Introduction
Nuclear protein of the testis (NUT) carcinoma (NC), which is also known as NUT midline carcinoma, is a rare, poorly-differentiated, highly aggressive carcinoma characterized by rearrangement of the NUT midline carcinoma family member 1 gene. First described in 1991, the majority of cases demonstrated a t(15;19) translocation resulting in a Bromodomain containing 4-NUT fusion oncogene, which binds chromatin, thereby inhibiting squamous differentiation. In recent years, additional NUT midline carcinoma family member 1 fusion partners have been identified such as BRD3, NSD3, ZNF532, and ZNF592, among others.1, 2, 3 NCs have been described in children and adults, and although they frequently arise in midline structures, such as the thorax, head, and neck, they have also been described in nonmidline structures, such as the kidneys and pancreas. The disease is often metastatic at the time of diagnosis, and in several cases, the primary tumor site cannot be identified.1 The frequency of NC cutaneous involvement is unclear. There has been at least 1 published case of primary cutaneous NC, and 3 cases of NC with cutaneous metastases.4, 5, 6, 7 We present an additional case of NC metastatic to the skin presenting as a solitary nodule.
Case presentation
A 49-year-old man with coronary artery disease, hypertension, and a 29-pack-a-year smoking history was evaluated by the inpatient dermatology service for a solitary nodule on the back. Two years prior to presentation, he received a diagnosis of renal cell carcinoma and was treated with nephrectomy. Months after his renal cell carcinoma diagnosis, chest computed tomography results demonstrated incidental lung nodules, and lung biopsy revealed a 3-cm carcinoma of the left upper lobe with lymphatic and visceral pleural invasion. The tumor exhibited a high-grade basaloid appearance with areas of necrosis, which did not resemble the patient’s chromophobe renal cell carcinoma (Fig 1, A). Immunohistochemical (IHC) staining results were positive for p40 and NUT, focally positive for CK7, pax8, and CD56, and negative for TTF-1, Napsin-A, CK20, chromogranin, and synaptophysin (Fig 1, B). Positron emission tomography and computed tomography revealed notable hilar disease with bronchial obstruction, as well as right adrenal and diffuse bony metastasis. He had been undergoing chemotherapy with ifosfamide and etoposide and received radiation for metastases to the femur. Physical examination revealed a solitary 1.8-cm firm, round, nontender, violaceous nodule on the lower portion of the left side of the back (Fig 2). Punch biopsy results of the lesion was consistent with a metastasis of the underlying NUT carcinoma and revealed high-grade tumor cells with basaloid nuclei in the dermis (Fig 3). Shortly after, the patient succumbed to respiratory failure.
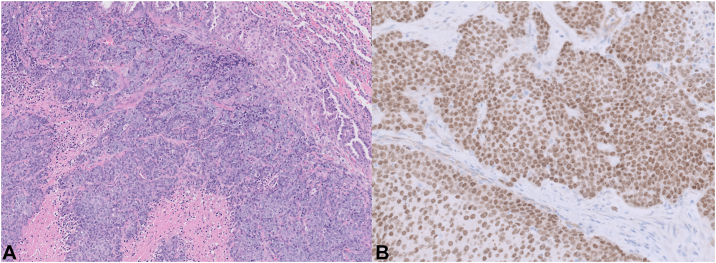
Fig 1.
A, Hematoxylin and eosin-stained section of the lung specimen showing high-grade tumor cells and areas of necrosis. B, Lung tumor cells showing strong nuclear positivity for NUT immunohistochemical stain. NUT, Nuclear protein of the testis. (A, Hematoxylin and eosin-stain; B, immunohistochemistry; original magnifications: A and B, ×20).
Fig 2.
Violaceous nodule on the lower portion of the left side of the back in the setting of metastatic NUT carcinoma. A, Clinical photo. B, clinical photo close-up. NUT, Nuclear protein of the testis.
Fig 3.
Skin punch biopsy of the lower portion of the left side of the back. A, Hematoxylin and eosin-stained section showing sheets of tumor cells in the dermis and (B) high-grade tumor cells with basaloid nuclei. (A and B, Hematoxylin and eosin-stain; original magnifications: A, ×20; B, ×200).
Discussion
Few cases of NC have been reported to date, although reporting patterns suggest that the true prevalence may be much higher than demonstrated by the literature. Lack of testing for NC by clinicians and pathologists is frequently cited as a barrier to diagnosis, as well as clinical trials, for this typically fatal condition, which carries a median survival of 6 to 9 months.1,2,8
Well-described reports of NC are also lacking in the dermatology literature. Among the aforementioned reports with cutaneous involvement, 2 have included clinical descriptions.4, 5, 6, 7 One report described an 11-year-old girl with NC of the pleura in whom pink-red dermal papules, plaques, and nodules subsequently developed on the right side of her neck, chest, and flank, prior to initiation of treatment.5 Another report described a 48-year-old male smoker with NC of the lung treated with chemotherapy and radiation in whom a persistently painful skin-colored to erythematous dermal plaque developed with grouped, tender nodules on the right side of the back/flank.6 In contrast, our patient exhibited a solitary nontender, violaceous nodule. He also had a similar tumor origin site and smoking history to the second prior case; however, NC is currently not believed to be associated with any particular risk factors, including smoking, family history, environmental exposures, or infectious agents.1,7,8
Despite the lack of distinctive clinical findings and histopathologic features, the diagnosis is relatively uncomplicated. Outside of the testes, NUT expression is rare; therefore, IHC staining for NUT with ≥50% nuclear positivity has been used to diagnose NC. When evaluating cutaneous lesions suspicious for NC, one should also keep in mind that NUT midline carcinoma family member 1 fusion genes have been reported in some poromas and porocarcinomas.9 IHC staining to rule out NC diagnosis should be considered for carcinomas with poorly-differentiated sheets of small-to-medium monomorphic cells, with or without squamous differentiation, which lack glandular differentiation or viral etiology. Involvement of midline structures can be supportive, but not required, and cases of unknown primary tumor should certainly be considered.1 Although fluorescence in situ hybridization or next-generation sequencing are not required to confirm the diagnosis, these can be used to identify the gene fusion partner, which may have prognostic and therapeutic implications.1,2 It is theorized that the fusion partner, rather than tumor morphology or immunohistochemistry, may best determine the clinical behavior of the tumor. For instance, the NSD3 and BRD3 fusion partners have been associated with better overall survival compared with Bromodomain containing 4.1
When a patient with known NUT carcinoma presents with a new skin lesion, dermatologists and dermatopathologists should be mindful of potential NC cutaneous presentations and general histopathologic features, as well as diagnostic testing via IHC staining for NUT. At this time, NC portends a grim prognosis and available treatments, including surgery, radiation, and various chemotherapies, are largely unsatisfactory for the majority of patients. With increased awareness and testing, more cases of NC can be accurately diagnosed, and potentially support the development and comparison of new therapies.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Lauer U.M., Hinterleitner M., Horger M., Ohnesorge P.V., Zender L. NUT carcinoma—an underdiagnosed malignancy. Front Oncol. 2022;12 doi: 10.3389/fonc.2022.914031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.French C.A., Cheng M.L., Hanna G.J., et al. Report of the First International Symposium on NUT Carcinoma. Clin Cancer Res. 2022;28(12):2493–2505. doi: 10.1158/1078-0432.CCR-22-0591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Diffalha S., Al Aukla N., Hasan S., Dickinson S., Khalil F. NUT midline carcinoma: a rare malignancy. Cancer Control. 2017;24(2):202–206. doi: 10.1177/107327481702400214. [DOI] [PubMed] [Google Scholar]
- 4.Vargas S.O., French C.A., Faul P.N., et al. Upper respiratory tract carcinoma with chromosomal translocation 15;19: evidence for a distinct disease entity of young patients with a rapidly fatal course. Cancer. 2001;92(5):1195–1203. doi: 10.1002/1097-0142(20010901)92:5<1195::aid-cncr1438>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 5.Young M.R., Millington K., Clarke L.E., Helm K. NUT midline carcinoma with cutaneous metastases. J Am Acad Dermatol. 2012;67(2):323–324. doi: 10.1016/j.jaad.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 6.Ko L.N., Weng Q.Y., Song J.S., Asel M., Granter S.R., Mostaghimi A. A 48-year-old male with cutaneous metastases of NUT midline carcinoma misdiagnosed as herpes zoster. Case Rep Oncol. 2017;10(3):987–991. doi: 10.1159/000481429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo W., Stevens T.M., Stafford P., Miettinen M., Gatalica Z., Vranic S. NUTM1-rearranged neoplasms-A heterogeneous group of primitive tumors with expanding spectrum of histology and molecular alterations—an updated review. Curr Oncol. 2021;28(6):4485–4503. doi: 10.3390/curroncol28060381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Costa B.A., Maraveyas A., Wilkoff M.H., et al. Primary pulmonary NUT carcinoma: case illustration and updated review of literature. Clin Lung Cancer. 2022;23(4):e296–e300. doi: 10.1016/j.cllc.2022.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Macagno N., Kervarrec T., Sohier P., et al. NUT is a specific immunohistochemical marker for the diagnosis of YAP1-NUTM1-rearranged cutaneous poroid neoplasms. Am J Surg Pathol. 2021;45(9):1221–1227. doi: 10.1097/PAS.0000000000001693. [DOI] [PubMed] [Google Scholar]