Dear Editor
Benign breast inflammation and infection accounts for 5 per cent of all breast-related hospital admissions1, costing €35842 per admission. Mastitis, defined as inflammation of breast tissue, can be broadly classified as either lactational or non-lactational. Complications, such as severe sepsis resulting in hospital admission and/or the need for surgical incision and drainage, can occur when treatment is delayed, incorrect, or ineffective. Breast abscess, characterized by a localized collection of purulent material within the breast, is a known complication of mastitis and occurs in up to 11 per cent3 of cases. The Mastitis and Mammary Abscess Management Audit (MAMMA) aims to review current practices and improve outcomes in the treatment of mastitis and breast abscesses in the UK and Ireland through national adoption of a best-practice protocol.
The accepted standard management of breast abscesses includes antibiotics and minimally invasive ultrasound-guided needle aspiration on an outpatient basis for patients who are well clinically3,4. Surgical incision and drainage represents an archetypal treatment that should be reserved for selected patients only, because it can lead to cosmetic disfigurement and, in lactational mastitis, involves an unnecessary hospital admission, separating the breastfeeding mother from her baby.
The acute nature of this presentation means that patients are more likely to present to the emergency department and/or general practitioners, and subsequently be managed by non-breast specialist general surgeons. This, alongside lack of a clear treatment protocol, is likely to contribute to wide variation in management4, particularly in areas such as antibiotic prescribing (both class and duration), rates of surgical incision and drainage, and the duration of inpatient treatment. A recent retrospective study4 in a multisite National Health Service Trust concluded that the implementation of a breast abscess pathway improved compliance with preferred antibiotic regimens, and reduced the rate of surgical incision and drainage, as well as hospital admissions. MAMMA aims to demonstrate similar improvements in practice at a national level.
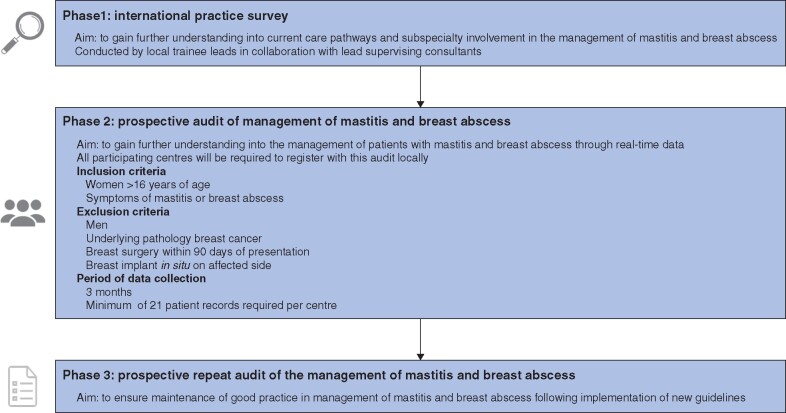
MAMMA is a prospective audit endorsed by the Association of Breast Surgery (ABS) UK, which involves three phases (Fig. 1). Phase 1 consists of a survey of current practice, phase 2 is a prospective audit of consecutive patients presenting with mastitis or breast abscess at participating sites in the UK and Ireland, and phase 3 is a prospective repeat audit, following the results of phase 2. To date, 73 sites in the UK and Ireland have signed up and completed phase 1 of the MAMMA study5. Each UK region has a trainee lead, who is responsible for recruitment of local sites to the study. MAMMA has a target of 100 sites to recruit to phase 1 by June 2021. All institutions involved in the care of patients with mastitis or breast abscess, irrespective of whether or not they have a specialist breast unit, are encouraged to register and contribute data to MAMMA.
Fig. 1.
Phases of the Mastitis and Mammary Abscess Management Audit
At present, the MAMMA collaborative is undertaking a systematic review of published literature on the management of mastitis and breast abscesses to determine international treatment patterns. An interim analysis of phase 1 results will be presented at the next Association of Breast Surgery (ABS) conference in May 2021.
Collaborators
Members of the MAMMA Steering Committee: N. Patani (University College London Hospital, London, UK); S. Potter (Bristol Medical School (Population Health Sciences (PHS)), University of Bristol, Bristol, UK); A. Gandhi (Manchester University NHS Foundation Trust, Manchester, UK); R. Dave (Manchester University NHS Foundation Trust, Nightingale Breast Cancer Centre, Wythenshawe Hospital, Manchester, UK); C. Ives (Royal Devon and Exeter NHS Foundation Trust, Exeter, UK); J. Murray (Forth Valley Royal Hospital, Larbert, UK); M. Dillon (Singleton Hospital, Swansea, UK); H. Mathers (Southern Health and Social Care Trust, Craigavon Area Hospital, Portadown, Craigavon, UK); G. Irwin (Belfast Health and Social Care Trust, Belfast City Hospital, Belfast, UK); R. Prichard (St Vincent’s University Hospital, Dublin, Ireland); P. O’Leary (Bon Secours Hospital, Cork, Ireland); P. Ziprin (Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK); T. G. Teoh (Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK); G. Satta (Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK); M. Gardiner (Kennedy Institute of Rheumatology, University of Oxford, Oxford, UK); R. Brown (Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK); H. Fatayer (Wythenshawe Hospital, Manchester, UK); R. O’Connell (Royal Marsden NHS FoundationTrust and Institute of Cancer Research, London, UK); A. Wilkins (York Teaching Hospitals, York, UK); V. Harmer (Imperial College Healthcare NHS Trust, Charing Cross Hospital, London, UK); R. Gallimore (Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK); L. Hookway (international board-certified lactation consultant); S. Paterson (patient representative).
Funding
The study is funded by a National Institute for Health Research Imperial Biomedical Research Centre Research Consumables Bursary.
Disclosure. The authors declare no conflict of interest.
Members of the MAMMA Steering Committee are co-authors of this study and are listed under the heading Collaborators.
Presented at the Association of Breast Surgery and published in abstract form in the European Journal of Surgical Oncology (https://doi.org/10.1016/j.ejso.2020.03.088 2). Presented at the Surgical Research Society Virtual Meeting, October 2020. Presented at the Fifth Mammary Fold Academic and Research Day, February 2020.
References
- 1.NHS Digital. Hospital Admitted Patient Care Activity 2019. –2020. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2019-20 (accessed 3 March 2021).
- 2.NHS England. 2018/19 National Cost Collection Data. National schedule of NHS Costs. https://www.england.nhs.uk/national-cost-collection/ (accessed 3 March 2021).
- 3.WHO. Mastitis. Causes and Management. https://apps.who.int/iris/bitstream/handle/10665/66230/WHO_FCH_CAH_00.13_eng.pdf?sequence=1 (accessed 3 March 2021).
- 4. Patani N, MacAskill F, Eshelby S, Omar A, Kaura A, Contractor K et al. Best-practice care pathway for improving management of mastitis and breast abscess. Br J Surg 2018;105:1615–1622. [DOI] [PubMed] [Google Scholar]
- 5.MAMMA. Mastitis and Mammary Abscess Management Audit. http://mammastudy.com (accessed 3 March 2021).