrán A.P., Ye J., Moller A.-B., Zhang J., Gülmezoglu A.M., Torloni M.R. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016;11(2) doi: 10.1371/journal.pone.0148343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boatin A.A., Schlotheuber A., Betran A.P., et al. Within country inequalities in caesarean section rates: observational study of 72 low and middle income countries. BMJ. 2018;360:k55. doi: 10.1136/bmj.k55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Betran A.P., Temmerman M., Kingdon C., et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018;392(10155):1358–1368. doi: 10.1016/S0140-6736(18)31927-5. [DOI] [PubMed] [Google Scholar]
- 10.National Institute of Population Research and Training (NIPORT) and ICF . NIPORT, ACPR, and ICF; Dhaka, Bangladesh: 2005. Bangladesh demographic and health survey 2004. [Google Scholar]
- 11.Haider M.R., Rahman M.M., Moinuddin M., Rahman A.E., Ahmed S., Khan M.M. Ever-increasing caesarean section and its economic burden in Bangladesh. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0208623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zbiri S., Rozenberg P., Goffinet F., Milcent C. Cesarean delivery rate and staffing levels of the maternity unit. PLoS One. 2018;13(11) doi: 10.1371/journal.pone.0207379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mia M.N., Islam M.Z., Chowdhury M.R., Razzaque A., Chin B., Rahman M.S. Socio-demographic, health and institutional determinants of caesarean section among the poorest segment of the urban population: evidence from selected slums in Dhaka, Bangladesh. SSM Popul Health. 2019;8 doi: 10.1016/j.ssmph.2019.100415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasan F., Alam M.M., Hossain M.G. Associated factors and their individual contributions to caesarean delivery among married women in Bangladesh: analysis of Bangladesh demographic and health survey data. BMC Pregnancy Childbirth. 2019;19(1):1–9. doi: 10.1186/s12884-019-2588-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rukhsana K.F. The Royal Tropical Institute; Amsterdam, The Netharlands: 2016. Factors affecting the increased rates of caesarean section in Bangladesh. [Google Scholar]
- 16.Rahman M., Shariff A.A., Shafie A., Saaid R., Tahir R.M. Caesarean delivery and its correlates in Northern Region of Bangladesh: application of logistic regression and cox proportional hazard model. J Health Popul Nutr. 2015;33(1):1–11. doi: 10.1186/s41043-015-0020-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan M.N., Islam M.M., Rahman M. Inequality in utilization of cesarean delivery in Bangladesh: a decomposition analysis using nationally representative data. Public Health. 2018;157:111–120. doi: 10.1016/j.puhe.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Khan M.N., Islam M.M., Shariff A.A., Alam M.M., Rahman M.M. Socio-demographic predictors and average annual rates of caesarean section in Bangladesh between 2004 and 2014. PLoS One. 2017;12(5) doi: 10.1371/journal.pone.0177579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ologunde R., Vogel J.P., Cherian M.N., Sbaiti M., Merialdi M., Yeats J. Assessment of cesarean delivery availability in 26 low-and middle-income countries: a cross-sectional study. Am J Obstet Gynecol. 2014;211(5):504. doi: 10.1016/j.ajog.2014.05.022. e1–e12. [DOI] [PubMed] [Google Scholar]
- 20.Panda B.K., Nayak I., Mishra U.S. Determinant of inequality in cesarean delivery in India: a decomposition analysis. Health Care Women Int. 2020;41(7):817–832. doi: 10.1080/07399332.2020.1711757. [DOI] [PubMed] [Google Scholar]
- 21.Amjad A., Amjad U., Zakar R., Usman A., Zakar M.Z., Fischer F. Factors associated with caesarean deliveries among child-bearing women in Pakistan: secondary analysis of data from the demographic and health survey, 2012–13. BMC Pregnancy Childbirth. 2018;18(1):1–9. doi: 10.1186/s12884-018-1743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Asfaw T., Tesema A. Determinant factors, trend and outcomes of cesarean delivery in Debre Berhan referral hospital, North Shewa Zone, Ethiopia. Pediatr Rep. 2020;12(2):42–45. doi: 10.4081/pr.2020.8430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burgert C.R., Prosnitz D. ICF International; Rockville, Maryland, USA: 2014. Linking DHS household and SPA facility surveys: data considerations and geospatial methods. DHS spatial analysis reports No. 10. [Google Scholar]
- 24.National Institute of Population Research and Training (NIPORT) aI . NIPORT and ICF; Dhaka, Bangladesh, and Rockville, Maryland, USA: 2020. Bangladesh demographic and health survey 2017-18. [Google Scholar]
- 25.2019 NIoPRaTNaI . NIPORT, ACPR, and ICF; Dhaka, Bangladesh: 2019. Bangladesh health facility survey 2017. [Google Scholar]
- 26.Schmitz T., Prunet C., Azria E., et al. Association between planned cesarean delivery and neonatal mortality and morbidity in twin pregnancies. Obstet Gynecol. 2017;129(6):986–995. doi: 10.1097/AOG.0000000000002048. [DOI] [PubMed] [Google Scholar]
- 27.Easter S.R., Robinson J.N., Carusi D., Little S.E. The US twin delivery volume and association with cesarean delivery rates: a hospital-level analysis. Am J Perinatol. 2018;35(4):345–353. doi: 10.1055/s-0037-1607316. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization . World Health Organization; 2010. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. 9241564059. [Google Scholar]
- 29.Tegegne T.K., Chojenta C., Forder P.M., Getachew T., Smith R., Loxton D. Spatial variations and associated factors of modern contraceptive use in Ethiopia: a spatial and multilevel analysis. BMJ Open. 2020;10(10) doi: 10.1136/bmjopen-2020-037532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khan M.N., Harris M., Loxton D. Modern contraceptive use following an unplanned birth in Bangladesh: an analysis of national survey data. Int Perspect Sex Reprod Health. 2020;46:77–87. doi: 10.1363/46e8820. [DOI] [PubMed] [Google Scholar]
- 31.Khan M.N., Harris M.L., Loxton D. Assessing the effect of pregnancy intention at conception on the continuum of care in maternal healthcare services use in Bangladesh: evidence from a nationally representative cross-sectional survey. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0242729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization . World Health Organization; 2015. WHO statement on caesarean section rates.https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf [Google Scholar]
- 33.Save the Children Bangladesh: 51% increase in “unnecessary” C-section in two years. 2018. https://www.savethechildren.net/news/bangladesh-51-cent-increase-“unnecessary”-c-sections-two-years Dhaka, Bangladesh.
- 34.Dumont A., Guilmoto C.Z. Too many yet too few: the double burden of caesarean births. Popul Soc. 2020;581(9):1–4. [Google Scholar]
- 35.Neuman M., Alcock G., Azad K., et al. Prevalence and determinants of caesarean section in private and public health facilities in underserved South Asian communities: cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open. 2014;4(12) doi: 10.1136/bmjopen-2014-005982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kingdon C., Downe S., Betran A.P. Women's and communities' views of targeted educational interventions to reduce unnecessary caesarean section: a qualitative evidence synthesis. Reprod Health. 2018;15(1):1–14. doi: 10.1186/s12978-018-0570-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.UNICEF Bangladesh: 51 percent increase in “unnecessary” C-section in two years. 2018. https://www.savethechildren.net/news/bangladesh-51-cent-increase-“unnecessary”-c-sections-two-years UNICEF, Dhaka, Bangladesh.
- 38.Andaleeb S.S. Public and private hospitals in Bangladesh: service quality and predictors of hospital choice. Health Policy Plan. 2000;15(1):95–102. doi: 10.1093/heapol/15.1.95. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization . WHO Regional Office for the Western Pacific; Manila: 2015. Bangladesh health system review. [Google Scholar]
- 40.Rahman M.M., Haider M.R., Moinuddin M., Rahman A.E., Ahmed S., Khan M.M. Determinants of caesarean section in Bangladesh: cross-sectional analysis of Bangladesh demographic and health survey 2014 data. PLoS One. 2018;13(9) doi: 10.1371/journal.pone.0202879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bogren M., Erlandsson K., Byrskog U. What prevents midwifery quality care in Bangladesh? A focus group enquiry with midwifery students. BMC Health Serv Res. 2018;18(1):1–9. doi: 10.1186/s12913-018-3447-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Edmonds J.K., Cwiertniewicz T., Stoll K. Childbirth education prior to pregnancy? Survey findings of childbirth preferences and attitudes among young women. J Perinat Educ. 2015;24(2):93–101. doi: 10.1891/1058-1243.24.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Torloni M.R., Betrán A.P., Montilla P., et al. Do Italian women prefer cesarean section? Results from a survey on mode of delivery preferences. BMC Pregnancy Childbirth. 2013;13(1):1–8. doi: 10.1186/1471-2393-13-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mi J., Liu F. Rate of caesarean section is alarming in China. Lancet. 2014;383(9927):1463–1464. doi: 10.1016/S0140-6736(14)60716-9. [DOI] [PubMed] [Google Scholar]
- 45.Islam M., Sultana N. Risk factors for pregnancy related complications among urban slum and non-slum women in Bangladesh. BMC Pregnancy Childbirth. 2019;19(1):1–7. doi: 10.1186/s12884-019-2392-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Islam M., Chowdhury R., Chakraborty N., Bari W., Akhter H. Factors associated with delivery complications in rural Bangladesh. Eur J Contracept Reprod Health Care. 2004;9(4):203–213. doi: 10.1080/13625180400017438. [DOI] [PubMed] [Google Scholar]
- 47.Zwergel C., von Kaisenberg C.S. IntechOpen; 2019. Maternal and fetal risks in higher multiple cesarean deliveries. Recent advances in cesarean delivery. [Google Scholar]
- 48.Epstein R.M., Gramling R.E. What is shared in shared decision making? Complex decisions when the evidence is unclear. Med Care Res Rev. 2013;70(1_suppl):94S–112S. doi: 10.1177/1077558712459216. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.