Abstract
Background
Intradural disc herniations (IDH) are uncommon and can be found in the cervical spine. It is commonly associated with Brown-Sequard syndrome (BSS). The case report describes cervical spine magnetic resonance imaging (MRI) findings that assists in identifying IDH pre-operatively and discusses surgical management.
Case Description
This is a case report regarding a 42-year-old obese male who developed atraumatic spontaneous bilateral upper extremity numbness, right upper extremity weakness and right lower extremity weakness. MRI showed a C6-7 herniated nucleus pulposus that focally protruded through the posterior longitudinal ligament with a beak-like projection similar to what has been described in previous reports. Clinical exam revealed an incomplete spinal cord injury (SCI) most consistent with BSS. He underwent anterior cervical discectomy and fusion at the level of C6-7. Intra-operatively, a disc fragment was found to be embedded in the dura. Three months post-operatively, the patient had persistent weakness in his right lower extremity but no longer had any bilateral upper extremity weakness.
Conclusions
An anterior cervical decompression and fusion was performed shortly after the patient presented, with adequate neurological recovery after 3 months. Advanced imaging with an MRI could lead to the diagnosis of an IDH and surgical intervention via the anterior approach could facilitate removal of the disc and adequate dura repair.
Keywords: Brown-Sequard syndrome (BSS), intradural cervical disc herniation, cervical discectomy and fusion, case report
Highlight box.
Key findings
• Triangular configuration of the disc seen on MRI is probably the most useful sign for preoperative diagnosis of an intradural disc herniation.
What is known and what is new?
• Cervical intradural disc herniation can present as a form of Brown Sequard syndrome.
• Cervical spine MRI is useful for diagnosing intradural disc herniation. Anterior cervical decompression and fusion is an acceptable treatment option.
What is the implication, and what should change now?
• An anterior approach is a safe and effective treatment for cervical intradural disc herniation as seen on MRI.
Introduction
The incidence of spinal cord injuries (SCI) worldwide is about 15 to 40 cases per million annually, with estimated cost of treatment in the United States to be up to $4 billion per year (1). Brown-Sequard syndrome (BSS) accounts for only about 3% of traumatic SCIs and is defined as ipsilateral weakness or paralysis and loss of proprioception associated with contralateral loss of pain and temperature sensation (2). Intradural disc herniations (IDH) are uncommon and were first described by Dandy et al. in 1942 with only 3% found in the cervical spine (3). According to a systematic review performed by Guan et al., 56.5% of cervical IDH patients present with a form of BSS (4). Because of the rarity of cervical IDH, there is no consensus on the imaging diagnosis or treatment apart from generalized surgical management and there is minimal literature on this topic. This case report will elucidate presentation and management of a cervical IDH patient and his post-operative course. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-22-82/rc).
Case presentation
Patient information
A 42-year-old obese male patient developed sudden onset of bilateral upper extremity numbness, right upper extremity weakness and right lower extremity weakness. When these symptoms did not improve, he presented to an outside hospital 5 days later. Advanced imaging was obtained and he was transferred to the University of Missouri Hospital for further work up and management. He reported a vague numbness over his arms, the inability to bear weight on his right lower extremity due to weakness, and bilateral upper extremity weakness, right more than left. Additionally, he reported symptoms concerning for myelopathy, including acute balance issues, clumsiness with his hands, and difficulty with fine-motor activities. He denied bowel or bladder involvement. These symptoms developed atraumatically and without any identifiable inciting event.
Prior to the onset of these symptoms, the patient reported no significant history of neck or spine issues and denied any prior symptoms similar to these. His spine was naïve to prior intervention, surgeries, or trauma. His past medical history is significant for obesity, with a body mass index (BMI) of 34 at presentation, as well as chronic bipolar and anxiety disorders for which he sees a psychiatrist. He was a pack per day smoker.
Clinical findings
His exam in the emergency department demonstrated significant weakness in bilateral upper extremities, right worse than left, at the levels of C6 and below—specifically (grade 4 to 4+ out of 5), he had appreciable weakness with wrist extension and flexion, metacarpal phalangeal extension and flexion, and in his intrinsics. He demonstrated a positive Hoffman’s sign bilaterally, hyperreflexic bilaterally, and a positive escape sign on the right. His sensation was deemed intact to light touch but diminished in a scattered and non-dermatomal pattern of his upper extremities. His lower extremity exam demonstrated weakness on the right side with no appreciable ability to flex or extend his knee or dorsiflex his ankle. There was appreciable plantarflexion strength against gravity, but not against resistance. He was hyperreflexic, with upgoing Babinski signs bilaterally.
Timeline
Patient presented to an outside hospital 5 days after the onset of his symptoms. A magnetic resonance imaging (MRI) was performed at that time. He was immediately transferred to the University of Missouri—a level 1 trauma center—where workup was continued, and the orthopaedic spine team was immediately involved. The patient was placed on the operating room (OR) schedule for the following morning and underwent the surgical intervention outlined below. Although his symptoms significantly improved postoperatively, he was left with significant weakness and sensory changes on the right upper and lower extremities that continued to improve through his postoperative care visits.
Diagnostic assessment
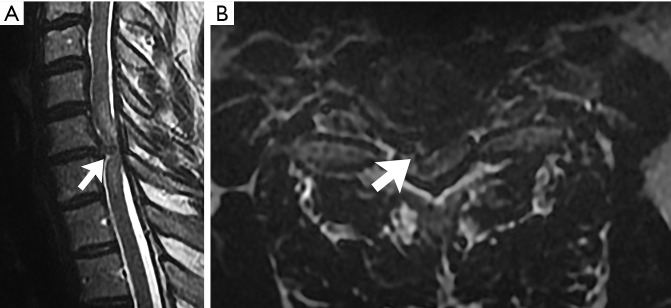
Advanced imaging (Figure 1) included cervical, thoracic, and lumbar spine MRIs. The cervical MRI demonstrated a large right paracentral C6-7 herniated nucleus pulposus that resulted in severe cord compression, central canal and neuroforaminal stenosis, and associated cord edema. There was a noticeable indentation of the spinal cord secondary to the herniated disc and significant surrounding abnormal high T2 signal intensity within the cord, spanning from C5-7T1 on the right. There was evidence of a posterior longitudinal ligament tear and the possibility of intradural herniation of the disc was raised. After thorough discussion with the patient, we elected to proceed with anterior cervical discectomy and fusion of C6-7.
Figure 1.
Cervical magnetic resonance imaging at time of presentation. (A) Sagittal T2W magnetic resonance imaging shows the beak-like projection of herniated disk (arrow). The configuration is strikingly different from the usual more oval shape of disk herniation. There is severe mass effect on the spinal cord, and edema centered at the disk. (B) Axial T2W magnetic resonance imaging shows that the intradural portion (arrow) is narrow, extending through a focal defect in the dura, beyond the contour of the broader herniation. T2W, T2 weighted.
Therapeutic intervention
The approach was taken through a standard left sided approach. An annulotomy was performed at the C6-7 disc space and the disc was removed. Posteriorly there was an obvious indentation in the posterior longitudinal ligament on the right side with multiple large disc fragments located posterior to this rent. There was a cerebrospinal fluid (CSF) leak identified after removal of these disc fragments. Careful examination showed adhesions of the posterior longitudinal ligament to the dura with a thin layer of arachnoid mater protruding through the dura mater. There was significant discoloration and hemorrhage of the dura. A disc fragment was identified as embedded in the dura. This disc fragment was removed from beneath the dura using a micropituitary, resulting in propagation of the CSF leak. After disc fragments were removed, the dura was repaired using DuraSeal and DuraGen (Integra LifeSciences, Princeton, NJ, USA).
Follow-up and outcomes
Immediately after the surgery, patient had improvement of his right sided weakness. The patient progressed with therapy over the course of 5 days in the hospital and was able to discharge to home. During his hospital stay, he had right shoulder pain that could not be completely explained by his disc herniation and was referred as an outpatient to a shoulder and elbow specialist. At approximately 3 months postoperatively he received a subacromial corticosteroid injection and his shoulder symptoms slowly resolved. At 3- and 6-month follow-up the patient had complete resolution of his right upper extremity weakness but did continue to have weakness in his right lower extremity (grade 4 to 4− out of 5). He could ambulate approximately 100 feet without the use of an assistive device but uses a cane for distances greater than 100 feet. Overall, the patient has been mostly satisfied with his improvement but has been unable to return to work due to the complex physical nature of his work. At 6-month follow-up the patient’s PROMIS physical and mental health scores were 34.9 and 33.8 respectively, and Neck Disability Index (NDI) score was 52.
Cervical MRI obtained 3-month postoperatively showed near complete resolution of spinal cord edema and no evidence of residual disc herniation causing mass effect on the spinal cord, as shown in Figure 2.
Figure 2.

Sagittal postoperative cervical magnetic resonance imaging at 3 months shows resolution of cord abnormality.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In this case report, we described a cervical intradural herniated disc resulting in BSS treated with anterior cervical decompression and fusion. Imaging diagnosis of an intradural herniated disc is desirable for operative planning, but there are only anecdotal reports of imaging findings. A literature review of cervical IDHs by Guan et al. in 2018 (4). found that a preoperative MRI diagnosis was suggested in only 3/23 (13%) of patients. A variety of suggestive imaging signs have been reported. Hidalgo-Ovejero et al. stated that the presence of epidural gas on computed tomography (CT) could be used as an indication of intradural herniated disc (5), but that finding is highly nonspecific, often present in uncomplicated disc herniations in the setting of underlying disc disease with vacuum phenomenon. MRI is the standard imaging study to diagnose cervical disc herniations. Several other signs have been anecdotally described. Choi et al. (6) described 2 cases showing a focal defect in the posterior longitudinal ligament (PLL), and a triangular, central disc projection compressing the cord, which they designated a “hawk-beak sign”. Börm et al. (7) and Celano et al. (8) both found that the intradural disc was surrounded by a high signal intensity halo on T2-weighted imaging. Although not described by the authors, both the halo sign and a beak-like central projection are also present in a case reported by Baudracco et al. (9).
D’Andrea et al. (10) employed intravenous gadolinium in the MRI evaluation of 4 cases of lumbar IDH, and found that 3 of the 4 showed ring enhancement. This most likely correlates to the high signal intensity halo seen on T2-weighted imaging by Börm and Celano, but the report by D’Andrea does not mention T2 findings. Gadolinium is rarely used for the preoperative diagnosis of disc herniation and therefore this sign is of limited usefulness. Sasaji et al. (11) reported a single case of a split between the dura and arachnoid mater creating a “Y-sign”; this sign has not been replicated in other reports.
Our case did not show a halo or a “Y” sign. It did show on both the sagittal and axial images the sharp, focal, triangular “beak sign” previously described. This appearance is quite different from the more rounded contour typically seen in disc herniations in the epidural space or contained by the PLL. We agree with previous authors that this triangular configuration of the disc herniation reflects extension through the focal dural compromise, and it is probably the most useful sign for preoperative diagnosis of an IDH.
Surgical intervention is the definitive treatment of cervical intradural herniated disc herniations, with all patients documented in the literature undergoing surgery (12). Reports in the literature, as well as our case report, indicate that anterior approach is able to directly access the herniated disc, facilitate removal of disc fragments and repair of the dura. Posterior approach to the cervical spine in this setting would not be warranted.
Conclusions
Triangular configuration of the disc seen on MRI is probably the most useful sign for preoperative diagnosis of an IDH. We performed an anterior cervical decompression and fusion shortly after the patient presented, which resulted in good neurological recovery after 3 months. Overall, this anterior approach is a safe and effective treatment for cervical IDH.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: Funding was obtained from within the Department of Orthopaedic Surgery at the University of Missouri-Columbia.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Footnotes
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-22-82/rc
Peer Review File: Available at https://acr.amegroups.com/article/view/10.21037/acr-22-82/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-22-82/coif). The authors have no conflicts of interest to declare.
References
- 1.Sekhon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976) 2001;26:S2-12. 10.1097/00007632-200112151-00002 [DOI] [PubMed] [Google Scholar]
- 2.Wirz M, Zörner B, Rupp R, et al. Outcome after incomplete spinal cord injury: central cord versus Brown-Sequard syndrome. Spinal Cord 2010;48:407-14. 10.1038/sc.2009.149 [DOI] [PubMed] [Google Scholar]
- 3.Dandy WE. Serious complications of ruptured intervertebral disks. JAMA 1942;119:474-7. [Google Scholar]
- 4.Guan Q, Xing F, Long Y, et al. Cervical intradural disc herniation: A systematic review. J Clin Neurosci 2018;48:1-6. 10.1016/j.jocn.2017.10.024 [DOI] [PubMed] [Google Scholar]
- 5.Hidalgo-Ovejero AM, Garcia-Mata S, Izco-Cabezon T, et al. Intradural disc herniation associated with epidural gas. Spine (Phila Pa 1976) 1998;23:281-3. 10.1097/00007632-199801150-00027 [DOI] [PubMed] [Google Scholar]
- 6.Choi JY, Lee WS, Sung KH. Intradural lumbar disc herniation—is it predictable preoperatively? A report of two cases. Spine J 2007;7:111-7. 10.1016/j.spinee.2006.02.025 [DOI] [PubMed] [Google Scholar]
- 7.Börm W, Bohnstedt T. Intradural cervical disc herniation. Case report and review of the literature. J Neurosurg 2000;92:221-4. [PubMed] [Google Scholar]
- 8.Celano EC, Sayah A, McGrail K. Cervical intradural disc herniation, case report and reflection on preoperative imaging. Radiol Case Rep 2019;14:1076-8. 10.1016/j.radcr.2019.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baudracco I, Grahovac G, Russo VM. Spontaneous cervical intradural disc herniation presenting with Brown-Séquard and Horner’s syndrome: lesson learned from a very unique case. Eur Spine J 2017;26:218-21. 10.1007/s00586-017-5044-4 [DOI] [PubMed] [Google Scholar]
- 10.D’Andrea G, Trillò G, Roperto R, et al. Intradural lumbar disc herniations: the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev 2004;27:75-80; discussion 81-2. 10.1007/s10143-003-0296-3 [DOI] [PubMed] [Google Scholar]
- 11.Sasaji T, Horaguchi K, Yamada N, et al. The specific sagittal magnetic resonance imaging of intradural extra-arachnoid lumbar disc herniation. Case Rep Med 2012;2012:383451. 10.1155/2012/383451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang HS, Oh YM, Eun JP. Cervical Intradural Disc Herniation Causing Progressive Quadriparesis After Spinal Manipulation Therapy: A Case Report and Literature Review. Medicine (Baltimore) 2016;95:e2797. 10.1097/MD.0000000000002797 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as