Abstract
Background
Preterm infants display certain behaviors to communicate their needs, known as preterm infant cues. However, the existing research on preterm infant cues primarily draws from studies conducted on bottle-fed infants rather than breastfed infants.
Objective
This study aimed to investigate the concept of preterm infant cues during breastfeeding and its appropriate instruments.
Design
A scoping review.
Data Sources
The articles published up to January 2022 were searched from multiple sources from EBSCOhost Web, namely CINAHL Plus with Full Text, MEDLINE, ERIC, and E-Journals.
Review Methods
The articles retrieved for this review were screened using PICO (Population, Intervention, Comparison, and Outcomes) format. Preferred Reporting Items for Systematic Reviews (PRISMA) checklist was used in selecting the articles, and Joanna Briggs Institute Critical Appraisal was utilized by two independent authors to assess the articles’ quality. A descriptive method was used to analyze the data.
Results
The initial review stage found 183 potential articles, but only four satisfied the criteria. The notion of preterm infant cues during breastfeeding is centered on the actions of preterm infants while positioned on their mother's chest. These feeding cues are identifiable before, during, and after breastfeeding and include cues for hunger, self-regulation, stress, satiation, approach, avoidance, and sucking quality. To effectively recognize these cues, tools such as the Preterm Infants Cues Coding System (PFCCS), Infant Driven Scale (IDS), Newborn Individualized Developmental Care and Assessment Program (NIDCAP), and Preterm Breastfeeding Behavior Scale (PIBBS) can be utilized.
Conclusion
The study findings highlight the importance of recognizing preterm infant cues during breastfeeding to facilitate proper feeding and developmental care. Observational studies have proven to be an effective means of observing these cues during breastfeeding. By leveraging the cues identified in this review alongside tools such as PFCCS, IDS, NIDCAP, and PIBBS, nurses can accurately interpret preterm infants' breastfeeding cues in neonatal care settings of all levels. This, in turn, can aid in developing care plans that promote better feeding ability outcomes.
Keywords: breastfeeding, cues, preterm infants, newborn
Background
Breastfeeding is a complex relationship between a mother as a breastfeeding woman and her infant as a feeder (Bomer Norton, 2014). To build a positive interaction, Barnard's model suggests that the infant must be able to communicate its needs through cues or behaviors, while the mother must be able to identify these cues and respond accordingly to meet the infant's needs (Oxford & Findlay, 2015). This paper focuses on the concept of breastfeeding cues for infants, which refers to the ability of infants to communicate their needs through cues or behaviors. This concept is essential for nurses working in neonatal care at levels 1, 2, or 3, who assist mothers in providing breast milk to their infants receiving treatment. Nurses play a critical role in understanding infants' signals, such as when they are hungry, and educating mothers to recognize these signals so they can breastfeed effectively, promoting optimal growth and development of the infant.
Breastfeeding premature infants can be a challenging experience for mothers due to weak sucking reflexes and frequent falling asleep while feeding (Dosani et al., 2016). In addition, premature infants often have low birthweight (Purwandari & Huang, 2020) and encounter various difficulties while breastfeeding, including poor sucking, cyanosis, choking (Rommel et al., 2011), and breathing issues (Celik et al., 2013; Fanaro, 2013). As a result, premature infants may struggle to reach an optimal feeding level, and their mothers may have difficulty understanding their cues and needs. According to Dosani et al. (2016), mothers may not recognize choking as a distress signal or mistake an infant's disorganized behavior for satiation, leading to inadequate feeding. Furthermore, preterm infants may struggle to latch properly onto the nipple, become tired, and discontinue feeding (Dosani et al., 2016). These obstacles can prevent mothers from providing optimal breastfeeding for their premature infants. Nurses play a crucial role in helping mothers overcome these barriers and successfully breastfeed their premature infants.
Accordingly, nurses play a critical role in helping mothers identify and understand preterm infants' feeding cues during breastfeeding. However, studies on preterm infants' cues mainly focus on bottle feeding (Chen et al., 2017; Girgin et al., 2018; Griffith et al., 2017; Howe & Sheu, 2020; Pineda et al., 2020; White-Traut et al., 2017), and there is a lack of research specifically on preterm infants' cues during breastfeeding. A search on Google Scholar using the keywords "preterm infants cues and breastfeeding" from 2017 to 2022 did not yield any relevant studies or reports, highlighting the need for further exploration of this topic. This scoping review aims to define the concept of preterm infants' cues during breastfeeding, identify behaviors related to this concept, and determine appropriate measurements for observing these cues. A clear understanding of preterm infants' cues during breastfeeding is crucial for nurses to educate mothers and help them recognize and respond appropriately to their infants' needs. Breastmilk is the optimal food for preterm infants, making it vital for nurses to understand this topic comprehensively. The study aimed to explore preterm infants' cues during breastfeeding and identify the most effective instrument for observing these cues to enhance nurses' knowledge and expertise.
Methods
Study Design
A scoping review was used to explore the concept of preterm infant cues when breastfeeding and to identify the best instrument for observing these cues. This design was utilized to establish the roadmap as the foundation of this research. In addition, the scoping review can demonstrate to what extent the research findings are used in the real-world scenario (Peters et al., 2015).
Search Method
The search method was performed to collect articles published up to January 2022 from multiple database sources using the EBSCOhost website, namely CINAHL Plus with Full Text, MEDLINE, ERIC, and E-Journals. Also, the authors conducted a manual search to add one article from Google Scholar. The keywords used in the searching process were made up of different combinations such as preterm infants’ cues AND breastfeeding, preterm infants’ cues AND instrument, tool or measures scales, preterm infants AND breastfeeding cues, preterm infants AND cues AND breastfeeding. Also, the authors used the keyword the development of preterm infants’ breastfeeding behavior to search from Google Scholar manually. In addition, the Preferred Reporting Items for Systematic Reviews (PRISMA) 2020 guide was used for article selection (Page et al., 2021). The detail of the article search can be seen in the Supplementary File. The articles were collected on 23 June 2022.
Inclusion and Exclusion Criteria
PICO (Population, Intervention, Comparison, and Outcomes) format was used (Table 1). For review articles, these inclusion criteria applied: (1) published articles, (2) written in English and Chinese, (3) original research, (4) involved preterm infants born before 37-week Gestational Age (GA) and were breastfeeding, (5) contained information related to the feeding cues of infants, and (6) illustrated the instruments for observing breastfeeding infants. In addition, articles that involved preterm infants with congenital anomalies, such as cleft lip and cleft palate, were excluded because it takes special observation to identify infant feeding cues.
Table 1.
PICO format
| PICO Format | |
|---|---|
| Population | Preterm infants aged < 37 weeks’ gestation and mothers |
| Intervention | No intervention |
| Comparison | No comparison group |
| Outcomes | The preterm infants’ breastfeeding cues and instruments |
Study Selection
To confirm the suitability of the articles for the intended population and outcomes, the first and second authors reviewed the titles. The abstracts were then assessed to determine if the articles were suitable for further review. The first and third authors evaluated the English articles independently, while the fourth author, who is proficient in Chinese, assessed the Chinese articles.
Quality Appraisal
Scoping review does not require an investigation of the quality of the articles (Munn et al., 2018). However, the authors decided to review the article’s quality, considering that the article’s quality would affect the outcome of the review quality. The Joanna Briggs Institute (JBI) was employed as the critical appraisal tool (Moola et al., 2020). The first, second, and third articles were subject to quality evaluation using JBI for the cross-sectional study. This instrument contains eight question items with four answer options: yes, no, unclear, and not applicable. The eight question items covered the sample, respondents, research site, validity, and reliability for measuring exposure, the standard for measurement, confounding variable, handling the confounding variable, validity and reliability for measuring outcome, and statistical analysis. In addition, the JBI instrument was used to analyze the quality of the case report study in the third article. This instrument consists of eight question items with four answer options: yes, no, unclear, and not applicable. The questions were patients’ demographics, history, clinical condition, diagnostic test and results, intervention, adverse events, and lessons learned from the case study. Four articles (Giannì et al., 2017; Lin et al., 2013; Nyqvist et al., 1996; Nyqvist et al., 1999) were assessed before extracting the data. The first and third authors worked independently to review articles that satisfied the criteria. Any disagreement arising in the process of reviewing article quality was subjected to discussion until a consensus was reached.
Data Extraction
The scoping review’s data extraction process used data charting. This process emphasizes summarizing descriptively and logically findings and adjusting them to the review’s objectives, questions, or scope review (Peters MDJ et al., 2020). The first, second, and third authors extracted the data by taking into account the authors, year of publication, country’s research site, purpose, framework, research design and samples, results, discussion, conclusions, and gaps. The fourth author ensured that the data extraction from articles written in Chinese was performed correctly.
Data Analysis
Several techniques are available for analyzing and presenting scoping reviews. One of these methods is the descriptive approach, which is used to map the findings without conducting an in-depth analysis (Peters MDJ et al., 2020). In this study, the authors adopted the descriptive approach to analyze the data. Initially, the researchers examined the article's scope to determine the definition of preterm infant cues during breastfeeding. Then, they identified the optimal time for observing preterm infant cues during breastfeeding based on the articles. Subsequently, the authors provided more comprehensive details regarding preterm infants' behavior while breastfeeding. Lastly, the focus was on the tool used for detecting preterm infant cues during breastfeeding.
Results
Search Outcomes
Figure 1 illustrates the diagram to search and select the relevant articles. The authors found 183 potential articles to be reviewed, and after going through the selection process, four articles satisfied the criteria for quality evaluation and review.
Figure 1.
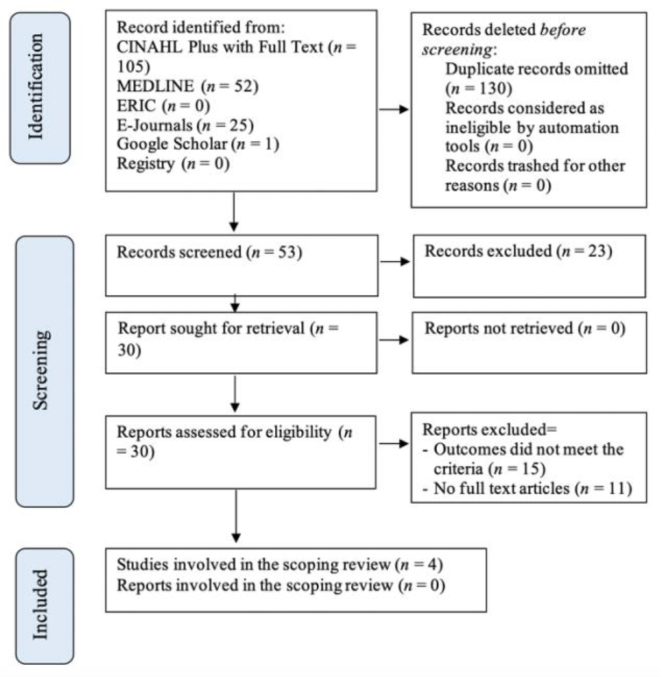
Selection of the articles based on PRISMA 2020
Quality Appraisal Results
The author used JBI critical appraisal for an observational study to evaluate the quality of the first, second, and third articles. Two authors reached a 100% consensus regarding their assessment of the quality of four articles. In the first article (Lin et al., 2013), the second (Giannì et al., 2017), and the fourth (Nyqvist et al., 1999), six items were labeled “yes,” and the rest two items were “unclear.” Although these articles did not explain confounding variables and how to handle them, they are generally good and viable for further review. In the third article (Nyqvist et al., 1996), six items were labeled “yes,” and one was “unclear.” Meanwhile, the third article did not specify the adverse event anticipations but was still regarded as a good and viable piece for further review.
Findings
The result of this study found articles that were published between 1996 and 2017 (see Table 2), and most of them (75%) were undertaken in Europe (Italy and Sweden), and the rest were in Asia (Taiwan). The articles were written in English (75%) and Chinese (25%). The findings are presented in three sections: 1) Scope of study and methodology; (2) Preterm infant cues during breastfeeding; and (3) Instrument.
Table 2.
Summary of studies on the preterm Infants’ cues during breastfeeding
| Author/year/country/language | Objectives/framework | Research Design /Sample | Instrument/developer | Results | Conclusion and gap |
|---|---|---|---|---|---|
| Lin et al. (2013) Taiwan, article in Chinese |
Comparing preterm infants’ behavioral cues between breastfeeding and bottle feeding |
|
|
|
|
| Giannì et al. (2017) Italy, article in English |
To investigate implementation of the Infants Driven Scale in NICU and to find the threshold in relation to belated feeding independency |
|
|
|
|
| Nyqvist et al. (1996) Sweden, article in English |
Describing the behavior of a very preterm infant before and after the mother was advised about behavioral cues during breastfeeding |
|
|
After two days of treatment, the preterm infant showed more wakefulness and more efficient sucking | The NIDCAP checklist is a mental checklist for assessment and advice |
| Nyqvist et al. (1999) Sweden, article in English |
Observing the development of preterm infants’ responses to the breast |
|
|
|
Cardiorespiratory stability, preview maturation condition, age, or weight, were considered for preterm infant’s breastfeeding initiation |
Scope of study and methodology
All reviewed articles (100%) focused on the activities of preterm infants on their mothers’ chests, especially during the breastfeeding session. The first article by Lin et al. (2013) compared the feeding cues of seven preterm infants aged 25-31 weeks’ GA observed from videotapes when infants were feeding from bottles or the mothers’ breasts. However, the authors only extracted data from the breastfeeding sessions. The second article by Giannì et al. (2017) applied consecutive samples of 47 infants born at <32 weeks’ gestational age in the level 3 neonatal care setting and investigated the implementation of the Infant Driven Scale. The third article by Nyqvist et al. (1996) involved one mother and her preterm born at 29 weeks’ GA focusing on the breastfeeding behavior of extremely preterm infants before and after the intervention of the NIDCAP approach. Finally, the fourth article by Nyqvist et al. (1999) studied 71 singleton infants born at 26.7 and 35.9 weeks’ GA focusing on PIBBS development. All these studies applied the observatory method that included observation of videotaped breastfeeding, descriptive study, or case study through direct observations.
The preterm infants’ cues during breastfeeding
The infants’ cues during breastfeeding may include 1) hungry, self-regulation, stress, and satiation; 2) sucking quality; 3) signal to approach and signal to avoid (step away) from the infants; and 4) infants’ behaviors (see Table 3).
Table 3.
The preterm infants’ cues during breastfeeding
| Author/year | The characteristic of the preterm infants’ cues during breastfeeding |
|
|---|---|---|
| Category | Behavior/indicator | |
| Lin et al. (2013) | Hunger cues | Suck searching, holding nipple, mouthing, and sucking |
| Self-regulation cues | Liquid loss/drooling, closing mouth, tongue extension and spit nipple out, grimace and frown, pause sucking, break/intermittent sucking, and yawning | |
| Stress cues | Nausea, changing color around mouth and nose/ cyanosis, breathing rapidly and nasal flaring, hiccup, reflux, coughing or choking, fussing, disturbing, consciousness change, back arching, crying/cry-like sound | |
| Satiation Cues | Falling asleep, turning head, and pushing away | |
| Giannì et al. (2017) | Sucking quality at breast* |
|
| Nyqvist et al. (1996) | Cues of approach |
Autonomic system Steady heartbeat, functional respiration, good oxygenation, unvaried skin color, normal digestive function, occasional twitches, and startles |
|
Motor System Controlling strength of muscles, flexing the arm kept; keeping the body and legs pressed against the breast, holding the mother’s body, holding the hand close to the face, or clenching the hand to the mouth, licking, smiling, pressing the breast like a cat, sucking, squeezing, scratching the breast, fitting on the mother’s body, and doing coordinated smooth movements | ||
|
Behavioral State Stable moment of wake and sleep; easy to distinguish states; focused look at mother, interested look, deep sleep; smooth state transitions: calm woken, fast asleep; behave to self-calming; quick stop stimulation | ||
|
Attention and interaction system Orienting towards mothers’ face, voice, other objects, or events; raising eyebrows, frowns; pursed lips; speech movement, face expression mimicking; making howl sounds | ||
| Cues of avoidance |
Autonomic system quick, slow pulse; dynamic breathing, slow-fast or irregular; changing skin color, light color, bluish, reddish, darkish; salivation, grunting sound of the bowel, gags, bowel movement grunting, sighs, puff and pants, hiccough, shiver, tremor |
|
|
Motor System Weak hand muscle, upper and lower extremities, body, open mouth, tongue exposed; body extension: flabby | ||
|
High muscle tone Body extension: uptight; extent arms, leg movement; moving forward-backward or turned head and body; spread fingers; tightly clenched fist, distorted expression; stretches tongues; overripe flexion; maladjustment to mother trunk; a wriggling movement; jerk and free movements. | ||
|
Behavioral State Sleepy, drowsiness, short awake, circling and staring, sensitive, hard to be calmed down, anxious, tempered crying | ||
|
Attention and interaction system Distracted view, looking around in many directions, sensible, crying, drowsiness, agitated, yawn, sneezes; cues of avoidance in autonomic/motor/behavior state system | ||
| Nyqvist et al. (1999) | Infant’s behavior | Rooting, areolar grasp, latch-on, sucking, longest sucking burst, and swallowing |
Instruments
The study in the first article used the PFCCS instrument to identify whether preterm infants were hungry, self-regulating, stressed, or satiated. The second article used IDS (Italian version) to evaluate the sucking quality during breastfeeding. The third article used NIDCAP to read preterm infants’ cues while breastfeeding and as a guide to formulate healthcare planning to support infants. The fourth article used PIBBS to observe preterm infants’ behavior while breastfeeding (see Table 4).
Table 4.
Summary of the detailed instrument from studies on preterm infants’ cues during breastfeeding
| Author/year/country/language | Instruments for observing the preterm infants’ cues |
||
|---|---|---|---|
| Instrument/developer | The instruments’ general description | Validity and reliability of the instrument | |
| Lin et al. (2013) |
|
|
|
| Giannì et al. (2017) | The modified instrument from Infant Driven Scale (IDS) (Newland et al., 2013) |
|
Not reported |
| Nyqvist et al. (1996) |
|
|
Reliability was checked before the study, but the test’s result was not reported |
| Nyqvist et al. (1999) |
|
The guideline for observing preterm infant cues during breastfeeding focuses on six infant cues that are: rooting, areolar grasp, latch-on, sucking, longest sucking burst, swallowing | Kappa values between mothers and nurses range from 0.68 to 0.94 or 80–97% agreement which indicated good agreement between raters |
Discussion
The scoping review focused on exploring the concept of “feeding cues for preterm infants when breastfeeding” and “finding the proper instrument for observing the feeding cues.” Therefore, this discussion section is divided into three, namely (1) the scope of the study and methodology; (2) the preterm infants’ cues when breastfeeding; (3) the instruments.
Scope of Study and Methodology
The scoping review discovered that the concept of "preterm infant cues when breastfeeding" encompasses all activities that infants engage in while on their mother's chest, including latch-on and other behaviors that indicate the infant's need for feeding. For instance, sucking on their own fingers and seeking before sucking are cues that infants want to feed at their mother's breast. These cues can be observed before, during, and after breastfeeding. Observation was the preferred method used to observe preterm infant cues during breastfeeding in all four articles reviewed. Direct behavioral observation is a robust way to investigate infant development and how to read an infant's behavior/cues, particularly when overt behavior is the focus of the research question (Chorney et al., 2015). Thus, future studies on preterm infant cues during breastfeeding may utilize direct observation or videotaping for data collection. The findings of this review are essential for nurses to improve their understanding of the occurrence and research methodology of "preterm infant cues when breastfeeding" among infants. Exploring the concept of infant feeding cues is closely related to the process of mother-infant interactions during breastfeeding. Any behavior exhibited by an infant on their mother's chest is considered a preterm infant cue when breastfeeding.
The Preterm Infants’ Cues During Breastfeeding
Barnard's model posits that positive interaction can occur when infants/children communicate their needs through clear cues, which their parents can understand and respond to appropriately, leading to reciprocal responses from the infants/children (Oxford & Findlay, 2015). The next section of this review will discuss the various cues/behaviors used by preterm infants to express their needs. The authors of this study identified four main categories of preterm infant cues when breastfeeding: hunger cues, self-regulation cues, stressed cues, and satiation cues. Hunger cues, such as sucking on their fingers or a pacifier or suckling the mother's nipple (Puckett et al., 2008), indicate that infants are ready to feed and require immediate attention. Thus, nurses should encourage mothers to breastfeed their infants when they observe these signs of hunger.
Self-regulation cues refer to infants’ ability to regulate themselves and return to a balanced state (Als, 1982). These cues may include excessive drooling (Bilgin & Wolke, 2017), lip compression (Oxford & Findlay, 2015), pulling the nipple, and pushing the nipple out, which are all considered self-regulation cues (Shaker, 2013). Nurses working in perinatology wards can observe infants self-regulating when they unlatch from their mother's nipples. Therefore, nurses should educate mothers to pause and give their infants time to self-regulate between breastfeeding sessions.
In infants, a stressed signal refers to unstable organizations (Als, 1982). Stressed signals during breastfeeding may include a change in an infant’s facial skin color, fast breathing, nasal flaring, choking, and chin tugging (Shaker, 2013). If nurses observe these signals in infants while breastfeeding, they can assist the mothers in adjusting the infants’ position to ensure normal breathing and avoid choking. In addition, signs that infants are satiated and no longer want to feed (Oxford & Findlay, 2015) include pushing away and falling asleep. When nurses notice these cues, they can suggest that the mother stop breastfeeding.
The article review revealed that an infant's signals could be classified as cues of approach or avoidance. Cues of approach indicate that the infant is willing and prepared to feed, and they approach the stimuli, such as their mother's breast, and interact with them. Cues of avoidance indicate an excess of stimuli that the infant cannot handle, more than infants can take into their mouth, and they actively try to avoid them (Als, 1995; Als & McAnulty, 2011). Hungry signals can be considered as cues of approach, indicating that nurses or mothers should attend to the infant and feed them.
On the other hand, self-regulation and stress cues can be considered avoidance cues, indicating that nurses or mothers should temporarily stop feeding and allow infants to regulate themselves until they are ready to resume breastfeeding. Likewise, the satiation signal is also an avoidance cue that indicates nurses or mothers should stop feeding as the infants have already reached fullness. Continuing to force infants to feed despite being full may cause distress and increase their risk of choking (Shaker, 2013).
Evaluating the quality of sucking during breastfeeding sessions with preterm infants is crucial since it affects the volume of milk intake. Unfortunately, late preterm infants often have weak sucking reflexes and may struggle to properly latch onto the mother’s breast (Dosani et al., 2016). However, mothers should not worry since the sucking ability of preterm infants improves over time, and interventions are available to enhance their sucking power, such as cue-based feeding. Studies have reported that implementing a “cue-based feeding approach of developmental care” has helped mothers and preterm infants transition to the feeding phase (Huang & Huang, 2019). This finding indicates that by paying attention to infants’ cues during breastfeeding and being sensitive to their needs, nurses can support the development of infants' sucking ability, leading to the success of feeding preterm infants.
This scoping review sheds light on the characteristics of preterm infant cues during breastfeeding and emphasizes their importance for nurses and mothers to understand this situation better.
Instruments
The scoping review identified four instruments for observing preterm infants' cues during breastfeeding: PFCCS, IDS (Italy modification version), NIDCAP framework, and PIBBS. The PFCCS is a coding system that comes with a film sample for training coders, a guidebook, and an observation checklist. To use PFCCS, coders must pass reliability tests that include inter- and intra-rater reliability using test-retest and achieve a minimum of 80% agreement (Chorney et al., 2015). The literature review revealed that PFCCS demonstrated good inter-rater and intra-rater reliability (test-retest), with coders achieving more than 80% agreement, indicating a reliable test.
The PFCCS has facilitated real-time observation of infants' behavior, which can be accomplished by watching a video of an infant breastfeeding. This also allows for video feedback to be provided to mothers, helping them to understand their infants' behavior and react appropriately. For instance, when a nurse notices an infant's cues, they may encourage the mother to breastfeed. However, if the infant regurgitates the breast milk, the mother will be advised to pause the feeding and give the infant time to self-regulate. Self-regulation refers to the infant's ability to regulate themselves and return to a balanced state (Als, 1982).
According to Cassibba et al. (2015), video feedback is an effective method to improve maternal responsiveness and infant attachment security, particularly for insecure mothers. Maternal sensitivity is the mother's ability to interpret an infant's cues accurately and react appropriately to meet the infant's needs (Shin et al., 2008). Although PFCCS has numerous benefits, it also has some limitations. Since it involves real-time observation using breastfeeding videos, coders require time to practice and implement inter- and intra-rater reliability tests. Furthermore, observing an infant's behavior second by second is time-consuming.
The Italian version of IDS assesses an infant’s readiness for peroral feeding by evaluating four domains, including sucking quality. This instrument is valuable for monitoring feeding development, identifying delayed oral feeding abilities, and improving full oral feeding capacity earlier in preterm infants born at <34 weeks GA (Wellington & Perlman, 2015). Unlike PFCCS, IDS does not offer real-time observation as breastfeeding behavior is only evident during breastfeeding sessions, and mothers need to be sensitive to the behavior to meet their infants’ needs. However, IDS uses the Likert scale to detect several behaviors, making it easier for researchers to differentiate between preterm infants' behaviors.
The NIDCAP framework serves as both a checklist and a guide for caregivers to understand an infant's cues and advocate for four systems: autonomic, motor, state, attention, and interaction. NIDCAP is an individualized developmental approach that aims to promote and manage infants by identifying their cues and designing individualized care plans that build on their strengths (Als & McAnulty, 2011). Because the ability to breastfeed varies among preterm infants, the NIDCAP approach is considered appropriate for facilitating breastfeeding due to its sensitivity to individual differences.
The PIBBS is a tool used to monitor six specific behaviors of breastfeeding infants: rooting, areolar grasp, latch-on, sucking, longest sucking burst, and swallowing. Inter-observer reliability tests have shown that the PIBBS is a reliable instrument (Lober et al., 2020), but proper training is required for observers to use it effectively. In addition, while PIBBS is equipped with a guideline for behavior coding, PIBBS does not include a tutorial video for new coders or real-time observation features.
This literature review identified four instruments that can assist nurses in understanding and responding appropriately to preterm infants' breastfeeding cues. These instruments, including PFCCS, IDS, NIDCAP, and PIBBS, can be utilized by nurses working in level 1, 2, and 3 neonatal care to establish care planning and improve feeding outcomes among preterm infants. The nurses can choose the appropriate instrument depending on their goals and needs. For instance, PFCCS allows for real-time observation of preterm infants' cues, while NIDCAP is ideal for identifying the best time to approach or stay away from infants. In addition, IDS provides a numerical scale to evaluate sucking quality, whereas PIBBS offers a numerical scale for assessing preterm infants' breastfeeding behavior. These instruments can serve as valuable nursing implications to promote optimal breastfeeding among preterm infants.
Conclusion
The range of preterm infant cues exhibited during breastfeeding includes all activities the infant performs while on the mother's chest. The concept of preterm infant cues refers to the infant's ability to express their needs through various behaviors. Preterm infant cues can be observed before, during, and after breastfeeding; observational studies are the most suitable method for examining them. This review found that preterm infant cues consist of hunger, self-regulation, stress, satiation, approach and avoidance, and sucking quality. The PFCCS, IDS, NIDCAP, and PIBBS are reliable and valid tools for detecting infant cues while breastfeeding.
Acknowledgment
The authors acknowledge the Directorate General of Resources for Science, Technology, and Higher Education in Indonesia for supporting this project.
Declaration of Conflicting Interest
The authors declared that they do not have any conflict of interest in this study.
Funding
This study was supported by the Directorate General of Resources for Science, Technology, and Higher Education of Indonesia [No 894/E4.4/K/2015].
Authors’ Contributions
HP has contributed to the work’s conception, the articles’ acquisition, analysis, and interpretation of data, as well as writing and manuscript revision. MDP contributed to the articles’ acquisition and analyzed the data. WAM reviewed the quality of the selected articles and analyzed the data. MCH has contributed to the analysis of the Chinese article and manuscript revision. All authors approved the final version of the manuscript to be published.
Authors’ Biographies
Haryatiningsih Purwandari, S.Kep., Ns., M.Kep., Sp.Kep is a Doctoral Candidate at the International Doctoral Nursing Program, Department of Nursing, College of Medicine, National Cheng Kung University, Tainan, Taiwan. She is also an Assistant Professor at the Department of Nursing, Jenderal Soedirman University, Indonesia.
Meivita Dewi Purnamasari, S.Kep., Ns., Me.Kep is an Assistant Professor at the Department of Nursing, Jenderal Soedirman University, Indonesia.
Dr. Wastu Adi Mulyono, S.Kp., M.Kep is an Assistant Professor at the Department of Nursing, Jenderal Soedirman University, Indonesia.
Mei-Chih Huang, PhD, RN is a Professor at the Department of Nursing, College of Medicine, National Cheng-Kung University, Tainan, Taiwan, and at the National Tainan Junior College of Nursing, Tainan, Taiwan.
Data Availability
Not applicable.
Ethical Consideration
Not applicable.
Declaration of Use of AI in Scientific Writing
Nothing to declare.
References
- Als, H. (1982). Toward a synactive theory of development: Promise for the assessment and support of infant individuality. Infant Mental Health Journal, 3(4), 229-243. [DOI] [Google Scholar]
- Als, H. (1995). Manual for the naturalistic observation of newborn behavior: Newborn individualized developmental care and assessment program (NIDCAP). Boston: Harvard Medical School. [Google Scholar]
- Als, H., & McAnulty, G. B. (2011). The newborn individualized developmental care and assessment program (NIDCAP) with kangaroo mother care (KMC): Comprehensive care for preterm infants. Current Women's Health Reviews, 7(3), 288-301. 10.2174/157340411796355216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilgin, A., & Wolke, D. (2017). Associations between feeding problems and maternal sensitivity across infancy: Differences in very preterm and full-term infants. Journal of Developmental & Behavioral Pediatrics, 38(7), 538-544. 10.1097/DBP.0000000000000466 [DOI] [PubMed] [Google Scholar]
- Bomer Norton, C. (2014). Breastfeeding: A holistic concept analysis. Public Health Nursing, 31(1), 88-96. 10.1111/phn.12047 [DOI] [PubMed] [Google Scholar]
- Cassibba, R., Castoro, G., Costantino, E., Sette, G., & Van Ijzendoorn, M. H. (2015). Enhancing maternal sensitivity and infant attachment security with video feedback: An exploratory study in Italy. Infant Mental Health Journal, 36(1), 53-61. 10.1002/imhj.21486 [DOI] [PubMed] [Google Scholar]
- Celik, I. H., Demirel, G., Canpolat, F. E., & Dilmen, U. (2013). A common problem for neonatal intensive care units: late preterm infants, a prospective study with term controls in a large perinatal center. The Journal of Maternal-Fetal & Neonatal Medicine, 26(5), 459-462. 10.3109/14767058.2012.735994 [DOI] [PubMed] [Google Scholar]
- Chen, C.-T., Wang, L.-Y., Wang, Y.-L., & Lin, B.-S. (2017). Quantitative real-time assessment for feeding skill of preterm infants. Journal of Medical Systems, 41(6), 95. 10.1007/s10916-017-0744-1 [DOI] [PubMed] [Google Scholar]
- Chorney, J. M., McMurtry, C. M., Chambers, C. T., & Bakeman, R. (2015). Developing and modifying behavioral coding schemes in pediatric psychology: A practical guide. Journal of Pediatric Psychology, 40(1), 154-164. 10.1093/jpepsy/jsu099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dosani, A., Hemraj, J., Premji, S. S., Currie, G., Reilly, S. M., Lodha, A. K., Young, M., & Hall, M. (2016). Breastfeeding the late preterm infant: Experiences of mothers and perceptions of public health nurses. International Breastfeeding Journal, 12(1), 1-10. 10.1186/s13006-017-0114-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanaro, S. (2013). Feeding intolerance in the preterm infant. Early Human Development, 89, S13-S20. 10.1016/j.earlhumdev.2013.07.013 [DOI] [PubMed] [Google Scholar]
- Giannì, M. L., Sannino, P., Bezze, E., Plevani, L., Esposito, C., Muscolo, S., Roggero, P., & Mosca, F. (2017). Usefulness of the Infant Driven Scale in the early identification of preterm infants at risk for delayed oral feeding independency. Early Human Development, 115, 18-22. 10.1016/j.earlhumdev.2017.08.008 [DOI] [PubMed] [Google Scholar]
- Girgin, B. A., Gözen, D., & Karatekin, G. (2018). Effects of two different feeding positions on physiological characteristics and feeding performance of preterm infants: A randomized controlled trial. Journal for Specialists in Pediatric Nursing, 23(2), e12214. 10.1111/jspn.12214 [DOI] [PubMed] [Google Scholar]
- Griffith, T., Rankin, K., & White-Traut, R. (2017). The relationship between behavioral states and oral feeding efficiency in preterm infants. Advances in Neonatal Care, 17(1), E12. 10.1097/ANC.0000000000000318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe, T.-H., & Sheu, C.-F. (2020). Predicting bottle-feeding performance using a reorganized Neonatal Oral-Motor Assessment Scale (NOMAS). American Journal of Occupational Therapy, 74(4_Supplement_1), 7411500015p7411500011. 10.5014/ajot.2020.74S1-PO3113 [DOI] [Google Scholar]
- Huang, C.-C., & Huang, M.-C. (2019). Helping a preterm infant through the transitional feeding period using a cue-based feeding approach of developmental care. Hu Li Za Zhi, 66(2), 101-106. 10.6224/JN.201904_66(2).13 [DOI] [PubMed] [Google Scholar]
- Lin, C.-H. (2005). Influence of feeding interaction program on maternal feeding behaviors with preterm infant. [Thesis, National Cheng Kung University; ]. Tainan City, Taiwan, ROC. [Google Scholar]
- Lin, S.-C., Lin, C.-H., Zhang, J.-W., Chen, S.-M., Chen, C.-L., & Huang, M.-C. (2013). Breast-and bottle-feeding in preterm infants: A comparison of behavioral cues. Hu Li Za Zhi, 60(6), 27. 10.6224/JN.60.6.27 [DOI] [PubMed] [Google Scholar]
- Lober, A., Dodgson, J. E., & Kelly, L. (2020). Using the Preterm Infant Breastfeeding Behavior Scale with late preterm infants. Clinical Lactation, 11(3), 121-129. 10.1891/CLINLACT-D-20-00001 [DOI] [Google Scholar]
- Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., Sfetcu, R., Currie, M., Qureshi, R., Mattis, P., Lisy, K., & Mu, P.-F. (2020). Chapter 7: Systematic reviews of etiology and risk. In E. Aromataris & Z. Munn (Eds). JBI Manual for Evidence Synthesis. JBI. https://synthesismanual.jbi.global [Google Scholar]
- Munn, Z., Peters, M. D., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 1-7. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newland, L., L’Huillier, M. W., Petrey, B., & Scheans, P. (2013). Implementation of cue-based feeding in a level III NICU. Neonatal Network, 32(2), 132-137. 10.1891/0730-0832.32.2.132 [DOI] [PubMed] [Google Scholar]
- Nyqvist, K. H., Ewald, U., & Sjödén, P.-O. (1996). Supporting a preterm infant's behaviour during breastfeeding: A case report. Journal of Human Lactation, 12(3), 221-228. 10.1177/089033449601200320 [DOI] [PubMed] [Google Scholar]
- Nyqvist, K. H., Sjödén, P.-O., & Ewald, U. (1999). The development of preterm infants’ breastfeeding behavior. Early Human Development, 55(3), 247-264. 10.1016/S0378-3782(99)00025-0 [DOI] [PubMed] [Google Scholar]
- Oxford, M., & Findlay, D. (2015). NCAST programs caregiver/parent-child interaction feeding manual. Seatlle: University of Washington, School of Nursing. [Google Scholar]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., & Brennan, S. E. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, 105906. 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- Peters, M. D., Godfrey, C. M., Khalil, H., McInerney, P., Parker, D., & Soares, C. B. (2015). Guidance for conducting systematic scoping reviews. International Journal of Evidence-based Healthcare, 13(3), 141-146. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, & Khalil, H. (2020). Chapter 11: Scoping Reviews (2020 version). In E. Aromataris & Z. Munn (Eds.), JBI Manual for Evidence Synthesis. 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- Pineda, R., Prince, D., Reynolds, J., Grabill, M., & Smith, J. (2020). Preterm infant feeding performance at term equivalent age differs from that of full-term infants. Journal of Perinatology, 40(4), 646-654. 10.1038/s41372-020-0616-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puckett, B., Grover, V. K., Holt, T., & Sankaran, K. (2008). Cue-based feeding for preterm infants: A prospective trial. American Journal of Perinatology, 25(10), 623-628. 10.1055/s-0028-1090583 [DOI] [PubMed] [Google Scholar]
- Purwandari, H., & Huang, M.-C. (2020). Short-term outcomes of preterm infants in a medical center at Banyumas Regency, Indonesia: A preliminary study. Babali Nursing Research, 1(2), 47-57. 10.37363/bnr.2020.1225 [DOI] [Google Scholar]
- Rommel, N., van Wijk, M., Boets, B., Hebbard, G., Haslam, R., Davidson, G., & Omari, T. (2011). Development of pharyngo-esophageal physiology during swallowing in the preterm infant. Neurogastroenterology & Motility, 23(10), e401-e408. 10.1111/j.1365-2982.2011.01763.x [DOI] [PubMed] [Google Scholar]
- Shaker, C. S. (2013). Cue-based feeding in the NICU: Using the infant’s communication as a guide. Neonatal Network, 32(6), 404-408. 10.1891/0730-0832.32.6.404 [DOI] [PubMed] [Google Scholar]
- Shin, H., Park, Y. J., Ryu, H., & Seomun, G. A. (2008). Maternal sensitivity: A concept analysis. Journal of Advanced Nursing, 64(3), 304-314. 10.1111/j.1365-2648.2008.04814.x [DOI] [PubMed] [Google Scholar]
- Wellington, A., & Perlman, J. M. (2015). Infant-driven feeding in premature infants: a quality improvement project. Archives of Disease in Childhood-Fetal and Neonatal Edition, 100(6), F495-F500. 10.1136/archdischild-2015-308296 [DOI] [PubMed] [Google Scholar]
- White-Traut, R., Liu, L., Norr, K., Rankin, K., Campbell, S. K., Griffith, T., Vasa, R., Geraldo, V., & Medoff-Cooper, B. (2017). Do orally-directed behaviors mediate the relationship between behavioral state and nutritive sucking in preterm infants? Early Human Development, 109, 26. 10.1016/j.earlhumdev.2017.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


