Abstract
With the current massive increases in drug-resistant microbial infection as well as the significant role of fungal infections in the death toll of COVID-19, discovering new antifungals is extremely important. Natural and synthetic xanthones are promising derivatives, although only few reports have demonstrated their antifungal mechanism of action in detail. Newly synthetized by us xanthone derivative 44 exhibited strong antifungal activity against reference and fluconazole resistant C. albicans strains. Our results indicate that the most active compounds 42 and 44 are not substrates for fungal ABC transporters (Cdr1p and Cdr2p) and Mdr1p, the main representative of the major facilitator superfamily efflux pumps, membrane proteins that are responsible for the development of resistance. Moreover, fungicidal mode of action reduces the probability of persistent or recurrent infections and resistance development. In this light, the demonstrated killing activity of the examined derivatives is their undoubted advantage. Novel synthesized compounds exhibited moderate cytotoxicity against human cell lines, although the selectivity index value for human pathogenic strains remained favourable. Our results also indicate that novel synthetized compounds 42 and 44 with antifungal activity target yeast topoisomerase II activity. In summary, further validation of xanthones applicability as antifungals is highly valuable.
Subject terms: Drug discovery, Microbiology, Chemistry
Introduction
Fungal microorganisms are etiological factors of severe, often deadly, infectious diseases, especially in immunocompromised patients. The number of these patients is growing rapidly, not only because of diseases resulting in immunodeficiency, like AIDS but also as a consequence of the frequent use of therapies that affect the human immune defense system (e.g.anticancer therapy with cytostatics, steroid therapy, use of the immunosuppressive agents in transplant patients). Systemic mycoses are caused in these patients mainly by yeast-like microorganisms from the Candida genus, especially Candida albicans and Candida glabrata, and filamentous fungi from the Aspergillus genus1. On the other hand, many fungal microorganisms are known as one of the most frequent reasons of nosocomial infections. C. albicans is considered the fourth most popular etiological agent of nosocomial infections worldwide. Moreover, chemotherapeutics used in clinical treatment have become factors stimulating the selection of resistant cells. A newly described pathogen, Candida auris, is an emerging multidrug-resistant organism that poses a global threat2. Additionally, invasive fungal infections complicate the clinical course of COVID-19 and are associated with a significant increase in mortality, especially in critically ill patients admitted to an intensive care unit3. Thus, with the current massive increases in drug-resistant microbial infections as well as the significant role of fungal infections in the death toll of COVID-19, discovering new antifungal compounds is extremely important.
There are several approaches in novel drug discovery. First of all, researchers are looking for new drugs targeting old pathways (e.g., ergosterol synthesis)4 or cell membranes5, while others are trying to find out new solutions. The biosynthesis of fungal proteins, DNA, and other essential molecules is extremely important6,7. As long as new targets are concerned, our group is looking for new drugs targeting fungal topoisomerases. Significant work has been done on the structure and function of topoisomerase I and II in fungi and results indicated that their activities are crucial for some specific strains8–10. Moreover, inhibition of yeast topoisomerase II resulted in antifungal activity11,12 and even managed to overcome fluconazole-resistance13,14.
Natural xanthone derivatives are a promising group of antifungal compounds15–17. They are present in nature as metabolites of various plant, lichen, fungal, and bacterial species18,19. The interesting structural scaffold and biological efficacy of those compounds lead many scientists to synthesize xanthone derivatives for the development of new prospective drug candidates as anticancer, antimicrobial, antimalarial, anti-HIV, antioxidant, anti-inflammatory, and antimalarial agents20. Several articles have been published highlighting the antifungal activity of synthetic xanthone analogues15,21–23, although only a few have been examined thoroughly in order to define their mechanism of action. According to previous reports, 1,2-dihydroxyxanthone is the most active compound against all fungal strains tested, showing its effect on sterol biosynthesis by reducing the amount of ergosterol detected24.
Emerging from previous studies performed for xanthone analogues as potential antimicrobials15–24, we have decided to analyze the antifungal activity of four new groups of compounds. As xanthone derivatives with anticancer activity are reported to be effective human topoisomerase inhibitors20, we have also analyzed the inhibitory effect of selected derivatives on yeast topoisomerase II activity (yTOPO II).
Results and discussion
Synthesis of xanthone derivatives
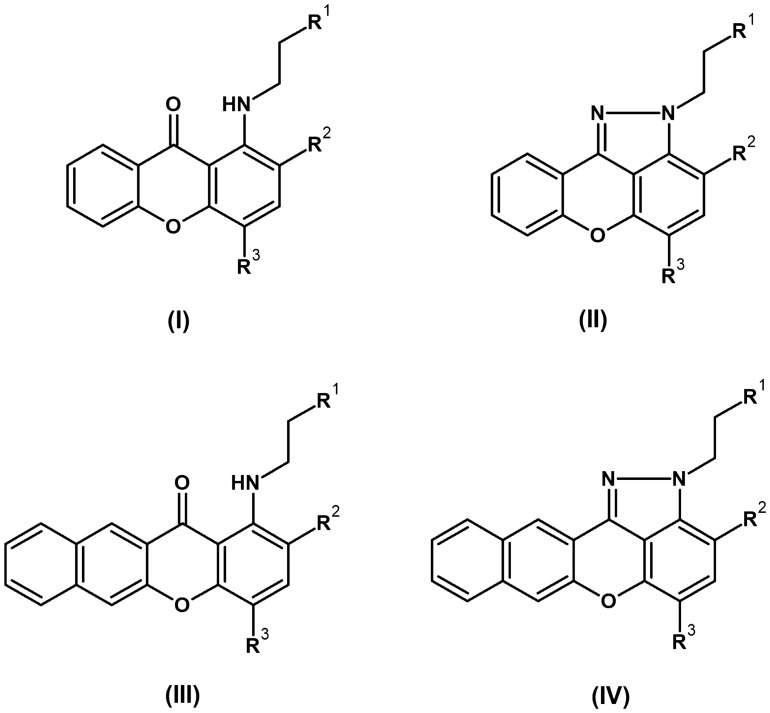
The structures of xanthone derivatives synthesized in this study are divided into four groups (Fig. 1). Compounds 1–16 and 34 were prepared according to a previously published procedure25,26, while 25, 26, 35–38, and 41–45 are newly synthesized analogues (Table 1). These groups (I–IV) differ in the nitro or amino substitution and the presence of a pyrazole or a benzene fused ring on the xanthone core (Fig. 1).
Figure 1.
Overall structures of derivatives that were analysed in this study. R1—aminosubstitution, R2 or R3—NO2 or H.
Table 1.
The list of xanthone (group I and II) and benzoxanthone (group III and IV) analoques.
| Compound | R1 | R2 | R3 |
|---|---|---|---|
| Group (I) | |||
| 1 | N(CH2CH3)2 | H | NO2 |
| 2 | N(CH2CH3)2 | H | H |
| 3 |  |
H | NO2 |
| 4 |  |
H | H |
| 25 | N(CH2CH3)2 | NO2 | H |
| 26 |  |
NO2 | H |
| Group (II) | |||
| 5 |  |
H | H |
| 6 |  |
H | NO2 |
| 7 | N(CH2CH3)2 | H | NO2 |
| 8 | N(CH3)2 | H | H |
| Group (III) | |||
| 9 |  |
H | NO2 |
| 10 | N(CH2CH3)2 | H | NO2 |
| 11 | N(CH3)2 | H | H |
| 34 |  |
NO2 | H |
| 35 | OCH2CH2OH | H | NO2 |
| 36 | CH2OH | H | NO2 |
| 37 | OH | H | NO2 |
| 38 | CH2OCH3 | H | NO2 |
| 41 |  |
H | NO2 |
| 42 |  |
H | NO2 |
| 43 |  |
H | NO2 |
| 44 |  |
H | NO2 |
| 45 |  |
H | NO2 |
| Group (IV) | |||
| 12 |  |
H | H |
| 13 | N(CH2CH3)2 | H | NO2 |
| 14 |  |
H | NO2 |
| 15 |  |
H | H |
| 16 | N(CH2CH3)2 | H | NO2 |
The list of xanthone and benzoxanthone analogues analyzed in this study is presented in Table 1.
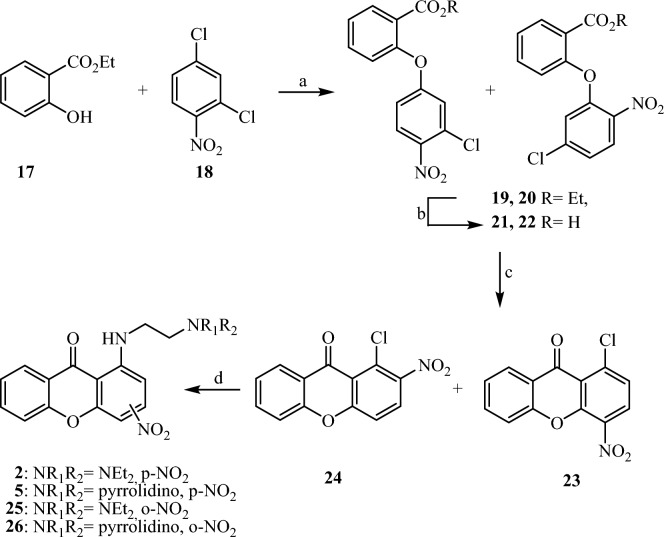
For the synthesis of the new compounds we have used an analogous synthetic procedure, with slight alterations (Figs. 2 and 3). Briefly, the reaction of ethyl salicylate (17) or ethyl 3-hydroxy-2-napthoate (27) with 2,4-dichloronitrobenzene (18) afforded a mixture of the isomeric diarylethers 19, 20 and 28, 29 respectively. Trituration of both mixtures with methanol resulted in pure 20 and 29, while we obtained a 1/1 mixture of 19, 20, and 28, 29, which could not be further purified . For the synthesis of the ortho-substituted amines 25, 26 and 34, each of the above mixtures was saponified under mild conditions. Without further purification, the resulting mixture of acids 21, 22, and 30, 31, was ring closed upon treatment with polyphosphoric acid (PPA) to afford nitro compounds 23, 24, and 32, 33 respectively, as inseparable mixtures. Reaction of the above mixtures with the suitable amines resulted in the aminoderivatives 2, 5, 25, 26, and 9, 34 respectively. Each aminoderivative was isolated in pure form by column chromatography and identified by means of 1H and 13C spectral data, using both direct and long-range experiments (HMBC and HMQC). In order to prepare the corresponding p-substituted nitro derivatives 35–38 and 41–45, ethyl ester 29 was saponified and ring closed upon treatment with PPA to afford the nitrosubstituted benzoxanthone 32 in pure form. Consequently, the amino derivatives 35–38 were prepared upon nucleophilic substitution of the chloro group of 32 by the appropriately substituted amines. For the synthesis of amines 41–45, compounds 37 and 38 were converted to the mesylates 39 and 40, which were treated with the appropriately substituted amines to result in the amino derivatives 41–43 and 44–45, respectively.
Figure 2.
Reaction and conditions: (a) K2CO3, Cu2O, DMF dry, 110 °C; (b) NaOH 40%, EtOH, rt; (c) PPA, 110 °C; (d) suitable amine, pyridine, reflux.
Figure 3.
Reaction and conditions: (a) K2CO3, Cu2O, DMF dry, 110 °C; (b) NaOH 40%, EtOH, rt; (c) PPA, 110 °C; (d) suitable amine, pyridine, reflux; (e) suitable amine, pyridine, reflux; (f) MsCl, Et3N, THF, rt; (g) suitable amine, EtOH, reflux.
Susceptibility testing of novel compounds against fungal strains
All 28 derivatives were tested for their in vitro antifungal activity against five reference fungal strains (from American Type Culture Collection, ATCC) (Table 2). The most active 13 compounds were tested against six C. albicans clinical isolates, sensitive (B3, Gu4 and F2) and resistant (B4, Gu5 and F5) to fluconazole27,28 (Table 3). Minimal inhibitory concentrations (MICs) of the studied compounds were determined by the microplate serial dilution method29.
Table 2.
Antifungal activity against reference strains. MIC90, minimal inhibitory concentration—a concentration that inhibits 90% of fungal cell growth.
| Compound | *MIC90 µg mL−1 | ||||
|---|---|---|---|---|---|
| Candida albicans ATCC 10231 | Candida glabrata ATCC 90030 | Candida krusei ATCC 6258 | Candida parapsilosis ATCC 22019 | Saccharomyces cerevisiae ATCC 9763 | |
| 1 | 32 | 32 | 32 | > 64 | 16 |
| 2 | > 64 | > 64 | 64 | 32 | 32 |
| 3 | 16 | 16 | 16 | 64 | 8 |
| 4 | > 64 | > 64 | 64 | 64 | 64 |
| 5 | 16 | > 64 | 32 | 32 | 32 |
| 6 | 16 | 8 | 16 | > 64 | 8 |
| 7 | 16 | 16 | 16 | > 64 | 16 |
| 8 | 32 | 64 | 32 | 32 | 16 |
| 9 | 4 | 4 | 4 | 8 | 4 |
| 10 | > 16 | > 16 | > 16 | > 16 | > 16 |
| 11 | > 64 | > 64 | > 64 | > 64 | > 64 |
| 12 | 8 | > 64 | 8 | > 64 | 8 |
| 13 | 8 | 4 | 4 | 16 | 2 |
| 14 | 8 | 4 | 4 | 16 | 4 |
| 15 | 8 | 32 | 8 | 64 | 4 |
| 16 | 32 | 16 | 8 | 32 | 16 |
| 25 | > 64 | > 64 | > 64 | 64 | 64 |
| 26 | > 64 | > 64 | 64 | 64 | 64 |
| 34 | 32 | > 32 | 8 | > 32 | 8 |
| 35 | > 64 | > 64 | > 64 | > 64 | > 64 |
| 36 | > 64 | > 64 | > 64 | > 64 | > 64 |
| 37 | > 64 | > 64 | > 64 | > 64 | > 64 |
| 38 | > 64 | > 64 | > 64 | > 64 | > 64 |
| 41 | > 64 | > 64 | > 64 | > 64 | > 64 |
| 42 | 8 | 4 | 4 | 8 | 4 |
| 43 | > 64 | > 64 | > 64 | > 64 | > 64 |
| 44 | 4 | 2 | 2 | 4 | 2 |
| 45 | 32 | 32 | 32 | 32 | 32 |
| Amphotericin B | 0.5 | 1 | 1 | 1 | 0.5 |
* > Means no activity at the concentration mentioned. In this assay, the MIC90 value of amphotericin B was recorded as a positive control. The experiments were performed in three replicates.
Table 3.
Antifungal activity of selected derivatives against clinical strains in comparison with C. albicans ATCC 10231.
| Compound | *MIC90 µg mL−1 | ||||||
|---|---|---|---|---|---|---|---|
| Candida albicans ATCC 10231 | Candida albicans B3 | Candida albicans B4 | Candida albicans Gu4 | Candida albicans Gu5 | Candida albicans F2 | Candida albicans F5 | |
| 3 | 16 | 16 | 32 | 16 | 32 | 16 | 32 |
| 5 | 16 | 64 | 64 | 64 | 64 | 32 | 64 |
| 6 | 16 | 16 | 64 | 16 | 64 | 32 | 32 |
| 7 | 16 | 32 | 64 | 32 | 32 | 32 | 32 |
| 8 | 32 | 32 | 32 | 32 | 32 | 32 | 32 |
| 9 | 4 | 8 | 8 | 8 | 8 | 8 | 8 |
| 12 | 8 | 64 | 64 | 64 | 64 | > 64 | > 64 |
| 13 | 8 | 16 | 16 | 16 | 16 | 16 | 16 |
| 14 | 8 | 16 | 16 | 8 | 8 | 8 | 8 |
| 15 | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| 42 | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| 44 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| 45 | 32 | 64 | 64 | 64 | 64 | 64 | 64 |
| Fluconazole | 8 | 1 | 16 | 4 | > 64 | 8 | > 64 |
* > Means no activity at the concentration mentioned. In this assay, the MIC90 value of fluconazole was recorded as a positive control. The experiments were performed at least in three replicates.
As reported in Table 2, the most active against reference strains from group III is derivative 9, and from group IV compounds 13–15, although it depends on the strain for the latter. Structure activity relationship analysis revealed that the presence of the naphthalene ring as well as the nitro group at R3 position (Fig. 1) is crucial for the antifungal activity. Thus, we decided to synthesize additional derivatives of compound 9 (35–38 and 41–45). This approach allowed us to obtain a derivative with even better antifungal activity (44) against reference strains than starting derivative 9.
For the most active compounds, MIC90 was also determined against six C. albicans clinical isolates, sensitive (B3, Gu4, and F2) and resistant (B4, Gu5, and F5) to fluconazole.
The FLU-resistant clinical C. albicans B4, Gu5 and F5 strains were sensitive to all selected by us derivatives (Table 3). For some of these derivatives at the same level as their FLU-sensitive counterparts B3, Gu4 and F2 while for other MICs are higher for FLU-resistant cells but still measurable. The most active against reference strains compounds: 9 as well as 42, 44 and 13–15 also exhibited the highest antifungal activity against clinical strains, including those FLU-resistant. Interestingly, antifungal activity of compound 15 against reference strains C. glabrata as well as C. parapsilosis is not significant (Table 2) but was found to be very active against clinical C. albicans strains, both sensitive and resistant. Strains Gu4, B3 and F2 are fluconazole-sensitive isolates obtained from early infection episodes, while Gu5, B4 and F5 are the corresponding fluconazole-resistant isolates obtained from later episodes in the same patients treated with fluconazole27,28. In the case of Gu5, the lack of susceptibility to fluconazole is a consequence of overexpression of CDR1/2 genes encoding ABC transporters, whereas the resistance of B4 and F5 strain is caused by overexpression of MDR1 gene encoding a membrane transport protein of the major facilitator superfamily (MFS)27,28. Our results indicate that the most active compounds 9, 13–15, 42 and 44 are not substrates for pumps that efflux drugs from resistant cells and their antifungal activity does not depend on the type of overexpressed pumps.
Molecular mechanism of antifungal activity
Killing activity of selected derivatives
To establish the possible mode of action of xanthone and benzoxanthone analogues we have analyzed the killing activity and determined the minimal fungicidal concentrations (MFCs) for selected derivatives (Table 4).
Table 4.
Fungicidal activity of selected compounds and amphotericin B (MFC—minimal fungicidal concentration—a concentration that inhibits 99% of fungal cell growth).
| Compound | *MFC µg mL−1 | |||
|---|---|---|---|---|
| Candida albicans ATCC 10231 | Candida glabrata ATCC 90030 | Candida krusei ATCC 6258 | Saccharomyces cerevisiae ATCC 9763 | |
| 1 | 64 | > 128 | > 128 | 16 |
| 2 | > 64 | > 64 | > 64 | 64 |
| 3 | 32 | 128 | 64 | 16 |
| 4 | > 64 | > 64 | > 64 | 64 |
| 5 | 64 | > 128 | 128 | 32 |
| 6 | 32 | 128 | 64 | 8 |
| 7 | 64 | > 128 | 128 | 16 |
| 8 | 64 | > 64 | 64 | 32 |
| 9 | 8 | 8 | 8 | 4 |
| 10 | > 16 | > 16 | > 16 | > 16 |
| 11 | > 64 | > 64 | > 64 | > 64 |
| 12 | > 64 | > 64 | > 64 | > 64 |
| 13 | 32 | 32 | 8 | 16 |
| 14 | 16 | 16 | 8 | 8 |
| 15 | 64 | 64 | 32 | 16 |
| 16 | 64 | 32 | 32 | 32 |
| 25 | > 64 | > 64 | > 64 | > 64 |
| 26 | > 64 | > 64 | > 64 | > 64 |
| 34 | > 32 | > 32 | 32 | 32 |
| 42 | 8 | 8 | 4 | 4 |
| 44 | 4 | 4 | 4 | 2 |
| 45 | 32 | 32 | 32 | 32 |
| Amphotericin B | 2 | 2 | 2 | 2 |
* > Means no 99% killing activity at the concentration mentioned. Higher concentrations have not been tested due to the solubility limitations of some compounds. In this assay, the MFC value of amphotericin B was recorded as a positive control. The experiments were performed at least in three replicates.
Our results indicate that the mode of action of the most active compounds is fungicidal. The higher fungicidal activity was determined for derivatives 9, 42 and 44 from group III and 14 from group IV. The use of fungicidal therapy of invasive candidiasis and candidemia is associated with a higher probability of early therapeutic success. A decreased probability of persistent or recurrent infection and resistance development is also expected. In addition, frequent use of available fungistatic drugs like fluconazole promotes drug resistance30. In this light, the demonstrated killing activity of the examined derivatives is their undoubted advantage.
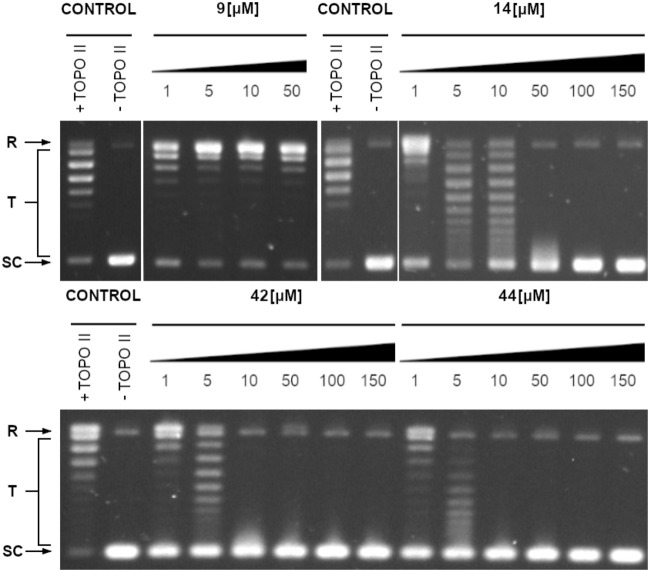
Inhibition of the relaxation activity of yeast topoisomerase II in vitro
The xanthone derivatives act as anticancer agents through several mechanisms of action. The most important are the activation of caspase proteins and the inhibition of protein kinases and topoisomerases31. Due to known activity of xanthone derivatives as human topoisomerase II inhibitors20,31, we decided to evaluate the influence of the six more active compounds on the fungal equivalent of that enzyme. The effect of selected compounds on yeast topoisomerase II-mediated relaxation activity suggests their molecular target (Table 5 and Fig. 4).
Table 5.
The concentrations of selected compounds that totally inhibited yeast topoisomerase II-mediated relaxation activity.
| Compound | Complete inhibition [µM] | IC50 [µM] |
|---|---|---|
| 9 | > 50* | – |
| 13 | > 150 | – |
| 14 | 50 | 18.62 ± 1.81 |
| 15 | > 150 | – |
| 42 | 10 | 5.86 ± 1.07 |
| 44 | 10 | 5.36 ± 1.22 |
For selected compounds IC50—inhibitory concentrations representing a concentration that inhibits 50% of enzyme activity were determined. The experiments were performed at least in three replicates.
*Higher concentrations have not been tested due to the low solubility of the compound.
Figure 4.
Inhibition of the catalytic activity of purified yeast DNA topoisomerase II by compounds 9, 14, 42 and 44 as measured by relaxation. Supercoiled pBR322 plasmid DNA (- TOPO II) was relaxed by purified yeast topoisomerase II in the absence (+ TOPO II) or presence of analyzed compounds 14, 42 and 44 at 1–150 μM concentrations or 1–50 μM for 9 (higher concentrations have not been tested due to the low solubility of the compound). The resulting topological forms of DNA were separated by gel electrophoreses. SC, supercoiled DNA; R, relaxed DNA; T, DNA topoisomers. Data shown are typical of three independent experiments and one set of representative pictures are shown. Original gels are presented in Supplementary Fig. S1.
As reported in Table 5, the most effective inhibitors towards fungal topoisomerase II are compounds 42 and 44. Surprisingly, no inhibition was observed in the tested concentration range for compound 9, the closely related to 42 and 44 derivatives. Thus, the molecular mode of action may vary between these compounds and needs more in depth analysis.
Selectivity in relation to mammalian cells
Selected compounds were screened for their in vitro antiproliferative activity towards a human embryonic kidney cell line (HEK-293) and human liver cancer cell line (HEPG2) using colorimetric MTT assay. Our results were compared with the cytotoxic activity determined previously for human colorectal adenocarcinoma cell line (HT29)26 and are presented in Table 6.
Table 6.
Determination of cytotoxic effect using MTT assay towards HEK293 and HEPG2 cell lines.
| Compound | HEK293 | HEPG2 | HT29 |
|---|---|---|---|
| 9 | 3.64 ± 0.23 | 1.94 ± 0.67 | – |
| 13 | 5.73 ± 1.64 | 1.92 ± 0.85 | 1.85 ± 0.21* |
| 14 | 5.99 ± 1.05 | 4.2 ± 0.71 | 1.83 ± 0.46* |
| 15 | 8.33 ± 0.75 | 2.53 ± 0.82 | 10.7 ± 3.25* |
| 42 | 5.38 ± 0.35 | 4.88 ± 0.31 | – |
| 44 | 3.57 ± 0.25 | 4.94 ± 0.56 | – |
| 45 | 48.47 ± 1.50 | 26.64 ± 2.36 | – |
| Etoposide | 1.91 ± 0.97 | 5.01 ± 0.22 | – |
| Doxorubicin | 6.52 ± 0.13** | – | – |
In vitro growth inhibitory activity of compounds presented as an EC50 ± SD (µM) value—a concentration that inhibits 50% of mammalian cell growth.
*Antiproliferative activity of compounds 13–15 published previously26.
**Antiproliferative activity of doxorubicin published previously32. In this assay, the EC50 value of etoposide was recorded as a positive control.
As indicated for etoposide and doxorubicin32, both chemotherapy drugs used to treat different types of cancers, results obtained for newly synthezised compounds are within acceptable cytotoxicity levels. To estimate the selectivity in relation to mammalian cells mycostatic selectivity index (MSI) for C. albicans ATCC 10231 was calculated as the ratio of EC50 to MIC90 values after converting the MIC90 value to micromolar concentrations. The results are presented in Table 7.
Table 7.
Mycostatic selectivity index values determined for C. albicans ATCC 10231 in relation to mammalian cell lines HEK293 and HEPG2.
| Compound | EC50HEK293/MIC90 | EC50HEPG2/MIC90 |
|---|---|---|
| 9 | 0.400 | 0.213 |
| 13 | 0.314 | 0.105 |
| 14 | 0.327 | 0.229 |
| 15 | 0.408 | 0.124 |
| 42 | 0.300 | 0.272 |
| 44 | 0.375 | 0.518 |
| 45 | 0.655 | 0.360 |
Positive mycostatic selectivity index values (MSI = EC50/MIC90) were obtained for all selected derivatives, ranging from 0.105 to 0.655. Our results indicate the possibility of using xanthone derivatives as efficient antifungal agents. However, it is necessary to improve their selectivity. Compound 44 is the most interesting, for which a higher level of MSI using HEPG2 cells was obtained. The HEPG2 cell line, derived from human liver cancer, is the most commonly used in studies on drug metabolism and toxicity33.
Material and methods
Chemical synthesis
General experimental procedures
All commercially available reagents and solvents were purchased from Alfa Aesar and used without any further purification. Melting points were determined on a Büchi apparatus and were uncorrected. All NMR spectra were recorded on 400 or 600 MHz Bruker spectrometers respectively Avance™ DRX and III instruments (Bruker BioSpin GmbH–Rheinstetten, Germany). 1H NMR (400 and 600 MHz) and 13C NMR (101 and 151 MHz, recorded with complete proton decoupling) spectra were obtained with samples dissolved in CDCl3 or DMSO‐d6 with the residual solvent signals used as internal references: 7.26 ppm for CHCl3, and 2.50 ppm for (CD3)(CD2H)S(O) regarding 1H NMR experiments; 77.2 ppm for CDCl3 and 39.4 ppm for (CD3)2S(O) concerning 13C NMR experiments. Chemical shifts (δ) are given in ppm to the nearest 0.01 (1H) or 0.1 ppm (13C). The coupling constants (J) are given in Hertz (Hz). The signals are reported as follows: (s = singlet, d = doublet, t = triplet, m = multiplet, br = broad). Assignments of 1H and 13C NMR signals were unambiguously achieved with the help of D/H exchange and 2D techniques: COSY, NOESY, HMQC, and HMBC experiments. Compounds 1–8, 10–16 and 34 were synthesized according to literature and their 1H NMR and 13C NMR were compared with those reported into the literature25,26. Flash chromatography was performed on Merck silica gel (40–63 μm) with the indicated solvent system using gradients of increasing polarity in most cases (Merck KGaA—Darmstadt, Germany). The reactions were monitored by analytical thin-layer chromatography (Merck pre-coated silica gel 60 F254 TLC plates, 0.25-mm layer thickness). Compounds were visualized on TLC plates by both UV radiation (254 and 365 nm). All solvents for absorption and fluorescence experiments were of spectroscopic grade. Mass spectra were recorded on a UPLC Triple TOF–MS {UPLC:Acquity of Waters (USA), SCIEX Triple TOF–MS 5600 + (USA)}.
General procedure for the synthesis of amino substituted xanthones 25 and 26
A solution of ethyl salicylate (1.66 g, 10 mmol, 17), 2,4-dichloronitrobenzene (1.91 g, 9.95 mmol, 18), K2CO3 (1.38 g, 10 mmol) and Cu2O (142 mg, 1 mmol) in dry DMF (10 mL) was heated at 110 °C for 12 h, under an argon atmosphere. After completion of the reaction the mixture was filtered hot, washed with EtOAc and the filtrate was vacuum evaporated. The oily residue was diluted in CH2Cl2, washed with water, dried over anh. Na2SO4 and evaporated to dryness. The obtained oily residue was triturated with hot ethanol (15 mL) with stirring and after cooling was filtrated to afford 1.0 g (36%) of 20 and 1.2 g (44%) of an oily mixture of esters 19 and 20 which was used for the next step without any further purification. To a suspension of the above mixture in ethanol (10 mL) a cold 40% NaOH solution was added and the resulting mixture was stirred at room temperature for 40 min. After completion of the reaction the mixture was poured into ice-water and acidified with 18% HCl solution. The resulting mixture of acids 21 and 22 was filtered, dried over P2O5 and dissolved in hot polyphosphoric acid. The resulting mixture was stirred at 110 °C for 1 h and upon cooling was poured into ice, and the precipitate was filtered and dried over P2O5 to afford xanthones 23 and 24 which were used for the next step without any further purification. Thus, 23 and 24 and the suitable amine, in dry pyridine, was refluxed for 1 1/2 h. After completion of the reaction, pyridine was vacuum evaporated, the oily residue was diluted in EtOAc, washed with water, dried over anh. Na2SO4 and evaporated to dryness. Flash chromatography on silica gel using a mixture of CH2Cl2/MeOH 93/7 as the elouent afforded the title compounds 25, 26 and their isomers 226 and 526, respectively.
Data for 1-((2-(diethylamino)ethyl)amino)-2-nitro-9H-xanthen-9-one (25)
Yield: 12%; M.p. 123–124 °C (EtOAc–n-Hexane); 1H NMR (400 MHz, CDCl3) δ 10.89 (s br, D2O exchang., 1H), 8.26 (dd, J = 7.9, 1.7 Hz, 1H), 8.09 (d, J = 9.2 Hz, 1H), 7.69 (td, J = 7.9, 1.7 Hz, 1H), 7.46–7.36 (m, 2H), 6.57 (d, J = 9.3 Hz, 1H), 3.03 (q, J = 5.7 Hz, 2H), 2.72 (t, J = 5.7 Hz, 2H), 2.65 (q, J = 7.1 Hz, 4H), 1.08 (t, J = 7.1 Hz, 6H). 13C NMR (400 MHz, CDCl3) δ 179.0, 161.0, 155.1, 148.2, 135.2, 134.3, 130.6, 126.8, 125.2, 122.2, 117.8, 109.8, 104.0, 52.1, 47.2, 45.4, 12.0. ( +) ESI QqToF (m/z): Calcd. for C19H22N3O4+: [M + H]+ 356.1605, found 356.1614.
Data for 2-nitro-1-((2-(pyrrolidin-1-yl)ethyl)amino)-9H-xanthen-9-one (26)
Yield: 9%; M.p. 173–175 °C (EtOAc–n-Hexane); 1H NMR (400 MHz, CDCl3) δ 10.88 (t, D2O exchang., J = 4.7 Hz, 1H), 8.21 (dd, J = 7.9, 1.7 Hz, 1H), 8.06 (d, J = 9.3 Hz, 1H), 7.68 (td, J = 8.6, 1.7 Hz, 1H), 7.45–7.32 (m, 2H), 6.56 (d, J = 9.3 Hz, 1H), 3.13 (q, J = 6.3 Hz, 2H), 2.84 (t, J = 6.3 Hz, 2H), 2.66 (m, 4H), 1.85 (m, 4H). 13C NMR (400 MHz, CDCl3) δ 178.9, 160.5, 154.6, 147.6, 134.9, 133.9, 130.1, 126.3, 124.8, 121.6, 117.4, 109.2, 103.7, 54.9, 54.0, 46.0, 23.7. ( +) ESI QqToF (m/z): Calcd. for C19H20N3O4+: [M + H]+ 354.1448, found 354.1440.
2-nitro-1-((2-(pyrrolidin-1-yl)ethyl)amino)-12H-benzo[b]xanthen-12-one (34)
This compound was prepared by an analogous procedure as described for 26 starting from ethyl 3-hydroxy-2-napthoate (27) with 2,4-dichloronitrobenzene (18). Flash chromatography on silica gel using a mixture of CH2Cl2/MeOH 94/6 as the elouent afforded the title compound 34, and the para nitro substitutent compound 926. Yield: 12%; M.p. > 220 °C (EtOAc); 1H NMR (400 MHz, CDCl3) δ 10.99 t, D2O exchang., J = 6.0 Hz, 1H), 8.85 (s, 1H), 8.17 (d, J = 9.4 Hz, 1H), 8.08 (d, J = 8.3 Hz, 1H), 7.93 (d, J = 8.3 Hz, 1H), 7.86 (s, 1H), 7.66 (t, J = 8.3 Hz, 1H), 7.55 (t, J = 8.3 Hz, 1H), 6.73 (d, J = 9.4 Hz, 1H), 3.31 (q, J = 6.5 Hz, 2H), 3,03 (t, J = 6.5 Hz, 2H), 2.88 (m, 4H), 1.96 (m, 4H). 13C NMR (400 MHz, CDCl3) δ 180.0, 161.2, 150.6, 148.0, 136.8, 134.5, 130.3, 130.2, 129.8, 129.6, 128.3, 127.2, 126.2, 120.6, 113.4, 108.6, 105.5, 54.0, 43.3, 23.5. ( +) ESI QqToF (m/z): Calcd. for C23H22N3O4+: [M + H]+ 401.1605, found 401.1616.
General procedure for the synthesis of amino substituted benzo[b]xanthones 35–38
A solution of pure benzo[b]xanthone 32, obtained from the synthesis of 34, and the suitable amine (× 10 equiv.) in dry pyridine (5 mL) was refluxed for 2 h. After completion of the reaction, pyridine was vacuum evaporated, the oily residue was diluted in EtOAc, washed with water, dried over anh. Na2SO4 and evaporated to dryness. Flash chromatography on silica gel, using a mixture of CH2Cl2/MeOH 100/1 as the elouent provided the title compounds 35–38.
Data for 1-((2-(2-hydroxyethoxy)ethyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (35)
Yield: 91%; Oil; 1H NMR (600 MHz, CDCl3) δ 10.95 (t, J = 5.0 Hz, 1H), 8.77 (s, 1H), 8.32 (d, J = 9.5 Hz, 1H), 8.01 (d, J = 8.3 Hz, 1H), 7.99 (s, 1H), 7.92 (d, J = 8.3 Hz, 1H), 7.62 (t, J = 8.2 Hz, 1H), 7.51 (t, J = 8.1 Hz, 1H), 6.42 (d, J = 9.5 Hz, 1H), 3.88 (m, 4H), 3.76–3.73 (m, 2H), 3.59 (q, J = 5.2 Hz, 2H). 13C NMR (600 MHz, CDCl3) δ 180.1, 155.9, 154.0, 150.7, 136.9, 134.1, 130.4, 129.8, 129.5, 127.8, 127.5, 126.3, 125.5, 120.9, 114.3, 104.8, 103.4, 72.9, 68.6, 62.1, 42.8. ( +) ESI QqToF (m/z): Calcd. for C21H19N2O6+: [M + H]+ 395.1238, found 395.1248.
Data for 1-((3-hydroxypropyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (36)
Yield: 84%; M.p. > 220 °C (EtOAc); 1H NMR (400 MHz, CDCl3) δ 10.78 (s, 1H), 8.77 (s, 1H), 8.33 (d, J = 9.6 Hz, 1H), 8.02 (d, J = 9.9 Hz, 2H), 7.93 (d, J = 8.4 Hz, 1H), 7.63 (t, J = 8.2 Hz, 1H), 7.52 (t, J = 8.2 Hz, 1H), 6.50 (d, J = 9.7 Hz, 1H), 3.91 (t, J = 5.8 Hz, 2H), 3.57 (q, J = 6.2 Hz, 2H), 2.07 (m, 2H). 13C NMR (400 MHz, CDCl3) δ 180.0, 156.1, 154.0, 150.7, 136.8, 134.0, 130.3, 129.8, 129.5, 127.6, 127.5, 126.3, 125.3, 120.9, 114.3, 104.6, 103.4, 60.3, 40.3, 31.5. ( +) ESI QqToF (m/z): Calcd. for C20H16N2O5Na+: [M + Na]+ 387.0951, found 387.0962.
Data for 1-((2-hydroxyethyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (37)
Yield: 89%; M.p. > 220 °C (EtOH-H2O); 1H NMR (400 MHz, CDCl3, MeOD) δ 8.75 (s, 1H), 8.30 (d, J = 8.4 Hz, 1H), 8.01 (d, J = 8.4 Hz, 1H), 7.97 (s, 1H), 7.91 (d, J = 8.4 Hz, 1H), 7.61 (t, J = 8.4 Hz, 1H), 7.50 (t, J = 8.3 Hz, 1H), 6.53 (d, J = 9.7 Hz, 1H), 3.89 (t, J = 5.6 Hz, 2H), 3.54 (t, J = 5.6 Hz, 2H). 13C NMR (400 MHz, CDCl3, MeOD) δ 180.4, 156.7, 154.5, 151.0, 137.3, 134.4, 130.8, 130.1, 129.9, 128.0, 127.9, 126.7, 125.5, 121.3, 114.6, 105.0, 104.2, 60.4, 45.7. (-) ESI QqToF (m/z): Calcd. for C19H13N2O5−: [M—H]− 349.0830, found 349.0825.
Data for 1-((3-methoxypropyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (38)
Yield: 94%; M.p. 174–176 °C (EtOAc); 1H NMR (400 MHz, CDCl3) δ 10.76 (s, 1H), 8.78 (s, 1H), 8.32 (d, J = 9.7 Hz, 1H), 8.03 (d, J = 8.4 Hz, 1H), 8.00 (s, 1H), 7.93 (d, J = 8.4 Hz, 1H), 7.63 (t, J = 8.3 Hz, 1H), 7.52 (t, J = 8.1 Hz, 1H), 6.48 (d, J = 9.7 Hz, 1H), 3.57 (t, J = 5.7 Hz, 2H), 3.55–3.49 (m, 2H), 3.41 (s, 3H), 2.05 (m, 2H). 13C NMR (400 MHz, CDCl3) δ 179.9, 156.1, 154.0, 150.7, 136.8, 134.0, 130.3, 129.8, 129.4, 127.6, 127.5, 126.2, 125.3, 121.0, 114.2, 104.6, 103.4, 69.9, 59.0, 40.6, 29.2. ( +) ESI QqToF (m/z): Calcd. for C21H18N2O5Na+: [M + Na]+ 401.1108, found 401.1115.
General procedure for the synthesis of amino substituted benzo[b]xanthones 41–43 and 44–45
Methanesulfonyl chloride (82 μL, 1.05 mmol) was added dropwise at 0 °C to a suspension of 36 (1 mmol) or 37 (1 mmol) and Et3N (279 μL, 2 mmol) in dry CH2Cl2 (10 mL) and the resulting mixture was stirred at room temperature for 6 h. After completion of the reaction the mixture was washed with 1N HCl (2 × 5 mL) and water (2 × 5 mL) and the organic layer was dried over Na2SO4 and vacuum evaporated. Without further purification, the obtained crude mesylate (39 and 40 respectivelly), was dissolved in absolute ethanol (10 mL) and to this solution a suitable amine (× 10 equiv.) was added. The resulting solution was stirred under reflux for 12 h. The solvent was then vacuum evaporated and the oily residue was purified by flash chromatography on silica gel, using a mixture of CH2Cl2/MeOH 9/1 as the elouent to provide the title compounds 41–43 and 44–45.
Data for 1-((3-morpholinopropyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (41)
Yield: 77%; M.p. 179–180 °C (EtOAc–n-Hexane); 1H NMR (400 MHz, CDCl3) δ 10.73 (t, D2O exchang., J = 5.5 Hz, 1H), 8.73 (s, 1H), 8.30 (d, J = 9.6 Hz, 1H), 8.00 (d, J = 8.4 Hz, 1H), 7.97 (s, 1H), 7.91 (d, J = 8.4 Hz, 1H), 7.62 (t, J = 8.2 Hz, 1H), 7.50 (t, J = 8.2 Hz, 1H), 6.47 (d, J = 9.7 Hz, 1H), 3.77 (m, 4H), 3.47 (q, J = 6.4 Hz, 2H), 2.59–2.45 (m, 6H), 1.96 (p, J = 6.4 Hz, 2H). 13C NMR (400 MHz, CDCl3) δ 179.7, 155.9, 153.8, 150.5, 136.6, 133.8, 130.2, 129.6, 129.3, 127.4 (2 C), 126.1, 125.1, 120.8, 114.1, 104.4, 103.3, 67.0, 56.0, 53.8, 41.3, 25.7. ( +) ESI QqToF (m/z): Calcd. for C24H24N3O5+: [M + H]+ 434.1710, found 434.1717.
Data for 1-((3-(4-methylpiperazin-1-yl)propyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (42)
Yield: 81%; Oil; 1H NMR (400 MHz, CDCl3) δ 10.74 (t, D2O exchang., J = 5.4 Hz, 1H), 8.73 (s, 1H), 8.30 (d, J = 9.6 Hz, 1H), 8.06–8.00 (d, J = 9.6 Hz, 1H), 7.96 (s, 1H), 7.94–7.89 (d, J = 9.6 Hz, 1H), 7.63 (t, J = 8.2 Hz, 1H), 7.51 (t, J = 8.2 Hz, 1H), 6.46 (d, J = 9.6 Hz, 1H), 3.47 (q, J = 6.3 Hz, 2H), 2.81 (m, 4H), 2.67 (m, 4H), 2.61 (t, J = 6.3 Hz, 2H), 2.54 (s, 3H), 1.97 (p, J = 6.3 Hz, 2H). 13C NMR (400 MHz, CDCl3) δ 179.5, 155.6, 153.6, 150.3, 136.5, 133.6, 130.0, 129.5, 129.2, 127.2, 127.1, 126.0, 125.0, 120.5, 114.0, 104.2, 103.1, 55.3, 54.1, 51.5, 44.7, 41.4, 25.5. ( +) ESI QqToF (m/z): Calcd. for C25H27N4O4 + : [M + H]+ 447.2027, found 447.2024.
Data for 4-nitro-1-((3-(pyrrolidin-1-yl)propyl)amino)-12H-benzo[b]xanthen-12-one (43)
Yield: 79%; M.p. 175–176 °C (EtOAc–n-Hexane); 1H NMR (600 MHz, CDCl3) δ 10.73 (t, D2O exchang., J = 5.3 Hz, 1H), 8.77 (s, 1H), 8.32 (d, J = 9.6 Hz, 1H), 8.02 (d, J = 8.3 Hz, 1H), 7.99 (s, 1H), 7.93 (d, J = 8.4 Hz, 1H), 7.63 (t, J = 8.2 Hz, 1H), 7.52 (t, J = 8.2 Hz, 1H), 6.50 (d, J = 9.6 Hz, 1H), 3.53 (q, J = 6.9, 2H), 2.80 (t, J = 6.9 Hz, 2H), 2.76 (brs, 4H), 2.10 (p, J = 7.0 Hz, 2H), 1.91 (brs, 4H). 13C NMR (600 MHz, CDCl3) δ 179.8, 155.8, 153.7, 150.5, 136.7, 133.8, 130.2, 129.6, 129.3, 127.4, 127.3, 126.0, 125.2, 120.8, 114.1, 104.4, 103.3, 54.0, 53.4, 41.3, 27.4, 23.5. ( +) ESI QqToF (m/z): Calcd. for C24H24N3O4+: [M + H]+ 418.1761, found 418.1764.
Data for 1-((2-morpholinoethyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (44)
Yield: 82%; M.p. > 220 °C (dec) (EtOAc—n-Hexane); 1H NMR (400 MHz, CDCl3) δ 10.87 (s, D2O exchang., 1H), 8.84 (s, 1H), 8.35 (d, J = 9.6 Hz, 1H), 8.06 (d, J = 8.4 Hz, 1H), 8.02 (s, 1H), 7.94 (d, J = 8.4 Hz, 1H), 7.68–7.61 (m, 1H), 7.58–7.48 (m, 1H), 6.45 (d, J = 9.6 Hz, 1H), 3.84 (m, 4H), 3.49 (brs, 2H), 2.80 (brs, 2H), 2.61 (m, 4H). 13C NMR (400 MHz, CDCl3) δ 179.8, 155.7, 154.0, 150.7, 136.8, 134.0, 130.4, 129.8, 129.4, 127.7, 127.5, 126.2, 125.5, 121.1, 114.3, 104.8, 103.6, 67.2, 56.4, 53.6, 40.2. ( +) ESI QqToF (m/z): Calcd. for C23H22N3O5+: [M + H]+ 420.1554, found 420.1560.
Data for 1-((2-(4-methylpiperazin-1-yl)ethyl)amino)-4-nitro-12H-benzo[b]xanthen-12-one (45)
Yield: 68%; M.p. > 220 °C (dec) (EtOAc–n-Hexane); 1H NMR (600 MHz, CDCl3) δ 10.83 (t, D2O exchang., J = 4.8 Hz, 1H), 8.81 (s, 1H), 8.34 (d, J = 9.5 Hz, 1H), 8.05 (d, J = 8.3 Hz, 1H), 8.01 (s, 1H), 7.94 (d, J = 8.4 Hz, 1H), 7.64 (t, J = 8.2 Hz, 1H), 7.53 (t, J = 8.2 Hz, 1H), 6.43 (d, J = 9.6 Hz, 1H), 3.48 (q, J = 5.8 Hz, 2H), 3.02–2.74 (m, 10H), 2.57 (s, 3H). 13C NMR (400 MHz, CDCl3) δ 180.0, 155.9, 154.2, 151.0, 137.1, 134.2, 130.6, 130.0, 129.7, 127.8, 127.8, 126.5, 125.8, 121.3, 114.5, 105.1, 103.8, 55.7, 54.9, 51.6, 45.3, 40.6. ( +) ESI QqToF (m/z): Calcd. for C24H25N4O4+: [M + H]+ 433.1870, found 433.1870.
Microorganisms strains and growth conditions
The following reference and clinical fungal strains were used: C. albicans ATCC 10231, C. glabrata ATCC 90030, C. krusei ATCC 6258, C. parapsilosis ATCC 22019, S. cerevisiae ATCC 9763, C. albicans B3, C. albicans B4, C. albicans Gu4, C. albicans Gu5, C. albicans F2, C. albicans F527,28. Fungal strains used in this investigation were routinely grown over 18 h at 30 °C in YPG liquid medium (1% yeast extract, 1% peptone, 2% glucose) in a shaking incubator. For growth on solid media, 1.5% agar was added to the YPG medium.
Antifungal activity assays
Antifungal in vitro activity was determined by the modified M27-A3 specified by the CLSI29 by minimal inhibitory concentrations (MICs) determination as described previously14. The MIC was defined as the lowest drug concentration at which at least a 90% decrease in turbidity, in comparison to the drug-free control, was observed. Antifungal activity was determined in RPMI-1640 medium buffered to pH 7.0. The final concentration of the compound solvent (DMSO) did not exceed 2.5% volume of final suspension in each well and did not influence the growth of microorganism.
Minimum fungicidal concentrations (MFCs) were determined as described previously13 by spot assay. The MFC was determined as the lowest concentration of the test compound in which no recovery of microorganisms was observed.
Yeast topoisomerase II relaxation assay and inhibition
The inhibition of yeast topoisomerase II was analysed according to the relaxation assay kit from Inspiralis (Inspiralis Limited, Norwich, UK) and as described previously14. The relaxation inhibition effectivity (IC50) of the analyzed compounds was determined by densitometry quantification of the transition from supercoiled to relaxed forms and was expressed in relation to the control. The gels were photographed with Gel Doc XR + Gel Documentation System (Bio-Rad: Hercules, CA, 647 USA) and image processing was performed by GIMP 2.10.18.
Antiproliferative activity determination
The human embryonic kidney cell line (HEK-293) and human liver cancer cell line (HEPG2) were purchased from ATCC (Manassas, Virginia, USA). HEK-293 was cultured in Dulbecco’s Modified Eagle Medium and HEPG2 in Minimum Essential Medium Eagle. For each cell line, the culture medium was supplemented with 10% fetal bovine serum, 2 mM l-glutamine, and antibiotics: penicillin 62.6 μg mL−1 and streptomycin 40 μg mL−1. The cells were cultured at the humidified atmosphere of 5% CO2/95% air and routinely tested for Mycoplasma contamination. Antiproliferative activity of the compounds was determined as previously described by MTT method14. Percentage of cell viability was calculated, and EC50 values were determined using GraphPad Prism® software (version 8.3.1).
Conclusions
28 xanthone and benzoxanthone analogues were synthesized and evaluated for their antifungal activity. Benzoxanthones proved to be the best antifungal agents with positive mycostatic selectivity index values in relation to HEK293 and HEPG2 cell lines. The fused benzene ring is thus crucial for their activity. The evaluation of biological properties suggests that the mode of action of the most effective derivatives is fungicidal. The demonstrated killing activity is associated with a higher probability of early therapeutic success and a decreased probability of resistance development. Moreover, the clinical strains of C. albicans resistant to fluconazole, due to the FLU-induced overexpression of Cdr1p/Cdr2p drug efflux pumps as well as Mdr1p membrane transport protein of the major facilitator superfamily (MFS), remained sensitive to our novel compounds. This finding suggests that the most active against clinical resistant strains compounds 9, 42 and 44 are not good substrates for ABC as well as MFS efflux pumps.
Since xanthone derivatives are human topoisomerase inhibitors, the antifungal activity of analyzed compounds may be related to their inhibitory effect on the fungal equivalent of that enzyme. Our results indicate a strong relationship between the antifungal activity and the inhibitory effectiveness against yeast topoisomerase II.
Summing up, we were able to show a proof of concept that xanthone modification may result in the discovery of a new group of selective antifungal drugs affecting fungal topoisomerase II. Moreover, our results indicate the possibility of using those derivatives against resistant fungal cells. Further validation of xanthones applicability as antifungals by designing, synthesizing and evaluating the activity of new inhibitors is highly valuable. Future investigations will be focused on improving selectivity.
Supplementary Information
Author contributions
K.R. conducted the experiments of antifungal activity determination and topoisomerase II inhibition studies, analyzed data, wrote manuscript; R.I. conducted the synthesis of the compounds, wrote manuscript; P.M. analyzed data; N.P. analyzed data; M.O. conducted the experiments of cytotoxic activity, analyzed data; I.K.K. and I.G. conceived the experiments, analyzed data, wrote manuscript. All authors reviewed the manuscript.
Data availability
All data generated or analysed during this study are included in this published article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-38963-4.
References
- 1.Pappas P, Lionakis M, Arendrup M, Ostrosky-Zeichner L, Kullberg BJ. Invasive candidiasis. Nat. Rev. Dis. Primers. 2018;4:18026. doi: 10.1038/nrdp.2018.26. [DOI] [PubMed] [Google Scholar]
- 2.Chowdhary A, Sharma C, Meis JF. Candida auris: A rapidly emerging cause of hospital-acquired multidrug-resistant fungal infections globally. PLoS Pathog. 2017;13(5):e1006290. doi: 10.1371/journal.ppat.1006290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Casalini G, Giacomelli A, Ridolfo A, Gervasoni C, Antinori S. Invasive fungal infections complicating COVID-19: A narrative review. J. Fungi. 2021;7(11):921. doi: 10.3390/jof7110921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicola AM, Albuquerque P, Paes HC, Fernandes L, Costa FF, Kioshima ES, Abadio AKR, Bocca AL, Felipe MS. Antifungal drugs: New insights in research and development. Pharmacol. Ther. 2019;195:21–38. doi: 10.1016/j.pharmthera.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Borzyszkowska-Bukowska J, Górska J, Szczeblewski P, Laskowski T, Gabriel I, Jurasz J, Kozłowska-Tylingo K, Szweda P, Milewski S. Quest for the molecular basis of improved selective toxicity of all-trans isomers of aromatic heptaene macrolide antifungal antibiotics. Int. J. Mol. Sci. 2021;22(18):10108. doi: 10.3390/ijms221810108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu N, Tu J, Dong G, Wang Y, Sheng C. Emerging new targets for the treatment of resistant fungal infections. J. Med. Chem. 2018;61(13):5484–5511. doi: 10.1021/acs.jmedchem.7b01413. [DOI] [PubMed] [Google Scholar]
- 7.Milewska MJ, Prokop M, Gabriel I, Wojciechowski M, Milewski S. Antifungal activity of homoaconitate and homoisocitrate analogs. Molecules. 2012;17(12):14022–14036. doi: 10.3390/molecules171214022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holm C, Goto T, Wang JC, Botstein D. DNA topoisomerase II is required at the time of mitosis in yeast. Cell. 1985;41:553–563. doi: 10.1016/S0092-8674(85)80028-3. [DOI] [PubMed] [Google Scholar]
- 9.Del Poeta M, Toaletti DL, Rude TH, Dykstra CC, Heitman J, Perfect JR. Topoisomerase I is essential in Cryptococcus neoformans: Role in pathobiology and as an antifungal target. Genetics. 1999;152:167–178. doi: 10.1093/genetics/152.1.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shen LL, Baranowski J, Fostel J, Montgomery DA, Lartey PA. DNA topoisomerases from pathogenic fungi: Targets for the discovery of antifungal drugs. Antimicrob. Agents Chemother. 1992;36:2778–2784. doi: 10.1128/AAC.36.12.2778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gabriel I. 'Acridines' as new horizons in antifungal treatment. Molecules. 2020;25(7):1480. doi: 10.3390/molecules25071480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gabriel I, Rząd K, Paluszkiewicz E, Kozłowska-Tylingo K. Antifungal activity of capridine β as a consequence of its biotransformation into metabolite affecting yeast topoisomerase II activity. Pathogens. 2020;10(2):189. doi: 10.3390/pathogens10020189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rząd K, Paluszkiewicz E, Gabriel I. A new 1-nitro-9-aminoacridine derivative targeting yeast topoisomerase II able to overcome fluconazole-resistance. Bioorg. Med. Chem. Lett. 2021;35:127815. doi: 10.1016/j.bmcl.2021.127815. [DOI] [PubMed] [Google Scholar]
- 14.Rząd K, Paluszkiewicz E, Neubauer D, Olszewski M, Kozłowska-Tylingo K, Kamysz W, Gabriel I. The effect of conjugation with octaarginine, a cell-penetrating peptide on antifungal activity of imidazoacridinone derivative. Int. J. Mol. Sci. 2021;22(24):13190. doi: 10.3390/ijms222413190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gopalakrishnan G, Banumathi B, Suresh G. Evaluation of the antifungal activity of natural xanthones from Garcinia mangostana and their synthetic derivatives. J. Nat. Prod. 1997;60(5):519–524. doi: 10.1021/np970165u. [DOI] [PubMed] [Google Scholar]
- 16.Zhao DL, Han XB, Wang M, Zeng YT, Li YQ, Ma GY, Liu J, Zheng CJ, Wen MX, Zhang ZF, Zhang P, Zhang CS. Herbicidal and antifungal xanthone derivatives from the alga-derived fungus aspergillus versicolor D5. J. Agric. Food Chem. 2020;68(40):11207–11214. doi: 10.1021/acs.jafc.0c04265. [DOI] [PubMed] [Google Scholar]
- 17.Resende DISP, Pereira-Terra P, Inácio ÂS, Costa PMD, Pinto E, Sousa E, Pinto MMM. Lichen xanthones as models for new antifungal agents. Molecules. 2018;23(10):2617. doi: 10.3390/molecules23102617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Masters KS, Bräse S. Xanthones from fungi, lichens, and bacteria: The natural products and their synthesis. Chem. Rev. 2012;112(7):3717–3776. doi: 10.1021/cr100446h. [DOI] [PubMed] [Google Scholar]
- 19.Vieira LM, Kijjoa A. Naturally-occurring xanthones: Recent developments. Curr. Med. Chem. 2005;12(21):2413–2446. doi: 10.2174/092986705774370682. [DOI] [PubMed] [Google Scholar]
- 20.Shagufta, Ahmad, I. Recent insight into the biological activities of synthetic xanthone derivatives. Eur J Med Chem. 116:267–280; 10.1016/j.ejmech.2016.03.058 (2016). [DOI] [PubMed]
- 21.Omolo JJ, Johnson MM, Vuuren SF, Koning CB. The synthesis of xanthones, xanthenediones, and spirobenzofurans: Their antibacterial and antifungal activity. Bioorg. Med. Chem. Lett. 2011;21:7085e7088. doi: 10.1016/j.bmcl.2011.09.088. [DOI] [PubMed] [Google Scholar]
- 22.Klesiewicz K, Żelaszczyk D, Trojanowska D, Bogusz B, Małek M, Waszkielewicz A, Szkaradek N, Karczewska E, Marona H, Budak A. Preliminary antifungal activity assay of selected chlorine-containing derivatives of xanthone and phenoxyethyl amines. Chem. Biol. Drug Des. 2018;92(5):1867–1875. doi: 10.1111/cbdd.13356. [DOI] [PubMed] [Google Scholar]
- 23.Resende DISP, Pereira-Terra P, Moreira J, Freitas-Silva J, Lemos A, Gales L, Pinto E, de Sousa ME, da Costa PM, Pinto MMM. Synthesis of a small library of nature-inspired xanthones and study of their antimicrobial activity. Molecules. 2020;25(10):2405. doi: 10.3390/molecules25102405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinto E, Afonso C, Duarte S, Vale-Silva L, Costa E, Sousa E, Pinto M. Antifungal activity of xanthones: Evaluation of their effect on ergosterol biosynthesis by high-performance liquid chromatography. Chem. Biol. Drug Des. 2011;77(3):212–222. doi: 10.1111/j.1747-0285.2010.01072.x. [DOI] [PubMed] [Google Scholar]
- 25.Kostakis IK, Tenta R, Pouli N, Marakos P, Skaltsounis AL, Pratsinis H, Kletsas D. Design, synthesis, and antiproliferative activity of some novel aminosubstituted xanthenones, able to overcome multidrug resistance toward MES-SA/Dx5 cells. Bioorg. Med. Chem. Lett. 2005;15(22):5057–5060. doi: 10.1016/j.bmcl.2005.07.079. [DOI] [PubMed] [Google Scholar]
- 26.Kostakis IK, Pouli N, Marakos P, Skaltsounis AL, Pratsinis H, Kletsas D. Design and synthesis of novel amino-substituted xanthenones and benzo[b]xanthenones: Evaluation of their antiproliferative activity and their ability to overcome multidrug resistance toward MES-SA/D×5 cells. Bioorg. Med. Chem. 2006;14(9):2910–2934. doi: 10.1016/j.bmc.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Franz R, Kelly SL, Lamb DC, Kelly DE, Ruhnke M, Morschhäuser J. Multiple molecular mechanisms contribute to a stepwise development of fluconazole resistance in clinical Candida albicans strains. Antimicrob. Agents Chemother. 1998;42:3065–3072. doi: 10.1128/AAC.42.12.3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Franz R, Ruhnke M, Morschhäuser J. Molecular aspects of fluconazole resistance development in Candida albicans. Mycoses. 1999;42:453–458. doi: 10.1046/j.1439-0507.1999.00498.x. [DOI] [PubMed] [Google Scholar]
- 29.Clinical and laboratory Standards Institute (CLSI). Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, Approved Standard, 4rd ed.; CLSI document M27-A3; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012
- 30.Bhattacharya S, Sae-Tia S, Fries BC. Candidiasis and mechanisms of antifungal resistance. Antibiotics. 2020;9(6):312. doi: 10.3390/antibiotics9060312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kurniawan YS, Priyangga KTA, Jumina, Pranowo HD, Sholikhah EN, Zulkarnain AK, Fatimi HA, Julianus J. An update on the anticancer activity of xanthone derivatives: A review. Pharmaceuticals. 2021;14(11):1144. doi: 10.3390/ph14111144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jin S, Shi K, Liu L, Chen Y, Yang G. Xanthones from the bark of garcinia xanthochymus and the mechanism of induced apoptosis in human hepatocellular carcinoma HepG2 cells via the mitochondrial pathway. Int. J. Mol. Sci. 2019;20(19):4803. doi: 10.3390/ijms20194803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jain AK, Singh D, Dubey K, Maurya R, Mittal S, Pandey AK. In Vitro Toxicology. Academic Press; 2018. Chapter 3—Models and methods for in vitro toxicity; pp. 45–65. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article.