Abstract
Introduction:
Social determinants of health (SDH) may influence children’s weight status. Our objective was to examine relationships between SDH and preschoolers’ weight status.
Methods:
This retrospective cohort study included 169465 children (aged 4–6 years) with anthropometric measurements taken at immunization visits from 2009 to 2017 in Edmonton and Calgary, Canada. Children were categorized by weight status based on WHO criteria. Maternal data were linked to child data. The Pampalon Material and Social Deprivation Indexes were used to assess deprivation. We used multinomial logistic regression to generate relative risk ratios (RRRs) to examine associations between ethnicity, maternal immigrant status, neighbourhood-level household income, urban/rural residence and material and social deprivation with child weight status.
Results:
Children of Chinese ethnicity were less likely than those in the General Population to have overweight (RRR=0.64, 95% CI: 0.61–0.69) and obesity (RRR=0.51, 0.42–0.62). Children of South Asian ethnicity were more likely than those in the General Population to have underweight (RRR=4.14, 3.54–4.84) and more likely to have obesity (RRR=1.39, 1.22–1.60). Children with maternal immigrant status were less likely than those without maternal immigrant status to have underweight (RRR=0.72,0.63–0.82) and obesity (RRR=0.71,0.66–0.77). Children were less likely to have overweight (RRR=0.95,0.94–0.95) and obesity (RRR=0.88,0.86–0.90) for every CAD 10000 increase in income. Relative to the least deprived quintile, children in the most materially deprived quintile were more likely to have underweight (RRR=1.36, 1.13–1.62), overweight (RRR=1.52,1.46–1.58) and obesity (RRR=2.83, 2.54–3.15). Relative to the least deprived quintile, children in the most socially deprived quintile were more likely to have overweight (RRR=1.21, 1.17–1.26) and obesity (RRR=1.40, 1.26–1.56). All results are significant to p < 0.001.
Conclusion:
Our findings suggest the need for interventions and policies to address SDH in preschoolers to optimize their weight and health.
Keywords: social determinants of health, child malnutrition, childhood overweight, population health
Highlights
We found associations between key social determinants of health and unhealthy weight status in preschoolers.
Children of Chinese ethnicity were less likely to have overweight and obesity, and children of South Asian ethnicity were more likely to have underweight and obesity.
Children with maternal immigrant status were less likely to have underweight and obesity.
Children were less likely to have overweight and obesity for every CAD 10 000 increase in income.
Children in the most materially deprived quintile were more likely to have underweight, overweight and obesity. Children in the most socially deprived quintile were more likely to have overweight and obesity.
Introduction
A healthy childhood is essential for optimal development and well-being across the lifespan.1 Many conditions such as obesity, heart disease and mental illness have roots in childhood.2 Since chronic health conditions can hinder economic potential and societal participation throughout life, interventions during early childhood can enhance physical, emotional and social development.3
Millions of children worldwide suffer from underweight, overweight and obesity. Underweight is a critical factor for preschool children, due to its association with delayed cognitive development and poorer academic performance.4,5 Overweight and obesity can increase the risk of chronic diseases (e.g. type 2 diabetes, heart disease) and impair psychological health and well-being.6,7 The impact of overweight and obesity on health and well-being has been heightened with the emergence of the coronavirus pandemic, since excess weight appears to increase risk of respiratory complications that accompany COVID-19.8
The World Health Organization (WHO) defines social determinants of health (SDH) as conditions in which people are born, grow, live, work and age.9 Several studies have documented important relationships between SDH and weight status in children. For example, ethnic minorities are disproportionately affected by child obesity in the United States.10 A Canadian report noted that the mean body mass index (BMI) z-scores of second-generation immigrant children (parents born in Canada) were higher than those of first-generation immigrants (parents born outside Canada) and children of grandparents born in Canada.11 Children were at increased odds of child obesity if they resided in neighbourhoods with low income, according to a Toronto-based study.12Although there are few data on neighbourhood deprivation or urban or rural residence and their associations with the weight status of Canadian children, a longitudinal study by Carter et al.13 found a positive association between neighbourhood material deprivation and weight gain in children.
The mechanism by which SDH influence child weight status involves a variety of factors (Appendix S1 in the supplementary material) such as cultural or income-based differences in weight perception, food parenting (i.e. parent-child feeding practices) and physical activity practices. These differences may protect children from or predispose them to unhealthy weights.
There are several limitations in the literature about the influence of SDH on weight status in preschoolers. First, some reports include self- or proxy-reported anthropometric data, which are prone to bias.14,15 Second, there is limited research on underweight children in developed countries; underweight may disproportionately impact specific demographic or socioeconomic groups. Finally, there is scant literature on the links between ethnicity, having maternal immigrant status and social and material deprivation and weight status in Canadian preschool children. An improved understanding of environmental contexts can better inform targeted health interventions and policies.16 With these issues in mind, our objective was to examine the associations between SDH—including ethnicity, maternal immigrant status, neighbourhood-level household income, urban/rural residency and material and social deprivation—and weight status in preschool children in Alberta, Canada.
Methods
Ethics approval
This study was approved by the University of Alberta Research Ethics Board (Pro00020230). The ethics panel determined that the research is a retrospective database review for which participant consent for access to personally identifiable health information would not be reasonable, feasible or practical.
Study population
This study included children born in Alberta, Canada, between 1 January 2005 and 29 November 2013, who had visited public health units in Edmonton and Calgary to receive immunizations during their preschool years (age range: 4–6 y) between January 2009 and November 2017. According to the Statistics Canada 2016 Census,17 relative to the national statistics, Edmonton and Calgary had a greater proportion of individuals of Chinese origin, South Asian origin and immigrant status. The mean 2015 household income in Edmonton and Calgary was also greater than that of Canada (Appendix S2 in the supplementary material).
SDH data sources and linkage
Anthropometric data from children were taken from the Alberta public health immunization records database. Public health nurses used standardized protocol18 (e.g. measuring weight with child standing in the centre of the scale, measuring height with child’s heels together) and equipment (e.g. child and adolescent scale, wheelchair scale) to collect child and parent data. Information on children’s date of birth, sex, age at measurement, measured height (to the nearest 0.1 cm) and measured weight (to the nearest 0.1 kg) was collected during immunization visits.
During the study period, data availability ranged from 17.6% in 2013 to 67.7% in 2008. An identical linking strategy was used throughout the study. BMI data were collected anywhere between children’s fourth and seventh birthdays; data availability was lower specifically towards the end of the study (birth years 2012 and 2013), as the children born in these years had not turned seven by November 2017 (the last month when BMI data were available). As shown in a previous study,19 we found some differences in demographic characteristics between mothers of children with and without BMI data; mothers with available child BMI data were slightly older, were of higher socioeconomic status, were more likely to be nulliparous and had slightly higher rates of gestational diabetes and hypertension during pregnancy when compared to mothers without available child BMI data. However, we do not believe that the missing BMI data impacted the internal validity of the study.
When weight or height data were available, erroneous values (i.e. implausible values such as 0 cm height, 0 kg weight, or weight and height values that resulted in a BMI of less than 10 or greater than 50) were assumed in 0.9% of measurements. The weight range in our study cohort was 9 kg to 78 kg and the height range was 62 cm to 156 cm.
Birth and infancy characteristics (date of birth, birth weight, gestational age at birth) were retrieved from the Alberta Vital Statistics Birth Registry. Child ethnicity, assumed to be equivalent to maternal ethnicity, was identified using surname algorithms from the University of Calgary Ethnicity Program and the Institute for Clinical Evaluative Studies Ethnicity Program. Child ethnicity was trichotomized into the following mutually exclusive categories: “Chinese” “South Asian,” and “General Population.”20-22 These algorithms were run on the earliest maternal surname in the Alberta Health Care Insurance Plan Registry. Maternal data (postal code, immigrant status, household income at the neighbourhood level, ethnicity) were also included. Postal codes were obtained from the Alberta Health Care Insurance Plan Registry. Urban/rural residency was determined using the Postal Code Translator File disseminated by Alberta Health. Maternal immigration status was determined using the Alberta Health Care Insurance Plan Central Stakeholder Registry, which has identified mothers entering Alberta from another country or province since 1984. Census data from Statistics Canada (2011) were linked at the Forward Sortation Area level, which was used to determine household income (in CAD) in 2010 at the neighbourhood level as a measure of neighbourhood socioeconomic status.
Material and social deprivation
The Pampalon Deprivation Indexes, two Quebec-based measures of social inequity, were used in this study to assess social and material deprivation.23 The material deprivation index accounts for relative differences in education, employment and income; the social deprivation index accounts for maternal marriage status, solitary living and single parenthood. Greater values signify greater deprivation. The indexes, which have been validated as adequate predictors of health outcomes,24 are based on Canadian dissemination areas and cover approximately 98% of Canada’s population. For our purposes, Pampalon material and social deprivation index data were retrieved using dissemination areas linked to maternal postal code data at childbirth and categorized into quintiles.25
Preschool child weight status
The outcome of interest was child weight status at preschool immunization visit, which occurred when children were aged 4 to 6 years. For children with multiple visits, we included only the last measurements in our study. Consistent with Canadian recommendations,26 the WHO body mass index (BMI) growth charts for Canada were used to categorize children’s weight status (Appendix S3 in the supplementary material). BMI was calculated by dividing weight (in kg) by height (in m2).
The WHO uses different terms to describe weight status categories based on age. For children under 5 years of age, “overweight” and “obesity” are defined as BMI>2 and >3 standard deviations (SDs) above the median, respectively. For children aged 5years and older, “overweight” and “obesity” are defined as BMI>1 and >2 SDs above the median, respectively. For our study, which included children both above and below 5 years of age, we defined our weight status categories in BMI z-scores (i.e. comparing children’s BMI to the national average, adjusted for age) as follows: “underweight” (zBMI<−2), “normal weight” (zBMI>−2 to≤1), “overweight” (zBMI>1 to ≤3 ) and “obese” (zBMI>3), irrespective of the child’s age at measurement. We also defined “excess weight” as a combination of the overweight and obese categories. This was done to ensure simplicity and consistency across age groups. A distribution of our study population z-scores can be found in Appendix S4 in the supplementary material.
Statistical analysis
For each weight category, we presented the child’s sex, anthropometric measurements at preschool age, age at measurement and SDH variables (ethnicity, maternal immigrant status, urban/rural residence, household income at neighbourhood level, material and social deprivation indexes). To assess the independent association of SDH factors and preschool weight, we used multinomial logistic regression models, yielding relative risk ratios (RRRs), with weight status at preschool age as a four-category outcome (i.e. underweight, normal weight, overweight, obese). The reference category was the normal weight category. The models estimated RRRs and 95% confidence intervals (95% CIs) of developing unhealthy weight status for each variable. We fit data on three models via generalized estimating equations with exchangeablecorrelation matrix. This was done to adjust for potential clustering and correlation with respect to multiple children of the same mother.
The first model (R2 =0.014) included ethnicity, maternal immigrant status, household income at neighbourhood level and urban/rural residence. The second (R2=0.0075) and third (R2=0.0047) models studied the material deprivation index and social deprivation index separately with the first quintile (least deprived) as the reference category. All models were adjusted for child sex and age at preschool weight measurement. Deprivation indexes were additionally adjusted for ethnicity, but were separately modelled, in recognition of the possible correlation between them and the other SDH variables. R2 values were calculated as proposed by Zheng27 to measure proportional reduction in variation and assess goodness of fit for marginal models.
To validate each model’s results, we assessed each model’s ability to discriminate between our child weight status outcome categories. This was done by estimating the polytomous discrimination index (PDI) of Van Calster et al. using the SAS macro of Dover et al.28,29 All multinomial models displayed discrimination abilities better than those of a classifier that selects at random among four categories, as all models had a PDI greater than the 25% threshold. The multinomial model that included individual SDH and the model that included the quintiles of the material deprivation index had the largest PDI, of 0.324 (95% CI: 0.318–0.331) and 0.326 (0.319–0.332), respectively. The model that included the quintiles of the social deprivation index had a lower PDI: 0.315 (0.309–0.322). This result showed that modelling using individual SDH had discrimination abilities superior to modelling using the social deprivation index on its own; the same is true for modelling using the material deprivation index and ethnicity compared to modelling using the deprivation index on its own.
The unit of analysis was the child. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, US). Parameters of multinomial logistic marginal models with correlated responses were estimated in SAS using the procedures proposed by Kuss and McLerran.30 Given the large sample size, we defined statistical significance at p<0.001.
Results
Our initial study population included 177284 records, but decreased because of missing child identification numbers, missing height and weight data, calculated BMI values of <10 kg/m2 or >50kg/m2 and repeat height and weight measurements. Our first model included 168387 children and 125778 mothers due to additional missing maternal neighbourhood income and residence data (urban or rural). Descriptive characteristics of our excluded population can be found in Appendix S5 in the supplementary material. Out of the 169465 children studied in models 2 and 3, there were 5558 children with missing deprivation indexes (due to missing dissemination area or missing maternal neighbourhood income data), leaving a population of 163907children and 122773 mothers.
Descriptive characteristics of our complete population of children and mothers are presented in Table 1 . There was a significantly greater proportion of males than females in the overweight (55.9%) and obese (64.0%) categories (both p<0.001).
Table 1. Child and maternal descriptive characteristics across weight status categories (n = 169 465).
With regard to ethnicity and maternal immigrant status, our first model ( Table 2 ) demonstrated that children of Chinese ethnicity (vs. General Population) were less likely to have overweight (RRR=0.64, 95% CI: 0.61–0.69) and obesity (RRR=0.51, 0.42–0.62; both p<0.001). Children of South Asian ethnicity (vs. General Population) were more likely to have underweight (RRR=4.14, 3.54–4.84), less likely to have overweight (RRR=0.80, 0.75–0.85) and more likely to have obesity (RRR=1.39, 1.22–1.60; all p<0.001). Children with maternal immigrant status (vs. Canadian-born status) were less likely to have underweight (RRR=0.72, 0.63–0.82) and obesity (RRR=0.71, 0.66–0.77; both p<0.001).
Table 2. Multinomial regression findings examining social determinants of health in relation to child weight status categories.
Our analyses related to neighbourhood-level household income revealed that children were less likely to have overweight (RRR=0.95, 95% CI: 0.94–0.95) and obesity (RRR=0.88, 0.86–0.90) with every CAD 10000 increase in income (p<0.001). There was no statistically significant association between urban/rural residence and child weight status risk in our first model.
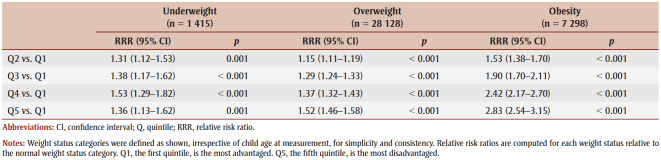
In Table 3 , data are presented showing the associations between material deprivation and child weight status. Children in the most materially deprived quintile (vs. the least deprived quintile) were more likely to have underweight (RRR=1.36, 95% CI: 1.13–1.62), overweight (RRR=1.52, 1.46–1.58) and obesity (RRR=2.83, 2.54–3.15; all p<0.001). The risk of having overweight and obesity increased as material deprivation increased across all quintiles. The greatest risks and risk changes per quintile were with respect to risk of obesity.
Table 3. Associations between material deprivation quintile and child weight status categories.
Data in Table 4 show the associations between social deprivation and child weight status. Children in the most socially deprived quintile (vs. the least deprived quintile) were more likely to have overweight (RRR=1.21, 95% CI: 1.17–1.26) and obesity (RRR=1.40, 1.26–1.56; both p<0.001). Those in the second and third most deprived quintiles (Q3 and Q4) had identical risk of having overweight. Although not all of the RRRs were statistically significant, the risk of having obesity increased as social deprivation increased across all quintiles.
Table 4. Associations between social deprivation quintile and child weight status categories.
Discussion
The purpose of our study was to examine associations between key SDH and weight status in a large population of preschoolers. Our analyses revealed several notable findings. We found that, compared with the General Population group, children of Chinese ethnicity were less likely to have overweight and obesity, while children of South Asian ethnicity were more likely to have either underweight or obesity. Children with maternal immigrant status were less likely to have both underweight and obesity compared to their peers with mothers born in Canada. Children were less likely to be in the overweight and obese categories as neighbourhood-level household income increased. Children in the most materially deprived quintile were more likely to have underweight, overweight and obese status. Finally, children in the most socially deprived quintile were more likely to have overweight and obesity relative to the least deprived category. Overall, this study adds to the limited literature on the influence of SDH on weight status of preschoolers.
Chinese ethnicity was associated with lower risk of excess weight among children; this aligns with existing findings of lower excess weight among children of Chinese ethnicity in America and children and youth of East Asian descent in Canada.31,32 However, our finding that South Asian ethnicity was associated with increased risk for both child underweight and child obesity is noteworthy and novel. While a similar trend was observed for children living in South Asian countries, the populations studied were low- to middle-income.33 To our knowledge, there is limited literature focussing on South Asian ethnicity and child underweight in high-income countries such as Canada.
We may have found an increased risk of child underweight associated with South Asian ethnicity because our study did not apply ethnicity-specific BMI cut-offs to define child weight status. These cut-offs can account for unique ethnicity-specific differences in body type; for example, a UK-based study reported increased body fat in South Asian (vs. White) child populations and called for lowered BMI cut-offs to categorize South Asian children.34 However, we are confident in WHO criteria, which are based on the WHO guidelines, which were developed using large samples of children raised in optimal environments from various regions, including India.35 The Dietitians of Canada, who have taken similar ethnicity-specific differences into consideration, still recommend the WHO charts as the best available reference for monitoring growth.26 Overall, further qualitative research may provide insight into the differences in outcomes with respect to ethnicity.
Our findings suggest a protective effect of maternal immigrant status against child underweight and obesity, which may be explained by new immigrants’ retention of healthier eating habits.36 Our findings contrast with a previous report that second-generation immigrant children (parents born in Canada but grandparents born outside Canada) had higher mean BMI z-scores relative to first-generation (parents born outside Canada) and to other children of parents born in Canada, although this is likely due to the older populations that were included in the report.11 Given the lack of published data on the association between maternal immigrant status and child underweight in high-income countries such as Canada, our findings provide a unique perspective on this issue.
Our observation that increased neighbourhood-level household income was associated with lower risk of excess weight aligns with the existing literature. For instance, Fiechtner et al.37 included a wide age range (4–18 years) in their study of neighbourhood median income and child weight status, finding that lower neighbourhood-level income amplified detrimental effects of food environment (e.g. close proximity to convenience stores) on increased child BMI z-score. Based on data collected from children (aged 2–11years) from Canada, Oliver and Hayes38 reported similar findings, with higher BMI percentile values for children living in low-income neighbourhoods. The association between neighbourhood-level income and child weight status may be related to differences in neighbourhood structure, which may pose barriers to maintaining a healthy diet (e.g. grocery store39and fast food outlet access40) and physical activity (e.g. increased screen time41) in children.
Our finding that increased material deprivation was associated with greater risk of overweight and obesity aligns with findings by Carter et al.,13 who reported a positive association between neighbourhood material deprivation and weight gain in children aged 4 to 10 years. The influence of material deprivation on children’s weight status may operate through parental income- or employment-related barriers to healthy lifestyle habits (e.g. limited time, limited funds), which manifest as overweight or obesity in children. Interestingly, we found that increased material deprivation was associated with greater risk of child underweight as well. There is currently scant literature on associations between material deprivation and child underweight in high-income countries. However, one study in the UK did not find an association between deprivation and underweight prevalence in children.42 Given that our study is the first to suggest an association between material deprivation and underweight in a high-income country, further study into the mechanism by which material deprivation affects weight status is needed to offer insight into this association.
We also found some increased risk of excess weight in children associated with social deprivation. Our findings contrast with Carter et al.,13 who found an inverse association between social deprivation and child weight gain. However, the study included a smaller cohort (n=1580) and broader age range (4–10 years of age), whereas our findings illustrate a more comprehensive picture of our population’s specific age range. A possible explanation for the association we found is that socially deprived parents may be more prone to stress and depression, which compromise their motivation to encourage healthy eating and physical activity in children. Positive associations have been noted between maternal chronic depression and increased risk of child overweight.43
Strengths and limitations
Our study contributes to the limited literature on determinants of preschool child weight status in Canada by highlighting some of the complex associations between social determinants of health and child weight status. This project used a large database of children and objective variable measures that were collected and analyzed using uniform procedures.
Despite these strengths, we acknowledge certain limitations. First, the ethnicity algorithm employed in our study only classified data into three categories, which limits the generalizability and precision of our findings towards ethnicities that are not South Asian or Chinese. Since children were only classified based on surnames, it is also possible that children of mixed ethnicity may have been misclassified. Nevertheless, the algorithm generated a high-level ethnicity categorization, and we were still able to detect varying risks between each of the ethnicity categories. Second, this study had a range of data availability over the years of data collection, although we still were able to work with a large and informative dataset. Third, the study lacked data on children beyond Edmonton and Calgary, which limited our perspective on rural and remote communities, where excess weight may be more prevalent. Fourth, the Alberta Health Care Insurance Plan Central Stakeholder Registry used to determine maternal immigrant status was unable to capture secondary migration (i.e. prior residence in a different province) and duration of residence in Alberta, which might have provided additional perspective on associations between having mothers that immigrated to Canada and child weight. Fifth, given that this cohort does not include homeschooled children or children who were not vaccinated, there is potential bias due to the absence of representation of this population.
Our study suggests that policies and interventions intended to maintain healthy weight in children should target populations based on SDH. Policies designed to reduce obesogenic factors related to low income (e.g. food accessibility, recreational opportunities) or interventions that adopt culturally sensitive approaches to at-risk populations (e.g. South Asian ethnicity) may be beneficial.
Conclusion
In a large, retrospective, population-based cohort study, we found significant associations between ethnicity, maternal immigrant status, neighbourhood-level household income, deprivation and child weight status. Our findings suggest a burden of malnutrition in the South Asian ethnic population, a protective effect of maternal immigrant status on unhealthy child weight, associations between increased material deprivation and child underweight and associations between increased social deprivation and child excess weight. Further research into the mechanisms behind these associations is required to inform policy planning and targeted interventions.
Acknowledgements
This study was funded by a grant from the Novo Nordisk Alberta Diabetes (NOVAD) Fund Competition, which was provided by the University Hospital Foundation, Government ofAlberta and Novo Nordisk Canada, Inc., and was based, in part, on data provided by Alberta Health and Alberta Health Services (AHS). We thank the Customer Relationship Management and Data Access Unit at Alberta Health for creating the linked database. PK holds a Canadian Institutes of Health Research Chair in Sex and Gender and a Research Chair from the Heart and Stroke Foundation of Canada. GDCB holds the AHS Chair in Obesity Research.
Data availability statement
The data underlying this article were provided by the Government of Alberta under the terms of a research agreement. Inquiries respecting access to the data can be made to health.resdata@gov.ab.ca.
Conflicts of interest
GDCB served as a member of the Novo Nordisk Canada Pediatric Expert Obesity National Advisory Board. The other authors have no conflicts of interest to declare.
Authors’ contributions and statement
JW, GDCB—conceptualization. JW, DCD, AS, GDCB—methodology. AS, JW—formal analysis. JW—writing—original draft. JW, PK, AS, SI, DCD, LEM, AMH, GDCB—writing—review & editing.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Alberta or of the Government of Canada. Neither the Government of Alberta nor Alberta Health express any opinion in relation to this study.
References
- Harvard University. Boston(MA): Lifelong health [Internet] Available from: https://developingchild.harvard.edu/science/deep-dives/lifelong-health/ [Google Scholar]
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS, et al. Childhood obesity: causes and conse-quences. J Family Med Prim Care. 2015;4((2)):187–92. doi: 10.4103/2249-4863.154628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockerham WC, Hamby BW, Oates GR, et al. The social determinants of chronic disease. Am J Prev Med. 2017;52((1 Suppl 1)):S5–S12. doi: 10.1016/j.amepre.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez MA, Adair LS, et al. Severity and timing of stunting in the first two years of life affect performance on cognitive tests in late childhood. J Nutr. 1999;129((8)):1555–62. doi: 10.1093/jn/129.8.1555. [DOI] [PubMed] [Google Scholar]
- White J, Rehkopf D, Mortensen LH, et al. Trends in socioeconomic inequalities in body mass index, underweight and obesity among English children, 2007– 2008 to 2011–2012. pone. 2016:e0147614–62. doi: 10.1371/journal.pone.0147614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly JJ, Kelly J, et al. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011:891–8. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- WHO. Geneva(CH): Obesity and overweight [Internet] Available from: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight. [Google Scholar]
- Lighter J, Phillips M, Hochman S, et al, et al. Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission [letter] Clin Infect Dis. 2020;71((15)):896–7. doi: 10.1093/cid/ciaa415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Geneva(CH): Social determinants of health [Internet] Available from: https://www.who.int/health-topics/social-determinants-of-health. [Google Scholar]
- Chatham RE, Mixer SJ, et al. Cultural influences on childhood obesity in ethnic minorities: a qualitative systematic review. J Transcult Nurs. 2020:87–99. doi: 10.1177/1043659619869428. [DOI] [PubMed] [Google Scholar]
- Blanchet R, Giroux I, Sanou D, Batal M, Nana CP, Bodnaruc AM, et al. The impact of generation status on weight of immigrant and non-immigrant school-aged children living in minority situation: preliminary results. Can J Diabetes. 2015:S39–99. [Google Scholar]
- Anderson LN, Fatima T, Shah B, et al, et al. Income and neighbourhood deprivation in relation to obesity in urban dwelling children 0–12 years of age: a cross-sectional study from 2013 to 2019. Anderson LN, Fatima T, Shah B, et al. 2021:274–80. doi: 10.1136/jech-2021-216455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter MA, Dubois L, Tremblay MS, Taljaard M, et al. The influence of place on weight gain during early childhood: a population-based, longitudinal study. J Urban Health. 2013;90((2)):224–39. doi: 10.1007/s11524-012-9712-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois L, Girad M, et al. Accuracy of maternal reports of pre-schoolers’ weights and heights as estimates of BMI values. Int J Epidemiol. 2007:132–8. doi: 10.1093/ije/dyl281. [DOI] [PubMed] [Google Scholar]
- Doolen J, Alpert PT, Miller SK, et al. Parental disconnect between perceived and actual weight status of children: a metasynthesis of the current research. J Am Acad Nurse Pract. 2009;21((3)):160–6. doi: 10.1111/j.1745-7599.2008.00382.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Costa MV, Odunlami AO, Mohammed SA, et al. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14((Suppl 6)):S8–S17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. Ottawa(ON): Census profile, 2016 Census [Internet] Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E. [Google Scholar]
- AHS. Edmonton(AB): Childhood Growth Measurement Protocol [Internet] Available from: https://www.albertahealthservices.ca/info/Page9810.aspx. [Google Scholar]
- Kaul P, Bowker SL, Savu A, Yeung RO, Donovan LE, Ryan EA, et al. Association between maternal diabetes, being large for gestational age and breast-feeding on being overweight or obese in childhood. Diabetologia. 2019;62((2)):249–58. doi: 10.1007/s00125-018-4758-0. [DOI] [PubMed] [Google Scholar]
- Cummins C, Winter H, Maric R, Silcocks P, et al. An assessment of the Nam Pehchan computer program for the identification of names of South Asian ethnic origin. J Public Health. 1999;21((4)):401–6. doi: 10.1093/pubmed/21.4.401. [DOI] [PubMed] [Google Scholar]
- Quan H, Wang F, Schopflocher D, et al, et al. Development and validation of a surname list to define Chinese ethnicity. Med Care. 2006;44((4)):328–33. doi: 10.1097/01.mlr.0000204010.81331.a9. [DOI] [PubMed] [Google Scholar]
- Shah BR, Chiu M, Amin S, Ramani M, Sadry S, Tu JV, et al. Surname lists to identify South Asian and Chinese ethnicity from secondary data in Ontario, Canada: a validation study. BMC Med Res Methodol. 2010:42–33. doi: 10.1186/1471-2288-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pampalon R, Hamel D, Gamache P, Raymond G, et al. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29((4)):178–91. [PubMed] [Google Scholar]
- Pampalon R, Hamel D, Gamache P, Simpson A, Philiberet MD, et al. Validation of a deprivation index for public health: a complex exercise illustrated by the Quebec index. Chronic Dis Inj Can. 2014;34((1)):12–22. [PubMed] [Google Scholar]
- Index of material and social deprivation compiled by the Bureau d’information et d’tudes en sant des populations (BIESP) from 1991, 1996, 2001, 2006, 2011 and 2016 Canadian Census data [Internet] Institut national de sant publique du Qubec (INSPQ) Available from: https://www.inspq.qc.ca/en/deprivation/material-and-social-deprivation-index. [Google Scholar]
- Dietitians of Canada. Ottawa(ON): WHO growth charts set 2 [Internet] Available from: https://www.dietitians.ca/Advocacy/Interprofessional-Collaborations-(1)/WHO-Growth-Charts/WHO-Growth-Charts-Set-2. [Google Scholar]
- Zheng B, et al. Summarizing the goodness of fit of generalized linear models for longitudinal data. Stat Med. 2000:1265–75. doi: 10.1002/(sici)1097-0258(20000530)19:10<1265::aid-sim486>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Calster B, Belle V, Vergouwe Y, Timmerman D, Huffel S, Steyerberg EW, et al. Extending the c-statistic to nominal polytomous outcomes: the polytomous discrimination index. Stat Med. 2012;31((23)):2610–26. doi: 10.1002/sim.5321. [DOI] [PubMed] [Google Scholar]
- Dover DC, Islam S, Westerhout CM, Moore LE, Kaul P, Savu A, et al. Computing the polytomous discrimination index. Stat Med. 2021;40((16)):3667–81. doi: 10.1002/sim.8991. [DOI] [PubMed] [Google Scholar]
- Kuss O, McLerran D, et al. A note on the estimation of the multinomial logistic model with correlated responses in SAS. Comput Methods Programs Biomed. 2007;87((3)):262–9. doi: 10.1016/j.cmpb.2007.06.002. [DOI] [PubMed] [Google Scholar]
- Shields M, et al. Overweight and obesity among children and youth. Health Rep. :17(3):27–42. [PubMed] [Google Scholar]
- Jain A, Mitchell S, Chirumamilla R, Zhang J, Horn IB, Lewin A, Huang ZJ, et al. Prevalence of obesity among young Asian-American children. Child Obes. 2012;8((6)):518–25. doi: 10.1089/chi.2011.0077. [DOI] [PubMed] [Google Scholar]
- Hossain FB, Shawon MS, Al-Abid MS, Mahmood S, Adhikary G, Bulbul MM, et al. Double burden of malnutrition in children aged 24 to 59 months by socioeconomic status in five South Asian countries: evidence from demographic and health surveys. BMJ Open. 2020;10((3)):e032866–25. doi: 10.1136/bmjopen-2019-032866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyre EL, Duncan M, Nevill A, et al. South Asian children have increased body fat in comparison to white children at the same body mass index. Children. 2017;4((11)):102–25. doi: 10.3390/children4110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Geneva(CH): 2006. WHO child growth standards: length/ height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. [Google Scholar]
- Hyman I, Guruge S, Cameron J, Micevski V, et al. Promotion of healthy eating: among new immigrant women in Ontario. Can J Diet Pract Res. 2002;63((3)):125–9. doi: 10.3148/63.3.2002.125. [DOI] [PubMed] [Google Scholar]
- Fiechtner L, Sharifi M, Sequist T, et al, et al. Food environments and childhood weight status: effects of neighborhood median income. Child Obes. 2015;11((3)):260–8. doi: 10.1089/chi.2014.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver LN, Hayes MV, et al. Effects of neighbourhood income on reported body mass index: an eight year longitudinal study of Canadian children. BMC Public Health. 2008 doi: 10.1186/1471-2458-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pabayo R, Spence JC, Cutumisu N, Casey L, Storey K, et al. Sociodemographic, behavioural and environmental correlates of sweetened beverage consumption among pre-school children. Pub Health Nutr. 2012;15((8)):1338–46. doi: 10.1017/S1368980011003557. [DOI] [PubMed] [Google Scholar]
- Smoyer-Tomic KE, Spence JC, Raine KD, et al, et al. The association between neighborhood socioeconomic status and exposure to supermarkets and fast food outlets. Health Place. 2008:740–54. doi: 10.1016/j.healthplace.2007.12.001. [DOI] [PubMed] [Google Scholar]
- Carson V, Spence JC, Cutumisu N, Cargill L, et al. Association between neighborhood socioeconomic status and screen time among pre-school children: a cross-sectional study. BMC Public Health. 2010:367–54. doi: 10.1186/1471-2458-10-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart R, Reilly JJ, Hughes A, et al, et al. Trends in socioeconomic inequalities in underweight and obesity in 5-year-old children, 2011–2018: a population-based, repeated cross-sectional study. BMJ Open. 2021;11((3)):a population–based, repeated cross. doi: 10.1136/bmjopen-2020-042023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampard AM, Franckle RL, Davison KK, et al. Maternal depression and childhood obesity: a systematic review. Prev Med. 2014:60–7. doi: 10.1016/j.ypmed.2013.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]