Abstract
Background:
Older people continue to be disproportionately affected by late HIV diagnosis, which results in increased morbidity and mortality. Despite high acceptance of HIV testing generally, older people are less likely to undergo testing than younger people. Two previous studies have been conducted, one focussing on patient-related and one focussing on clinician-related factors associated with HIV testing in older age (⩾50 years)
Objective:
This study is an integrated analysis from two linked studies – one focussed on patients, and one focussed on clinicians – to understand overlap in views and experiences of HIV testing in older age, to outline the clinical implications of the findings, and to highlight potential interventions to improve testing in this group.
Methods:
This qualitative study utilised semi-structured interviews conducted with 20 clinicians who were not HIV care specialists, but who had recently seen an older person prior to their HIV diagnosis, and 20 people who had been diagnosed late with HIV aged 50+. Interviews were audio recorded, transcribed verbatim and thematically analysed. The combined synthesis reported here was planned a priori as part of a sequential design.
Results:
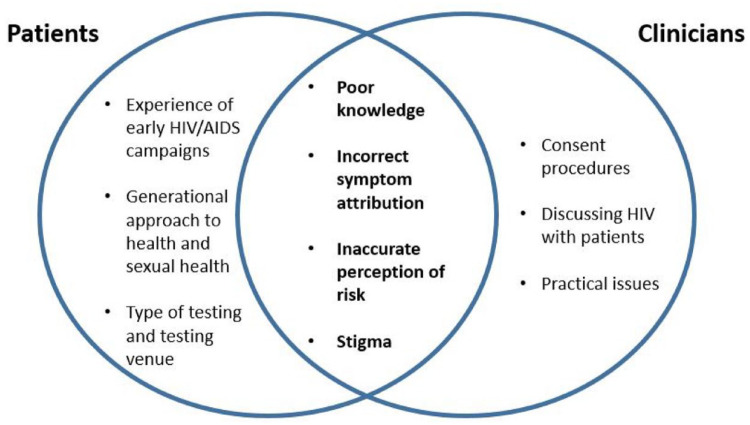
Seven clinician- and seven patient-related themes were associated with undergoing HIV testing in older age. This article discusses the four themes that were common to both groups: poor knowledge, incorrect symptom attribution, inaccurate perception of risk, and stigma.
Conclusion:
Both clinician and patient factors associated with testing will have to be addressed in order to increase HIV testing in older people, and reduce the likelihood of late diagnosis. Findings from overlapping themes suggest several areas for intervention: (1) routine screening as part of existing clinical contacts aimed at older people to eliminate the need to attribute symptoms to HIV or assess risk; (2) specific and tailored education materials for clinicians and older people which utilise appropriate modalities; (3) tailored HIV testing services: either specific clinics for older people at existing sexual health services, or dedicated services in primary care.
Keywords: health services research, HIV, HIV testing, late diagnosis, older people
Introduction
In recent years, HIV prevention strategies have been successful in reducing the number of new HIV diagnoses. These strategies include pre-exposure prophylaxis (PrEP), intensified testing of high-risk individuals, treatment as prevention and continued condom use. 1 However despite this success, the rates of new diagnoses across much of Europe among older people (those aged ⩾50 years) have continued to increase. 2 Furthermore, an HIV diagnosis in older age continues to be associated with disproportionate rates of late diagnosis (a diagnosis with a CD4 count of <350 cells/µl or presentation with an AIDS defining event) when compared with younger people. 1 Although the number of older people newly diagnosed with HIV is fairly small compared with other conditions, which commonly affect this group (e.g. heart disease and cancer), high rates of late diagnosis result in increased morbidity and mortality and onward transmission. 1
Despite the common perception of asexuality in older age, 3 many older people are sexually active, and sex remains important to quality of life as people age. 4 Behavioural factors, many of which promote and facilitate sex in older age, put this group at continued risk. These include relationship transitions such as widowhood and divorce, a lack of condom use,5,6 the increased use of websites and social media which target older people, 7 and the availability of drugs to treat sexual dysfunction. This can partly explain increasing rates of sexually transmitted infections observed in this group. However, despite ongoing risk of HIV, many older adults do not perceive themselves to be at risk, even among those reporting risk behaviours. 8 Similarly, many clinicians perceive older people to be at lower risk of HIV, and evidence suggests that many feel uncomfortable discussing HIV testing with older patients. 9 This may partly explain why clinicians are significantly less likely to offer HIV testing to older patients. 10
Previous articles have reported patient- and clinician-related factors associated with testing for HIV in people aged ⩾50 years.9,11 This article synthesises findings from overlapping themes. The aims of this article are to explore the overlap in views and experiences between patients and clinicians, to outline the clinical implications of the findings, and to highlight potential areas for interventions to improve testing in this group.
Methods
Study design
This was a qualitative study with integrated analysis of patient and clinician data. With an intentional design, the data from previously reported qualitative studies conducted concurrently – one with patients 11 and one with clinicians 9 – were analysed for this study. The integrated analysis reported in this study was planned a priori. 12
Participant selection
Two linked qualitative studies were conducted concurrently: one with patient participants and one with clinician participants. This article presents novel analyses designed to synthesise the common themes from those two studies. Full details of study methods utilised are reported elsewhere.9,11 Briefly, eligible patient participants (see Box 1) were identified and contacted by a member of their local HIV team. Contact details of interested participants were passed to the first author who contacted them directly to arrange a study visit located in a private room at their usual HIV centre. Eligible clinician participants (see Box 1) were non-HIV specialists who were identified via a healthcare utilisation questionnaire conducted with patient participants, and from a review of patient participants’ medical records to identify clinicians they had seen in the 3 years preceding diagnosis. To maintain patient confidentiality, clinician participants were not given details of the patient they had seen. However, despite this, eligible clinicians were only contacted if the patient agreed for contact to be made. Clinician participants were contacted via email to arrange interviews located in a private room within their National Health Service (NHS) Trust.
Box 1.
Eligibility criteria for patient and clinician participants.
| Patient participants | Clinician participants |
|---|---|
| • Aged ⩾50 years at time of HIV diagnosis • Diagnosed late with HIV (defined as a diagnosis with a CD4 <350 cells/μl, or with an AIDS defining event) 13 • Diagnosed with HIV in the previous 1–36 months • Able to give informed consent |
• Had been involved in the care of a patient participant up to 3 years before their HIV diagnosis, but were not HIV specialists • Patient participant agreed for the clinician to be contacted |
Study setting
All recruitment was conducted in HIV centres and NHS Trusts in South East England. Purposive sampling ensured participation of patient participants from areas of high and low HIV prevalence, from large and small HIV centres, and with a range of demographics. This strategy also ensured participation of clinician participants working in areas of high and low local HIV prevalence, and those from a range of clinical specialities.
Data collection
Each participant was invited to an interview with the first author, who was previously unknown to them. At the time of the interview, the interviewer was a doctoral student with previous experience conducting qualitative interviews. At the study visit, the participant was given information about the study and written informed consent was sought. All participants completed a basic demographic questionnaire providing self-reported data to aid recruitment. All participants completed a semi-structured qualitative interview lasting approximately 45 min. Interview topic guides were based on the results of a systematic review conducted by the research team, which highlighted patient- and clinician-related barriers and facilitators to testing for HIV in older age, 14 and were updated as data collection and analysis progressed. 15
Data analysis
All interviews were audio recorded, transcribed verbatim and checked for accuracy. Transcripts were analysed using Braun & Clark’s 16 six-step guide for Thematic Analysis (details of analysis have previously been reported).9,11 Data were managed using NVIVO 11. A pragmatic critical realist approach was used. 15 Due to the exploratory nature of the study, analysis was data driven and therefore no specific theoretical framework was used. This approach meant that data collection and analysis was not restrained by a previously specified theory, and novel factors that were identified could be explored with subsequent participants. At all stages of analysis, the first author consulted co-authors to agree coding and interpretation. Although participants were not consulted to review and agree transcripts or findings, a multidisciplinary study steering group consisting of clinicians, methodological experts and a patient expert in HIV provided feedback from patient and clinician perspectives.
Patient and public involvement
A patient representative and member of the study steering group was involved in all aspects of the study. They were recruited through a community organisation, and had previously worked with members of the study team. The patient is an expert in HIV care and has lived experience of living with HIV. They contributed to the overall design of the study, advised on the recruitment strategy, assisted with the development of study materials, commented on analysis and interpretation of study results, and has reviewed all conference abstracts and articles for publication.
Ethical considerations
Ethical approval was granted by the South Central – Hampshire B Research Ethics Committee (Ref: 16/SC/0279). Written informed consent was sought for every participant in accordance with Good Clinical Practice (GCP) guidelines. 17
Results
Forty qualitative interviews were performed (20 with patient participants and 20 with clinician participants). Both groups varied in terms of their demographics (Table 1).
Table 1.
Participant demographics.
| Patient participants n, (%) | ||
|---|---|---|
| Age in (median, range) | 58 years (52–80) | |
| Gender | Male | 14 (60) |
| Female | 6 (30) | |
| Sexuality | Heterosexual | 12 (60) |
| Gay | 6 (30) | |
| Bisexual | 2 (10) | |
| Ethnicity | White | 16 (80) |
| Black African/Caribbean | 4 (20) | |
| High/low prevalence area | High | 12 (60) |
| Low | 8 (40) | |
| Clinician participants n, (%) | ||
| Speciality | Medicine | 10 (50) |
| Surgery | 7 (35) | |
| Acute/emergency medicine | 3 (15) | |
| High/low prevalence area | High | 12 (60) |
| Low | 8 (40) | |
Seven patient- and seven clinician-related factors associated with whether an older person undergoes HIV testing were identified. Full results from these two studies have been separately reported elsewhere.9,11Figure 1 shows that there was substantial overlap in the views and experiences of patients and clinicians. Four themes were identified in both the patient and clinician interviews – poor knowledge, incorrect symptom attribution, inaccurate perception of risk, and stigma. Each of these is discussed below, and illustrated with quotes presented with participant information.
Figure 1.
Venn diagram displaying unique and overlapping patient- and clinician-related factors associated with undergoing HIV testing in older age.
Poor knowledge
Patients and clinicians both reported having outdated HIV-related knowledge, which acted as a barrier to seeking or offering an HIV test in older age. For many patients, their knowledge of HIV was informed by early HIV/AIDS campaigns. A lack of health promotion materials outside of gay venues or media since this time meant that the majority were misinformed about HIV. Not only did this extend to misperceptions about the clinical outcomes associated with an HIV diagnosis, but some did not even know where to go to undertake testing. The majority of clinicians reported that they had not received HIV-related information since medical school or early in their career. Most reported that their knowledge tended to be focussed on their specialist clinical area, so they were not exposed to updated information about HIV. Both groups felt that older people in particular had poor HIV-related knowledge and would benefit from targeted health promotion messages as a way of improving HIV testing in this group:
This whole thing about being over 50, it’s a lot of . . .. you’re just simply not exposed to it [HIV-related information], in the way that you would have been. (patient, 53, white, gay)
Younger people might be more, more up to date about it, because they may be exposed to the possibility. So, I think older people might feel that . . .. it’s more a serious condition . . .. the outlook is bleak. (clinician, medical speciality, high prevalence)
Although both groups discussed the need for updated information, the information they felt they required was different. Clinicians reported a requirement for structural and practical information regarding testing such as updates on HIV testing guidelines and consenting procedures. Patients reported a need for updates on the medical advances in HIV, and for basic information such as where they could go to test for HIV:
I never knew this clinic existed. I’ve lived in this town 40 years, didn’t know really what it was, until that young girl at work said to me the week before that she’d been here. (patient, 57, white, female)
Incorrect symptom attribution
Both groups discussed the important influence of symptom attribution on whether an older person undergoes HIV testing. Patients and clinicians both tended to associate symptoms in an older person with something other than HIV, often something age-related:
Some of my symptoms I would have put down, and I think other medical people would have put down, to my age. You know is it all part of the process of getting older anyway. (patient, 68, white, heterosexual man)
I would consider usually a pneumonia to be just something that you’re, that when you’re elderly and have lots of medical problems that you’re susceptible to, and I wouldn’t be thinking HIV. (clinician, acute/emergency medicine, high prevalence)
Although the perception that older people were less at risk of HIV was a significant driver towards this opinion in both groups, for patients this was compounded by their experience of other health conditions. For this reason, patients tended to attribute symptoms to conditions they were aware of through health promotion campaigns, such as cancer, or something a friend or loved one had previously experienced. Although clinicians also believed older people to be at lower risk of HIV, this misattribution of symptoms was compounded by their own perceptions of illness burden among older groups. Clinicians associated HIV with an ‘unusual presentation’. For this reason, many found it difficult to identify symptoms which indicated HIV in older patients who often present with pre-existing comorbidities. In this older cohort, illness was expected and therefore it was often felt that further investigation such as HIV testing was not warranted:
A 35-year-old person, it’s much more uncommon for them to get pneumonia and you think ‘well why is that? They shouldn’t be immune-compromised’. Whereas nearly every elderly person I see has got a reason for being immuno-compromised. So yes, you would think of it differently with age. (clinician, acute/emergency medicine, high prevalence)
Patients and clinicians both discussed the potential impact of treating symptoms in isolation and how this can potentially lead to a delay in undergoing HIV testing. Clinicians reported that they tended to treat symptoms in isolation and usually within the realms of their own speciality, which in some instances resulted in an HIV diagnosis having been missed. This supported patients’ claims that receiving care from several clinicians within primary and secondary care resulted in a lack of consistency whereby individual symptoms were treated separately rather than holistically:
When you see a constellation of symptoms and, and clinical features, you’re going to think of the respiratory things first – and then you’ll try and fit them into your particular way of, um, way of seeing things. (clinician, medical speciality, high prevalence)
I think the lack of consistency means that not one person will sit there and say ‘Well we’ve tried this, we’ve thought of this’, nobody did that, it was just you present, you’re given five minutes, let’s think what the most likely thing is. (patient, 57, white, heterosexual woman)
Inaccurate perception of risk
The perception that older people are at lower risk of HIV – held by both patients and clinicians – was identified as a barrier to undergoing HIV testing in older age. When a person did not feel at risk of HIV, there was no motivation to seek testing. Interviewees noted that their low perceived risk of HIV was influenced by media messages and images that associated HIV risk with particular groups such as men who have sex with men (MSM), people who inject drugs, younger people, or people who had a history of risky sexual behaviours such as unprotected intercourse and/or multiple partners. This stereotyping was often informed by early HIV/AIDS media campaigns, and was commonly reported by both groups:
I think the media only tells you what the media wants you to know and . . .. it paints a picture of these people that are all sharing needles in alleyways and things like that and then, oh dear, then they get HIV, or promiscuous, gay people. (patient, 57, white, heterosexual woman)
I still got the impression you know, that it’s a relatively young, well a disease affecting the young, and relatively young. (clinician, medical speciality, low prevalence)
There was agreement between both groups that the perception of low risk of HIV in older age was due to the belief that older people were more sensible and therefore less likely to take part in risky behaviour associated with HIV acquisition. As a result of these stereotypes, some patients reported that they felt clinicians were less likely to offer them an HIV test:
I don’t fit into the demographic, do I? I’m not a young, I’m not a gay person, I’m not African, I’m not any of those things am I? In their mind I’m just a middle aged . . .. I think they thought I was a middle aged hypochondriac to be honest (patient, 57, white, heterosexual woman)
However, despite clinicians agreeing that older patients did not fit within their perceptions of a high risk person, they reported that this was not a driver in a decision to offer an HIV test to an older person. This highlights an inconsistency in the views of patients and clinicians. Despite this, some clinicians did discuss how they formed stereotypes of their whole cohort rather than of individual patients. This was usually based on their perception that their entire patient cohort was at low risk due to features such as advanced age, ethnic mix, or social class:
I tend to think they’re all low risk around here to be honest. (clinician, medical speciality, low prevalence)
Although some clinicians reported that they would not let individual stereotypes influence whether they offered HIV tests, some reported that they would be more likely to offer an HIV test to an older patient if they reported risky behaviours. However, more commonly, clinicians reported that they were unlikely to do any kind of risk assessment for HIV, particularly in older patients.
Stigma
Stigma was commonly discussed by both patients and clinicians. Both groups reported that HIV-related stigma was due to HIV being seen as a disease affecting particular sub-groups, including MSM, injecting drug users or people engaging in high risk sexual behaviours. As a result, HIV was often seen as socially unacceptable, and there was an element of shame or blame associated with a diagnosis of HIV:
If you’ve got lung cancer, even if you are a heavy smoker and always have been a heavy smoker, there is a certain amount of sympathy for you . . .. But somehow, lung cancer in a smoker is socially acceptable, HIV in anybody else isn’t. (patient, 68, white, heterosexual man)
I think people do know about HIV and they associate it with either risky behaviour or homosexuality, which they might not be very tolerant of. (clinician, medical speciality, low prevalence)
Patients commonly felt that people made assumptions about someone living with HIV, and as a result this potentially had an impact on whether they would seek HIV testing. Some older people felt people would treat them differently if they were diagnosed with HIV and feared social isolation. Patients and clinicians both reported an added stigma in being diagnosed with HIV in older age. Commonly it was agreed that this was due to the perception that older people either they do not engage in sexual activity, or do not engage in high risk behaviours commonly associated with HIV:
I would tend to use the phrase ‘old enough to know better’. If you were some sort of rampant teenager caught up in the excitement of your first time or whatever, then you could understand them not taking the necessary precautions. (patient, 68, white, heterosexual man)
Well everybody these days thinks people over thirty are old don’t they? But yeah in older life, possibly they think that people don’t have more partners, don’t have unprotected sex, aren’t still promiscuous. (patient, 55, white, gay)
Clinicians found it difficult to discuss sexual health with older people, and perceived that older patients would be offended by the offer of an HIV test. However, patients were happy to discuss sexual health with a clinician and would almost always agree to the offer of an HIV test:
I suspect some older patients will have erm, ideas about what that means and, and what you’re suggesting and might be offended I imagine, of a suggestion that that is something that you need to test for. (clinician, acute/emergency medicine, high prevalence)
Being a doctor is not a game, you’re dealing with people’s lives, so you’ve gotta look at all options no matter how bad they might be, no matter how good they might be. So maybe you might not mention something because you don’t want to offend, but at the end of the day something has to be done or mentioned to make that person better. (patient, 55, black African, heterosexual man)
As a result of stigma, many patients reported a dislike of utilising sexual health services and avoided testing services. However, although clinicians acknowledged stigma within the healthcare setting, they perceived it differently to patients. Clinicians discussed how ongoing stigma meant that HIV records were kept separately to general medical records and as a result, they were not able to access them. Clinicians also felt that testing for HIV was unique and required a lengthy pre-test counsel.
Discussion
The analysis identified four factors associated with undergoing HIV testing in older age where there was significant overlap between the views and experiences of patients and clinicians. Because of this overlap, these factors identify potential areas for intervention to address patient- and clinician-related barriers to undergoing HIV testing in older age.
Having poor and outdated HIV-related knowledge was found to be a potential barrier to either seeking an HIV test in older age, or offering an HIV test to an older person. These findings are consistent with literature, which also indicated that a lack of HIV-related knowledge was a barrier to undergoing HIV testing in older age.14,18–22 The majority of current health promotion materials regarding HIV are aimed at a younger audience, 23 and as a result are unlikely to have a strong influence on the testing behaviours of older people. This also leads to older people continuing to be uninformed about HIV and to hold on to outdated beliefs about HIV transmission.7,24 This suggests that health promotion materials which target this group may help to overcome this barrier. Such information should be tailored to this group to address gaps in knowledge, and the modality would need to be appropriate for the target audience. 25
Our findings reflected previous literature suggesting that many clinicians remain unfamiliar with HIV testing guidelines26–31 and that many report a lack of understanding regarding requirements for consent.18,20,32 However, the majority of patients and clinicians in these studies tended to report receiving information passively rather than actively seeking it. As a result, information will have to be disseminated directly to the intended group, rather than the onus being on the patient/clinician to seek information.
Improved patient and clinician knowledge of HIV may help normalise HIV testing and reduce stigma by challenging common misperceptions about HIV. 33 This study revealed that both groups commonly held misconceptions about the type of person who may be at risk of HIV infection, and clinicians often had preconceptions about how an older person might react to the offer of an HIV test. Stigma continues to be an ongoing problem for people living with HIV, and many people living with HIV are worried about how they will be treated by others because of their positive status. 34 Patients and clinicians in these studies both reported an added stigma related to an HIV diagnosis in older age. Commonly it was agreed that this was due to the perception that older people either do not engage in sexual activity, or do not engage in high-risk behaviours associated with HIV. Although in this study, the majority of older people likely acquired HIV through heterosexual sex, both clinician and patient participants perceived ‘high-risk’ behaviours to be largely associated with multiple partners or ‘promiscuity’, unprotected intercourse, and/or male same-sex behaviour. Previous research supports this finding that commonly people perceive that older people do not engage in sexually activity.14,35,36 However, this is in contrast with the observation that many older adults are sexually active and that sex remains important to quality of life as people age.4,37 Evidence suggests that ageism felt by older people living with or diagnosed with HIV in older age has led to them feeling rejected by clinicians. 38 This ageist stereotype will have to be challenged in order to improve HIV testing within the older group.
Clinicians in this study found it difficult to discuss sexual health with older people and perceived that older patients would be offended by the offer of an HIV test. This was in direct conflict with patient reports, which suggested they would not be offended. Although it is acknowledged that the older people included in the study would all have benefitted from earlier testing and so their views may not be reflective of older people generally, clinicians who had experience offering HIV testing to older people reported that they almost always accepted. Despite this, clinicians still felt uncomfortable having a conversation around HIV with older people. Clinicians’ reluctance to discuss sexuality with an older person, or being unsure about how to approach this type of conversation with an older patient is evident from the literature.37,39 However, these studies and existing literature also indicate that one of the biggest facilitators to undergoing HIV testing is being offered a test or being encouraged to test by a clinician.14,40–42 Furthermore, results from these studies suggest that older patients are happy to discuss sexual health with a clinician and would almost always agree to the offer of an HIV test. This finding has been previously reported, even when patients do not perceive themselves to be at risk. 42 Despite this, evidence suggests that clinicians would rather an older patient initiate discussion regarding sexual health. 43 This may explain why older patients are significantly less likely to be offered an HIV test than a younger person,10,44 despite high acceptability among patients generally. 45 This highlights the importance of addressing clinicians’ preconceived notions about how an HIV test will be received by an older patient in order to increase testing in this group.
For older patients who wish to seek a test, these studies indicated that many older patients reported a dislike of utilising specialist sexual health services, and some even avoided any kind of HIV testing service. To address this, services will need to be better set up in order to meet the needs of this group. This may include dedicated services aimed at older people which run in primary care, where anonymity will help to overcome the barrier associated with attending sexual health services. Offering HIV testing in primary care, particularly when testing is routinely offered to everyone, regardless of age, would also help to address some of the barriers associated with perception of risk, which was another overlapping theme among patients and clinicians identified in these studies.9,11 This could include adding HIV testing to current health screening in primary care (e.g. for other conditions such as cardiovascular disease), and alongside ongoing management of long-term conditions, as a way of targeting older people.
Low perceived risk is a barrier to undergoing testing in patients of any age, 46 and can be seen despite the disclosure of high-risk behaviours.21,22,47 These studies indicated that both patients and clinicians stereotype older people to be at low risk of HIV because they perceive this group to be less likely to be part of a hig risk group or take part in risky behaviour. Indeed, HIV continues to be associated with high-risk behaviours, and a disease which is more likely to affect younger people. 48 Some patients reported that these stereotypes made clinicians less likely to offer them an HIV test. Some clinicians reported that they would not let individual stereotypes influence whether they offered HIV tests, and some reported that they would be more likely to offer an HIV test to an older patient if they reported risk behaviours. However, clinicians commonly reported that they were unlikely to do any kind of risk assessment for HIV, particularly in older patients. This is consistent with previous findings suggesting that general screening is unlikely to include any kind of sexual history,39,49,50 and that many clinicians are not prepared to conduct a sexual health screen. 50 However, clinicians who have received training feel more confident to perform a sexual health screen and are more likely to offer appropriate testing.50–53
Routinely offering screening would also help to address barriers to HIV testing associated with symptom attribution. Attributing symptoms to something other than HIV, such as ageing, was reported by patients and clinicians in these studies. Existing literature supports this finding, suggesting older people find it more difficult to interpret their symptoms than younger people, and often attribute symptoms to ageing and/or the presence of other health conditions.54,55 Clinicians also reported that they tended to attribute symptoms in older patients to something age-related rather than HIV. This misattribution of symptoms was compounded by their own perceptions of illness burden among older groups, which led to difficulty identifying symptoms indicating HIV in a patient with pre-existing comorbidities. 9 This is consistent with previous research, which reported that clinicians are likely to assign symptoms in older patients to something more common in older age. Often this is exacerbated by the presence of other chronic health conditions, and results in delayed HIV testing.14,56–58 Commonly clinical indicator conditions (CICs) associated with HIV are seen in patients diagnosed late with HIV.59,60 Up to a quarter of patients diagnosed late with HIV received a CIC diagnosis more than a year before receiving an HIV diagnosis. 59 Failure to recognise a CIC remains a barrier to offering HIV testing,14,61 so information regarding common conditions, which may indicate HIV may be important when designing education materials for clinicians.
Recommendations to increase HIV testing
Based on the overlapping factors reported by older patients and clinicians as associated with HIV testing, there are several recommendations to improve HIV testing in this group.
Routine screening
The routine offer of HIV testing to people regardless of age or the presence of symptoms could help to overcome several barriers highlighted in these studies. This includes having to identify symptoms associated with HIV, performing risk assessments, and having a perceived uncomfortable conversation with an older patient. It could also address some practical factors such as time. Adding routine HIV testing to the primary care setting within current health screening strategies or well-man/well-woman clinics might serve as an opportunity for offering testing to older people. Better dissemination of HIV testing and consenting guidance, and having routine testing as part of hospital policy could potentially help to encourage the offer of testing.
Education
Updated information regarding HIV needs to be disseminated to clinicians and to the public. In terms of clinicians, this should be focussed on practical issues such as testing guidance, consenting procedures and CICs. This information should be tailored and brief – for example, to include a list of CICs that relate specifically to their speciality. For the public, this information also needs to be tailored to the older audience. Current health promotion materials, such as those used for the National HIV testing week campaign, often exclude older people and as such, older people do not acknowledge them. Information should include basic information such as where to go for HIV testing, as well as updates on who can be at risk, and advances in HIV treatment and outcomes.
Tailored HIV testing services
Many older patients reported a dislike for utilising sexual health services, which was often associated with stigma. Dedicated sexual health sessions for older patients within existing sexual health clinics may help to overcome these barriers. However, this would not be suitable for those who avoided these services entirely. For such people, dedicated HIV testing services in primary care may be preferable as this affords a level of anonymity.
Strengths and limitations
A key strength of the studies were the included participants. All of the patient participants were aged ⩾50 years, with a maximum age of 80 years. The patients had a range of demographics to ensure representation of people with a range of ethnicities, ages, gender identities and sexualities. Similarly, clinician participants were purposively sampled to ensure representation of those from a range of specialities, and those working in areas of high and low HIV prevalence. Clinician participants had also recently seen an older patient diagnosed late with HIV, which ensure views were captured from clinicians who had seen an older patient where an HIV diagnosis had potentially been missed. Despite these strengths, some limitations remained. Although included clinicians were from a range of specialities, it was not possible to include clinicians working in primary care. Selection bias could mean that participants who consented to the study had particularly strong views about HIV testing in older age. Furthermore, the focus on older people with a late diagnosis of HIV infection meant that the views of other older people were not considered: it is possible that their views of issues including routine testing may have been different.
Conclusion
Older people are disproportionately affected by a late diagnosis of HIV, and diagnosis in older age is associated with increased morbidity and mortality. Despite high acceptance of HIV testing in this group, offer rate remains low. The included studies reported seven patient-related and seven clinician-related factors associated with undergoing HIV testing in older age. There was significant overlap in four of these factors: poor knowledge; incorrect symptom attribution, inaccurate perception of risk, and stigma, which are opportunities for intervention. Addressing these factors could help to improve HIV testing among older people. Recommendations include routinely screening patients for HIV regardless of patient age or presenting condition; improving knowledge among clinicians and older people via tailored information and health promotion materials; and designing tailored HIV testing services for older people – either within existing sexual health settings or in primary care settings.
Acknowledgments
Not applicable.
Footnotes
ORCID iD: Elaney Youssef  https://orcid.org/0000-0001-6897-2015
https://orcid.org/0000-0001-6897-2015
Contributor Information
Elaney Youssef, Department of Medical Education, Brighton and Sussex Medical School, University of Brighton, Falmer Campus, Watson Building, Brighton BN1 9PH, UK.
Juliet Wright, Brighton and Sussex Medical School, Brighton, UK.
Kevin Davies, Brighton and Sussex Medical School, Brighton, UK.
Valerie Delpech, Public Health England, London, UK.
Alison Brown, Public Health England, London, UK.
Vanessa Cooper, University College London, London, UK.
Memory Sachikonye, Positively UK, Brighton, UK.
Richard de Visser, Department of Medical Education, Brighton and Sussex Medical School, Brighton, UK, University of Brighton, Brighton, UK.
Declarations
Ethics approval and consent to participate: Ethical approval was granted on 21 June 2016 by the South Central – Hampshire B Research Ethics Committee (Ref: 16/SC/0279). Written informed consent was sought from every participant prior to participation in the study in accordance with Good Clinical Practice (GCP) guidelines.
Consent for publication: All participants gave consent for parts of their interviews to be included in publications. Steps were taken to ensure anonymity including the use of pseudonyms and/or study numbers.
Author contributions: Elaney Youssef: Conceptualisation; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Visualisation; Writing – original draft; Writing – review & editing.
Juliet Wright: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Resources; Supervision; Validation; Visualisation; Writing – review & editing.
Kevin Davies: Conceptualisation; Data curation; Formal analysis; Investigation; Resources; Supervision; Validation; Visualisation; Writing – review & editing.
Valerie Delpech: Conceptualisation; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Resources; Software; Supervision; Validation; Visualisation; Writing – review & editing.
Alison Brown: Conceptualisation; Formal analysis; Funding acquisition; Methodology; Supervision; Validation; Writing – review & editing.
Vanessa Cooper: Conceptualisation; Data curation; Formal analysis; Funding acquisition; Methodology; Supervision; Validation; Writing – review & editing.
Memory Sachikonye: Conceptualisation; Data curation; Funding acquisition; Investigation; Methodology; Validation; Visualisation; Writing – review & editing.
Richard de Visser: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Resources; Supervision; Validation; Visualisation; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is funded by the National Institute of Health Research Doctoral Research Fellowship (REF: DRF-2015-08-086). This article presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, NHIR or Department of Health.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1.O’Halloran C, Sun S, Nash S, et al. HIV in the United Kingdom: towards zero HIV transmissions by 2030 – 2019 report. London: Public Health England, 2019. [Google Scholar]
- 2.Tavoschi L, Gomes Dias J, Pharris A, et al. New HIV diagnoses among adults aged 50 years or older in 31 European countries, 2004-15: an analysis of surveillance data. Lancet HIV 2017; 4: e514–e521. [DOI] [PubMed] [Google Scholar]
- 3.Nay R, McAuliffe L, Bauer M. Sexuality: from stigma, stereotypes and secrecy to coming out, communication and choice. Int J Older People Nurs 2007; 2: 76–80. [DOI] [PubMed] [Google Scholar]
- 4.de Visser RO, Badcock PB, Simpson JM, et al. Attitudes toward sex and relationships: the second Australian study of health and relationships. Sex Health 2014; 11: 397–405. [DOI] [PubMed] [Google Scholar]
- 5.Schick V, Herbenick D, Reece M, et al. Sexual behaviors, condom use, and sexual health of Americans over 50: Implications for sexual health promotion for older adults. J Sex Med 2010; 7(Suppl. 5): 315–329. [DOI] [PubMed] [Google Scholar]
- 6.de Visser RO, Badcock PB, Rissel C, et al. Safer sex and condom use: findings from the second Australian study of health and relationships. Sex Health 2014; 11: 495–504. [DOI] [PubMed] [Google Scholar]
- 7.Brooks JT, Buchacz K, Gebo KA, et al. HIV infection and older Americans: the public health perspective. Am J Public Health 2012; 102: 1516–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Syme ML, Cohn TJ, Barnack-Tavlaris J. A comparison of actual and perceived sexual risk among older adults. J Sex Res 2017; 54: 149–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Youssef E, Wright J, A, Davies K, et al. Factors associated with offering HIV testing to people aged ⩾ 50 years: a qualitative study. Int J STD AIDS 2022; 33: 289–295. [DOI] [PubMed] [Google Scholar]
- 10.Health Protection Agency (HPA). Time to test for HIV: Expanding HIV testing in healthcare and community services in England. London: HPA, 2011. [Google Scholar]
- 11.Youssef E, Wright J, Delpech V, et al. Factors associated with testing for HIV in people aged ⩾50 years: a qualitative study. BMC Public Health 2018; 18: 1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morse J. Simultaneous and sequential qualitative mixed method designs. Qualitative Inquiry 2010; 16: 483–491. [Google Scholar]
- 13.Antinori A, Coenen T, Costagiola D, et al. Late presentation of HIV infection: a consensus definition. HIV Med 2011; 12: 61–64. [DOI] [PubMed] [Google Scholar]
- 14.Youssef E, Cooper V, Delpech V, et al. Barriers and facilitators to HIV testing in people age 50 and above: a systematic review. Clin Med 2017; 17: 508–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Youssef E. Understanding late diagnosis of HIV in people aged 50 and above. Brighton: Brighton and Sussex Medical School, 2019. [Google Scholar]
- 16.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006; 3: 77–101. [Google Scholar]
- 17.National Institute for Health Research (NIHR). Good clinical practice (GCP) reference guide. Leeds: NIHR, 2016. [Google Scholar]
- 18.Burke R, Sepkowitz K, Bernstein K, et al. Why don’t physicians test for HIV? A review of the us literature. AIDS 2007; 21: 1617–1624. [DOI] [PubMed] [Google Scholar]
- 19.Davies C, Gompels M, May M. Public and healthcare practitioner attitudes towards HIV testing: review of evidence from the United Kingdom (UK). International STD Research & Reviews 2015; 3: 91–122. [Google Scholar]
- 20.Simmons E, Brown M, Slye K, et al. Barriers and facilitators to testing in primary care among health care providers. J Nat Med Assoc 2011; 103: 432–438. [DOI] [PubMed] [Google Scholar]
- 21.Sankar A, Nevedal A, Neufeld S, et al. What do we know about older adults and HIV? A review of social and behavioral literature. AIDS Care 2011; 23: 1187–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Negin J, Geddes L, Brennan-Ing M, et al. Sexual behavior of older adults living with HIV in Uganda. Arch Sex Behav 2016; 45: 441–449. [DOI] [PubMed] [Google Scholar]
- 23.Orel NA, Wright JM, Wagner J. Scarcity of HIV/aids risk-reduction materials targeting the needs of older adults among state departments of public health. Gerontologist 2004; 44: 693–696. [DOI] [PubMed] [Google Scholar]
- 24.Hughes AK, Alford KR. HIV transmission: myths about casual contact and fear about medical procedures persist among older adults. Soc Work Public Health 2017; 32: 49–52. [DOI] [PubMed] [Google Scholar]
- 25.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull 2007; 133: 673–693. [DOI] [PubMed] [Google Scholar]
- 26.Cabana M, Rand C, Powe N, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999; 282: 1458–1465. [DOI] [PubMed] [Google Scholar]
- 27.Hudson AL, Heilemann MV, Rodriguez M. Missed opportunities for universal HIV screening in primary care clinics. J Clin Med Res 2012; 4: 242–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jain CL, Wyatt CM, Burke R, et al. Knowledge of the centers for disease control and prevention’s 2006 routine HIV testing recommendations among New York City internal medicine residents. AIDS Patient Care STDs 2009; 23: 167–176. [DOI] [PubMed] [Google Scholar]
- 29.Mohajer MA, Lyons M, King E, et al. Internal medicine and emergency medicine physicians lack accurate knowledge of current CDC HIV testing recommendations and infrequently offer HIV testing. J Int Assoc Physicians AIDS Care 2012; 11: 101–108. [DOI] [PubMed] [Google Scholar]
- 30.Myers JJ, Koester KA, Dufour MS. Barriers and facilitators to enhancing HIV testing in publicly funded primary care clinics: findings from San Francisco. AIDS Educ Prev 2011; 23(Suppl. 3): 84–95. [DOI] [PubMed] [Google Scholar]
- 31.Reilley B, Redd JT, Giberson S, et al. Physician and nurse perspectives on implementation of universal adult HIV screening guidelines in the Indian Health Service: results of a randomized survey. J Public Health Manag Pract 2010; 16: 450–456. [DOI] [PubMed] [Google Scholar]
- 32.White BL, Walsh J, Rayasam S, et al. What makes me screen for HIV? Perceived barriers and facilitators to conducting recommended routine HIV testing among primary care physicians in the Southeastern United States. J Int Assoc Provid AIDS Care 2015; 14: 127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nyblade L, Stangl A, Weiss E, et al. Combating HIV stigma in health care settings: what works? J Int AIDS Soc 2009; 12: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.STIGMA. HIV in the UK: changes and challenges; actions and answers. The people living with HIV Stigma Survey, UK 2015. London: STIGMA, 2015. [Google Scholar]
- 35.Alencar RA, Ciosak SI. Late diagnosis and vulnerabilities of the elderly living with HIV/aids. Rev Esc Enferm USP 2015; 49: 229–235. [DOI] [PubMed] [Google Scholar]
- 36.Barnett L. Factors contributing to the increase in HIV/aids and late diagnoses of the virus among older adults. https://scholarworks.waldenu.edu/dissertations/905/
- 37.Bauer M, McAuliffe L, Nay R. Sexuality, health care and the older person: an overview of the literature. Int J Older People Nurs 2007; 2: 63–68. [DOI] [PubMed] [Google Scholar]
- 38.Emlet CA. ‘You’re awfully old to have this disease’: experiences of stigma and ageism in adults 50 years and older living with HIV/aids. Gerontologist 2006; 46: 781–790. [DOI] [PubMed] [Google Scholar]
- 39.Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med 2004; 58: 2093–2103. [DOI] [PubMed] [Google Scholar]
- 40.Slinkard MS, Kazer MW. Older adults and HIV and STI screening: the patient perspective. Geriatr Nurs 2011; 32: 341–349. [DOI] [PubMed] [Google Scholar]
- 41.Mack KA, Bland SD. HIV testing behaviors and attitudes regarding HIV/aids of adults aged 50-64. Gerontologist 1999; 39: 687–694. [DOI] [PubMed] [Google Scholar]
- 42.Baumann K, Hemmige V, Kallen M, et al. Whether patients want it or not, physician recommendations will convince them to accept HIV testing. J Int Assoc Provid AIDS Care 2018; 17: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arya M, Patel S, Kumar D, et al. Why physicians don’t ask: interpersonal and intrapersonal barriers to HIV testing-making a case for a patient-initiated campaign. J Int Assoc Provid AIDS Care 2016; 15: 306–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mody N, Perry N, Richardson D, et al. Routine HIV testing in acute hospital admissions. HIV Med 2016; 17: 634. [DOI] [PubMed] [Google Scholar]
- 45.Elmahdi R, Gerver S, Gomez Guillen G, et al. Low levels of HIV test coverage in clinical settings in the UK: a systematic review of adherence to 2008 guidelines. Sex Transm Infect 2014; 90: 119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Deblonde JDKP, Hamers FF, Fontaine J, et al. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health 2010; 20: 422–432. [DOI] [PubMed] [Google Scholar]
- 47.Pringle K, Merchant RC, Clark MA. Is self-perceived HIV risk congruent with reported HIV risk among traditionally lower HIV risk and prevalence adult emergency department patients? Implications for HIV testing. AIDS Patient Care STDS 2013; 27: 573–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lekas HM, Schrimshaw EW, Siegel K. Pathways to HIV testing among adults aged fifty and older with HIV/aids. AIDS Care 2005; 17: 674–687. [DOI] [PubMed] [Google Scholar]
- 49.Nusbaum MR, Hamilton C. The proactive sexual health history. Am Fam Physician 2002; 66: 1705–1712. [PubMed] [Google Scholar]
- 50.Pakpreo P. Why do we take a sexual history? Virtual Mentor 2005; 7: 677–682. [DOI] [PubMed] [Google Scholar]
- 51.Faulder GS, Riley SC, Stone N, et al. Teaching sex education improves medical students’ confidence in dealing with sexual health issues. Contraception 2004; 70: 135–139. [DOI] [PubMed] [Google Scholar]
- 52.Ashton MR, Cook RL, Wiesenfeld HC, et al. Primary care physician attitudes regarding sexually transmitted diseases. Sex Transm Dis 2002; 29: 246–251. [DOI] [PubMed] [Google Scholar]
- 53.Torkko KC, Gershman K, Crane LA, et al. Testing for chlamydia and sexual history taking in adolescent females: results from a Statewide Survey of Colorado primary care providers. Pediatrics 2000; 106: E32. [DOI] [PubMed] [Google Scholar]
- 54.Siegel K, Dean L, Schrimsha E. Symptom ambiguity among late-middle-aged and older adults with HIV. Research on Aging 1999; 21: 595–618. [Google Scholar]
- 55.Siegel K, Schrimshaw EW, Dean L. Symptom interpretation: implications for delay in HIV testing and care among HIV-infected late middle-aged and older adults. AIDS Care 1999; 11: 525–535. [DOI] [PubMed] [Google Scholar]
- 56.Alencar RA, Ciosak SI. Aids in the elderly: reasons that lead to late diagnosis. Rev Bras Enferm 2016; 69: 1140–1146. [DOI] [PubMed] [Google Scholar]
- 57.Moore LW, Amburgey LB. Older adults and HIV. AORN J 2000; 71: 873–876. [DOI] [PubMed] [Google Scholar]
- 58.Pratt G, Gascoyne K, Cunningham K, et al. Human immunodeficiency virus (HIV) in older people. Age and Ageing 2010; 39: 289–294. [DOI] [PubMed] [Google Scholar]
- 59.Lin Y, Garner S, Lau J, et al. Prevalence of HIV indicator conditions in late presenting patients with HIV: a missed opportunity for diagnosis? QJM 2019; 112: 17–21. [DOI] [PubMed] [Google Scholar]
- 60.Wohlgemut J, Lawes T, Laing R. Trends in missed presentations and late HIV diagnosis in a UK teaching hospital: a retrospective comparative cohort study. BMC Infect Dis 2012; 12: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mensforth S, Goodall L, Bodasing N, et al. Late diagnosis among our ageing HIV population: a cohort study. J Int AIDS Soc 2014; 17(Suppl. 3): 19692. [DOI] [PMC free article] [PubMed] [Google Scholar]