Abstract
Social media use is rapidly expanding in terms of frequency, duration, and the diversity of platforms available. Given evidence for associations between social media use, body image disturbances, and disordered eating it is important to identify potentially harmful aspects of social media use that could serve as intervention targets. This study surveyed two demographically diverse undergraduate student cohorts in 2015 and 2022 to compare patterns in social media use, body image, and disordered eating behaviors between samples, including as a function of the COVID-19 pandemic, and to test the hypothesized moderating role of specific content consumed in the association between social media use and maladaptive outcomes. Participants in 2022 reported greater body image disturbances, more frequent vomiting and laxative use, and more time spent on a greater number of social media accounts, with significantly greater use of image-based platforms such as Snapchat, TikTok, and YouTube. Moderated regression analyses suggest that type of content consumed, but not the amount of time spent on social media or diversity of platforms utilized, is associated with body image disturbances and disordered eating behaviors after controlling for gender and body mass index. Specifically, exposure to weight loss content was associated with lower body appreciation, greater fears of negative appearance evaluation, and more frequent binge eating. Contrary to initial hypotheses, exposure to body positivity/neutrality content did not have protective effects. Findings suggest that interventions targeting negative consequences of social media use should focus on addressing content consumed, rather than time spent on social media platforms.
Keywords: Social media, Body image, Disordered eating, Body positivity, Body neutrality, Weight loss
1. Introduction
Social media (SM) use has become ubiquitous in recent decades. In 2021, 72 % of U.S. adults reported using at least one SM site, an increase from about 60 % in 2014 (Center, 2021). Americans now subscribe to an average of seven SM accounts (Dean, 2021). These trends suggest that SM use has been expanding in terms of overall usage and the number and diversity of platforms available. This pattern may be, in part, due to the COVID-19 pandemic, during which SM use increased, particularly among young adults (Fitzgerald, Yue, Wong, & Green, 2022). SM use offers many benefits, including increased social interaction and peer support (Naslund, Bondre, Torous, & Aschbrenner, 2020). However, growing evidence documents the potential negative impact of SM on quality of life and mental health, including possible associations between SM use and poor body image and disordered eating (Holland & Tiggemann, 2016; Zhang, Wang, Li, & Wu, 2021). For example, Facebook use has been shown to positively correlate with measures of body image concern and eating-related pathology (Eckler, Kalyango, & Paasch, 2016; Mabe, Forney, & Keel, 2014; Tiggemann & Slater, 2013). Eating disorder (ED) symptom severity and incidence of probable ED diagnosis also increased during the COVID-19 lockdown (Linardon, Messer, Rodgers, & Fuller-Tyszkiewicz, 2022), underscoring the importance of considering the pandemic when examining the relation between SM use and ED symptoms.
1.1. Quantifying social media use: duration versus content
Research on the association among SM use and body image disturbances and EDs remain mixed, perhaps in part because SM use has been measured in various ways. Indeed, some previous studies report no associations among duration of SM use and body image and eating-related pathology in adolescents (Ferguson, Muñoz, Garza, & Galindo, 2014; Meier & Gray, 2014) and adults (Kim & Chock, 2015). Further, a recent meta-analysis concluded that the valence of the relation between SM use and body image dissatisfaction is unclear, partly because of how social media use was operationalized across studies. Taken together, these findings highlighting the importance of identifying potential moderators that account for discrepant findings in prior research (Saiphoo & Vahedi, December 2018).
Most extant research has assessed SM exposure in terms of intensity of use, typically operationalized as estimated daily frequency and duration (Fardouly & Vartanian, 2015) or weekly amount of use (Mabe et al., 2014). Importantly, these assessments do not consider other dimensions of SM use, such as total number and diversity of platforms accessed. Studies to date have generally also not accounted for the impact of specific content consumed on SM on outcomes related to body image or disordered eating behaviors. Given the established relation between dieting, EDs, and body image disturbance (Ackard, Croll, & Kearney-Cooke, 2002; Hilbert, Pike, Goldschmidt, et al., 2014; Marks, de Foe, & Collett, 2020), assessing the specific impact of weight loss content is an important area of research, especially considering the frequent and varied SM discourse about weight (Chou, Ying, Prestin, & Kunath, 2014). The current study addresses these critical gaps in knowledge and seeks to identify specific aspects of SM use and trends in SM across two time points that relate to adverse outcomes and may serve as effective intervention targets.
1.2. Rise of image-based platforms
SM use has increasingly shifted toward image-based platforms such as Instagram and Snapchat (Vogels, Gelles-Watnick, & Teens, 2022), which disproportionately disseminate content related to appearance (Simpson & Mazzeo, 2016), and specifically weight loss, and also serve as informal resources for health promotion (Fung, Blankenship, Ahweyevu, et al., 2020). Numerous studies suggest that engagement with appearance-focused content on SM (e.g., “thinspiration” or “fitspiration”) has significant adverse consequences on body image (Casale, Gemelli, Calosi, Giangrasso, & Fioravanti, 2019; Cohen, Newton-John, & Slater, 2017; Fardouly & Vartanian, 2016; González-Nuevo, Cuesta, & Muñiz, 2021; Jiotsa, Naccache, Duval, Rocher, & Grall-Bronnec, 2021; Marks et al., 2020; Meier & Gray, 2014). Although the latter ostensibly implies promotion of a more adaptive perspective toward health, research suggests both thinspiration and fitspiration SM content portray harmful messages around objectification, restrictive eating, and weight loss (Alberga, Withnell, & von Ranson, 2018; Boepple & Thompson, 2016). Much of this literature was published before the emergence of TikTok, an image-based SM platform which has rapidly gained popularity as the most accessed domain (Moreno, December 29, 2021) worldwide, with approximately 136.5 million American users in 2022 (Ceci, 2022). Understanding the impact of these ongoing changes in SM use patterns on body image and disordered eating behaviors through exploring shifts in use and/or ways of engaging with different platforms over time is critical.
1.3. Impact of exposure to body positivity and neutrality content
Appearance-related content is now increasingly available on SM with the rising popularity of image-based platforms. Importantly, the nature of this content has shifted over time, most markedly with the proliferation of body positive and body neutral content. Body positivity attempts to challenge the “thin ideal” by encouraging body acceptance at all shapes and sizes (Rodgers, Wertheim, Paxton, Tylka, & Harriger, 2022). Relatedly, body neutrality promotes the belief that the body is worthy of respect regardless of appearance (Perry, Watson, Hayden, & Inwards-Breland, 2019). Preliminary research suggests that exposure to body positive SM content is associated with higher body satisfaction (Stevens & Griffiths, 2020). To our knowledge, no studies to date have examined the relationship between body neutrality content and body image or disordered eating.
While there is some evidence to suggest beneficial effects of body positive SM content on body image, its potentially protective impact on eating behaviors remains unknown. Furthermore, recent content analyses revealed that most individuals portrayed in body positive posts displayed some aspect of mainstream beauty ideals (Lazuka, Wick, Keel, & Harriger, 2020), suggesting that body positivity content does not always convey the intended message and instead can negatively impact viewer body image Given recent movements to incorporate body positivity and/or neutrality into the treatment of EDs (Cook-Cottone, 2015; Perry et al., 2019), more work is needed to delineate the relationship between these constructs as disseminated by SM, body image, and disordered eating behaviors.
1.4. Current study
We surveyed two demographically diverse undergraduate samples in 2015 and 2022 to examine SM use at two time points and the relation of aspects of SM use to disordered body image and eating behaviors. Aims and a priori hypotheses were as follows:
Aim 1: To compare patterns in SM use, body image disturbances, and disordered eating behaviors between samples, including as a function of the COVID-19 pandemic, across two cohorts of undergraduate students.
Hypothesis 1a. Compared to 2015 participants, the 2022 sample will report greater duration of daily SM use via a higher number of accounts.
Hypothesis 1b. Participants in the 2022 sample will attribute changes in their SM use in part to the impacts of the COVID-19 pandemic.
Hypothesis 1c. Compared to 2015 participants, the 2022 sample will report greater body image dissatisfaction and more frequent disordered eating behaviors.
Aim 2: To examine if associations among SM use and disordered body image and eating behaviors are moderated by specific content consumed in a current sample of undergraduates.
Hypothesis 2a. Associations between SM use (duration and number of platforms) and body image disturbances and disordered eating behaviors will be moderated by exposure to weight loss content, such that more use is associated with adverse outcomes specifically in participants consuming any weight loss content.
Hypothesis 2b. Associations between SM use (duration and number of platforms) and body image disturbances and disordered eating behaviors will be moderated by exposure to body positivity/neutrality content, with fewer adverse outcomes specifically in participants consuming body positivity/neutrality content.
2. Materials and methods
All methods and materials were reviewed and approved by the local Institutional Review Board. Participants provided informed consent after being informed of the purpose and anonymous and voluntary nature of the research. Data collection proceeded in two waves in 2015 and 2022. Participants received course credit.
2.1. Participants
Participants were undergraduate students at a large University in the northeastern United States who provided information via the secure online servers SurveyMonkey as part of larger experimental study of the impact of SM on body image and eating behaviors (2015) and remotely via Qualtrics using a link provided to them via email (2022).
2.2. Measures
2.2.1. Demographics
Participants reported their current age, gender identity, race and ethnicity, and height and weight (to calculate BMI).
2.2.2. Social media use
Participants indicated the types and total number of SM accounts they use along with an estimate of minutes spent on SM each day.
2.2.3. Body Appreciation Scale (BAS) (Avalos, Tylka, & Wood-Barcalow, 2005)
The 13-item BAS quantifies participants’ acceptance of and respect for their bodies. Items are rated on five-point Likert Scale (1 = never to 5 = always), with higher scores reflecting more positive body image. Internal consistency reliability of the unidimensional scale was excellent in the 2015 and 2022 samples (Cronbach’s α = 0.94 and 0.95, respectively).
2.2.4. Fear of Negative Appearance Evaluation Scale (FNAES) (Lundgren, Anderson, & Thompson, 2004)
The six-item, single factor FNAES measures individuals’ concerns about others’ negative evaluations of their appearance and has been shown to be significantly associated with measures of body image and eating disturbances. Internal consistency reliability was excellent in the 2015 and 2022 samples (Cronbach’s α = 0.94 and 0.96, respectively).
2.2.5. Disordered eating behaviors
Past 28-day frequency of binge eating, vomiting, and laxative use for the purpose of controlling weight and shape, were quantified via individual items of the Eating Disorder Examination — Questionnaire, a widely used and well-validated screening tool for EDs, including in community samples (Mond, Hay, Rodgers, Owen, & Beumont, 2004), in a manner comparable to prior work (Lengvenyte, Strumila, Maimoun, et al., 2021; Lowe, Thomas, Safer, & Butryn, 2007; Mathisen, Rosenvinge, Friborg, et al., 2020).
2.2.6. 2022 cohort social media use
Respondents recruited in 2022 described the perceived impact of the COVID-19 pandemic on their SM use, including pre- to post-pandemic increases or decreases in time spent on SM, more positive or negative experiences using SM, and any changes in motivations for their SM use. They also indicated if the SM sites they use allow them to view a range of diverse content and include people who look like them, and the extent to which they seek out specific SM content related to weight loss and/or body positivity/neutrality via yes/no items (see Supplementary Material).
2.3. Statistical analyses
Analyses were conducted in SPSS version 27 (IBM Corp., 2021). To account for discrepancies in the assessment of gender and race in 2015 versus 2022, we recoded gender into three categories: female (cis or trans), male (cis or trans) and other (non-binary, other) and created one variable coding both samples into White and non-White participants. Impossible/unlikely values for time spent on SM each day (i.e., values >24 h) and BMI (<10 kg/m2) were excluded. Demographics and basic patterns of SM use of the 2015 and 2022 samples were compared via chi-square and independent samples t-tests. Changes in SM use and measures of body dissatisfaction and disordered eating behaviors over time and gender differences in these constructs were examined in a series of univariate analyses of variance (ANOVA) with timepoint and gender as fixed factors.
Moderated multiple regression analyses were conducted with data from the 2022 sample to determine if SM use (i.e., time spent and number of accounts), SM content consumed (i.e., weight loss and body positivity/neutrality), or their interaction were significant predictors of body dissatisfaction and disordered eating behaviors. Continuous variables were mean centered and all models were adjusted for participant gender and BMI, in consideration of prior literature (Cohen et al., 2017; Zhang et al., 2021) and preliminary analyses in the current study that suggested significant gender differences in SM use and associations between specific content viewed and BMI. The dichotomized categorical variables were dummy coded in the regression models. Covariates were entered in Step 1, followed by main effects in Step 2, and interaction effects in Step 3. Statistical significance was evaluated after applying a Bonferroni correction (p ≤ .003).
Missing data ranged from 0.6 %–1.4 % and 6.2 %–6.5 % for the BAS and from 0.3 to 1.1 % and 6.9 %–7.3 % for the FNAES in the 2015 and 2022, respectively; 0.6 % of the 2015 sample did not provide responses to the three EDE-Q items of interest; 7.3 % of the 2022 respondents had missing data on those items. In both samples, skewness values were within the acceptable range (<3) for the BAS and FNAES and assessments of time spent on SM and number of SM accounts used, indicating sufficient normality. Scores on the three EDE-Q items were heavily skewed by the large number of respondents who did not report engagement in the behaviors assessed, as expected for behavioral count variables assessing ED behaviors in a non-clinical population (Hilbert, de Zwaan, & Braehler, 2012; Serier, 2016). There was no evidence for multicollinearity in any of the models.
3. Results
3.1. Aim 1
To compare patterns in SM use, body image disturbances, and disordered eating behaviors between samples, including as a function of the COVID-19 pandemic, across two cohorts of undergraduate students.
Participants recruited in 2015 and 2022 did not differ significantly in mean age or BMI; the 2022 sample was significantly more diverse than the 2015 cohort in terms of reported race and gender identity (see Table 1 for all Aim 1 analyses).
Table 1.
2015 versus 2022 sample demographics, social media use, body image, and disordered eating behaviors.
| 2015 % (n) | 2022 % (n) | Statistic | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Gender identity | Female | 54.9 (197) | 54.3 (145) | X2(2) = 7.09, p = .03, φ = 0.11 | |||
| Male | 44.6 (160) | 42.3 (113) | |||||
| Other | 0.6 (2) | 3.4 (9) | |||||
| Race | Non-White | 49.0 (176) | 59.3 (163) | X2 = 6.57, p = .01, φ = 0.10 | |||
| White | 51.0 (183) | 40.7 (112) | X2 = 128.96, p < .001, φ = 0.45 | ||||
| Social media accounts used | 92.8 (333) | 53.8 (148) | X2 = 1.22, p = .29, φ = 0.04 | ||||
| 93.6 (336) | 91.3 (251) | X2 = 6.23, p = .01, φ = 0.10 | |||||
| 70.2 (252) | 60.7 (167) | X2 = 272.23, p < .001, φ = 0.66 | |||||
| Snapchat | 23.4 (84) | 89.5 (246) | X2 = 464.79, p < .001, φ = 0.86 | ||||
| TikTok | — | 82.9 (228) | X2 = 51.20, p < .001, φ = 0.28 | ||||
| YouTube | 57.9 (208) | 84.4 (232) | X2 = 128.96, p < .001, φ = 0.45 | ||||
|
| |||||||
| 2015 M (SD) | 2022 M (SD) | Statistic | Male M (SD) | Female M (SD) | Statistic | ||
|
| |||||||
| Age (yrs) | 19.38 (2.87) | 19.05 (1.50) | t (632) = 1.86, p = .06, d = 0.14 | ||||
| BMI (kg/m2) | 24.10 (4.57) | 24.78 (5.79) | t (620) = 1.57, p = .06, d = 0.13 | ||||
| Min SM | 199.14 (142.56) | 244.06 (144.11) | 200.05 (133.57) | 232.30 (151.84) | |||
| # SM | 4.87 (2.25) | 7.18 (3.23) | 5.42 (2.84) | 6.10 (2.90) | |||
| BAS | 5.14 (1.19) | 4.88 (1.31) | 5.33 (1.10) | 4.79 (1.31) | |||
| FNAES | 2.40 (1.09) | 2.76 (1.25) | 2.14 (0.98) | 2.89 (1.20) | |||
| EDE-Q binge | 2.02 (4.09) | 2.43 (5.10) | 1.42 (3.57) | 2.83 (5.11) | |||
| EDE-Q vomit | 0.14 (0.95) | 0.41 (2.17) | 0.11 (0.67) | 0.40 (2.20) | |||
| EDE-Q laxative | 0.19 (1.73) | 0.61 (2.71) | 0.11 (0.85) | 0.56 (2.84) | |||
Note: EDE–Q = Eating Disorder Examination — Questionnaire; BMI = body mass index, Min SM — minutes spent daily on social media, # SM = total number of social media accounts, BAS = Body Appreciation Scale, FNAES = Fear of Negative Appearance Evaluation Scale, EDE–Q Binge = EDE–Q frequency of binge eating (in days/past 28 days), EDE–Q Vomit = EDE–Q frequency of vomiting in days/past 28 days), EDE–Q Laxative = EDE–Q frequency of laxative use in days/past 28 days).
3.1.1. Hypothesis 1a
There were significant univariate main effects of timepoint on minutes spent on SM per day and total number of SM accounts, with more use reported by 2022 participants. There was a significant univariate main effect of gender on time spent on SM and number of accounts held, with women engaging in more frequent SM use via reporting use of more SM accounts at both timepoints. Compared to respondents in 2015, 2022 participants were significantly more likely to use Snapchat, TikTok, and YouTube and significantly less likely to use Facebook and Twitter, with no significant differences in the reported use of Instagram.
3.1.2. Hypothesis 1b
Two thirds of participants in the 2022 sample reported using SM more since the start of the COVID-19 pandemic (n = 163, 64.2 %), 23.6 % (n = 60) stated that the pandemic had not changed how often they use SM, and 11.0 % (n = 28) described a decrease in SM use as a result of the pandemic. The sample was about evenly split when describing the impact of SM on their life since the start of the pandemic, with 31.4 % (n = 80) describing mostly positive impacts, 29.0 % (n = 74) endorsing negative effects, and 37.6 % (n = 96) denying any impact of the COVID-19 pandemic on their experience of SM.
3.1.3. Hypothesis 1c
Compared to the 2015 sample, 2022 participants reported significantly greater body image and related difficulties as reflected in scores on the BAS and FNAES. Women reported significantly lower BAS scores and significantly greater fears of negative appearance evaluation at both timepoints.
There were significant univariate main effects of timepoint on frequency of vomiting and laxative use, with 2022 respondents reporting greater frequency of these behaviors. There were significant univariate main effects of gender on frequency of binge eating and laxative use, with women in both samples reporting significantly greater frequency of these behaviors.
3.2. Aim 2: to examine if associations among SM use and disordered body image and eating behaviors are moderated by specific content consumed in a current sample of undergraduates
Most 2022 respondents agreed that SM allows them to view a range of diverse content (87.1 %, n = 222) that includes people who look like them (73.3 %, n = 187). A substantial proportion of participants reported that they seek out specific SM content related to weight loss (22.9 %, n = 63) and body positivity/neutrality (31.6 %, n = 87). Participants active on Facebook, Instagram, Twitter, Snapchat, and TikTok were especially likely to report seeking content related to body positivity/neutrality compared to participants not active on these platforms (all p < .05), with no significant associations between use of specific SM platforms and the likelihood of seeking out content related to weight loss.
Female respondents were significantly more likely than men to report seeking content related to weight loss and body positivity/neutrality (both p < .05). Compared to respondents not exposed to this content, respondents seeing weight loss content or content related to body positivity/neutrality reported significantly higher BMI, lower body appreciation, greater fears of negative appearance evaluation, and more frequent binge eating, and laxative use (all p < .05).
Time spent on SM each day was significantly and inversely associated with BAS scores and significantly and positively correlated with BMI, ratings on the FNAES, and frequency of binge eating and vomiting; number of SM accounts subscribed to was significantly and positively correlated with FNAES scores and frequency of binge eating (p < .05) [see Supplemental Materials for detailed descriptives and analyses].
3.2.1. Hypothesis 2a
Regression models examining the main and interactive effects of time spent on SM and exposure to weight loss content on body appreciation and fear of negative appearance evaluation scores and frequency of binge eating and laxative use were significant (Table 2). There were significant main effects of exposure to weight loss content, but not time spent on SM, on BAS and FNAES scores and frequency of binge eating. Time spent on SM and exposure to weight loss content interacted to predict binge eating frequency, such that respondents spending more time on SM (as defined via a median split of reports of minutes spent on SM each day) only reported high binge frequency if they were also exposed to weight loss content (Fig. 1).
Table 2.
Moderated regression analyses assessing main and interactive effects of the impact of time spent on social media, total number of social media accounts used, and exposure to weight loss content on body image and disordered eating behaviors.
| Step | Body Appreciation Scale | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | 0.46 (0.15, 0.77) | 0.18 | 2.92* | 0.15 | 0.15 | 20.00*,# | 2232 | Gender | 0.47 (0.15, 0.78) | 0.18 | 2.99* | 0.12 | 0.12 | 16.00*,# | 2225 |
| BMI | −0.06 (−0.08, −0.03) | −0.25 | −3.99*,# | BMI | −0.05 (−0.08, −0.02) | −0.22 | −3.49*,# | |||||||||
| 2 | Min SM | −0.001 (−0.002, 0.001) | −0.06 | −0.80 | 0.20 | 0.05 | 6.95*,# | 2230 | # SM | −0.04 (−0.10, 0.01) | −0.11 | −1.62 | 0.17 | 0.05 | 6.05*,# | 2223 |
| WL | −0.62 (−0.99, −0.26) | −0.21 | −3.37*,# | WL | −0.60 (−0.98, −0.23) | −0.21 | −3.20*,# | |||||||||
| 3 | Min SM × WL | 0.000 (−0.003, 0.002) | −0.02 | −0.32 | 0.20 | 0.00 | 0.10 | 1229 | # SM × WL | 0.06 (−0.06, 0.18) | 0.07 | 0.98 | 0.17 | 0.004 | 0.95 | 1222 |
|
| ||||||||||||||||
| Step | Fear of Negative Appearance Evaluation Scale | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −0.81 (−1.10, −0.51) | −0.32 | −5.41*,# | 0.18 | 0.18 | 24.43*,# | 2227 | Gender | −0.81 (−1.10, −0.51) | −0.32 | −5.44*,# | 0.17 | 0.17 | 23.15*,# | 2221 |
| BMI | 0.02 (−0.003, 0.05) | 0.11 | 1.73 | BMI | 0.02 (−0.01, 0.04) | 0.07 | 1.19 | |||||||||
| 2 | Min SM | 0.001 (−0.001, 0.002) | 0.06 | 0.79 | 0.24 | 0.07 | 10.03*,# | 2225 | # SM | 0.07 (0.02, 0.12) | 0.19 | 2.80* | 0.27 | 0.09 | 13.83*,# | 2219 |
| WL | 0.70 (0.35, 1.04) | 0.25 | 4.02*,# | WL | 0.70 (0.36,1.04) | 0.25 | 4.06*,# | |||||||||
| 3 | Min SM × WL | 0.001 (−0.001, 0.003) | 0.05 | 0.68 | 0.25 | 0.002 | 0.46 | 1224 | # SM × WL | −0.01 (−0.12, 0.10) | −0.01 | −0.14 | 0.27 | 0.000 | 0.02 | 1218 |
|
| ||||||||||||||||
| Step | Binge eating frequency | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −1.11 (−2.30, 0.09) | −0.11 | −1.83 | 0.14 | 0.14 | 18.56*,# | 2233 | Gender | −1.44 (−2.64, −0.24) | −0.15 | −2.37* | 0.11 | 0.11 | 13.89*,# | 2226 |
| BMI | 0.22 (0.12, 0.33) | 0.25 | 4.15*,# | BMI | 0.17 (0.06, 0.29) | 0.19 | 3.07*,# | |||||||||
| 2 | Min SM | −0.002 (−0.01, 0.003) | −0.06 | −0.85 | 0.20 | 0.06 | 8.86*,# | 2231 | # SM | 0.14 (−0.06, 0.29) | 0.10 | 1.40 | 0.18 | 0.07 | 9.31*,# | 2224 |
| WL | 2.54 (1.14, 3.94) | 0.22 | 3.58*,# | WL | 2.67 (1.27, 4.08) | 0.24 | 3.75*,# | |||||||||
| 3 | Min SM × WL | 0.01 (0.01, 0.02) | 0.22 | 2.97*,# | 0.23 | 0.03 | 8.79*,# | 1230 | # SM × WL | 0.10 (−0.35, 0.55) | 0.03 | 0.44 | 0.18 | 0.001 | 0.19 | 1223 |
|
| ||||||||||||||||
| Step | Frequency of vomiting | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −0.22 (−0.78, 0.34) | −0.05 | −0.77 | 0.02 | 0.02 | 2.05 | 2233 | Gender | −0.32 (−0.91, 0.26) | −0.07 | −1.09 | 0.02 | 0.02 | 1.94 | 2226 |
| BMI | 0.01 (−0.04, 0.06) | 0.03 | 0.45 | BMI | 0.02 (−0.04, 0.07) | 0.05 | 0.69 | |||||||||
| 2 | Min SM | 0.001 (−0.002, 0.003) | 0.05 | 0.63 | 0.05 | 0.04 | 4.37* | 2231 | # SM | −0.01 (−0.11, 0.09) | −0.01 | −0.17 | 0.04 | 0.02 | 2.41 | 2224 |
| WL | 0.60 (−0.05, 1.25) | 0.12 | 1.81 | WL | 0.75 (0.07, 1.44) | 0.15 | 2.16 | |||||||||
| 3 | Min SM × WL | 0.004 (0.000, 0.01) | 0.14 | 1.79 | 0.07 | 0.01 | 3.20 | 1230 | # SM × WL | 0.03 (−0.19, 0.25) | 0.02 | 0.26 | 0.04 | 0.000 | 0.07 | 1223 |
|
| ||||||||||||||||
| Step | Frequency of laxative use | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −0.43 (−1.12, 0.25) | −0.08 | −1.24 | 0.03 | 0.03 | 4.06* | 2233 | Gender | −0.59 (−1.28, 0.10) | −0.11 | −1.70 | 0.05 | 0.05 | 6.44*,# | 2226 |
| BMI | 0.03 (−0.03, 0.09) | 0.07 | 1.09 | BMI | 0.06 (−0.002, 0.13) | 0.13 | 1.92 | |||||||||
| 2 | Min SM | −0.001 (−0.004, 0.002) | −0.06 | −0.74 | 0.07 | 0.03 | 4.05* | 2231 | # SM | −0.02 (−0.14, 0.10) | −0.02 | −0.31 | 0.08 | 0.02 | 2.77 | 2224 |
| WL | 0.90 (0.09, 1.70) | 0.15 | 2.20* | WL | 0.83 (0.02, 1.64) | 0.14 | 2.03* | |||||||||
| 3 | Min SM × WL | 0.01 (0.002, 0.01) | 0.22 | 2.73* | 0.10 | 0.03 | 7.45* | 1230 | # SM × WL | 0.28 (0.02, 0.54) | 0.15 | 2.10* | 0.10 | 0.02 | 4.39* | 1223 |
Note: B, β and t reflect values from the final regression equation; BMI = body mass index, Min SM = minutes spent daily on social media, # SM = total number of social media accounts, WL = exposure to weight loss content.
p < .05 (Bonferroni adjusted).
p < .003 (Bonferroni adjusted).
Fig. 1.
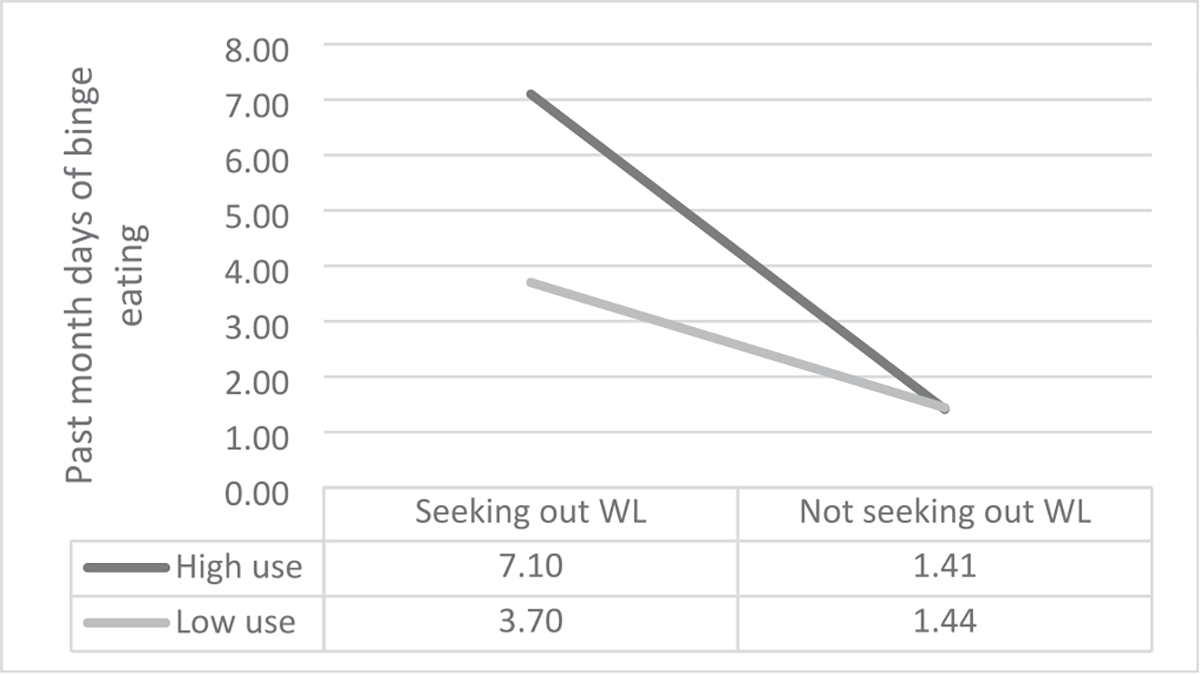
Interactive effects of time spent on social media and exposure to weight loss content on past month days of binge eating as measured via the Eating Disorders Examination — Questionnaire.
Note: High versus low use was defined via a median split of responses to the question about minutes spent on social media per day.
Regression models examining the main and interactive effects of total number of SM accounts used and exposure to weight loss content on body appreciation and fear of negative appearance evaluation scores and frequency of binge eating and laxative use were also significant, with exposure to weight loss content, but not total number of SM accounts used, emerging as a significant predictor in all models and no evidence for any interaction effects (Table 2).
3.2.2. Hypothesis 2b
Regression models examining the main and interactive effects of frequency of SM use and exposure to body positivity/neutrality content on body appreciation and fear of negative appearance evaluation scores and binge eating frequency were significant; however, addition of main effects in Step 2 and the interaction term in Step 3 did not produce significant R2 changes and none emerged as significant predictors in the final model (Table 3). Similarly, linear regression models examining the main and interactive effects of total number of SM accounts used and exposure to body positivity/neutrality content on BAS and FNAES scores and binge eating frequency were significant but neither main effect emerged as a significant predictor in the final model and addition of the interaction term in Step 3 did not produce a significant R2 change.
Table 3.
Moderated regression analyses assessing main and interactive effects of the impact of time spent on social media, total number of social media accounts used, and exposure to body positivity/negativity content on body image and disordered eating behaviors.
| Step | Body Appreciation Scale | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | 0.48 ((0.14, 0.81) | 0.18 | 2.80* | 0.15 | 0.15 | 20.00*,# | 2232 | Gender | 0.48 (0.13, 0.82) | 0.19 | 2.77* | 0.12 | 0.12 | 16.00*,# | 2225 |
| BMI | −0.07 (−0.10, −0.04) | −0.30 | −4.89*,# | BMI | −0.06 (−0.09, −0.03) | −0.26 | −4.21*,# | |||||||||
| 2 | Min SM | −0.001 (−0.003, 0.000) | −0.13 | −1.57 | 0.16 | 0.01 | 1.66 | 2230 | # SM | −0.06 (−0.12, 0.000) | −0.15 | −1.97* | 0.14 | 0.01 | 1.54 | 2223 |
| BP | −0.24 (−0.59, 0.12) | −0.09 | −1.33 | BP | −0.21 (−0.58, 0.15) | −0.08 | −1.14 | |||||||||
| 3 | Min SM × BP | 0.001 (−0.001, 0.003) | 0.08 | 0.93 | 0.16 | 0.003 | 0.86 | 1229 | # SM × BP | 0.08 (−0.02, 0.19) | 0.12 | 1.54 | 0.15 | 0.01 | 2.37 | 1222 |
|
| ||||||||||||||||
| Step | Fear of Negative Appearance Evaluation Scale | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −0.79 (−1.10, 0.48) | −0.32 | −4.95*,# | 0.18 | 0.18 | 24.43*,# | 2227 | Gender | −0.80 (−1.12, −0.49) | −0.32 | −5.02*,# | 0.17 | 0.17 | 23.15*,# | 2221 |
| BMI | 0.04 (0.01, 0.06) | 0.18 | 2.96*,# | BMI | 0.03 (0.003, 0.06) | 0.13 | 2.19* | |||||||||
| 2 | Min SM | 0.002 (0.000, 0.003) | 0.16 | 2.09* | 0.20 | 0.03 | 3.86* | 2225 | # SM | 0.07 (0.02, 0.13) | 0.19 | 2.16* | 0.22 | 0.05 | 6.70*,# | 2219 |
| BP | 0.42 (0.09, 0.75) | 0.16 | 2.49* | BP | 0.30 (−0.04, 0.64) | 0.11 | 1.74 | |||||||||
| 3 | Min SM × BP | −0.002 (−0.004, 0.001) | −0.12 | −1.52 | 0.21 | 0.01 | 2.30 | 1224 | # SM × BP | −0.02 (−0.12, 0.08) | −0.03 | −0.37 | 0.22 | 0.000 | 0.14 | 1218 |
|
| ||||||||||||||||
| Step | Binge eating frequency | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −1.23 (−2.55, 0.08) | −0.12 | −1.84 | 0.14 | 0.14 | 18.56*,# | 2233 | Gender | −1.60 (−2.89, −0.30) | −0.16 | −2.42* | 0.11 | 0.11 | 13.89*,# | 2226 |
| BMI | 0.28 (0.18, 0.39) | 0.32 | 5.19*,# | BMI | 0.23 (0.12, 0.34) | 0.25 | 4.02*,# | |||||||||
| 2 | Min SM | 0.004 (−0.002, 0.01) | 0.09 | 1.16 | 0.15 | 0.01 | 1.78 | 2.231 | # SM | 0.22 (−0.004, 0.45) | 0.15 | 1.94* | 0.13 | 0.02 | 2.24 | 2224 |
| BP | 1.10 (−0.28, 2.49) | 0.10 | 1.57 | BP | 0.60 (−0.80, 2.00) | 0.06 | 0.85 | |||||||||
| 3 | Min SM × BP | −0.003 (−0.01, 0.01) | −0.05 | −0.54 | 0.15 | 0.001 | 0.30 | 1230 | # SM × BP | −0.15 (−0.55, 0.25) | −0.06 | −0.74 | 0.13 | 0.002 | 0.54 | 1223 |
|
| ||||||||||||||||
| Step | Frequency of vomiting | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −0.17 (−0.76, 0.43) | −0.04 | −0.55 | 0.02 | 0.02 | 2.05 | 2233 | Gender | −0.25 (−0.87, 0.37) | −0.06 | −0.80 | 0.02 | 0.02 | 1.94 | 2226 |
| BMI | 0.02 (−0.03, 0.07) | 0.06 | 0.89 | BMI | 0.03 (−0.02, 0.09) | 0.08 | 1.26 | |||||||||
| 2 | Min SM | 0.001 (−0.002, 0.004) | 0.05 | 0.62 | 0.04 | 0.03 | 3.17* | 2231 | # SM | −0.01 (−0.12, 0.10)0 .02 (−0.18, 0.21) | −0.02 | −0.22 | 0.03 | 0.01 | 1.22 | 2224 |
| BP | 0.40 (−0.22, 1.03) | 0.09 | 1.27 | BP | 0.51 (−0.15, 1.18) | 0.11 | 1.52 | |||||||||
| 3 | Min SM × BP | 0.03 (−0.001, 0.01) | 0.12 | 1.41 | 0.05 | 0.01 | 1.98 | 1230 | # SM × BP | 0.02 (−0.18, 0.21) | 0.01 | 0.17 | 0.03 | 0.000 | 0.03 | 1223 |
|
| ||||||||||||||||
| Step | Frequency of laxative use | |||||||||||||||
|
| ||||||||||||||||
| B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | B (95 % CI) | β | t | R2 | ΔR (Dean, 2021) | ΔF | df | |||
|
| ||||||||||||||||
| 1 | Gender | −0.39 (−1.13, 0.35) | −0.07 | −1.03 | 0.03 | 0.03 | 4.06* | 2233 | Gender | −0.53 (−1.27, 0.21) | −0.10 | −1.41 | 0.05 | 0.05 | 6.44*,# | 2226 |
| BMI | 0.05 (−0.01, 0.11) | 0.12 | 1.77 | BMI | 0.09 (0.02, 0.15) | 0.18 | 2.73* | |||||||||
| 2 | Min SM | 0.001 (−0.003, 0.004) | 0.03 | 0.35 | 0.05 | 0.02 | 2.04 | 2231 | # SM | 0.05 (−0.08, 0.18) | 0.06 | 0.76 | 0.07 | 0.01 | 1.33 | 2224 |
| BP | 0.64 (−0.14, 1.42) | 0.11 | 1.62 | BP | 0.58 (−0.22, 1.37) | 0.10 | 1.44 | |||||||||
| 3 | Min SM × BP | 0.002 (−0.004, 0.01) | 0.06 | 0.64 | 0.05 | 0.002 | 0.40 | 1230 | # SM × BP | −0.05 (−0.28, 0.18) | −0.03 | −0.42 | 0.07 | 0.001 | 0.18 | 1223 |
NOTE: B, β and t reflect values from the final regression equation; BMI = body mass index, Min SM = minutes spent daily on social media, #SM = total number of social media accounts, BP = exposure to body positivity content.
p < .05 (Bonferroni adjusted).
p < .003 (Bonferroni adjusted).
4. Discussion
Growing evidence points to an adverse impact of SM use on body image and eating behaviors (Marks et al., 2020; Santarossa & Woodruff, 2017; Vandenbosch, Fardouly, & Tiggemann, 2022). The aims of this study were twofold. First, we sought to compare patterns in SM use, body image disturbances, and disordered eating behaviors in across two cohorts of undergraduate students over the course of a time period that included the exponential rise of image-based SM platforms as well as the COVID-19 pandemic. Second, we aimed to assess the extent to which exposure to specific SM content may exacerbate or protect against the adverse effects of time spent on SM on body image and eating behaviors.
In support of our hypotheses, participants in the 2022 sample reported a greater amount of time spent on SM and accounts held compared to those in the 2015 sample, with a majority of participants attributing these changes at least in part to the impact of the COVID-19 pandemic. Participants described consumption of a broad range of diverse SM content, including weight loss and body positivity/neutrality content. As hypothesized, participants in the 2022 sample endorsed significantly more body image disturbances and disordered eating behaviors compared to those in the 2015 sample.
Analyses generally did not support our hypotheses regarding a moderating role of SM content consumed in the relationship between intensity of use (i.e., duration and number of platforms accessed) and measures of body image and disordered eating behaviors. Time spent on SM and number of platforms accessed were generally unrelated to outcomes of interest. However, there were consistent significant main effects of viewing weight loss content on SM on indices of body image satisfaction and disordered eating behaviors, with exposure to weight loss content associated with lower body appreciation, greater fears of negative appearance evaluation, and more frequent binge eating. Exposure to weight loss content was assessed as a binary (yes/no) variable; this finding may be even more relevant if this variable was measured continuously, in order to assess the extent to which more exposure may be associated with greater risk. Contrary to our initial hypotheses, consuming body positive/neutral content was neither harmful nor beneficial for participants in terms of body image or disordered eating behaviors. Although unexpected, these findings align with recent research suggesting that exposure to body positive media exacerbated the positive association between TikTok use and body dissatisfaction, and less exposure to the thin-ideal and societal expectations of bodies did not moderate the relationship between TikTok use and body dissatisfaction (Mink & Szymanski, 2022). Perhaps individuals who report higher levels of body acceptance and critiquing of appearance expectations may pay more, rather than less, attention to idealized body images on SM, which may lead to increased appearance comparison. The relationship between SM use and body image disturbance may be less influenced by sociocultural beauty ideals, and more so by the increased opportunity for appearance comparisons compared to people who do not use SM (Mink & Szymanski, 2022).
Taken together, our results suggest that it is not how long someone spends on SM, or the breadth of platforms accessed, but rather what type of content they are engaging with, that is associated with body image disturbance and disordered eating behaviors. Indeed, the one significant interaction identified in our analyses indicates that large amounts of time spent on SM are only predictive of binge eating frequency if participants are also exposed to weight loss content. Given the detrimental effects of mere exposure to weight loss content on physical and mental health outcomes, it is imperative to tailor prevention and treatment efforts to account for these impacts and to consider the ethical responsibilities of SM platforms and relevant stakeholders when it comes to monitoring this type of content (Marks et al., 2020).
4.1. Limitations and future directions
Important limitations to the current study include our assessment strategy, which did not reflect the distinction in recent research between body positivity and body neutrality in the context of ED treatment (Hartman-Munick et al., 2021), but instead quantified engagement with one or the other (i.e., “Do you seek out specific content on SM related to body positivity/neutrality?”). Though there is currently limited research on this question, it is possible that the two constructs (positivity versus neutrality) differ in meaningful ways, including in their impact on body image and eating behaviors. It should also be noted that although we asked participants to indicate the number of SM platforms they subscribe to, this question did not capture the extent to which they were active on each of these platforms. Future research should investigate the effects of body positivity and body neutrality content separately, given their potentially different impacts on body image.
The cross-sectional nature of our Aim 2 analyses inhibits causal explanations for associations between exposure to weight-loss content and relevant outcomes. As an alternative explanation to the adverse effects of exposure to weight loss content on body image disturbances and disordered eating behaviors, it is possible that individuals struggling with these issues are especially likely to seek out weight loss content on SM. Longitudinal studies are needed to clarify the exact nature and direction of these associations. Finally, EDE-Q data quantifying frequency of disordered eating behaviors were skewed due to many participants reporting no engagement in these behaviors; results from analyses of these data should therefore be interpreted with some caution. Future studies could address this limitation by using analytic methods with different distributions, such as zero-inflated models.
4.2. Conclusion
In 2022, emerging adults are using SM more than in years prior, with significantly more time spent on image-based platforms such as Snapchat, TikTok, and YouTube. Exposure to weight loss content is associated with poorer body image and disordered eating behaviors in the absence of main effects of time spent on SM or diversity of platforms accessed. Consumption of content related to body positivity/neutrality does not appear to exert meaningful protective effects. Continuing to investigate SM use with a more fine-grained approach is crucial to discern both its helpful and harmful effects and to inform effective prevention and intervention strategies.
Supplementary Material
Acknowledgments
Preparation of this manuscript is supported in part by the National Science Foundation Graduate Research Fellowship [Grant No. 1645421], awarded to Christina Sanzari. Dr. Gorrell is supported by the National Institutes of Mental Health (K23MH126201); Dr. Anderson is supported by the National Institutes of Mental Health (K23MH123910); Dr. Reilly is supported by the National Institutes of Mental Health (K23MH131871)
Footnotes
Declaration of competing interest
The authors have no conflicts of interest/disclosures to report.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eatbeh.2023.101722.
Data availability
Data will be made available on request.
References
- Center, P. R. (April 7, 2021). Social media fact sheet. Published. Pew Research Center; https://www.pewresearch.org/internet/fact-sheet/social-media/. [Google Scholar]
- Dean B (October 10, 2021). How many people use social media in 2022? (65+ Statistics) Accessed October 12, 2022. BACKLINKO; https://backlinko.com/social-media-users. [Google Scholar]
- Fitzgerald K, Yue Z, Wong JCS, & Green MC (2022). Entertainment and social media use during social distancing: Examining trait differences in transportability and need for social assurance. Psychology of Popular Media, 11(3), 305–310. 10.1037/ppm0000365 [DOI] [Google Scholar]
- Naslund JA, Bondre A, Torous J, & Aschbrenner KA (2020). Social media and mental health: Benefits, risks, and opportunities for research and practice. Journal of Technology in Behavioral Science, 5(3), 245–257. 10.1007/S41347-020-00134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland G, & Tiggemann M (2016). A systematic review of the impact of the use of social networking sites on body image and disordered eating outcomes. Body Image, 17, 100–110. 10.1016/j.bodyim.2016.02.008 [DOI] [PubMed] [Google Scholar]
- Zhang J, Wang Y, Li Q, & Wu C (2021). The relationship between SNS usage and disordered eating behaviors: A meta-analysis. Frontiers in Psychology, 12(August). 10.3389/fpsyg.2021.641919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiggemann M, & Slater A (2013). NetGirls: The internet, Facebook, and body image concern in adolescent girls. International Journal of Eating Disorders, 46(6), 630–633. 10.1002/EAT.22141 [DOI] [PubMed] [Google Scholar]
- Mabe AG, Forney KJ, & Keel PK (2014). Do you “like” my photo? Facebook use maintains eating disorder risk. International Journal of Eating Disorders, 47(5), 516–523. 10.1002/EAT.22254 [DOI] [PubMed] [Google Scholar]
- Eckler P, Kalyango Y, & Paasch E (2016). Facebook use and negative body image among U.S. college women. Women & Health, 57(2), 249–267. 10.1080/03630242.2016.1159268 [DOI] [PubMed] [Google Scholar]
- Linardon J, Messer M, Rodgers RF, & Fuller-Tyszkiewicz M (2022). A systematic scoping review of research on COVID-19 impacts on eating disorders: A critical appraisal of the evidence and recommendations for the field. International Journal of Eating Disorders, 55(1), 3–38. 10.1002/eat.23640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson CJ, Muñoz ME, Garza A, & Galindo M (2014). Concurrent and prospective analyses of peer, television and social media influences on body dissatisfaction, eating disorder symptoms and life satisfaction in adolescent girls. Journal of Youth and Adolescence, 43(1), 1–14. 10.1007/S10964-012-9898-9/FIGURES/4 [DOI] [PubMed] [Google Scholar]
- Meier EP, & Gray J (2014). Facebook photo activity associated with body image disturbance in adolescent girls. Cyberpsychology, Behavior and Social Networking, 17 (4), 199–206. 10.1089/cyber.2013.0305 [DOI] [PubMed] [Google Scholar]
- Kim JW, & Chock TM (2015). Body image 2.0: Associations between social grooming on Facebook and body image concerns. Computers in Human Behavior, 48, 331–339. 10.1016/J.CHB.2015.01.009 [DOI] [Google Scholar]
- Saiphoo AN, & Vahedi Z (December 2018). A meta-analytic review of the relationship between social media use and body image disturbance. Computers in Human Behavior, 2019(101), 259–275. 10.1016/j.chb.2019.07.028 [DOI] [Google Scholar]
- Fardouly J, & Vartanian LR (2015). Negative comparisons about one’s appearance mediate the relationship between Facebook usage and body image concerns. Body Image, 12(1), 82–88. 10.1016/J.BODYIM.2014.10.004 [DOI] [PubMed] [Google Scholar]
- Marks RJ, de Foe A, & Collett J (2020). The pursuit of wellness: Social media, body image and eating disorders. Children and Youth Services Review, 119(May), Article 105659. 10.1016/j.childyouth.2020.105659 [DOI] [Google Scholar]
- Hilbert A, Pike KM, Goldschmidt AB, et al. (2014). Risk factors across the eating disorders. Psychiatry Research, 220(1–2), 500–506. 10.1016/j.psychres.2014.05.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackard DM, Croll JK, & Kearney-Cooke A (2002). Dieting frequency among college females: Association with disordered eating, body image, and related psychological problems. Journal of Psychosomatic Research, 52(3), 129–136. 10.1016/S0022-3999(01)00269-0 [DOI] [PubMed] [Google Scholar]
- Chou W, Ying S, Prestin A, & Kunath S (2014). Obesity in social media: A mixed methods analysis. Translational Behavioral Medicine, 4(3), 314–323. 10.1007/s13142-014-0256-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogels EA, Gelles-Watnick R, & Teens MN (August 10, 2022). Social media and technology 2022 Accessed October 12, 2022. Pew Research Center; https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/. [Google Scholar]
- Simpson CC, & Mazzeo SE (2016). Skinny is not enough: A content analysis of fitspiration on Pinterest. Health Commuunications, 32(5), 560–567. 10.1080/10410236.2016.1140273 [DOI] [PubMed] [Google Scholar]
- Fung ICH, Blankenship EB, Ahweyevu JO, et al. (2020). Public health implications of image-based social media: A systematic review of Instagram, Pinterest, Tumblr, and Flickr. The Permanente Journal, 24. 10.7812/TPP/18.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casale S, Gemelli G, Calosi C, Giangrasso B, & Fioravanti G (2019). Multiple exposure to appearance-focused real accounts on Instagram: Effects on body image among both genders. Current Psychology, 40(6), 2877–2886. 10.1007/S12144-019-00229-6 [DOI] [Google Scholar]
- González-Nuevo C, Cuesta M, & Muñiz J (2021). Concern about appearance on Instagram and Facebook: Measurement and links with eating disorders. Cyberpsychology: Journal of Psychosocial Research on Cyberspace, 15(2), 9. 10.5817/CP2021-2-9 [DOI] [Google Scholar]
- Cohen R, Newton-John T, & Slater A (2017). The relationship between Facebook and Instagram appearance-focused activities and body image concerns in young women. Body Image, 23, 183–187. 10.1016/j.bodyim.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Fardouly J, & Vartanian LR (2016). Social media and body image concerns: Current research and future directions. Current Opinion in Psychology, 9, 1–5. 10.1016/j.copsyc.2015.09.005 [DOI] [Google Scholar]
- Jiotsa B, Naccache B, Duval M, Rocher B, & Grall-Bronnec M (2021). Social media use and body image disorders: Association between frequency of comparing one’s own physical appearance to that of people being followed on social media and body dissatisfaction and drive for thinness. International Journal of Environmental Research and Public Health, 18(6), 1–14. 10.3390/IJERPH18062880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberga AS, Withnell SJ, & von Ranson KM (2018). In, 6(39). Fitspiration and thinspiration: A comparison across three social networking sites (pp. 1–10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boepple L, & Thompson JK (2016). A content analytic comparison of fitspiration and thinspiration websites. International Journal of Eating Disorders, 49(1), 98–101. 10.1002/eat.22403 [DOI] [PubMed] [Google Scholar]
- Moreno J (December 29, 2021). TikTok surpasses Google, Facebook as world’s most popular web domain Accessed September 30, 2022. Forbes; https://www.forbes.com/sites/johanmoreno/2021/12/29/tiktok-surpasses-google-facebook-as-worlds-most-popular-web-destination/?sh=37838bad43ef. [Google Scholar]
- Ceci L (September 15, 2022). TikTok users by country 2022 | Statista Accessed September 30, 2022. Statista; https://www.statista.com/statistics/1299807/number-of-monthly-unique-tiktok-users/. [Google Scholar]
- Rodgers RF, Wertheim EH, Paxton SJ, Tylka TL, & Harriger JA (2022). #Bopo: Enhancing body image through body positive social media- Evidence to date and research directions. Body Image, 41, 367–374. 10.1016/j.bodyim.2022.03.008 [DOI] [PubMed] [Google Scholar]
- Perry M, Watson L, Hayden L, & Inwards-Breland D (2019). Using body neutrality to inform eating disorder management in a gender diverse world. The Lancet Child & Adolescent Health, 3(9), 597–598. 10.1016/S2352-4642(19)30237-8 [DOI] [PubMed] [Google Scholar]
- Stevens A, & Griffiths S (2020). Body Positivity (#BoPo) in everyday life: An ecological momentary assessment study showing potential benefits to individuals’ body image and emotional wellbeing. Body Image, 35, 181–191. 10.1016/J.BODYIM.2020.09.003 [DOI] [PubMed] [Google Scholar]
- Lazuka RF, Wick MR, Keel PK, & Harriger JA (2020). Are we there yet? Progress in depicting diverse images of beauty in Instagram’s body positivity movement. Body Image, 34, 85–93. 10.1016/J.BODYIM.2020.05.001 [DOI] [PubMed] [Google Scholar]
- Cook-Cottone CP (2015). Incorporating positive body image into the treatment of eating disorders: A model for attunement and mindful self-care. Body Image, 14, 158–167. 10.1016/J.BODYIM.2015.03.004 [DOI] [PubMed] [Google Scholar]
- Avalos L, Tylka TL, & Wood-Barcalow N (2005). The Body Appreciation Scale: Development and psychometric evaluation. Body Image, 2(3), 285–297. 10.1016/J.BODYIM.2005.06.002 [DOI] [PubMed] [Google Scholar]
- Lundgren JD, Anderson DA, & Thompson JK (2004). Fear of negative appearance evaluation: Development and evaluation of a new construct for risk factor work in the field of eating disorders. Eating Behaviors, 5(1), 75–84. 10.1016/S1471-0153(03)00055-2 [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C, & Beumont PJV (2004). Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy, 42(5), 551–567. 10.1016/S0005-7967(03)00161-X [DOI] [PubMed] [Google Scholar]
- Lowe MR, Thomas JG, Safer DL, & Butryn ML (2007). The relationship of weight suppression and dietary restraint to binge eating in bulimia nervosa. International Journal of Eating Disorders, 40(7), 640–644. 10.1002/EAT.20405 [DOI] [PubMed] [Google Scholar]
- Lengvenyte A, Strumila R, Maimoun L, et al. (2021). A specific association between laxative misuse and suicidal behaviours in patients with anorexia nervosa and bulimia nervosa. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity, 27(1), 307–315. 10.1007/S40519-021-01180-X [DOI] [PubMed] [Google Scholar]
- Mathisen TF, Rosenvinge JH, Friborg O, et al. (2020). Is physical exercise and dietary therapy a feasible alternative to cognitive behavior therapy in treatment of eating disorders? A randomized controlled trial of two group therapies. The International Journal of Eating Disorders, 53(4), 574–585. 10.1002/EAT.23228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. (2021). SPSS Statistics for Windows, Version 28.0. Published online. [Google Scholar]
- Serier K (2016). Measurement invariance of the eating disorder examination questionnaire (EDE-Q) in a college sample of non-Hispanic white and Hispanic women. University of New Mexico. [DOI] [PubMed] [Google Scholar]
- Hilbert A, de Zwaan M, & Braehler E (2012). How frequent are eating disturbances in the population? Norms of the eating disorder examination-questionnaire. PLoS One, 7(1). 10.1371/journal.pone.0029125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenbosch L, Fardouly J, & Tiggemann M (2022). Social media and body image: Recent trends and future directions. Current Opinion in Psychology, 45, Article 101289. 10.1016/j.copsyc.2021.12.002 [DOI] [PubMed] [Google Scholar]
- Santarossa S, & Woodruff SJ (2017). #Socialmedia: Exploring the relationship of social networking sites on body image, self-esteem, and eating disorders. Social Media and Society, 3(2). 10.1177/2056305117704407 [DOI] [Google Scholar]
- Mink DB, & Szymanski DM (2022). TikTok use and body dissatisfaction: Examining direct, indirect, and moderated relations. Body Image, 43, 205–216. 10.1016/j.bodyim.2022.09.006 [DOI] [PubMed] [Google Scholar]
- Hartman-Munick SM, Silverstein S, Guss CE, Lopez E, Calzo JP, & Gordon AR (2021). Eating disorder screening and treatment experiences in transgender and gender diverse young adults. Eating Behaviors, 41(April), Article 101517. 10.1016/j.eatbeh.2021.101517 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.


