Abstract
Background
Continuous combination of MAPK pathway inhibition (MAPKi) and anti-programmed death-(ligand) 1 (PD-(L)1) showed high response rates, but only limited improvement in progression-free survival (PFS) at the cost of a high frequency of treatment-related adverse events (TRAE) in patients with BRAFV600-mutated melanoma. Short‐term MAPKi induces T-cell infiltration in patients and is synergistic with anti-programmed death-1 (PD‐1) in a preclinical melanoma mouse model. The aim of this phase 2b trial was to identify an optimal regimen of short-term MAPKi with dabrafenib plus trametinib in combination with pembrolizumab.
Methods
Patients with treatment-naïve BRAFV600E/K-mutant advanced melanoma started pembrolizumab 200 mg every 3 weeks. In week 6, patients were randomized to continue pembrolizumab only (cohort 1), or to receive, in addition, intermittent dabrafenib 150 mg two times per day plus trametinib 2 mg one time per day for two cycles of 1 week (cohort 2), two cycles of 2 weeks (cohort 3), or continuously for 6 weeks (cohort 4). All cohorts continued pembrolizumab for up to 2 years. Primary endpoints were safety and treatment-adherence. Secondary endpoints were objective response rate (ORR) at week 6, 12, 18 and PFS.
Results
Between June 2016 and August 2018, 33 patients with advanced melanoma have been included and 32 were randomized. Grade 3–4 TRAE were observed in 12%, 12%, 50%, and 63% of patients in cohort 1, 2, 3, and 4, respectively. All planned targeted therapy was given in 88%, 63%, and 38% of patients in cohort 2, 3, and 4. ORR at week 6, 12, and 18 were 38%, 63%, and 63% in cohort 1; 25%, 63%, and 75% in cohort 2; 25%, 50%, and 75% in cohort 3; and 0%, 63%, and 50% in cohort 4. After a median follow-up of 43.5 months, median PFS was 10.6 months for pembrolizumab monotherapy and not reached for patients treated with pembrolizumab and intermittent dabrafenib and trametinib (p=0.17). The 2-year and 3-year landmark PFS were both 25% for cohort 1, both 63% for cohort 2, 50% and 38% for cohort 3 and 75% and 60% for cohort 4.
Conclusions
The combination of pembrolizumab plus intermittent dabrafenib and trametinib seems more feasible and tolerable than continuous triple therapy. The efficacy is promising and appears to be favorable over pembrolizumab monotherapy.
Trial registration number
Keywords: Melanoma; Immune Checkpoint Inhibitors; Clinical Trials, Phase II as Topic
WHAT IS ALREADY KNOWN ON THIS TOPIC
Continuous triple combination of BRAF plus mitogen-activated protein kinase (MEK) inhibition and anti-programmed death-1 (PD-1) has been shown in several randomized trials, to only marginally improve progression-free survival at cost of high toxicity. In addition it reduces second-line treatment options.
WHAT THIS STUDY ADDS
Short-time addition of dabrafenib and trametinib to pembrolizumab is feasible and has promising activity.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
These results provide a rationale for further investigations preferably in patients who do not respond to anti-PD-1 monotherapy.
Introduction
Targeted therapy (TT) with BRAF plus mitogen-activated protein kinase (MEK) inhibition and checkpoint inhibition (CPI) have significantly improved the outcome of patients with advanced BRAFV600E mutation-positive melanoma. Combined BRAF plus MEK inhibition with dabrafenib plus trametinib, vemurafenib plus cobimetinib, or encorafenib plus binimetinib, have all shown high response rates (up to 70%), but relative short progression-free survival (PFS) with a median PFS of 12–15 months1–3, and a 5-year PFS rate of 19%.1 In contrast, the response rates to CPI are lower (45% and 46% for nivolumab and pembrolizumab, respectively, and 58% for nivolumab plus ipilimumab),4 5 but responses are often durable. The PFS reaches a plateau of 36% at 5 years for the combination of nivolumab plus ipilimumab and 29% for nivolumab monotherapy,6 with a recently reported 7.5-year melanoma specific survival of 55% for combination CPI.7
The diametrically different patterns of response and PFS rates of TT and CPI, and the distinct mechanisms of action have led early on to the idea of combining MAPK pathway inhibition and programmed death-1 (PD-1) blockade.8 The combination of cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) blockade plus BRAF inhibition was the first that was explored but declared to be too toxic with high frequency of hepatic and gastrointestinal toxicity.9 10 Translational studies supported the addition of BRAF±MEK inhibition to CPI as it increases tumor T-cell infiltration, induces tumor inflammation characterized by a higher interferon (IFN) gene expression signature, and increases programmed death-ligand 1 (PD-L1) expression,11–15 all parameters associated with increased responsiveness towards PD-1 blockade.16 17 In melanoma mouse models, this combination indeed demonstrated durable responses.15 Based on these data, several early phase trials have been initiated, testing continuous combination of BRAF plus MEK inhibition plus PD-(L)1 blockade.18–21 All four trials observed high response rates, but also considerable higher grade 3–4 toxicity than expected from BRAF plus MEK inhibition or anti-PD-(L)1 alone.
Another question is how long triplet therapy needs to be given, or whether triplet induction followed by CPI consolidation might be better tolerated and equally effective. Such a schedule would also offer the option to switch back to BRAF plus MEK inhibition as a second-line therapy. An interesting observation that supports this strategy is that BRAF±MEK inhibition-induced tumor T-cell infiltration seems to be transient and has been described to be diminished at progression or even early on after several weeks of TT.11 12 22 Therefore, we tested short-term BRAF and MEK inhibition combined with PD-1 blockade in a BRAF/PTEN-driven mouse melanoma model. We observed improved tumor growth control as compared with PD-1 blockade or BRAF plus MEK inhibition alone, and ongoing complete responses in almost 50% of the mice.22
Our preclinical data have led to the hypothesis, that intermittent short-term BRAF plus MEK inhibition (dabrafenib and trametinib) in combination with PD-1 blockade (pembrolizumab) might be equally effective in immune activation, but less toxic as compared with continuous triple combination. To address this question, the phase 2 IMPemBra trial was designed. IMPemBra compared the safety and feasibility of three schedules of short-term BRAF and MEK inhibition plus anti-PD-1 to PD-1 blockade alone, and analyzed in a descriptive manner, the activity and immune-activating capacity of these schemes.
Methods
Study design and participants
The investigator-initiated single-center, open-label phase 2 randomized controlled IMPemBra trial compared the addition of different schemes of short-term continuous or intermittent dabrafenib plus trametinib to pembrolizumab as compared with pembrolizumab monotherapy.
Eligible patients were 18 years or older, diagnosed with histologically or cytologically confirmed unresectable stage III or stage IV BRAFV600E/K-mutated melanoma. All patients needed to have a WHO performance status of 0–2, measurable disease according to the response evaluation criteria in solid tumors (RECIST) version 1.1. and at least one lesion easy-accessible (subcutaneous or lymph node) for biopsies. Key exclusion criteria were prior treatment with anti-PD-(L)1, anti-CTLA-4 or BRAF and/or MEK inhibition, untreated or unstable brain metastases, and a history of autoimmune disease requiring systemic treatment.
All patients provided written informed consent before registration. The trial was conducted in accordance with the protocol, Good Clinical Practice guidelines and the Declaration of Helsinki. The trial was sponsored by the Netherlands Cancer Institute (NKI) and funded by Merck Sharp & Dohme (MSD, grant number MK3475-272). The sponsor maintained the study database and reported annually to the medical ethics committee of the NKI. The database lock for the presented analysis took place on 8 February, 2022.
Randomization and masking
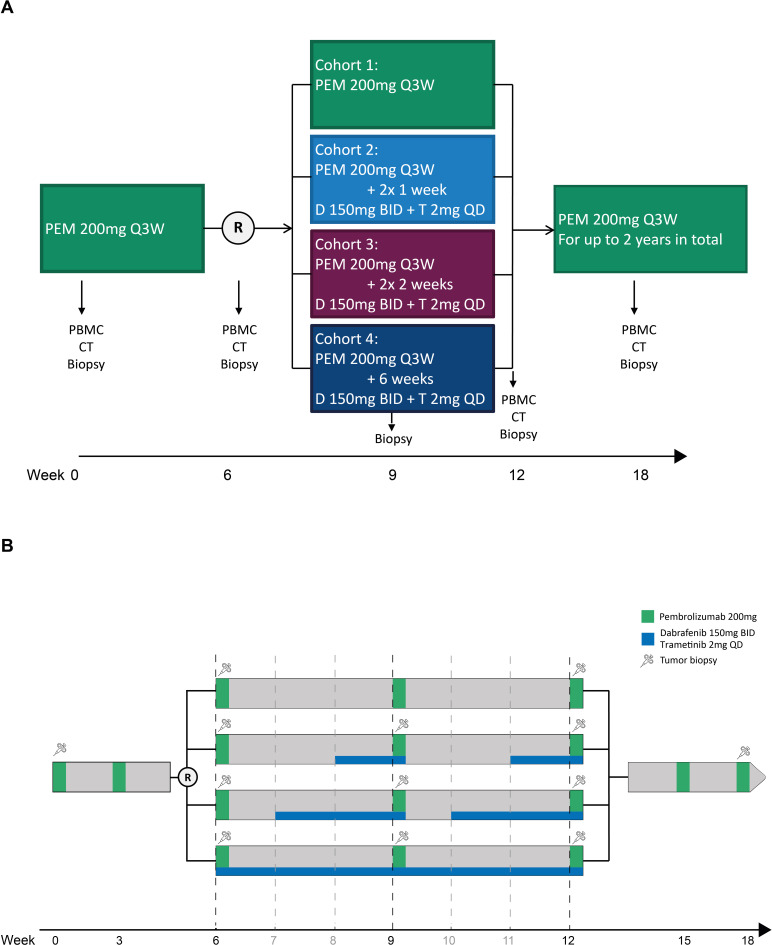
All patients started with two cycles of pembrolizumab (figure 1A). In week 6, patients were randomized to receive either pembrolizumab monotherapy (cohort 1), pembrolizumab plus two times 1 week dabrafenib plus trametinib (cohort 2), pembrolizumab plus two times 2 weeks dabrafenib plus trametinib (cohort 3), or pembrolizumab plus 6 weeks dabrafenib plus trametinib (cohort 4) (figure 1B). To ensure comparability randomization was stratified according to baseline lactate dehydrogenase (LDH) level.
Figure 1.
Overview of trial design and treatment schedules. (A) Schematic overview of trial design. (B) Overview of treatment schedules, starting at week six after randomization. BID, two times a day; D, dabrafenib; PBMC, peripheral blood mononuclear cells; PEM, pembrolizumab; QD, once a day; Q3W, every 3 weeks; T, trametinib.
Patients were enrolled by the local investigators. After verification of eligibility criteria, patients were randomized, stratified by LDH level, using Pocock and Simon minimization,23 in ALEA randomization software. If patients no longer fulfill the eligibility criteria after having signed informed consent but before randomization, they were withdrawn and replaced by another patient. This was an open-label trial; the investigators, site staff, and patients were aware of the treatment assignment during the study participation.
Procedures
Treatment and assessments
All patients started with two cycles of pembrolizumab 200 mg intravenously every 3 weeks (q3w). From week 6 to week 12 patients in cohort 1 continued with pembrolizumab 200 mg q3w; patients in cohort 2 received in addition to the pembrolizumab two cycles of 1 week dabrafenib plus trametinib q3w; patients in cohort 3 received in addition to the pembrolizumab two cycles of 2 weeks dabrafenib plus trametinib q3w; patients in cohort 4 received continuously for 6 weeks dabrafenib plus trametinib in addition to the pembrolizumab. Dabrafenib and trametinib were given at standard doses: dabrafenib 150 mg two times a day and trametinib 2 mg one time a day. From week 12 and onwards all patients continued with pembrolizumab 200 mg q3w only, for up to a maximum total treatment duration of 2 years. Pembrolizumab was manufactured and provided by MSD, dabrafenib and trametinib were manufactured by Novartis and funded by MSD.
Patients were treated until unacceptable toxicity, withdrawal of consent, disease progression or completion of the total treatment schedule. Pembrolizumab was withheld for treatment-related grade 4 hematological, grade ≥3 non-hematological and severe or life-threatening adverse events. In case toxicity did not resolve to grade 0–1 within 6 weeks (within 3 weeks during the first 12 weeks of the trial) after the last infusion, trial treatment was discontinued. Dose reductions were not permitted. Standard discontinuation criteria in the event of immune-related toxicity are described in the online supplemental file 2 (page 36–37).
jitc-2023-006821supp002.pdf (910.4KB, pdf)
Adverse events and laboratory values were graded by the investigators throughout the trial according to the National Cancer Institute Common Terminology Criteria for Adverse Events V.4.03, from the first dose of study treatment until 2 years after treatment initiation or start of other systemic therapy. Serious adverse events were reported until 100 days after discontinuation of the study drug.
Laboratory tests, hematology and chemistry (including endocrine axis), were tested at baseline and before every pembrolizumab infusion. Targeted physical examination and measurement of vital parameters were performed before every infusion of pembrolizumab. Patients with ongoing clinical benefit after cessation of therapy were evaluated every 3 months post-treatment by targeted physical examination and laboratory testing, up until 3 years. CT evaluation of chest, abdomen and pelvis was performed at baseline, week 6, 12 and 18, and subsequently every 3 months for up to 3 years. Subsequent structured follow-up was performed according to current national melanoma guidelines, with imaging every 6 months for year 4 and 5 and once a year for years 6–10.
Collection of blood and tumor samples
Blood and serum samples for isolation of plasma and peripheral blood mononuclear cells (PBMCs) were collected at baseline, week 6, 12 and 18, and subsequently every 3 months during treatment. Tumor biopsies were taken from an easy and safe accessible metastatic lesion by a radiologist using ultrasound. Biopsies were collected at baseline, week 6, week 9 (only for patients in cohorts 2–4), week 12 and week 18. The obtained samples were immediately snap-frozen and formalin-fixed and paraffin-embedded (FFPE). In case of tumor relapse or progression, additional biopsies, blood and serum samples and PBMCs were collected, if possible.
Translational research
RNA sequencing
From patients with sufficient tumor material in the frozen tumor samples, based on the pathologist’s scoring (at least 30% tumor cells of HE stained cryostat frozen section), RNA was isolated. A total of 27 patients had sufficient tumor cells in their frozen biopsies from up to four time points. RNA was isolated from fresh-frozen tumor frozen sections (10 µm) with the AllPrep DNA/RNA/miRNA Universal isolation kit (QIAGEN, 80224), according to the manufacturers’ protocol, using the QIAcube.
RNA sequencing was performed by CeGaT. The quantity of total RNA were assessed by the 2100 Bioanalyzer using a Nano chip (Agilent), in which samples having 100 ng RNA were subjected to library generation. Using TruSeq Stranded mRNA sample preparation kit (Illumina), strand-specific libraries were generated according to the manufacturer’s instructions. The resulting libraries were sequenced with 2×100 bp reads on the NovaSeq 6000 system.
Demultiplexing of the sequencing reads was performed with Illumina bcl2fastq (2.20). Adapters were trimmed with Skewer (V.0.2.2).24 The quality of FASTQ files was analyzed with FastQC (V.0.11.5-cegat) (Andrews, 2010).25 Plots were created using ggplot2 in R (V.3.6.1). The FASTQ files were mapped to the human reference genome (Homo.sapiens.GRCh38.v82). Normalized gene expression data per data set was centered by subtracting the row means and scaling by dividing the columns by the SD. Next, the previously defined gene expression immune signatures IFN-γ signature,17 major histocompatibility complex (MHC)-I and MHC-II signatures18 were analyzed and pathway analyses were performed using the hallmark gene set collection.26
Immunohistochemistry
Intratumoral immune cell infiltration at different time points was determined by immunohistochemistry assays of FFPE tumor blocks (3 µm). Immunohistochemistry of the FFPE tumor samples was performed on a BenchMark Ultra autostainer. Briefly, paraffin sections were cut at 3 µm, heated at 75°C for 28 min and deparaffinized in the instrument with EZ prep solution (Ventana Medical Systems). Heat-induced antigen retrieval was carried out using Cell Conditioning 1 (CC1, Ventana Medical Systems) for 32 min at 95°C (CD3, CD8), 48 min at 95°C (PD-L1).
CD3 was detected using clone SP7 (1:100 dilution, 32 min at 37°C, Spring/ITK), CD8 clone C8/144B (1:200 dilution, 32 min at 37°C, DAKO/Agilent) and PD-L1 using clone 22C3 (1:40 dilution, 1-hour room temperature, DAKO/Agilent). Bound antibody was detected using the OptiView DAB Detection Kit (Ventana Medical Systems). Slides were counterstained with Hematoxylin and Bluing Reagent (Ventana Medical Systems). Scoring was performed by a blinded pathologist.
Cell staining and flow cytometry
Single-cell suspensions were generated from frozen peripheral PBMCs by resuspension of frozen PBMCs in fetal bovine serum (Invitrogen) and centrifuged for 5 min at 1500 rotations per minute (RPM). The cell pellet was resuspended in RPMI medium 1640 (Thermo Fisher Scientific) supplemented with 10% human serum (Sigma Aldrich) and 100× benzonase nuclease (Merck). Cells were incubated at 37°C for 20 min. Next, cells were centrifugated for 5 min at 1500 RPM and 2×106 cells were stained at 4°C for 20 min with the following antibodies diluted in Brilliant Stain Buffer (BD Biosciences): 1 µL anti-human CD14-APC-H7 (BD Biosciences, clone MφP9), 2 µL anti-human CD19-APC-H7 (BD Biosciences, clone SJ25C1), 3 µL anti-human CD3-BUV805 (BD Biosciences, clone SK7), 1 µL anti-human CD4-BB515 (BD Biosciences, clone SK3), 2 µL anti-human CD8-AF700 (Thermo Fisher, clone 3B5), 0.7 µL anti-human CD45RA-BUV737 (BD Biosciences, clone HI100), 1 µL anti-human CD14-PE-CF594 (BD Biosciences, clone 150503), 1 µL anti-human CD197 (CCR7) (BD Biosciences, clone 150503) and 1 µL anti-human PD-1-BV480 (BD Biosciences, clone 26D5). Subsequently, cells were stained with 0.125 µL LIVE/DEAD Fixable Near-IR Dead Cell Stain (Thermo Fisher) in phosphate-buffered saline (PBS) at 4°C for 10 min. The cells were washed, then fixed and permeabilized with Fixation/Permeabilization Concentrate and Diluent (Invitrogen) according to manufacturer’s protocol. The cells were stained with 1 µL anti-Ki67-PercP-Cy5.5 (BD Biosciences, clone B56) and incubated at 4°C for 30 min. After incubation, cells were washed twice and data acquisition was performed on BD FACSymphony flow cytometer (BD Biosciences) with FACSDiva software. The following gating strategy was used to identify (PD-1 positive) CD8+ T cells and (PD-1 positive) CD4+T cells: (1) selection of live cells (LIVE/DEAD near-IR dead cell dim) of single-cell lymphocytes, (2) selection of anti-CD3 positive and anti-CD14, anti-19 negative cells, (3) selection for CD8+ or CD4+ and PD-1+ population.
ctDNA
Blood was collected in 10 mL K2-EDTA tubes. Cell-free plasma was obtained within 4 hours by a two-step centrifugation at room temperature: 20 min at 380 g followed by 10 min at 20,000 g. Cell-free plasma was stored in 1–4 mL aliquots at −80ºC. Cell-free DNA (cfDNA) isolation was done using the QIAsymphony Circulating DNA kit (article number 1091063, QIAGEN, Dusseldorf, Germany) with the QIAsymphony (QIAGEN). Elution volume was set to 60 µl and samples were stored at 4ºC until use. Droplet digital PCR was performed on the Bio-Rad QX200 using the BRAF V600 screening kit (article number 12001037, Bio-Rad Laboratories, Hercules, California, USA) For each replicate: 9 ul of the sample, 1 ul each of the mutant and wildtype probes and 11 ul ddPCR Supermix for Probes (no dUTP) (Bio-Rad, cat# 186–3023) were used. Droplets were generated with QX200 Droplet Generator and measured with QX200 Droplet Reader, data were analyzed with QuantaSoft (Bio-Rad, V.1.7.4.0917) and according to the described ALPACA method. 27
Outcomes
The primary objectives of the IMPemBra trial were to compare safety and feasibility of the three schedules of short-term dabrafenib plus trametinib in combination with pembrolizumab. The safety endpoint was defined as the occurrence of suspected unexpected serious adverse reactions (SUSARs) during the first 18 weeks. Furthermore, the percentage of treatment-related adverse events within the different treatment cohorts was observed. The other primary endpoint was determination of the immune-activating capacity of the different treatment regimens. Secondary endpoints were rates of response at week 6, 12 and 18, PFS and long-term toxicity rates. Radiologic response was assessed by local radiologist and scored according to RECIST V.1.1 criteria.28 PFS was defined as time from randomization until date of first progression, or death from any cause, whichever occurred first. Patients with no evidence of disease progression were censored at the last date of contact, also patients who started a new therapy before progression were censored at the start date of this new treatment. Overall survival (OS) was defined as time from randomization until date of death from any cause. Duration of response was defined as time from first complete or partial response until date of first progression or death from any cause, whichever occurred first.
Statistical analysis
A treatment cohort was defined as not safe and feasible, if two out of the first five patients (point estimate 0.4 (95% CI 0.05 to 0.85)) in each of the triple combination cohorts (cohorts 2–4) would experience immune-related adverse events (irAEs) unknown for pembrolizumab monotherapy, leading to non-adherence to the study scheme (except for irAEs being already present at week 6).
One of the secondary endpoints was the PFS rate in the different treatment cohorts. All 32 patients had to be followed for at least 2 years. Assuming an improvement in median PFS from 3 to 6 months, eight patients in each arm would be required to allow detection of a HR of 0.5 with 80% power at a one-sided α level of 0.15. The control group (cohort 1) would provide a reference value for the median PFS. In case of a clearly different PFS reference value from the assumption, the three cohorts together could still be contrasted to the median PFS of the standard cohort. Comparison between standard and experimental treatment in 32 patients in four cohorts (one standard compared with the three experimental groups together) would provide approximately 70–80% power (one-sided α of 0.15) to detect a hazard of 0.5 with small deviations in the assumed median PFS.
All analyses were performed in all patients who were randomized and had received at least one dose of the study drug. Survival outcome curves (PFS and OS) for every cohort were estimated using Kaplan-Meier methodology. The log-rank test was used to compare differences between treatment arms. Median follow-up from randomization was calculated using the reverse Kaplan-Meier approach. Analyses were performed using R Studio V.1.14.17 and GraphPad Prism (V.9.02).
Results
Baseline characteristics
Between June 2016 and August 2018, 40 patients with advanced melanoma were screened, 33 have been included and 32 were randomly assigned to one of the four different cohorts at week 6 (figure 1A). One of the patients was not randomized because of fast progressive disease and clinical deterioration. All patients had relatively favorable prognostic clinical characteristics with an Eastern Cooperative Oncology Group (ECOG) performance score of 0–1 and in 88% a normal LDH level at baseline (table 1). The majority of patients, 53%, had M1c disease, 81% had a BRAFV600E and 19% had a BRAFV600K mutation. Characteristics were well balanced between the cohorts, with the only exception of more patients with irresectable stage IIIC disease who were included in cohort 4.
Table 1.
Baseline characteristics for all patients included and reported per treatment cohort
| Characteristics | Total (n=32) |
Cohort 1 PEM (n=8) |
Cohort 2 PEM + 2×1W D+T (n=8) |
Cohort 3 PEM + 2×2W D+T (n=8) |
Cohort 4 PEM + 6W D+T (n=8) |
|||||
| Median age, year (range) | 56 | (22–78) | 58 | (46–71) | 52 | (34–73) | 56 | (34–78) | 54 | (22–78) |
| Sex, male | 18 | (56%) | 6 | (75%) | 4 | (50%) | 4 | (50%) | 4 | (50%) |
| ECOG | ||||||||||
| 0 | 30 | (94%) | 7 | (88%) | 7 | (88%) | 8 | (100%) | 8 | (100%) |
| 1 | 2 | (6%) | 1 | (12%) | 1 | (12%) | – | – | – | – |
| Stage | ||||||||||
| IIIc | 2 | (6%) | – | – | – | – | – | – | 2 | (25%) |
| M1a | 5 | (16%) | 2 | (25%) | – | – | 1 | (12%) | 2 | (25%) |
| M1b | 8 | (25%) | 1 | (12%) | 3 | (38%) | 2 | (25%) | 2 | (25%) |
| M1c | 17 | (53%) | 15 | (63%) | 5 | (63%) | 5 | (63%) | 2 | (25%) |
| BRAF mutation | ||||||||||
| V600E | 26 | (81%) | 5 | (63%) | 8 | (100%) | 5 | (63%) | 8 | (100%) |
| V600K | 6 | (19%) | 3 | (38%) | 3 | (38%) | – | – | ||
| LDH | ||||||||||
| <ULN | 28 | (88%) | 7 | (88%) | 7 | (88%) | 7 | (88%) | 7 | (88%) |
| >ULN | 4 | (12%) | 1 | (12%) | 1 | (12%) | 1 | (12%) | 1 | (12%) |
D+T, dabrafenib+trametinib; ECOG, Eastern Cooperative Oncology Group; LDH, lactate dehydrogenase; PEM, pembrolizumab; ULN, upper limit of normal; W, weeks.
Feasibility and toxicity
We observed no SUSARs in any of the treatment cohorts and there were no unexpected irAEs during triple therapy. Any grade treatment-related adverse events (TRAEs) were seen in 88% of patients in the pembrolizumab cohort and in 100% in the pembrolizumab plus dabrafenib and trametinib cohorts.
The grade 3–4 TRAE rates were 12%, 12%, 50%, and 63% for patients in cohort 1, 2, 3, and 4, respectively (table 2). This difference in toxicity led to differences in treatment adherence among the cohorts. All planned dabrafenib and trametinib were given in 88% of patients in cohort 2 and 63% in cohort 3 but only in 38% of patients in cohort 4 (table 2). Most patients needed to interrupt or discontinue TT due to fever (n=2) or elevated liver enzymes (n=4). In total, three patients needed to discontinue pembrolizumab, due to myalgia (n=1, cohort 2), uveitis and neurological toxicity (n=2, cohort 3). These patients completed the dabrafenib and trametinib treatment according to the protocol and needed to stop pembrolizumab after 3, 5 and 12 cycles. The patient who needed to stop pembrolizumab after three cycles was treated in cohort 2 and stopped pembrolizumab because of myalgia with resolution of symptoms after the start of low-dose prednisone. Despite therapy being stopped early, this patient still has an ongoing response. Six patients were treated with high dose steroids, three due to elevated liver enzymes (all cohort 4) during triple therapy and the other three for irAEs that occurred beyond 12 weeks, during pembrolizumab monotherapy.
Table 2.
Adverse events and effect on further treatment, reported per treatment cohort
| Adverse event | Cohort 1 (n=8) PEM |
Cohort 2 (n=8) PEM + 2×1W D+T |
Cohort 3 (n=8) PEM + 2×2W D+T |
Cohort 4 (n=8) PEM + 6W D+T |
||||||||||||
| All grades | Grade 3–4 | All grades | Grade 3–4 | All grades | Grade 3–4 | All grades | Grade 3–4 | |||||||||
| Any adverse event | 7 | (88) | 1 | (12) | 8 | (100) | 1 | (12) | 8 | (100) | 4 | (50) | 8 | (100) | 5 | (63) |
| Fatigue | 4 | (50) | 6 | (75) | 7 | (88) | 7 | (88) | ||||||||
| Headache | 1 | (12) | 3 | (38) | 3 | (38) | 1 | (12) | 6 | (75) | ||||||
| Fever | 1 | (12) | 5 | (62) | 1 | (12) | 6 | (75) | 1 | (12) | ||||||
| ALT increased | 1 | (12) | 5 | (62) | 5 | (62) | 3 | (38) | ||||||||
| Influenza like symptoms | 4 | (50) | 3 | (38) | 1 | (12) | 4 | (50) | ||||||||
| Rash | 2 | (25) | 1 | (12) | 1 | (12) | 2 | (25) | 1 | (12) | 5 | (62) | 1 | (12) | ||
| AST increased | 5 | (62) | 5 | (62) | 4 | (50) | ||||||||||
| Arthralgia | 1 | (12) | 4 | (50) | 5 | (62) | ||||||||||
| Pruritus | 2 | (25) | 3 | (38) | 2 | (25) | 4 | (50) | ||||||||
| Nausea | 3 | (38) | 3 | (38) | 3 | (38) | ||||||||||
| Myalgia | 1 | (12) | 4 | (50) | 1 | (12) | 2 | (25) | 1 | (12) | ||||||
| Diarrhea | 4 | (50) | 2 | (25) | 2 | (25) | ||||||||||
| Neutrophil count decreased | 2 | (25) | 2 | (25) | 2 | (25) | 1 | (12) | ||||||||
| Hypothyroidism | 1 | (12) | 2 | (25) | 3 | (38) | ||||||||||
| Vomiting | 1 | (12) | 2 | (25) | 3 | (38) | ||||||||||
| Dry mouth | 1 | (12) | 3 | (38) | 2 | (25) | ||||||||||
| Dysgeusia | 1 | (12) | 2 | (25) | 2 | (25) | ||||||||||
| Hyperthyroidism | 1 | (12) | 2 | (25) | 2 | (25) | ||||||||||
| Skin hypopigmentation | 2 | (25) | 1 | (12) | 2 | (25) | ||||||||||
| Mucositis oral | 1 | (12) | 1 | (12) | 1 | (12) | ||||||||||
| Pancreatitis | 1 | (12) | 1 | (12) | ||||||||||||
|
Cohort 1
PEM |
Cohort 2
PEM + 2×1W D+T |
Cohort 3
PEM + 2×2W D+T |
Cohort 4
PEM + 6W D+T |
|||||||||||||
| Led to interruption of D+T | NA | – | – | 1 (12) | ||||||||||||
| Led to discontinuation of D+T | NA | 1 (12) | 3 (38) | 4 (50) | ||||||||||||
| Led to interruption of PEM | 1 (12) | – | 3 (38) | 5 (63) | ||||||||||||
| Led to discontinuation of PEM | – | 1 (12) | 2 (25) | – | ||||||||||||
| Treatment with steroids | ||||||||||||||||
| <1 mg/kg | 2 (25) | 2 (25) | 2 (25) | 2 (25) | ||||||||||||
| ≥1 mg/kg | – | – | 2 (25) | 4 (50) | ||||||||||||
ALT, alanine aminotransferase; AST, aspartate aminotransferase; D+T, dabrafenib+trametinib; PEM, pembrolizumab; W, weeks.
Efficacy
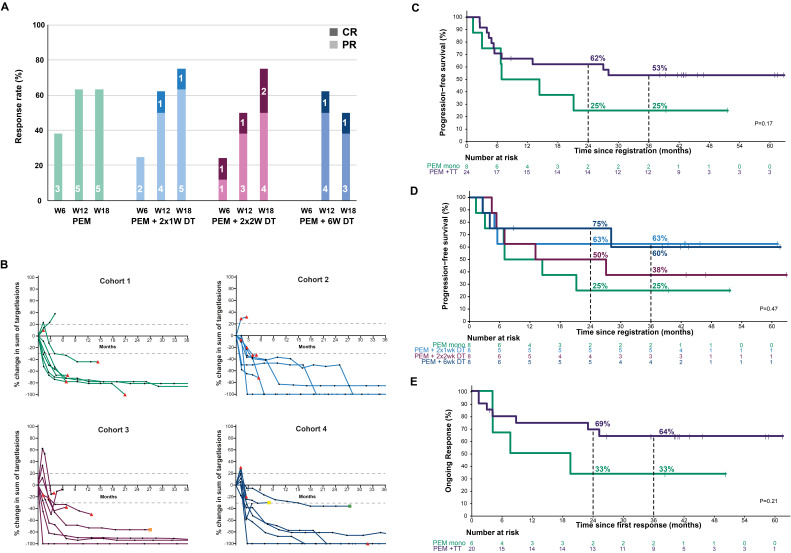
In all cohorts the response rates were increasing over time and the largest increases were observed between week 6 and week 12 (figure 2A), the period that the patients in cohorts 2–4 received the additional TT. The best objective response rate (ORR) was 75% (95% CI 35% to 97%) in cohort 1 and 2 and 88% (95% CI 47% to 100%) in cohort 3 and 4. The ORR for cohort 1 at different time points were 38%, 63%, and 63% at week 6, week 12, and week 18, respectively. In cohort 2, 25%, 63%, and 75% of patients had responses at, respectively, week 6, week 12, and week 18. ORR in cohort 3 were 25%, 50%, and 75% and in cohort 4 were 0%, 63%, and 50% (table 3). The responses per individual patient per cohort are illustrated in figure 2B.
Figure 2.
Antitumor response. (A) Responses plotted as percentage per cohort at different time points, with distinction made between complete (dark) and partial response (light). The numbers in the bar graph indicate the number of patients with a PR and CR. (B) Spider plots illustrating the response as change in targeted lesions (according to RECIST V.1.1.) compared with baseline over time. In every panel, the response per cohort for every individual patient is plotted. New lesions are marked with red triangles. The orange square represents surgery because of mild increase in one of the target lesions, the resection specimen demonstrated viable tumor cells; the green square represents surgery of a rest lesion, in the resection specimen no viable tumor was found, the yellow square represents a patient that changed therapy during response as the response was declared as not deep enough. (C) Progression-free survival curve, comparing patients treated with pembrolizumab only (green) to patients who received pembrolizumab with short-term dabrafenib plus trametinib (purple). (D) Progression-free survival curves of all individual cohorts. (E) Duration of response, comparing the patients treated with pembrolizumab only (green) to patients who received pembrolizumab with short-term dabrafenib plus trametinib (purple). CR, complete response; DT, dabrafenib plus trametinib; PR, partial response; PEM, pembrolizumab; RECIST, the response evaluation criteria in solid tumors; TT, targeted therapy; W, weeks.
Table 3.
Objective response rate at different time points, reported per treatment cohort
| Cohort 1 PEM |
Cohort 2 PEM + 2×1W D+T |
Cohort 3 PEM + 2×2W D+T |
Cohort 4 PEM + 6W D+T |
|||||||||||||
| BOR | W6 | W12 | W18 | BOR | W6 | W12 | W18 | BOR | W6 | W12 | W18 | BOR | W6 | W12 | W18 | |
| ORR | 75% (35%–97%) | 38% | 63% | 63% | 75% (35%–97%) | 25% | 63% | 75% | 88% (47%–100%) | 25% | 50% | 75% | 88% (47%–100%) | – | 63% | 50% |
| CR | 12% (0%–53%) | – | – | – | 50% (16%–84%) | – | 12% | 12% | 25% (3%–65%) | 12% | 12% | 25% | 38% (8%–76%) | – | 12% | 12% |
| PR | 63% (24%–91%) | 38% | 63% | 63% | 25% (3%–65%) | 25% | 50% | 63% | 63% (24%–91%) | 12% | 38% | 50% | 50% (16%–84%) | – | 50% | 38% |
| SD | – | 38% | 12% | 12% | – | 50% | 12% | – | 12% (0%–53%) | 50% | 50% | – | – | 88% | 25% | 25% |
| PD | 25% (3%–65%) | 25% | 12% | 12% | 25% (3%–65%) | 25% | 25% | 12% | 25% | – | 25% | 12% (0%–53%) | 12% | 12% | 12% | |
| NA | – | – | 12% | 12% | – | – | 12% | – | – | – | – | – | 12% | |||
BOR, best objective response; CR, complete response; D+T, dabrafenib+trametinib; NA, not assessable; ORR, overall response rate; PD, progressive disease; PEM, pembrolizumab; PR, partial response; SD, stable disease; W, weeks.
After a median follow-up of 43.5 months (IQR 42.9–60.3 months) with a minimum follow-up of 38.2 months for the patients alive, the median PFS of patients treated with pembrolizumab monotherapy was 10.6 months (95% CI 6.7 to not reached) and was not reached (95% CI 13 to not reached) for all patients in cohorts 2–4 combined, treated with pembrolizumab and short-term dabrafenib plus trametinib (p=0.17, figure 2C). The estimated 2-year and 3-year PFS were 25% for patients treated with pembrolizumab and 62% and 53% for patients treated with additional TT. Median PFS for the individual cohorts of patients treated with additional dabrafenib plus trametinib was 20.0 months in cohort 3 and not reached in cohorts 2 and 4 (figure 2D). The estimated 2-year and 3-year PFS were both 63% for cohort 2, 50% and 38% for cohort 3 and 75% and 60% for cohort 4.
Duration of response was longer for the combination cohorts than for the pembrolizumab monotherapy cohort (p=0.21, figure 2E). Median duration of response was 13.6 months for the patients treated with pembrolizumab and not reached for patients treated with additional TT. Responses were ongoing for >3 years in 33% of responding patients treated with pembrolizumab monotherapy and 64% of patients that received additional dabrafenib and trametinib in combination with pembrolizumab (figure 2E).
Median OS was 40.5 months for patients treated with pembrolizumab monotherapy and not reached for patients treated with pembrolizumab and short-term dabrafenib and trametinib (p=0.32, (online supplemental figure S1A, B). Estimated 3-year OS was 63% for patients treated with pembrolizumab and 71% for patients treated with additional TT. The estimated 3-year OS for the individual cohorts that were treated with additional TT were 63% for cohort 2, and 75% for cohort 3 and 4 (online supplemental figure S1B).
jitc-2023-006821supp001.pdf (540.4KB, pdf)
Translational research
Comprehensive biomarker analyses were performed with the aim to examine treatment-induced changes in the tumor and blood, and to identify patients benefiting from pembrolizumab or intermittent dabrafenib plus trametinib in combination with pembrolizumab.
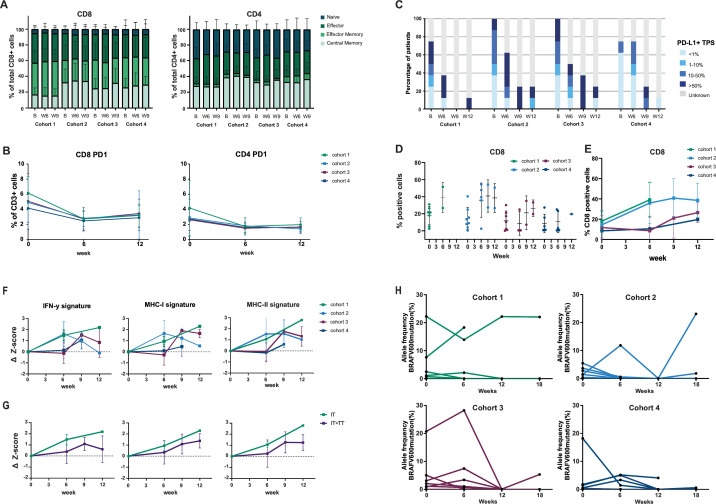
We observed no changes in composition of T-cell subsets in the peripheral blood during treatment and no differences between the cohorts (figure 3A). The percentage of PD-1 positive CD8 and CD4 T-cells in the peripheral blood slightly decreased on therapy. Again, no differences were seen between patients that received pembrolizumab monotherapy and patients that received additional TT (figure 3B).
Figure 3.
Translational research. (A) Subpopulations of CD8+ and CD4+ T cells in peripheral blood over time, shown per cohort, determined by flow cytometry. (B) Percentage of CD8+/PD-1+ and CD4+/PD-1+ cells within the population of CD3+ cells in peripheral blood determined by flow cytometry. The squares represent the means per cohort at different time points. (C) Distribution of the PD-L1 tumor proportion score (TPS) of tumor biopsies over time, per cohort. (D) Percentage of CD8+ T cells within tumor biopsies over time, shown per cohort, as determined by IHC staining. (E) Percentage of CD8+ T cells in tumor biopsy, each line represents the mean per cohort per time point. (F) Expression levels of IFN-γ, MCH I and MCH II signatures over time, per cohort. X-axis represents the time in weeks while Y-axis expresses the differences in signature score as compared with baseline score. Each data point in the plot corresponds to the average change in signature score compared with the baseline of the patients included in the cohort for that specific time point. (G) Same analyses as in F, but patients that received additional targeted therapy (cohorts 2–4) were grouped and compared with patients in cohort 1. (H) Allele frequency of BRAFV600E mutation, determined by ddPCR mutation assay on DNA extracted from plasma samples. Allele frequencies of BRAFV600E mutation per individual patient per time point are shown, each panel represents one cohort. B, baseline; ddPCR, digital droplet PCR; IFN-γ, interferon-gamma; IHC, immunohistochemistry; MHC-I, major histocompatibility complex I; MHC-II: major histocompatibility complex II; PD-1, programmed death-1; PD-L1, programmed death-ligand 1; TT, targeted therapy; W6, week 6; W9, week 9; W12, week 12.
Biopsies were taken at baseline, week 6, week 9 (cohorts 2–4), week 12, week 18 and at time of progressive disease. In several biopsies, mostly those of responding patients, there were no viable tumor cells left. This was seen in several of the biopsies taken at week 9 and later, but also in some of the biopsies taken at week 6.
PD-L1 expression on tumor cells increased from week 0 to week 6 and even further when comparing week 9 to week 6 in the cohorts that received additional TT (figure 3C). In cohort 1 and 2 and increase in the percentage of CD8+ cells in the tumor was observed in week 6 as compared with baseline. In cohort 3 and 4 there we observed a slight (non-significant) increase in infiltration of CD8+ cells after week 6, so after the addition of TT (figure 3D, E).
During treatment, an increase in expression of IFN-γ related genes was also observed within the tumor. In cohort 1 and 2, an increase in IFN-γ signature in the tumor was already observed after 6 weeks of pembrolizumab. In cohort 3 and 4, an increase in IFN-γ signature was observed in week 9, after addition of dabrafenib and trametinib. The same was seen for the MHC-I and MHC-II signatures (figure 3F, G, online supplemental figure S2A–C). In addition, pathway analyses revealed upregulation of several pro-inflammatory pathways after 6 weeks of pembrolizumab (online supplemental figure 2D). Likewise, when comparing biopsies from week 9 of patients in cohorts 2–4, with biopsies from the same patients in week 6, also predominantly pro-inflammatory pathways were upregulated after the addition of TT (online supplemental figure 2E).
Circulation tumor DNA (ctDNA) plasma analyses revealed that all patients who received TT in addition to pembrolizumab had a decline in the allele frequency of mutated BRAF between week 6 and week 12 (figure 3H). In some patients a decrease was already observed after 6 weeks of pembrolizumab, reflecting an early response on pembrolizumab monotherapy.
Discussion
IMPemBra is the first trial that has evaluated the addition of short-term intermittent BRAF and MEK TT to anti-PD-1 therapy. Adding dabrafenib and trametinib for a few weeks to pembrolizumab was feasible and had a manageable safety profile. Response rates increased after initiation of TT and many of these responses seem durable. Although the treatment cohorts were small and the study was not powered to compare between cohorts, PFS and duration of response seem to be in favor of the cohorts that received short-term TT.
With two effective treatment modalities with different response patterns and a good rationale to combine TT and CPI based on preclinical and translational data11 13 15 many efforts have been made to find the best combination and/or sequence strategy. The ultimate goal of first-line therapy is to reach a durable antitumor immune response in as many patients as possible. The DREAMseq trial recently confirmed this hypothesis and showed that first-line combination CPI followed by TT at progression is associated with a better PFS and OS as compared with the reversed sequence starting with dabrafenib plus trametinib.29 The SECOMBIT trial confirmed these data and showed that short-term induction with TT followed by combination CPI followed by TT at progression (sandwich approach) is feasible. Although the trial was not designed to compare between arms, the sequential scheme seems as effective as upfront CPI followed by TT at progression.30 For patients with elevated LDH at baseline, the sandwich approach induction appears to have the most promising PFS.31 Randomized trials comparing the triple combination approach of an anti-PD-(L)1 antibody, a BRAF and a MEK inhibitor versus BRAF plus MEK inhibition demonstrated only a mild PFS benefit.32–34 While the absolute PFS benefit is in the same range, due to the statistical design and performance of the control arm, two of these trials, the COMBI-I and the KEYNOTE-022, did not meet their primary endpoint and those triple combinations were not approved by the Food and Drug Administration. Moreover, toxicity was very high. Unfortunately, no data are yet available of how the triple combination performs against anti-PD-1 monotherapy (currently tested in STARBOARD35) or combined ipilimumab and nivolumab, which are standard of care options for first-line treatment.36
IMPemBra adds to these data by investigating the addition of MAPK pathway inhibition (MAPKi) to anti-PD-1 monotherapy in an ultra-short-term manner. The target population is slightly different and aimed at patients with a lower tumor load and more favorable baseline characteristics like a good performance status and a normal baseline LDH level for whom anti-PD-1 monotherapy is the first-line therapy of choice. The response rate of anti-PD-1 monotherapy in such a selected patient population is higher than what has been reported in the phase 3 trials, and ranged from 51% for patients with a normal LDH in the CheckMate 067 study37 to over 70% for selected patients with several favorable characteristics. In our trial, the response rate to anti-PD-1 monotherapy was with 75% (95% CI 35% to 97%) within this range.38 39 Although response rates are high, only about 35–50% of these patients will have a durable response,5 38 still a proportion has intrinsic resistance and is in need additional therapy.
In our trial, toxicity was dependent on the total duration of the TT. In cohort 2, we observed the same rate of grade 3–4 AEs as in cohort 1 where patients were only treated with pembrolizumab monotherapy. The rate of grade 3–4 adverse events for cohort 3 was 50% and in cohort 4 was 63%. In the triple combination arms of the phase 3 trials, this was even higher than in any arm of IMPemBra, with approximately 70% grade 3–4 AEs.32–34 The most common toxicities in our trial were fatigue, headache, fever, elevated liver enzymes and rash, all of which were consistent with what was observed for the continuous triple combinations. Pneumonitis, which was seen in 17% of patients in KEYNOTE-22 testing the same triple combination of pembrolizumab, dabrafenib and trametinib, was observed in our trial only once, in cohort 4, but was only of low grade.33 Since the majority of patients in cohort 4 could not complete TT according to protocol due to toxicities, and 50% needed high dose steroids, this regimen is of less interest for future studies.
In addition to a better tolerability, short-term addition of TT has a low risk of development of acquired resistance to TT, and creates as such, the opportunity to re-treat with TT in a later line of therapy. The latter has also been demonstrated in the SECOMBIT trial where the response rates to second-line BRAF and MEK inhibition after combination CPI was the same in the group that already had an induction of short-term TT as compared with the group that only had received CPI, namely 62.2% versus 57.9%.30 Furthermore, for CPI, unlike TT, it is known that many patients have ongoing responses after cessation of therapy due planned stop according to the protocol or due to toxicity.4 6 40 41
If patients are treated with continuous triple therapy, it will be difficult to discontinue therapy if you do not know if patients have an ongoing immune response or respond to the TT only. In IMPemBra all patients were treated for a maximum of 6 weeks with TT and for up to 2 years with pembrolizumab. Nevertheless, median duration of response has not been reached after a minimum follow-up of 38 months arguing for immune-related responses in all our patients. Finally, and as mentioned before, translational data support the short-term addition of TT approach, as immune infiltration is increased after induction with TT.13 42 43 Our translational analyses confirm these data and show a mild increase of T-cell infiltration and IFN-γ and MHC related gene expression after the short-term addition of dabrafenib and trametinib to pembrolizumab.
Not all patients will need the addition of BRAF and MEK inhibition. Notably, we observed in 7 out of 32 patients a very early response to pembrolizumab after 6 weeks. These patients probably can be spared the risk of additional toxicity of adding TT. The drop of BRAF ctDNA levels at week 6 could be helpful here, as week 6 CT scans underestimated the week 12 response to pembrolizumab monotherapy. Vice versa, absence of drop in ctDNA level, can potentially be used as a marker to identify those patients who can benefit from additional intermittent TT. The value of ctDNA evaluation in addition to radiologic evaluation in CPI therapy has also been demonstrated before.44–46
The most important limitation of our trial is that interpretation of the data is hampered by the small sample size. Although our data suggest that addition of short-term intermittent TT is more efficacious than pembrolizumab monotherapy this should first be tested in a larger cohort. Another limitation is that randomization was not stratified for the response at week 6. Unexpectedly, a substantial proportion of patients responded already after two cycles of pembrolizumab, and this percentage was different between the cohorts. This imbalance favored the pembrolizumab monotherapy arm (and disfavored cohort 4), and thus the effect of addition of short-term MAPKi might even be underestimated. Lastly, in many of the on-treatment biopsies of responding patients there were no viable tumor cells left, skewing the translational research to non-responder patient analyses.
In conclusion, IMPemBra demonstrated that addition of short-term intermittent dabrafenib plus trametinib (for two times 1 or 2 weeks) to pembrolizumab is a well-tolerated scheme, with a possible favorable efficacy. Such an approach conserves the possibility for TT as ‘second line’ therapy when patients develop progressive disease, which is not the case for the continuous triple combination schemes. Based on our data a larger randomized trial evaluating the short-term addition of intermittent BRAF plus MEK inhibition (two times 1 or 2 weeks) to upfront anti-PD-1 should be considered.
Footnotes
Contributors: CUB designed the study and wrote the study protocol. EAR coordinated the trial, analyzed and interpreted clinical and translational data and wrote the first draft of the manuscript with JMV. EAR, JWBdG, SW, MAV, JVvT, JBAGH and CUB recruited and treated patients and collected data. BCH and SWTPJH reviewed the scans and BAvdW reviewed the biopsies. AS and LGG-O were responsible for local data management. PD performed the bioinformatics analysis. KS and ML-Y did the statistical analysis of the clinical data. EPH and DR performed the flow cytometry analyses. DvdB was responsible for the circulating tumor DNA analyses. AB was responsible for the RNA isolations and performance of the staining of the biopsies. BAvdW and CF scored the stainings. CUB is the guarantor for this article. All authors interpreted the data, reviewed the manuscript, and approved the final version.
Competing interests: All authors declare no direct conflicts with this work. For unrelated conflicts, EAR, JMV, KS, EPH, PD, DR, RL, LGG-O, ML-Y, BCH, CF, AS, SWTPJH, AB, JWBdG, MAV and JVvT report no competing interests. BAvdW reports an advisory role for BMS. DvdB reports expert testimony and honoraria from Roche Diagnostics, both paid to the institution. JBAGH reports an advisory role for Achilles Therapeutics, BioNTech, Bristol-Myers Squibb, Immunocore, Instil Bio, Iovance Biotherapeutics, Ipsen, Molecular Partners, MSD Oncology, Neogene Therapeutics, Novartis, PokeAcel, Roche/Genentech, Sanofi, Third Rock Ventures and T-Knife; has received research funding, paid to the institute, from Amgen, Asher Biotherapeutics, BioNTech, Bristol-Myers Squibb, MSD, Neon Therapeutics, Novartis; and is stock owner of Neogene Therapeutics. SW reports serving on advisory boards for Eisai, Bristol-Myers Squibb, Pfizer, Novartis and Pierre Fabre all paid to the institution. CUB reports advisory roles for BMS, MSD, Roche, Novartis, GSK, AZ, Pfizer, Lilly, GenMab, Pierre Fabre, Third Rock Ventures, research funding from BMS, Novartis, Nanostring, and 4SC, co-founder, shareholder and advisor of Immagene B.V and co-founder of Signature Oncology.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data are available on reasonable request for academic use and within the limitations of the provided informed consent. Every request will be reviewed by the institutional review board of the NKI; the researcher will need to sign a data access agreement with the NKI after approval.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The full protocol, including one amendment and the informed consent form, were approved by the medical ethical committee of the Netherlands Cancer Institute - Antoni van Leeuwenhoek Hospital (METC-AVL) under the study identification number N15IMP. Participants gave written informed consent to participate in the study before registration.
References
- 1.Robert C, Grob JJ, Stroyakovskiy D, et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N Engl J Med 2019;381:626–36. 10.1056/NEJMoa1904059 [DOI] [PubMed] [Google Scholar]
- 2.Ascierto PA, McArthur GA, Dréno B, et al. Cobimetinib combined with vemurafenib in advanced BRAF(V600)-mutant melanoma (coBRIM): updated efficacy results from a randomised, double-blind, phase 3 trial. Lancet Oncol 2016;17:1248–60. 10.1016/S1470-2045(16)30122-X [DOI] [PubMed] [Google Scholar]
- 3.Ascierto PA, Dummer R, Gogas HJ, et al. Update on tolerability and overall survival in COLUMBUS: landmark analysis of a randomised phase 3 trial of encorafenib plus binimetinib vs vemurafenib or encorafenib in patients with BRAF V600-mutant melanoma. Eur J Cancer 2020;126:33–44. 10.1016/j.ejca.2019.11.016 [DOI] [PubMed] [Google Scholar]
- 4.Robert C, Ribas A, Schachter J, et al. Pembrolizumab versus ipilimumab in advanced melanoma (KEYNOTE-006): post-hoc 5-year results from an open-label, multicentre, randomised, controlled, phase 3 study. Lancet Oncol 2019;20:1239–51. 10.1016/S1470-2045(19)30388-2 [DOI] [PubMed] [Google Scholar]
- 5.Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 2019;381:1535–46. 10.1056/NEJMoa1910836 [DOI] [PubMed] [Google Scholar]
- 6.Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Long-term outcomes with nivolumab plus ipilimumab or nivolumab alone versus ipilimumab in patients with advanced melanoma. J Clin Oncol 2022;40:127–37. 10.1200/JCO.21.02229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hodi FS, Chiarion -Sileni V, Lewis KD, et al. Long-term survival in advanced melanoma for patients treated with nivolumab plus ipilimumab in checkmate 067. JCO 2022;40(16_suppl):9522. 10.1200/JCO.2022.40.16_suppl.9522 [DOI] [Google Scholar]
- 8.Robert L, Ribas A, Hu-Lieskovan S. Combining targeted therapy with immunotherapy. can 1+1 equal more than 2? Semin Immunol 2016;28:73–80. 10.1016/j.smim.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ribas A, Hodi FS, Callahan M, et al. Hepatotoxicity with combination of vemurafenib and ipilimumab. N Engl J Med 2013;368:1365–6. 10.1056/NEJMc1302338 [DOI] [PubMed] [Google Scholar]
- 10.Minor DR, Puzanov I, Callahan MK, et al. Severe gastrointestinal toxicity with administration of trametinib in combination with dabrafenib and ipilimumab. Pigment Cell Melanoma Res 2015;28:611–2. 10.1111/pcmr.12383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilmott JS, Long GV, Howle JR, et al. Selective BRAF inhibitors induce marked T-cell infiltration into human metastatic melanoma. Clin Cancer Res 2012;18:1386–94. 10.1158/1078-0432.CCR-11-2479 [DOI] [PubMed] [Google Scholar]
- 12.Kakavand H, Wilmott JS, Menzies AM, et al. PD-L1 expression and tumor-infiltrating lymphocytes define different Subsets of MAPK inhibitor-treated melanoma patients. Clin Cancer Res 2015;21:3140–8. 10.1158/1078-0432.CCR-14-2023 [DOI] [PubMed] [Google Scholar]
- 13.Frederick DT, Piris A, Cogdill AP, et al. BRAF inhibition is associated with enhanced melanoma antigen expression and a more favorable tumor microenvironment in patients with metastatic melanoma. Clin Cancer Res 2013;19:1225–31. 10.1158/1078-0432.CCR-12-1630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amaria RN, Prieto PA, Tetzlaff MT, et al. Neoadjuvant plus adjuvant dabrafenib and trametinib versus standard of care in patients with high-risk, surgically resectable melanoma: a single-centre, open-label, randomised, phase 2 trial. Lancet Oncol 2018;19:181–93. 10.1016/S1470-2045(18)30015-9 [DOI] [PubMed] [Google Scholar]
- 15.Hu-Lieskovan S, Mok S, Homet Moreno B, et al. Improved antitumor activity of immunotherapy with BRAF and MEK inhibitors in BRAF(V600E) melanoma. Sci Transl Med 2015;7:279ra41. 10.1126/scitranslmed.aaa4691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tumeh PC, Harview CL, Yearley JH, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 2014;515:568–71. 10.1038/nature13954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ayers M, Lunceford J, Nebozhyn M, et al. IFN-y-related mRNA profile predicts clinical response to PD-1 blockade. J Clin Invest 2017;127:2930–40. 10.1172/JCI91190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ribas A, Lawrence D, Atkinson V, et al. Combined BRAF and MEK inhibition with PD-1 blockade Immunotherapy in BRAF-mutant Melanoma. Nat Med 2019;25:936–40. 10.1038/s41591-019-0476-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ribas A, Butler M, Lutzky J, et al. Phase I study combining anti-PD-L1 (medi4736) with BRAF (Dabrafenib) and/or MEK (Trametinib) inhibitors in advanced Melanoma [abstract # 3003]. JCO 2015;33(15_suppl):3003. 10.1200/jco.2015.33.15_suppl.3003 [DOI] [Google Scholar]
- 20.Sullivan RJ, Hamid O, Gonzalez R, et al. Atezolizumab plus cobimetinib and vemurafenib in BRAF-mutated melanoma patients. Nat Med 2019;25:929–35. 10.1038/s41591-019-0474-7 [DOI] [PubMed] [Google Scholar]
- 21.Long GV, Lebbe C, Atkinson V, et al. The anti–PD-1 antibody Spartalizumab (S) in combination with Dabrafenib (D) and Trametinib (T) in previously untreated patients (Pts) with advanced BRAF V600–mutant Melanoma: updated efficacy and safety from parts 1 and 2 of COMBI-I. JCO 2019;37:9531. 10.1200/JCO.2019.37.15_suppl.9531 [DOI] [Google Scholar]
- 22.Deken MA, Gadiot J, Jordanova ES, et al. Targeting the MAPK and Pi3K pathways in combination with Pd1 blockade in melanoma. Oncoimmunology 2016;5:e1238557. 10.1080/2162402X.2016.1238557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 1975;31:103–15. [PubMed] [Google Scholar]
- 24.Jiang H, Lei R, Ding S-W, et al. Skewer: a fast and accurate adapter trimmer for next-generation sequencing paired-end reads. BMC Bioinformatics 2014;15:182. 10.1186/1471-2105-15-182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andrews S. FastQC, a quality control tool for high throughput sequence data. Cambridge, UK: Babraham Bioinformatics, Babraham Institute, 2010. [Google Scholar]
- 26.Liberzon A, Birger C, Thorvaldsdóttir H, et al. The molecular signatures database hallmark gene set collection. Cell Syst 2015;1:417–25. 10.1016/j.cels.2015.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vessies DCL, Linders TC, Lanfermeijer M, et al. An automated correction algorithm (ALPACA) for ddPCR data using adaptive limit of blank and correction of false positive events improves specificity of Mutation detection. Clin Chem 2021;67:959–67. 10.1093/clinchem/hvab040 [DOI] [PubMed] [Google Scholar]
- 28.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 29.Atkins MB, Lee SJ, Chmielowski B, et al. Combination dabrafenib and trametinib versus combination nivolumab and ipilimumab for patients with advanced BRAF-mutant melanoma: the dreamseq trial - ECOG-ACRIN Ea6134. J Clin Oncol 2023;41:186–97. 10.1200/JCO.22.01763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ascierto PA, Mandalà M, Ferrucci PF, et al. Sequencing of ipilimumab plus nivolumab and encorafenib plus binimetinib for untreated BRAF-mutated metastatic melanoma (SECOMBIT): a randomized, three-arm, open-label phase II trial. J Clin Oncol 2023;41:212–21. 10.1200/JCO.21.02961 [DOI] [PubMed] [Google Scholar]
- 31.Ascierto PA, Mandala M, Ferrucci PF, et al. Lba41 phase II study SECOMBIT (sequential combo immuno and target therapy study): 4-years OS data and preliminary biomarkers evaluation. Annals of Oncology 2022;33:S1408–9. 10.1016/j.annonc.2022.08.040 [DOI] [Google Scholar]
- 32.Dummer R, Long GV, Robert C, et al. Randomized phase III trial evaluating spartalizumab plus dabrafenib and trametinib for BRAF V600-mutant unresectable or metastatic melanoma. J Clin Oncol 2022;40:1428–38. 10.1200/JCO.21.01601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ferrucci PF, Di Giacomo AM, Del Vecchio M, et al. KEYNOTE-022 part 3: a randomized, double-blind, phase 2 study of pembrolizumab, dabrafenib, and trametinib in BRAF-mutant melanoma. J Immunother Cancer 2020;8:e001806. 10.1136/jitc-2020-001806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gutzmer R, Stroyakovskiy D, Gogas H, et al. Atezolizumab, vemurafenib, and cobimetinib as first-line treatment for unresectable advanced BRAFV600 mutation-positive melanoma (Imspire150): primary analysis of the randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2020;395:1835–44. 10.1016/S0140-6736(20)30934-X [DOI] [PubMed] [Google Scholar]
- 35.Schadendorf D, Dummer R, Robert C, et al. STARBOARD: encorafenib + binimetinib + pembrolizumab for first-line metastatic/unresectable BRAF V600-mutant melanoma. Future Oncol 2022;18:2041–51. 10.2217/fon-2021-1486 [DOI] [PubMed] [Google Scholar]
- 36.Garbe C, Amaral T, Peris K, et al. European consensus-based Interdisciplinary guideline for melanoma. part 2: treatment - update 2022. Eur J Cancer 2022;170:256–84. 10.1016/j.ejca.2022.04.018 [DOI] [PubMed] [Google Scholar]
- 37.Larkin J, et al. Efficacy of nivolumab plus ipilimumab combination in patients with advanced melanoma and elevated serum lactate dehydrogenase: a pooled analysis. Society for Melanoma Research (SMR) Congress, 2016. [Google Scholar]
- 38.Pires da Silva I, Ahmed T, McQuade JL, et al. Clinical models to define response and survival with anti–PD-1 antibodies alone or combined with ipilimumab in metastatic Melanoma. JCO 2022;40:1068–80. 10.1200/JCO.21.01701 [DOI] [PubMed] [Google Scholar]
- 39.Nosrati A, Tsai KK, Goldinger SM, et al. Evaluation of Clinicopathological factors in PD-1 response: derivation and validation of a prediction scale for response to PD-1 monotherapy. Br J Cancer 2017;116:1141–7. 10.1038/bjc.2017.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hamid O, Robert C, Daud A, et al. Five-year survival outcomes for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. Ann Oncol 2019;30:582–8. 10.1093/annonc/mdz011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stege H, Haist M, Schultheis M, et al. Discontinuation of BRAF/MEK-directed targeted therapy after complete remission of metastatic melanoma-a retrospective multicenter adoreg study. Cancers 2021;13:2312. 10.3390/cancers13102312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ascierto PA, Dummer R. Immunological effects of BRAF+MEK inhibition. Oncoimmunology 2018;7:e1468955. 10.1080/2162402X.2018.1468955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu C, Peng W, Xu C, et al. BRAF inhibition increases tumor infiltration by T cells and enhances the antitumor activity of adoptive immunotherapy in mice. Clin Cancer Res 2013;19:393–403. 10.1158/1078-0432.CCR-12-1626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee JH, Long GV, Boyd S, et al. Circulating tumour DNA predicts response to anti-Pd1 antibodies in metastatic melanoma. Ann Oncol 2017;28:1130–6. 10.1093/annonc/mdx026 [DOI] [PubMed] [Google Scholar]
- 45.Lipson EJ, Velculescu VE, Pritchard TS, et al. Circulating tumor DNA analysis as a real-time method for monitoring tumor burden in melanoma patients undergoing treatment with immune checkpoint blockade. J Immunother Cancer 2014;2:42. 10.1186/s40425-014-0042-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Herbreteau G, Vallée A, Knol A-C, et al. Quantitative monitoring of circulating tumor DNA predicts response of cutaneous metastatic melanoma to anti-Pd1 immunotherapy. Oncotarget 2018;9:25265–76. 10.18632/oncotarget.25404 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2023-006821supp002.pdf (910.4KB, pdf)
jitc-2023-006821supp001.pdf (540.4KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data are available on reasonable request for academic use and within the limitations of the provided informed consent. Every request will be reviewed by the institutional review board of the NKI; the researcher will need to sign a data access agreement with the NKI after approval.