Abstract
This was a single-centre, retrospective study of transgender women undergoing genital gender-affirming surgery. A chart study was conducted, recording individual demographics, all genital surgical procedures, and surgical techniques. Procedure incidence, techniques employed, and demographic variations over the years were analysed.
Introduction
The number of transgender people seeking medical and surgical care is increasing worldwide1,2. Genital gender-affirming surgery (gGAS) in transgender women may comprise bilateral orchiectomy, vaginoplasty, or gender-confirming vulvoplasty (GCV). Vaginoplasty combines penectomy, orchiectomy, labiaplasty, clitoroplasty, and creation, and lining, of a neovaginal canal. In GCV, no neovaginal canal is dissected and only external female genitalia are constructed.
Penile inversion vaginoplasty is the vaginoplasty standard, in which a penile skin flap is used for the neovaginal lining3. Alternatives are full- or partial-thickness skin graft, or intestinal or peritoneal vaginoplasty4–6. Genital anatomy may influence the chosen technique. This article provides information on demographic and surgical gGAS trends among transgender women in the authors’ institution.
Methods
The majority of surgical transgender healthcare countrywide is performed in the authors’ centre, making it suited for analyses of demographic and surgical trends. In the diagnostic and treatment phases, the World Professional Association for Transgender Health Standard of Care is followed7. Individuals may opt for gGAS after thorough psychological screening, 12 months of hormone treatment, more than 6 months of testosterone suppression, surgical eligibility screening, and multidisciplinary consultation. In this centre, smoking, BMI below 18 and above 30 kg/m2 are considered contraindications to vaginoplasty and GCV. Institutional review board approval of the study protocol was obtained (METC2014322).
Retrospective chart study
All transgender women who underwent primary gGAS between January 1980 and January 2020 were identified from a departmental database.
A retrospective chart study was performed, with recording of gGAS procedures, surgical (sub)techniques, individual demographics (age, previous use of puberty-suppressing hormones, age, and Tanner stage at start of puberty suppression, BMI, history of smoking and drug abuse, fertility preservation), neovaginal depth, measured after surgery and, if present, revision vaginoplasty procedures, techniques, and indications.
Sexual orientation (towards men, towards women, towards both men and women, asexual, unclear for the individual) has been asked at surgical intake at the outpatient clinic since 2011 as an exploratory step in the assessment of postoperative sexual desires.
Procedure incidence, techniques employed, and demographic variations over the years were analysed.
Statistical analysis
Categorical variables were compared using the χ2 test; independent-samples t test or ANOVA was used for normally distributed continuous variables, and the Mann–Whitney U test or Kruskal–Wallis test for those with a non-normal distribution. Predictors for choosing fertility preservation were identified using backward logistic regression.
Results
Trends in genital gender-affirming surgery
A total of 1531 transgender women underwent gGAS at this institution during the study period. The number of transgender women undergoing gGAS increased over time, particularly in recent years (Fig. S1).
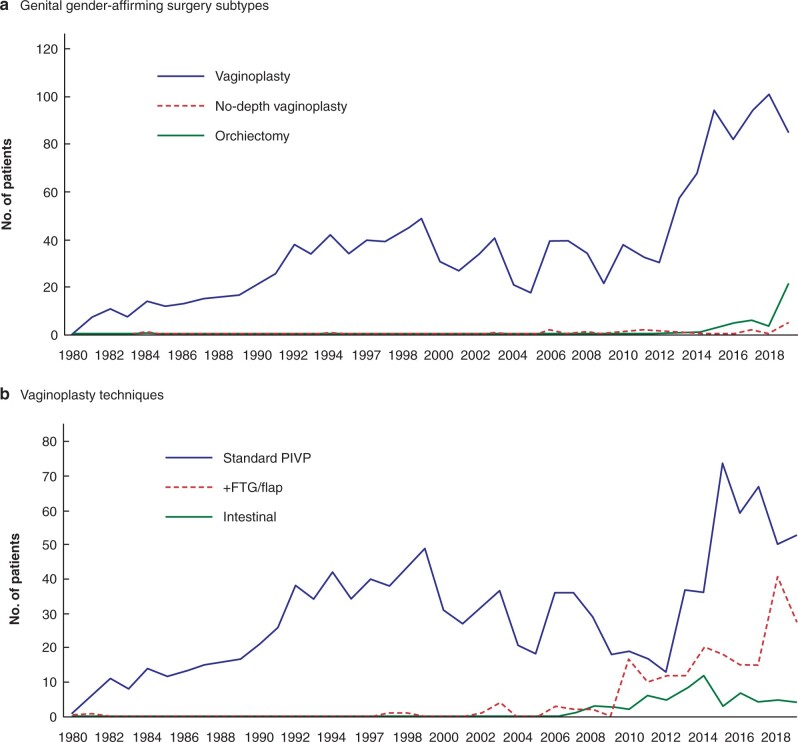
Of the 1531 transgender women, 1468 (95.9 per cent)underwent vaginoplasty (1405 penile inversion, 63 intestinal vaginoplasty), 19 (1.2 per cent) GCV, and 44 (2.9 per cent) orchiectomy (Table 1). Mean(s.d.) neovaginal depth after vaginoplasty was 13.1(2.1) cm. Before 2002, almost all transgender women underwent vaginoplasty as gGAS. More recently, orchiectomy and GCV were requested more frequently. For example, in 2019, 85 vaginoplasty procedures (77 per cent), 21 orchiectomies (19 per cent), and five GCVs (5 per cent) were performed (Fig. 1)8,9.
Table 1.
Demographics of transgender women undergoing primary genital gender-affirming surgery at the authors’ institution between January 1980 and January 2020
| Total | Vaginoplasty | Orchiectomy | GCV | P | |
|---|---|---|---|---|---|
| (n = 1531) | (n = 1468) | (n = 44) | (n = 19) | ||
| Age at surgery (years)* | 33 (25–44) | 33 (24–44) | 32 (26–45) | 54 (45–60) | <0.001# |
| BMI at surgery (kg/m2) † | 23.7(3.5) | 23.6(3.3) | 26.4(6.6) | 24.0(2.4) | <0.001** |
| History of puberty suppression | 135 (8.8) | 132 (9.0) | 3 (6.8) | 0 (0) | 0.355 |
| Sexual orientation at surgical intake ‡ | 699 (100) | 645 (100) | 42 (100) | 12 (100) | <0.001 |
| Solely towards men | 372 (53) | 357 (55) | 13 (31) | 2 (17) | |
| Solely towards women | 217 (31) | 194 (31) | 15 (36) | 8 (75) | |
| Towards both men and women | 85 (12) | 75 (12) | 9 (21) | 1 (8) | |
| Asexual | 4 (1) | 1 (0.2) | 2 (5) | 1 (8) | |
| Unclear for the individual | 14 (2) | 11 (2) | 3 (7) | 0 (0) | |
| Unknown to researcher | 7 (1) | 7 (1) | 0 (0) | 0 (0) | |
| Opted for fertility preservation § | 117 of 1047 (11) | 109 of 987 (11) | 6 of 43 (14) | 2 of 17 (12) | 0.832 |
Values in parentheses are percentages unless indicated otherwise; values are median (i.q.r.) and †mean (s.d.). Data available for 2011–2019; §data available for 2000–2019. GCV, gender-confirming vulvoplasty. ¶χ2 test, except #Kruskal–Wallis test and **ANOVA.
Fig. 1.
Genital gender-affirming surgery subtypes and vaginoplasty techniques over time.
a Genital gender-affirming surgery subtypes and b vaginoplasty techniques. PIVP, penile inversion vaginoplasty; FTG, full-thickness skin graft.
Intestinal vaginoplasty was performed as the primary gGAS procedure since 2007 and undertaken 63 times since. Surgical indications were: penoscrotal hypoplasia owing to a history of puberty suppression (46 procedures), shortage of penile skin due to circumcision (7), and biological variation (10). A sigmoid (62) or ileal (1) segment was used as neovaginal lining.
Of 1468 primary vaginoplasty procedures, 34 individuals (2.3 per cent) underwent revision vaginoplasty. Indications and techniques for revision vaginoplasty are provided in Table S1. Currently, laparoscopic intestinal vaginoplasty is preferred for this indication, because of the lower risk of rectal perforation10.
Median age at the time of surgery was 33 (i.q.r. 25–44) years (Figs S2 and S3). Individuals who opted for GCV were generally older, had no history of puberty suppression, and were more frequently sexually oriented towards women (Table 1).
Puberty suppression
An increase in individuals with a history of puberty suppression was observed, from 2000 (2 of 31) to 2019 (18 of 111, 16 per cent) (Fig. S4). Age and Tanner stage at the start of puberty suppression influenced the vaginoplasty technique chosen. When puberty suppression was started at Tanner stage G2–3, penoscrotal hypoplasia led to the choice of intestinal vaginoplasty in approximately 70 per cent of individuals (Table S2).
Fertility preservation
Over time, more transgender women opted for semen cryopreservation (Fig. S5). In 2000, 1 of 31 transgender women opted for semen cryopreservation before gGAS. In 2019, this number increased to 28 of 111 (25 per cent). Being younger at time of gGAS (odds ratio (OR) 0.90, 95 per cent c.i. 0.87 to 0.93; P < 0.001), having a history of puberty suppression (OR 5.01, 2.42 to 10.41; P < 0.001), and undergoing gGAS more recently (OR 1.21, 1.12 to 1.34) were identified as predictors for choosing for fertility preservation.
Discussion
Parallel to the observed increase in transgender women seeking psychological and medical care, a drastic increase in gGAS procedures was observed. Vaginoplasty is the most commonly performed gGAS procedure, although a rise in orchiectomy procedures was observed in 2019.
The observed surgical trends are a result of patient-related factors (more transgender individuals seeking medical care), societal factors (changed laws, increased awareness and recognition of gender diversity, insurance policies, technological factors), and institutional factors (capacity, availability of specific surgical skills). Currently, the choice of a specific gGAS subtype is based on a combination of surgical and anatomical possibilities, and individual preferences. GCV and orchiectomy as surgical options may be a result of client-centred care and shared-decision making.
Individuals undergoing specific subtypes of gGAS represent unique subgroups, with intergroup demographic differences. Reported sexual orientation was more frequently towards men in the vaginoplasty group, which may reflect postoperative sexual desires. Individuals undergoing GCV were older and did not have a history of puberty suppression.
Puberty suppression has a positive effect on quality of life in transgender women who apply for treatment during their adolescent years11,12. An increase was observed in transgender women who used puberty-suppressing hormones opting for gGAS. When starting puberty suppression at a prepubertal or early pubertal stage (Tanner G2–3), penoscrotal hypoplasia may limit the surgical possibilities for vaginoplasty owing to a shortage of penoscrotal skin, which makes standard penile inversion vaginoplasty impossible. Alternative strategies, such as additional (scrotal) skin grafts/scrotal flaps or skin graft, intestinal or peritoneal vaginoplasty may be necessary6,13,14. This should be a point of attention for users and prescribers of puberty-suppressing hormones, and should be discussed with adolescents opting for this treatment15. If the percentage increase in individuals taking puberty-suppressing hormones continues, the incidence of non-standard vaginoplasty procedures will increase simultaneously. With increased use of puberty-suppressing hormones, gender surgeons may need to gain experience in alternative vaginoplasty techniques.
The number of transgender women opting for fertility preservation before gGAS increased over the years to 25 per cent in 2019, whereas rates reported in the literature vary from 0 to 62 per cent16–19. Since 2015, extensive fertility preservation counselling has been implemented in the authors’ clinic and semen cryopreservation costs have been covered by insurance. Improved availability of, and access to, fertility care may play a major role in its increased use. The increase in individuals starting puberty suppression at early pubertal stages, when serum testosterone concentrations are insufficient for spermatogenesis, may lead to an increase in individuals without options for preservation of fertility.
A strength of this study is the unique large study population in a centre with long-term gGAS experience. A limitation is its retrospective nature.
This study has identified remarkable demographic trends. The topic of fertility preservation and the influence of puberty suppression on surgical technique must be taken into account during counselling of transgender women.
Disclosure. The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS online.
Supplementary Material
Contributor Information
W B van der Sluis, Department of Plastic, Reconstructive and Hand Surgery, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands; Centre of Expertise on Gender Dysphoria, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands.
I de Nie, Centre of Expertise on Gender Dysphoria, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands; Department of Endocrinology, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands.
T D Steensma, Centre of Expertise on Gender Dysphoria, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands; Department of Medical Psychology, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands.
N M van Mello, Centre of Expertise on Gender Dysphoria, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands; Department of Gynaecology and Obstetrics, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands.
B I Lissenberg-Witte, Department of Epidemiology and Data Science, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands.
M -B Bouman, Department of Plastic, Reconstructive and Hand Surgery, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands; Centre of Expertise on Gender Dysphoria, Amsterdam UMC, location VUMC, Amsterdam, The Netherlands.
References
- 1. Nolan IT, Kuhner CJ, Dy GW. Demographic and temporal trends in transgender identities and gender confirming surgery. Transl Androl Urol 2019;8:184–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arcelus J, Bouman WP, Van Den Noortgate W, Claes L, Witcomb G, Fernandez-Aranda F. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry 2015;30:807–815 [DOI] [PubMed] [Google Scholar]
- 3. Buncamper ME, van der Sluis WB, van der Pas RS, Özer M, Smit JM, Witte BI et al. Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women. Plast Reconstr Surg 2016;138:999–1007 [DOI] [PubMed] [Google Scholar]
- 4. Watanyusakul S. Vaginoplasty modifications to improve vulvar aesthetics. Urol Clin North Am 2019;46:541–554 [DOI] [PubMed] [Google Scholar]
- 5. Bouman MB, van Zeijl MC, Buncamper ME, Meijerink WJ, van Bodegraven AA, Mullender MG. Intestinal vaginoplasty revisited: a review of surgical techniques, complications, and sexual function. J Sex Med 2014;11:1835–1847 [DOI] [PubMed] [Google Scholar]
- 6. Jacoby A, Maliha S, Granieri MA, Cohen O, Dy GW, Bluebond-Langner R et al. Robotic Davydov peritoneal flap vaginoplasty for augmentation of vaginal depth in feminizing vaginoplasty. J Urol 2019;201:1171–1176 [DOI] [PubMed] [Google Scholar]
- 7. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J et al. Standards of care for the health of transsexual, transgender, and gender nonconforming people, 7th version. Int J Transgend 2012;13:165–232 [Google Scholar]
- 8. Van der Sluis WB, Steensma TD, Bouman MB. Orchiectomy in transgender individuals: a motivation analysis and report of surgical outcomes. Int J Transgender Health 2020;21:176–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Van der Sluis WB, Steensma TD, Timmermans FW, Smit JM, de Haseth KB, Özer M et al. Gender-confirming vulvoplasty in transgender women in the Netherlands: incidence, motivation analysis, and surgical outcomes. J Sex Med 2020;17:1566–1573 [DOI] [PubMed] [Google Scholar]
- 10. Van der Sluis WB, Bouman MB, Buncamper ME, Mullender MG, Meijerink WJ. Revision vaginoplasty: a comparison of surgical outcomes of laparoscopic intestinal versus perineal full-thickness skin graft vaginoplasty. Plast Reconstr Surg 2016;138:793–800 [DOI] [PubMed] [Google Scholar]
- 11. de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics 2014;134:696–704 [DOI] [PubMed] [Google Scholar]
- 12. Mahfouda S, Moore JK, Siafarikas A, Zepf FD, Lin A. Puberty suppression in transgender children and adolescents. Lancet Diabetes Endocrinol 2017;5:816–826 [DOI] [PubMed] [Google Scholar]
- 13. Buncamper ME, van der Sluis WB, de Vries M, Witte BI, Bouman MB, Mullender MG. Penile inversion vaginoplasty with or without additional full-thickness skin graft: to graft or not to graft? Plast Reconstr Surg 2017;139:649e–656e [DOI] [PubMed] [Google Scholar]
- 14. Bouman MB, van der Sluis WB, Buncamper ME, Özer M, Mullender MG, Meijerink WJ. Primary total laparoscopic sigmoid vaginoplasty in transgender women with penoscrotal hypoplasia: a prospective cohort study of surgical outcomes and follow-up of 42 patients. Plast Reconstr Surg 2016;138:614e–623e [DOI] [PubMed] [Google Scholar]
- 15. van de Grift TC, van Gelder ZJ, Mullender MG, Steensma TD, de Vries ALC, Bouman MB. Timing of puberty suppression and surgical options for transgender youth. Pediatrics 2020;146:e20193653. [DOI] [PubMed] [Google Scholar]
- 16. Chen D, Simons L, Johnson EK, Lockart BA, Finlayson C. Fertility preservation for transgender adolescents. J Adolesc Health 2017;61:120–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nahata L, Tishelman AC, Caltabellotta NM, Quinn GP. Low fertility preservation utilization among transgender youth. J Adolesc Health 2017;61:40–44 [DOI] [PubMed] [Google Scholar]
- 18. Pang KC, Peri AJS, Chung HE, Telfer M, Elder CV, Grover S et al. Rates of fertility preservation use among transgender adolescents. JAMA Pediatr 2020;174:890–891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brik T, Vrouenraets LJJJ, Schagen SEE, Meissner A, de Vries MC, Hannema SE. Use of Fertility preservation among a cohort of transgirls in the Netherlands. J Adolesc Health 2019;64:589–593 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.