Introduction
Leptomeningeal carcinomatosis occurs when tumor cells infiltrate the leptomeninges of the brain, spinal cord, and cerebrospinal fluid.1 Although seen with greater frequency in breast cancer, lung cancer, and malignant melanoma, it is extremely rare in cutaneous squamous cell carcinoma (CSCC). We present a case of recurrent CSCC with perineural invasion (PNI) that progressed to leptomeningeal carcinomatosis.
Case report
A 69-year-old man with a history of idiopathic pulmonary fibrosis status post bilateral lung transplant in 2015, chronic kidney disease, and heart failure presented with pain in the lower portion of his back and weakness in his left leg in fall of 2022. In 2015, he had Mohs micrographic surgery for a CSCC of the right side of his temple. In 2018, he developed a local recurrence of an infiltrative poorly differentiated CSCC with PNI involving skeletal muscle. Positron emission tomography-computed tomography scan (PET-CT) revealed no evidence of metastatic disease, but orbital magnetic resonance imaging (MRI) showed right supraorbital PNI. During the workup, he developed an in-transit metastasis on the right side of forehead. The patient declined orbital exenteration and underwent definitive electron beam radiation therapy (total dose of 55 Gy completed summer of 2018). The patient presented with pain on the right side of the forehead in summer of 2020 and MRI showed recurrent right supraorbital PNI. The patient again declined orbital exenteration and was treated with proton beam radiation to the right orbit and course of V1 to the cavernous sinus (total dose of 66 Gy completed fall of 2020). Over the next 2 years, serial brain MRI revealed stable nodular enhancement of the right V1, V2, and V3 branches of the trigeminal nerve.
In fall of 2022, the patient developed pain in the lower portion of his back and weakness in the lower extremity. MRI of the spine revealed degenerative disk disease, and he was treated over the next 3 months with steroid injections and physical therapy. The patient’s symptoms progressed, and in early 2023, he underwent an MRI of the spine that demonstrated abnormal diffuse thickening and enhancement of the cauda equina nerve roots (Fig 1). The patient was admitted to the hospital and a brain MRI showed posttreatment enhancement of the right supraorbital nerve and cavernous sinus with no evidence of intracranial leptomeningeal metastases. Lumbar punctures showed a mild lymphocytic pleocytosis and elevated protein but no evidence of malignancy; however, an open nerve root biopsy showed metastatic CSCC of the cauda equina (Fig 2). Shortly after the nerve root biopsy, the patient developed slurred speech and facial nerve weakness consistent with leptomeningeal carcinomatosis. He received palliative radiation to the lumbosacral spine for progressive neurologic symptoms and was discharged home with hospice care. He passed away 1 week later.
Fig 1.
Axial (A) and sagittal (B) T1-weighted postcontrast images show diffuse thickening and enhancement of the cauda equina nerve roots (arrows).
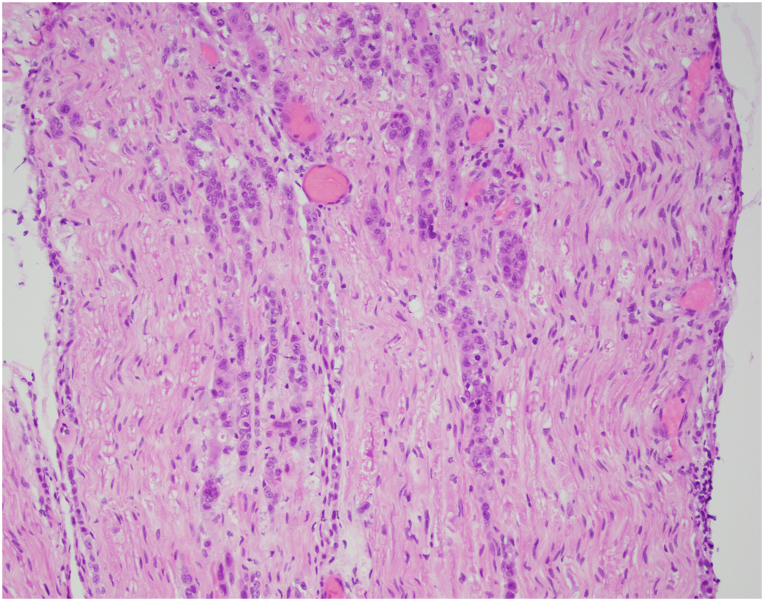
Fig 2.
Clusters and cords of large epithelioid cells with prominent mitotic activity involving the myelinated nerve fibers of the cauda equina. The epithelioid cells were positive for p40 by immunohistochemistry.
Discussion
Leptomeningeal carcinomatosis from a CSCC is extremely rare with only 6 cases reported in the literature. Patients with leptomeningeal carcinomatosis have a median survival time of 3 to 4 months.2 Treatment is mainly palliative, but 1 case reported successful disease stabilization using intrathecal methotrexate and systemic epidermal growth factor receptor (EGFR) inhibitors.3 In patients with leptomeningeal melanoma metastases, intrathecal interferon alfa and interleukin 2, and systemic ipilimumab and nivolumab have been reported to prolong survival.4 Previous cases of cauda equina syndrome because of metastatic CSCC were published before approval of immunotherapy for CSCC. One recent case of a CSCC invading the skull and leptomeninges reported a complete response to pembrolizumab with concurrent radiotherapy.5 However, given our patient’s lung transplant, he was not a candidate for immunotherapy, and he declined intrathecal and systemic chemotherapy because of his poor performance status, high risk of adverse effects, and low likelihood of benefit. Although rare, it is important for clinicians to be aware that metastatic CSCC can present with leptomeningeal carcinomatosis.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Lamba N., Wen P.Y., Aizer A.A. Epidemiology of brain metastases and leptomeningeal disease. Neuro Oncol. 2021;23(9):1447–1456. doi: 10.1093/neuonc/noab101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palmisciano P., Sagoo N.S., Kharbat A.F., et al. Leptomeningeal metastases of the spine: a systematic review. Anticancer Res. 2022;42(2):619–628. doi: 10.21873/anticanres.15519. [DOI] [PubMed] [Google Scholar]
- 3.van Vugt V.A., Saria M.G., Javier A., Kesari N., Turpin T., Kesari S. Neurological improvement of perineural and leptomeningeal spread of squamous cell carcinoma treated with intrathecal chemotherapy and systemic EGFR inhibition. CNS Oncol. 2017;6(4):269–274. doi: 10.2217/cns-2017-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gutzmer R., Vordermark D., Hassel J.C., et al. Melanoma brain metastases - interdisciplinary management recommendations 2020. Cancer Treat Rev. 2020;89 doi: 10.1016/j.ctrv.2020.102083. [DOI] [PubMed] [Google Scholar]
- 5.Lavaud J., Blom A., Longvert C., Fort M., Funck-Brentano E., Saiag P. Pembrolizumab and concurrent hypo-fractionated radiotherapy for advanced non-resectable cutaneous squamous cell carcinoma. Eur J Dermatol. 2019;29(6):636–640. doi: 10.1684/ejd.2019.3671. [DOI] [PubMed] [Google Scholar]