Abstract
The Lancet Commission on Diagnostics highlighted a huge gap in access to diagnostic testing even for basic tests, particularly at the primary care level, and emphasised the need for countries to include diagnostics as part of their universal health coverage benefits packages. Despite the poor state of diagnostic-related services in low-income and middle-income countries (LMICs), little is known about the extent to which diagnostics are included in the health benefit packages. We conducted an analysis of seven Asian LMICs—Cambodia, India, Indonesia, Nepal, Pakistan, Philippines, Viet Nam—to understand this issue. We conducted a targeted review of relevant literature and applied a health financing framework to analyse the benefit packages available in each government-sponsored scheme. We found considerable heterogeneity in country approaches to diagnostics. Of the seven countries, only India has developed a national essential diagnostics list. No country presented a clear policy rationale on the inclusion of diagnostics in their scheme and the level of detail on the specific diagnostics which are covered under the schemes was also generally lacking. Government-sponsored insurance expansion in the eligible populations has reduced the out-of-pocket health payment burden in many of the countries but overall, there is a lack of access, availability and affordability for diagnostic-related services.
Keywords: diagnostics and tools, health insurance, health policy
What is already known on this topic
Lack of access, availability and affordability for diagnostic-related services in low-income and middle-income countries (LMIC) is widely known. The Lancet Commission on Diagnostics estimated that nearly half of the world’s population has very little access to diagnostics, with lack of access particularly acute in primary care.
What this study adds
Our study is the first to examine whether government-sponsored health benefit schemes include diagnostic-related services in seven Asian LMICs: Cambodia, India, Indonesia, Nepal, Pakistan, Philippines and Viet Nam. We show that none of the countries present a clear policy rationale or detailed information about which diagnostic-related services are covered. Only India has developed a national essential diagnostics list (NEDL).
How this study might affect research, practice or policy
We demonstrate ways in which countries can prioritise diagnostics in their health benefit packages, align with NEDLs and embed diagnostics for all as part of Universal Health Coverage. We make several recommendations:
Government health benefit schemes should include diagnostics, drawing on appropriate population health information such as disease burden
Data should be collected about diagnostic usage, including on diagnostics provided through vertical programmes
Schemes should invest in knowledge and educational information to encourage population enrolment
Financing of diagnostics requires linkages to both public and private providers. Financial integration of vertical programmes, cross-subsidisation and setting reimbursement case rates for diagnostics could help to mitigate the high out-of-pocket payments patients currently face in these settings
Introduction
The Lancet Commission on diagnostics provided compelling evidence that scarcity of diagnostic capacity and capability remains a challenge in low-income and middle-income countries (LMICs).1 The Commission estimated that nearly half of the world’s population has little to no access to diagnostics and highlighted the gap in access to diagnostic testing even for basic tests, particularly at the primary care level. It also emphasised the need for countries to include diagnostics as part of their journey towards universal health coverage (UHC). Another key finding was that public financing plays an important role in improving access: government-sponsored health insurance schemes are a key financing mechanism for UHC.2 A major recommendation of the Commission was that all countries develop their national diagnostics strategy, based on an integrated and tiered network, including an evidence-based national essential diagnostics list (NEDL), with a prioritised subset for UHC.
Health financing schemes are the main building blocks of the functional structure of a country’s health financing system through which health services are paid for and through which people can access healthcare.2 3 This paper follows the System of Health Accounts classification of healthcare financing schemes.3 These include government financing arrangements, compulsory health insurance and voluntary financing arrangements, as shown in table 1.
Table 1.
Features of healthcare financing schemes3
| Government financing | Compulsory health insurance schemes (predominantly social health insurance) | Voluntary financing |
|
|
|
All schemes may not necessarily cover the total price of the included services and involve cost sharing through copayments, or caps on financial protection requiring out-of-pocket (OOP) payments. The ways in which health financing can support the inclusion of diagnostics in country government-sponsored health insurance schemes was not fully explored in the Lancet Commission on diagnostics.
In this paper, we build on the Commission’s analysis and fill this knowledge gap by investigating the extent to which diagnostics are included in government health insurance schemes in seven LMICs in Asia—Cambodia, India, Indonesia, Nepal, Pakistan, Philippines and Viet Nam. We selected these countries because we wanted to understand varied approaches to the design of government-sponsored health insurance schemes in countries which have highly privatised health systems, and to include schemes with a range of maturity and population coverage. All seven countries have embarked on UHC agendas, and progress towards UHC is tracked as Sustainable Development Goal 3.8. In heavily privatised systems, the inclusion of diagnostics in government insurance schemes would help to reduce the OOP payments associated with testing. Collectively, the population of these seven countries is approximately 2.15 billion people, almost a quarter of the world’s population, making the design and performance of these schemes of substantial global health importance.4
All seven countries are undergoing a health financing transition; this concept refers to a transition from a stage where total health spending was low and primarily OOP, to later stages where government health spending is higher and a higher proportion of funds are primarily pooled to purchase healthcare services.2 5 Pooling allows financial risk to be spread across the population, so no individual carries all the financial burden to pay for healthcare costs. In higher-income countries, where a higher proportion of funds are primary pooled, diagnostics are included in the benefit basket of government-sponsored schemes; for example, in Australia laboratory services account for 3% of total health expenditure6 compared with 10% in India.7
Our work had four objectives:
To examine the benefit package of the government health insurance scheme for seven LMICs in Asia with substantial private sector involvement in healthcare.
To ascertain the population coverage of each government health insurance scheme.
To examine the mechanisms adopted to include diagnostics in each government health insurance scheme.
To identify ways to improve the benefit packages of the government health insurance schemes to support UHC.
In the paper, we defined diagnostics as pathology and laboratory medicine (PALM) and diagnostic imaging (DI) including at the point of care.1 A health financing template developed for this study supported information gathering; government sponsored schemes refer to both government financing and compulsory health insurance (online supplemental appendix 1). The search looked at the following aspects: scheme development, policy rationale, population coverage, financial coverage including copayments, caps and premiums, diagnostics included in the scheme, purchasing arrangements, performance of the scheme, access to diagnostics and alignment with vertical programmes.
bmjgh-2023-012512supp001.pdf (326.2KB, pdf)
We conducted a targeted literature review in seven countries: Cambodia, India, Indonesia, Nepal, Pakistan, Philippines and Viet Nam. The following databases were searched from 2012 to 2022 for literature relating to each country’s health insurance scheme: PubMed, CINHAL, EBSCO. The search included PALM, DI, benefit package, health insurance, UHC coverage, health financing, health system (online supplemental appendix 1). Government and health ministry websites were searched for documents relating to government-sponsored health insurance schemes published in English. The websites of the following additional organisations were searched for relevant data on each of the seven countries: WHO, Partners for Health, Results for Development, World Bank, Institute for Health Metrics and Evaluation, Overseas Development Institute and Center for Global Development. Country coauthors supported the identification of relevant publications, including those not readily available in English.
The Lancet Commission on diagnostics used access to tests for diabetes, hypertension, HIV, tuberculosis (TB), hepatitis B in pregnant women and syphilis in pregnant women as a measure of diagnostic availability in an outpatient setting.1 We mapped these six priority conditions onto the country schemes to determine their inclusion in the benefit basket. Where schemes included treatment for a given disease but did not specify relevant diagnostics (eg, TB), we assumed the diagnostics were included.
Health financing overview
Government sponsored health insurance schemes are in place in all seven countries but are at differing stages of development. The schemes in the Philippines and Viet Nam began in the 1990s, those in Cambodia and India in the 2000s and those in Indonesia, Nepal and Pakistan in the 2010s. All schemes are backed by legislation outlining the design of the benefit scheme service packages and eligibility requirements for coverage. The country’s entire population is eligible in Nepal, Philippines and Viet Nam, although registration rates vary from 21% in Nepal8 to 92% in Viet Nam.9 The remaining countries have hybrid systems, with insurance schemes in place for lower-income groups or those living in certain areas. The scheme in Cambodia is available to households identified as poor (24%),10 in India to households identified as poor or vulnerable (approximately 40%, with registration ongoing)11 and in Pakistan to all permanent residents of provinces and territories participating in the scheme.12 A summary of the key features of the financing of the schemes in each country is given in table 2 with country-specific details provided in online supplemental appendices 2 and 3.
Table 2.
Key features of government-sponsored health insurance schemes and financing for diagnostics in seven LMICs in Asia
| Country | Scheme name and year of establishment | Eligible population | Eligible population coverage (% eligible population) | Scheme design and coverage | Copayments, premiums and caps | Purchasing arrangements |
| Cambodia | Health Equity Fund (HEF) (2000) | Individuals identified in the IDPoor registry and certain categories of informal workers, exclusion for people who inject drugs | 24% (2020) | Preventive or curative care (outpatient, inpatient or in emergencies). Transportation costs to referral hospitals and funeral expenses for inpatient deaths are included with no cost ceiling | No copayments, premiums or caps. OOP payment | Diagnostics and laboratory testing are implicitly included in the service packages. Reimbursement is based on the number of service packages provided to HEF beneficiaries and deductions are made for any penalties associated with the submission of false claims or incomplete documentation |
| India | Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (2018) | Households identified as poor or vulnerable (~40%) | 32% (2021), 164 million e-cards issued | Cashless unremarkable scheme covering secondary and tertiary hospitalisation at public and private empanelled hospitals up to a cost ceiling | Cap of INR500 000 (US$6074) per family per year, then OOP payment. No copayments or premiums | 53% of participating hospitals are public, with the remainder private. States can either purchase services through an insurance company, purchase directly by the state-owned agency or a mixture of both |
| Indonesia | Jaminan Kesehatan Nasional (2014, on consolidation of previous schemes) | Country population, with some exclusions | 83% (2019) | Primary care, inpatient and outpatient care included with no cost ceiling | Those formally working are registered by their employers while informal workers must enrol themselves and pay a monthly premium. No copayments or caps | The scheme contracts with all public and most private providers, including private hospitals, private clinics and individual private physicians |
| Nepal | Health Insurance Board (2016) | Country population (100%) | 20% (2022) | Outpatient, inpatient and emergency care included up to a cost ceiling | Family premium of NPR3500 (US$28) per year with subsidies for certain groups. Cap of NPR100 000 (US$806) per family per year but can be higher for certain groups, then OOP payment | Private laboratories are not yet integrated into the scheme, but private medical colleges, private nursing homes, and community-based healthcare facilities are |
| Pakistan | Sehat Sahulat Programme from 2018 (regional schemes between 2014 and 2018) | Full population in most provinces and territories | 89% (2022) | Cashless unremarkable scheme covering inpatient and emergency, but not outpatient. Health services in empanelled hospitals up to a cost ceiling | No copayments or premiums. Cap of Rs1 000 000 (US$3840) per family per year for priority diseases with an extra Rs60 000 (US$277) for secondary diseases, then OOP payment | The scheme contracts directly with empanelled hospitals (public or private) |
| Philippines | Philippine Health Insurance Corporation (PhilHealth) (1995) | Country population (100%) | 86% (2021) | Benefit packages (primary care, outpatient, and inpatient) in accredited or contracted public or private facilities up to a cost ceiling | Premium of 4% of monthly salary up to a maximum of PHP 3200 (US$61) for formal employees. Means-tested premium subsidies for those informally employed. Copayment required for non-basic hospital accommodation but not for basic or ward accommodation. Cap of PHP 32 000 (US$600), then OOP payment | Health facilities can put in place a memorandum of understanding with other health facilities to provide diagnostic services when not available in their own facility |
| Viet Nam | Social Health Insurance (1992) | Country population (100%) | 92% (2022) | Inpatient and outpatient hospital care in public and government-approved private facilities and other health facilities, as well as transportation services in poor and mountainous areas, included up to a cost ceiling | Premium of 4.5% of basic monthly salary with subsidies for certain groups. Copayments at 20% except for fully subsidised groups. Copayment ceiling equivalent to 6 months’ basic salary for those with 5 years of continuous membership. Cap in place for high cost technical services | Contracting in place with both public and private providers, though public sector predominates. Unregistered facilities can be reimbursed if a reference letter from a registered facility is provided before patient transfer |
Note: all dollar amounts are in US dollars.
LMICs, low-income and middle-income countries; OOP, out of pocket.
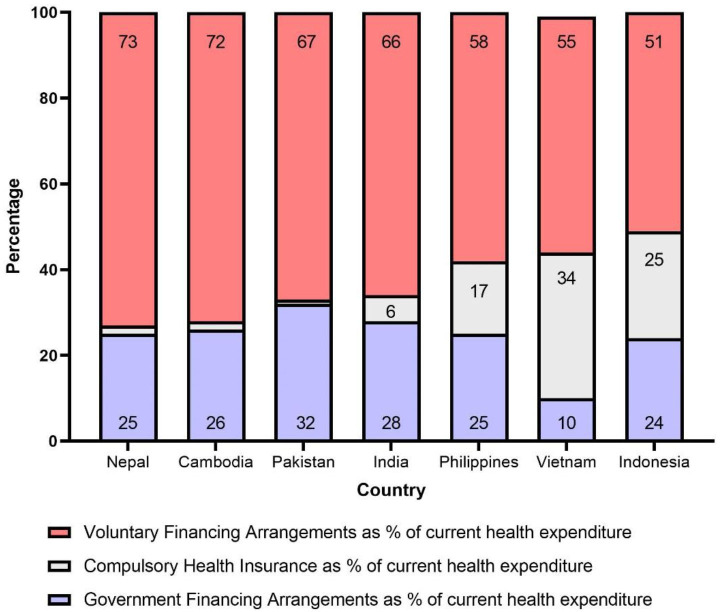
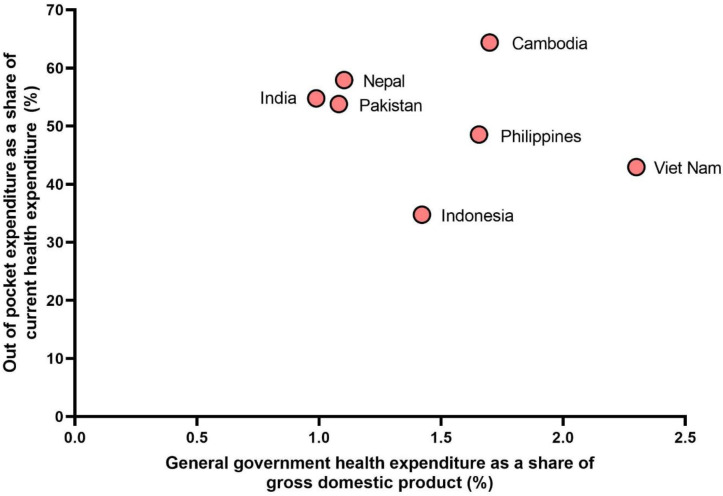
All seven countries have highly privatised healthcare systems: government financing and compulsory health insurance together ranged from 27% in Nepal to 49% in Indonesia in 2019 (figure 1). OOP payments as a share of current health expenditure (CHE) ranged from 35% in Indonesia to 64% in Cambodia while government health expenditure as a share of gross domestic product (GDP) ranged from 0.9% in India to 2.3% in Vietnam in 2019 (figure 2). Figure 2 illustrates that the seven countries are at different stages of how they finance their healthcare system, from earlier stages where health spending is primarily OOP (eg, India), to later stages where health spending is higher and primarily pooled (eg, Viet Nam). The financing and delivery of vertical programmes often rely on external partners, ranging from 0.4% in the Philippines of CHE to 11.9% in Nepal (online supplemental appendix 3).
Figure 1.
Sources of health financing schemes by country. Data from Global Health Expenditure Database (2019).
Figure 2.
Out of pocket expenditure as a share of current health expenditure and general government health expenditure as a share of gross domestic product by country. Data from Global Health Expenditure Database (2019).
Scheme designs and financial coverage
The most recent published information on the benefit packages varied by country: Cambodia (2018), Nepal (2017), India (2019), Indonesia (2017), Pakistan (2021), Philippines (2020) and Viet Nam (2016). The seven schemes are organised differently with respect to the services included in the benefit basket, premiums, copayments and caps on usage. Cambodia13 and Nepal14 cover inpatient, outpatient and emergency care, and Cambodia additionally covers transportation costs and funeral expenses. India covers secondary and tertiary hospitalisation.11 Indonesia15 16 and the Philippines cover primary care, inpatient and outpatient care.17 Pakistan covers inpatient and emergency, but not outpatient care.12 18 Viet Nam covers inpatient and outpatient care.19–21
Most of the schemes are organised into benefit packages covering the treatment and management of different groups of conditions. Some schemes, such as those in Nepal22 23 and Pakistan,24 strictly cover only specifically listed conditions whereas others, such as the scheme in the Philippines, have broader packages such as ‘General Out-Patient Consultation’.25 Cambodia13 and Indonesia26 have no caps on usage. India has a cap of INR500 000 (US$6074) per family per year,11 Nepal has a cap of NPR100 000 (US$806) per family per year, with extra allowances for certain population groups,14 27 Pakistan has a cap of Rs1 000 000 (US$3840) per family per year, with an extra allowance to cover certain diseases,24 Philippines has a cap of PHP32 000 (US$600),28 and Viet Nam has a cap for each episode equivalent to the country minimum salary over 40 months.19 Beyond the caps, payment is OOP.
Cambodia, India and Pakistan do not require the payment of premiums by the beneficiaries. In Indonesia, informal workers must enrol themselves and pay a monthly premium while formal workers are registered by their employers.15 In Nepal, a family of five must pay NPR3500 (US$28) per year, with an extra NPR700 (US$6) per additional family member, with subsidies for certain groups.27 In the Philippines, the premium is 4% of monthly salaries up to a cap28 29 while in Viet Nam it is 4.5% of basic monthly salary,19 20 and both countries have subsidies for certain groups.30 Viet Nam requires copayments, set at 20% of incurred costs except for subsidised groups including those with at least 5 years of participation and an annual total payment amount capped at 6 months of basic monthly salary.20
Provision of diagnostics in the schemes
Of the seven countries, only India has developed an NEDL31; it has guidelines on the use of diagnostics in the treatment packages in the scheme. However, it is unclear to what extent the Indian NEDL has informed the availability of diagnostics in their Free Diagnostics Service Initiative under the National Health Mission32 or the Pradhan Mantri Jan Arogya Yojana (PM-JAY) insurance scheme.11 Viet Nam is in the process of developing its NEDL but has not yet completed the project. In some countries, including Pakistan24 and the Philippines,33 34 the rationale for the inclusion of certain medical conditions in the scheme coverage is explicitly described based on conditions with substantial burdens or that are common causes of catastrophic health costs in the country. However, descriptions of the rationale behind the inclusion of the specific diagnostics within the schemes are generally poor or non-existent across countries.
The schemes cover diagnostics in all settings for which they cover care. All schemes, therefore, cover at least some inpatient diagnostics, but many also include diagnostics in primary care and outpatient hospital settings. India is the exception where diagnostics in primary care are not linked to the scheme and the availability of diagnostics for outpatient care is not made explicit. Descriptions of available diagnostics from most countries are vague and either list the medical conditions for which diagnostics are available without specifying the exact diagnostic type or brand or do not list the available diagnostics at all. Procedures or treatments listed in the schemes implicitly include diagnostics as seen in India, Indonesia, Pakistan and the Philippines. Nepal, specifies 125 laboratory tests and 77 radiological and other diagnostic services, though official documents do not distinguish the levels of the health system at which different diagnostics are available.35 Pakistan includes diagnostics for inpatient services but explicitly excludes admissions specifically for the purpose of diagnosis.
Purchasing and reimbursing providers for diagnostics
Legislative tools are in place in all the countries for purchasing, and to reimburse providers. In most countries, contracts include both public and private providers. In Nepal, private laboratories are not yet integrated into the scheme.14 In Indonesia, all public and most private providers are contracted.26 In the Philippines, an agreement can be put in place with another health facility to provide diagnostics when not available in the facility in question. India is moving towards putting in place a hub and spoke model for accessing diagnostics.
In Viet Nam, unregistered providers can be reimbursed if a reference letter from a registered facility is provided before patient transfer.36
Availability of Lancet Commission tracer conditions
To examine the state of diagnostics access globally, the Lancet Commission identified six priority conditions: diabetes, hypertension, HIV, TB, hepatitis B in pregnant women and syphilis in pregnant women.1
The seven countries did not all explicitly include diagnostics for these priority conditions in their government schemes (table 3). In Cambodia, diabetes, HIV and TB, syphilis are included, though it is unclear if they are provided to pregnant women; hypertension and hepatitis B for pregnant women were not specified.13 In India, diabetes, hypertension, HIV, TB, hepatitis B are included for inpatients, but syphilis is not mentioned. In Nepal, diabetes and hypertension are included; those for hepatitis B and syphilis are also included, though it is unclear if they are provided to pregnant women; HIV and TB are provided through vertical programmes outside the scheme.35 In Pakistan only complications requiring admission are included, but these include diagnostics for diabetes, hypertension, HIV, TB and hepatitis B. Most diagnostic provision in Pakistan is supported by donors such as the Global Fund to Fight AIDS, Tuberculosis and Malaria. Sexually transmitted diseases (STDs) are generally excluded including syphilis.24 In the Philippines, diabetes, hypertension, HIV and TB are included. Hepatitis B and syphilis are also included, though it is unclear if they are provided to pregnant women. In Viet Nam, diabetes, hypertension, hepatitis B and syphilis are included for all, including pregnant women. HIV and TB are provided through vertical programmes. There are no details about the tracer conditions in the benefit package for Indonesia.
Table 3.
Key features of the inclusion of diagnostics in government-sponsored health insurance schemes in seven LMICs in Asia
| Country | NEDL in place | Does the scheme explicitly include diagnostics? | Lancet Commission tracer conditions | ||
| Cambodia | No | Yes | Primary care and hospital settings not specified | Yes | Diabetes, HIV and TB; those for syphilis are also included, though it is unclear if they are provided to pregnant women. Hypertension and hepatitis B for pregnant women not specified but may be included in general service packages covering investigations as indicated by consultation |
| India | Yes | Yes | Yes for inpatient care | Yes | Diabetes, hypertension, HIV, TB; hepatitis B included. Syphilis is not mentioned |
| Indonesia | No | Yes | Yes for primary, outpatient and inpatient care | No | No details |
| Nepal | No | Yes | Not specified in which settings diagnostics are available | Yes | Diabetes and hypertension are included; those for hepatitis B and syphilis are also included, though it is unclear if they are provided to pregnant women. HIV and TB are provided through vertical programmes |
| Pakistan | No | Yes | Yes for inpatient care (admission for diagnostics excluded) | Yes | Complications requiring admission includes diagnostics for diabetes hypertension, HIV, TB and hepatitis B. HIV is included, (STDs) are generally excluded including syphilis |
| Philippines | No | Yes | Yes for primary, outpatient and inpatient care | Yes | Diabetes, hypertension, HIV and TB are included. Hepatitis B and syphilis are also included, though it is unclear if they are provided to pregnant women |
| Viet Nam | No | Yes | Early diagnosis for some diseases and prenatal tests specified in primary, outpatient and inpatient care | Yes | Diabetes, hypertension, hepatitis B and syphilis are included for all, including pregnant women. HIV and TB are provided through vertical programmes |
HIV, human immunodeficiency virus; LMICs, low-income and middle-income countries; NEDL, national essential diagnostics list; STDs, sexually transmitted diseases; TB, tuberculosis.
Vertical alignment
In Nepal, the vertical programme of TB is integrated into the government sponsored health insurance scheme with similar plans for TB in Viet Nam.37 In Nepal and Viet Nam, HIV testing are provided through vertical programmes integrated into the government sponsored health insurance schemes. It remains unclear the extent to which vertical alignment of programmes are working in practice with government sponsored health insurance schemes in the remaining six countries. In India, there are national programmes (eg, for cancer and dialysis) but it is unclear if these programmes are aligned with the PM-JAY.
Scheme performance
Despite the range of caps from US$600 in the Philippines to US$6074 in India (table 2), the evidence on the performance of the schemes with respect to accessing diagnostics is mixed. Philippines is the only country to publicly share data on diagnostics claims, which accounted for 2% of total claims in 2021, but this may not reflect all diagnostic activity, some of which could be included under other claim categories. Despite efforts to expand insurance coverage in many of the countries, more work is needed—for example, Nepal faces challenges to prevent enrolled families from dropping out of the scheme.27 38 Changes to OOP expenditure with the introduction of these schemes is mixed. Indonesia experienced a drop in the overall share of OOP payments, but its progressivity has declined, suggesting that the poorest citizens are not making full use of the financial protection provided by the scheme.26 39 Cambodia’s scheme is pro-poor with the lower-income individuals paying less and receiving more PHC spending than higher-income individuals.40 41 India42 and Viet Nam43 44 still have high levels of OOP payment. In India, this may involve paying upfront while waiting for reimbursement, or patients visiting a private hospital where they are required to pay for the packages not covered. Covid-related testing and hospitalisation show large differences between public and private sector facilities in India. Patients forego tests because of high OOP payments in the private sector or are forced to seek care in the private sector due to poor availability and access in the public sector.45 In Pakistan, impoverishment increased despite the introduction of the scheme, with questions around the financial sustainability of the scheme due to current economic conditions and fiscal tightening.46–48 Earlier iterations of the scheme only covered those in extreme poverty meaning that those living in poverty were not eligible. Furthermore, not all hospitals are empanelled in the scheme, restricting provision of available services.
Taken together with the availability of diagnostics using the Lancet Commission tracer conditions, distribution and availability of diagnostics remains a challenge in all seven countries, reflecting a global trend reported in the Lancet Commission.1
Conclusion
In conclusion, there is considerable heterogeneity in the country approaches to diagnostics in the government-sponsored health insurance schemes. The level of detail on the availability of diagnostics in the benefit packages varies, including for the six Lancet tracer conditions. A clear policy rationale on which diagnostics are included or not included is absent from all schemes. Insurance expansion across the countries has mitigated some of the OOP burden, but the overall lack of access, availability and affordability for diagnostics-related services remains a problem.
Our analysis has several limitations. Our study only included Asian countries with a focus on seven countries, to capture differences in scheme development within highly privatised health systems. Our targeted review focused on the most relevant evidence and was not systematic in design. Furthermore, the analysis is based on available information on the benefit packages to date and will not have captured current changes underway and so we are unable to verify the published information in the field, although we did seek input from experts from most of the countries and include them as coauthors. The referenced publications were predominantly in English and so is not exhaustive of publications in each country’s native language.
The focus of this work was on diagnostic inclusion in the benefits package. It did not study links to other benefit schemes (eg, social benefits) that may be accessible to eligible populations and their direct or indirect contribution towards health financing, or other large schemes in operation (eg, the Employees' State Insurance scheme in India). We did not examine links to payment systems and incentives, including bundling and contractual arrangements. The intersection between insurance, diagnostics and how payment systems function is an important policy area worthy of future work but was outside the scope of this analysis.
Based on our findings, we set out the following recommendations. First, all government-funded health insurance schemes should explicitly include diagnostics and specify the range of available diagnostics in different settings, with that range determined by the disease profile in each country. Second, since only one of seven countries has developed a national essential diagnostics list, the development of NEDLs in all countries will bring greater attention to diagnostics and promote their inclusion and alignment with government-sponsored insurance schemes. Third, data should be collected and published on the use of diagnostics in government-sponsored schemes, including by regularly identifying high cost, high burden diseases which require specific diagnostics. Fourth, data should also be collected on the use of diagnostics provided through vertical programmes outside the government-sponsored schemes (including those accessible through the private sector). Fifth, systematic data collection on health financing for diagnostics is necessary in each country including pricing, reimbursement and purchasing arrangements. Sixth, there are knowledge gaps in the uptake of the schemes among the eligible populations, which would require a range of stakeholders working together to support and improve its uptake. Seventh, supportive financing policies should be better aligned with the inclusion of diagnostics around domestic resource mobilisation and innovative financing. The financing of diagnostics requires linkages to the wider health system between public and private providers including how to support diagnostics found in vertical delivery programmes that sit outside the government sponsored schemes. This could include financial integration of vertical programmes, cross-subsidisation and setting reimbursement case rates for diagnostics as part of these services. Finally, a country’s UHC strategy should draw on its own NEDL, reflected in the benefit package, that contains clear criteria such as clinical guidelines and cost-effectiveness analyses.
Our study identifies broader policy implications in taking a diagnostics-wide lens across a package of care that could be valuable to countries (eg, standardisation of care, contract negotiations) to improve consistency in care, equity and efficiency in health systems. The provision of diagnostics is vital for successfully introducing UHC. The UHC Compendium49 and the Global Atlas of Medical Devices50 aim to inform investment decisions around the benefits packages by drawing on the EDL. Internationally, the WHO Executive Board decided to recommend a resolution on strengthening diagnostic capacity at the 76th World Health Assembly.51 UHC offers the opportunity to rethink how to bring diagnostics more formally into the government sponsored health insurance schemes, so that diagnostics are embedded and prioritised as part of the broader country’s health system response and progress towards to UHC.
Acknowledgments
We thank Adriana Velazquez Berumen at the WHO for comments on an earlier draft.
Footnotes
Handling editor: Seye Abimbola
Twitter: @jacobbigio, @paimadhu, @r_das20, @hbhuy, @aamirchmd, @dr_vijayashree, @divyasrivast
Contributors: DS designed the template for the targeted review. DS and JB drafted the manuscript. RD contributed to the literature search and commented on the manuscript. EH and MP commented on the research design and earlier drafts. BA, ASC, HH, UZ, LM, TAN, SS, AVR, SCV and VY commented on earlier versions of the draft.
Funding: DS received funding from FIND Diagnostics.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Fleming KA, Horton S, Wilson ML, et al. The Lancet Commission on diagnostics: transforming access to diagnostics. Lancet 2021;398:1997–2050. 10.1016/S0140-6736(21)00673-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Global spending on health 2020: weathering the storm. Geneva: World Health Organization, 2020. [Google Scholar]
- 3.OECD Eurostat and World Health Organization . A system of health accounts 2011, Rev. edn. Paris, 2017. [Google Scholar]
- 4.Our World in Data . Population 2021. 2023. Available: https://ourworldindata.org/grapher/population?time=latest&country=KHM~IND~IDN~NPL~PAK~PHL~VNM
- 5.World Health Organization . Primary health care on the road to universal health coverage: 2019 monitoring report. Geneva: World Health Organization, 2020. [Google Scholar]
- 6.The Centre for International Economics . The economic value of pathology: achieving better health, and a better use of health resources. 2016. [Google Scholar]
- 7.Duggal R, Kurian O, Bhate-Deosthali P, et al. Political economy of Healthcare in India (special issue of journal Health for the millions). Health for the Millions 2012:1–70. [Google Scholar]
- 8.Khanal GN, Bharadwaj B, Upadhyay N, et al. Evaluation of the national health insurance program of Nepal: are political promises translated into actions Health Res Policy Syst 2023;21:7. 10.1186/s12961-022-00952-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dương N. Hơn 91 Triệu Người Tham Gia Bảo Hiểm Y Tế, Bao Phủ Trên 92% Dân Số. VnEconomy 2023. [Google Scholar]
- 10.Ministry of Planning . Data query. 2022. Available: https://www.idpoor.gov.kh/reporting/builder
- 11.National Health Authority Government of India . About Pradhan Mantri JAN Arogya Yojana (PM-JAY) 2019. n.d. Available: https://nha.gov.in/PM-JAY
- 12.Sehat Sahulat Program . Frequently asked questions 2022. n.d. Available: https://www.pmhealthprogram.gov.pk/faqs
- 13.Ministry of Health . Guidelines for the benefit package and provider payment of the health equity fund for the poor. Phnom Penh: Ministry of Health, 2018. [Google Scholar]
- 14.Shah S, Jha N, Khanal VK, et al. Utilization of social health security scheme among the households of Illam district, Nepal. PLOS ONE 2022;17:e0265993. 10.1371/journal.pone.0265993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maulana N, Soewondo P, Adani N, et al. How Jaminan Kesehatan Nasional (JKN) coverage influences out-of-pocket (OOP) payments by vulnerable populations in Indonesia. PLOS Glob Public Health 2022;2:e0000203. 10.1371/journal.pgph.0000203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.BPJS Kesehatan . Benefits. 2017. Available: https://www.bpjs-kesehatan.go.id/bpjs/pages/detail/2014/12
- 17.Philippine Health Insurance Corporation . Changing gears: moving philHealth on high speed - the 2021-2023 PhilHealth strategic plan. Manila, 2020. [Google Scholar]
- 18.Ministry of National Health Services Regulations and Coordination . “Charter of services” Sehat Sahulat program. Government of Pakistan, 2021. [Google Scholar]
- 19.Le QN, Blizzard L, Si L, et al. The evolution of social health insurance in Vietnam and its role towards achieving universal health coverage. Health Policy OPEN 2020;1:100011. 10.1016/j.hpopen.2020.100011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen LH, Hoang ATD. Willingness to pay for social health insurance in central Vietnam. Front Public Health 2017;5:89. 10.3389/fpubh.2017.00089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Todini N, Hammett TM, Fryatt R. Integrating HIV/AIDS in Vietnam’s social health insurance scheme: experience and lessons from the health Finance and governance project, 2014–2017. Health Systems & Reform 2018;4:114–24. 10.1080/23288604.2018.1440346 [DOI] [Google Scholar]
- 22.Government of Nepal Health Insurance Board . Benefit package. Health Insurance Board, 2017. [Google Scholar]
- 23.Government of Nepal Health Insurance Board . Partial package update list. Health Insurance Board, 2017. [Google Scholar]
- 24.Sehat Sahulat Program . Sehat Sahulat Program "Benefit Package (2019-2021). Sehat Sahulat Program, 2019. [Google Scholar]
- 25.Philippine Health Insurance Corporation . Circular 2019-10: guidelines on the granting of immediate eligibility to members. Manila, 2019. [Google Scholar]
- 26.World . Indonesia - National Health Insurance (JKN) Reforms and Results Program (English). Washington, DC, 2021. [Google Scholar]
- 27.Sharma P, Yadav DK, Shrestha N, et al. Dropout analysis of a national social health insurance program at Pokhara metropolitan city, Kaski. Int J Health Policy Manag 2021;11:2476–88. 10.34172/ijhpm.2021.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.UNAIDS . Key populations are being left behind in universal health coverage: landscape review of health insurance schemes in the Asia-Pacific region. Geneva, 2022. [Google Scholar]
- 29.Philippine Health Insurance Corporation . Circular 2020-05: Premium Contribution Schedule in the National Health Insurance Program (NHIP) Pursuant to the R.A. no.11223 Known as the “Universal Health Care Act” (Revision 1). Manila. 2020. [Google Scholar]
- 30.Philippine Health Insurance Corporation . Circular 2020-24: governing policies on no co-payment/no balance billing for philHealth benefit packages. Manila, 2020. [Google Scholar]
- 31.Indian Council of Medical Research . National essential diagnostics list. New Dehli. 2019. [Google Scholar]
- 32.Ministry of Health & Family Welfare . National health mission: free diagnostics service initiative. 2011. [Google Scholar]
- 33.Philippine Health Insurance Corporation . Circular 2012-48: Implementing guidelines on the Z benefit package. 2012. [Google Scholar]
- 34.Philippine Health Insurance Corporation . Circular 2012-29: governing policies on philHealth benefit package for case type Z. Manila, 2012. [Google Scholar]
- 35.Government of Nepal Health Insurance Board . Payment Mechanism and Rates. Health Insurance Board, 2017. [Google Scholar]
- 36.Socialist Republic of Viet Nam Ministry of Health . Circular on transfer between medical facilities no: 14/2014/TT-BYT 2014. n.d. Available: https://thuvienphapluat.vn/van-ban/The-thao-Y-te/Circular-No-14-2014-TT-BYT-transfer-between-medical-facilities-291869.aspx
- 37.USAID . USAID supports Vietnam’s inclusion of tuberculosis care under national health insurance. 2023. Available: https://www.usaid.gov/vietnam/news/jan-13-2023-usaid-supports-vietnams-inclusion-tuberculosis-care-under-national-health-insurance
- 38.Ranabhat CL, Subedi R, Karn S. Status and determinants of enrollment and dropout of health insurance in Nepal: an Explorative study. Cost Eff Resour Alloc 2020;18:40. 10.1186/s12962-020-00227-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheng Q, Asante A, Susilo D, et al. Equity of health financing in Indonesia: A 5-year financing incidence analysis (2015-2019). Lancet Reg Health West Pac 2022;21:100400. 10.1016/j.lanwpc.2022.100400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Annear PL, Tayu Lee J, Khim K, et al. Protecting the poor? impact of the national health equity fund on utilization of government health services in Cambodia, 2006-2013. BMJ Glob Health 2019;4:e001679. 10.1136/bmjgh-2019-001679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Asante AD, Ir P, Jacobs B, et al. Who benefits from Healthcare spending in Cambodia? evidence for a universal health coverage policy. Health Policy Plan 2019;34:i4–13. 10.1093/heapol/czz011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Health Mission . Free drugs & diagnostics service initiative. Ministry of Health & Family Welfare, Government of India, 2022. Available: https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1218&lid=192 [Google Scholar]
- 43.Teo HS, Bales S, Bredenkamp C, et al. The Future of Health Financing in Vietnam: Ensuring Sufficiency, Efficiency, and Sustainability (English). Washington, DC, 2019. 10.1596/32187 [DOI] [Google Scholar]
- 44.World Bank . Vietnam - Health Financing Trends: 2008-2017 (English). Washington, DC, 2020. [Google Scholar]
- 45.Yellapa V, Devadasan N, Krumeich A, et al. How patients navigate the diagnostic Ecosystem in a fragmented health system: a qualitative study from India. Glob Health Action 2017;10:1350452. 10.1080/16549716.2017.1350452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bashir S, Kishwar S, Salman . Incidence and determinants of catastrophic health expenditures and Impoverishment in Pakistan. Public Health 2021;197:42–7. 10.1016/j.puhe.2021.06.006 [DOI] [PubMed] [Google Scholar]
- 47.International Labour Organization . Actuarial analysis of the federal Sehat Sahulat program. Geneva: International Labour Office, 2019. [Google Scholar]
- 48.Hasan SS, Mustafa ZU, Kow CS, et al. Sehat Sahulat program": A leap into the universal health coverage in Pakistan. Int J Environ Res Public Health 2022;19:6998. 10.3390/ijerph19126998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.World Health Organization . UHC compendium. 2023. Available: https://www.who.int/universal-health-coverage/compendium
- 50.World Health Organization . Global atlas of medical devices. Geneva: World Health Organization, 2022. [Google Scholar]
- 51.World Health Organization Executive Board . Strengthening diagnostics capacity. 2023. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2023-012512supp001.pdf (326.2KB, pdf)
Data Availability Statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information.