Abstract
Background
The potential benefit of eHealth interventions in patients with abdominal aortic aneurysm (AAA) is uncertain. The primary aim of this study was to investigate the effect of an eHealth intervention on anxiety in patients with AAA undergoing surgery.
Methods
A single-centre randomized clinical trial of patients with AAA scheduled for surgical repair was undertaken. The intervention group received an eHealth tool and psychosocial support besides standard care. The control group received standard care. The analysis of treatment effects was performed as intention-to-treat and per protocol analysis. The primary outcome measure was anxiety mean score (Hospital Anxiety and Depression Scale Anxiety (HADS)-A). Secondary outcomes measures were HADS Depression and short-form 12-item health survey mean scores.
Results
Some 120 participants were randomized. No effect on anxiety mean scores was found in the intention-to-treat analysis (−1.21 versus −0.54, P = 0.330). Among those randomized to the intervention, only 30 of 60 participants used the eHealth tool (application (app) users). The app users were younger and had a higher educational level. A decrease in anxiety mean scores was noted in those who used the app in the per protocol analysis (−2.00 versus −0.54, P = 0.028). The intervention group stated a lower physical-component health-related quality of life (HRQoL) (−4.32 versus −1.16, P = 0.042) but mental-component HRQoL and depressive symptoms were unchanged.
Conclusions
Delivery of an eHealth intervention in this RCT did not result in an improvement in anxiety scores in patients awaiting AAA surgery. Uptake of the eHealth tool was low, although it resulted in lower anxiety scores in those participants who actually used it.
Clinical Trial Registration number
This systematic review of RCTs shows that continuous subcuticular open appendicectomy wound closure is not associated with an increased risk of developing postoperative wound infection. This method of wound closure is associated with a reduced risk of wound dehiscence and better cosmetic outcomes .
Introduction
The choice of treatment for abdominal aortic aneurysm (AAA) (none, open repair (OR) or endovascular aortic repair (EVAR)) is based on age, co-morbidity, aneurysm diameter and morphology1. While patients should participate in the surgical decision-making process, they are reported to be insufficiently informed and engaged to enable shareddecision making2.
AAAs have an impact on physical and mental wellbeing, including anxiety and impact on health-related quality of life (HRQoL)3,4. Preoperative anxiety is a common condition in patients planned for major surgery5, and has been linked to increased mortality and major morbidity in patients undergoing cardiac surgery6. It is estimated that 29 per cent of patients planned for surgical repair of AAA suffer from borderline or clinical anxiety7. A previous study highlighted the importance of balanced information from a trusted healthcare professional to minimize the anxiety that information may impose on patients and next of kin8. The learning needs of AAA patients were found to be insufficiently met by healthcare staff, and improved information and support were required8.
The rapid development in digital health technology entails new challenges to provide patients with adequate information. The available online patient education materials regarding AAA have been shown to be difficult to comprehend9,10. Furthermore, familiarity with digital health technology is limited among the elderly11. Concerns about the negative effects of implementing inadequately validated eHealth solutions have been raised and further scientific evaluations are warranted12.
The primary aim of this study was to investigate the effect of an eHealth intervention compared with standard care on anxiety mean scores in patients undergoing surgical treatment of AAA. The secondary aim was to investigate the effect of the intervention on depression mean scores and HRQoL.
Methods
CONSORT guidelines were followed for a single-centre, parallel group, superiority randomized controlled trial evaluating the effect of an eHealth intervention on anxiety in patients undergoing AAA surgery. The study represents the third paper in a mixed methodology project using participatory design methodology to develop patient-education material that aligns with the learning needs of patients with AAA. The first step was to explore the learning needs of patients regarding their AAA and the care trajectory8. The second step entailed the development and validation of the eHealth tool in collaboration with patients and healthcare staff, aiming to enhance the usability and relevance of the tool13. The present study presents the final step of development, where the eHealth tool was tested and implemented in a real-life setting with patients planned for surgical treatment of AAA. The study was conducted in a vascular surgery department of a university hospital and was registered in the Clinical Trials database (registration number: NCT03157973, http://www.clinicaltrials.gov).
The project complied with the Declaration of Helsinki and was approved by the regional
Human Research Ethics Committee (Dnr 2016/1253–31/4), Stockholm, Sweden. Written informed consent was obtained from all participants prior to inclusion in the study.
Recruitment
All patients scheduled for AAA repair were considered for inclusion. Potential study participants were identified from the surgical waiting list and were considered eligible if they were 50 years or older and were scheduled for elective surgical treatment of an infrarenal AAA. Exclusion criteria were patients diagnosed cognitive dysfunction, severe hearing or visual impairment, inability to speak or understand Swedish, suprarenal or thoracoabdominal aneurysms, or any severe co-morbidity that may hinder the patient from completing the study. Once scheduled for AAA repair, eligible patients were sent a patient-information leaflet. All patients attended a visit for clinical examination and information regarding the perioperative routine 1 week prior to scheduled surgery. Informed consent was obtained at this visit. Randomization was done by the first author in a 1 : 1 ratio by use of permuted block technique with a block size of 10 to minimize spill-over between the control group and intervention group. Due to the study design, blinding was not possible after randomization.
Procedures and interventions
At inclusion in the study, 1 week prior to treatment, all participants completed questionnaires, and baseline characteristics including sociodemographic characteristics, medical history and medication were collected. Since the vascular department also gives service to patients outside the region, some patients could not participate at a baseline visit 1 week prior to treatment. These patients filled out the questionnaires the day before treatment (TableS1).
The control group obtained information and follow-up according to standard clinical routine, consisting of verbal preoperative information from a vascular surgeon, anaesthesiologist and registered nurse and a leaflet containing information about the surgical procedure and general recovery advice. The intervention group received the same standard care, augmented with an intervention programme comprising two parts: an eHealth tool and a psychosocial support programme initiated by a registered nurse at baseline, with a scheduled follow-up prior to discharge. The intervention programme aimed to prepare participants for surgery and to support them through the peri- and postoperative period. The psychosocial support programme started with an orientating session provided by a contact nurse trained in person-centred care and motivational interviewing. The participants were encouraged to reach out to their contact nurse if questions or concerns arose after discharge. Both groups were scheduled for a standard follow-up appointment within 4–6 weeks after surgery. At this appointment, questionnaire data were collected.
The eHealth tool could be accessed via the application (app) My aorta (version 1) on a smartphone or a tablet. The patients were offered a tablet free-of-charge during the whole study period. The content of My aorta (version 1) was also made available as a print-out for those who preferred paper format instead of using the app. The eHealth tool aimed to provide structured and balanced information and consisted of six chapters regarding the condition, self-care and surgical treatment13. It was designed to enable self-directed navigation and did not include time triggers or forced entries. The eHealth tool has been described and validated prior to this study (Fig.S1). Participants in the intervention group were offered free access to the eHealth tool and those who accepted were assigned unique login credentials through a web-based user management system. The content of the tool was adjusted to the planned surgical treatment (EVAR or OR). The app can be downloaded to iOS or android devices and is password protected.
Instruments and definitions
The intervention was evaluated using validated instruments, the Hospital Anxiety and Depression Scale (HADS) and short-form 12-item health survey (SF-12). HADS aims to measure self-reported symptoms of anxiety and depression in individuals in somatic care14. HADS consists of two subscales: HADS Anxiety (HADS-A) and HADS Depression (HADS-D), with seven claims for each subscale, and evaluates feelings during the last 7 days. A cut-off score of 8 or above gives a specificity of 0.78 and a sensitivity of 0.9 for clinical anxiety (HADS-A) and a specificity of 0.79 and a sensitivity of 0.83 for clinical depression (HADS-D)14. A HADS score greater than or equal to 8 was registered as anxiety or depression in this study. The minimal clinically important difference (MCID) is a measure to convert the significance of interventions to clinical situations, defined as the smallest change in a treatment outcome that is of clinical significance. The MCID of HADS-A has been reported to be 1.29–1.67 depending on comparisons between patients or within a group15.
The SF-12 assesses physical and mental health components of wellbeing and is a reliable and well validated instrument16. The survey comprises 12 questions regarding the respondents’ feelings relating to their social and everyday activities due to physical or mental limitations in the last week. The SF-12 measures eight dimensions of HRQoL: general health, physical functioning, role limitations (due to physical health), bodily pain, vitality, social functioning, mental health and role limitations (due to emotional health). It produces two components of HRQoL: the physical component summary (PCS) and the mental component summary (MCS). The values obtained for the two component summaries follow a standard T distribution where the population presents a mean of 50 and a standard deviation of 10. Higher PCS or MCS scores indicate a better state of health.
Sociodemographic characteristics, co-morbidity and pharmaceutical use were obtained from hospital charts at baseline. All clinical demographics were registered at baseline, or at a prior visit to the vascular outpatient clinic within 3 months. Hypertension was registered if the patients had ongoing medication. Current daily smokers and sporadic smokers were considered current smokers whereas those with more than 4 weeks’ abstinence were considered as previous smokers. Coronary heart disease was defined as a composite of previous ischaemic event, diagnosed pectoral angina or diagnosed congestive heart failure. Use of the eHealth tool was defined as using the app ‘My aorta’ on one occasion or more. The subset of participants in the intervention group who utilized the eHealth tool are referred to as app users.
Outcomes
The primary outcome measure was anxiety mean scores in the study cohort measured by HADS-A and in a complementary per protocol analysis of app users in the intervention group versus controls. The secondary outcome measures were depression mean scores and HRQoL measured by HADS-D and SF-12, also presented in an intention-to-treat and per protocol analysis.
Statistical analysis
According to the sample size calculation, 45 participants were needed in each treatment arm to detect a 50 per cent difference in the anxiety scores measured by HADS-A between the treatment groups from baseline to follow-up (with 80 per cent power, 5 per cent significance level). These estimations were based on two randomized controlled trials of education interventions to reduce perioperative anxiety17,18. Drop-out estimation motivated inclusion of 60 patients in each treatment arm.
All study data were continuously recorded in a local registry and anonymized prior to analysis. χ2 test and Fischer’s exact test were used to compare categorical variables and independent t test to compare continuous data. For comparisons of independent groups, Student’s t test was used for normally distributed data, and Mann–Whitney was used for non-parametric data. Continuous variables are presented as mean(s.d.), categorical variables are presented as counts and proportions as appropriate. Primary analysis was performed per intention-to-treat for control group versus intervention groups. Secondary, exploratory subgroup analyses were performed per protocol for control group versus app users, and the participants in the intervention group who used the app (app users) versus non-users respectively.
SF-12 scores were calculated using the Quality Metric Health OutcomesTM PRO CoRE Scoring Software (Optum®; QualityMetric, Lincoln, Rhode Island, USA). All statistical analyses were performed in IBM SPSS Statistics for Macintosh, version 26 (IBM Corp., Armonk, N.Y., USA) , and in Stata (Version IC.16.1 Stata Corp, College Station, Texas, USA) in collaboration with the statistician (M. Kotopouli, Institute of Environmental Medicine (IMM), Karolinska Institutet (KI)).
Results
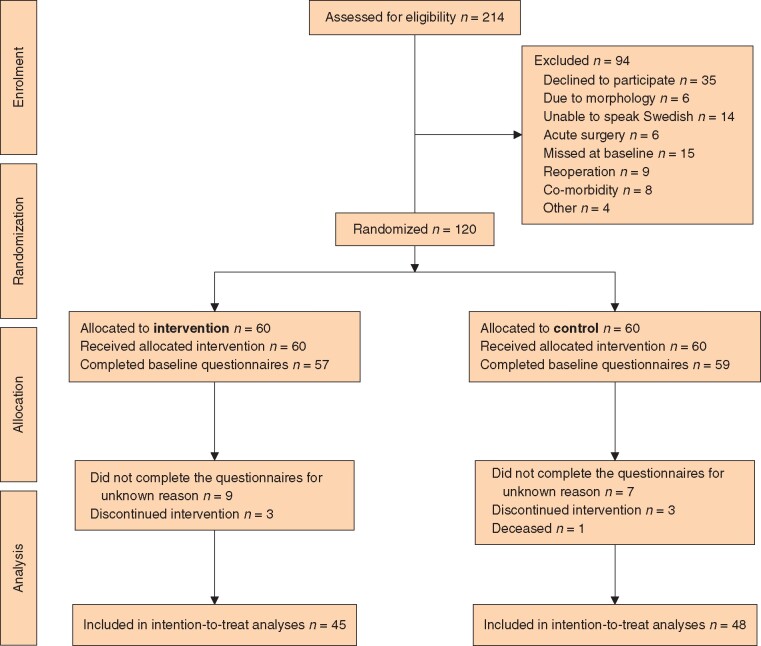
Some 120 patients were randomized between November 2016 and February 2020 (60 participants in each treatment arm) (Fig. 1). A total of 214 patients were screened for the study and among the 94 patients who were eligible but not included, 82 (87 per cent) were male and the mean age was 75 years (Fig. 1). Among the 35 persons who declined to participate, the most common reasons were hesitancy in using modern technology, lack of time or interest, and emotional strain. There were no significant differences in demographic characteristics, such as age or education, between the intervention and control group at baseline (Table 1).
Fig. 1.
CONSORT diagram
Flow diagram describing the design of the study: enrolment, intervention, follow-up and data analysis.
Table 1.
Clinical characteristics and surgical outcomes of patients in the control group and intervention group
| Control (n = 60) |
Intervention (n = 60) |
P ‡ | |
|---|---|---|---|
| Demographics | |||
| Age (years)* | 73.3(5.79) | 72.6(7.20) | 0.227 |
| Male | 55 (92) | 49 (82) | 0.110 |
| Never smoker | 4 (7) | 7 (12) | 0.420 |
|
Educational level Junior compulsory Senior high school Postgraduate/university |
13 (22) 28 (47) 18 (30) |
15 (25) 23 (38) 21 (35) |
0.830§ |
| Co-morbidity | |||
| Diabetes mellitus (any) | 15 (25) | 10 (17) | 0.370 |
| Hypertension | 44 (73) | 48 (80) | 0.520 |
| Coronary artery disease | 18 (30) | 8 (13) | 0.030 |
| Cerebrovascular disease | 6 (10) | 10 (17) | 0.420 |
| Peripheral arterial disease | 8 (13) | 6 (10) | 0.780 |
| Chronic obstructive pulmonary disease | 20 (33) | 21 (35) | 1.000 |
| Depression | 8 (13) | 6 (10) | 0.110 |
| Physiological characteristics | |||
| Systolic blood pressure (mm Hg)† | 142 (17.6) | 139 (16.8) | 0.420 |
| Ankle brachial pressure index† | 0.85 (0.49) | 0.94 (0.46) | 0.330 |
| AAA diameter (mm)† | 57.83 (7.83) | 58.3 (5.36) | 0.250 |
| Surgical data | |||
| EVAR | 35 (58) | 28 (47) | 0.200 |
| Length of hospital stay (days)† | 5.07 (3.44) | 8.07 (8.56) | 0.004 |
| Days in ICU† | 0.67 (1.08) | 1.49 (2.85) | 0.130 |
| Deceased within 30 days | 1 | 0 | n/a |
| HADS-A at inclusion | |||
| HADS-A† | 3.83 (3.87) | 4.68 (3.80) | 0.161 |
| HADS-A ≥8 | 10 (17) | 13 (23) | 0.289 |
| eHealth tool | |||
| Participants who utilized the tool | n/a | 30 (50) | n/a |
Values in parentheses are percentages unless indicated otherwise;
values are median(s.d.),
values are mean(s.d.). AAA, abdominal aortic aneurysm; EVAR, endovascular aortic repair; ICU, intensive care unit; HADS-A, Hospital Anxiety and Depression Scale Anxiety.
Tested for differences in proportions by χ2-test, except
ANOVA. Significance level set at P ≤ 0.005.
Most patients were male (104 patients, 87 per cent) and the mean age was 73 years. The control group had a higher proportion of patients with a history of coronary heart disease, but all other co-morbidities were similar. Most patients reported a smoking history, only 9 per cent were never smokers. Women and men did not differ regarding age and aneurysm diameter. Average hospital stay was longer in women than in men (10 versus 6 days, P = 0.010). Women were, to a larger extent, treated with OR (69 per cent versus 44 per cent in men, P = 0.059). There was no difference in anxiety mean(s.d.) scores between women and men at baseline (5.53(4.85) versus 4.06(3.66), P = 0.167). The mean AAA diameter was 58 mm and more patients were treated with EVAR than OR. Hospital stay and ICU stay were prolonged in patients treated with OR compared with EVAR patients (10.5 versus 3.01 days, P < 0.001) (Table S2).
In the intervention group, 45 participants (75 per cent) completed the questionnaires at both timepoints, compared with 48 (80 per cent) in the control group. The eHealth tool was utilized by 30 out of 60 patients in the intervention group (Table 1). Users of the eHealth tool were younger (70 versus 76 years, P = 0.010) and were more well educated than non-users (43 per cent university level among app users versus 27 per cent in non-users, P = 0.030) (Table S3).
Anxiety
At baseline, a similar proportion of patients had anxiety symptoms by the definition of HADS-A of 8 points or above (17 versus 23 per cent, P = 0.289) (Table 1). In the primary, intention-to-treat analysis of the entire intervention and control groups, no significant differences in HADS-A mean scores could be detected between the groups, neither in the crude analysis nor in a separate analysis by the threshold of 8 points or above (Table S4). Changes in HADS-A scores from baseline to follow-up are presented in Table 3. The hypothesized reduction in HADS-A mean scores of 50 per cent in the intervention group compared with the control group would entail a minimal difference of −0.813 from the baseline values. The observed difference in the intervention group was −1.21, exceeding the hypothesized effect. In subgroup analyses of surgical treatment type and sex, no significant effect on anxiety mean scores was noted (Table 2).
Table 3.
Intention-to-treat and per protocol analyses of the secondary outcomes measures
| Mean change |
Mean difference between groups | P* | ||
|---|---|---|---|---|
| Control | Intervention | |||
| HADS-D | −0.833 | −0.233 | 0.149 (−1.03, 1.33) | 0.410 |
| SF-12 | ||||
| PCS | −1.16 | −2.820 | 1.660 (−0.62, 3.94) | 0.209 |
| MCS | 0.141 | −0.352 | 0.493 (−2.70, 3.69) | 0.966 |
| Control | App users | |||
| HADS-D | −0.833 | −0.6667 | 0.583 (−0.62, 1.78) | 0.335 |
| SF-12 | ||||
| PCS | −1.160 | −4.322 | 3.163 (0.52, 5.80) | 0.042 |
| MCS | 0.141 | 1.364 | −1.223 (−4.93, 2.48) | 0.476 |
Subgroup analysis on participants in the intervention group by use of the eHealth tool. Values in parentheses are 95% confidence intervals. HADS-D, Hospital Anxiety and Depression Scale Depression; SF-12, short-form 12-item health survey; PCS, physical component summary; MCS, mental component summary.
*Mann–Whitney test.
Table 2.
Intention-to-treat analyses of changes between baseline and postoperative Hospital Anxiety and Depression Scale Anxiety mean scores
| Participants and subgroups |
Mean change in HADS-A
Baseline to after operation |
Mean difference between groups | P* | |
|---|---|---|---|---|
| Control (n = 48) | Intervention (n = 45) | |||
| All | −0.542 | −1.209 | 0.668 (−0.70, 2.03) | 0.334 |
| Age (years) | ||||
| ≤69 | −1.423 | −2.000 | 0.571 (−1.79, 2.94) | 0.536 |
| 70–79 | −0.265 | −1.227 | 0.963 (1.09, 3.01) | 0.382 |
| ≥80 | −1.000 | 0.125 | 1.125 (3.62, 1.37) | 0.592 |
| Educational level | ||||
| Junior compulsory | −0.417 | 1.600 | −2.017 (−4.92, 0.89) | 0.218 |
| High school | −0.227 | −1.833 | 1.606 (−0.17, 3.38) | 0.028 |
| University | −1.143 | −2.333 | 1.190 (−1.52, 3.90) | 0.673 |
| Surgical technique | ||||
| OR | 0.167 | −1.636 | 1.803 (−0.82, 4.42) | 0.117 |
| EVAR | −0.967 | −0.762 | −0.205 (−1.63, 1.22) | 0.900 |
| Sex | ||||
| Men | −0.465 | −0.943 | 0.478 (−1.01, 1.97) | 0.319 |
| Women | −1.200 | −2.375 | 0.175 (−2.91, 5.26) | 0.767 |
Subgroup analyses of age, educational level, sex and surgical technique are also presented. Values in parentheses are 95% confidence intervals. HADS-A, Hospital Anxiety and Depression Scale Anxiety; OR, open repair; EVAR, endovascular aortic repair.
*Mann–Whitney test.
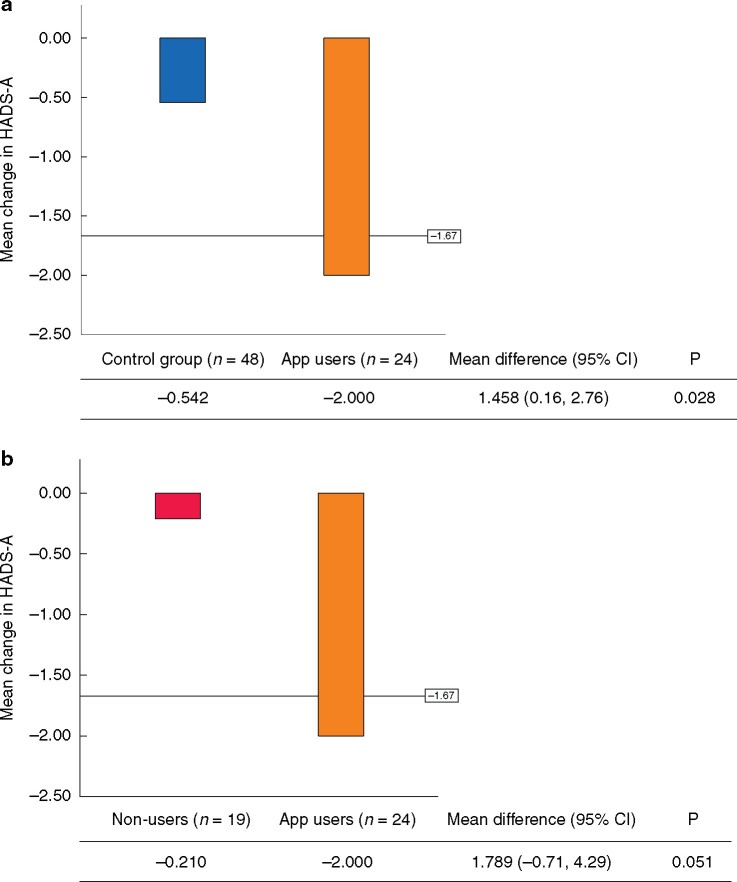
In the per protocol analysis, statistically and clinically significant differences were found in both within-group and between-group estimations. In the intervention group, the subgroup of participants who received the complete intervention comprising the eHealth tool and psychosocial support had a greater reduction in HADS-A mean scores than the control group (−0.54 in the control group versus −2.0 for app users in the intervention group, P = 0.028), illustrated in Fig. 2. In analyses within the intervention group, users of the eHealth tool reported a larger reduction in HADS-A mean scores than non-users (−0.21 non-users versus −2.00 app users, P = 0.051) (Fig. 2). Larger reductions in HADS-A mean scores were noted in patients with higher educational level (Table 2).
Fig. 2.
Per protocol analyses of mean differences in Hospital Anxiety and Depression Scale Anxiety scores from baseline to follow-up
The reference line indicates the minimal clinically important difference. a Changes in Hospital Anxiety and Depression Scale Anxiety (HADS-A) mean scores for control group versus users of the eHealth tool. b Changes in HADS-A mean scores for users versus non-users of the eHealth tool in the intervention group.
Depression and HRQoL
The distribution of patients with HADS-D of 8 points or greater were similar in the intervention group (13 participants, 23 per cent) and the control group (10 participants, 17 per cent) at baseline (TableS4). In the primary, intention-to-treat analysis, no significant difference in HADS-D mean scores was detected between the control group and intervention group at follow-up (Table 3). The secondary, per protocol analysis of the effect of the eHealth tool did not reveal statistically significant effects on either HADS-D or SF-12. In subgroup analyses of changes in HADS-D and SF-12 stratified by surgical treatment method or sex, no significant differences were detected (data not shown). The PCS score of the SF-12 instrument was similar between the intervention group and the control group at baseline and at the postoperative follow-up. Both groups decreased in physical functioning following surgical repair. Among patients who used the eHealth tool and received psychosocial support in the intervention, the decrease in PCS score was more pronounced than in the control group (−4.32 versus −1.16, P = 0.042). No differences were detected between the groups regarding the MCS score at baseline or postoperatively. The MCS scores did not differ significantly between the timepoints between the groups.
Discussion
The eHealth intervention as delivered in this study did not prove effective in reducing anxiety symptoms in those participants randomized to receive it. Unfortunately, within the intervention group, only half of the patients utilized the eHealth tool. There were clinically and statistically significant reductions in HADS-A mean scores among those who utilized the eHealth tool and received psychosocial support. Those who only received psychosocial support had less evidence of benefits from the intervention. The effects of the intervention were not reflected in the secondary outcomes of depression and HRQoL.
Anxiety measured by HADS-A has been described with a prevalence of 17 per cent in adults admitted to hospital19. Anxiety levels in AAA patients facing surgery are reportedly even higher7. In the current study, a high proportion of patients in both the control group and the intervention group presented with borderline or clinical anxiety at baseline. When facing major surgery, anxiety is a natural and unavoidable phenomenon, and following surgery anxiety levels can be expected to decrease20. It is essential to differentiate the natural course of anxiety from that mediated by the intervention when assessing the effect of this eHealth intervention. A reported minimal clinically important difference in HADS-A scores for interventions in patients with cardiovascular disease is 1.29–1.6715. In the current study, the mean reduction in HADS-A scores for participants utilizing the eHealth tool and receiving psychosocial support by far exceeded this threshold, representing a clinically important reduction in anxiety. Furthermore, the hypothesized 50 per cent decrease in anxiety mean scores in the intervention group was exceeded compared with the control group (1.21 versus expected 0.81), signifying the clinical benefit of the intervention. Interestingly, the detected mean anxiety scores in the present trial were lower than those reported from eHealth interventions targeting cardiac patients with higher baseline scores17.
Despite being offered an introduction to the eHealth tool and a tablet during the study period, only half of the participants in the intervention group chose to utilize the tool. In the current study, app users were younger and had higher educational level than non-users. Educational level correlates strongly to poorer health outcomes, and health literacy has been proposed as a potential explanation21. Health literacy, defined as the degree to which individuals can obtain, process and utilize health information, has been found to be inadequate in 76 per cent of patients with vascular disease22. Although the use of digital health technology is increasing rapidly among the elderly, the low acceptability of the eHealth tool in the present study may pertain to a continued reluctance to use digital health technology in the older population11. In the scientific community, increasing emphasis has been put on the need for improved eHealth services targeting older adults and vulnerable groups. In the field of vascular surgery, this development is, however, challenged by the limited health literacy, and a general reluctance to use digital health technology22, as reflected in the study findings. For successful implementation of eHealth, adaptation to the health literacy and utilization of modern technology in this patient cohort is imperative. According to the Technology Acceptance Model, determinants of technology acceptance among older adults include perceived usefulness and perceived ease of use23. These aspects were attended to in the design of the eHealth tool by employing a participatory design process, but the final product nonetheless failed to attract a large proportion of its potential end users. An earlier introduction of the eHealth tool during surveillance with personalized technical assistance may have yielded a higher proportion of app users, especially among older participants and those with lower educational level.
Several aspects of adherence should be considered when interpreting the results of the current study. For logistical reasons, participants were recruited 1 week prior to surgery. At that point, patients may already have started to become increasingly anxious, possibly rendering them insusceptible to the intervention. Furthermore, the content and structure of the psychosocial support sessions were based on the concept of person-centred care but were not fixed and there may have been variations in the delivery of this part of the intervention.
It is interesting to note that the reported mean scores of depression throughout the study, measured by HADS-D, reflect reported levels in the general population19. There were no significant alterations in HADS-D scores by the intervention, even if both groups reported improved scores after surgical treatment. The possible association between depression and development of cardiovascular diseases and higher mortality should render more attention in the preventive care of these patients. This would, however, presumably require other measures and interventions over a longer period for proper evaluation. The SF-12 has the benefit of being a short instrument, alleviating the respondent burden, but has been found to have psychometric shortcomings24. The instrument is weighted by a factor derived from a general US sample, and no scoring algorithm for the Swedish population is available. The two components, MCS and PCS, can be analysed separately, but further in-depth analysis by the eight inherent items was not considered suitable due to the relatively small sample in this study. The lower physical functioning by PCS in the intervention group at follow-up could be associated with the higher proportion undergoing open repair in this group. The MCS levels were largely unchanged between baseline and follow-up within and between the treatment groups. The impact of having an asymptomatic but potentially lethal condition such as AAA on HRQoL, may, however, not be adequately captured by the SF-12 instrument. Validated HRQoL instruments with a high sensitivity and specificity in capturing aspects of physical and mental health during the perioperative period have been developed but are currently not available in Swedish and were therefore not used in the present study25,26.
For successful implementation of eHealth, adaptation to the health literacy and utilization of modern technology in this patient cohort is imperative. As the per protocol analysis indicated the intervention did reduce anxiety when delivered as intended, future studies should assume a limited acceptability of eHealth services in this cohort of patients when planning and designing similar interventions. An earlier introduction of the intervention could possibly have provided more time to provide participants with psychosocial support and may have yielded a higher proportion of app users.
Supplementary Material
Acknowledgements
We wish to express our gratitude to all patients who contributed to the study. We also want to express our gratitude to co-workers at the research unit for the collection of data (Alicia Garcia Lantz, Mariette Aderö, Iva Jergovic and Mareia Talvitie) and to the statistician Maria Ionna Kotopouli for advice in the statistical analysis.
Author contributions are as follows.
Conceptualization: O.N., R.H., A.L.; data curation: O.N., R.H.; formal analysis: O.N., R.H.; funding acquisition: R.H.; investigation: O.N., R.H.; methodology: O.N., R.H.; project administration: O.N.; resources: R.H.; supervision: R.H., A.L.; writing – original draft: R.H., O.N.; writing – review and editing: R.H., O.N., M.S., A.L.
Funding
This research was supported by the Heart and Lung Association (FA 2019:28), the Swedish Heart-Lung Foundation (grant numbers: 20140722, 20160266, 20190553) and through the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet (Hultgren). All authors confirm independence from funders. All study data were fully available to the authors, maintaining the integrity of the data and accuracy of the data analysis.
Disclosure. The authors declare no conflictsof interest.
Supplementary material
Supplementary material is available at BJS online.
References
- 1. Wanhainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T. et al. Editor's Choice –European Society for Vascular Surgery (ESVS) 2019 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg 2019;57:8–93 [DOI] [PubMed] [Google Scholar]
- 2. Santema TB, Stoffer EA, Kunneman M, Koelemay MJ, Ubbink DT.. What are the decision-making preferences of patients in vascular surgery? A mixed-methods study. BMJ Open 2017;7:e013272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lyttkens L, Wanhainen A, Svensjo S, Hultgren R, Bjorck M, Jangland E.. Systematic review and meta-analysis of health related quality of life and reported experiences in patients with abdominal aortic aneurysm under ultrasound surveillance. Eur J Vasc Endovasc Surg 2020;59:420–427 [DOI] [PubMed] [Google Scholar]
- 4. Ericsson A, Kumlien C, Ching S, Carlson E, Molassiotis A.. Impact on quality of life of men with screening-detected abdominal aortic aneurysms attending regular follow ups: a narrative literature review. Eur J Vasc Endovasc Surg 2019;57:589–596 [DOI] [PubMed] [Google Scholar]
- 5. Eberhart L, Aust H, Schuster M, Sturm T, Gehling M, Euteneuer F. et al. Preoperative anxiety in adults – a cross-sectional study on specific fears and risk factors. BMC Psychiatry 2020;20:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Williams JB, Alexander KP, Morin JF, Langlois Y, Noiseux N, Perrault LP. et al. Preoperative anxiety as a predictor of mortality and major morbidity in patients aged >70 years undergoing cardiac surgery. Am J Cardiol 2013;111:137–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu XY, Ma YK, Zhao JC, Wu ZP, Zhang L, Liu LH.. Risk factors for preoperative anxiety and depression in patients scheduled for abdominal aortic aneurysm repair. Chin Med J (Engl) 2018;131:1951–1957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nilsson O, Hultgren R, Letterstal A.. Perceived learning needs of patients with abdominal aortic aneurysm. J Vasc Nurs 2017;35:4–11 [DOI] [PubMed] [Google Scholar]
- 9. Scott BB, Johnson AR, Doval AF, Tran BN, Lee BT.. Readability and understandability analysis of online materials related to abdominal aortic aneurysm repair. Vasc Endovascular Surg 2020;54:111–117 [DOI] [PubMed] [Google Scholar]
- 10. Radonjic A, Fat HNN, Harlock J, Naji F.. YouTube as a source of patient information for abdominal aortic aneurysms. J Vasc Surg 2020;71:637–644 [DOI] [PubMed] [Google Scholar]
- 11. Berner J, Rennemark M, Jogreus C, Anderberg P, Skoldunger A, Wahlberg M. et al. Factors influencing Internet usage in older adults (65 years and above) living in rural and urban Sweden. Health Informatics J 2015;21:237–249 [DOI] [PubMed] [Google Scholar]
- 12. Barello S, Triberti S, Graffigna G, Libreri C, Serino S, Hibbard J. et al. eHealth for patient engagement: a systematic review. Front Psychol 2016;6:2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nilsson O, Hultgren R, Letterstal A.. eHealth tool for patients with abdominal aortic aneurysm: development and initial evaluation. Scand J Caring Sci 2020;34:348–356 [DOI] [PubMed] [Google Scholar]
- 14. Bjelland I, Dahl AA, Haug TT, Neckelmann D.. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77 [DOI] [PubMed] [Google Scholar]
- 15. Lemay KR, Tulloch HE, Pipe AL, Reed JL.. Establishing the minimal clinically important difference for the hospital anxiety and depression scale in patients with cardiovascular disease. J Cardiopulm Rehabil Prev 2019;39:E6–E11 [DOI] [PubMed] [Google Scholar]
- 16. Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE. et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998;51:1171–1178 [DOI] [PubMed] [Google Scholar]
- 17. Guo P, East L, Arthur A.. A preoperative education intervention to reduce anxiety and improve recovery among Chinese cardiac patients: a randomized controlled trial. Int J Nurs Stud 2012;49:129–137 [DOI] [PubMed] [Google Scholar]
- 18. Arnold J, Goodacre S, Bath P, Price J.. Information sheets for patients with acute chest pain: randomised controlled trial. BMJ 2009;338:b541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sjoberg L, Karlsson B, Atti AR, Skoog I, Fratiglioni L, Wang HX.. Prevalence of depression: comparisons of different depression definitions in population-based samples of older adults. J Affect Disord 2017;221:123–131 [DOI] [PubMed] [Google Scholar]
- 20. Korbmacher B, Ulbrich S, Dalyanoglu H, Lichtenberg A, Schipke JD, Franz M. et al. Perioperative and long-term development of anxiety and depression in CABG patients. Thorac Cardiovasc Surg 2013;61:676–681 [DOI] [PubMed] [Google Scholar]
- 21. van der Heide I, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, Uiters E.. The relationship between health, education, and health literacy: results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun 2013;18:172–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Strijbos RM, Hinnen JW, van den Haak RFF, Verhoeven BAN, Koning OHJ.. Inadequate health literacy in patients with arterial vascular disease. Eur J Vasc Endovasc Surg 2018;56:239–245 [DOI] [PubMed] [Google Scholar]
- 23. Portz JD, Bayliss EA, Bull S, Boxer RS, Bekelman DB, Gleason K. et al. Using the technology acceptance model to explore user experience, intent to use, and use behavior of a patient portal among older adults with multiple chronic conditions: descriptive qualitative study. J Med Internet Res 2019;21:e11604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hagell P, Westergren A, Arestedt K.. Beware of the origin of numbers: standard scoring of the SF-12 and SF-36 summary measures distorts measurement and score interpretations. Res Nurs Health 2017;40:378–386 [DOI] [PubMed] [Google Scholar]
- 25. Suckow BD, Schanzer AS, Hoel AW, Wyers M, Marone LK, Veeraswamy RK. et al. A novel quality of life instrument for patients with an abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 2019;57:809–815 [DOI] [PubMed] [Google Scholar]
- 26. Peach G, Romaine J, Wilson A, Holt PJ, Thompson MM, Hinchliffe RJ. et al. Design of new patient-reported outcome measures to assess quality of life, symptoms and treatment satisfaction in patients with abdominal aortic aneurysm. Br J Surg 2016;103:1003–1011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.