Abstract
Background
This was a prospective, multicentre, non-blinded, randomized clinical trial involving two parallel groups of patients.
Methods
Adult patients with symptomatic unilateral primary inguinal hernia were included in this study. Patients were enrolled and treated in five Finnish hospitals. Eligible patients were randomized by use of a computer-based program to receiving either open anterior repair (modified Lichtenstein) with glue mesh fixation or totally extraperitoneal (TEP) repair. The primary aims were to compare 30-day patient-reported pain scores and return to work after surgery between the two groups.
Results
A total of 202 patients were randomized: 98 patients to TEP repair and 104 patients to open repair. All randomized patients received their allocated treatment. A total of 86 patients (88 per cent) in the TEP group and 94 patients (90 per cent) in the Lichtenstein group completed the 30-day follow-up. Patients experienced less early pain (P < 0.001) and used less analgesics after TEP repair, compared to those who had modified Lichtenstein repair. Two patients in the TEP group and five in the Lichtenstein group developed superficial wound infection (P = 0⋅446). Only one reoperation was performed in the Lichtenstein group due to haematoma.
Conclusion
TEP inguinal hernia repair is associated with less early postoperative pain compared to the open glue mesh fixation technique.
Trial registration
In this randomized clinical trial, we compared totally extraperitoneal (TEP) repair of groin hernia to open repair of groin hernia. The main outcome was patient-reported pain scores within the first 30 days after the index operation. Patients experienced less pain after TEP repair, compared to those who had open repair.
Introduction
Background
The lifetime risk of inguinal hernia surgery is estimated at twenty-seven per cent for men and three per cent for women1. Many different types of hernia repair have been described, without a consensus on the optimal surgical procedure2. A Lichtenstein repair3 is the most common open repair technique2. The Lichtenstein technique has evolved, with the modified techniques usually referred to as open anterior repair. Many guidelines consider the Lichtenstein procedure as a standard reference, because it is easy to learn and has short operating times and low costs, and it is possible to be performed under local anaesthesia for high-risk patients2,4,5. In addition to open repair, minimally invasive inguinal hernia repair has also gained popularity2.
The most frequently used laparoscopic techniques are transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP)2. TEP repair does not require intraperitoneal entry, and thus the incidence of intra-abdominal injuries is lower compared to that in TAPP repair2. In Nordic countries, the preferred laparoscopic technique is TEP repair6,7, with previous research reporting a decrease in early postoperative pain, with earlier return to work, when compared to the Lichtenstein method4–7. However, TEP repair is a more technically demanding operation and must be performed under general anaesthesia. Also, direct costs to the hospital are higher in TEP repair due to the need for general anaesthesia and disposable materials used6. Since widespread use of mesh repairs, recurrent hernias are rare2,8. However, chronic, as well as acute, pain remains a challenging problem2. Only very few studies have compared the Lichtenstein method versus TEP repair in terms of early (≤ 30 days) postoperative pain response5. Such data are important in young hernia patients who aim to resume physical activities and work as early as possible after the operation. Some studies have reported lower early and chronic pain when Lichtenstein repair is performed with glue fixation versus traditional suture fixation9. Therefore, this present study compared the patient-reported outcome measure (PROM) of early postoperative pain (≤ 30 days) after TEP repair without fixation and the Lichtenstein method with glue fixation of the mesh. The primary endpoint was early pain and recovery during the first 30 days following surgery. The secondary endpoints were return to work or normal physical activity and analgesic use.
Methods
Trial design
This was a prospective, non-blinded, randomized clinical trial. Patients were randomized in parallel groups, with an allocation ratio of 1 : 1. Two university hospitals and three central hospitals participated in this study.
The study was approved by the University of Eastern Finland Committee of Research Ethics and registered in ClinicalTrials.gov (ClinicalTrials.gov identifier: NCT03566433).
Patients
Men and women aged from 18 to 80 years presenting with symptomatic unilateral primary inguinal hernia were included in this study. Patients with previous lower abdominal surgery (such as Pfannenstiel or lower midline laparotomy incision), high operative risk (ASA grade > III), bilateral hernia, large scrotal hernia, or femoral hernia were excluded. All operations were planned as day case. Participating surgeons recruited eligible patients consecutively from the waiting list, and written informed consent was obtained before randomization.
Operative techniques
Six highly experienced senior hernia surgeons performed both open and TEP procedures. In the TEP technique, three ports were used: a 10-mm view port in the midline under the umbilicus and two 5-mm working ports under the 10-mm port. A balloon dissector was used to create the preperitoneal working space. Dissection was carried medially to the pubic bone, laterally to the anterior superior iliac spine, inferiorly under the spermatic cord, and for a few centimetres below the pubic bone. A polypropylene mesh (Optilene™, B. Braun, Melsungen, Germany) measuring 12 × 15 cm was used to cover the hernia orifice. The mesh was not secured with tackers or glue. In TEP repair, a volume of 4–5 ml of bupivacaine (Marcain® 5 mg/ml, AstraZeneca, Cambridge, UK) was locally injected in the skin wounds to anaesthetize trocar sites.
The open repair was performed as described by Lichtenstein3, with some modifications to the technique10. Tension-free hernioplasty was performed by using a 9 × 13-cm trimmed mesh (Optilene™). The sac of an indirect hernia was either resected or just inverted into the abdomen. If the hernia sac was large and direct, it was inverted with absorbable 2–0 sutures (Vicryl™ polyglactin, Johnson & Johnson Medical N.V., Machelen, Belgium). The mesh was placed between the conjoint tendon, the inguinal ligament, the pubic bone, and the internal oblique aponeurosis. The ilioinguinal, genitofemoral, and iliohypogastric nerves were identified, if possible, and carefully preserved. Mesh was fixed using n-butyl-2-cyanoacrylate tissue glue (Histoacryl®, B. Braun). Open repairs were always performed under local anaesthesia. The anaesthetic used for local infiltration was a 1 : 1 mixture of bupivacaine (Marcain® 5 mg/ml) and lidocain with adrenaline (10 mg/ml + 10 µg/ml, Orion, Kuopio, Finland). A bolus of 0.5–1.0 mg of intravenous alfentanil was administered (Rapifen®, AstraZeneca) if the patient felt pain during the operation.
No prophylactic antibiotics were used for either of the techniques. All patients were advised to return to normal daily activities and work as soon as possible after the operation. After surgery, patients were given 7 days of sick leave and those patients who needed more time were given an extension of their sick leave based on a telephone conversation. Ibuprofen or paracetamol were prescribed for postoperative pain.
Outcomes
Demographic data, predisposing factors and hernia-related pain scores were recorded before the operation. Duration of the operation, the type and size of the hernia defect, length of hospital stay, and perioperative and immediate complications were recorded. PROMs were used to evaluate pain and recovery following surgery. Patients were given a pain diary on their discharge from hospital. Patients reported postoperative pain at rest, during exercise, and on coughing. Pain level was recorded twice a day for 7 days after surgery and then postoperatively at days 14, 21, and 30. A numerical rating scale (NRS) of 0 to 10 was used. Patients reported the day of complete recovery from the operation when they could perform normal physical activities or work without difficulty. Use and doses of all analgesics were recorded. Computerized patient records in each hospital for every patient were screened 1 month after surgery for further hospital visits, complications, and reoperations.
Sample size
Power calculation showed that 80 subjects per treatment group were needed for the study to achieve a statistical power of 0.90, with a P-value of 0⋅05 (two-tailed). Calculations were made for postoperative pain at 7 days after surgery, assuming a pain difference of twenty per cent between treatment groups. Allowing a dropout rate of twenty per cent during 30-day follow-up, the study was set up to include randomization of > 200 patients.
Randomization
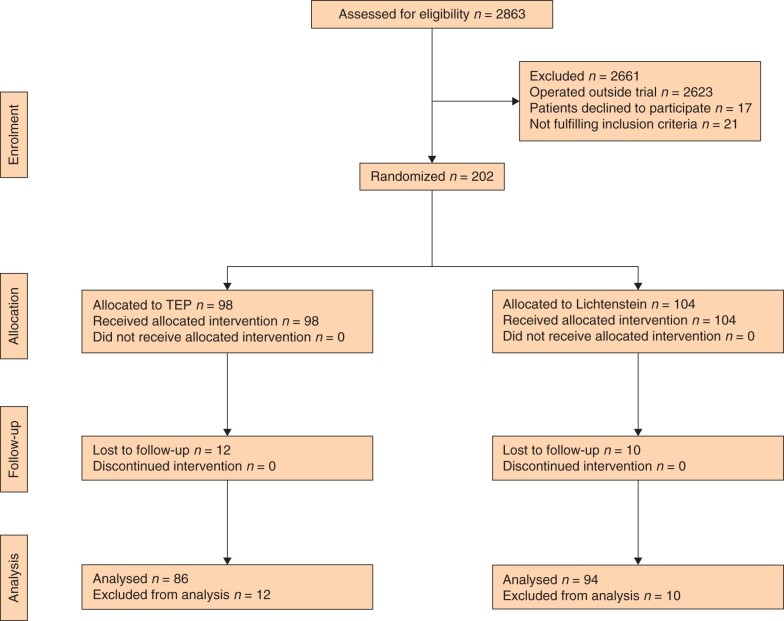
Immediately after giving informed consent, patients were randomized by participating surgeons at each centre to having either Lichtenstein or TEP surgery (Fig. 1). Block randomization in blocks of 40 patients in each centre was performed using a web-based HUSeCRF (University of Helsinki, electronic case report form) program.
Fig. 1.
Study flow chart
Statistical analysis
Data analysis was carried out with SPSS for Windows, Release 27.0 (IBM SPSS, Chicago, Illinois, USA). Continuous data were presented as means, and analysed with Student’s t test (two-tailed) for parametric data and with Mann–Whitney U test for non-parametric data. Categorical variables were analysed using Pearson’s chi-squared test and Fisher’s exact test. A mixed model analysis was used to analyse pain scores. P < 0⋅05 was considered as significant for all tests.
Results
A total of 202 patients who underwent inguinal hernia surgery between June 2017 and October 2020 consented to participate in the study. Baseline patient data are provided in Table 1. Ninety-eight patients were randomly allocated to the TEP group and 104 to the Lichtenstein group (Fig. 1). A total of 86 patients (eighty-eight per cent) in the TEP group and 94 patients (ninety per cent) in the Lichtenstein group completed follow-up by completing and returning their pain diaries.
Table 1.
Patient and operation characteristics
| Lichtenstein (n = 104) | TEP (n = 98) | P-value | |
|---|---|---|---|
| Age (years) * | 56 (22–77) | 53 (18–79) | 0.17 |
| Sex ratio (M : F) | 95:05:00 | 96:05:00 | 0.803 |
| BMI (kg/m2) * | 25 | 25 | 0.967 |
| Smoker | 18 | 14 | 0.827 |
| Duration of symptoms (months) * | 3 | 3 | 0.876 |
| Combined hernia | 2 | 4 | |
| Preoperative pain * † | 3 | 3 | 0.19 |
| Preoperative need of analgesics for hernia pain | 0.68 | ||
| Not needed | 74 | 76 | |
| 1–4 times per month | 17 | 19 | |
| 1–6 times per week | 7 | 3 | |
| Daily | 2 | 2 | |
| Absence from work due to hernia | 11 | 7 | 0.424 |
| Outpatient surgery | 99 | 96 | 0.209 |
| Operating time (min)* | 37 | 36 | 0.322 |
| Hernia orifice size (cm)* | 2 | 2 | 0.223 |
| Type of hernia | 0.578 | ||
| Lateral hernia | 70 | 65 | |
| Medial hernia | 28 | 31 |
Values in parentheses are percentages unless indicated otherwise.
*Values are median (i.q.r.).
†Number rating Scale (0–10).
Operations
Every patient received their allocated treatment. Mean operating times were similar: TEP 36 minutes (range 17–80) versus Lichtenstein 37 minutes (range 20–85) (P = 0⋅318). No intraoperative complications or conversions from laparoscopic to open surgery were observed. One patient in the Lichtenstein group (monitoring due to sleep apnoea) and four patients in the TEP group (two patients due to urinary retention and two for social reasons) needed overnight hospital admission. Few, and mostly minor, postoperative complications were reported. One patient in the Lichtenstein group needed reoperation due to haematoma, whereas no reoperations were performed in the TEP group. Five patients in the Lichtenstein group versus two patients in the TEP group needed antibiotics for minor surgical site infection (P = 0⋅446). No recurrent hernias were observed during the 1-month follow-up.
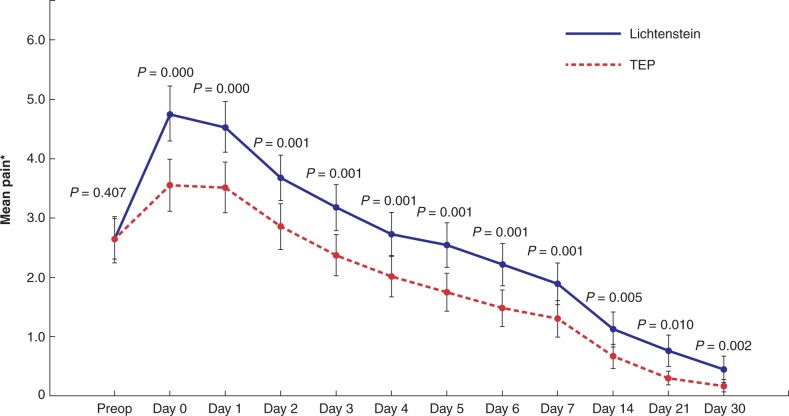
Primary and secondary outcome
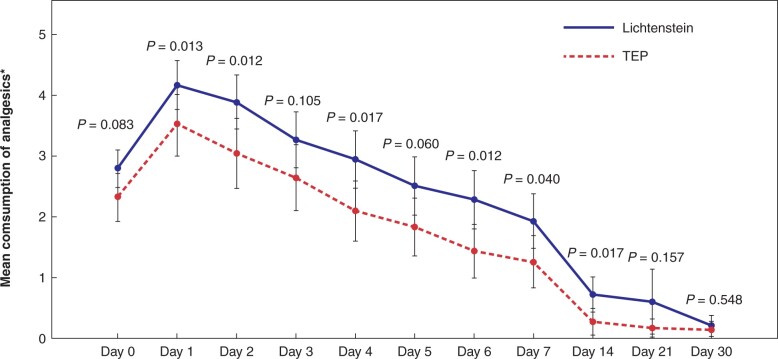
Postoperative pain scores were lower after TEP repair, compared to Lichtenstein repair (P < 0⋅001), at all postoperative measurement points (Fig. 2). Patients in the TEP group returned to work or normal physical activities slightly earlier than those in the Lichtenstein group: 14 days (range 1–31) versus 17 days (range 1–84), respectively (P = 0⋅048). However, on exclusion from analysis of one patient from the Lichtenstein group who had an exceptionally long recovery time (84 days), then there was no statistical difference in recovery times between the two groups. Use of analgesics was more frequent in the Lichtenstein group, although this difference levelled off towards the end of the 30-day follow-up, with significant differences only observed at days 1, 2, 4, 6, 7, and 14 (Fig. 3).
Fig. 2.
Postoperative pain scores
*Numerical rating scale. Error bars: 95 per cent confidence interval. P-values analysed with independent samples t test.
Fig. 3.
Consumption of analgesics. *One unit is equivalent to 1 gram of paracetamol or 600 mg of ibuprofen per orally
*One unit is equivalent to 1 g oral paracetamol or 600 mg oral ibuprofen. Error bars: 95 per cent confidence interval. P-values analysed with independent samples t test.
Discussion
As inguinal hernia repair is one of the commonest surgeries performed worldwide, it is important to find the optimal treatment2. As open Lichtenstein repair is less expensive and easier to teach and learn, it is still commonly used in many patients who could potentially benefit from minimally invasive surgery. However, the current trend is to offer patients tailored hernia surgery. Especially in young patients who may appreciate a rapid return to their usual activities, it is important to know whether endoscopic repair has advantages over the open technique. In the present study, TEP repair resulted in less painful recovery, compared to the open Lichtenstein method. The clinical significance of this finding was emphasized by the observation that TEP patients required less analgesics than patients who received Lichtenstein repair.
The absolute difference in NRS values between the two groups was not large. However, we consider the difference to be clinically significant, as in the TEP group, the mean NRS value decreased to the mild pain level within 2 days, whereas in the Lichtenstein group, the corresponding pain level was reached at day 4.
In all previously published studies, the open surgical technique included mesh fixation with a penetrating method. We aimed to minimize surgical bias by using non-penetrating fixation in the open group and the same mesh in both groups. Performing TEP repair without fixation or open repair with glue fixation has been previously evaluated to be safe and possibly less painful, compared to penetrating fixation9,11–13. Our present study findings are in keeping with these studies comparing recovery after TEP repair versus after Lichtenstein repair with penetrating mesh fixation4,6,7,14. In a well planned study, Eklund and co-workers7 compared the TEP versus the Lichtenstein method by carefully evaluating postoperative pain once per day for the first week and then once per week up to 6 weeks. Their results are in agreement with our findings, demonstrating faster and less painful recovery after TEP repair. The present study also showed that even with use of non-penetrating fixation in open Lichtenstein repair, TEP repair was superior in terms of early recovery.
In many previous studies, the operating time for TEP repair was shown to be significantly longer5. In the present study, the operating time in both groups was short, with no difference between the two groups which may reflect the experience in, and skill for, both techniques by the operating surgeons participating in this study. This highlights the fact that the operating time itself is not a relevant factor when choosing the preferred operating technique.
The obvious limitation in our study is the short follow-up period, with few patients still reporting pain 4 weeks after surgery – even early recurrences are usually diagnosed later than 30 days after surgery. Also, there was no clinical or monitoring, possibly resulting in some surgical complications or early recurrent hernias being undetected. The strength of our study was its carefully planned, multicentre design, with robust randomization, standardized surgical techniques with few complications, and successful completion and return of patient pain diaries to minimize potential biases. Also highly experienced senior surgeons performed all operations, which helped to minimize technical bias in terms of causing excess pain. When interpreting our results in the context of clinical practice, it is important to consider that due to the longer learning curve, many studies have demonstrated inferior results when TEP repair is not performed by experienced surgeons15.
Funding
No funding was received.
Disclosure. The authors declare no conflict of interest.
Supplementary Material
References
- 1. Primatesta P, Goldacre MJ.. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 1996;25:835–839. [DOI] [PubMed] [Google Scholar]
- 2. HerniaSurge Group. International guidelines for groin hernia management. Hernia 2018;22:1–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lichtenstein IL, Shulman AG, Amid PK, Montllor MM.. The tension-free hernioplasty. Am J Surg 1989;157:188–193. [DOI] [PubMed] [Google Scholar]
- 4. Dahlstrand U, Sandblom G, Ljungdahl M, Wollert S, Gunnarsson U.. TEP under general anesthesia is superior to Lichtenstein under local anesthesia in terms of pain 6 weeks after surgery: results from a randomized clinical trial. Surg Endosc 2013;27:3632–3638. [DOI] [PubMed] [Google Scholar]
- 5. Gavriilidis P, Davies RJ, Wheeler J, de'Angelis N, Di Saverio S.. Total extraperitoneal endoscopic hernioplasty (TEP) versus Lichtenstein hernioplasty: a systematic review by updated traditional and cumulative meta-analysis of randomised-controlled trials. Hernia 2019;23:1093–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Langeveld HR, van’t Riet M, Weidema WF, Stassen LP, Steyerberg EW, Lange J. et al. Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 2010;251:819–824. [DOI] [PubMed] [Google Scholar]
- 7. Eklund A, Rudberg C, Smedberg S, Enander LK, Leijonmarck CE, Österberg J. et al. Short‐term results of a randomized clinical trial comparing Lichtenstein open repair with totally extraperitoneal laparoscopic inguinal hernia repair. Br J Surg 2006;93:1060–1068. [DOI] [PubMed] [Google Scholar]
- 8. Matikainen M, Kössi J, Kössi J, Silvasti S, Silvasti S.. Randomized clinical trial comparing cyanoacrylate glue versus suture fixation in Lichtenstein hernia repair: 7-year outcome analysis. World J Surg 2017;41:108–113. [DOI] [PubMed] [Google Scholar]
- 9. Campanelli G, Hidalgo Pascual M, Hoeferlin A, Rosenberg J, Champault G, Kingsnorth A. et al. Randomized, controlled, blinded trial of tisseel/tissucol for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: results of the TIMELI Trial. Ann Surg 2012;255:650–657. [DOI] [PubMed] [Google Scholar]
- 10. Rönkä K, Vironen J, Kössi J, Hulmi T, Silvasti S, Hakala T. et al. Randomized multicenter trial comparing glue fixation, self-gripping mesh, and suture fixation of mesh in Lichtenstein hernia repair (FinnMesh Study). Ann Surg 2015;262:714–720. [DOI] [PubMed] [Google Scholar]
- 11. Golani S, Middleton P, Middleton P.. Long-term follow-up of laparoscopic total extraperitoneal (TEP) repair in inguinal hernia without mesh fixation. Hernia 2017;21:37–43. [DOI] [PubMed] [Google Scholar]
- 12. Sun P, Cheng X, Deng S, Hu Q, Sun Y, Zheng Q.. Mesh fixation with glue versus suture for chronic pain and recurrence in Lichtenstein inguinal hernioplasty. Cochrane Database Syst Rev 2017;2:CD010814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bracale U, Rovani M, Picardo A, Merola G, Pignata G, Sodo M. et al. Beneficial effects of fibrin glue (Quixil) versus Lichtenstein conventional technique in inguinal hernia repair: a randomized clinical trial. Hernia 2014;18:185–192. [DOI] [PubMed] [Google Scholar]
- 14. Sevinç B, Damburacı N, Güner M, Karahan Ö.. Comparison of early and long-term outcomes of open Lichtenstein repair and totally extraperitoneal herniorrhaphy for primary inguinal hernias. Turk J Med Sci 2019;49:38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chen L-S, Chen W-C, Kang Y-N, Wu C-C, Tsai L-W, Liu M-Z. et al. Effects of transabdominal preperitoneal and totally extraperitoneal inguinal hernia repair: an update systematic review and meta-analysis of randomized controlled trials. Surg Endosc 2019;33:418–428. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.