Abstract
Objective:
This updated systematic review and meta-analysis aimed to assess maternal and fetal outcomes of pregnancies based on the Institute of Medicine (IOM) guidelines of gestational weight gain (GWG).
Methods:
PubMED, SCOPUS, EMBASE and Web of Science were searched up to 30th July 2022. All studies evaluating maternal and/or neonatal outcomes of twin pregnancies based on the IOM guidelines of gestational weight gain were included.
Results:
Twenty two studies were included. Mothers with twin pregnancies experiencing inadequate GWG showed higher incidence of gestational diabetes with the risk ratio (RR) 1.22 95% CI (0.95,1.57), p=0.0005, i2= 69% and premature rupture of membrane (PROM) with RR 1.14 95% CI (0.99, 1.30), p=0.07; i2=0% that coincided with higher rates of preterm birth, low birth weight, small for gestational age (SGA) and admission to NICU in neonates. Mothers with excessive GWG had higher risk of developing gestational hypertension with RR 1.59 95% CI (1.22, 2.07), p=0.0006, i2=75% and extremely preterm delivery (<32 weeks).
Conclusion:
Within the limitations of this review, GWG was found to be a predictable risk factor for adverse maternal and neonatal outcomes of twin pregnancies.
KEYWORDS: Twin pregnancy, Gestational weight gain, Meta-analysis, Maternal and neonatal outcomes
INTRODUCTION
Last two to three decades saw an increase in the incidences of twin pregnancies1 that are associated with almost 2.5 times higher in-utero mortality and four times higher first-year mortality compared to singleton pregnancies.2,3 According to the statistics, twins make up 3.2% of all births but account for more than 20% of the burden of preterm birth.4 Twin pregnancies put women at higher risk of pre-eclampsia, incidence of gestational diabetes, premature delivery by rupture of membrane, increased risk of caesarean delivery, etc.5,6 Poor neonatal outcomes that are associated with twin pregnancies include low pre-term birth weight, small for gestational age (SGA) neonates due to restricted fetal growth, perinatal death, and increased need of Neonatal intensive care unit (NICU) admission.7 These complications are governed mainly by amount of gestational weight gained by mothers during their pregnancy.8
Therefore, the Institute of Medicine (IOM) developed detailed guidelines that define the optimal weight gain for twin pregnancies.9 Since the gestational weight gain (GWG) is an easily modifiable factor, controlling it may potentially prevent complications related to adverse outcomes for pregnant women and neonates. Two prior meta-analyses summarized existing analyses of the influence of gestational weight gain on women with twin pregnancies, but the number of included studies was small (11 to 14 studies). Study by Zhong et al. 202110 included 11 reports and concluded that inadequate weight gain in mothers with twin pregnancy led to increased risk of gestational diabetes, reduced risk of hypertension and cesarean delivery among mothers and increased risk of delivery before term, low birthweight (PTLBW), SGA and neonatal intensive unit (NICU) admission. Excessive weight gain was also associated with elevated risk of pre-eclampsia and cesarean section. Study by Lipworth et al. 202211 included 14 manuscripts and concluded that inadequate weight gain leads to fetal growth restriction, and high weight gain leads to gestational diabetes and pre-eclampsia. Current study aims to review new reports that were published over the last two years and to conduct an updated systematic review and meta-analysis to assess maternal and fetal outcomes of twin pregnancies based on the IOM guidelines of GWG.
METHODS
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 guidelines12 were followed. The protocol of the review was registered at PROSPERO, (CRD42022348819).
Search Strategy:
PubMED, SCOPUS, EMBASE and Web of Science were searched up to 30th July 2022, using relevant keywords: “gestational weight gain”, “twin pregnancy”, “multiple pregnancy”, “maternal outcomes”, “neonatal outcomes”, “pre-natal”, “peri-natal”, “post-natal”. The search strategy used is as follows: ((“gestational weight gain”[All Fields]) AND ((((“twin pregnancy”) OR (“multiple pregnancy”)) OR (double)) OR (twins))) AND ((maternal outcome) OR (neonatal outcome)). Additionally, bibliography of previous systematic reviews and meta-analyses were thoroughly screened for any potentially eligible articles. The citations were deduplicates. Titles and abstracts of the final set of citations were thoroughly screened for eligibility based on relevancy. Full text analysis of the selected studies was then done by the two reviewers based on predefined eligibility criteria. (Supplementary Table-I)
Supplementary Table-I.
Eligibilty Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Studies that evaluated maternal and/or neonatal outcomes of twin pregnancies | Studies that only included singleton pregnancies or pregnancies with higher-order multiples |
| Studies that included women who were pregnant with twins | Studies that did not report on GWG in twin pregnancies or used a different reference for assessing GWG |
| Studies that used the Institute of Medicine (IOM) guidelines for gestational weight gain (GWG) as a reference for assessing GWG in twin pregnancies | Studies that focused solely on the effect of maternal BMI or other factors on pregnancy outcomes, without reporting on the relationship between GWG and outcomes in twin pregnancies |
| Studies that reported on the association between GWG and maternal and/or neonatal outcomes in twin pregnancies | Studies that were not peer-reviewed or were published as conference abstracts, case reports, or letters to the editor |
| Studies that were published in English | Studies that only included singleton pregnancies or pregnancies with higher-order multiples |
Eligibility Criteria:
All studies evaluating outcomes (both for mothers and neonates) of twin pregnancies based on the IOM guidelines of GWG were included. Studies not reporting relevant outcomes and not following the IOM guideline criteria were excluded.
Data Collection & Quality assessment:
The data were collected by the two reviewers and the information was fed into the excel spreadsheet (Microsoft Office 365, 2020 version, Microsoft, USA). The study characteristics included demographic data such as study design, duration, and setting, sample size, assessed outcomes, Body mass index (BMI) stratification, GWG and number of participants per group. The maternal outcomes i.e., incidence of gestational diabetes, gestation hypertension, caesarean delivery, post-partum hemorrhage, PROM and neonatal outcomes like pre-term birth at 37 and 32 weeks, SGA, low birth weight (less than 2500gm), and admission to NICU, whichever available, were collected. Quality of the included studies was assessed by the New-castle Ottawa Scale (NOS).13
Data Analysis:
The maternal and neonatal outcomes data were dichotomous and combined to generate pooled risk ratio (RR) with 95% confidence interval (CI) using RevMan (Review Manager software). The heterogeneity among the included studies were calculated using I2 statistics. A sensitivity analysis was performed to check influence of each study on the outcome.
RESULTS
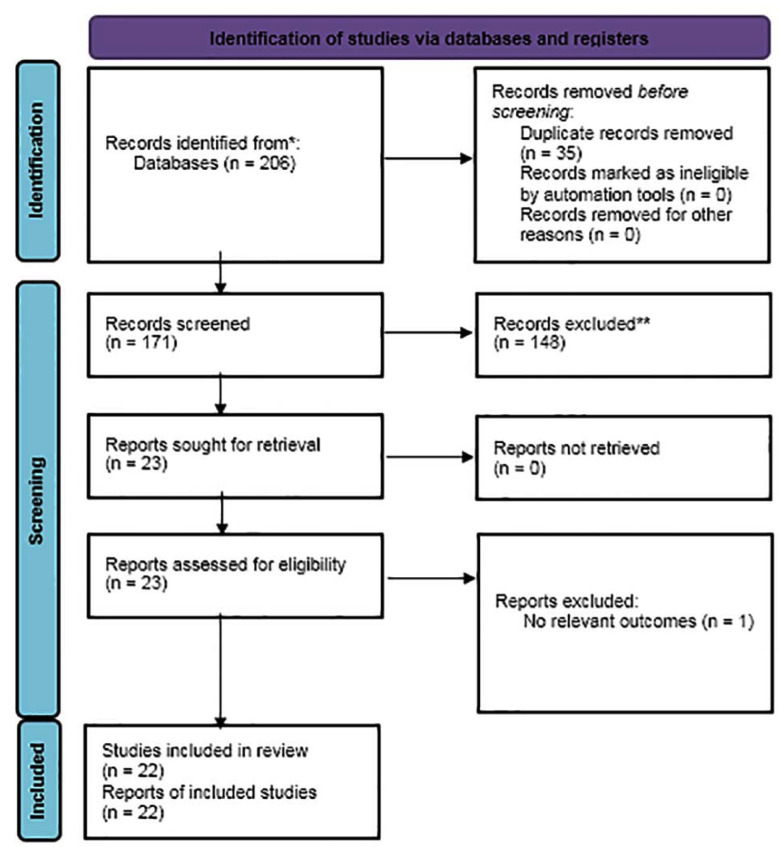
A total of 22 studies14–35 were included in this review. The comprehensive search of digital databases and hand search identified a total of 206 citations. Duplicates were removed and title and abstract of the remaining 171 citations were reviewed. Finally, full text assessment was done on 23 records, of which, twenty-two studies were finally included in the current review.(Supplementary Fig.1)
Supplementary Fig.1.
PRISMA flow chart depicting the study selection process.
All the included studies were retrospective in design. Data on total of 74222 mothers with twin pregnancy were reported. Of them, 43,765 mothers had inadequate GWG below IOM range of weight gain and 30,457 mothers had excessive GWG above the IOM range. In few studies participants were also stratified according to BMI. As summarized in Table-I, a total of 4567 mothers were under-weight, 16789 were of normal weight, 15678 were overweight and 6546 were obese. The mean age of the included mothers was 25.6±7.7 years. All included studies were of good quality.(Supplementary Table-II)
Table-I.
Demographic characteristics of included studies
| SL. No. | Author | Year | Study design | Study Duration | No. of Women | GWG | NOS score | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Below IOM | Above IOM | |||||||
| 1 | Lin et al. | 2022 | Retrospective study | 2014 to 2018 | 931 | 309 | 269 | 8 |
| 2 | Maeda et al. | 2022 | Retrospective study | 2007 to 2015 | NW-17973, UW-4394 | UW-11.79(4.64), NW-11.49(4.83) | ||
| 3 | Lipworth et al. | 2021 | Retrospective cohort study | 2000 to 2014 | 1274 (UW-43, NW-777, OW-278, Obese-176) | UW-14(33), NW-238(31), OW-71(26), Obese-58(33) | UW-4(9), NW-121(16), OW-61(22), Obese-30(17) | 8 |
| 4 | Liu et al. | 2021 | Retrospective cohort study | 2005 to 2017 | 609 | 223 | NR | 7 |
| 5 | Choi et al. | 2020 | Retrospective study | 2005 to 2019 | 1738 | 881 | 163 | 8 |
| 6 | Shimura et al | 2020 | Retrospective study | 2006 to 2018 | 265 | 226 | NR | 8 |
| 7 | Bodnar et al. | 2019 | population-based cohort study | 2003 to 2013 | 27.723 | 17+/-8.5 | ||
| 8 | Lin et al. | 2019 | Retrospective cohort study | 2015 to 2018 | 645 | 97 | 281 | 8 |
| 9 | Pecheux et al. | 2019 | Retrospective cohort study | 1997 to 2013 | 878 | 468 | 64 | 8 |
| 10 | Algeri et al. | 2018 | Retrospective cohort study | 2010 to 2013 | 175 | 91 | 11 | 9 |
| 11 | Wang et al. | 2018 | Retrospective cohort study | 2015 to 2016 | 350 | 145 | 35 | 8 |
| 12 | Kosinska-Kaczynska et al. | 2017 | Prospective cohort study | 2007 to 2016 | 295 | 77 | 25 | 8 |
| 13 | Lutsiv et al. | 2017 | Retrospective cohort study | 2003 to 2014 | 741 | 201 | 220 | 7 |
| 14 | Ozcan et al. | 2016 | Retrospective cohort study | 2004 to 2014 | 5897 | NR | NR | 7 |
| 15 | Pettit et al. | 2015 | Retrospective cohort study | 2001 to 2014 | 489 | NR | 203 | 8 |
| 16 | Lal et al. | 2015 | Retrospective cohort study | 2002 to 2008 | 2654 | 1040 | 517 | 7 |
| 17 | Shamshiraz et al. | 2014 | Retrospective cohort study | 1991 to 2011 | 570 | NR | NR | 8 |
| 18 | Pettit et al. | 2014 | Retrospective cohort study | 2001 to 2013 | 489 | 93 | NR | 8 |
| 19 | Gavard et al. | 2014 | Population-based historical cohort study | 1998 to 2005 | 831 | 256 | 252 | 8 |
| 20 | Gonzalez-Quintero et al. | 2012 | Retrospective study | 5129 | n=1366; 23.4+/- 8.4 pounds | n=1646; 47.7 +/-13.3 pounds | 8 | |
| 21 | Fox et al. | 2011 | Retrospective cohort study | 2005 to 2010 | 170 | 55 | 39 | 9 |
| 22 | Fox et al. | 2010 | Cohort study | 2005 to 2009 | 297 | 105 | NR | 8 |
Supplementary Table II.
Quality of included studies.
| Study | Year | Selection | Comparability | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Representativeness of the exposed cohort | Selection of the nonexposed cohort | Ascertainment of exposure | Demonstration that outcome of interest | Basis of the design or analysis | Assessment of outcome | follow-up long enough for outcomes | Adequate follow up | Total | ||
| Lin et al. | 2022 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Maeda et al. | 2022 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Lipworth et al. | 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Liu et al. | 2021 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Choi et al. | 2020 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Shimura et al | 2020 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Bodnar et al. | 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Lin et al. | 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Pecheux et al. | 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Algeri et al. | 2018 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Wang et al. | 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Lutsiv et al. | 2017 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Ozcan et al. | 2016 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Pettit et al. | 2015 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Lal et al. | 2015 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Shamshiraz et al. | 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Pettit et al. | 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Gavard et al. | 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Gonzalez-Quintero et al. | 2012 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Fox et al. | 2011 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Fox et al. | 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
Meta-Analysis:
Inadequate GWG versus Adequate GWG:
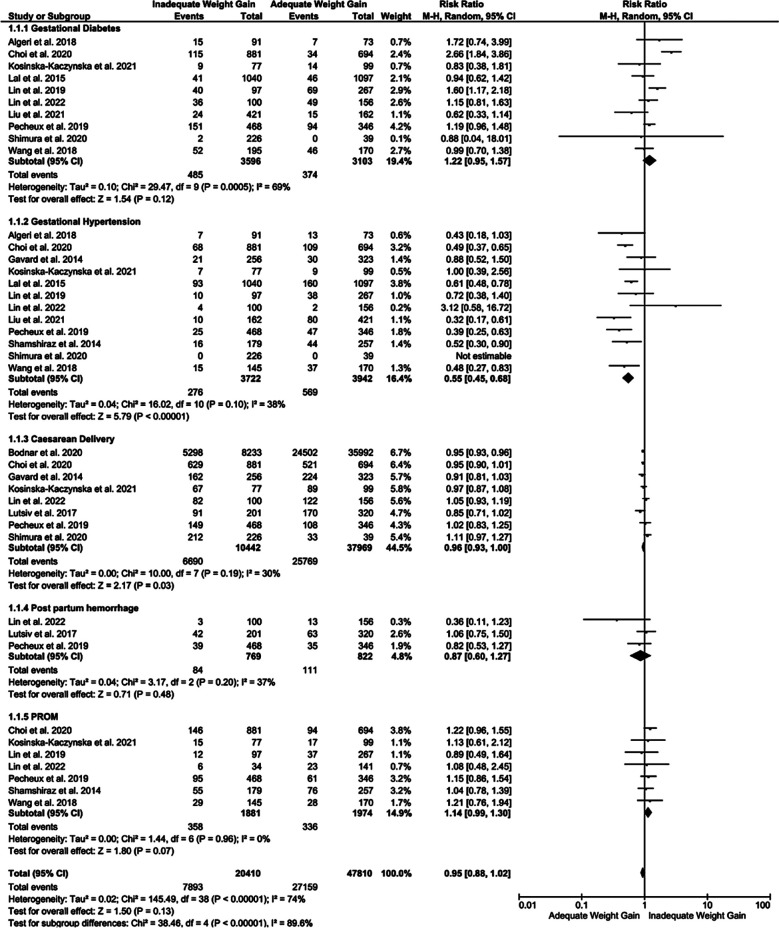
Inadequate GWG correlated with higher incidence of gestational diabetes in women with twin pregnancies (RR 1.22, 95% CI [0.95,1.57], p=0.0005) with moderate heterogeneity (i2= 69%). However, the risk of developing gestational hypertension was low among the mothers with twin pregnancy with inadequate GWG, with RR of 0.55 95% CI [0.45,0.68], p<0.0001, i2=38%. Inadequate GWG also correlated with lower risk of caesarian delivery compared to mothers with adequate GWG (RR of 0.96). There was no difference in the effect estimate for post-partum hemorrhage between mothers with inadequate GWG compared to adequate GWG with RR 0.87 95% CI [0.60,1.27], p=0.48. As shown in Fig.1, the incidence of PROM was also higher in women with twin pregnancies with inadequate GWG (RR of 1.14 95% CI [0.99, 1.30], p=0.07; i2=0%).
Fig.1.
Forest plot showing comparison of maternal outcomes among the mothers with twin pregnancy showing inadequate or adequate GWG.
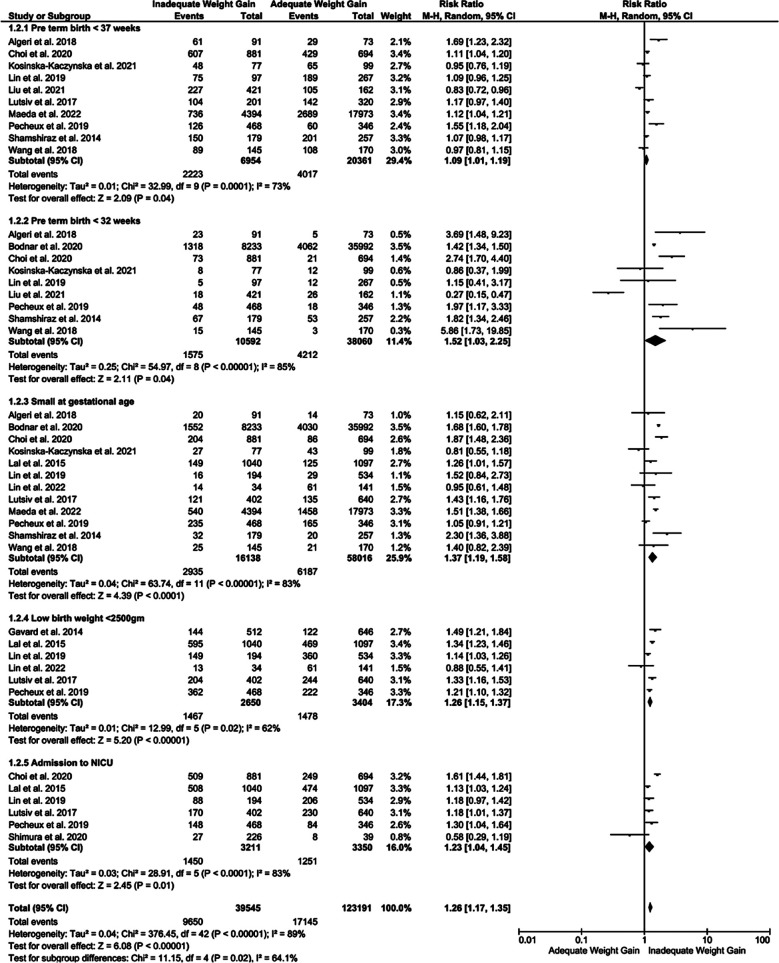
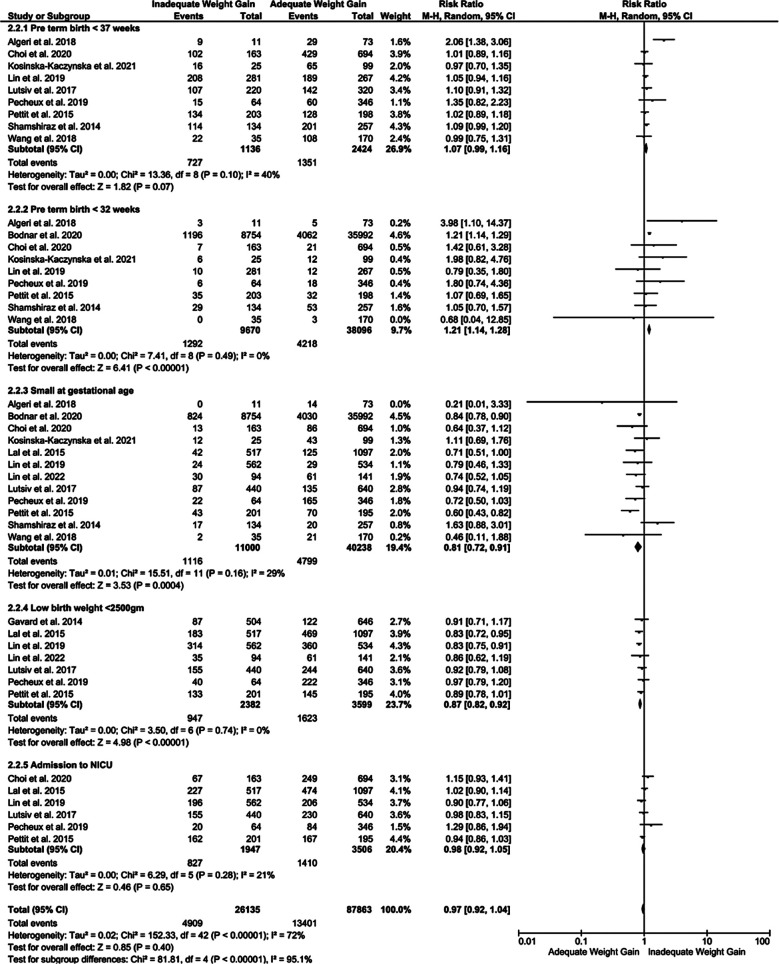
In terms of the neonatal outcomes, women with inadequate GWG were at higher risk of preterm (<37 weeks) and very preterm (<32 weeks) delivery with RR 1.09 (p=0.04) and RR 1.52 (p=0.04), respectively. Similarly, risk of SGA, low birth weight neonates (<2500 gm) and risk of neonatal admission to NICU immediately after birth was higher [RR 1.37 (p<0.001), 1.26 (p<0.001) and 1.23 (p<0.02)], respectively, in cases of inadequate GWG compared adequate GWG (Fig.2).
Fig.2.
Forest plot showing comparison of neonatal outcomes among the mothers with twin pregnancy showing inadequate or adequate GWG.
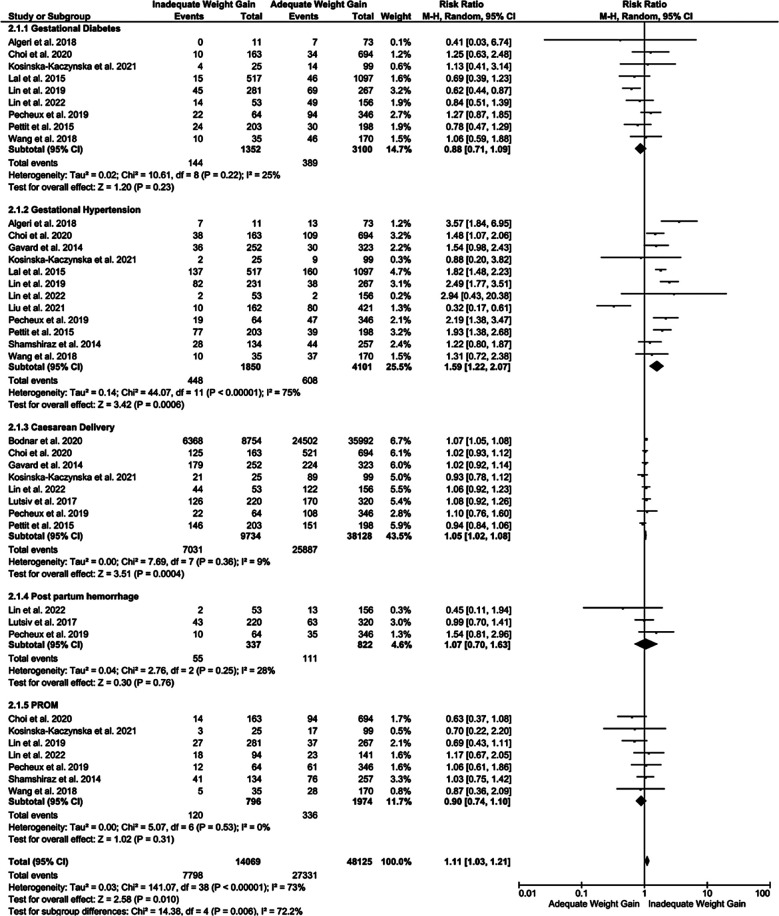
Excessive GWG versus Adequate GWG:
The risk of developing gestational hypertension was higher among mothers with twin pregnancy with excessive GWG [RR of 1.59 95% CI [1.22, 2.07], p=0.0006, i2=75%], compared to mothers with adequate GWG. However, no major difference was observed in the incidence of gestational diabetes, caesarean delivery, post-partum hemorrhage and PROM (Fig.3).
Fig.3.
Forest plot showing comparison of maternal outcomes among the mothers with twin pregnancy showing excessive or adequate GWG.
Excessive GWG in mother with twin pregnancy correlated with significantly higher incidence of very preterm (<32 weeks) birth [RR of 1.21 95% CI [1.14, 1.28], p<0.0001, i2=0%], compared to women with adequate GWH. The rate of preterm delivery (< 37 weeks) and admission to NICU was similar between the groups. Additionally, the risk of delivering SGA and low birth weight neonates was also low (RR 0.81 and 0.87 respectively) in mothers with twin pregnancy and excessive GWG compared to adequate GWG (Fig.4). Sensitivity analysis identified the outliers which could possibly change the effect estimate based on their weight. (Refer Supplementary Table-III).
Fig.4.
Forest plot showing comparison of neonatal outcomes among the mothers with twin pregnancy showing excessive or adequate GWG.
Supplementary Table-III.
Sensitivity analysis of the effect estimate of each outcome by toggling through each included study.
| Outcomes | Studies included | Change in significance of RR | ||
|---|---|---|---|---|
| 1 | Comparison of outcomes between Inadequate GWG versus Adequate GWG in twin mothers | |||
| 1.1 | Maternal Outcomes | |||
| 1.1.1 | Gestational Diabetes | 9 | Removing other studies | No Major Change |
| Removing Liu et al. 2021 | 1.30 [1.01, 1.66], p=0.04 | |||
| 1.1.2 | Gestational Hypertension | 12 | Removing each study | No Major Change |
| 1.1.3 | Caesarean Delivery | 8 | Removing Other studies | No Major Change |
| Removing Bodnar et al. 2020 | 0.97 [0.92, 1.03], p=0.37 | |||
| Removing Choi et al. 2020 | 0.97 [0.92, 1.02], p=0.23 | |||
| Removing Shimura et al. 2020 | 0.95 [0.93, 0.96], p<0.0001 | |||
| 1.1.4 | Post-partum haemorrhage | 3 | Removing each study | No Major Change |
| 1.1.5 | Premature rupture of membrane | 6 | Removing other studies | No Major Change |
| Removing Lin et al. 2019 | 1.15 [1.00, 1.33], p=0.05 | |||
| 1.2 | Neonatal Outcomes | |||
| 1.2.1 | Pre-term birth <37 weeks | 10 | Removing each study | No Major Change |
| 1.2.2 | Pre-term birth <32 weeks | 8 | Removing other studies | No Major Change |
| Removing Liu et al. 2021 | 1.87 [1.40, 2.50], p<0.0001 | |||
| 1.2.3 | Small at Gestational Age | 12 | Removing each study | No Major Change |
| 1.2.4 | Low birth weight <2500gm | 6 | Removing each study | No Major Change |
| 1.2.5 | Admission to NICU | 6 | Removing each study | No Major Change |
| 2 | Comparison of outcomes between Excessive GWG versus Adequate GWG in twin mothers | |||
| 2.1 | Maternal Outcomes | |||
| 2.1.1 | Gestational Diabetes | 9 | Removing other studies | No Major Change |
| Removing Pecheux et al. 2019 | 0.78 [0.64, 0.95], p<0.01 | |||
| 2.1.2 | Gestational Hypertension | 12 | Removing each study | No Major Change |
| 2.1.3 | Caesarean Delivery | 8 | Removing Other studies | No Major Change |
| Removing Bodnar et al. 2020 | 1.05 [1.02, 1.08], p=0.0004 | |||
| 2.1.4 | Post-partum haemorrhage | 3 | Removing each study | No Major Change |
| 2.1.5 | Premature rupture of membrane | 7 | Removing each study | No Major Change |
| 2.2 | Neonatal Outcomes | |||
| 2.2.1 | Pre-term birth <37 weeks | 9 | Removing each study | No Major Change |
| 2.2.2 | Pre-term birth <32 weeks | 9 | Removing each study | No Major Change |
| 2.2.3 | Small at Gestational Age | 12 | Removing each study | No Major Change |
| 2.2.4 | Low birth weight <2500gm | 7 | Removing each study | No Major Change |
| 2.2.5 | Admission to NICU | 6 | Removing each study | No Major Change |
DISCUSSION
Our study aimed to evaluate the maternal and neonatal outcomes of twin pregnancies in women with inadequate or excessive GWG compared to the normal range of GWG as delineated by the IOM guidelines for twin pregnancy. The results of this systematic review were derived from the pooled estimate of twenty-one studies reporting maternal and neonatal outcomes, with two or more studies available for each outcome. Our result showed increased rates of gestational diabetes and PROM in mothers with twin pregnancies and inadequate GWG. Additionally, neonates from mothers with twin pregnancies and inadequate GWG had higher risk of being delivered preterm (at less than 37 and 32 weeks), being SGA, and low birth weight. Inadequate GMG coincided with higher rate of neonatal admission to NICU at birth. Mothers with twin pregnancies and excessive GWG has higher risk of developing gestational hypertension. Additionally, excessive GWG was associated with slightly higher (but not statistically significant) risks of cesarean delivery and post-partum hemorrhage.
Inadequate GWG is typically associated with nutritional deficiencies, insufficient plasma volume expansion, and metabolic state that could prevent the weight gain.36 These factors may also increase the risk of infection or inflammation. The state of nutritional deficiency increases women’s susceptibility to a wide range of infection, which may directly or indirectly affect the maternal and fetal outcomes.37 The state of long-term infection in mothers with inadequate GWG may lead to the risk of preterm delivery due to early oxytocin release in the presence of pro-inflammatory cytokines. In addition, this state of surge in inflammatory cytokines is also responsible for the release of certain proteins and interleukins which inhibit the insulin signaling pathways, interfering with the insulin release and leading to potentially elevated blood sugar levels and gestational diabetes.38
Excessive GWG also possesses a risk for pro-inflammatory state in mothers due to the release of pro-inflammatory cytokines from adipocytes. The increase in the acute phase reactants and pro-inflammatory cytokines could induce PROMs and vasoconstriction, leading to relative rise in the blood pressure. Therefore, excessive GWG in mothers with high BMI may result in a state of preeclampsia, where the blood pressure rises abnormally, leading to various complications.39
The results of our updated systematic review and meta-analysis confirm findings of previous systematic reviews by Zhong et al.10particularly in singleton pregnancies, has been well-linked with maternal and infant outcomes. The aim of the current meta-analysis was to evaluate the effects of gestational weight gain on maternal and fetal outcomes in women with twin pregnancies., Methods: A systematic search was conducted using the PubMed, Scopus, and Google Scholar databases. Studies, either retrospective or prospective in design, evaluating the effects of gestational weight gain (defined using Institute of Medicine (IOM and Lipworth et al.11 Study by Zhong et al.10particularly in singleton pregnancies, has been well-linked with maternal and infant outcomes. The aim of the current meta-analysis was to evaluate the effects of gestational weight gain on maternal and fetal outcomes in women with twin pregnancies., Methods: A systematic search was conducted using the PubMed, Scopus, and Google Scholar databases. Studies, either retrospective or prospective in design, evaluating the effects of gestational weight gain (defined using Institute of Medicine (IOM included eleven papers and concluded that inadequate weight gain in mothers with twin pregnancy led to increased risk of gestational diabetes, reduced risk of hypertension and cesarean delivery among mothers and increased risk of PTLBW38, SGA and NICU admission in neonates. Moreover, excessive weight gain was associated with increased risk of preeclampsia and cesarean delivery. Lipworth et al.11 included fourteen studies and concluded that inadequate weight gain led to fetal growth restriction and high weight gain lead to gestational diabetes and preeclampsia.
Limitations:
All included studies were retrospective observational with low number of participants. Moreover, most of the included studies did not take into account variables such as BMI, age, chorionicity of twins, assisted reproductive technologies, accessibility to medical facilities etc that can potentially be cofounding. The BMI of mothers prior to gestation is an important risk factor in the mothers with twin pregnancy.39 The attempt of BMI stratification was carried out to provide a more comprehensive result based on prepartum BMI. Few studies had a clear distinction of underweight, normal weight, overweight and obese mothers. However, the results provided by these studies were not stratified accordingly.
Therefore, we did not attempt a sub-group analysis based on BMI. The number of included studies was not enough to justify the use of subgroup analysis in rest of the outcomes with most of the outcomes included in one study. Other potential confounding factors that could have influenced the results of the included studies include maternal age, parity, ethnicity, and socioeconomic status, as well as the number and chorionicity of the twin fetuses. These factors have been shown to be associated with GWG and pregnancy outcomes in general, and may also be relevant in the context of twin pregnancies.
The age of the mothers with twin pregnancy and chorionicity of twins are also among risk factors which have to be considered while evaluating these maternal and neonatal outcomes. Additionally, the included studies varied in terms of their study design, sample size, and methodological quality, which could have also affected the results. For example, some studies may have had a higher risk of bias due to incomplete outcome reporting or confounding factors that were not adequately controlled for. Further prospective and other observational studies are required to strengthen the evidence by considering the limitations mentioned above.
CONCLUSION
GWG was found to be a predictable risk factor for adverse maternal and neonatal outcomes in mothers with twin pregnancies. Inadequate GWG correlated with increased rates of gestational diabetes and PROM in women with twin pregnancies, as well as preterm birth, low birth weight, SGA and admission to NICU in neonates. Women with excessive GWG had higher risk of developing gestational hypertension and very preterm (at <32 weeks) delivery. As GWG is a potentially modifiable factor, mothers with twin pregnancies should be counselled on the importance of optimal GWG to prevent potential adverse maternal and fetal/neonatal outcomes. Healthcare providers should educate mothers on the IOM guidelines for GWG and provide individualized recommendations based on their pre-pregnancy BMI and other relevant factors. Regular monitoring of weight gain during prenatal visits can also help identify mothers who may be at risk of inadequate or excessive GWG and provide appropriate interventions.
Authors’ contributions:
XW conceived and designed the study.
MY, ZX and LZ collected the data and performed the analysis.
XW was involved in the writing of the manuscript and is responsible for the integrity of the study.
All authors have read and approved the final manuscript.
REFERENCES
- 1.Monden C, Pison G, Smits J. Twin Peaks:more twinning in humans than ever before. Hum Reprod. 2021;36(6):1666–1673. doi: 10.1093/humrep/deab029. doi:10.1093/humrep/deab029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santana DS, Silveira C, Costa ML, Souza RT, Surita FG, Souza JP, et al. Perinatal outcomes in twin pregnancies complicated by maternal morbidity:evidence from the WHO Multicountry Survey on Maternal and Newborn Health. BMC Pregnancy Childbirth. 2018;18:449. doi: 10.1186/s12884-018-2082-9. doi:10.1186/s12884-018-2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The ESHRE Capri Workshop Group. Multiple gestation pregnancy. Hum Reprod. 2000;15(8):1856–1864. doi:10.1093/humrep/15.8.1856. [PubMed] [Google Scholar]
- 4.Roman A, Ramirez A, Fox NS. Screening for preterm birth in twin pregnancies. Am J Obstet Gynecol MFM. 2022;4(2S):100531. doi: 10.1016/j.ajogmf.2021.100551. doi:10.1016/j.ajogmf.2021.100531. [DOI] [PubMed] [Google Scholar]
- 5.Li S, Gao J, Liu J, Hu J, Chen X, He J, et al. Perinatal Outcomes and Risk Factors for Preterm Birth in Twin Pregnancies in a Chinese Population:A Multi-center Retrospective Study. Front Med. 2021. [Accessed September 21, 2022]. p. 8. https: //www.frontiersin.org/articles/10.3389/fmed.2021.657862 . [DOI] [PMC free article] [PubMed]
- 6.Zhou S, Yang Y, Zhang X, Mu X, Quan Q, Zhong Q, et al. Perinatal outcomes of twin pregnancies with preterm premature rupture of the membranes at 24-34 weeks'gestation. Sci Rep. 2021;11:23419. doi: 10.1038/s41598-021-02884-x. doi:10.1038/s41598-021-02884-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Refuerzo JS, Momirova V, Peaceman AM, Sciscione A, Rouse DJ, Caritis SN, et al. Neonatal Outcomes in Twin Pregnancies Delivered Moderately Preterm, Late Preterm and Term. Am J Perinatol. 2010;27(7):537–542. doi: 10.1055/s-0030-1248940. doi:10.1055/s-0030-1248940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kominiarek MA, Peaceman AM. Gestational weight gain. Am J Obstet Gynecol. 2017;217(6):642–651. doi: 10.1016/j.ajog.2017.05.040. doi:10.1016/j.ajog.2017.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine (US) Committee on Nutritional Status during Pregnancy and Lactation. Nutrition During Pregnancy:Part I Weight Gain:Part II Nutrient Supplements. National Academies Press (US) 1990. [Accessed September 21, 2022]. http: //www.ncbi.nlm.nih.gov/books/NBK235228/ [PubMed]
- 10.Zhong W, Fan X, Hu F, Chen M, Zeng F. Gestational Weight Gain and Its Effects on Maternal and Neonatal Outcome in Women With Twin Pregnancies:A Systematic Review and Meta-Analysis. Front Pediatr. 2021;9:674414. doi: 10.3389/fped.2021.674414. doi:10.3389/fped.2021.674414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lipworth H, Barrett J, Murphy K, Redelmeier D, Melamed N. Gestational weight gain in twin gestations and pregnancy outcomes:a systematic review and meta-analysis. BJOG Int J Obstet Gynaecol. 2022;129(6):868–879. doi: 10.1111/1471-0528.17011. doi:10.1111/1471-0528.17011. [DOI] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions:explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. doi:10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. doi:10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 14.Lin LH, Weng YL, Lin YY, Huang XX, Lin Y, Xiu XY, et al. Examining the effects of second-and third-trimester gestational weight gain rates on the perinatal outcomes among Chinese twin pregnancies:a retrospective cohort study. BMC Pregnancy Childbirth. 2022;22(1):137. doi: 10.1186/s12884-022-04467-8. doi:10.1186/s12884-022-04467-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maeda Y, Ogawa K, Morisaki N, Sago H. The association between gestational weight gain and perinatal outcomes among underweight women with twin pregnancy in Japan. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. doi: 10.1002/ijgo.14122. Published online January 30, 2022. doi:10.1002/ijgo.14122. [DOI] [PubMed] [Google Scholar]
- 16.Lipworth H, Melamed N, Berger H, Geary M, McDonald SD, Murray-Davis B, et al. Maternal weight gain and pregnancy outcomes in twin gestations. Am J Obstet Gynecol. 2021;225(5):532.e1–532.e12. doi: 10.1016/j.ajog.2021.04.260. doi:10.1016/j.ajog.2021.04.260. [DOI] [PubMed] [Google Scholar]
- 17.Liu LY, Zafman KB, Fox NS. The Association between Gestational Weight Gain in Each Trimester and Pregnancy Outcomes in Twin Pregnancies. Am J Perinatol. 2021;38(6):567–574. doi: 10.1055/s-0039-1700853. doi:10.1055/s-0039-1700853. [DOI] [PubMed] [Google Scholar]
- 18.Shimura M, Obata S, Misumi T, Miyagi E, Aoki S. Are the Institute of Medicine guidelines for optimal gestational weight gain in twin pregnancies applicable to Japanese women? J Obstet Gynaecol Res. 2021;47(1):337–342. doi: 10.1111/jog.14529. doi:10.1111/jog.14529. [DOI] [PubMed] [Google Scholar]
- 19.Choi BY, Hong S, Jeon M, Park JY, Oh KJ, Hong JS. Gestational weight gain in twin pregnancies in Korea:application of the 2009 Institute of Medicine recommendations. Obstet Gynecol Sci. 2020;63(6):690–699. doi: 10.5468/ogs.20133. doi:10.5468/ogs.20133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bodnar LM, Himes KP, Abrams B, Lash TL, Parisi SM, Eckhardt CL, et al. Gestational Weight Gain and Adverse Birth Outcomes in Twin Pregnancies. Obstet Gynecol. 2019;134(5):1075–1086. doi: 10.1097/AOG.0000000000003504. doi:10.1097/AOG.0000000000003504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin D, Fan D, Wu S, Chen G, Li P, Ma H, et al. The effect of gestational weight gain on perinatal outcomes among Chinese twin gestations based on Institute of Medicine guidelines. BMC Pregnancy Childbirth. 2019;19(1):262. doi: 10.1186/s12884-019-2411-7. doi:10.1186/s12884-019-2411-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pécheux O, Garabedian C, Drumez E, Mizrahi S, Cordiez S, Deltomber S, et al. Maternal and neonatal outcomes according to gestational weight gain in twin pregnancies:Are the Institute of Medicine guidelines associated with better outcomes? Eur J Obstet Gynecol Reprod Biol. 2019;234:190–194. doi: 10.1016/j.ejogrb.2019.01.010. doi:10.1016/j.ejogrb.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 23.Wang L, Wen L, Zheng Y, Zhou W, Mei L, Li H, et al. Association Between Gestational Weight Gain and Pregnancy Complications or Adverse Delivery Outcomes in Chinese Han Dichorionic Twin Pregnancies:Validation of the Institute of Medicine (IOM) 2009 Guidelines. Med Sci Monit Int Med J Exp Clin Res. 2018:24. doi: 10.12659/MSM.911784. doi:10.12659/MSM.911784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Algeri P, Pelizzoni F, Bernasconi DP, Russo F, Incerti M, Cozzolino S, et al. Influence of weight gain, according to Institute of Medicine 2009 recommendation, on spontaneous preterm delivery in twin pregnancies. BMC Pregnancy Childbirth. 2018;18(1):6. doi: 10.1186/s12884-017-1645-5. doi:10.1186/s12884-017-1645-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lutsiv O, Hulman A, Woolcott C, Beyene J, Giglia L, Armson BA, et al. Examining the provisional guidelines for weight gain in twin pregnancies:a retrospective cohort study. BMC Pregnancy Childbirth. 2017;17(1):330. doi: 10.1186/s12884-017-1530-2. doi:10.1186/s12884-017-1530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ozcan T, Bacak SJ, Zozzaro-Smith P, Li D, Sagcan S, Seligman N, et al. Assessing Weight Gain by the 2009 Institute of Medicine Guidelines and Perinatal Outcomes in Twin Pregnancy. Matern Child Health J. 2017;21(3):509–515. doi: 10.1007/s10995-016-2134-6. doi:10.1007/s10995-016-2134-6. [DOI] [PubMed] [Google Scholar]
- 27.Kosinska-Kaczynska K, Szymusik I, Kaczynski B, Wielgos M. Observational study of associations between gestational weight gain and perinatal outcomes in dichorionic twin pregnancies. Int J Gynecol Obstet. 2017;138(1):94–99. doi: 10.1002/ijgo.12171. doi:10.1002/ijgo.12171. [DOI] [PubMed] [Google Scholar]
- 28.Pettit KE, Lacoursiere DY, Schrimmer DB, Alblewi H, Moore TR, Ramos GA. Maternal and neonatal outcomes in women with twin pregnancies with excessive gestational weight gain. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2016;29(13):2182–2185. doi: 10.3109/14767058.2015.1079613. doi:10.3109/14767058.2015.1079613. [DOI] [PubMed] [Google Scholar]
- 29.Lal AK, Kominiarek MA. Weight gain in twin gestations:are the Institute of Medicine guidelines optimal for neonatal outcomes? J Perinatol Off J Calif Perinat Assoc. 2015;35(6):405–410. doi: 10.1038/jp.2014.237. doi:10.1038/jp.2014.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pettit KE, Lacoursiere DY, Schrimmer DB, Alblewi H, Moore TR, Ramos GA. The association of inadequate mid-pregnancy weight gain and preterm birth in twin pregnancies. J Perinatol Off J Calif Perinat Assoc. 2015;35(2):85–89. doi: 10.1038/jp.2014.160. doi:10.1038/jp.2014.160. [DOI] [PubMed] [Google Scholar]
- 31.Shamshirsaz AA, Haeri S, Ravangard SF, Sangi-Haghpeykar H, Gandhi M, Ozhand A, et al. Perinatal outcomes based on the institute of medicine guidelines for weight gain in twin pregnancies. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2014;27(6):552–556. doi: 10.3109/14767058.2013.836177. doi:10.3109/14767058.2013.836177. [DOI] [PubMed] [Google Scholar]
- 32.Gavard JA, Artal R. Gestational weight gain and maternal and neonatal outcomes in term twin pregnancies in obese women. Twin Res Hum Genet Off J Int Soc Twin Stud. 2014;17(2):127–133. doi: 10.1017/thg.2013.91. doi:10.1017/thg.2013.91. [DOI] [PubMed] [Google Scholar]
- 33.González-Quintero VH, Kathiresan ASQ, Tudela FJ, Rhea D, Desch C, Istwan N. The association of gestational weight gain per institute of medicine guidelines and prepregnancy body mass index on outcomes of twin pregnancies. Am J Perinatol. 2012;29(6):435–440. doi: 10.1055/s-0032-1304824. doi:10.1055/s-0032-1304824. [DOI] [PubMed] [Google Scholar]
- 34.Fox NS, Saltzman DH, Kurtz H, Rebarber A. Excessive weight gain in term twin pregnancies:examining the 2009 Institute of Medicine definitions. Obstet Gynecol. 2011;118(5):1000–1004. doi: 10.1097/AOG.0b013e318232125d. doi:10.1097/AOG.0b013e318232125d. [DOI] [PubMed] [Google Scholar]
- 35.Fox NS, Rebarber A, Roman AS, Klauser CK, Peress D, Saltzman DH. Weight gain in twin pregnancies and adverse outcomes:examining the 2009 Institute of Medicine guidelines. Obstet Gynecol. 2010;116(1):100–106. doi: 10.1097/AOG.0b013e3181e24afc. doi:10.1097/AOG.0b013e3181e24afc. [DOI] [PubMed] [Google Scholar]
- 36.Wang X, Zhang X, Zhou M, Juan J, Wang X. Association of prepregnancy body mass index, rate of gestational weight gain with pregnancy outcomes in Chinese urban women. Nutr Metab. 2019;16(1):54. doi: 10.1186/s12986-019-0386-z. doi:10.1186/s12986-019-0386-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schaible UE, Kaufmann SHE. Malnutrition and Infection:Complex Mechanisms and Global Impacts. PLoS Med. 2007;4(5):e115. doi: 10.1371/journal.pmed.0040115. doi:10.1371/journal.pmed.0040115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chin JR, Murtaugh MA, Silver R. Obesity:Implications for Women's Reproductive Health. Curr Epidemiol Rep. 2014;1(1):17–26. doi:10.1007/s40471-013-0003-z. [Google Scholar]
- 39.Torloni MR, Betrán AP, Daher S, Widmer M, Dolan SM, Menon R, et al. Maternal BMI and preterm birth:a systematic review of the literature with meta-analysis. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2009;22(11):957–970. doi: 10.3109/14767050903042561. doi:10.3109/14767050903042561. [DOI] [PubMed] [Google Scholar]