Abstract
Background
Inconsistent definitions of complications and unexpected events have limited accurate analysis of surgical outcomes. Perioperative outcome classifications currently used for adult patients have limitations when used for children.
Methods
A multidisciplinary group of experts modified the Clavien–Dindo classification to increase its utility and accuracy in paediatric surgery cohorts. Organizational and management errors were considered in the novel Clavien–Madadi classification, which focuses on procedural invasiveness rather than anaesthetic management. Unexpected events were prospectively documented in a paediatric surgery cohort. Results of the Clavien–Dindo and Clavien–Madadi classifications were compared and correlated with procedure complexity.
Results
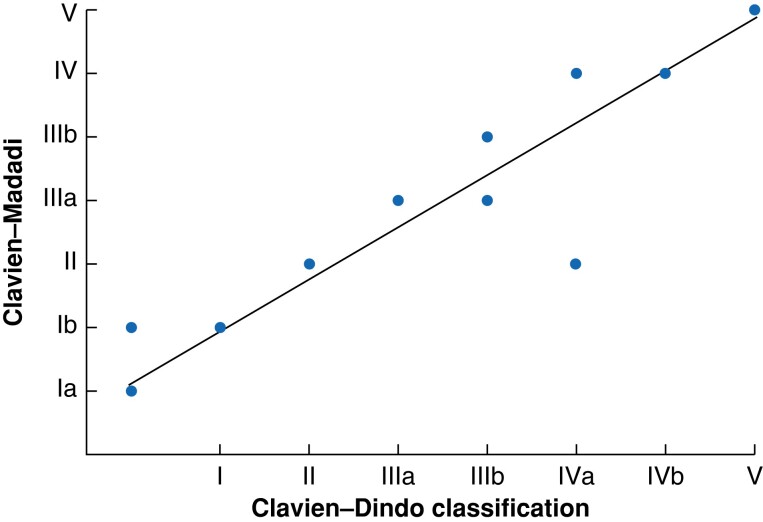
Unexpected events were prospectively documented in a cohort of 17 502 children undergoing surgery between 2017 and 2021. The results of both classifications were highly correlated (ρ = 0.95), although the novel Clavien–Madadi classification identified 449 additional events (organizational and management errors) over the Clavien–Dindo classification, increasing the total number of events by 38 per cent (1605 versus 1158 events). The results of the novel system correlated significantly with the complexity of procedures in children (ρ = 0.756). Furthermore, grading of events > grade III according to the Clavien–Madadi classification showed a higher correlation with procedure complexity (ρ = 0.658) than the Clavien–Dindo classification (ρ = 0.198).
Conclusion
The Clavien–Madadi classification is a tool for the detection of surgical and non-medical errors in paediatric surgery populations. Further validation in paediatric surgery populations is required before widespread use.
The authors report a novel instrument for the grading of unexpected events in paediatric surgery by a multidisciplinary expert group, and based on the Clavien–Dindo classification. The Clavien–Madadi classification was tested and validated in a cohort of 17 502 children and proved to be a valuable instrument in daily paediatric surgical practice.
Introduction
Complications and unexpected events are known to have a substantial impact on mortality, quality of life, and cost in surgical patients1,2. In clinical practice, the use of severity grading systems for complications has resulted in structured documentation and analysis of adverse events, aiming to further improve patient care3,4. These classification systems have become valuable tools for outcome assessment and the comparison of outcome data between institutions and surgical disciplines5,6.
Prior to the introduction of the Clavien–Dindo classification in 2004, there were inconsistent definitions of complications and adverse events in adult surgery7,8. Since then, the classification has been frequently used and validated, and has become an integral part of clinical practice in many surgical specialties9,10.
Initially, this classification had minor impacts on clinical and academic paediatric surgical practice; however, the number of studies examining the application of the Clavien–Dindo classification and reporting unexpected events following surgery in children has increased in the last decade11–14.
Five classification systems have shown a high correlation with graded postoperative events in children, but it has not been possible to confirm the superiority of any of these cyctems15. The Clavien–Dindo classification offered the highest differentiation and proved to be an excellent tool for audit purposes (morbidity and mortality meetings) and the systematic analysis of unexpected events. However, recent reports have pointed out shortcomings of the Clavien–Dindo classification in children15–17.
Limitations of the Clavien–Dindo classification in paediatric surgery have been attributed to the fact that the majority of interventions in children are performed under general anaesthesia, and that the management of complications might seriously differ based on age group (preterm infants, neonates, adolescents) and institutional facilities, and that the duration of hospital stay or time to recovery after events are not considered16–18. Despite these shortcomings, the Clavien–Dindo classification has been adopted in paediatric oncological surgery12,19,20. These developments illustrate the necessity of a standardized classification tailored for children. The aim of this study was to modify the Clavien–Dindo classification to improve the documentation of perioperative unexpected events in paediatric surgery. The study planned to incorporate non-medical errors and organizational problems into the new classification scheme as these are widely understood to impact the care and outcomes of surgical patients21,22.
Methods
Ethical approval for this study was obtained from the University Ethics Committee of Hannover Medical School (No. 10259_B0_K_2022), and the study was registered at clinicaltrials.gov prior to data analysis (NCT05277441). The authors followed the STROBE reporting guidelines23.
Study design
This single-centre prospective cohort study was conducted at the tertiary Hannover paediatric surgical centre. A novel classification of unexpected events was established and tested in a paediatric cohort. The study included the following steps: unexpected events in all patients treated at our institution during the study period from 1 January 2017 to 31 December 2021 were prospectively recorded; each event was immediately classified according to the Clavien–Dindo classification by a designated team; each event was discussed during monthly morbidity and mortality (M&M) conferences and, when necessary, reclassified according to the Clavien–Dindo classification by the entire surgical staff; a novel instrument for classification of unexpected events in children (Clavien–Madadi classification) was established by a multidisciplinary group of experts; all (prospectively recorded) events were graded using the novel classification, henceforth referred to as the Clavien–Madadi classification, based on the adjustment of the Clavien-Dindo classification for paediatric cohorts; and the accurate grading of the severity of an event according to the novel instrument was then validated based on the hypothesis that a more complex procedure results in a more severe or higher-graded unexpected event, based on the protocol by Dindo et al.7. For this purpose, the ranking of the complexity of the initial procedure was correlated with the grading according to the Clavien–Dindo and Clavien–Madadi classification.
Study centre characteristics
The study was performed in the only tertiary academic institution in the German Federal State of Lower–Saxony, serving approximately 8 million inhabitants, 1.5 million of whom are under the age of 18 years. The clinical spectrum of the department includes treatment of neonatal, gastrointestinal, hepatobiliary, thoracic, oncological, urological, and trauma surgery. Furthermore, endoscopic and radiological interventions are also delivered within the unit.
Definition of unexpected events
Events were stratified as follows: events with subsequent deviation from the planned pre-, intra-, and postoperative courses of patients; events with subsequent changes in management with any modifications in treatment or recovery courses of patients; and events related to underlying diseases/disabilities13,14,24. All unexpected events following surgical and non-surgical management were included. In addition, organizational problems such as miscommunication and postponement of operations due to limited capacities for admission, anaesthesia, surgery, or intensive care were included. Errors related to facility use for the organization and scheduling of interventions or perioperative diagnostics were also documented.
Documentation of unexpected events
Algorithms for the assessment and documentation of unexpected events have been previously reported13–15. Briefly, the documentation of unexpected events was performed by designated team members during routine daily conferences. Inpatient, outpatient, and paediatric emergency department events were all documented. On-call team members and other staff reported on any unexpected event that had occurred within the previous 24 or 72 hours after weekends during daily morning conferences. The data included patient demographics, diagnoses, types of treatment, types of events, and the consequences of each event. All data were stored in a password-encrypted database by designated team members.
All events were then analysed by designated department team members and presented and discussed during monthly M&M meetings attended by surgical and non-surgical staff. All event classifications were further discussed, approved, or reclassified according to attendee consensus. All M&M meeting decisions were documented separately, and changes in standard operating procedures were circulated within the surgical team.
Initial classification of events
The severity of adverse events was classified prospectively according to the Clavien–Dindo classification (Table 1) by the designated team7. The final classification was based on the results of team discussions during M&M meetings.
Table 1.
The Clavien–Dindo classification for severity grading of postoperative complications and the Clavien–Madadi classification for grading of perioperative unexpected events in paediatric surgery
| Grade | Clavien–Dindo classification7 | Grade | Clavien–Madadi classification | ||
|---|---|---|---|---|---|
| I | Any deviation from the normal postoperative course with the need for pharmacological treatment Allowed therapeutic regimens are: drugs as antiemetics, antipyretics, analgesics, diuretics, electrolytes, and physiotherapy This grade also includes wound infections opened at the bedside |
I | A | Any deviation from the planned course due to management and/or organizational problems | |
| B | Any deviation from the planned clinical course with the need for pharmacological treatment, such as antiemetics, antipyretics, analgesics, diuretics, electrolytes, and physiotherapy This grade also includes wound infections opened at the bedside |
||||
| II | Requiring pharmacological treatment with drugs other than such allowed for grade I complications Blood transfusions and total parenteral nutrition are also included |
II | Requiring pharmacological treatment with drugs other than such listed for Grade Ib Blood transfusions and parenteral nutrition are also included |
||
| III | A | Intervention not under general anaesthesia | III | A | Endoscopic- and radiologically guided interventions Interventions via laparoscopy/thoracoscopy Interventions under anaesthesia (other than such listed for grade IIIb) |
| B | Intervention under general anaesthesia | B | Interventions via laparotomy/thoracotomy | ||
| IV | A | Single-organ dysfunction (including dialysis) | IV | Multiorgan dysfunction* | |
| B | Multiorgan dysfunction | ||||
| V | Death of a patient | V | Death of a patient | ||
Multiorgan dysfunction is defined as the concurrent dysfunction of two or more organs or systems, including respiratory, cardiovascular, haematological, neurological, gastrointestinal, hepatic, and renal25.
Novel Clavien–Madadi classification
The local study team (O.M.S., J.F.K., J.B., and B.M.U.) reviewed the prospectively collective data from previous studies for the identification of drawbacks of the Clavien–Dindo classification14,15. Despite the high numbers of organizational and management errors, most problems of differentiations were identified for Clavien–Dindo grade III (differentiation between interventions with and without general anaesthesia) and grade IV (single- and multiorgan dysfunction). Those results were discussed with the study group from the Department of Surgery and Transplantation in Zurich (A.D. and P.A.C) and the alternative Clavien–Madadi classification was created. Owing to their expertise in this field and their conceptualization of the Clavien–Dindo classification, the Zurich study group supervised the study. The novel instrument was then presented to a multidisciplinary group of experts that consisted of paediatric surgeons (A.M.), methodologists (S.E.), and statisticians (S.W.) from three European Reference Network for rare Inherited and Congenital Anomalies (ERNICA) centres. All group members individually reviewed the modifications and the data, their comments were implemented into the classification, and the final version was applied in the presented cohort (Fig. S1).
The goal was to create a tool for the assessment and grading of unexpected events in paediatric surgery, on the basis of the well-established structure of the Clavien–Dindo classification. This novel classification aimed to meet the specific requirements of differentiation in a paediatric cohort, focusing on the management and treatment of children.
A previous analysis performed by the study team found that 55 per cent of unexpected events were associated with management and organization15. Although these events were documented and classified in recent studies, these alterations were within Clavien–Dindo grade I, thereby pooling the non-medical events in the group of medical events defined for a grade I event. This strategy increased the number of grade I events in the present cohort massively, without adequately weighing the impact of the patients’ treatment and convalescence. Therefore, it was decided to substratify grade I events into Ia (any deviation from the planned course due to management and/or organizational problems); and Ib (any deviation from the planned clinical course resulting in the need for pharmacological treatment; previously grade I under the Clavien–Dindo classification).
The definition of grade II was adopted from the Clavien–Dindo classification without modifications.
Regarding Clavien–Dindo grade III, the previous analysis revealed that the vast majority of procedures following unexpected events in children were performed under general anaesthesia15. Therefore, the traditional differentiation between events with and without anaesthesia was not suitable for the differentiation of the severity of an event in the paediatric cohort. Grade III events were also stratified into grade IIIa and grade IIIb, based on the invasiveness of procedures as a consequence of unexpected events but adapted to the paediatric cohort, with grade IIIa defined as endoscopic, radiological, and minimally invasive (laparoscopy and thoracoscopy) interventions; and grade IIIb defined as open laparotomy and thoracotomy procedures (Table 1). This stratification of grade III is based on the invasiveness and trauma of open (laparotomy, thoracotomy) versus less invasive procedures; and the expected longer duration of recovery after open versus minimally invasive procedures.
In terms of grade IV stratification of organ failure, a previous study confirmed that most paediatric surgical patients experience a rapid deterioration resulting in multiorgan failure following complications, although the analysis showed only minor and temporary organ dysfunction in a group of children with single-organ failure15. The Clavien–Madadi classification reduced grade IV to a single grade which includes multiorgan dysfunction. Clavien-Madadi grade V is identical to that of the Clavien–Dindo classification, including the death of a patient.
All members of the multidisciplinary group of experts agreed on the final classification (Table 1), and all events were subsequently graded using the Clavien–Madadi classification by designated team members.
Definition of the complexity of surgery
A modified version of the grading system used to validate the Clavien–Dindo classification in the original work was adopted for definition of procedure complexity26. Briefly, in class A interventions patients did not undergo surgery; class B interventions included procedures that did not enter the abdominal or thoracic cavities, such as inguinal hernia repairs, orchidopexies, or thyroglossal duct cyst resections; class C interventions included laparoscopic and thoracoscopic procedures, such as laparoscopic cholecystectomies, laparoscopic fundoplication, and thoracoscopic diaphragmatic hernia repairs; and class D interventions included open procedures that entered the abdominal and/or thoracic cavities such as oesophageal atresia repairs, gastric pull-ups, Kasai procedures, hepatectomies, and pancreatectomies.
Statistical analysis
Statistical analysis was performed using GraphPad Prism v8.0 (GraphPad Software, San Diego, California, USA) and SAS v9.4 (SAS Institute, Cary, North Carolina, USA). The correlation between the Clavien–Dindo and Clavien–Madadi classifications, as well as between complication grades and surgery complexity, was analysed using Spearman’s rho (ρ). A Spearman’s ρ of 0.7 was considered to represent a strong level of correlation.
Results
Within the 5-year study period, treatment was provided to 17 502 inpatients, outpatients, and patients in the paediatric emergency department. A total of 970 (5.5 per cent) experienced at least one unexpected event; of these, 296 (30.5 per cent) experienced more than one unexpected event.
A total of 1605 unexpected events were documented, including 445 (27.7 per cent) organizational and management errors (non-medical events) and 1160 medical events (72.3 per cent) with deviations from the clinical course and medical or interventional consequences.
Comparison of the Clavien–Dindo and Clavien–Madadi classification in paediatric cohort
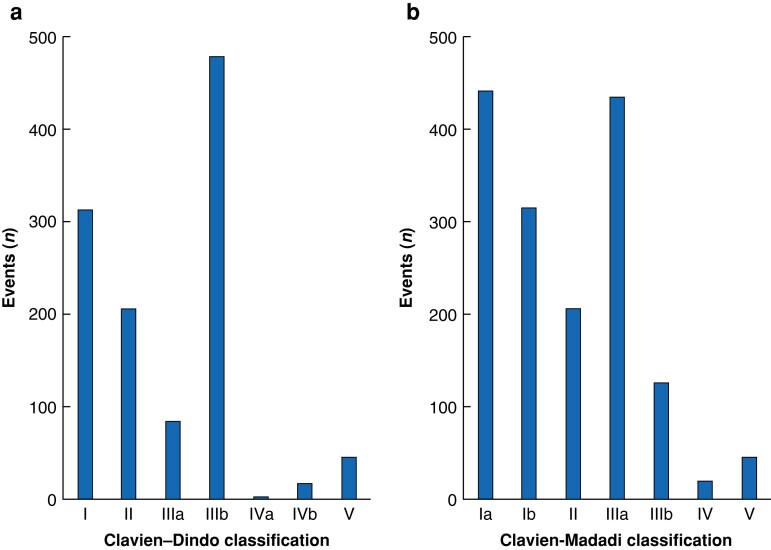
The Clavien–Madadi classification identified 449 additional unexpected events over the Clavien–Dindo classification due to inclusion of organizational and management problems. The modified classification increased the total number of events by 38 per cent (1158 versus 1605 events).
The two classifications were highly correlated (ρ = 0.95084) with graded events (Fig. 1 and Table S1). The Clavien–Madadi classification led to a downgrading of 352 events from grade IIIb (Clavien–Dindo) to grade IIIa (Clavien–Madadi), and five events were downgraded from grade IVa (Clavien–Dindo; single-organ dysfunction) to grade II (Clavien–Madadi). Of the five patients who were downgraded, three presented with postoperative respiratory distress managed with continuous positive airway pressure or high-flow nasal oxygen, without need for reintubation. No events were upgraded under the Clavien–Madadi system as compared with the Clavien–Dindo classification.
Fig. 1.
Correlation of the Clavien–Dindo and the novel Clavien–Madadi classification grading results of 1605 events in 970 children
Grading according to the Clavien–Dindo and Clavien–Madadi classifications
A detailed analysis of grades revealed similar results for grade Ib Clavien–Madadi and grade I Clavien–Dindo classifications (P > 0.9) (Fig. 2 and Table 2).
Fig. 2.
Grading of 1605 events according to two classification systems
a Clavien–Dindo. b Clavien–Madadi.
Table 2.
Grading of all events between 2017 and 2021 according to the Clavien–Dindo and Clavien–Madadi classification
| Grade | Clavien–Dindo classification (n) | Grade | Clavien–Madadi classification (n) | ||
|---|---|---|---|---|---|
| I | 314 | I | A | 445 | |
| B | 317 | ||||
| II | 207 | II | 209 | ||
| III | A | 86 | III | A | 438 |
| B | 480 | III | B | 128 | |
|
|
|||||
| IV | A | 5 | IV | 21 | |
| B | 19 | V | 47 | ||
| V | 47 | ||||
| Total number | 1158 | Total number | 1605 | ||
Only minor differences were observed for grade II in both classification systems (P > 0.9).
The modification of grade III in the Clavien–Madadi classification system led to significant changes compared with the Clavien–Dindo classification (P ≤ 0.0001). The Clavien–Madadi classification documented 438 grade IIIa events versus 86 events under the Clavien–Dindo classification, and 128 grade IIIb events versus 480 events under the Clavien–Dindo classification.
Grade IV of the Clavien–Madadi classification (multiorgan dysfunction) was equal to grade IVb of the Clavien–Dindo classification (n = 19; P ≥ 0.9).
Grade V equals death in both classification systems (n = 47).
Grading of reinterventions according to the Clavien–Dindo and Clavien–Madadi classifications
A total of 566 events resulted in reinterventions in the present cohort. The Clavien–Dindo classification differentiates between procedures without general anaesthesia (grade IIIa; n = 86 (15.2 per cent)) and with general anaesthesia (grade IIIb; n = 480 (84.8 per cent)). The Clavien–Madadi classification differentiates between minimally invasive procedures (grade IIIa; n = 438 (77.4 per cent)) and surgical procedures in which the abdominal or thoracic cavities are opened (grade IIIb; n = 128 (22.6 per cent)).
Procedures received following 566 unexpected events included 19 radiological or endoscopic interventions (3.4 per cent), 39 minimally invasive procedures (6.9 per cent), and 380 procedures (67.1 per cent) that did not enter the abdominal or thoracic cavities (e.g. wound revisions). Laparotomies or thoracotomies following an unexpected event were performed in 128 patients (22.6 per cent).
The majority of the 86 interventions without general anaesthesia (Clavien–Dindo grade IIIa) were wound revisions (thoracic, abdominal, or inguinal) and radiologically guided drains (abdomen and thorax), of which 27 (31.4 per cent) were performed in the paediatric intensive care unit.
All endoscopic and radiological interventions were managed under general anaesthesia.
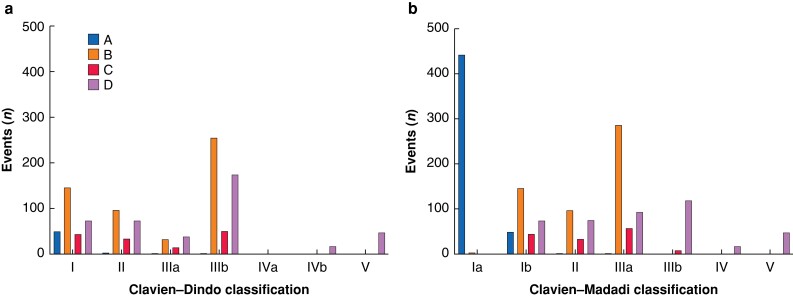
Correlation between event grading and procedure complexity in a cohort of 17 502 patients
In terms of the complexity of initial procedures (class A–D), a stronger correlation was identified for the Clavien–Madadi classification (ρ = 0.7558) than for the Clavien–Dindo classification (ρ = 0.2470). Following further stratification of events higher than grade III (reinterventions), the Clavien–Madadi classification showed much higher correlation with the complexity of the initial procedures (ρ = 0.6580) than the conventional Clavien–Dindo classification (ρ = 0.1977) (Table S2).
For the analysis, the Clavien–Madadi grade Ia events were excluded, as they represent organizational and management problems not associated with any treatment, and not considered in the Clavien–Dindo classification (Fig. 3).
Fig. 3.
Grading of two classification systems according to the complexity of initial procedures
a Clavien–Dindo. b Clavien–Madadi. Definition of procedure complexity based on modifications proposed by Klotz et al.26: A, patients who did not undergo surgery; B, procedures that did not enter the abdominal or thoracic cavity; C, laparoscopic and thoracoscopic procedures; D, open procedures that entered the abdominal and/or thoracic cavities.
Discussion
Previous reports have pointed out that the Clavien–Dindo classification has several drawbacks when used in paediatric surgical patients. It does not sufficiently differentiate the severity of varied interventions used to treat complications in children based on in-house facilities and patient age16. In preterm neonates and infants, conservative and interventional approaches are preferred for some conditions where surgery would normally be considered, which may result in a downgrading of complications in some cases, despite their severity.
For these reasons, it was felt that a modification of the Clavien–Dindo classification was necessary for use in preterms, neonates, and children. The novel Clavien–Madadi classification considers all aspects mentioned above and included three modifications, including alterations in organization and management plans for treatment (grade Ia); stratification of interventions or reinterventions for complications according to procedure invasiveness (grade IIIa: minimally invasive; grade IIIb: laparotomy and thoracotomy); and all organ failure events were defined as multiorgan dysfunction (grade IV). The modified classification system retained most of the original structure and grades of the Clavien–Dindo classification system and still focuses on the therapeutic consequences of unexpected events. The study aimed to maintain the frequently appraised benefits of the Clavien–Dindo classification in minimizing the potential of subjective interpretation.
A comparison of the Clavien–Dindo classification and the novel Clavien–Madadi classification showed an increase in the number of registered unexpected events by 38 per cent (1158 events according to Clavien–Dindo versus 1605 events according to Clavien–Madadi). Within the 5-year study period, 449 organizational and management errors were identified. Despite the additional events documented according to the Clavien–Madadi classification, the results of both grading systems were highly correlated. Grading of postoperative and postinterventional events according to the novel classification was correlated with the complexity of initial procedures in this paediatric cohort, indicating that complications following complex procedures result in more invasive management. Grade III (interventions) events under the Clavien–Madadi classification showed a higher correlation with the complexity of initial procedures than the conventional Clavien–Dindo classification.
The high incidence and relevance of management and organization problems with subsequent changes in planned courses was confirmed in our recent study. Incidents such as miscommunication and lack of appropriate equipment occurred in 49 of 438 events (11.2 per cent) and accounted for 18 per cent of all unexpected events14. These events would have been missed under the classical Clavien–Dindo classification, while a recent study has emphasized the negative effect of interprofessional miscommunication between surgeons and nurses, and organizational and technical errors on the outcome and well-being of general surgical patients27. In particular, interprofessional miscommunication or disruption of communication has repeatedly been reported to be associated with an increase in clinical (e.g. drug administration on the ward) and surgical errors, with a negative effect on patients’ well-being28–30.
The differentiation between interventions with or without general anaesthesia by the Clavien–Dindo classification did not add additional value to the present cohort15. Various procedures for treating complications in adults such as radiological- or endoscopic-guided interventions are performed under sedation or local anaesthesia25,31. In children, the vast majority of reinterventions are performed under general anaesthesia. A shift was observed from a low number of grade IIIa events to a high number of grade IIIb events with the use of the Clavien–Dindo classification in the present cohort15. However, those grade IIIb events included local wound dressings under general anaesthesia, relaparotomies with adhesiolysis, bowel resections, and others. Therefore, the classification system used in this cohort did not accurately differentiate the severity of these complications, and, based on previous results, the focus of the novel instrument was the invasiveness of procedures rather than anaesthetic management.
Furthermore, the Clavien–Dindo classification differentiates between single- and multiorgan dysfunction. Sepsis or surgical complications rarely lead to single-organ failure in preterms, neonates, and infants—these patients mostly develop multiorgan failure32–34. In the current literature, complications of preterms, neonates, and infants leading to organ failure are differently interpreted as grade IV events according to the Clavien–Dindo classification35. Most patients experienced rapid deterioration resulting in multiorgan dysfunction rather than single-organ failure. Previous analysis of sentinel events in our paediatric cohort confirmed that the majority occurred in the group of neonatal surgery, including 67 per cent of all grade IV and 86 per cent of all grade V events15. Although analysis of the majority of grade IV events in neonates showed single-organ failures, further analysis revealed at least dysfunctions of another organ system15. Some authors have bypassed this problem in their analysis of complications following neonatal surgery by defining grade IV as a combination of severe single- and multiorgan dysfunction35.
Recently, the study team has reported on the benefits of the Comprehensive Complication Index (CCI®), a numeric metric of overall postoperative morbidity, in the evaluation of the perioperative management of paediatric patients15,36–38. In children with multiple unexpected events, the CCI® adequately weighted the sentinel events and corresponded with the duration of hospital stay in critically ill children15. Despite the fact that the CCI® is based on a prior grading of events according to the Clavien–Dindo classification, we strongly recommended its use in prospective studies in paediatric surgery as its formula also allows observation of morbidity over the course of time, which is especially important in the paediatric population, considering that 30 per cent of patients with unexpected events in our cohort experienced more than one event. While the advantages of the CCI® in the documentation of postoperative complications, the applicability with the Clavien–Madadi classification might be subject of future studies.
The current study has some limitations. This was a single-institution study, and multicentre studies using this novel instrument need to be conducted for further validation. Data on unexpected events were collected prospectively from 2017 to 2021 and classified during M&M meetings by an entire paediatric surgical team using the Clavien–Dindo classification. The novel Clavien–Madadi classification was applied by selected members of the team using the same prospectively collected data, which might have resulted in bias. The number of experts who participated in the instrument setup was small. However, the majority of experts were members of ERNICA, which assures high-quality standards. Finally, the implementation of our approach in dealing with unexpected events during daily routines may prove challenging, as evidenced by the fact that this study was conducted over several years at our institution. However, the results of our previous study confirm that the effort is worth it, providing information on 64 changes of standard operating procedures since the implementation of our systematic assessment of unexpected events, subsequently improving outcomes in paediatric surgical patients15.
Supplementary Material
Acknowledgements
Simon Eaton acknowledges support from the NIHR Biomedical Research Centre at Great Ormond Street Hospital.
Contributor Information
Omid Madadi-Sanjani, Department of Pediatric Surgery, Hannover Medical School, Hannover, Germany; European Reference Network for Rare Inherited and Congenital Anomalies (ERNICA).
Joachim F Kuebler, Department of Pediatric Surgery, Hannover Medical School, Hannover, Germany; European Reference Network for Rare Inherited and Congenital Anomalies (ERNICA).
Julia Brendel, Department of Pediatric Surgery, Hannover Medical School, Hannover, Germany; European Reference Network for Rare Inherited and Congenital Anomalies (ERNICA).
Soeren Wiesner, Institute of Biostatistics, Hannover Medical School, Hannover, Germany.
Annika Mutanen, European Reference Network for Rare Inherited and Congenital Anomalies (ERNICA); Department of Pediatric Surgery, New Children´s Hospital, Helsinki University Hospital and University of Helsinki, Helsinki, Finland.
Simon Eaton, European Reference Network for Rare Inherited and Congenital Anomalies (ERNICA); Stem Cells and Regenerative Medicine Section, UCL Great Ormond Street Institute of Child Health, London, UK.
Anja Domenghino, Department of Surgery and Transplantation, University Hospital Zurich, Zurich, Switzerland.
Pierre-Alain Clavien, Department of Surgery and Transplantation, University Hospital Zurich, Zurich, Switzerland.
Benno M Ure, Department of Pediatric Surgery, Hannover Medical School, Hannover, Germany; European Reference Network for Rare Inherited and Congenital Anomalies (ERNICA).
Author contributions
Omid Madadi-Sanjani (Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Writing—original draft, Writing—review & editing), Joachim Kuebler (Conceptualization, Data curation, Formal analysis, Methodology, Software, Validation, Writing—original draft, Writing—review & editing), Julia Brendel (Conceptualization, Data curation, Methodology, Validation, Writing—review & editing), Soeren Wiesner (Formal analysis, Investigation, Software, Validation, Visualization, Writing—review & editing), Annika Mutanen (Conceptualization, Investigation, Methodology, Supervision, Validation, Writing—review & editing), Simon Eaton (Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing—review & editing), Anja Domenghino (Conceptualization, Formal analysis, Methodology, Resources, Supervision, Validation, Writing—review & editing), Pierre-Alain Clavien (Conceptualization, Methodology, Supervision, Validation, Writing—review & editing), and Benno Ure (CRediT contribution not specified).
Funding
This work was financed by the general budgets of the departments involved.
Disclosure
The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS online.
Data availability
The data presented in this study are available on request from the corresponding author.
References
- 1. Longo WE, Virgo KS, Johnson FE, Oprian CA, Vernava AM, Wade TP et al. Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum 2000;43:83–91 [DOI] [PubMed] [Google Scholar]
- 2. Tevis SE, Cobian AG, Truong HP, Craven MW, Kennedy GD. Implications of multiple complications on the postoperative recovery of general surgery patients. Ann Surg 2016;263:1213–1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mariette C, Markar SR, Dabakuyo-Yonli TS, Meunier B, Pezet D, Collet D et al. Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med 2019;380:152–162 [DOI] [PubMed] [Google Scholar]
- 4. Xu L, Su X, He Z, Zhang C, Lu J, Zhang G et al. Short-term outcomes of complete mesocolic excision versus D2 dissection in patients undergoing laparoscopic colectomy for right colon cancer (RELARC): a randomised, controlled, phase 3, superiority trial. Lancet Oncol 2021;22:391–401 [DOI] [PubMed] [Google Scholar]
- 5. Altmann J, Chekerov R, Fotopoulou C, Muallem MZ, du Bois A, Cliby W et al. Ten years of live surgical broadcast at Charité-MAYO conferences (2010–2019): a systematic evaluation of the surgical outcome. Int J Gynecol Cancer 2022;32:746–752 [DOI] [PubMed] [Google Scholar]
- 6. Abdelsattar JM, Mourany J, Afridi FG, Musgrove K, Shaffer L, Khan U et al. Enhancing the educational value and faculty attendance of a morbidity and mortality conference. J Surg Educ 2020;77:905–910 [DOI] [PubMed] [Google Scholar]
- 7. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187–196 [DOI] [PubMed] [Google Scholar]
- 9. Amara D, Parekh J, Sudan D, Elias N, Foley DP, Conzen K et al. Surgical complications after living and deceased donor liver transplant: the NSQIP transplant experience. Clin Transplant 2022;36:e14610 [DOI] [PubMed] [Google Scholar]
- 10. Inaraja-Pérez GC, Júlvez-Blancas M. Usefulness of the Clavien-Dindo classification to rate complications after carotid endarterectomy and its implications in patient prognosis. Ann Vasc Surg 2019;55:232–238 [DOI] [PubMed] [Google Scholar]
- 11. Klunder MB, Bruggink JLM, Huynh LDH, Bodewes FAJA, van der Steeg AFW, Kraal KCJM et al. Surgical outcome of children with a malignant liver tumour in The Netherlands: a retrospective consecutive cohort study. Child Basel Switz 2022;9:525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beltman L, Labib H, Oosterlaan J, van Heurn E, Derikx J. Risk factors for complications in patients with Hirschsprung disease while awaiting surgery: beware of bowel perforation. J Pediatr Surg 2022;57:561–568 [DOI] [PubMed] [Google Scholar]
- 13. Sethi MVA, Zimmer J, Ure B, Lacher M. Prospective assessment of complications on a daily basis is essential to determine morbidity and mortality in routine pediatric surgery. J Pediatr Surg 2016;51:630–633 [DOI] [PubMed] [Google Scholar]
- 14. Zoeller C, Kuebler JF, Ure BM, Brendel J. Incidence of complications, organizational problems, and errors: unexpected events in 1605 patients. J Pediatr Surg 2021;56:1723–1727 [DOI] [PubMed] [Google Scholar]
- 15. Madadi-Sanjani O, Zoeller C, Kuebler JF, Hofmann AD, Dingemann J, Wiesner S et al. Severity grading of unexpected events in paediatric surgery: evaluation of five classification systems and the Comprehensive Complication Index (CCI®). BJS Open 2021;5:zrab138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thompson H, Jones C, Pardy C, Kufeji D, Nichols E, Murphy F et al. Application of the Clavien-Dindo classification to a pediatric surgical network. J Pediatr Surg 2020;55:312–315 [DOI] [PubMed] [Google Scholar]
- 17. Dwyer ME, Dwyer JT, Cannon GM, Stephany HA, Schneck FX, Ost MC. The Clavien-Dindo classification of surgical complications is not a statistically reliable system for grading morbidity in pediatric urology. J Urol 2016;195:460–464 [DOI] [PubMed] [Google Scholar]
- 18. Astolfi D, Wildhaber BE. Classification of pediatric complications: time for a new concept. J Neurosurg Pediatr 2021;28:620–620 [DOI] [PubMed] [Google Scholar]
- 19. Matthyssens LE, Nuchtern JG, Van De Ven CP, Gabra HOS, Bjornland K, Irtan S et al. A novel standard for systematic reporting of neuroblastoma surgery: the International Neuroblastoma Surgical Report Form (INSRF): a joint initiative by the pediatric oncological cooperative groups SIOPEN, COG, and GPOH. Ann Surg 2022;275:e575–e585 [DOI] [PubMed] [Google Scholar]
- 20. Beltman L, Roorda D, Backes M, Oosterlaan J, van Heurn LWE, Derikx JPM. Risk factors for short-term complications graded by Clavien-Dindo after transanal endorectal pull-through in patients with Hirschsprung disease. J Pediatr Surg 2022;57:1460–1466 [DOI] [PubMed] [Google Scholar]
- 21. Slawomirski L, Auraaen A, Klazinga NS. The Economics of Patient Safety: Strengthening a Value-based Approach to Reducing Patient Harm at National Level. OECD Health Working Papers 2017. Paris: OECD Publishing. [Google Scholar]
- 22. Proctor ML, Pastore J, Gerstle JT, Langer JC. Incidence of medical error and adverse outcomes on a pediatric general surgery service. J Pediatr Surg 2003;38:1361–1365 [DOI] [PubMed] [Google Scholar]
- 23. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mazeh H, Cohen O, Mizrahi I, Hamburger T, Stojadinovic A, Abu-Wasel B et al. Prospective validation of a surgical complications grading system in a cohort of 2114 patients. J Surg Res 2014;188:30–36 [DOI] [PubMed] [Google Scholar]
- 25. Müller PC, Morell B, Vetter D, Raptis DA, Kapp JR, Gubler C et al. Preemptive endoluminal vacuum therapy to reduce morbidity after minimally invasive Ivor Lewis esophagectomy: including a novel grading system for postoperative endoscopic assessment of GI-anastomoses. Ann Surg 2021;274:751–757 [DOI] [PubMed] [Google Scholar]
- 26. Klotz HP, Candinas D, Platz A, Horvath A, Dindo D, Schlumpf R et al. Preoperative risk assessment in elective general surgery. Br J Surg 1996;83:1788–1791 [DOI] [PubMed] [Google Scholar]
- 27. Krecko LK, Pavuluri Quamme SR, Carnahan S, Steege LM, Tipple S, Bavery L et al. To page or not to page? A qualitative study of communication practices of general surgery residents and nurses. Surgery 2022;172:1102–1108 [DOI] [PubMed] [Google Scholar]
- 28. Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM. Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery 2007;142:658–665 [DOI] [PubMed] [Google Scholar]
- 29. Fabri PJ, Zayas-Castro JL. Human error, not communication and systems, underlies surgical complications. Surgery 2008;144:557–563; discussion 563-565 [DOI] [PubMed] [Google Scholar]
- 30. Karsh BT, Wiegmann D, Wetterneck T, Carayon P. Communication and systems factors might still underlie surgical complications. Surgery 2009;145:686–687 [DOI] [PubMed] [Google Scholar]
- 31. Sandström P, Røsok BI, Sparrelid E, Larsen PN, Larsson AL, Lindell G et al. ALPPS improves resectability compared with conventional two-stage hepatectomy in patients with advanced colorectal liver metastasis. Ann Surg 2018;267:833–840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Weiss SL, Balamuth F, Hensley J, Fitzgerald JC, Bush J, Nadkarni VM et al. The epidemiology of hospital death following pediatric severe sepsis: when, why, and how children with sepsis die. Pediatr Crit Care 2017;18:823–830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lin JC, Spinella PC, Fitzgerald JC, Tucci M, Bush JL, Nadkarni VM et al. New or progressive multiple organ dysfunction syndrome in pediatric severe sepsis: a sepsis phenotype with higher morbidity and mortality. Pediatr Crit Care 2017;18:8–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Proulx F, Joyal JS, Mariscalco MM, Leteurtre S, Leclerc F, Lacroix J. The pediatric multiple organ dysfunction syndrome. Pediatr Crit Care Med J Soc 2009;10:12–22 [DOI] [PubMed] [Google Scholar]
- 35. Catré D, Lopes MF, Madrigal A, Oliveiros B, Cabrita AS, Viana JS et al. Predictors of major postoperative complications in neonatal surgery. Rev Col Bras Cir 2013;40:363–369 [DOI] [PubMed] [Google Scholar]
- 36. Clavien PA, Vetter D, Staiger RD, Slankamenac K, Mehra T, Graf R et al. The Comprehensive Complication Index (CCI®): added value and clinical perspectives 3 years “down the line”. Ann Surg 2017;265:1045–1050 [DOI] [PubMed] [Google Scholar]
- 37. Staiger RD, Cimino M, Javed A, Biondo S, Fondevila C, Périnel J et al. The comprehensive complication Index (CCI®) is a novel cost assessment tool for surgical procedures. Ann Surg 2018;268:784–791 [DOI] [PubMed] [Google Scholar]
- 38. Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 2013;258:1–7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.