Abstract
Background
The definition, classification and management of rectus diastasis (RD) are controversial in the literature and a variety of different surgical treatments have been described. This article reports on the European Hernia Society (EHS) Clinical Practice Guideline for RD.
Method
The Guideline group consisted of eight surgeons. The Grading of Recommendation, Assessment, Development and Evaluation (GRADE) approach and the Appraisal of Guidelines for Research and Evaluation (AGREE) instrument were used. A systematic literature search was done in November 2018 and updated in November 2019 and October 2020. Nine Key Questions (KQs) were formulated.
Results
Literature reporting on the definition, classification, symptoms, outcomes and treatments was limited in quality, leading to weak recommendations for the majority of the KQs. The main recommendation is to define RD as a separation between rectus muscles wider than 2 cm. A new classification system is suggested based on the width of muscle separation, postpregnancy status and whether or not there is a concomitant hernia. Impaired body image and core instability appear to be the most relevant symptoms. Physiotherapy may be considered before surgical management. It is suggested to use linea alba plication in patients without concomitant hernia and a mesh-based repair of RD with concomitant midline hernias.
Conclusion
RD should be defined as a separation of rectus muscles wider than 2 cm and a new classification system is suggested.
The European Hernia Society has decided to develop a Clinical Practice Guideline in order to optimize the management of rectus diastasis patients. The Grading of Recommendation, Assessment, Development and Evaluation (GRADE) approach and the Appraisal of Guidelines for Research and Evaluation (AGREE) instrument were used. The main recommendation is to define rectus diastasis as a separation between rectus muscles wider than 2 cm. A new classification system is suggested based on the width of muscle separation, post pregnancy status and whether there is a concomitant hernia or not. Physiotherapy may be considered prior to surgical management. It is suggested to use linea alba plication in patients without concomitant hernia and a mesh-based repair of rectus diastasis with concomitant midline hernias
Introduction
The definition, classification, and management of rectus diastasis (RD) is controversial, with a variety of different surgical treatments described. Consequently, the European Hernia Society (EHS) has developed a Clinical Practice Guideline on the management of RD. The executive summary is presented here, with a full version of the methodology and discussion of the evidence underpinning the guidelines available as Supplementary material.
Methods
The Guideline Group consisted of eight surgeons. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach and the Appraisal of Guidelines for Research and Evaluation (AGREE) instrument were used. A systematic literature search was done in November 2018 and updated in October 2020.
Results
Nine key questions (KQs) were formulated.
KQ1 What is the definition of RD?
Statement: There is limited evidence on an exact definition of RD. RD is an abnormal separation of the two rectus abdominis muscles caused by a thinning and widening of the linea alba. A separation of the rectus muscles of 2 cm or less might be considered physiologically normal.
Recommendation: As a good practice statement, rectus diastasis is defined as a widening of the linea alba exceeding 2 cm.
Quality of evidence: Low
Strength of recommendation: Strong (upgraded)
KQ2 Which modalities are most suitable for diagnosis and assessment of RD?
Statement: Clinical examination and measurement using the ‘finger width’ method appears adequate for diagnosing RD. Measurement of the inter-rectus distance using either ultrasound imaging or calipers is a reliable method. There is limited evidence to support the use of CT.
Recommendation: Clinical examination is suggested for diagnosing RD in most patients. CT may be useful in detecting a concomitant hernia and for surgical planning. For more precise measurement, the use of ultrasound imaging or calipers at 3 cm above the umbilicus is suggested.
Quality of evidence: Low
Strength of recommendation: Weak
KQ3 What are the classification systems for RD?
Statement: None of the existing classification systems seems to be optimal for classifying RD or to serve as a basis for treatment strategy.
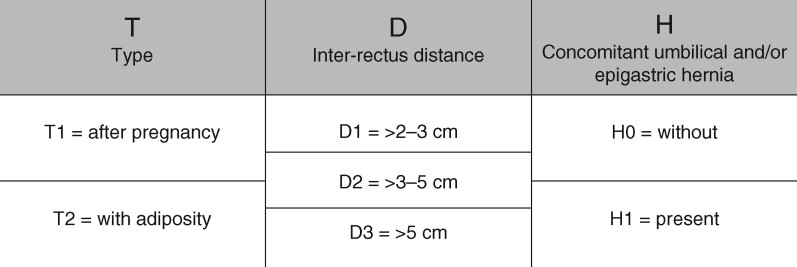
Recommendation: A new classification system for RD is suggested based on the width of muscle separation, postpregnancy status, and whether or not there is a concomitant hernia (Fig. 1).
Quality of evidence: Low
Strength of recommendation: Strong (upgraded)
KQ4 What symptoms are associated with RD?
Statement: A range of symptoms is reported to be associated with RD. It is unknown whether the width of the diastasis is related to the severity of symptoms. Impaired body image and core instability seem to be the most common symptoms.
Recommendation: As a clinical expertise guidance, impaired body image and core instability appear to be the most relevant symptoms to report on and to investigate in future studies.
Quality of evidence: Low
Strength of recommendation: Weak
KQ5 Which outcome measures should be used to evaluate treatment for RD?
Statement: Studies describing outcome measures are very limited. The inter-rectus distance may be an objective measure, although the correlation with clinical presentation is unclear. Patient-reported outcome measures are the best tool to evaluate clinical symptoms, such as body image and core instability. The Short Form 36 and Body Image Questionnaire are helpful.
Recommendation: It is suggested that future studies should focus on core instability and body image.
Quality of evidence: Low
Strength of recommendation: Weak
KQ6 Are there non-operative treatment options for RD?
Statement: There is limited evidence to support a benefit from non-operative treatment. Physiotherapy seems to reduce inter-rectus distance. Several different training programmes have been described, but no specific regimen can be recommended. It is unknown whether symptoms and quality of life can be improved using a specific exercise programme.
Recommendation: No specific non-operative treatment for RD can be recommended. However, physiotherapy may be considered before surgical management of the rectus diastasis.
Quality of evidence: Moderate
Strength of recommendation: Weak
KQ7 What are the surgical treatment options in patients without concomitant hernias?
Statement: RD without concomitant midline hernias can be treated surgically using linea alba plication (suture) with or without mesh augmentation, both via an open or a laparoendoscopic approach. Studies comparing different options are scarce, heterogeneous and of low quality.
Recommendation: If surgery is performed, the technique used should result from a shared decision-making process between the patient and surgeon. As a clinical expertise guidance, linea alaba plication is suggested in patients without concomitant hernia. No recommendation on the type of suture or suturing technique can be made.
Quality of evidence: Low
Strength of recommendation: Weak
KQ8 What is the optimal treatment of rectus diastasis with concomitant umbilical or epigastric hernias?
Statement: Mesh-based repair is recommended according to the European Hernia Society and Americas Hernia Society Guidelines for Treatment of Umbilical and Epigastric Hernias. Plication of the anterior rectus sheath may be sufficient to repair the smallest (less than 1 cm) umbilical or epigastric hernias. Other approaches have been reported. The endoscopic subcutaneous dissection followed by linea alba plication with an onlay mesh was the most reported technique.
Recommendation: A mesh-based repair of RD with concomitant midline hernias is suggested. Plication of the linea alba may be sufficient to repair a diastasis associated with small (less than 1 cm) umbilical/epigastric hernias.
Quality of evidence: Low
Strength of recommendation: Weak
KQ9 Is there a role for specific postoperative management of RD repair?
Statement: Abdominal binders appear to aid mobilization, and reduce postoperative pain and psychological stress. They have no effect on seroma formation or pulmonary function. No specific postoperative rehabilitation programme is used worldwide.
Recommendation: As a clinical expertise guidance, the use of an abdominal binder in the postoperative period can be suggested. The noted advantages of reduced pain, enhanced mobilization, and their perceived psychological support after surgery, make their contribution modest but of value. No specific postoperative rehabilitation programme can be recommended.
Quality of evidence: Very low
Strength of recommendation: Weak
Discussion
The literature reporting on the definition, classification, symptoms, outcomes, and treatments was very limited in quality, leading to weak recommendations for the majority of the KQs. The main recommendation of this guidance is to define RD as a separation between rectus muscles wider than 2 cm. A new classification system is suggested based on the width of muscle separation, postpregnancy status, and whether or not there is a concomitant hernia (Fig. 1). Until new research is available, management and treatment strategy options need to be discussed adequately with patients to assist them in making informed decisions and understanding as much as possible about the procedures they are agreeing to.
Fig. 1.
European Hernia Society RD classification
Supplementary material
Supplementary material is available at BJS online.
Supplementary Material
Contributor Information
P Hernández-Granados, General Surgery Unit, Fundación Alcorcón University Hospital, Rey Juan Carlos University, Alcorcón, Spain.
N A Henriksen, Department of Surgery, Gastro Unit, Herlev Hospital, Zealand University Hospital and University of Copenhagen, Copenhagen, Denmark.
F Berrevoet, General and Hepatopancreatobiliary Surgery and Liver Transplantation, Ghent University Hospital, Ghent, Belgium.
D Cuccurullo, Department of General, Laparoscopic and Robotic Surgery, AORN dei Colli, Monaldi Hospital, Naples, Italy.
M López-Cano, Abdominal Wall Surgery Unit, Val d’Hebrón University Hospital, Universidad Autónoma de Barcelona, Barcelona, Spain.
S Nienhuijs, Surgery, Catharina Hospital, Eindhoven, the Netherlands.
D Ross, Department of Plastic Surgery, The London Clinic and St Thomas' Hospital, London, UK.
A Montgomery, Surgical Department, Skåne University Hospital Malmö, Lund University, Sweden.
Full guidelines to accompany this executive summary are available online.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.