Abstract
Background:
There are 2 treatment options for adolescent athletes with anterior cruciate ligament (ACL) injuries—rehabilitation alone (nonsurgical treatment) or ACL reconstruction plus rehabilitation. However, there is no clear consensus on how to include strength and neuromuscular training during each phase of rehabilitation.
Purpose:
To develop a practical consensus for adolescent ACL rehabilitation to help provide care to this age group using an international Delphi panel.
Study Design:
Consensus statement.
Methods:
A 3-round online international Delphi consensus study was conducted. A mix of open and closed literature-based statements were formulated and sent out to an international panel of 20 ACL rehabilitation experts. Statements were divided into 3 domains as follows: (1) nonsurgical rehabilitation; (2) prehabilitation; and (3) postoperative rehabilitation. Consensus was defined as 70% agreement between panel members.
Results:
Panel members agreed that rehabilitation should consist of 3 criterion-based phases, with continued injury prevention serving as a fourth phase. They also reached a consensus on rehabilitation being different for 10- to 16-year-olds compared with 17- and 18-year-olds, with a need to distinguish between prepubertal (Tanner stage 1) and mid- to postpubertal (Tanner stages 2-5) athletes. The panel members reached a consensus on the following topics: educational topics during rehabilitation; psychological interventions during rehabilitation; additional consultation of the orthopaedic surgeon; duration of postoperative rehabilitation; exercises during phase 1 of nonsurgical and postoperative rehabilitation; criteria for progression from phase 1 to phase 2; resistance training during phase 2; jumping exercises during phase 2; criteria for progression from phase 2 to phase 3; and criteria for return to sports (RTS). The most notable differences in recommendations for prepubertal compared with mid- to postpubertal athletes were described for resistance training and RTS criteria.
Conclusion:
Together with available evidence, this international Delphi statement provides a framework based on expert consensus and describes a practice guideline for adolescent ACL rehabilitation, which can be used in day-to-day practice. This is an important step toward reducing practice inconsistencies, improving the quality of rehabilitation after adolescent ACL injuries, and closing the evidence-practice gap while waiting for further studies to provide clarity.
Keywords: adolescent athlete, anterior cruciate ligament injury, nonsurgical rehabilitation, postoperative rehabilitation, prehabilitation
Anterior cruciate ligament (ACL) ruptures are among the most severe knee injuries in children and adolescents, and their annual incidence has increased 2-fold from 2004 to 2014 in Finnish girls and boys.2,26 Also, secondary ACL rupture rates (ACL graft ruptures and contralateral ACL tears) are up to 2.7 times higher in adolescents than in adults.6,25,28 According to the International Olympic Committee (IOC), there are 2 possible treatment options for children and adolescents with an ACL rupture—rehabilitation alone (nonsurgical treatment) or surgical ACL reconstruction (ACLR) plus rehabilitation.2,16 The goals of each treatment regimen are to restore a stable, well-functioning knee to reduce the impact of existing meniscal or chondral injury, limit the risk of future injury, and minimize the risk of growth disturbances. 2
The IOC statement recommends the use of a multistage criteria-based rehabilitation—3 supervised rehabilitation phases plus a fourth phase of ongoing injury prevention. 2 In a supplement to the IOC statement, some specific exercises to perform during all the 3 rehabilitation phases are described; however, a clear consensus on how to include strength and neuromuscular training during each phase of this rehabilitation is lacking. Also, it is not described which treatment modalities are needed in addition to this short list of exercises. 2 Moreover, the specific functional performance tests used as criteria to progress from one phase to another or to return to sports (RTS) are extracted from a systematic review and practice guideline that described rehabilitation for athletes aged ≥16 years. 24 A recent review of RTS criteria after ACL injuries or reconstruction for children and adolescents concluded that many studies used “adult” RTS tests in the adolescent population. 7 It is unknown whether these tests are valid in this younger population. 7 As a result, the day-to-day practitioner may still be uncertain about how to rehabilitate patients and when to allow RTS for adolescent athletes after an ACL injury or ACLR.
It is this gap in research that encouraged the development of this practical consensus to help provide care for this age group.
Consensus Methods
Terminology
During the Delphi process, we chose to use the term “adolescent” instead of “pediatric” or “child.” This is because according to the World Health Organization, children are 2 to 9 years old, adolescents are 10 to 18 years old, and young adults are aged ≥19 years. 29 In our opinion, the term “pediatric,” which is a collective term for children and adolescents, should be avoided when referring to specific age groups. 29
We were aware of the fact that the adolescent age group considers athletes at different physical development stages. Instead of using the definitions “skeletally immature” and “skeletally mature,” which are terms based on radiological findings that could be important when deciding to operate or not, we chose to use the terms “prepubertal” (Tanner stage 1), “mid-pubertal” (Tanner stage 2-3), and “postpubertal” (Tanner stage 4-5) to differentiate between stages of physical development.13,14 Self-rated Tanner staging—both by the adolescents or their parent(s)—has been shown to have a good association with the onset of puberty (Tanner stage 1 vs stages 2-5). Self-rated Tanner staging is easy to use in day-to-day practice for every sports medicine professional. 3
Delphi Consensus Domains
Based on recent literature covering the rehabilitation of adults and adolescents after an ACL injury or ACLR, we defined 3 rehabilitation domains—nonsurgical rehabilitation; prehabilitation; and postoperative rehabilitation.2,7,24
Although sport levels and concomitant injuries could also influence these domains—in terms of minimum duration and specific exercises—our goal was to develop a rehabilitation framework for recreational adolescent patients with ACL injuries who participated in cutting or pivoting sports before their injury, with no concomitant injuries or procedures that could influence the duration of the rehabilitation protocol. Elite athletes and athletes with concomitant injuries that influence rehabilitation duration fall outside of this framework and may need a more experienced clinician to guide rehabilitation.
International Delphi Expert Panel
Panel members were recruited via the personal network of the first author (N.v.M.) and social media. They could only participate in this Delphi consensus study if they were rehabilitating adolescent athletes with ACL injuries on a regular basis. They did not need to be researchers per se. Panel members were contacted by email in January 2021 and invited to participate in a 3-round online Delphi consensus. Twenty international panel members agreed to participate. Their characteristics are listed in Table 1.
Table 1.
Characteristics of the International Delphi Expert Panel (N = 20) a
| Characteristic | Value |
|---|---|
| Profession | |
| Sports physical therapist | 9 |
| Sports physical therapist and junior researcher | 6 |
| Sports physical therapist and postdoctoral researcher | 5 |
| Work location | |
| Africa | 0 |
| Asia | 1 |
| Europe | 6 |
| North America | 8 |
| Oceania | 3 |
| South America | 0 |
| Work experience with adolescent athletes with ACL injuries, years | 15 (7-30) |
| The annual number of athletes with ACL injuries | 20 (3-150) |
a Data are reported as No. of panelists or median (range). ACL, anterior cruciate ligament.
Delphi Procedure
All panel members agreed to use the 2018 IOC statement 2 and the 2016 ACL practice guideline 24 as the starting point for this Delphi consensus process. A mix of open and closed literature-based questions regarding rehabilitation and RTS in adolescent athletes with ACL injuries was formulated and sent out to the panel members. The first Delphi round aimed at developing a rehabilitation framework. The second and third Delphi rounds were used to ask more in-depth questions about training parameters in different rehabilitation phases. Consensus was defined as 70% agreement between the panel members.1,9,15,22 All but 1 panel member agreed on this percentage.
Results
Rehabilitation According to Patient Age and Physical Development
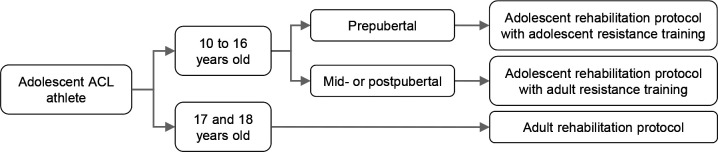
Regarding patient age and stage of physical development, adolescent patients with ACL injuries can be divided into different groups, for which rehabilitation protocols and RTS criteria differ. Two age groups were used when describing high-quality rehabilitation in detail as follows: 10- to 16-year-olds and 17- and 18-year-olds (Figure 1).
Figure 1.
Rehabilitation according to age and physical development for adolescent athletes with ACL injuries. ACL, anterior cruciate ligament.
Distinguishing between pre-, mid-, and postpubertal athletes is of importance in 10- to 16-year-olds. These phases are directly related to the hormonal production and influence on the ability to adapt to resistance training. 5 Changes in blood concentrations of sex hormones might play a key role in the observed differences in strength gains between immature and mature athletes. 5 If so, one would expect trainability to increase significantly with the onset of puberty because of the sudden increases in sex hormones during that time. 5 The increase in hormones will give boys a boost through strengthening, while girls may add fat mass during puberty, which reduces strength relative to body weight.27,30 Strength gains in prepubertal athletes will be slower and mainly due to an increase in the number of motor neurons that are recruited with each contraction, while in mid- and postpubertal athletes, strength gains are more likely associated with muscle hypertrophy. 20 Therefore, the panel members reached a consensus (80%) about midpubertal athletes being treated similarly to postpubertal athletes when it comes to resistance training. Only prepubertal athletes need to be treated differently. These differences will be outlined below when describing rehabilitation in detail.
The panel members reached a consensus (95%) regarding 17- and 18-year-old adolescents being treated according to an “adult” rehabilitation protocol as defined in the 2016 ACL practice guideline. 24 However, some details differed between 17- and 18-year-olds and adults, which are as follows:
It would be ideal to consider the biological age of 17- and 18-year-old athletes since their hormonal response to training could be limited if they are not mid- or postpubertal (85% consensus). In day-to-day practice, this would only be considered if the adolescent is not responding to resistance training as expected.
Additional attention needs to be paid to social support from parents and/or coaches (90% consensus).
Concerning postoperative ACL rehabilitation, a consensus was reached (95%) for RTS progression in 2 steps. Patient with ACL injuries aged 17 to 18 years are allowed to RTS (full training) after 9 months but only when they are able to meet the “adult” RTS criteria. From 9 to 12 months postoperatively, patients will progress their independence toward the preinjury sport level. These guidelines and treatment recommendations always need to be tailored to the patient.
Educational Topics During Rehabilitation
Education of both patients and parents is important during every rehabilitation domain, both for 10- to 16-year-olds and 17- and 18-year-olds. All topics that reached consensus are listed in Table 2.
Table 2.
Educational Topics During Nonsurgical Rehabilitation, Prehabilitation, or Postoperative Rehabilitation With >70% Consensus a
| Educational Topic | Domains |
|---|---|
| Patients and parents’ expectations | Non, Pre, Post |
| Key stakeholders during the rehabilitation process | Non, Pre, Post |
| School requirements and social activity expectations within the first several weeks of rehabilitation | Non, Pre, Post |
| A short overview of the rehabilitation period | Non, Pre, Post |
| Variability in recovery between athletes | Non, Pre, Post |
| Knee symptoms and when to visit a physical therapist or an orthopaedic surgeon | Non, Post |
| Long-term knee health and appropriate activities safe for the current level of function | Non, Post |
| Injury prevention | Non, Post |
| Realistic minimum RTS targets | Non, Post |
| Realistic minimum RTS times | Non, Post |
| Risks and benefits of nonsurgical rehabilitation | Non |
| Details of surgery | Pre |
| Details of the first postoperative week, including use of crutches, transfers, home management, and first postoperative exercises | Pre |
| Details of further postoperative rehabilitation | Pre |
a Non, nonsurgical rehabilitation; Post, postoperative rehabilitation; Pre, prehabilitation; RTS, return to sports.
Psychological Interventions During Rehabilitation
For all adolescent athletes with ACL injuries, psychological interventions are also an important part of rehabilitation. A consensus was reached by the panel for short-term goal setting (100%) and graded exposure (75%). Other psychological treatment regimens (eg, imagery, meditation, breathing techniques, and discussion groups with fellow patients) were used by <70% of panel members.
Additional Consultation With the Orthopaedic Surgeon
In addition to prearranged outpatient appointments with the orthopaedic surgeon, there could be a few important reasons to schedule an additional consultation during the rehabilitation process. These reasons are divided into 4 main topics as follows: (1) concerns for serious medical complications; (2) concerns for motion complications; (3) concerns for reinjury; (4) and concerns for failure to progress. Each consensus-based reason is listed in Table 3.
Table 3.
Reasons With >70% Consensus to Schedule Additional Outpatient Consultations With the Orthopaedic Surgeon During the Rehabilitation Process a
| Topic and Reason | Domain |
|---|---|
| Concerns for serious medical complications | |
| Issues with wound healing or potential infection | Post |
| Suspicion of deep vein thrombosis | Post |
| Concerns for motion complications | |
| Persistent passive knee extension deficit beyond 6 weeks (indicative of arthrofibrosis) | Post |
| Worsening passive knee extension deficit with anterior knee pain if forced (indicative of cyclops lesion) | Post |
| Concerns for reinjury | |
| New trauma, recurrence of giving way, and/or positive Lachman or pivot-shift test (indicative of graft failure) | Post |
| Knee locking (indicative of meniscal or chondral defects) | Non, Pre, Post |
| Concerns for failure to progress | |
| Persistent effusion, despite appropriate rehabilitation | Non, Pre, Post |
| Prolonged (postoperative) pain interfering with rehabilitation | Non, Post |
a Non, nonsurgical rehabilitation; Post, postoperative rehabilitation; Pre, prehabilitation.
Rehabilitation Domains for 10- TO 16-Year-Olds
Nonsurgical and postoperative rehabilitation are similar in many ways. Therefore, we decided to describe these domains together. It will be explicitly stated if specific exercises are different between those domains. Prehabilitation—the rehabilitation period before surgery—is described separately. However, phases and exercises from nonsurgical rehabilitation could be copied to this domain, depending on the time spent in prehabilitation.
Prehabilitation
Duration of Prehabilitation
The panel members did not reach a consensus on the duration of prehabilitation. According to 12 panel members (60%), only meeting the criteria is important, not the time. The other 8 panel members argued that meeting the criteria is important as well but aimed for a minimum duration of 3 to 6 weeks (25%), 6 to 8 weeks (10%), and 12 weeks (5%).
Criteria for Surgery
A minimum set of criteria an athlete should meet before undergoing an ACLR is described in Table 4.
Table 4.
A Minimum Set of Criteria an Adolescent Athlete With ACL Injury Should Meet Before Undergoing Surgery a
| Clinical Signs | Neuromuscular Control | Psychology |
|---|---|---|
| • Trace to no effusion (95% consensus) • Full ROM, particularly extension, minor flexion loss (>95% compared with noninjured knee or 120° at minimum) is acceptable (100% consensus) • Minimal to no pain (NPRS, 2 at most) (80% consensus) |
• Ability to control lower limb alignment during functional tasks (90% consensus) • Good quadriceps function, defined as SLR without lag and ability to control the knee during gait and single-leg stance (90% consensus) • Normal gait without crutches (90% consensus) |
• Emotional readiness for surgery and postoperative rehabilitation (80% consensus) |
a ACL, anterior cruciate ligament; NPRS, Numeric Pain Rating Scale; ROM, range of motion; SLR, straight leg raise.
Nonsurgical and Postoperative Rehabilitation
When describing nonsurgical rehabilitation, 2 groups of athletes emerge. First, those who try to avoid surgery completely and tend to manage their ACL injury nonsurgically. Their main goal is to return to their desired activities without any episodes of functional instability or additional knee injuries.
Second, those who are skeletally immature receive the advice to postpone surgery until they have reached skeletal maturity. According to expert opinion, this latter group would benefit from additional education regarding activity modification to avoid functional instability or recommendations for wearing a knee brace during pivoting activities. 2 This period of nonsurgical rehabilitation would be comparable with an extended version of preoperative rehabilitation, as some will eventually undergo surgery.
Similar to postoperative rehabilitation, nonsurgical rehabilitation should consist of 3 criterion-based phases (85% consensus), with a fourth phase of continued injury prevention (95% consensus). The “11+ Kids” program is advised as a secondary prevention program with 75% consensus.4,18 This program was originally designed as a warm-up exercise routine for 7- to 13-year-old children and has been proven to reduce injuries, improve performance, and reduce health care costs compared with a regular warm-up.4,17–19
Duration of Rehabilitation
The panel members did not reach a consensus regarding the duration of nonsurgical rehabilitation. Eleven panel members (55%) stated that the time is not important but only meeting the criteria is. The other 9 panel members argued that meeting the criteria is important as well but aimed for a minimum duration of 3 to 4 months (10%), 6 months (25%), and 9 months (10%).
Adolescent patients who had an ACLR should only return to full group training postoperatively when they meet the RTS criteria. At least 4 to 6 weeks of full group training are needed before returning to competition (85% consensus). As described before in the IOC statement, 2 patients should not return to pivoting sports competitions 12 months after ACLR (75% consensus).
Phase 1 of Nonsurgical and Postoperative Rehabilitation
General Principles of Phase 1
The panel members agreed (70% consensus) that prepubertal and mid- to postpubertal athletes could be treated the same way in phase 1.
Exercises During Phase 1
The IOC statement 2 already recommends the following exercises to be performed in phase 1: stationary bicycling; active extension (unloaded); quadriceps setting; squat variations with and without support; single-limb standing (with control of isometric terminal knee extension); and closed chain hip and pelvic control exercises. The panel members reached a consensus on additional exercises as follows:
Heel props or prone hangs when needed to reach full extension (95% consensus)
Straight leg raises (without extension lag) (85% consensus)
Prone hip extensions (75% consensus)
Side-lying abductions (75% consensus)
Standing position pulley/elastic band–resisted terminal knee extensions (70% consensus)
Heel raises (75% consensus)
Gait retraining (85% consensus)
Prescribing any exercise is dependent on individual limitations in function.
Criteria for Progression From Phase 1 to Phase 2
Table 5 lists all criteria that should be met before progressing from phase 1 to phase 2 during nonsurgical or postoperative rehabilitation. The panel members added 2 criteria to the preexisting list of 3 criteria from the IOC statement. 2 These criteria to progress are the same for prepubertal and mid- to postpubertal athletes.
Table 5.
Minimum Set of Criteria for Progressing From Phase 1 to Phase 2 During Nonsurgical or Postoperative Rehabilitation a
| Clinical Signs | Neuromuscular Control | Psychology |
|---|---|---|
| • Trace to no effusion
a
• Full active extension and 120° of flexion a |
• Ability to hold terminal knee extension during single-leg standing
a
• Correct gait pattern without crutches (85% consensus) |
• Emotionally ready to start phase 2 resistance training exercises (70% consensus) |
a Already included in the International Olympic Committee consensus statement. 2
Phase 2 of Nonsurgical and Postoperative Rehabilitation
General Principles of Phase 2
The panel members reached a consensus regarding the rehabilitation of adolescent athletes needing extra focus on neuromuscular training and movement quality and less on resistance training (75% consensus) compared with adult rehabilitation. Additionally, more parental involvement is needed in adolescents (80% consensus).
Resistance Training During Phase 2
All resistance exercises for both prepubertal and mid- to postpubertal athletes recommended by the panel members are listed in Table 6.
Table 6.
Resistance Exercises Recommended for Prepubertal and Mid- to Postpubertal Athletes a
| Quadriceps-Dominant Exercises | Hamstring-Dominant Exercises | Other |
|---|---|---|
| • Double- or single-leg knee extension variations (isometrics, isometrics against Powerball, resistance from elastic bands or machine) (100% consensus) • Double- or single-leg leg press (80% consensus) • Double- or single-leg squat variations (isometrics, minisquat, TRX-assisted squat, Spanish squat, Bulgarian split squat, pistol squat) (95% consensus) • Lunges in all directions (75% consensus) • Hip thrust variations (75% consensus) |
• Double- or single-leg bridge variations (isometrics, bent or straight knee, with Powerball) (80% consensus) • Double- or single-leg hamstring curl variations (prone lying or standing, with Powerball, resistance from elastic bands or machine) (75% consensus) • Double- or single-leg dead lift variations (Romanian, stiff-legged, hip hinge) (75% consensus) |
• Hip abduction variations (side-lying or standing, resistance from elastic bands or pulley) (70% consensus) • Double- or single-leg straight knee calf raise variations (standing, jumping rope) (85% consensus) • Double- or single-leg bent knee calf raise variations (seated or standing) (80% consensus) • Trunk exercises (70% consensus) |
| Combined exercises (eg, squat to lunge, Romanian dead lift to step up) (85% consensus) | ||
a Powerball, a large (diameter, 40-75 cm) inflatable ball, also called a gym ball or an exercise ball; TRX, a lightweight suspension training tool that enables bodyweight exercises against gravity.
As stated earlier in this Delphi consensus, phase 2 is different for prepubertal athletes compared with mid- to postpubertal athletes, especially because of the differences in hormonal response to resistance training. The main focus during resistance training for prepubertal athletes is maintaining correct movement quality. Resistance training for prepubertal athletes could be progressed according to the following steps (95% consensus):
Start with functional movements and an emphasis on technical development with correct movement quality (low load, 15-25 repetitions);
Progress to resistance training (increase load; decrease repetitions to <12; rate of perceived exertion, 7-9): combine body weight exercises (from double- to single-leg, or combined exercises) and plyometric type exercises with fun and gamelike elements (manipulating tempo, use ball throws or unstable surfaces).
Mid- to postpubertal athletes are able to follow resistance training programs designed for adults (95% consensus). Such an adult program could be designed as follows:
One or 2 exercises (quadriceps dominant, eg, squat) with progression according to the size principle and reversed size principle;
Other exercises with progression to 3 to 4 sets of 8 to 12 repetition maximum, and only increases in weights thereafter.
Jumping Exercises During Phase 2
The panel members reached a consensus (80%) that hopping and jumping should be part of phase 2. To start jumping and running in phase 2, athletes should have equal range of motion, no effusion, and sufficient leg strength (limb symmetry index [LSI] >70%) (85% consensus). There should always be a focus on correct movement quality during jumping. Progression for both prepubertal and mid- to postpubertal athletes is recommended as follows (85% consensus):
Partial weightbearing jumps or prejumping tasks as minitramp marching (focus on neuromuscular control, gain confidence);
Double-leg drop downs from a small height (to gain confidence in landing and encourage symmetrical loading);
Double-leg vertical jumps (countermovement jumps, squat jumps, tuck jumps, rope jumps);
Double-leg horizontal jumps (broad jumps);
Double-leg plyometric work;
Change direction from forward and upward to backward, lateral, diagonal, and rotational;
Progress as above for double- to single-leg jumps;
Progress as above for single-leg jumps;
Add variations and external challenges in terms of height (eg, boxes, hurdles), pacing (athlete-controlled timing to externally paced activities), speed, surface, sensory input (eyes open/eyes closed), perturbation (push by a physical therapist or unanticipated location and direction), and cognitive load (external demands of attention, double tasks).
Criteria for Progression From Phase 2 to Phase 3
Table 7 lists all criteria that should be met before progressing from phase 2 to phase 3 during nonsurgical or postoperative rehabilitation. These were already prescribed by the IOC statement. 2 These criteria are the same for prepubertal and mid- to postpubertal athletes.
Table 7.
Minimum Set of Criteria for Progressing From Phase 2 to Phase 3 During Nonsurgical or Postoperative Rehabilitation a
| Clinical Signs | Neuromuscular Control |
|---|---|
| • No effusion • Full ROM |
• Ability to jog for 10 minutes with good form and no subsequent effusion • LSI >80% on the single-leg sit-to-stand test (prepubertal athletes only) or isokinetic quadriceps and hamstrings strength (mid- to postpubertal athletes only) • LSI >80% on hop tests (mid- to postpubertal athletes only) |
a LSI, limb symmetry index; ROM, range of motion.
Phase 3 of Nonsurgical and Postoperative Rehabilitation
General Principles of Phase 3
The emphasis in phase 3 should be on returning to training in a gradual progression from highly controlled to highly chaotic activity-related tasks. This could be under the supervision of a skilled physical therapist or physical trainer, in consultation with a club trainer (85% consensus).
Prepubertal athletes should have more restrictions and supervision on the field than mid- to postpubertal athletes because they have limited capacity to appraise risk and differentiate between safe and unsafe situations (90% consensus). Also, the progression of resistance training exercises remains different between prepubertal and mid- to postpubertal athletes.
Criteria for RTS
According to panel members (85% consensus), clearance for RTS should always be a shared decision-making process between the patient, parents, physical therapist, and orthopaedic surgeon. Table 8 highlights all RTS criteria.
Table 8.
A Minimum Set of Criteria for RTS Clearance a
| Clinical Signs | Neuromuscular Control | Psychology |
|---|---|---|
| • No functional instability episodes (95% consensus) • No effusion (100% consensus) • Full ROM (100% consensus) • Pain-free in tasks that mimic their goal (95% consensus) |
• LSI >95% on the single-leg sit-to-stand test (prepubertal athletes only) (70% consensus) • LSI >95% isokinetic quadriceps and hamstrings strength (mid- to postpubertal athletes only) (85% consensus) • LSI >95% on the hop test battery (mid- to postpubertal athletes only) (80% consensus) • Movement quality during videotaped single-leg hopping and jumping variations (70% consensus) • Movement quality during videotaped field training (jumping, landing, accelerating, decelerating, cutting) (70% consensus) |
• Confident in tasks that mimic their goal (75% consensus) • Psychological readiness measured with ACL-RSI (mid- to postpubertal athletes only) (85% consensus) |
a ACL-RSI, Anterior Cruciate Ligament–Return to Sport after Injury scale; LSI, limb symmetry index; ROM, range of motion.
Using this Guideline in Day-to-Day Practice
When an adolescent athlete with an ACL injury has one’s first appointment, it is important to know how to apply this practice guideline to that specific athlete. Most 17- and 18-year-old athletes with ACL injuries could be treated according to adult ACL practice guidelines 24 (see Figure 1). A prolonged rehabilitation until 12 months should be considered for this age group. The treatment algorithm for 10- to 16-year-old athletes with ACL injuries in Figure 2 could help in translating Delphi study results to day-to-day practice.
Figure 2.
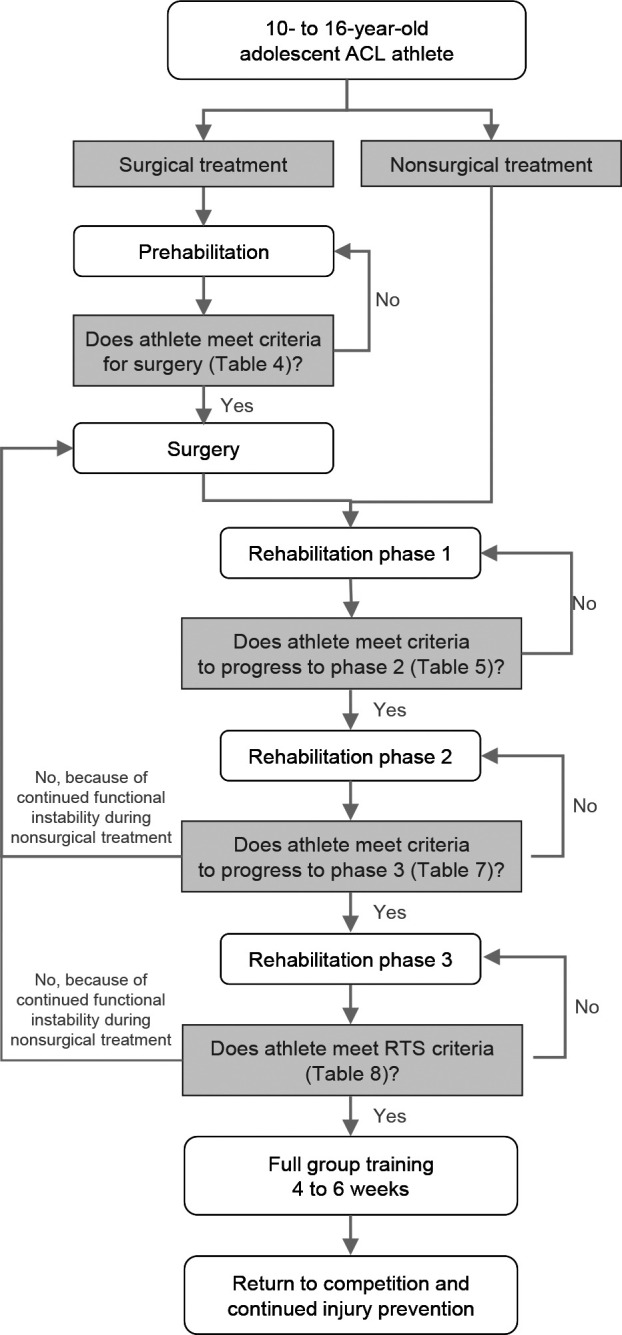
Treatment algorithm for 10- to 16-year-old adolescent athletes with ACL injuries. ACL, anterior cruciate ligament; RTS, return to sports.
First, it is important to know whether a treatment decision has already been made. Will the adolescent athlete have surgical treatment as soon as possible, opt for nonsurgical treatment, or start with nonsurgical treatment and proceed to surgical treatment when skeletally mature? If the treatment decision has not yet been made, physical therapists play an important role in educating the patient and parents (see Table 2).
Second, as discussed with the panel members, a distinction should be made between 10- to 16-year-old and 17- and 18-year-old athletes. The latter could be treated according to adult rehabilitation guidelines, 24 while 10- to 16-year-old athletes need an adapted adolescent rehabilitation protocol, which is described in this Delphi consensus practice guideline. The most important differences between adult and adolescent (10- to 16-year-old) rehabilitation are as follows: more emphasis on neuromuscular training and movement quality for adolescents; more parental involvement for adolescents; and longer postoperative rehabilitation for adolescents (a minimum of 12 months vs a minimum of 9 months). The recommendation for a longer postoperative rehabilitation is based on expert opinion as a means to reduce reinjuries; however, there is no evidence to support the benefits or downsides of a 12-month versus a 9-month rehabilitation period.
Third, physical therapists should distinguish between prepubertal athletes and mid- to postpubertal athletes, which can easily be done using the self-rated Tanner staging. 3 This is important since resistance training principles are dependent on these physical development stages. Also, the criteria to progress during rehabilitation or the criteria for RTS clearance differ between those groups. Prepubertal athletes should preferably not be measured with isokinetic strength tests or hop tests alone, as these tests require a change above 16% to 25% to represent a true change in this specific group of athletes. 11 In comparison, the measurement error for isokinetic strength tests in young adults (≥19 years) is <5%; thus, these tests are possibly less useful in day-to-day practice for prepubertal athletes. 8 Therefore, the panel members chose to add a single-leg sit-to-stand test for these prepubertal athletes (Table 9). This test has high intertester reliability (intraclass correlation coefficient, 0.960) and a good negative correlation with hip and knee extensor strength (r = –0.72 and –0.711, respectively) in healthy young adults. 21 Although it has been used in adolescents with various injuries, the reliability and validity of this test in athletes with ACL injuries in this age group are unknown.
Table 9.
The Single-Leg Sit-to-Stand Test
| • Use a chair (or treatment table) without arms and backrest that could be adjusted in height to have 90° of flexion at both the hip and knee. |
| • The test is performed barefooted, with the arms folded across the chest. |
| • The opposing limb has to be lifted just above the floor throughout the whole test. If this leg touches the floor, the test is invalid. |
| • Instruction: “Rise from the chair 5 times as fast as possible. Fully extend your hip and knee when standing and make firm contact with the chair when sitting.” Start timing when the physical therapist says “go” and stop when the athlete sits on the chair for the fifth time. |
| • Perform 2 valid trials and register the fastest one for calculating a limb symmetry index. |
Finally, the panel members decided to use an LSI >95% on isokinetic strength tests, hop tests, and the single-leg sit-to-stand test. A stricter criterion than applied to adults, where an LSI of >90% is common.10,12,23 The predictive validity of this LSI criterion and all RTS criteria has not yet been examined in adolescents; thus, we challenge the day-to-day practitioner to be critical and perform sound clinical reasoning when deciding to clear an adolescent athlete with an ACL injury to RTS.
Conclusion
Rehabilitation of adolescent athletes with ACL injuries remains challenging because of a lack of evidence-based guidance for treatment decisions. This international Delphi study provides a framework based on expert consensus and describes a practice guideline for adolescent ACL rehabilitation, which can be used in day-to-day practice. This is an important step toward reducing practice inconsistencies, improving the quality of rehabilitation of adolescent athletes after ACL injuries, and closing the evidence-practice gap while waiting for further studies to provide clarity.
Authors
William Claussen, PT (Shelbourne Knee Center at Community Hospital East, Indianapolis, Indiana, USA); Elliot M. Greenberg, PT, DPT, PhD (Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, USA); Hege Grindem, PT, PhD (Oslo Sport Trauma Research Center, Department of Sports Medicine, Norwegian School of Sports Sciences, Oslo, Norway; Stockholm Sports Trauma Research Center, Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm, Sweden); Sharon Kearney, PT (Netball New Zealand, Ellerslie, New Zealand); Matthijs van Keulen, PT, MSc (SMC Amsterdam, Amsterdam, the Netherlands); Martijn Lips, PT, MSc (Medifit Fysiotherapie, Breda, the Netherlands; SOMT University of Physiotherapy, Amersfoort, the Netherlands); Lenny Macrina, PT, MSPT, SCS, CSCS (Champion PT & Performance, Waltham, Massachusetts, USA); David McWilliam, PT (Alder Hey Children’s Hospital, Alder Hey Children’s NHS Foundation Trust, Liverpool, UK); Håvard Moksnes, PT, PhD (Oslo Sports Trauma Research Center [OSTRC], Oslo, Norway; Idrettens Helsesenter, Oslo, Norway) Richard Norris, PT, MSc (Department of Trauma and Orthopaedics, Aintree University Hospital, Liverpool, UK); Mark V. Paterno, PT, PhD (Cincinnati Children’s Hospital Medical Center, Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA); Brice Picot, PT, PhD candidate (French Handball Federation, Creteil, France; French Society of Sports Physical Therapists [SFMKS Lab], Pierrefite, France; Inter-University Laboratory of Human Movement Biology [LIBM], Savoie Mont-Blanc University, Chambéry, France); David Piskulic, PT, DPT, SCS, ATC (Young Athlete Center, St Louis Children’s Hospital, St Louis, Missouri, USA); Luis F. Prato, PT, DPT (Lakeshore Bone and Joint Institute Sports Rehabilitation and Health Enhancement Center, Portage, Indiana, USA); Timothy A. Sayer, PT, PhD (Department of Physiotherapy, Melbourne School of Health Sciences, The University of Melbourne, Victoria, Australia; Melbourne CBD Physiotherapy, Victoria, Australia); Faraz Sethi, PT, MSc (Valiant Clinic and Hospital, Dubai, United Arab Emirates); Holly Silvers-Granelli, PT, MPT, PhD (Velocity Physical Therapy, Santa Monica, California, USA; Major League Soccer Medical Committee, New York, New York, USA); Linda Truong, PT, PhD candidate (Faculty of Physical Therapy, Department of Medicine, University of British Columbia, Vancouver, Canada; Arthritis Research Canada, Vancouver, Canada); Matthew Whalan, PT, PhD (Centre of Medical and Exercise Physiology, School of Medical, Indigenous & Health Sciences, University of Wollongong, Australia; Medical Department, Football Australia, Sydney, Australia); Erik Witvrouw, PT, Prof. (Department of Rehabilitation Sciences, Faculty of Medicine and Health Sciences, Gent University, Belgium).
Footnotes
Final revision submitted February 6, 2023; accepted February 22, 2023.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1.Albarquoni L, Hoffman T, Straus S, et al. Core competencies in evidence-based practice for health care professionals: consensus statement based on a systematic review and Delphi study. JAMA Netw Open. 2018;1(2):e180281. [DOI] [PubMed] [Google Scholar]
- 2.Ardern CL, Ekås G, Grindem H, et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):989–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balzer BWR, Gardem FL, Amatoury M, et al. Self-rated Tanner stage and subjective measures of puberty are associated with longitudinal gonadal hormone changes. J Pediatr Edocrinol Metab. 2019;32(6):569–576. [DOI] [PubMed] [Google Scholar]
- 4.Beaudouin F, Rössler R, Aus der Fünten K, et al. Effects of the “11+ Kids” injury prevention programme on severe injuries in children’s football: a secondary analysis of data from a multicentre cluster-randomised controlled trial. Br J Sports Med. 2019;53(22):1418–1423. [DOI] [PubMed] [Google Scholar]
- 5.Behringer M, vom Heede A, Yue Z, Mester J. Effects of resistance training in children and adolescents: a meta-analysis. Pediatrics. 2010;126(5):e1199–e1210. [DOI] [PubMed] [Google Scholar]
- 6.Costa Astur D, Marcon Cachoeira C, da Silva Vieira T, Debieux P, Cohen Kaleka C, Cohen M. Increased incidence of anterior cruciate ligament revision surgery in paediatric versus adult population. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1362–1366. [DOI] [PubMed] [Google Scholar]
- 7.Dietvorst M, Brzoskowski M, van der Steen M, Delvaux E, Janssen RPA, van Melick N. Limited evidence for return to sport testing after ACL reconstruction in children and adolescents under 16 years: a scoping review. J Exp Orthop. 2020;7(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duarte JP, Valente-dos-Santos J, Coelho-e-Silva MJ, et al. Reproducibility of isokinetic strength assessment of knee muscle actions in adult athletes: torques and antagonist-agonist ratios derived at the same angle position. PLoS One. 2018;13(8):e0202261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gates M, Gates A, Pieper D, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ. 2022;378:e070849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grindem H, Engebretsen L, Axe M, Snyder-Mackler L, Risberg MA. Activity and functional readiness, not age, are the critical factors for second anterior cruciate ligament injury—the Delaware-Oslo ACL cohort study. Br J Sports Med. 2020;54(18):1099–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnsen MB, Eitzen I, Moksnes H, Risberg MA. Inter- and intrarater reliability of four single-leg hop tests and isokinetic muscle torque measurements in children. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):1907–1916. [DOI] [PubMed] [Google Scholar]
- 12.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 13.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45(239):13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in girls. Arch Dis Child. 1969;44(235):291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCall A, Pruna R, van der Horst N, et al. Exercise-based strategies to prevent muscle injury in male elite footballers: an expert-led Delphi survey of 21 practitioners belonging to 18 teams from the Big-5 European Leagues. Sports Med. 2020;50(9):1667–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moksnes H, Engebretsen L, Risberg MA. The current evidence for treatment of ACL injuries in children is low: a systematic review. J Bone Joint Surg. 2012;94(12):1112–1119. [DOI] [PubMed] [Google Scholar]
- 17.Polmares-Noguera C, Ayala F, Robles-Palazón FJ, et al. Training effects of the FIFA 11 + Kids on physical performance in youth football players: a randomized control trial. Front Pediatr. 2018;6:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rössler R, Junge A, Bizzini M, et al. A multinational cluster randomised controlled trial to assess the efficacy of “11+ kids”: a warm-up programme to prevent injuries in children’s football. Sports Med. 2018;48(6):1493–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rössler R, Verhagen E, Rommers N, et al. Comparison of the “11+ Kids” injury prevention programme and regular warmup in children’s football (soccer): a cost effectiveness analysis. Br J Sports Med. 2019;53(5):309–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stricker PR, Faigenbaum AD, McCambridge TM; Council on Sports Medicine and Fitness. Resistance training for children and adolescents. Pediatrics. 2020;145(6):e20201011. [DOI] [PubMed] [Google Scholar]
- 21.Thongchoomsin S, Bovonsunthonchai S, Joseph L, Chamnongkich S. Clinimetric properties of the one-leg sit-to-stand test in examining unilateral lower limb muscle strength among young adults. Int J Clin Pract. 2020;74(9):e13556. [DOI] [PubMed] [Google Scholar]
- 22.van der Horst N, van Denderen R. Isokinetic hamstring and quadriceps strength interpretation guideline for football (soccer) players with ACL reconstruction: a Delphi consensus study in the Netherlands. Sci Med Footb. 2022;6(4):434–445. [DOI] [PubMed] [Google Scholar]
- 23.van Melick N, Pronk Y, Nijhuis-van der Sanden MWG, Rutten S, van Tienen TG, Hoogeboom TH. Meeting movement quantity or quality return to sport criteria is associated with reduced second ACL injury rate. J Orthop Res. 2022;40(1):117–128. [DOI] [PubMed] [Google Scholar]
- 24.van Melick N, van Cingel REH, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506–1515. [DOI] [PubMed] [Google Scholar]
- 25.Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 26.Weitz FK, Sillanpää PJ, Mattila VM. The incidence of paediatric ACL injury is increasing in Finland. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wells JCK. Sexual dimorphism of body composition. Best Pract Res Clin Endocrinol Metab. 2007;21(3):415–430. [DOI] [PubMed] [Google Scholar]
- 28.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. Adolescent health. Accessed January 12, 2021. https://www.who.int/health-topics/adolescent-health/#tab=tab_1
- 30.Xu Y, Wen Z, Deng K, Li R, Yu Q, Xiao SM. Relationships of sex hormones with muscle mass and muscle strength in male adolescents at different stages of puberty. PLoS One. 2021;16(12):e0260521. [DOI] [PMC free article] [PubMed] [Google Scholar]