Abstract
STUDY DESIGN:
Retrospective cohort study.
OBJECTIVE:
To evaluate falls among elective orthopaedic inpatients at a musculoskeletal hospital.
BACKGROUND:
Falls are the most commonly reported hospital incidents. Approximately 30% of in-hospital falls result in minor injury, and up to 8% of falls result in moderate to severe injury. Given the projected rise in elective orthopaedic procedures, it is important to better understand fall patterns in this population.
METHODS:
A retrospective review of electronic medical records and patient charts (2000–2009) was conducted to identify falls in patients admitted for elective orthopaedic procedures.
RESULTS:
There were 868 falls among orthopaedic patients older than 18 years. The fall rate was 0.9% of admissions, or 2.0 falls per 1000 inpatient days. The average age of the patients who had fallen was 68 years, and 57.6% were women. Knee replacements (38.2%), spine procedures (18.5%), and hip replacements (14.7%) were the procedures most commonly associated with falls. Three hundred eighty-six falls (45.8%) involved bathroom usage. One hundred ten first falls (13.1%) resulted in injuries. Twenty-eight falls (3.3%) resulted in serious events, including 5 returns to the operating room, 3 transfers to a higher level of care, 14 prosthesis dislocations, 6 fractures, 2 intracranial bleeds, and 1 hemorrhage. Patients with serious injuries were more likely to fall earlier (mean postoperative days, 2.7 versus 4.1; mean difference, 1.4 days; 95% confidence interval: 0.51, 2.3; P = .003) and to have had hip replacement (odds ratio = 3.7; 95% confidence interval: 1.7, 8.2). Serious injuries were not associated with body mass index, age, gender, hospital location, day, or fall history.
CONCLUSION:
Falls are avoidable events that are poorly described among orthopaedic patients having elective procedures. This large series identifies hip replacement patients as being at almost 4-fold risk of having a serious adverse event after falling. Larger prospective trials are needed to confirm results and to inform prevention strategies.
Keywords: adverse event, fear-avoidance, hip replacement, injury, inpatient care, postoperative risk
Falls are the most commonly reported incidents in hospitals.14 Approximately 30% of in-hospital falls result in minor injury, and up to 8% of falls result in moderate to severe injury.8,10,12,16,18 Falls also lead to longer hospital stays3,13 and increased costs.3 Even falls without serious sequelae can contribute to a pernicious “fear of falling” cycle, which can continue after discharge.19
Studies evaluating falls have focused primarily on falls in the community, falls in long-term residential care institutions, and falls in sick hospitalized patients. However, falls that occur during admission for elective orthopaedic procedures are less well characterized. It is known that risk of falling is associated with poor walking ability,17 which suggests that the postoperative period, when pain and weakness can affect walking ability, may be a time of increased risk. Given the projected rise in elective orthopaedic procedures over the coming decades,18 it will be increasingly important to better understand fall patterns in this population, and especially risks for falls resulting in serious injuries. This study evaluates falls among orthopaedic patients admitted to a musculoskeletal specialty hospital from 2000 to 2009.
METHODS
This is a retrospective cohort study evaluating falls at the Hospital for Special Surgery, a musculoskeletal specialty hospital in New York City. All falls between 2000 and 2009 were included in the calculation of hospital fall rates. Only orthopaedic inpatients over 18 years of age were included in subsequent analyses of falls among admitted adult orthopaedic patients. Because the hospital has no emergency room or urgent care department, orthopaedic patients are admitted almost exclusively for elective procedures. A small percentage of inpatients are admitted for chronic pain, medical complications of orthopaedic procedures, or rheumatologic complaints.
Patients who fell were identified by nurses on the inpatient units. Nurses were required to report any fall that occurred during their shift, prior to leaving the hospital, and to conduct a standardized interview with the patient as soon as possible after the fall—usually within 24 hours. Falls were defined as “an unexpected event in which the participant comes to rest on the ground, floor, or lower level.”14
Results from the patient interview were recorded on paper forms and manually entered into an electronic database. Chart review was performed to obtain missing data. Type of surgical procedure was identified from the hospital’s Information Technology department, using ICD-9 procedure codes. Information Technology reports were also used to validate the date of birth and procedure date for all patients. To ensure that the sample was not biased and did not preferentially miss falls during certain days or on certain shifts, a complementary case-finding strategy was employed. Electronic hospital administrative data were used to identify patients who received an ICD-9 fall code (720.2, E849.7, E880-E888, E928.9, E929.3) from 2000 to 2009. The charts of these patients were reviewed. When a record of an in-hospital fall and the patient met the study inclusion criteria, the patient was added to the cohort, if not already included. Newly identified falls had additional chart review to obtain similar clinical data obtained on other falls. All patients received standardized, procedure-specific, postoperative rehabilitation, with early ambulation as the goal for lower extremity arthroplasties. Specific physical therapy protocols varied over the study period.
Patients were considered to be at high risk of falling if they reported a previous fall in any location or had a documented history of an in-hospital fall. A serious fall was defined as one resulting in return to the operating room, transfer to a higher level of care, prosthesis dislocation, fracture, intracranial bleed, or death.
This study was approved by the Institutional Review Board at Hospital for Special Surgery.
Statistical Methods
Frequency distributions were calculated to summarize the characteristics of falls in these patients. Risk factors associated with falling or serious falls were calculated using chi-square or t test statistics, as appropriate. A logistic regression was performed to identify variables associated with having a serious fall among patients who fell. This model controlled for age, gender, and covariates that were significantly correlated with serious falls in univariate analyses. A P value of .05 was considered statistically significant. No adjustment was made for multiple comparisons.
RESULTS
There were a total of 911 falls from January 1, 2000 to December 31, 2009. Eight hundred ninety-one falls were identified using the nursing data, with an additional 20 identified from ICD-9 codes. These falls represented 0.9% of admissions, or 2.0 falls per 1000 inpatient days. Falls were evenly distributed over days of the week (TABLE 1). There was no discernible trend in rates over the decade studied (FIGURE), although there was a near significant reduction in 2009 compared to previous years (P = .053). This may have been due to a nursing initiative to decrease falls, which was implemented that year. Of the 911 falls, 868 occurred in 842 orthopaedic inpatients 18 years of age or older, and were included in subsequent analyses.
TABLE 1.
Day of the Week That the First Fall Occurred
| Day of the Week | Frequency, n | Percent |
|---|---|---|
| Monday | 108 | 12.8 |
| Tuesday | 114 | 13.5 |
| Wednesday | 117 | 13.9 |
| Thursday | 126 | 15.0 |
| Friday | 127 | 15.1 |
| Saturday | 126 | 15.0 |
| Sunday | 123 | 14.6 |
| Total* | 841 | 100.0 |
1 missing.
FIGURE.
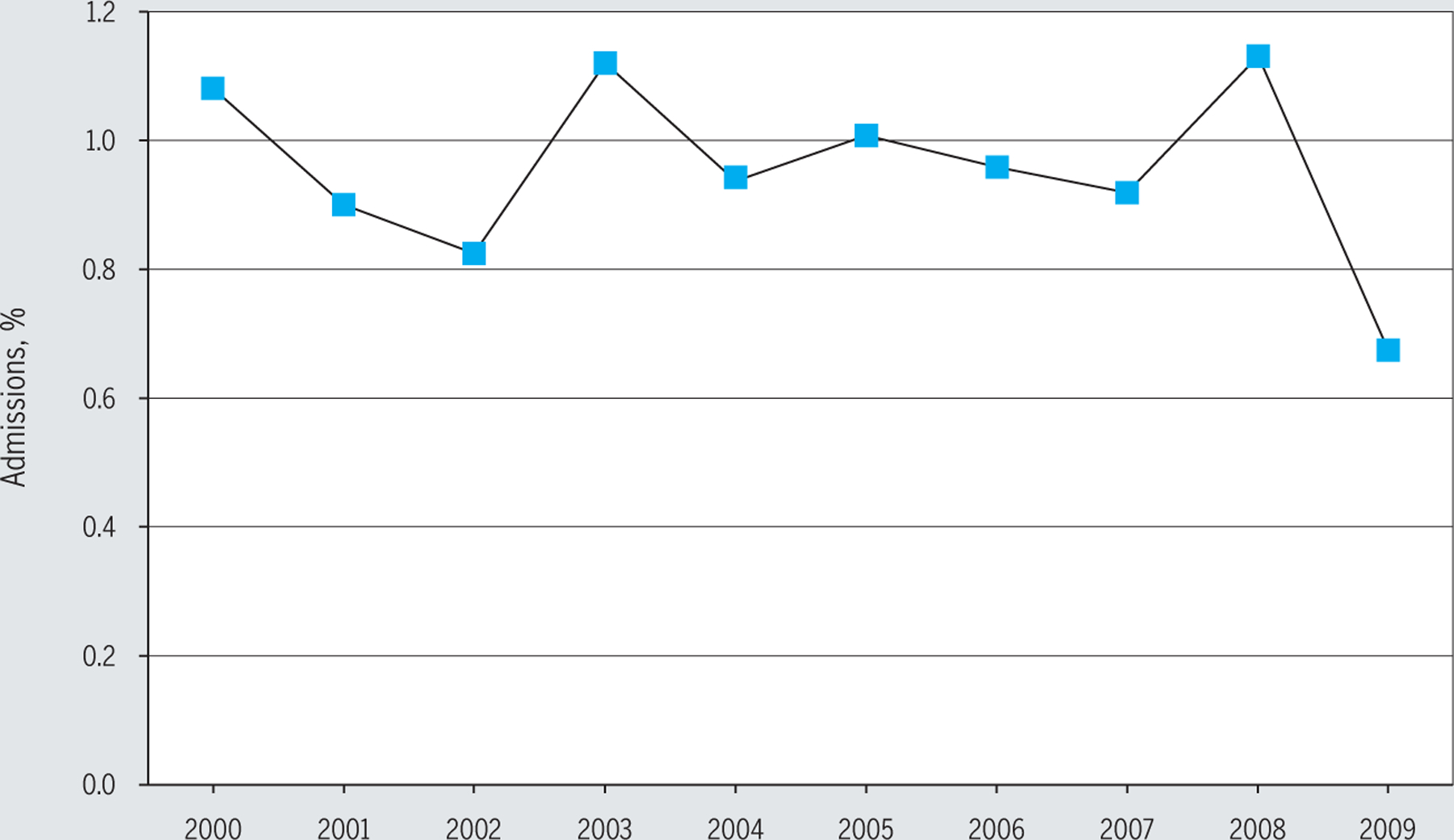
Rates of falls by percentage of admissions over a 10-year period.
Among patients who fell, 322 (38.2%) had a total knee replacement (TKR), including revisions or unicondylar procedures; 156 (18.5%) had a spine procedure; 124 (14.7%) had a total hip replacement (THR), including revisions or hip resurfacing procedures; 97 (11.5%) had a lower extremity procedure other than TKR or THR; 97 (11.5%) had other miscellaneous orthopaedic procedures; and 46 (5.5%) had an upper extremity procedure. Approximately 1.2% of all TKR patients fell, compared with approximately 0.47% of THR patients, over the 10-year period. Other procedure-specific rates could not be calculated. Twenty-six falls (3%) were second or third falls in the same patient during the same admission.
Of the 842 first falls during an admission, 386 (45.8%) involved using the bathroom (going to, entering, or leaving) and 145 (17.2%) occurred in patients with a known history of previous falls. One hundred seventy-six (20.9%) first falls were observed, and in 165 (19.6%) falls the patient was assisted to the ground by someone else in the room. Six hundred nineteen (73.5%) falls occurred in patients who were using some type of assistive device at the time of the fall. Ninety-six (11.4%) were prescribed patient-controlled anesthesia during their admission, and 19 (2.3%) had a central line in place at the time of fall. Six hundred four (71.7%) patients had mental status documented, and of those, 122 (20.2%) were documented to be confused at the time of fall.
One hundred ten first falls (13.1%) resulted in injuries, most of which were minor soft tissue scrapes or contusions (TABLE 3). However, 28 (3.3%) first falls resulted in serious injuries or outcomes, including 5 returns to the operating room, 3 transfers to a higher level of care, 14 prosthesis dislocations, 6 fractures, 2 intracranial bleeds, and 1 hemorrhage (n>28, as some patients had more than 1 serious adverse event). There were no deaths. Neither first falls resulting in injury (n = 110) nor falls resulting in serious outcomes (n = 28) were significantly associated with day of the week or time of day. There was no significant association of serious falls with body mass index, age, gender, previous history of falling, having a central line, being prescribed patient-controlled anesthesia, or being noted at time of fall as being confused. Of the 26 falls that were second or third falls in the same patient during the same admission, 1 resulted in an epidural hematoma, the only serious injury in this group.
TABLE 3.
Adverse Events Sustained During a First Fall: 2000 to 2009
| Characteristic | n |
|---|---|
| Total number of falls among orthopaedic inpatients | 868 |
| Number of first falls during an admission | 842 |
| No adverse event | 732 |
| Minor adverse events (abrasions, cuts, ecchymoses, etc) | 82 |
| Falls resulting in serious adverse events | 28 |
| Type of serious adverse event* | |
| Returns to the operating room | 5 |
| Transfers to a higher level of care | 3 |
| Fractures | 6 |
| Prosthesis dislocation | 14 |
| Intracranial bleed | 2 |
| Hemorrhage | 1 |
n>28, as some falls had more than 1 adverse outcome.
Patients whose first fall resulted in a serious injury or outcome were more likely to fall earlier in their stay (mean postoperative days, 2.7 versus 4.1; mean difference, 1.4; 95% confidence interval: 0.51, 2.3; P = .003) and to have had a THR (P = .001).
In a regression analysis controlling for age, gender, and postoperative day, patients who had a THR had a statistically significant increased risk of having a fall with a serious outcome, compared with other procedures (odds ratio = 3.7; 95% confidence interval: 1.7, 8.2) (TABLE 4).
TABLE 4.
Results of Multivariable Regression Analysis
| β | P Value | Odds Ratio | 95% CI | |
|---|---|---|---|---|
| Age | .01 | .48 | 1.01 | 0.98, 1.04 |
| Gender | .19 | .63 | 1.21 | 0.56, 2.6 |
| Postoperative day | .02 | .68 | 1.02 | 0.95, 1.09 |
| THR | 1.3 | .001 | 3.72 | 1.68, 8.23 |
Abbreviations: CI, confidence interval; THR, total hip replacement.
DISCUSSION
Falls are a significant problem in hospitals and can result in severe injury or even death. However, most fall studies focus on the elderly, members of assisted-living communities, or sick hospitalized inpatients. Elective orthopaedic inpatients represent an understudied demographic that is worthy of further consideration. Patients who have elective orthopaedic procedures are unique, as they are, by definition, healthy enough for a major surgical procedure, unlike many frail elderly or hospitalized medical patients. In addition, these procedures are common. In 2008, approximately 668 333 TKRs and 425 700 THRs were performed in the United States.9 By applying our fall rates, we estimated that over 10 000 postoperative falls occurred that year in this patient subset alone. With the projected increase in elective orthopaedic procedures, it will become increasingly important to understand and prevent falls in this patient population to minimize both clinical injury and downstream costs.
This study of 868 falls over a 10-year period is by far the largest study of falls among orthopaedic inpatients to date. To our knowledge, there is only 1 published report evaluating falls among orthopaedic inpatients, which was a small retrospective study of 70 falls over a 2-year period.1 Interestingly, our study found very similar fall rates: 0.9% versus 1% of admissions, and 2.0 versus 2.5 falls per 1000 inpatient days. Because our patients were “medically cleared” prior to surgery and did not include patients referred from an emergency room setting, we anticipated a lower rate of falls in this sample compared with a general hospitalized population. Although our rate of 2.0 falls per 1000 inpatient days is on the low end of published estimates, it is still within the reported range of 0 to 10.7 per 1000 patient days in other general acute hospitals and retirement and long-term facility settings.2,10,13,15,16
Fortunately, the risk of serious injuries resulting from falls in this patient population was very low (3.3%), which is reassuring for patients undergoing elective orthopaedic procedures. However, patients whose fall resulted in a serious outcome were more likely to fall earlier in their stay (mean postoperative days, 2.7 versus 4.1; P = .003). In addition, among patients who fell, having had a THR increased the risk of having a serious adverse event almost 4-fold.
Almost a fifth of falls occurred in patients known to have had a previous fall. These patients may benefit from more intensive precautions both presurgery and postsurgery. By contrast, multiple falls during an admission were uncommon, accounting for only 3% of all falls, with only 1 serious outcome in this group. Inconsistent definitions make it challenging to compare overall rates of serious adverse events between studies. However, our rate of fracture (0.7%) appears much lower than that reported among other orthopaedic inpatients (3%),1 hospitalized inpatients (3.6%),5 or the hospitalized elderly (3%).7 This may reflect the underlying health of our cohort, which was primarily a population of those who had elective surgeries.
Almost half of first falls in our cohort involved using the bathroom, which is a well-described, high-risk activity. Others have reported that up to 64% of all falls in orthopaedic inpatients are elimination-related.1 Convincing adults to ask for assistance when using the toilet is clearly a challenge that has not been successfully addressed. Better education is needed to warn patients of the fall risk associated with activities like toileting. In addition, 20.1% of first falls were observed, and in 19.6% the patient was assisted to the ground. In this subset of fallers, the presence of another person in the room—even someone close enough to intervene during the fall—was not protective against falling. This suggests that fall interventions could involve trained bystanders to remind patients to ask for appropriate assistance. Of those with mental status documented, 20.2% were noted by nursing to be confused at the time of fall, similar to the 26% reported among other orthopaedic inpatients.1 It would have also been informative to know what proportion of patients who fell while using an assistive device also used an assistive device at home, though this information was not available.
Unfortunately, medication use was not consistently recorded over the study period, so we cannot comment on the pharmacologic impact of medication on mental status. However, although medication use has been associated with falls among community-dwelling and assisted-living elders,4,6 the associations among confusion, medication use, and falls in hospitalized patients remain unclear.5 As medication may be one of the few potentially modifiable risk factors, it is important that future prospective fall studies rigorously evaluate this factor.
The strengths of this study include a very large sample size from a single center, which provided the power to look at risk factors for rare but potentially devastating adverse events. Studies of falls among orthopaedic inpatients should also be performed in smaller centers. Although it is well known that functional outcomes of orthopaedic surgery are positively correlated with hospital volume, it is not known if hospital volume impacts fall rates or outcomes.11 In addition, because fall-specific data were collected within 24 hours of the fall, this study avoids the biases inherent in retrospective chart reviews. The study also had excellent case ascertainment. Our complementary case-finding strategy found only 20 cases that were missed over the entire 10-year study period, so it is extremely unlikely that there may have been hidden or systematic bias due to missing falls.
Limitations of the current study include the lack of a control group, which would have allowed us to better understand differences between patients who fell and those who did not. Because this was a retrospective study, only associations, not causal relationships, could be inferred from the findings. Although we were able to calculate an overall fall rate and procedure-specific fall rates for hip and knee replacements, we were unable to calculate fall rates for other types of procedures. In addition, although physical therapy protocols were standardized, we could not link specific protocols with individual patients or accurately account for any changes in physical therapy regimens over time. Also, we could not link pharmacy data with falls, which would have been particularly important in patients noted to be confused. We did know when patient-controlled anesthesia had been prescribed but not when it was used, and we had no data on comorbidities or type of surgical anesthesia.
CONCLUSION
Falls are avoidable events. although the risk of serious adverse events was relatively low in our cohort, these unexpected complications are particularly problematic when they occur in healthy patients having elective surgery. This large series identifies THR patients as being at almost 4-fold risk of having a serious adverse event secondary to a fall, which to our knowledge has not previously been reported. Larger prospective studies are needed to confirm these results and to inform fall-prevention strategies in this important and rapidly growing group of orthopaedic patients.
TABLE 2.
Orthopaedic Inpatient Falls (n = 842)*
| Characteristic | Values |
|---|---|
| Mean age, y (range) | 68 (18–93) |
| Female, n (%) | 485 (57.6) |
| Mean BMI, kg/m2 (range)† | 28.7 (15.6–54.1) |
| Mean postoperative days (range) | 4.1 (0–56) |
| Time of fall by quartiles‡ | |
| First quartile | 12:01 am to 5 am |
| Second quartile | 5:01 am to 11 am |
| Third quartile | 11:01 am to 5:30 pm |
| Fourth quartile | 5:31 pm to midnight |
| Past history of falls, n (%) | 145 (17.2) |
| Fall occurred using the bathroom, n (%) | 386 (45.8) |
| Patient assisted to the ground by someone in the room, n (%) | 165 (19.6) |
| Using some type of assistive device at the time of fall, n (%) | 619 (73.5) |
| Prescribed patient-controlled anesthesia, n (%) | 96 (11.4) |
| Central line in place at time of fall, n (%) | 19 (2.3) |
| Confused at time of fall, n (%) | 122 (20.2 of those with documented mental status) |
Abbreviation: BMI, body mass index.
Includes first fall of each admission.
Available on 520 patients.
Each quartile represents approximately 210 falls.
KEY POINTS.
FINDINGS:
Patients whose fall resulted in a serious outcome were more likely to fall earlier in their stay, and THR patients had an almost 4-fold risk of having a serious adverse event secondary to a fall. Almost half of all falls involved using the bathroom.
IMPLICATIONS:
All patients should be monitored carefully, especially during high-risk activities such as toileting.
CAUTION:
A control group would allow us to better understand differences between patients who fell and those who did not.
ACKNOWLEDGEMENTS:
Thanks to Nonie Pegoraro and the Hospital for Special Surgery Quality Research Center for their assistance with data management.
REFERENCES
- 1.Ackerman DB, Trousdale RT, Bieber P, Henely J, Pagnano MW, Berry DJ. Postoperative patient falls on an orthopedic inpatient unit. J Arthroplasty 2010;25:10–14. 10.1016/j.arth.2008.09.025 [DOI] [PubMed] [Google Scholar]
- 2.Aizen E, Shugaev I, Lenger R. Risk factors and characteristics of falls during inpatient rehabilitation of elderly patients. Arch Gerontol Geriatr 2007;44:1–12. 10.1016/j.archger.2006.01.005 [DOI] [PubMed] [Google Scholar]
- 3.Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med 1995;99:137–143. [DOI] [PubMed] [Google Scholar]
- 4.Blake AJ, Morgan K, Bendall MJ, et al. Falls by elderly people at home: prevalence and associated factors. Age Ageing 1988;17:365–372. [DOI] [PubMed] [Google Scholar]
- 5.de Vries OJ, Peeters GM, Elders PJ, et al. Multifactorial intervention to reduce falls in older people at high risk of recurrent falls: a randomized controlled trial. Arch Intern Med 2010;170:1110–1117. 10.1001/archinternmed.2010.169 [DOI] [PubMed] [Google Scholar]
- 6.Granek E, Baker SP, Abbey H, et al. Medications and diagnoses in relation to falls in a long-term care facility. J Am Geriatr Soc 1987;35:503–511. [DOI] [PubMed] [Google Scholar]
- 7.Haines TP, Hill AM, Hill KD, et al. Patient education to prevent falls among older hospital inpatients: a randomized controlled trial. Arch Intern Med 2011;171:516–524. 10.1001/archinternmed.2010.444 [DOI] [PubMed] [Google Scholar]
- 8.Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients: a predictive model based on routinely available data. J Clin Epidemiol 2001;54:1258–1266. [DOI] [PubMed] [Google Scholar]
- 9.Healthcare Cost and Utilization Project databases Available at: http://www.hcup-us.ahrq.gov/databases.jsp. Accessed December 11, 2012.
- 10.Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med 2004;19:732–739. 10.1111/j.1525-1497.2004.30387.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katz JN, Phillips CB, Baron JA, et al. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum 2003;48:560–568. 10.1002/art.10754 [DOI] [PubMed] [Google Scholar]
- 12.Krauss MJ, Evanoff B, Hitcho E, et al. A case-control study of patient, medication, and care-related risk factors for inpatient falls. J Gen Intern Med 2005;20:116–122. 10.1111/j.1525-1497.2005.40171.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lane AJ. Evaluation of the fall prevention program in an acute care setting. Orthop Nurs 1999;18:37–43. [PubMed] [Google Scholar]
- 14.Morgan VR, Mathison JH, Rice JC, Clemmer DI. Hospital falls: a persistent problem. Am J Public Health 1985;75:775–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Poe SS, Cvach MM, Gartrelu DG, Radzik BR, Joy TL. An evidence-based approach to fall risk assessment, prevention, and management: lessons learned. J Nurs Care Qual 2005;20:107–116; quiz 117–118. [DOI] [PubMed] [Google Scholar]
- 16.Schwendimann R, Bühler H, De Geest S, Milisen K. Characteristics of hospital inpatient falls across clinical departments. Gerontology 2008;54:342–348. 10.1159/000129954 [DOI] [PubMed] [Google Scholar]
- 17.Stel VS, Smit JH, Pluijm SM, Lips P. Balance and mobility performance as treatable risk factors for recurrent falling in older persons. J Clin Epidemiol 2003;56:659–668. [DOI] [PubMed] [Google Scholar]
- 18.Vassallo M, Vignaraja R, Sharma JC, Briggs R, Allen S. The relationship of falls to injury among hospital in-patients. Int J Clin Pract 2005;59:17–20. 10.1111/j.1742-1241.2004.00265.x [DOI] [PubMed] [Google Scholar]
- 19.Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing 1997;26:189–193. [DOI] [PubMed] [Google Scholar]


