Abstract
Climate change is one of the major public health emergencies with already unprecedented impacts on our planet, environment and health. Climate change has already resulted in substantial increases in temperatures globally and more frequent and extreme weather in terms of heatwaves, droughts, dust storms, wildfires, rainstorms and flooding, with prolonged and altered allergen and microbial exposure as well as the introduction of new allergens to certain areas. All these exposures may have a major burden on patients with respiratory conditions, which will pose increasing challenges for respiratory clinicians and other healthcare providers. In addition, complex interactions between these different factors, along with other major environmental risk factors (e.g. air pollution), will exacerbate adverse health effects on the lung. For example, an increase in heat and sunlight in urban areas will lead to increases in ozone exposure among urban populations; effects of very high exposure to smoke and pollution from wildfires will be exacerbated by the accompanying heat and drought; and extreme precipitation events and flooding will increase exposure to humidity and mould indoors. This review aims to bring respiratory healthcare providers up to date with the newest research on the impacts of climate change on respiratory health. Respiratory clinicians and other healthcare providers need to be continually educated about the challenges of this emerging and growing public health problem and be equipped to be the key players in solutions to mitigate the impacts of climate change on patients with respiratory conditions.
Educational aims
To define climate change and describe major related environmental factors that pose a threat to patients with respiratory conditions.
To provide an overview of the epidemiological evidence on climate change and respiratory diseases.
To explain how climate change interacts with air pollution and other related environmental hazards to pose additional challenges for patients.
To outline recommendations to protect the health of patients with respiratory conditions from climate-related environmental hazards in clinical practice.
To outline recommendations to clinicians and patients with respiratory conditions on how to contribute to mitigating climate change.
Tweetable abstract
Climate change is a major threat to lung patients due to increasing temperatures, more extreme weather, poorer air quality, and altered allergen and microbial exposure. Respiratory clinicians must be educated to mitigate this burden to their patients. https://bit.ly/43lE32N
Introduction
The continuous increase in anthropogenic emissions of carbon dioxide and other greenhouse gases since the industrial period is dramatically changing the climate at all scales. Burning fossil fuels (i.e. coal, oil, gas) for transport, industry, energy production and residential heating and cooking, burning solid waste, cutting down forests, agricultural activities (i.e. use of fertilisers containing nitrogen), farming livestock (i.e. methane from cows and sheep) and fluorinated gases (F-gases) from equipment and products are increasingly influencing the climate and the Earth's temperature. The sixth assessment report of the Intergovernmental Panel on Climate Change (IPCC), the most important panel of experts in the field, concluded that it is unequivocal that human influence has warmed the climate at a rate that is unprecedented in at least the past 2000 years, resulting in a world that is currently 1.1°C warmer than in the preindustrial period [1]. This temperature rise has had impacts on physical systems, including a rise in sea level, and led to an increase in climate variability with a higher frequency, intensity and severity of extreme weather events, such as heatwaves, floods and hurricanes. Additionally, these weather changes have led to a worsening of air quality (e.g. more frequent and severe wildfires, altered pollen levels, dust storms and an increase in ground-level ozone levels), changes in transmissibility of vector-borne diseases and alteration of crop production. Climate scenarios for the next century show that warming will progress at a much faster and alarming speed if no reductions in greenhouse gas emissions occur.
The impacts of climate change on human health are pervasive, profound, and substantial; they affect everyone and are expected to amplify in the near future [2, 3]. The health impact of climate change is considered the biggest and most important global public health issue and threat to humanity of this century, as stated by the World Health Organization (WHO) [4]. Health impacts are variable in magnitude and severity, depending on the location. This variation is mostly driven by preparedness, level of vulnerability and adaptation capacity. On top of the ongoing warming and changing patterns in other climate-related hazards, existing societal challenges (e.g. social inequality, progressive urbanisation, ageing populations) will amplify the health burden attributed to climate change [5, 6]. For example, vulnerable and already marginalised populations are and will continue to be disproportionally impacted by climate change, including impoverished and undernourished communities. Chronic disease patients, older populations, children, pregnant women, and outdoor workers are considered particularly vulnerable to climate-related hazards. It has been estimated that by 2050, climate change will result in at least 250 000 deaths every year related to heat stress, malnutrition, malaria, and diarrhoea [3]. An additional burden will arise from climate-related population migrations, conflicts, poverty, and disruption of healthcare and ecosystems.
The climate crisis is challenging the fundamental mission of health professionals, which is to improve health, prevent harm, and advance equity. Here we aim to guide clinicians and other healthcare professionals, patients and patient organisations on how global warming can be addressed in clinical practice. We summarise current evidence on the impact of climate change on respiratory health and discuss how mitigation and adaptation strategies synergise with other policies for respiratory health (i.e. clean air policies, sustainable urban development), how climate change impacts daily activities in clinical practice and patient behaviour, and how clinicians and patients can act as advocates for climate-friendly policies from the clinical practice.
The impact of climate change on respiratory health
Climate change affects health directly, due to the impact of extreme weather events, such as heatwaves, dust storms or floods, and indirectly, via climate change-caused alterations in allergen levels, prolonged allergen seasons, worsened air quality and occurrence of transmittable viral infections and vector-borne diseases [7, 8]. Patients with chronic respiratory disease are arguably among those most susceptible to the adverse effects of climate change [9]. In particular, patients with an already impaired lung function due to asthma, COPD, lung cancer or interstitial lung disease are considered especially vulnerable to weather changes and extreme conditions, with increased risks of exacerbations (e.g. coughing, wheeze, shortness of breath, difficulties breathing, emergency room visits or hospitalisations) and death [9–12]. Also in the general population, climate change events and exposures may adversely affect lung function, increase allergic responses, and trigger new-onset asthma, COPD and also lung cancer [13–16].
Increase in temperatures, heatwaves and respiratory health
Temperature and its effects on health have been the most studied aspect of climate change. High temperatures have been associated with increased risks of respiratory disease hospitalisations and mortality [17]. Exposure to high temperatures or extreme heat, especially in the summer, can trigger respiratory symptoms that may require extra use of rescue medication, healthcare visits to the general practitioner or emergency room, hospital admission or even intensive care with respiratory support [18–20]. Furthermore, increasing temperatures in combination with increasing humidity also pose an additional burden, especially to asthma and allergy patients. Breathing hot and humid air is “heavy” and harder to breathe, causing increased respiration rate and respiratory ventilation rate in healthy subjects [21], airway irritation and cough in patients with allergic rhinitis [12], and bronchoconstriction and cough in patients with asthma [11]. This is also apparent in the increased risks of emergency room visits and hospitalisations for these respiratory diseases on days with high temperature and humidity [11]. Another concern relates to physical activity outdoors (e.g. walking, cycling, jogging) during periods with high temperatures, as exercise can exacerbate adverse effects of heat, especially in patients with respiratory diseases [22]. Rising frequency of days and hours with uncomfortable temperatures will likely lead to a decrease in physical activity outdoors [23]. City-wide adaptations (e.g. building of green cycling lines that provide shade, greening in general for shade and lowering of temperature) and personal physical activity interventions (e.g. shifting to activities indoors in cooled areas, timing activities for less warm hours of the day, increasing hydration during exercise) are needed to sustain physical activity levels in the face of shifting temperatures due to climate change [24, 25]. Children may be even more susceptible to extreme temperatures than adults, given their physiological properties (discussed later in this review) and typically more limited opportunities to influence their position or physical activity [20, 26].
Aeroallergen levels, pollen seasons and respiratory health
Recent data suggest shifts in pollen and other aeroallergens' level and intensity, peak season and exposure duration in Europe and globally [27]. Climate change is believed to be partly responsible for these changing temporal and spatial patterns in the pollen season and in pollen composition, which are expected to continue in the next years. There are also reports of the introduction of new aeroallergens to new areas, which may disturb the balance of ecological systems and negatively affect biodiversity [28]. Changes in allergen levels and season will give rise to challenges for both patients (longer/altered pollen seasons, new allergens) as well as caregivers (new patient groups, diagnostics for new allergens, etc.). Increasing grass pollen concentration has also been associated with an increased risk of non-respiratory conditions like food allergy and eczema flares in children, which is important to consider from a clinical point of view [29]. In addition, air pollutants can interact with airborne allergens and enhance the risk of allergic sensitisation and exacerbation of symptoms in sensitised individuals, especially under conditions where drought spells (or thunderstorms) promote resuspension of dust particles and increase air pollution exposure. Despite strong evidence from small experimental studies in humans showing significant allergen–air pollutant interactions, evidence from epidemiological studies is still mixed. This is likely to be due to exposure misclassification, failure to examine subgroups at risk, inadequate statistical power or the absence of population-level effects, demanding more research on this topic [30]. Climate change will probably increase the frequency of thunderstorms, which have been associated with increasing allergic asthma outbreaks mediated through allergen exposure, notably pollens and wet-air fungal spora [31, 32]. Finally, changes in weather linked to climate change can drive changes in the composition, production and spread of other aeroallergens [33]. For example, extreme weather events, such as heavy rainfall and floods, can exacerbate indoor mould or dust mite exposure leading to worsened respiratory health [34, 35]. Strong associations between residential exposure to moisture damage or mould during early childhood and a persistent wheezing phenotype later in childhood have already been observed [36].
Infections and vector-borne disease and respiratory health
Climate change is making the weather more variable, by altering the seasonality of weather conditions and/or causing sudden changes in temperature and precipitation [1]. These changing weather patterns will alter the survival, reproduction, and distribution of some climate-sensitive pathogens causing respiratory infections [37, 38]. For example, recent studies have suggested that an increase in temperature may be associated with an increased risk of pulmonary tuberculosis [39, 40]. Additionally, it is unclear whether winter respiratory infections will actually decrease with increasing global temperatures. Recent studies have shown that fluctuating temperatures may affect the incidence of and mortality from respiratory infections [41]. Other studies found that warm winters are usually followed by more severe influenza epidemics [42]. Extreme precipitation events have been associated with an increased risk of respiratory infections [43]. With a warmer climate, problems like vector-borne diseases may become more frequent in areas hitherto not affected. One such example from the allergy domain is mammalian meat allergy, which is linked to tick bites and the development of IgE specific for the carbohydrate allergen galactose-alpha-1,3-galactose (alpha-gal) [44]. More specifically, tick bites by the Amblyomma americanum tick and other species lead to sensitisation to alpha-gal, a carbohydrate present in the tick's gastrointestinal tract. Since alpha-gal is also present in many red meats, sensitised individuals may experience allergic reactions after eating beef and other mammalian meats. With a warmer climate, ticks are reported to thrive and spread to “new” areas and regions.
Climate change and children's health
Children are considered especially vulnerable to climate change, as their lungs and immune systems are still under development, they breathe faster than adults, breathing in (polluted air, hot air, or air with aeroallergens) about 2–3 times as much as adults, and they spend more time outside and are more physically active than adults. Furthermore, children cannot influence their living conditions or exposures and rely on caregivers and society to take responsibility for a healthy environment. Global warming with extended pollen seasons may have severe consequences for children and adolescents with allergic asthma, which is the dominant phenotype in these age groups [45, 46]. Sensitisation rates and respiratory allergies to airborne allergens, including grass pollen, tree pollen or dust mites, have increased globally in recent years [45]. Importantly, climate change impacts children's health from conception. Exposure to hot temperatures during pregnancy can increase the risk of preterm birth, low birth weight and even stillbirths, and pregnant women with asthma are among those with the highest risk [47]. Critical periods also include the first years of life with detectable respiratory effects of, for example, air pollution exposure on the developing lung [48]. It has become apparent that chronic lung disease in adults, such as COPD, may have origins in childhood and that the underlying pathophysiology can be explained by a series of events due to gene–environment interactions across the lifespan [49]. Also, for classic diseases that have been linked to tobacco smoking (e.g. chronic bronchitis) there are clear associations with air pollution exposure early in life [49, 50]. Therefore, prevention of chronic respiratory disease and efforts to mitigate adverse effects of climate change and environmental exposures should start as early as possible.
Climate change and air pollution: two sides of the same coin
Ambient air pollution is the most important environmental risk factor, responsible for 6.7 million deaths globally in 2019 [51], and 373 000 in Europe [52]. Climate change and air pollution are intrinsically connected, as greenhouse gases and air pollutants share the same major sources: fossil fuel and biomass combustion (wood and coal burning for energy production and residential heating and cooking, etc.), animal production emitting methane and greenhouse gases as well as ammonia, which forms particulate matter and may be harmful to patients with respiratory conditions. Additionally, weather can aggravate already poor air quality by altering its dispersion capacity, composition, and toxicity. For example, higher temperatures and extended sunlight exposure increase the formation of ground-level ozone, a powerful lung irritant that can trigger asthma and mortality due to respiratory diseases [53, 54]. Prolonged heat and drought events increase the risk of wildfires and dust storms, causing massive air pollution exposures to local communities with devastating consequences for their health, but also produce harmful particles that can travel thousands of kilometres affecting populations far away from the source for up to several weeks [55–57]. Another concern for patients with respiratory conditions, especially patients with severe allergic asthma, is the interaction between air pollution and pollen/aeroallergen exposure, although evidence on the topic is still mixed and sparse [30]. Poorer air quality, frequency and severity of wildfires and dust storms can impair lung function and growth, especially in children [58], increasing the risk of hospitalisations and death [55, 57].
Nature, climate change, and patients with respiratory conditions
With rapid urbanisation, more time spent indoors, and a decline in human contact with nature globally, scientific interest in the health benefits of nature contact have grown [59]. Current research shows overwhelming evidence on the benefits of living close to green spaces for both physical and mental health, by providing spaces and opportunity for physical activity, social interaction, rest, relaxation and recreation. This supports the development of strategies to increase green spaces in urban areas, to improve health and well-being directly, but also as an efficient adaptation strategy for climate change by reducing exposure to increasing temperatures, providing shade and reducing the impact of urban heat island effects [60]. Increasing green infrastructure in cities also reduces the risk of urban flooding, as increased vegetation improves the storage capacity of the soil and reduces storm water runoff, improving urban drainage systems [61]. Although the effect of nature and green spaces on mitigating heat and flooding risks in urban environments carry clear benefits for patients with respiratory diseases, these may be outweighed for some by the risk related to a possible increase in aeroallergen exposure [62]. Thus, more research is needed in understanding the complex relationship of nature and exposure to green spaces on asthma and allergy patients. In the meantime, there is a clear need for guidelines for the design and planning of urban green spaces with a low allergy impact, which could include increased biodiversity, the use of low pollen producing and exotic species, the adoption of appropriate management and maintenance strategies, and active consultation with botanists [63]. Primary care and respiratory clinicians can actively advise, or even prescribe, that their patients increase the time they spend in nature, by nature prescribing, also referred to as nature therapy, ecotherapy, forest bathing or forest therapy [64]. They can recommend nature-based activities in “green spaces” (walking or running in parks and forests, animal care or gardening) or “blue spaces” (walking by water, swimming, sailing), but taking precautions with patients with allergic diseases related to aeroallergen exposures.
Climate change, social inequality and vulnerable patients
With respect to climate change effects on patients with respiratory diseases, special focus should be given to social inequalities, raising awareness of the need for extra efforts to help those most disadvantaged [65]. Climate change is already affecting vulnerable populations disproportionately. The most socioeconomically disadvantaged groups are less able to mitigate against the various impacts of climate change, in terms of modifications to their lifestyle (cannot afford more climate friendly diets, organic produce), adaption to their dwellings (cannot afford investment in air conditioning, air purifiers, insulation, or flood proofing and extra drainage in their homes), or the ability to move to less impacted locations [66]. Lower socioeconomic status is also closely related to occupations with higher exposure to heat and aeroallergens, such as construction workers working outside, people working in the agricultural sector, firefighters, etc. Finally, people who are less affluent may have poorer access to good healthcare and medication, and information about risks and how to mitigate them, and are less capable of having the means to manage their respiratory illness and adapt to new climate change related threats, leading to poorer prognosis of their diseases. This relationship between climate change and social inequality is characterised by a vicious cycle, whereby initial inequality causes the disadvantaged groups to suffer disproportionately from the adverse effects of climate change, resulting in greater subsequent inequality [65]. These factors impact at both the individual level, within cities and countries, as well as at regional level and between countries. For example, in Europe, where South and South-eastern Europe is more prone to heatwaves and wildfires, and where many countries suffer from higher levels of air pollution and socioeconomic disadvantages than North and Western Europe. This demands special focus on these groups by clinicians, as well as national and city governments in planning of climate mitigation plans.
Implications for healthcare providers and the patient
The role of respiratory physicians in the climate crisis
We have recently witnessed unprecedented action from healthcare professionals who have united to advocate on behalf of their patients and communities for climate action, under the unanimous motto “the climate crisis is a health crisis”. Through this action, health experts have pointed out that health is already being harmed by changes in the climate and the destruction of the natural world, and that “only fundamental and equitable changes in our society will reverse current trajectories”. Details of this call for action has been outlined in a recent joint statement of the editors of more than 200 health journals [67].
The 2021 United Nations Climate Change Conference (COP26) in Glasgow demonstrated the growing interest and engagement of the health community in the climate fight. This is significant, as there had been a general lack of focus and interest in climate change impacts on health at previous COPs. For the first time in Glasgow, the health agenda was part of the meeting, and the COP26 Health Programme, led by the UK government, WHO, Health Care Without Harm, and the United Nations Framework Convention on Climate Change Climate Champions was presented as a flagship initiative highlighting the health argument for climate action. In what was called COP1 for health and climate change, COP26 delivered key commitments by over 50 countries, including the implementation of strategies to build climate-resilient and low-carbon systems, but also heightened the crucial role of healthcare professionals and patients in this health crisis as activists.
Health professionals, as primary healthcare providers, have been traditionally considered one of the main actors in adaptation strategies (e.g. providing advice to patients to protect themselves during heatwaves, changing allergen seasons and wildfire episodes, prescribing spending time in nature). However, recent calls have been made to expand this point of view and engage health professionals, public health institutions and medical education systems to become active partners in climate change mitigation efforts. In particular, there is a growing interest and need to redesign healthcare systems and services with an increased focus on sustainability and planetary health. Planetary health refers to the interlinkages between human-induced deleterious changes in the environment, including climate change, and its impact on human health. The aim is to develop strategies that will help create an equitable, sustainable and healthy world [68]. A critical element here is the concept of “co-benefits”, which refers to how climate change mitigation activities can help advance other policy goals and improve health at the same time. Health co-benefits of climate mitigation strategies are particularly attractive for policymakers, as the overall balance in the form of health benefits is larger than the cost of actions [69, 70]. Co-benefits arise from the reductions in air pollution levels, increase in exposure to nature and green spaces, and promotion of active travel, physical activity and sustainable diets, which have been seen to translate into immediate improvements in health, including reducing the risk of cardiorespiratory diseases and other comorbidities. Special caution must be taken for patients with respiratory diseases with respect to the risks associated with increased exposure to heat, for example related to physical activity in summer months, as well as to increased exposure to aeroallergens when spending more time in nature and green areas.
There are several ways that respiratory physicians, nurses and other professionals, in their clinical practice, can contribute to reducing greenhouse gas emissions. These range from strategies for greening healthcare systems, to promoting green prescriptions and advocating for larger engagement of communities and individuals with climate-friendly activities (box 1), to the specific recommendations for respiratory clinicians on what advice to give to support their patients in mitigating the risks of climate change on their health (box 2). Importantly, reduced greenhouse gas emissions may be achieved by “simple” and straightforward measures like following clinical guidelines, adherence to the respective disease action plans and a personalised medicine approach that can optimise disease control, improve inhaler technique and, for asthma (and COPD) patients, minimise short-acting β-agonist (SABA) overuse [72, 73]. SABA overuse is not only associated with an increased risk of asthma exacerbations in both children and adults [74, 75], but also contributes a large part of the carbon footprint of the respiratory community, due to the release of F-gases with use of SABA inhalers. F-gases are commonly used as they act as a propellant to quickly release the liquid medication into the lungs effortlessly. They have been widely used in recent years as they do not damage the atmospheric ozone layer, but they are powerful greenhouse gases, contributing substantially to climate change. Since dry powder inhalers (DPIs) have a much lower global warming potential than pressurised metered-dose inhalers (pMDIs), choosing a DPI over a pMDI, when possible, is thus encouraged [46]. For more information on the European Respiratory Society (ERS) position statement on asthma and environment, where these issues are discussed in more detail, please visit the ERS website (https://www.ersnet.org/news-and-features/news/ers-publishes-position-statement-asthma-environment/).
BOX 1 A selection of some of the co-benefit actions proposed by the World Organization of Family Doctors (WONCA) [71], which could apply to safeguard the health of patients with respiratory conditions
• Transition to more sustainable food choices, such as diets with reduced use of meat (especially beef), vegetarian or purely plant-based diets.
• Promote active transport (e.g. cycling, walking and using public transport) instead of driving a car to reduce greenhouse gas emissions and air pollution and increase physical activity.
• Connect with nature to improve physical and mental health.
• Carry out sustainable drug prescribing, to reduce emissions of greenhouse gases (i.e. F-gases in asthma/COPD pressurised metered-dose inhalers) and prevent the impacts of some active pharmaceutical ingredients in the environment.
• Promote disease prevention activities to reduce the carbon footprint burden of healthcare systems.
BOX 2 Priority areas for climate change mitigation for respiratory clinicians
• Acknowledge and discuss climate change effects on respiratory health with patients and colleagues.
• Improve and provide continued education for respiratory healthcare professionals on the impact of climate change.
• Focus attention on high-risk and vulnerable populations, including elderly citizens, children, pregnant women, chronic disease patients, socioeconomically disadvantaged groups, and people and occupational groups who work primarily outdoors.
• Use nature prescribing to improve the health of patients with respiratory diseases and to mitigate effects of climate change, but be aware of aeroallergen exposure.
• Establish environmental monitoring of new allergenic species as potential triggers for allergic respiratory conditions.
• Advocate for the provision of “cool places” or “cooling devices” to be made available to individuals with respiratory conditions at high risk during heatwave conditions.
• Promote climate-friendly activities and lifestyle among clinicians and patients that will lead to personal health and planetary co-benefits.
• Use health professionals as trusted members of communities to raise awareness of the impacts of climate change and to boost national/international policy action.
• Conduct interdisciplinary research to advance knowledge on climate change health impacts and adaptation mechanisms.
• Act as an example in reducing greenhouse gas emissions in clinical practice (e.g. prescribe dry powder inhalers instead of pressurised metered-dose inhalers when possible) and in our daily activities.
Paving the way for the next generations: lessons learnt from the COVID-19 pandemic
We are still mapping the full consequences of the coronavirus disease 2019 (COVID-19) pandemic, a public health crisis that has caused unprecedented loss of life, disease burden, and damage to our societies and economy, and has forced a re-examination of our existing public health strategies to face future global crises, such as climate change [76]. Both climate change and the COVID-19 pandemic are major global public health threats for which ambitious strategies at the local, regional and global scales are required to efficiently reduce their health burden. The ongoing COVID-19 pandemic has triggered new awareness about the delicate links between a fossil fuel-based economy, our lifestyle, climate change, agriculture and the way we produce food, the deterioration of natural biodiversity, the emergence of new infections, and planetary and human health, with the respiratory disease patient at its epicentre. The waste, such as extensive use of plastics, our treatment of animals, etc. requires solutions at the national and even global level. It clearly demonstrates that all societies, even the most advanced, can be severely impacted by such global crises with unexpected disruptions and wide-ranging effects at all levels, especially when public health systems are not well prepared. The crucial role of interdisciplinary research to solve novel, complex, and fast-emerging global health crises is another lesson from the pandemic. Open collaboration and communication between experts across disciplines, including clinicians, epidemiologists, public health officials, researchers, and experts in natural sciences, as well as patients, to efficiently guide policy have been pivotal in this battle and a similar approach is proposed as the way to go in our fight against climate change.
Conclusion
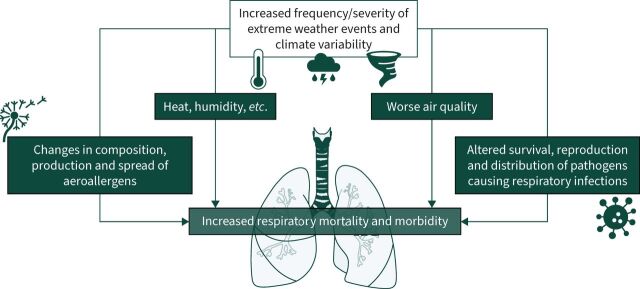
Climate change represents a major threat to patients living with respiratory conditions, through several different direct and indirect pathways (figure 1), including the increase in temperature, increase in ozone exposure, prolonged aeroallergen seasons and introduction of aeroallergens to new areas, increased frequency of extreme weather events such as heatwaves, droughts, wildfires, wind and dust storms, heavy rainfall and flooding, among others. Indirect effects include stress on society due to migration, conflicts, and economic burdens with adverse consequences for healthcare systems, ecosystems, and education. Furthermore, as the climate emergency progresses, it will become more likely that there will be compounding events. For example, extreme heat and drought events will lead to an increased risk of wildfires, causing both high levels of pollution and disruption of critical infrastructure including the electricity grid or contamination of water sources, as well as disruptions to healthcare systems, further impacting on the health of individuals with respiratory conditions. The scale of the climate change impact on the planet and human health that is now irreversible calls on physicians and other health professionals around the world to unite to advocate for the protection of our planet and for the health of people that live and depend on it. We have reached a point of no return. As recent extreme weather events have shown, we need to prepare our community for a much more complex future adapting to the ever-increasing impact of climate-related respiratory disease. It is important to add that apart from recommendations and guidelines aimed at individuals (healthcare workers, patients) on how to reduce their own contribution to climate change and mitigate its adverse effects, innovative solutions to slow climate change must also come from governments supporting bold regulation of greenhouse gases emissions in all sectors (industry, transport, heating, waste, agriculture, food production). Here medical and patient societies must, on behalf of their members and patients, engage, demand and advocate for such policies at European Union, national and regional/city level.
FIGURE 1.
Summary scheme of the pathways linking climate change and impacts of respiratory health.
Key points
Climate change is causing an increase in temperatures, heatwaves, droughts, dust storms, wildfires, rainstorms, flooding, and altered allergen and microbial exposures.
These exposures pose increasing threats to patients with respiratory conditions.
Climate change will worsen air pollution exposure in many places, adding additional complexity and challenges for patients.
Education of healthcare professionals about climate change is the key to reducing adverse health effects.
Knowledge and awareness of climate change will enable individualised measures empowering the patient and the clinician.
Self-evaluation questions
What aspects of climate change may be detrimental to respiratory health?
What type of patients are most likely to be affected?
In what way can climate change influence respiratory allergy diagnostics?
How may extreme heat conditions influence patients with respiratory conditions?
In our daily clinical practice, how can we reduce our carbon footprint?
Suggested answers
All aspects of climate change can be detrimental for respiratory patients: increase in temperatures and higher frequency of heatwaves, droughts, dust storms, wildfires, rainstorms, flooding, and altered allergen and microbial exposures.
Patients with an existing respiratory disease such as asthma, COPD, lung cancer or interstitial lung disease, and/or those with impaired lung function are considered especially vulnerable to weather changes and extreme conditions related to climate change.
Climate change is linked to shifts in pollen and other aeroallergen levels and intensity, peak season and exposure duration. New allergens may also appear in a given region. Therefore, allergy diagnostics must keep up to date with these trends (i.e. testing for relevant allergens).
High temperatures cause increased respiration and ventilation rates, and can increase the risk of symptoms and exacerbations in patients with respiratory diseases, i.e. need for medication, emergency room visits, hospitalisations and even mortality. These effects can be worsened in combination with high humidity and high air pollution (ozone, resuspended particles from dust related to droughts, or from wildfires).
Optimise asthma and allergy control in our patients. Minimise SABA overuse (if applicable). Prescribe dry powder inhalers instead of pressurised metered-dose inhalers when possible. Promote climate-friendly activities and lifestyle among clinicians and patients that will lead to personal health and planetary co-benefits.
Footnotes
Conflict of interest: Z.J. Andersen reports receiving support for attending meetings and/or travel from European Respiratory Society (ERS), outside the submitted work; and is Chair of the ERS Environment and Health Committee (EHC), and Executive Council member (councillor) of the International Society for Environmental Epidemiology (ISEE). A.M. Vicedo-Cabrera has nothing to disclose. B. Hoffmann has received honoraria for advisory board meetings from the Health Effects Institute, outside the submitted work; and is a member of the ERS Advocacy Council. E. Melén has received honoraria for lectures or advisory board meetings from ALK, AstraZeneca, Chiesi, Novartis and Sanofi outside the submitted work; and is a member of the ERS Environment and Health Committee (EHC).
References
- 1.Masson-Delmotte V, Zhai P, Pirani A, et al., eds. Climate change 2021: the physical science basis. Contribution of working group I to the sixth assessment report of the Intergovernmental Panel on Climate Change. Cambridge, Cambridge University Press, 2021. doi: 10.1017/9781009157896 [DOI] [Google Scholar]
- 2.Romanello M, Napoli CD, Drummond P, et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet 2022; 400: 1619–1654. doi: 10.1016/S0140-6736(22)01540-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pörtner H-O, Roberts DC, Tignor MMB, et al., eds. Climate change 2022: impacts, adaptation and vulnerability. Contribution of working group II to the sixth assessment report of the Intergovernmental Panel on Climate Change. Cambridge, Cambridge University Press, 2022. doi: 10.1017/9781009325844.2022 [DOI] [Google Scholar]
- 4.World Health Organization . Climate change and health. Date last updated: 30 October 2021. www.who.int/news-room/fact-sheets/detail/climate-change-and-health
- 5.Chen K, Vicedo-Cabrera AM, Dubrow R. Projections of ambient temperature- and air pollution-related mortality burden under combined climate change and population aging scenarios: a review. Curr Environ Health Rep 2020; 7: 243–255. doi: 10.1007/s40572-020-00281-6 [DOI] [PubMed] [Google Scholar]
- 6.Zhang W, Li Y, Li Z, et al. Impacts of climate change, population growth, and urbanization on future population exposure to long-term temperature change during the warm season in China. Environ Sci Pollut Res Int 2020; 27: 8481–8491. doi: 10.1007/s11356-019-07238-9 [DOI] [PubMed] [Google Scholar]
- 7.Ebi KL, Hasegawa T, Hayes K, et al. Health risks of warming of 1.5°C, 2°C, and higher, above pre-industrial temperatures. Environ Res Lett 2018; 13: 063007. doi: 10.1088/1748-9326/aac4bd [DOI] [Google Scholar]
- 8.Haines A, Ebi K. The imperative for climate action to protect health. N Engl J Med 2019; 380: 263–273. doi: 10.1056/NEJMra1807873 [DOI] [PubMed] [Google Scholar]
- 9.Bernstein AS, Rice MB. Lungs in a warming world: climate change and respiratory health. Chest 2013; 143: 1455–1459. doi: 10.1378/chest.12-2384 [DOI] [PubMed] [Google Scholar]
- 10.Aitken ML, Marini JJ. Effect of heat delivery and extraction on airway conductance in normal and in asthmatic subjects. Am Rev Respir Dis 1985; 131: 357–361. [DOI] [PubMed] [Google Scholar]
- 11.Hayes D, Collins PB, Khosravi M, et al. Bronchoconstriction triggered by breathing hot humid air in patients with asthma: role of cholinergic reflex. Am J Respir Crit Care Med 2012; 185: 1190–1196. doi: 10.1164/rccm.201201-0088OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khosravi M, Collins PB, Lin R-L, et al. Breathing hot humid air induces airway irritation and cough in patients with allergic rhinitis. Respir Physiol Neurobiol 2014; 198: 13–19. doi: 10.1016/j.resp.2014.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tong M, Wondmagegn B, Xiang J, et al. Hospitalization costs of respiratory diseases attributable to temperature in Australia and projections for future costs in the 2030s and 2050s under climate change. Int J Environ Res Public Health 2022; 19: 9706. doi: 10.3390/ijerph19159706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lakhoo DP, Blake HA, Chersich MF, et al. The effect of high and low ambient temperature on infant health: a systematic review. Int J Environ Res Public Health 2022; 19: 9109. doi: 10.3390/ijerph19159109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu Y, Cheng J, Liu S, et al. Evaluation of climate change adaptation measures for childhood asthma: a systematic review of epidemiological evidence. Sci Total Environ 2022; 839: 156291. doi: 10.1016/j.scitotenv.2022.156291 [DOI] [PubMed] [Google Scholar]
- 16.De Sario M, Katsouyanni K, Michelozzi P. Climate change, extreme weather events, air pollution and respiratory health in Europe. Eur Respir J 2013; 42: 826–843. doi: 10.1183/09031936.00074712 [DOI] [PubMed] [Google Scholar]
- 17.Baccini M, Biggeri A, Accetta G, et al. Heat effects on mortality in 15 European cities. Epidemiology 2008; 19: 711–719. doi: 10.1097/EDE.0b013e318176bfcd [DOI] [PubMed] [Google Scholar]
- 18.Iñiguez C, Royé D, Tobías A. Contrasting patterns of temperature related mortality and hospitalization by cardiovascular and respiratory diseases in 52 Spanish cities. Environ Res 2021; 192: 110191. doi: 10.1016/j.envres.2020.110191 [DOI] [PubMed] [Google Scholar]
- 19.Royé D, Tobías A, Figueiras A, et al. Temperature-related effects on respiratory medical prescriptions in Spain. Environ Res 2021; 202: 111695. doi: 10.1016/j.envres.2021.111695 [DOI] [PubMed] [Google Scholar]
- 20.Schinasi LH, Kenyon CC, Hubbard RA, et al. Associations between high ambient temperatures and asthma exacerbation among children in Philadelphia, PA: a time series analysis. Occup Environ Med 2022; 79: 326–332. doi: 10.1136/oemed-2021-107823 [DOI] [PubMed] [Google Scholar]
- 21.Zuo C, Luo L, Liu W. Effects of increased humidity on physiological responses, thermal comfort, perceived air quality, and Sick Building Syndrome symptoms at elevated indoor temperatures for subjects in a hot-humid climate. Indoor Air 2021; 31: 524–540. doi: 10.1111/ina.12739 [DOI] [PubMed] [Google Scholar]
- 22.Sawka MN, Wenger CB, Young AJet al. Physiological responses to exercise in the heat. In: Marriott BM, ed. Nutritional Needs in Hot Environments: Applications for Military Personnel in Field Operations. Washington, National Academies Press (US), 1993. [PubMed] [Google Scholar]
- 23.Ho JY, Goggins WB, Mo PKH, et al. The effect of temperature on physical activity: an aggregated timeseries analysis of smartphone users in five major Chinese cities. Int J Behav Nutr Phys Act 2022; 19: 68. doi: 10.1186/s12966-022-01285-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nieuwenhuijsen MJ. New urban models for more sustainable, liveable and healthier cities post covid19; reducing air pollution, noise and heat island effects and increasing green space and physical activity. Environ Int 2021; 157: 106850. doi: 10.1016/j.envint.2021.106850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abu-Omar K, Gelius P, Messing S. Physical activity promotion in the age of climate change. F1000Res 2020; 9: 349. doi: 10.12688/f1000research.23764.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uibel D, Sharma R, Piontkowski D, et al. Association of ambient extreme heat with pediatric morbidity: a scoping review. Int J Biometeorol 2022; 66: 1683–1698. doi: 10.1007/s00484-022-02310-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glick S, Gehrig R, Eeftens M. Multi-decade changes in pollen season onset, duration, and intensity: a concern for public health? Sci Total Environ 2021; 781: 146382. doi: 10.1016/j.scitotenv.2021.146382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang Y, Steiner AL. Projected climate-driven changes in pollen emission season length and magnitude over the continental United States. Nat Commun 2022; 13: 1234. doi: 10.1038/s41467-022-28764-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Idrose NS, Lodge CJ, Peters RL, et al. The role of short-term grass pollen exposure in food skin-prick test reactivity, food allergy, and eczema flares in children. Pediatr Allergy Immunol 2022; 33: e13862. doi: 10.1111/pai.13862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lam HCY, Jarvis D, Fuertes E. Interactive effects of allergens and air pollution on respiratory health: a systematic review. Sci Total Environ 2021; 757: 143924. doi: 10.1016/j.scitotenv.2020.143924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D'Amato G, Vitale C, D'Amato M, et al. Thunderstorm-related asthma: what happens and why. Clin Exp Allergy 2016; 46: 390–396. doi: 10.1111/cea.12709 [DOI] [PubMed] [Google Scholar]
- 32.Andrew E, Nehme Z, Bernard S, et al. Stormy weather: a retrospective analysis of demand for emergency medical services during epidemic thunderstorm asthma. BMJ 2017; 359: j5636. doi: 10.1136/bmj.j5636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.D'Amato G, Chong-Neto HJ, Monge Ortega OP, et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy 2020; 75: 2219–2228. doi: 10.1111/all.14476 [DOI] [PubMed] [Google Scholar]
- 34.Rao CY, Riggs MA, Chew GL, et al. Characterization of airborne molds, endotoxins, and glucans in homes in New Orleans after Hurricanes Katrina and Rita. Appl Environ Microbiol 2007; 73: 1630–1634. doi: 10.1128/AEM.01973-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rando RJ, Kwon C-W, Lefante JJ. Exposures to thoracic particulate matter, endotoxin, and glucan during post-Hurricane Katrina restoration work, New Orleans 2005–2012. J Occup Environ Hyg 2014; 11: 9–18. doi: 10.1080/15459624.2013.839879 [DOI] [PubMed] [Google Scholar]
- 36.Tischer C, Täubel M, Kirjavainen PV, et al. Early-life residential exposure to moisture damage is associated with persistent wheezing in a Finnish birth cohort. Pediatr Allergy Immunol 2022; 33: e13864. doi: 10.1111/pai.13864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mirsaeidi M, Motahari H, Taghizadeh Khamesi M, et al. Climate change and respiratory infections. Ann Am Thorac Soc 2016; 13: 1223–1230. doi: 10.1513/AnnalsATS.201511-729PS [DOI] [PubMed] [Google Scholar]
- 38.Michelozzi P, Accetta G, De Sario M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 2009; 179: 383–389. doi: 10.1164/rccm.200802-217OC [DOI] [PubMed] [Google Scholar]
- 39.Xiao Y, He L, Chen Y, et al. The influence of meteorological factors on tuberculosis incidence in Southwest China from 2006 to 2015. Sci Rep 2018; 8: 10053. doi: 10.1038/s41598-018-28426-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chaw L, Liew SQR, Wong J. Association between climate variables and pulmonary tuberculosis incidence in Brunei Darussalam. Sci Rep 2022; 12: 8775. doi: 10.1038/s41598-022-12796-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu Z, Hu W, Tong S. Temperature variability and childhood pneumonia: an ecological study. Environ Health 2014; 13: 51. doi: 10.1186/1476-069X-13-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Towers S, Chowell G, Hameed R, et al. Climate change and influenza: the likelihood of early and severe influenza seasons following warmer than average winters. PLoS Curr 2013; 5: ecurrents.flu.3679b56a3a5313dc7c043fb944c6f138. doi: 10.1371/currents.flu.3679b56a3a5313dc7c043fb944c6f138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liang SY, Messenger N. Infectious diseases after hydrologic disasters. Emerg Med Clin North Am 2018; 36: 835–851. doi: 10.1016/j.emc.2018.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bircher AJ, Hofmeier KS, Link S, et al. Food allergy to the carbohydrate galactose-alpha-1,3-galactose (alpha-gal): four case reports and a review. Eur J Dermatol 2017; 27: 3–9. 10.1684/ejd.2016.2908. [DOI] [PubMed] [Google Scholar]
- 45.Melén E, Koppelman GH, Vicedo-Cabrera AM, et al. Allergies to food and airborne allergens in children and adolescents: role of epigenetics in a changing environment. Lancet Child Adolesc Health 2022; 6: 810–819. doi: 10.1016/S2352-4642(22)00215-2 [DOI] [PubMed] [Google Scholar]
- 46.Porsbjerg C, Melén E, Lehtimäki L, et al. Asthma. Lancet 2023; 401: 858–873. doi: 10.1016/S0140-6736(22)02125-0 [DOI] [PubMed] [Google Scholar]
- 47.Chersich MF, Pham MD, Areal A, et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: systematic review and meta-analysis. BMJ 2020; 371: m3811. doi: 10.1136/bmj.m3811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lundberg B, Gruzieva O, Eneroth K, et al. Air pollution exposure impairs lung function in infants. Acta Paediatr 2022; 111: 1788–1794. doi: 10.1111/apa.16412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Agustí A, Melén E, DeMeo DL, et al. Pathogenesis of chronic obstructive pulmonary disease: understanding the contributions of gene-environment interactions across the lifespan. Lancet Respir Med 2022; 10: 512–524. doi: 10.1016/S2213-2600(21)00555-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang G, Hallberg J, Um Bergström P, et al. Assessment of chronic bronchitis and risk factors in young adults: results from BAMSE. Eur Respir J 2021; 57: 2002120. doi: 10.1183/13993003.02120-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.The Health Effects Institute (HEI) . State of Global Air 2020. Special Report. Boston, Health Effects Institute, 2020. www.stateofglobalair.org/ [Google Scholar]
- 52.European Environment Agency (EEA) . Air Quality in Europe – 2020 Report. Luxembourg, Publications Office of the European Union, 2020. https://data.europa.eu/doi/10.2800/786656 [Google Scholar]
- 53.Chen K, Wolf K, Breitner S, et al. Two-way effect modifications of air pollution and air temperature on total natural and cardiovascular mortality in eight European urban areas. Environ Int 2018; 116: 186–196. doi: 10.1016/j.envint.2018.04.021 [DOI] [PubMed] [Google Scholar]
- 54.Stafoggia M, Schwartz J, Forastiere F, et al. Does temperature modify the association between air pollution and mortality? A multicity case-crossover analysis in Italy. Am J Epidemiol 2008; 167: 1476–1485. doi: 10.1093/aje/kwn074 [DOI] [PubMed] [Google Scholar]
- 55.Chen G, Guo Y, Yue X, et al. Mortality risk attributable to wildfire-related PM2.5 pollution: a global time series study in 749 locations. Lancet Planet Health 2021; 5: e579–e587. doi: 10.1016/S2542-5196(21)00200-X [DOI] [PubMed] [Google Scholar]
- 56.Burke M, Driscoll A, Heft-Neal S, et al. The changing risk and burden of wildfire in the United States. Proc Natl Acad Sci USA 2021; 118: e2011048118. doi: 10.1073/pnas.2011048118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Achakulwisut P, Anenberg SC, Neumann JE, et al. Effects of increasing aridity on ambient dust and public health in the U.S. southwest under climate change. Geohealth 2019; 3: 127–144. doi: 10.1029/2019GH000187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schultz ES, Litonjua AA, Melén E. Effects of long-term exposure to traffic-related air pollution on lung function in children. Curr Allergy Asthma Rep 2017; 17: 41. doi: 10.1007/s11882-017-0709-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Frumkin H, Bratman GN, Breslow SJ, et al. Nature contact and human health: a research agenda. Environ Health Perspect 2017; 125: 075001. doi: 10.1289/EHP1663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kondo MC, Fluehr JM, McKeon T, et al. Urban green space and its impact on human health. Int J Environ Res Public Health 2018; 15: 445. doi: 10.3390/ijerph15030445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zimmermann E, Bracalenti L, Piacentini R, et al. Urban flood risk reduction by increasing green areas for adaptation to climate change. Procedia Engineering 2016; 161: 2241–2246. doi: 10.1016/j.proeng.2016.08.822 [DOI] [Google Scholar]
- 62.Wu B, Guo X, Liang M, et al. Association of individual green space exposure with the incidence of asthma and allergic rhinitis: a systematic review and meta-analysis. Environ Sci Pollut Res Int 2022; 29: 88461–88487. doi: 10.1007/s11356-022-23718-x [DOI] [PubMed] [Google Scholar]
- 63.Cariñanos P, Casares-Porcel M. Urban green zones and related pollen allergy: a review. Some guidelines for designing spaces with low allergy impact. Landsc Urban Plan 2011; 101: 205–214. doi: 10.1016/j.landurbplan.2011.03.006 [DOI] [Google Scholar]
- 64.Ivers R, Astell-Burt T. Nature Rx: Nature prescribing in general practice. Aust J Gen Pract 2023; 52: 183–186. doi: 10.31128/AJGP-01-23-6671 [DOI] [PubMed] [Google Scholar]
- 65.Islam SN, Winkel J. Climate Change and Social Inequality. UN Department of Economic and Social Affairs (DESA) Working Papers, No. 152. New York, United Nations, 2017. https://digitallibrary.un.org/record/3859027?ln=en [Google Scholar]
- 66.Friel S. Climate change, society, and health inequities. Med J Aust 2022; 217: 466–468. doi: 10.5694/mja2.51731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Atwoli L, Baqui AH, Benfield T, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. BMJ 2021; 374: n1734. doi: 10.1136/bmj.n1734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Whitmee S, Haines A, Beyrer C, et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation–Lancet Commission on planetary health. Lancet 2015; 386: 1973–2028. doi: 10.1016/S0140-6736(15)60901-1 [DOI] [PubMed] [Google Scholar]
- 69.Scovronick N, Budolfson M, Dennig F, et al. The impact of human health co-benefits on evaluations of global climate policy. Nat Commun 2019; 10: 2095. doi: 10.1038/s41467-019-09499-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Haines A. Health co-benefits of climate action. Lancet Planet Health 2017; 1: e4–e5. doi: 10.1016/S2542-5196(17)30003-7 [DOI] [PubMed] [Google Scholar]
- 71.WONCA Working Party on the Environment, the Planetary Health Alliance, the Clinicians for Planetary Health Working Group . Declaration Calling for Family Doctors of the World to Act on Planetary Health. World Organization of Family Doctors (WONCA), 2019. https://www.wonca.net/site/DefaultSite/filesystem/documents/Groups/Environment/2019%20Planetary%20health.pdf [Google Scholar]
- 72.Ten Have P, van Hal P, Wichers I, et al. Turning green: the impact of changing to more eco-friendly respiratory healthcare – a carbon and cost analysis of Dutch prescription data. BMJ Open 2022; 12: e055546. doi: 10.1136/bmjopen-2021-055546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Janson C, Maslova E, Wilkinson A, et al. The carbon footprint of respiratory treatments in Europe and Canada: an observational study from the CARBON programme. Eur Respir J 2022; 60: 2102760. doi: 10.1183/13993003.02760-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Melén E, Nwaru BI, Wiklund F, et al. Short-acting β2-agonist use and asthma exacerbations in Swedish children: a SABINA Junior study. Pediatr Allergy Immunol 2022; 33: e13885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nwaru BI, Ekström M, Hasvold P, et al. Overuse of short-acting β2-agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. Eur Respir J 2020; 55: 1901872. doi: 10.1183/13993003.01872-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Andersen ZJ, Hoffmann B, Morawska L, et al. Air pollution and COVID-19: clearing the air and charting a post-pandemic course: a joint workshop report of ERS, ISEE, HEI and WHO. Eur Respir J 2021; 58: 2101063. doi: 10.1183/13993003.01063-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]