Abstract
Introduction:
The goal of neuromuscular scoliosis (NMS) surgery is to improve sitting balance, facilitate daily care, and alleviate pain. In nonambulatory patients, where sitting balance is key, fusion to the pelvis is usually required. However, in minimally ambulatory patients, fusion to the pelvis remains controversial, and there is considerable practice variability in this patient population. The purpose of this study is to evaluate and summarize the available evidence regarding fusion constructs in minimally ambulatory patients with NMS and to provide expert opinion regarding when fusion to the pelvis should be considered.
Methods:
A search of the English literature was performed using PubMed to identify papers pertaining to patients with NMS treated with instrumented posterior spinal fusion. Papers published before 2000, case reports, and level V evidence were excluded.
Results:
The authors identified 8 studies for review. The majority included both nonambulatory and minimally ambulatory patients. Structured review of the literature demonstrated fusion to the pelvis may allow for greater curve and pelvic obliquity correction, but it is also associated with increased blood loss and operative time. There is no evidence that fusing to the pelvis decreases ambulatory status in minimally ambulatory patients.
Conclusions:
In minimally ambulatory patients with NMS, fusion short of the pelvis may be considered in patients with adequate head control without the presence of hip subluxation or dislocation and when pelvic obliquity is <15 degrees. Fusion to the pelvis is recommended in patients who do not meet these criteria.
Keywords: neuromuscular scoliosis, pelvic fixation, pelvic instrumentation, spinal fusion
Progressive neuromuscular scoliosis (NMS) impairs daily care and sitting balance and can lead to poor gastrointestinal motility and cardiac and respiratory compromise.1–3 The goals of treatment are to preserve function, improve sitting balance, promote respiratory and digestive function, and reduce the caregiver burden.1,2,4,5 Surgical intervention aims to reconstruct a well-aligned, compensated spine over a balanced pelvis while minimizing complications.2,6,7
Pelvic obliquity (PO) is frequently seen in children with NMS,8 which may be managed with the extension of the fusion to include the pelvis. Techniques for pelvic instrumentation commonly used at present are iliac and sacral-alar-iliac screws.9 Although modern techniques result in reduced implant-related complications as compared to their predecessors, prominence, pseudoarthrosis, implant failure/fracture, and wound complications persist regardless of technique.1,2 Pelvic instrumentation is also associated with additional incremental risks, including longer operative times, more technically demanding surgery, and increased infection risk.10–13
Overall, literature regarding when to include pelvic instrumentation is largely limited to retrospective reviews of small, diverse patient populations. Further, some authors have described successful results in treating NMS fusing short of the pelvis. The goal of this review is to summarize the current literature regarding pelvic instrumentation in the management of NMS, to highlight its advantages and disadvantages, and to provide an expert opinion of when it should be included as part of the surgical treatment of this complex, heterogenous patient population.
METHODS
A search of PubMed was performed to find literature published between January 2000 and January 2020 that examined the use of pelvic instrumentation in the management of NMS. Case reports and level V evidence were excluded. This search was conducted using MeSH and EMBASE terms. The search terms included “scoliosis,” “neuromuscular”, “pelvis fixation”, or synonyms of these terms. Studies were included based on the following: (1) patients diagnosed with NMS, (2) patients treated with posterior spinal fusion with fixation to the low lumbar spine or pelvis, and (3) cohort size >20 patients.
Eight studies met inclusion criteria and were included for review. Data extracted from these studies included the following: author, publication year, journal, type of study, cohort size, ambulatory status of included patients (if described), indications for pelvic instrumentation (when performed), preoperative and postoperative major curve angle, PO, coronal and sagittal balance, the presence of complications, and duration of follow-up.
The results section highlights the most impactful studies that guide our decision making in treating minimally ambulatory patients with NMS. The literature is handicapped in that few studies indicate the ambulatory status of the included population, and almost no studies are exclusive of nonambulatory subjects.
The senior authors of this publication are both board-certified pediatric orthopaedic surgeons who treat patients with NMS. The authors offer their expert perspective on when to consider fusion to the pelvis as part of surgical management for minimally ambulatory patients with NMS.
RESULTS
Table 1 has a summary of the 8 studies identified during our literature review.
TABLE 1.
Summary of Studies Included in Review
| Reference | Diagnosis | No. of Patients | Comparison Groups | Follow-up Duration | Outcomes | Take Home Message |
|---|---|---|---|---|---|---|
|
| ||||||
| McCall and Hayes6 | CP | 55 | Fusion to pelvis with unit rods vs. fusion to L5 with U rods | Mean 4.3 y | Similar correction of scoliosis and PO No significant loss of correction at follow-up Fusions to L5 had reduced blood loss, postoperative infections, and operative time |
Fusion to L5 is a viable alternative to fusion to the sacrum, with the benefits of decreased blood loss, decreased operating time, and maintenance of a mobile L5/S1 disk space |
| Mohamad et al11 | 129 CP, 9 Rett syndrome, 8 myelomeningocele, 29 other | 175 | Fusion to pelvis vs. L5 or above | — | 44% of patients with sacropelvic fixation experienced complications, compared with 26% of patients with fusions ending at L5 or above | Pelvic instrumentation may be a risk factor for perioperative complications in patients with NMS |
| Takaso et al14 | DMD | 28 | Fusion to L5 in all, PO < 10 degrees and L5 tilt < 15 degrees vs. PO > 10 degrees and L5 tilt > 15 degrees | Minimum 2y, mean 3.3 y | Residual PO measuring > 15 degrees if preoperative PO > 15 degrees No significant loss of curve correction or PO at 2 y |
L5 is a safe and effective alternative to fusion to the pelvis in patients with DMD scoliosis if L5 tilt is <15 degrees, indicating a stable L5/S1 articulation |
| Modi et al9 | 28 CP, 17 DMD, 10 SMA | 55 | Group 1: PO > 15 degrees, fusion to lower lumbar Group II: PO > 15 degrees, fusion to pelvis with iliac screws Group III: PO <15 degrees, fusion to lower lumbar |
Minimum 2y, mean 2.5 y | Correction of major curve angle maintained in all groups Group I demonstrated a significant loss of PO correction with associated deterioration in sitting balance |
In PO <15 degrees, correction and balance can be maintained long term with fusion ending at the lumbar level |
| Akesen et al15 | 11 CP, 5 muscular dystrophy, 4 myelomeningocele, 4 epilepsy, and 12 other | 36 | Fusion to S1 vs. pelvis with iliac screws | Minimum 6 mo, median 20 mo | Fusion to S1 demonstrated a significant correction in thoracosacral angle Fusion to pelvis resulted in a significant correction of PO and significantly greater improvement in physical SF-36 score No complications recorded for pelvic instrumentation group |
Fusion to the pelvis with iliac screws may result in better functional outcomes without increased risk of complications |
| Nielson et al7 | 185 CP, 26 spina bifida, 17 SMA, 13 DMD, 44 other | 285 | Fusion to pelvis at index procedure vs. inclusion of pelvis at subsequent revision | Minimum 2y | Fusion to pelvis at index operation resulted in slightly greater, nonsignificant correction of PO Significantly fewer patients underwent reoperation if treated with fusion to pelvis at index procedure Revision group had significantly higher rates of implant failure |
Preoperative decision making requires balancing the increased rates of reoperation, implant failure, and pseudoarthrosis in revision surgery with the benefits of an unfused L5-S1 junction in those without significant PO |
| Stiel et al16 | 13 CP, 6 DMD, 18 others | 37 | Fusion to lower lumbar (PO < 20 degrees and parallel endplates of L5 and S1) vs. fusion to pelvis (PO > 20 degrees and nonparallel endplates of L5 and S1) | Minimum 2y | Significant correction of major curve angle, PO, and T1 tilt angle No significant loss of correction at 2 y |
Pelvic instrumentation is recommended if PO > 20 degrees and if endplates of L5 and S1 are in nonparallel orientation |
| Tondevold et al17 | 46 CP, 12 central motor involvement, 10 mixed motor involvement, 10 muscular degenerative, 6 peripheral motor involvement, and 7 other | 91 | Fusion to L5 vs. pelvis | Minimum 2y | Fusion to pelvis resulted in significantly greater scoliosis correction No difference in PO correction Loss of PO correction was more frequent in the L5 cohort at 2 y |
Fixation to pelvis indicated in patients with NMS with preoperative coronal and sagittal imbalance |
CP indicates cerebral palsy; DMD, Duchenne muscular dystrophy; NMS, neuromuscular scoliosis; PO, pelvic obliquity; SF-36, 36-Item Short Form Survey; SMA, spinal muscular atrophy.
DISCUSSION
Fusion to the Pelvis
Pros
The balance of the literature demonstrates significantly greater correction of PO in patients where fusion was extended to the pelvis compared with patients where fusion stopped at L5.17,18 In 2 comparative retrospective reviews, Modi et al18 and Akesen15 noted increased PO correction when fusion included the pelvis (Fig. 1). Interestingly, Tondevold et al17 also noted a significant advantage in mean curve correction in patients who were treated with pelvic fixation (57% vs. 79%), a finding that has been corroborated by other authors,4 demonstrating that the benefits of pelvic fixation may extend proximal to the spinopelvic region.
FIGURE 1.
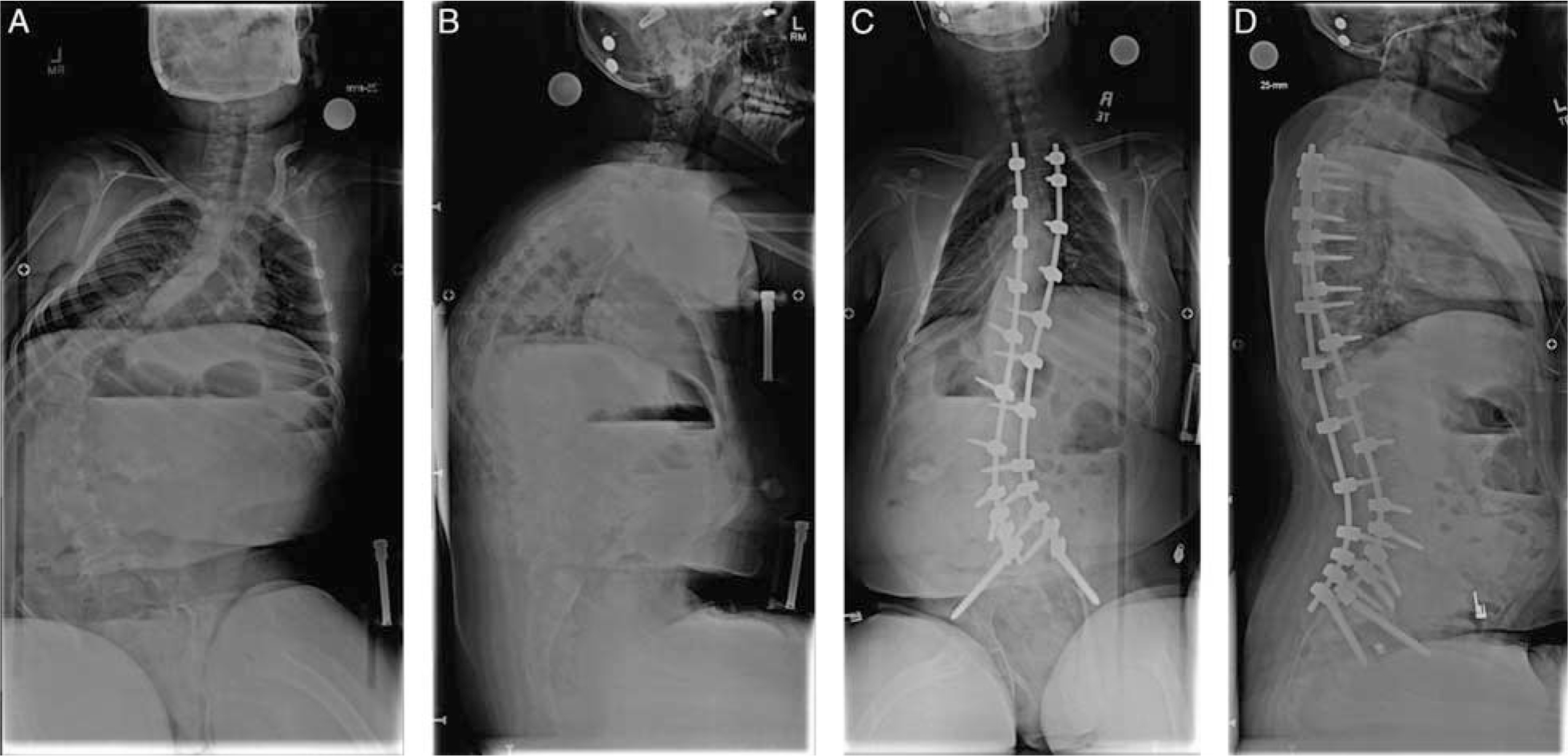
Preoperative upright AP (A) and lateral (B) scoliosis radiographs in a 14-year-old boy with cerebral palsy (GMFCS 4) who is minimally ambulatory (transfers and a few steps with assistance). Preoperative major curve 90 degrees, thoracic kyphosis 75 degrees, lumbar lordosis 40 degrees. Three-year postoperative upright AP (C) and lateral (D) scoliosis radiographs. The patient has maintained baseline ambulatory status. Postoperative major curve 30 degrees, thoracic kyphosis 35 degrees, lumbar lordosis 50 degrees. The patient has maintained baseline ambulatory status. AP indicates anteroposterior.
Not only is the initial correction of PO more effective with fusion to the pelvis,15,17 but this correction is more successfully maintained over time.9,17 Postoperative loss of PO correction has been found in patients with initial preoperative PO exceeding 15 degrees who were not fused to the pelvis9 and in patients with severe preoperative coronal or sagittal imbalance.17 Loss of PO leads to loss of sitting balance over time, which is a key consideration in patients who primarily utilize wheelchairs for mobility.9 As such, pelvic fixation may assist in providing longstanding correction not only in patients with severe PO but also in patients with more severe curves who may benefit from additional stability.
Most importantly, pelvic fixation may lead to additional gains in functional outcomes. Akesen et al15 demonstrated that the use of iliac screws in addition to spinal fusion resulted in a statistically significant improvement in physical 36-Item Short Form Survey scores compared with patients where iliac screws were not used (7.6 vs. 3.6 points; P = 0.0007), without significantly altering infection rate, blood loss, or surgical time. This likely is a result of enhanced PO correction, with subsequent improvement in sitting balance. In minimally ambulatory patients, correction of sitting balance is a major goal of surgery as it has been shown to significantly improve overall health and quality of life.4,19 Further, with regard to function, at a mean of 2.9 years after posterior spinal fusion with pelvic instrumentation in a cohort of minimally moderately ambulatory patients with NMS, Tsirikos et al20 found the maintenance of ambulatory ability in 23 of 24 patients without any objective alterations in gait pattern in 12 patients where these data were available. As such, fusion to the pelvis need not be precluded for fear of causing declines in mobility and independence.
Cons
Pelvic instrumentation requires an extension of the surgical incision and additional dissection, placing the wound in close proximity to the anus, which is especially concerning in a population of patients that is frequently incontinent. Likely, as a result, pelvic fixation has been demonstrated to be an independent risk factor for infection and wound complications.11,12,21 In addition, some authors have shown that pelvic instrumentation is associated with increased estimated blood loss (EBL) and surgical time,13 whereas other researchers have not validated these findings.15,17
In part because of their relatively high profile compared with spinal fixation, patients with pelvic instrumentation are at risk for hardware-associated complications. Without adequate soft tissue coverage, high rates of implant prominence, irritation, and sacral sores have been reported.9,22,23 This problem has been considerably reduced with the development of low-profile sacral-alar-iliac fixation techniques, which have been found to not only reduce implant prominence but also improve PO correction and decrease rates of implant failure.23,24 Beyond prominence, pelvic instrumentation has been associated with high rates of screw breakage, screw loosening, screw pullout, and/or implant disengagement.22,25,26 Rates of iliac screw fixation failure have been described to be as high as 24% to 35%.23,25,27 This risk can be mitigated by utilizing more points of fixation in the lumbosacral spine and pelvis22,27 and by supplementing fixation with the addition of a distal crosslink.25 Myung and colleagues found an early failure rate of 35% when <6 screws combined were placed in L5, S1, and the pelvis. Conversely, there were no early failures in those with ≥6 points of fixation.22
Fusion Sparing the Pelvis
Pros
In comparable patient populations, fusing short of the pelvis in NMS has been consistently associated with low hardware-associated complication rates as compared to fusing to the pelvis. Instrumentation to the lower lumbar spine has the benefit of decreased EBL, operative time, and surgical site infection risks (Fig. 2).11–13,28 For patients presenting with minimal PO (<10 to 15 degrees), numerous authors have reported adequate PO correction without pelvic instrumentation.6,13,14,16,18,29–32 McCall and Hayes6 and Takaso et al14 demonstrated the durability of this correction, demonstrating maintenance of PO correction at long-term follow-up in their respective studies.
FIGURE 2.

Preoperative upright AP (A) and lateral (B) scoliosis radiographs in a 12-year-old girl with Pierre Robin syndrome and unspecified seizure disorder who is a household ambulator with assistance. Preoperative major curve 70 degrees, thoracic kyphosis <10 degrees, and lumbar lordosis 35 degrees. Two-year postoperative upright AP (C) and lateral (D) scoliosis radiographs. Postoperative major curve 30 degrees, thoracic kyphosis 20 degrees, and lumbar lordosis 25 degrees. The patient has maintained baseline ambulatory status. AP indicates anteroposterior.
Although pelvic fixation provides for a more rigid construct, which may confer advantages with regard to long-term sitting balance, a trade-off exists in terms of mobility loss at the L5-S1 joint. Mobility at the L5-S1 joint may confer advantages in performing transfers, weight shifts, and rotational mobility,6 which are key components of wheelchair activities and mobility in minimally ambulatory patients. Preserving motion at this joint, therefore, should be considered in appropriate patients without severe preoperative PO.
Cons
In patients with NMS, avoiding additional trips to the operating room is paramount. These patients are medically complex, at high risk for perioperative complications,33,34 and subject to numerous surgeries throughout their lifetime as a result of their underlying condition, regardless of their spinal status. Some studies suggest that fusion ending shy of the pelvis cannot correct nor maintain severe PO (>15 to 20 degrees)9,13,14,16 and including pelvic instrumentation at index surgery reduces the need for revision surgery for loss of PO correction.15,17
Further, when revising patients fused to L5 initially with extensions to the pelvis, there is a higher overall complication rate, risk of implant failure, pseudarthrosis, and revision surgery compared with patients in whom the pelvis was included in the initial operation.7 In a multi-center retrospective review, Nielsen demonstrated that compared with those with initial pelvic instrumentation, those that were revised to include the pelvis had decreased PO correction (18 vs. 22 degrees).7 Significantly fewer patients underwent reoperation if treated with fusion to the pelvis at the index procedure (23% vs. 50%), and the revision group had significantly higher rates of implant failure (43% vs. 7%). Furthermore, operative times and EBL were comparable between cohorts, subjecting patients to a similar surgical risk profile on a second occasion.
CONCLUSION
For the majority of individuals with progressive NMS, spinal correction typically includes pelvic instrumentation, especially in nonambulatory patients. However, fusion to the lower lumbar spine is a safe and effective alternative in appropriately selected minimally ambulatory patients. Retrospective and prospective studies have demonstrated fusion sparing the lumbosacral junction results in a balanced spine, with adequate, durable correction of PO in appropriately selected patients with minimal pre-existing PO.
Unfortunately, there is little reported evidence describing the results of spinal surgery in NMS into adulthood. Patients who achieve and maintain spinal balance regardless of whether they are fused to the pelvis or not are expected to have the most satisfactory results as adults. Achieving and maintaining balance is more likely with a fusion to the pelvis, at the cost of potentially higher short-term complications as reported by several studies. Whether or not a fusion to the pelvis impacts ambulatory status into adulthood compared with a fusion short of the pelvis is not known.
All decision making should be shared with the family of the affected patient weighing the pros and cons of each approach as described. Given its improved safety profile, we consider fusion to the lower lumbar spine in minimally ambulatory patients with NMS who have adequate head control in the absence of any pre-existing hip subluxation or dislocation when PO <15 degrees (Table 2). Fusion to the pelvis is recommended in patients who do not meet these criteria. Based on the best available evidence, we believe this approach maximizes the quality and safety of spinal deformity correction in patients with NMS.
TABLE 2.
Specific Considerations for Fusion to Lumbar Spine Versus Pelvis in the Patients With Minimally Ambulatory Neuromuscular Scoliosis
| Relative indications for fusion to lumbar level |
| Pelvic obliquity <15 degrees |
| Presence of adequate head control |
| Relative contraindications |
| Pelvic obliquity >15 degrees |
| Hip subluxation or dislocation (or at high risk for hip subluxation, ie, patient with cerebral palsy with high head-shaft angle and elevated Tonnis angle) |
Acknowledgments
All other authors have nothing to disclose. No external funding received for this work.
S.G. reports other from ACI Clinical, other from Medtronic, other from Nuvasive, grants and other from Pediatric Orthopaedic Society of North America, grants and other from Scoliosis Research Society, other from US News and World Report Best Children’s Hospitals Orthopedics Working Group, outside the submitted work. The remaining authors declare no conflicts of interest.
REFERENCES
- 1.Roberts SB, Tsirikos AI. Factors influencing the evaluation and management of neuromuscular scoliosis: a review of the literature. J Back Musculoskelet Rehab. 2016;29:613–623. [DOI] [PubMed] [Google Scholar]
- 2.Vialle R, Thévenin-Lemoine C, Mary P. Neuromuscular scoliosis. Orthop Traumatol Surg Res. 2013;99(suppl 1):S124–S139. [DOI] [PubMed] [Google Scholar]
- 3.Peelle MW, Lenke LG, Bridwell KH, et al. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine (Phila Pa 1976). 2006;31:2392–2398. [DOI] [PubMed] [Google Scholar]
- 4.Mercado E, Alman B, Wright JG. Does spinal fusion influence quality of life in neuromuscular scoliosis? Spine (Phila Pa 1976). 2007;32(suppl 19):S120–S125. [DOI] [PubMed] [Google Scholar]
- 5.Pehrsson K, Larsson S, Oden A, et al. Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine (Phila Pa 1976). 1992;17:1091–1096. [DOI] [PubMed] [Google Scholar]
- 6.McCall RE, Hayes B. Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine (Phila Pa 1976). 2005;30:2056–2060. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen E, Andras LM, Bellaire LL, et al. Don’t you wish you had fused to the pelvis the first time: a comparison of reoperation rate and correction of pelvic obliquity. Spine (Phila Pa 1976). 2019;44:E465–E469. [DOI] [PubMed] [Google Scholar]
- 8.Winter R Classification and Terminology. In: Lonstein JBD, Winter R, Ogilvie J, eds. Moe’s Textbook of Scoliosis and Other Spinal Deformities, 3rd ed. Philadelphia, PA: Saunders; 1994:39–43. [Google Scholar]
- 9.Modi HN, Suh SW, Song HR, et al. Evaluation of pelvic fixation in neuromuscular scoliosis: a retrospective study in 55 patients. Int Orthop. 2010;34:89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minhas SV, Chow I, Feldman DS, et al. A predictive risk index for30-day readmissions following surgical treatment of pediatric scoliosis. J Pediatr Orthop. 2016;36:187–192. [DOI] [PubMed] [Google Scholar]
- 11.Mohamad F, Parent S, Pawelek J, et al. Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop. 2007;27:392–397. [DOI] [PubMed] [Google Scholar]
- 12.Ramo BA, Roberts DW, Tuason D, et al. Surgical site infections after posterior spinal fusion for neuromuscular scoliosis: a thirty-year experience at a single institution. J Bone Joint Surg Am. 2014;96:2038–2048. [DOI] [PubMed] [Google Scholar]
- 13.Sengupta DK, Mehdian SH, McConnell JR, et al. Pelvic or lumbar fixation for the surgical management of scoliosis in Duchenne muscular dystrophy. Spine (Phila Pa 1976). 2002;27:2072–2079. [DOI] [PubMed] [Google Scholar]
- 14.Takaso M, Nakazawa T, Imura T, et al. Can the caudal extent of fusion in the surgical treatment of scoliosis in Duchenne muscular dystrophy be stopped at lumbar 5? Eur Spine J. 2010;19:787–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akesen B, Atici T, Eken G, et al. The comparison of the results after spinal fusion with or without iliac screw insertion in the treatment of neuromuscular scoliosis. Acta Orthop Traumatol Turc. 2018;52:435–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stiel N, Ozden J, Ridderbusch K, et al. Pedicle screw instrumentation with or without pelvic fixation in neuromuscular scoliosis: outcome and complications in a series of 37 patients with a minimum 2-year follow-up. Surgeon. 2020;18:e7–e12. [DOI] [PubMed] [Google Scholar]
- 17.Tondevold N, Lastikka M, Andersen T, et al. Should instrumented spinal fusion in nonambulatory children with neuromuscular scoliosis be extended to L5 or the pelvis? Bone Joint J. 2020;102-b:261–267. [DOI] [PubMed] [Google Scholar]
- 18.Modi HN, Hong JY, Mehta SS, et al. Surgical correction and fusion using posterior-only pedicle screw construct for neuropathic scoliosis in patients with cerebral palsy: a three-year follow-up study. Spine (Phila Pa 1976). 2009;34:1167–1175. [DOI] [PubMed] [Google Scholar]
- 19.Kolman SE, Glanzman AM, Prosser L, et al. Factors that predict overall health and quality of life in non-ambulatory individuals with cerebral palsy. Iowa Orthop J. 2018;38:147–152. [PMC free article] [PubMed] [Google Scholar]
- 20.Tsirikos AI, Chang WN, Shah SA, et al. Preserving ambulatory potential in pediatric patients with cerebral palsy who undergo spinal fusion using unit rod instrumentation. Spine (Phila Pa 1976). 2003; 28:480–483. [DOI] [PubMed] [Google Scholar]
- 21.Gitelman A, Joseph SA Jr, Carrion W, et al. Results and morbidity in a consecutive series of patients undergoing spinal fusion with iliac screws for neuromuscular scoliosis. Orthopedics. 2008;31:1201–1208. [DOI] [PubMed] [Google Scholar]
- 22.Myung KS, Lee C, Skaggs DL. Early pelvic fixation failure in neuromuscular scoliosis. J Pediatr Orthop. 2015;35:258–265. [DOI] [PubMed] [Google Scholar]
- 23.Shabtai L, Andras LM, Portman M, et al. Sacral Alar Iliac (SAI) screws fail 75% less frequently than iliac screws in neuromuscular scoliosis. J Pediatr Orthop. 2017;37:e470–e475. [DOI] [PubMed] [Google Scholar]
- 24.Sponseller PD, Zimmerman RM, Ko PS, et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976). 2010;35:1887–1892. [DOI] [PubMed] [Google Scholar]
- 25.Garg S, Holland C, LaGreca J, et al. Predicting failure of iliac fixation in neuromuscular spine deformity. Spine Deform. 2014;2:214–218. [DOI] [PubMed] [Google Scholar]
- 26.Zahi R, Vialle R, Abelin K, et al. Spinopelvic fixation with iliosacral screws in neuromuscular spinal deformities: results in a prospective cohort of 62 patients. Childs Nerv Syst. 2010;26:81–86. [DOI] [PubMed] [Google Scholar]
- 27.Phillips JH, Gutheil JP, Knapp DR Jr. Iliac screw fixation in neuromuscular scoliosis. Spine (Phila Pa 1976). 2007;32:1566–1570. [DOI] [PubMed] [Google Scholar]
- 28.Anari JB, Spiegel DA, Baldwin KD. Neuromuscular scoliosis and pelvic fixation in 2015: where do we stand? World J Orthop. 2015; 6:564–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takaso M, Nakazawa T, Imura T, et al. Two-year results for scoliosis secondary to Duchenne muscular dystrophy fused to lumbar 5 with segmental pedicle screw instrumentation. J Orthop Sci. 2010; 15:171–177. [DOI] [PubMed] [Google Scholar]
- 30.Takei S, Miyagi M, Saito W, et al. Safety and efficacy of treatment for scolios is secondary to spinal muscular atrophy fused to lumbar 5 level. Spine Surg Relat Res. 2018;2:294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whitaker C, Burton DC, Asher M. Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with lumbar pedicle screw anchorage. Spine (Phila Pa 1976). 2000;25:2312–2318. [DOI] [PubMed] [Google Scholar]
- 32.Wild A, Haak H, Kumar M, et al. Is sacral instrumentation mandatory to address pelvic obliquity in neuromuscular thoracolumbar scoliosis due to myelomeningocele? Spine (Phila Pa 1976). 2001;26:E325–E329. [DOI] [PubMed] [Google Scholar]
- 33.Sharma S, Wu C, Andersen T, et al. Prevalence of complications in neuromuscular scoliosis surgery: a literature meta-analysis from the past 15 years. Eur Spine J. 2013;22:1230–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murphy NA, Firth S, Jorgensen T, et al. Spinal surgery in children with idiopathic and neuromuscular scoliosis. What’s the difference? J Pediatr Orthop. 2006;26:216–220. [DOI] [PubMed] [Google Scholar]


