Abstract
PURPOSE
During the COVID-19 pandemic, telemedicine emerged as an important tool in primary care. Technology and policy-related challenges, however, revealed barriers to adoption and implementation. This report describes the findings from weekly and monthly surveys of primary care clinicians regarding telemedicine during the first 2 years of the pandemic.
METHODS
From March 2020 to March 2022, we conducted electronic surveys using convenience samples obtained through social networking and crowdsourcing. Unique tokens were used to confidentially track respondents over time. A multidisciplinary team conducted quantitative and qualitative analyses to identify key concepts and trends.
RESULTS
A total of 36 surveys resulted in an average of 937 respondents per survey, representing clinicians from all 50 states and multiple specialties. Initial responses indicated general difficulties in implementing telemedicine due to poor infrastructure and reimbursement mechanisms. Over time, attitudes toward telemedicine improved and respondents considered video and telephone-based care important tools for their practice, though not a replacement for in-person care.
CONCLUSIONS
The implementation of telemedicine during COVID-19 identified barriers and opportunities for technology adoption and highlighted steps that could support primary care clinics’ ability to learn, adapt, and implement technology.
Key words: COVID-19, health policy, primary health care, telemedicine
INTRODUCTION
Innovation requires not only the development of new tools but also effective implementation. Within primary care, inadequate payment and resources can be barriers to implementation of innovative strategies,1 including electronic or digital ones.2 New technology often requires training and involves a learning curve for both clinicians and patients. Primary care practices often lack the time and other resources needed to investigate, adapt, learn, and implement new technology.3,4 As a result, innovations can be difficult to implement and slow to catch on.5
Primary care, fundamentally informed by the patient-clinician relationship, is the most common access point to health care for patients. Primary care is responsible for over 50% of all ambulatory medical visits each year,6 but receives less than 7% of national health expenditures,7,8 none of which is earmarked for the implementation of new technologies.
At the beginning of the COVID-19 pandemic, telemedicine was lauded as a key to reaching patients in a way that was cost-effective, convenient, and safe.9-12 Its use increased dramatically during the early months of the pandemic,13,14 but health care policy and payment models struggled to respond quickly enough to accommodate the new demand. Technical issues further complicated telemedicine implementation for many practices and patients. These facts are known, but unknown are the basic lessons learned from this experience that can inform post-pandemic primary care delivery and financing.
Few data exist that track the evolution of telemedicine use and primary care clinicians’ point of view during the pandemic. We sought to examine and describe the rapid adoption of video-based and telephone-based care in primary care settings through surveys distributed from 2020 to 2022 to primary care clinicians across the United States. With these data, our goal was to understand the status of adoption, barriers to adoption, and benefits of adoption to primary care clinicians and practices. Such an understanding may provide insights for policy and the financing of primary care going forward.
METHODS
Study Design
Initially weekly and then monthly from March 13, 2020 to March 1, 2022, 36 electronic surveys (called Quick COVID-19 Surveys) were opened on Fridays at 9:00 AM EST and closed Mondays at 11:59 PM PST. Each survey included 4 key components: core questions, a new topical (flash) question, basic respondent demographics, and an option for open-ended comments. The core questions rotated among common topical domains of COVID-related practice strain, such as access to materials, staffing or payment issues, social drivers of health, and digital health. These core topical domains remained largely stable from survey to survey, with some minor variations in how they were asked to be responsive to the changing care delivery environment.
Each survey’s flash question addressed events relevant to care delivery at the current stage of the pandemic. Examples of flash question topics included: the impact of structural racism on health after the murder of George Floyd and the availability and receipt of Paycheck Protection Program loans to primary care clinicians.
All questions were vetted by the National Advisory Committee established for the survey. The National Advisory Committee included subject matter experts from family medicine, internal medicine, public health, social science, and pediatrics; patients; and policymakers.
Sampling Frame and Partners
We used a convenience sample gained through social networking and crowdsourcing, creating cross-sectional samples at each survey period. Survey invitations were distributed through the Larry A. Green Center; collaborators such as the Primary Care Collaborative; and partnerships with professional societies and organizations, listservs, and practice-based research networks—a group of over 150 partners. Each survey offered participants the option to sign up for an automated mailing to receive the next new link directly.
All links sent directly to survey participants contained a unique token. In addition, each respondent generated a unique token when answering a survey. In this way, we could maintain anonymity within our data set and connect individual responses to unique respondents. The tokens allowed us to track the same (anonymous) respondent over time, thus identifying a longitudinal cohort among subscribers.
We collected e-mail addresses for subscribers and internet protocol addresses for all participants in a platform separate from the survey to maintain confidentiality. Internet protocol addresses were combined with zip codes and used to determine the extent to which respondents represented unique care delivery settings. The generated tokens prevented the same person from answering the survey more than once. No survey resulted in less than 90% unique settings for respondents; most surveys were confirmed as greater than 92% unique respondents.
Data Analysis
Each morning after the survey closed, we downloaded the responses. A multidisciplinary team of 4 people—an anthropologist and professor of family medicine, a family nurse practitioner, a health policy statistician, and a health services analyst with expertise in finance and primary care—analyzed the data on an iterative, ongoing basis. We conducted quantitative analyses and qualitative analyses separately and then together during regular analysis meetings. We shared preliminary summary results with the National Advisory Committee before completion, giving them an opportunity to comment on results and implications.
Open text comments were coded using a grounded approach, as described in Glaser,15 and key themes within the data were identified. There was opportunity for open text comments in every survey and it was used by 40% to 50% of respondents. Some surveys included questions that required open text comments. In those cases, open text comments were received by all survey respondents. Comments were coded by the team of 4 and then grouped analytically to identify key themes. Example quotations that represented themes (appearing in a minimum of 15% of comments) were identified and added to the executive summary.
While we do not report the results of the qualitative analyses here, we used the qualitative comments to inform changes to questions, to suggest new questions for future surveys, or to challenge any bias that might have been unnoticed in previous survey wording. No longitudinal analysis was performed.
RESULTS
General Characteristics
The number of survey respondents ranged from 538 (first survey) to 3,131, with an average of 937 respondents per survey and all 50 states and the District of Columbia were represented, with frequent response from a few in US territories (Figure 1a). The majority of respondents (60% to 75%) self-identified as family medicine clinicians (Figure 1b). Specialties included family medicine, pediatrics, internal medicine, geriatrics, pharmacy, psychology, and a handful of others. Both rural and urban areas were represented, as were both large and small practices (Figure 1c). Between one-fifth and one-third of responding practices indicated that more than one-half of their patients were covered by Medicare or Medicaid (Figure 1d).
Figure 1a.
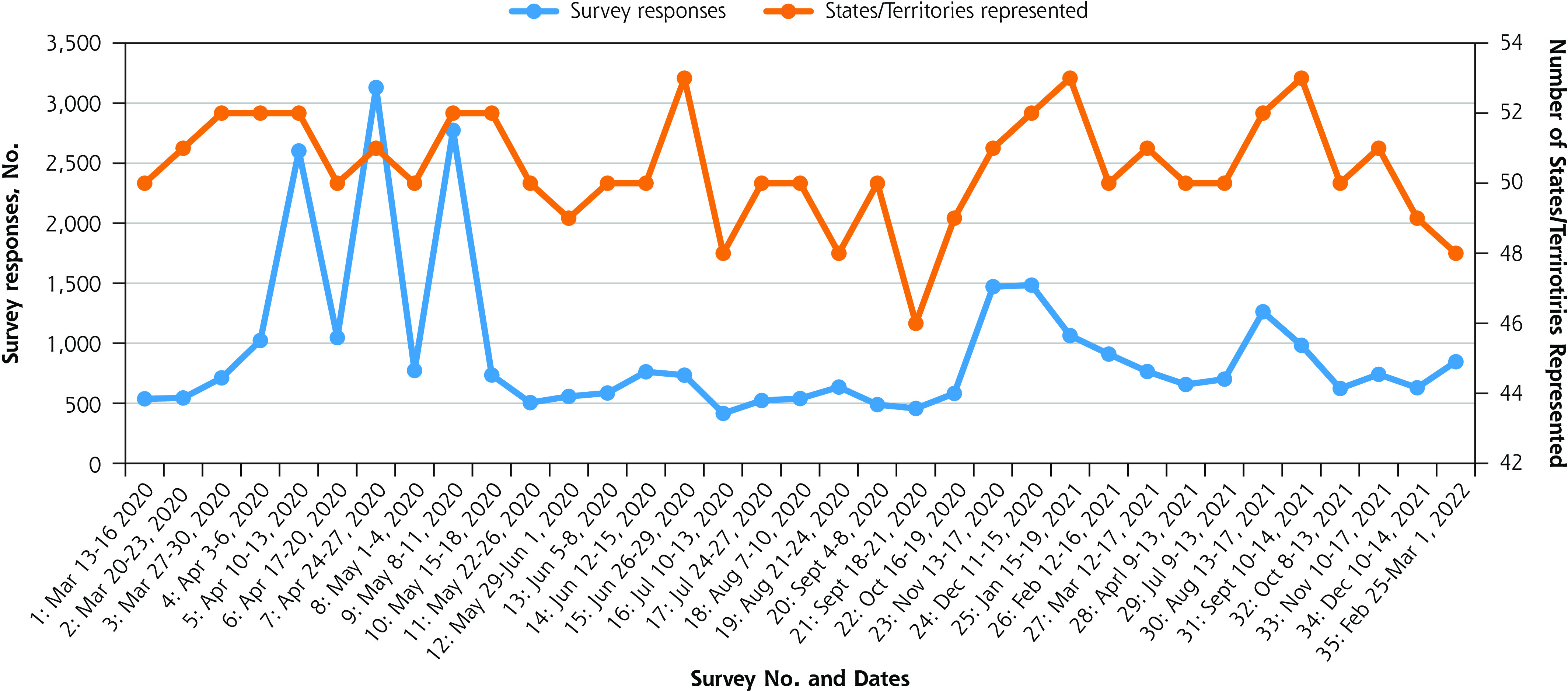
Number of respondents and geographic areas represented.
Figure 1b.
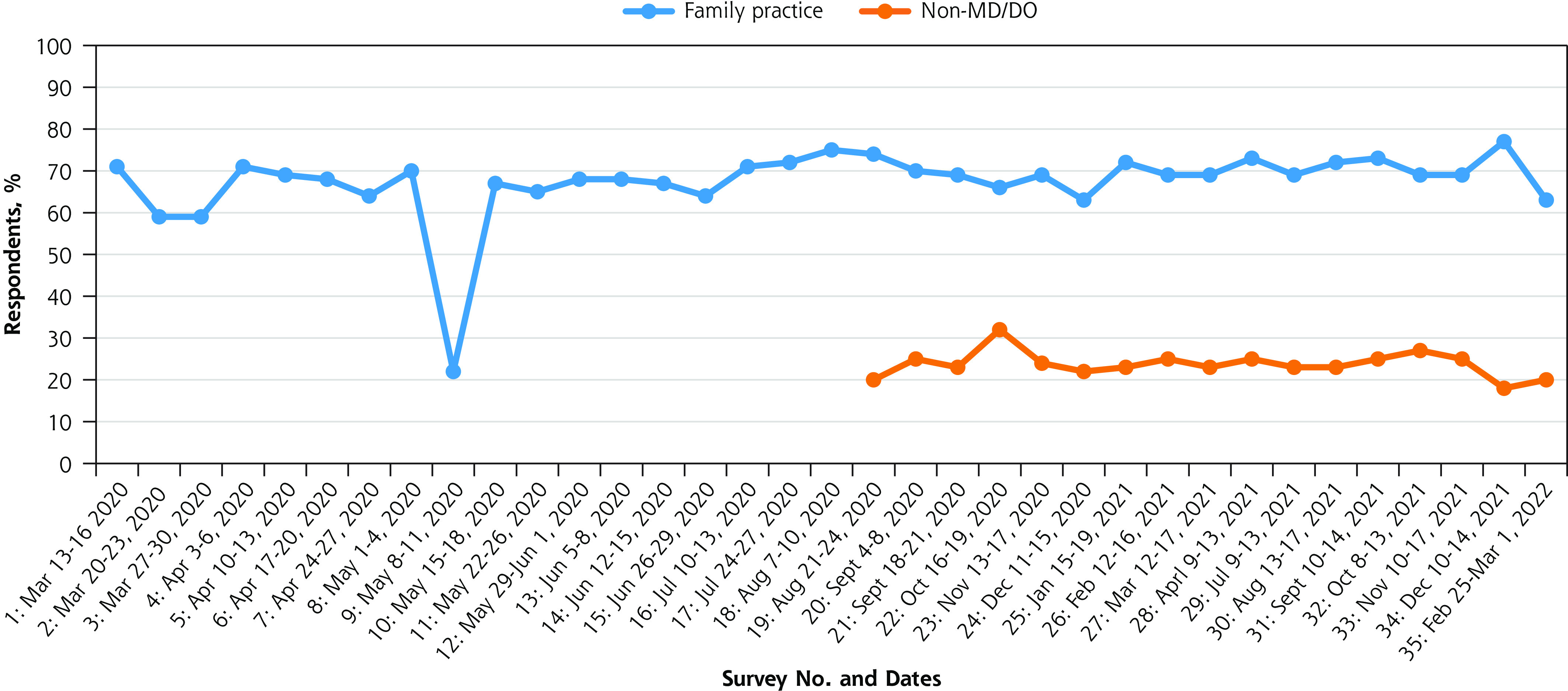
Clinician type of respondents.
DO = doctor of osteopathy; MD = medical doctor.
Note: The survey from May 8-11, 2020 was heavily promoted within internal medicine, resulting in an oversample of that specialty, thus the unusually low percentage of family medicine. The study design allowed for any clinician in primary care to participate. Information regarding type of certification was not initially tracked. Tracking started in August 2020.
Figure 1c.
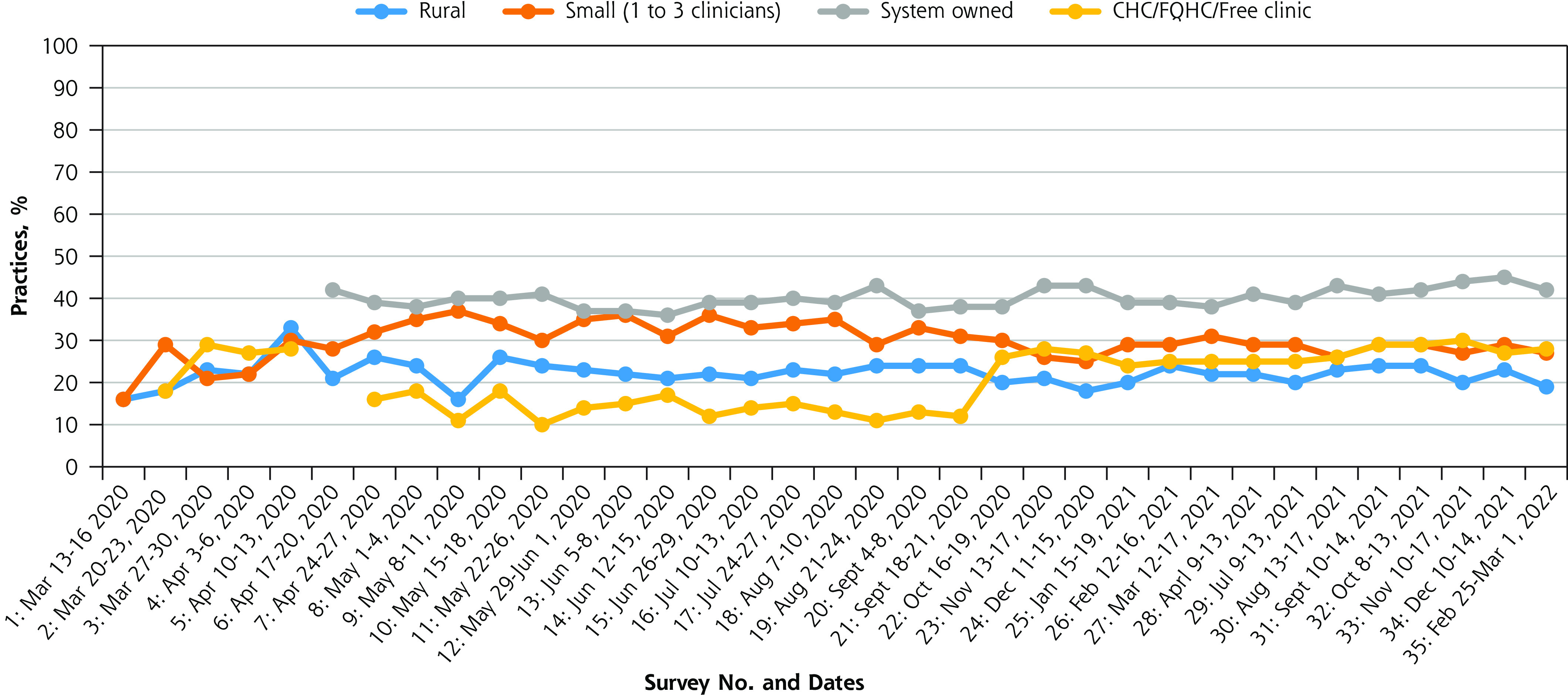
Rurality and practice size of respondents.
CHC = community health center; FQHC = federally qualified health center.
Figure 1d.
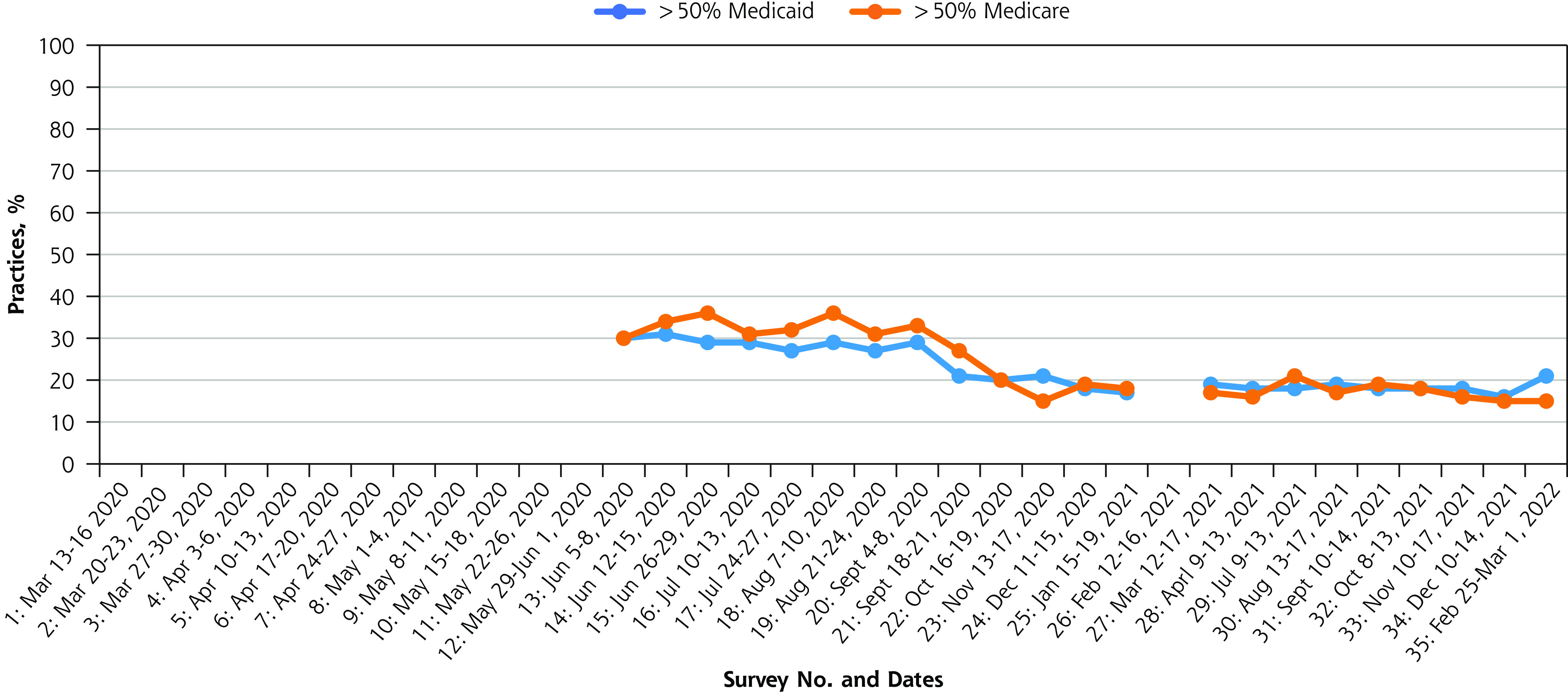
Medicare and medicaid representation of clinics.
Telemedicine
In this report, the term telemedicine refers to video-based and telephone-based care delivery. Early in the pandemic, use of telemedicine was limited within primary care but increased quickly. In March 2020, 41% of respondents indicated that their practice had no video-based visits, but by May 2020 that percentage was 13% (Figure 2a). Over that same period, the percentage of clinicians who indicated that video visits comprised more than one-half of all visits jumped from 22% to as high as 40%, before declining to 27% (Figure 2a).
Figure 2a.
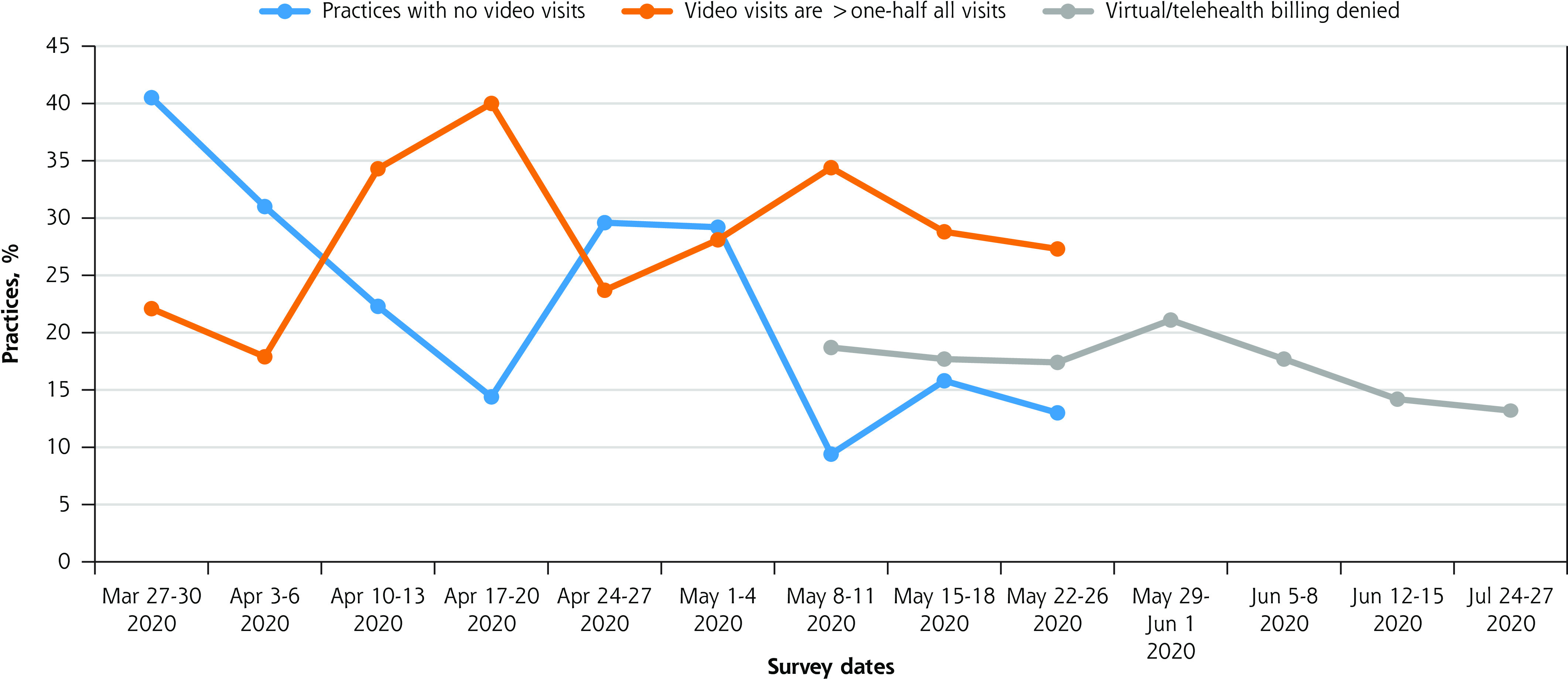
Early telemedicine usage patterns.
Note: Not all survey dates during the period are included.
The infrastructure necessary to conduct telemedicine was sometimes lacking but generally increased over time. Data from May 8 through May 11, 2020, indicates that 32% of respondents obtained equipment and 50% to 51% acquired technical knowledge or training to conduct telemedicine visits specifically in response to pandemic care delivery needs (Table 1). Respondents from a practice owned by a hospital or health system more often reported that they obtained equipment (40%) and technical knowledge (55%) compared with others. Of those who self-identified as independent but part of a larger group, 31% obtained equipment and 49% gained technical knowledge. For those who were fully self-owned, 25% obtained equipment and 47% gained technical knowledge.
Table 1.
Telemedicine Infrastructure Barriers
| In order to conduct virtual health visits, do you have… | May 8-11, 2020, % |
|---|---|
| Broadband Internet access | |
| Yes, since before COVID-19 | 79 |
| Yes, as a result of COVID-19 | 13 |
| I’m working on it | 4 |
| No | 4 |
| Equipment best suited for the need | |
| Yes, since before COVID-19 | 44 |
| Yes, as a result of COVID-19 | 32 |
| I’m working on it | 17 |
| No | 7 |
| Technical knowledge to use virtual platforms | |
| Yes, since before COVID-19 | 27 |
| Yes, as a result of COVID-19 | 50 |
| I’m working on it | 19 |
| No | 5 |
| Training to conduct virtual health w/ confidence | |
| Yes, since before COVID-19 | 17 |
| Yes, as a result of COVID-19 | 51 |
| I’m working on it | 25 |
| No | 7 |
| Virtual health payment parity with in-person visits | |
| Yes, since before COVID-19 | 5 |
| Yes, as a result of COVID-19 | 38 |
| I’m working on it | 31 |
| No | 26 |
Eventually, the use of telemedicine began to decline as use of in-office visits returned. In October 2020 and January 2021, 38% to 45% of respondents said they used video-based care and 35% said they used telephone-based care for at least 1 in 5 patients. By November 2021, however, only 20% said they used video-based care for at least 1 in 5 patients. These percentages were similar across practice size and ownership status.
In addition to changing patterns of use, opinions regarding the usefulness and effectiveness of telemedicine evolved over time. Initially, telemedicine caused frustration, but it eventually came to be seen as an important tool for many primary care clinicians. Unfortunately, lack of certainty related to payment, and persistently low or denied payments for telemedicine prevented many from being able to take full advantage of its newfound usefulness. From April to May 2020, 65% to 84% said a source of stress was their patients’ struggle with virtual health.
From May to August 2020, between 14% and 21% of respondents reported they had virtual/telehealth insurance billing that had been denied (Figure 2a). Despite these obstacles, from October 2020 to November 2021, over 60% of respondents, on average, agreed with the several positive statements about telemedicine (Figure 2b). A year later, in October of 2022, most respondents (54%) indicated that “video- and phone-based care have become essential to maintaining our practice capacity.”
Figure 2b.
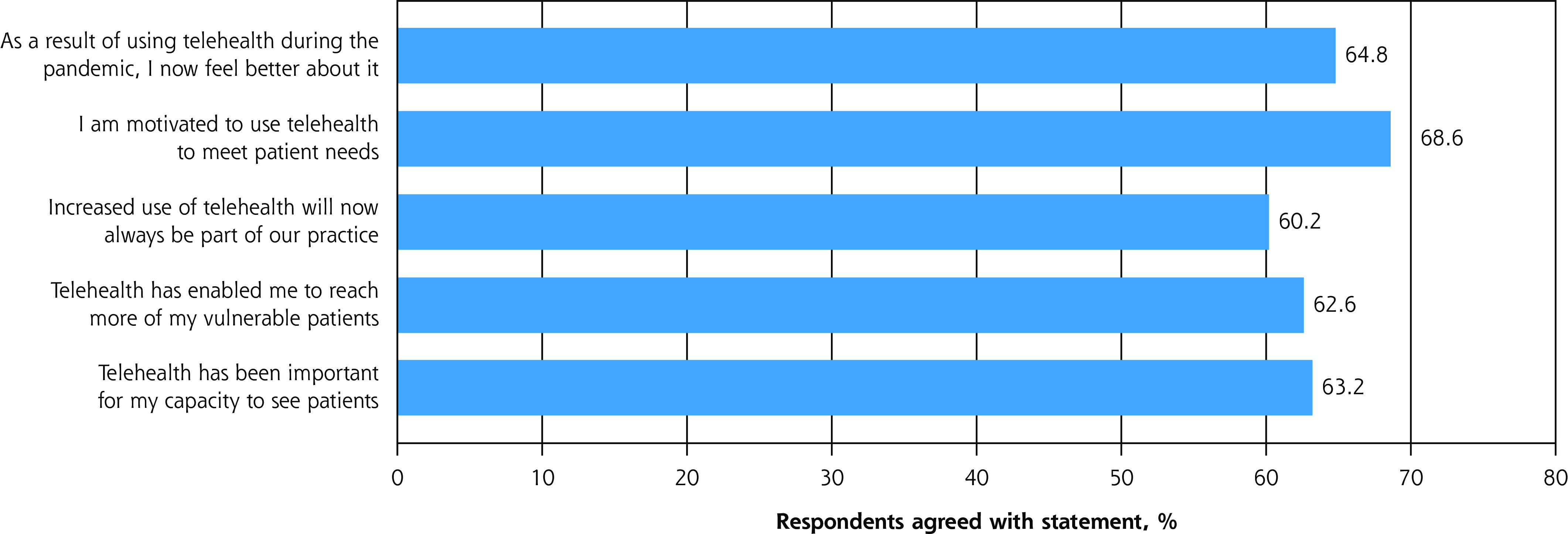
Later feelings towards telemedicine.
NOTE: Values represent mean results across 1 to 3 surveys between October 2020 and November 2021.
When asked about their experience with telemedicine, respondents from February 12 through February 16, 2021, indicated it had been helpful for improving access to patients in general and especially for reaching vulnerable patients, while also increasing capacity to see patients (Table 2). Additionally, more than 90% of respondents indicated it was well suited for behavioral health counseling, mental health counseling, monitoring a stable chronic condition, and also suited for other visit types (Table 2).
Table 2.
Benefits of Telemedicine
| OVER THE LAST 4 WEEKS, what has been your experience with telehealth (video- or telephone-based care)? It has been helpful for… | Feb 12-16, 2021, % |
|---|---|
| Improving access in general | 80 |
| Reaching my vulnerable patients | 72 |
| My capacity to see patients | 64 |
| How well suited is telehealth for each of the following types of primary care visits? | Well suited, % |
| Behavioral health counseling | 95 |
| Mental health counseling | 94 |
| Stable chronic condition monitoring | 93 |
| Adult preventative medicine | 73 |
| Acute illness | 69 |
| Development assessment | 59 |
DISCUSSION
The results presented here provide insight into clinicians’ evolving experiences with telemedicine during the COVID-19 pandemic. While these results are specific to telemedicine during this time frame and limited to the context of the fielded surveys, they reflect the realities of current regulatory and reimbursement policies for primary care. Findings show how some of the changes forced by the pandemic came to be valued, despite limited recognition and support of the frontline needs of primary care practice. The COVID-19 pandemic necessitated the implementation of several types of innovative technologies to meet patient needs while maintaining safety. The patterns of adoption and use of video- and telephone-based care during this time allow us to observe barriers associated with the adoption of technology and to learn lessons specific to primary care delivery and payment.
A notable aspect of telemedicine is that it was a technology available long before the pandemic.16 Its ability to address physician shortages and improve patient access and convenience were previously identified,17-19 but with only moderate adoption rates. Prior reservations about the practicality or usefulness of telemedicine were set aside as the options for in-person visits became more cumbersome during the pandemic (moving outdoors to parking lots, etc). During the initial months of the pandemic, clinicians and patients struggled with navigating technical literacy and practical limitations in technical capabilities.20,21 Lags in policy and difficulties in billing procedures resulted in delays or denials of payment for many clinicians and practices.21 Telemedicine was faulted by some as inadequate and a poor substitute for in-person visits. Over time, however, its value became apparent—not as a new form of care, but as an instrument able to support care delivery and enhance practice capacity. As a tool, telemedicine is useful for certain situations and under specific circumstances. However, it is seen by primary care practitioners not as an alternative line of service delivery, but as a complement to in-person care when physical exams, procedures, or close interpersonal interaction are not required. During the pandemic, 24 months of use under pressure allowed clinicians to learn how to effectively wield this tool. By the end of our study period, most clinicians saw telemedicine as critical to their practice’s future success.
Unfortunately, lack of adoption before the pandemic and lack of policy and infrastructure to facilitate rapid adoption created unnecessary weaknesses within primary care in the face of a public health emergency. Clinicians and practices were forced to grapple with issues of payment, technical components, training, and workflow redesign, while also determining how best to implement telemedicine with patients and maintain high quality standards. Moving forward, time and resources should be allocated for clinicians and practices to learn new technology before they are required to implement it.
Studying our collective experience during the COVID-19 pandemic offers us a unique opportunity to plan for the future. After any crisis or disaster, one of the key components to recovery is to conduct a gap analysis to inform future needs.3,22 Public health emergencies will happen. We can learn from this one through analyses that identify ways we were unnecessarily vulnerable before the pandemic. And by asking, what vulnerabilities existed and contributed to avoidable burden and harm, and how might we prevent that avoidable suffering in the future?
We know that global travel and movement will expose us to future pandemics. When faced with our next pandemic or crisis where technologic innovations could be rapidly deployed and implemented, there are several policy changes that, if implemented, could reduce some health burdens and harms. For example, creation of a new billing code for “new technology used during a crisis” could be activated and used until permanent codes specific to a given crisis or emergency could be developed. During the COVID-19 pandemic, such a code would have accelerated appropriate resources being shared with practices and would have prevented unnecessary harm and confusion created by constantly changing billing codes.
A second possibility would be to create payment models that are not dependent on face-to-face clinical encounters alone and that do not define covered services based on modality of care delivery. Crisis care delivery will almost always cause interruption to usual workflows. The pandemic demonstrated the unnecessary weakness of structuring policy around the mode of care delivery, rather than the care delivered. To adequately support primary care, a long-term solution is needed. We believe such a plan is feasible and possible in our current funding environment if partnered with an appropriate transition plan. Planned for accordingly, specific workflow changes and documentation changes could be designed to meet the challenges associated with emergency and disaster scenarios. This would allow innovations to be more easily adopted and incorporated during and after a crisis. Additionally, as the payment failures and interruptions of the COVID-19 pandemic have taught us, policy that allows payers to influence when and how telemedicine is used by linking payment to specific care modalities is inappropriate, especially during a public health crisis. Clinicians are medical professionals, trusted with stewarding the health of the population, and can be trusted to determine on their own when use of telemedicine is appropriate for their patients. Central support for frontline innovation is more likely to be successful than command and control top-down solutions.
Another key lesson from the pandemic pattern of telemedicine adoption is that if clinicians had the opportunity to become familiar with the technical requirements and practical implementation of telemedicine beforehand, it would have been easier for practices and patients to incorporate during the crisis. Although no formal comparisons were made, it appears that available resources differ by practice size and ownership; we observed some differences in the percent who acquired equipment and training for telemedicine by ownership. A flexible payment mechanism that allows for adaptation during an emergency would mitigate some of the issues faced by practices and patients and potentially level the playing field when it comes to the ability to invest in the needed technology and training. Limitations of fee-for-service (FFS) payment models are highlighted by our results: the current FFS structure focuses on face-to-face transactions as opposed to the process of, access to, or quality of care. Practices and clinicians are too vulnerable to the periodic decision making of payers. The National Academies of Sciences, Engineering, and Medicine have identified primary care as a common good23 and have suggested that practices require a system of support for transitions. An example of such support would be the Primary Care Extension Service, established as a federal mandate in the Patient Protection and Affordable Care Act, but never funded. There currently exists a skeleton of the intended Primary Care Extension Service, created through the interests of individual states, researcher-led grant projects, and a few forward-thinking philanthropies. A simple solution would be for the federal government to claim ownership of this starter scaffolding, fund it, and grow it into the national infrastructural support as intended.
The strengths of this study include the large number of respondents across the United States from a variety of geographic areas and clinical specialties. Additionally, the large number of surveys were consistently conducted over 2 years and included the consistent and longitudinal participation of many clinicians. The results, however, should be viewed in light of the study’s limitations. First, while within all surveys there were individuals who consistently responded, each survey had a unique cohort of respondents, so caution should be used when interpreting any trends. Second, survey questions were changed with each survey without sufficient time to cognitively test them. It is therefore possible that respondents could have misinterpreted or misunderstood a question when answering. The combined use of qualitative comments with structured questions was one of the ways we attempted to mediate this limitation. Additionally, while the survey captured clinicians’ current experiences, certain results elicit questions that cannot be answered with the available data. For example, we observed an increase in the use of video visits early in the series of surveys followed by a decline in video visits. While this pattern may reflect the timing of shelter in place policies (and the easing of those policies), we cannot say for sure what this pattern reflects as our surveys did not attempt to identify the causes of certain observed patterns. As another example, while respondents reported the percent who obtained equipment and acquired technical knowledge or training for telemedicine, it was beyond the scope of the survey to ascertain the type or nature of the training. Recognizing these limitations, it remains true that this is the only data set to capture the natural evolution of primary care capacity and response during the pandemic. A key component not captured by these data are the patient experience of telemedicine during the same time period. While critical to assessing access to care and the potential for widening of health disparities related to technology access and literacy, the current data focused only on the clinicians’ experiences. Future studies should examine patient experiences of telemedicine during the COVID-19 pandemic.
Our study results illustrate current shortcomings in the type and level of support for primary care when it comes to the adoption and implementation of technology in practice. Steps are needed to address these shortcomings given the critical role primary care plays in ensuring the health and wellness of our communities. Additionally, examination of patient experiences would allow for more context when designing and implementing future policies related to telemedicine.
Footnotes
Conflicts of interest: C.A.S receives consulting fees from the American Board of Family Medicine. All other authors report none.
Funding support: The data collected and analyzed for this study were funded by a grant by Agency for Healthcare Research and Quality (1R01HS028253-1), the Corey and Andrew Morris-Singer Foundation, the Samueli Foundation, the University Suburban Health Center Foundation, and the American Board of Family Medicine Foundation.
REFERENCES
- 1.Seckler E, Regauer V, Rotter T, Bauer P, Müller M.. Barriers to and facilitators of the implementation of multi-disciplinary care pathways in primary care: a systematic review. BMC Fam Pract. 2020; 21(1): 113. 10.1186/s12875-020-01179-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baines R, Tredinnick-Rowe J, Jones R, Chatterjee A.. Barriers and enablers in implementing electronic consultations in primary care: scoping review. J Med Internet Res. 2020; 22(11): e19375. 10.2196/19375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Willis VC, Thomas Craig KJ, Jabbarpour Y, et al. Digital health interventions to enhance prevention in primary care: scoping review. JMIR Med Inform. 2022; 10(1): e33518. 10.2196/33518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, Shelley DR.. Rapid transition to telehealth and the digital divide: Implications for primary care access and equity in a post-COVID era. Milbank Q. 2021; 99(2): 340-368. 10.1111/1468-0009.12509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bodenheimer T, Becerra I, Kong M.. Primary care clinician attitudes about the telehealth revolution. Family Medicine Case Notes from the COVID-19 Frontlines. Published May 4, 2020. Accessed May 22, 2020. https://medium.com/case-notes-from-the-covid-19-front-lines/primary-care-clinician-attitudes-about-the-telehealth-revolution-fe405cd0434b
- 6.National Center for Health Statistics . National Ambulatory Medical Care Survey: 2016 National Summary Tables. Accessed Jun 28, 2022. https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_web_tables.pdf
- 7.Baillieu R, Kidd M, Phillips R, et al. The Primary Care Spend Model: a systems approach to measuring investment in primary care. BMJ Glob Health. 2019; 4(4): e001601. 10.1136/bmjgh-2019-001601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reid R, Damberg C, Friedberg MW.. Primary care spending in the fee-for-service medicare population. JAMA Intern Med. 2019; 179(7): 977-980. 10.1001/jamainternmed.2018.8747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N.. COVID-19 and telemedicine: immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020; 126: 104345. 10.1016/j.jcv.2020.104345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwamm LH, Erskine A, Licurse A.. A digital embrace to blunt the curve of COVID19 pandemic. NPJ Digit Med. 2020; 3: 64. 10.1038/s41746-020-0279-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020; 26(5): 309-313. 10.1177/1357633x20916567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ohannessian R, Duong TA, Odone A.. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020; 6(2): e18810. 10.2196/18810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mann DM, Chen J, Chunara R, Testa PA, Nov O.. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020; 27(7): 1132-1135. 10.1093/jamia/ocaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF.. Implementation and usefulness of telemedicine during the COVID-19 Pandemic: a scoping review. J Prim Care Community Health. 2020; 11: 2150132720980612. 10.1177/2150132720980612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glaser BG. The Grounded Theory Perspective II: Description’s Remodeling of Grounded Theory Methodology. Sociology Press; 2003. [Google Scholar]
- 16.Dunn EV, Conrath DW, Bloor WG, Tranquada B.. An evaluation of four telemedicine systems for primary care. Health Serv Res. 1977; 12(1): 19-29. [PMC free article] [PubMed] [Google Scholar]
- 17.Bashshur RL, Howell JD, Krupinski EA, Harms KM, Bashshur N, Doarn CR.. The empirical foundations of telemedicine interventions in primary care. Telemed J E Health. 2016; 22(5): 342-375. 10.1089/tmj.2016.0045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL.. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017; 15(3): 225-229. 10.1370/afm.2095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pravia CI, Diaz YM.. Primary care: practice meets technology. Cleve Clin J Med. 2019; 86(8): 525-528. 10.3949/ccjm.86a.18122 [DOI] [PubMed] [Google Scholar]
- 20.Breton M, Sullivan EE, Deville-Stoetzel N, et al. Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. BMC Fam Pract. 2021; 22(1): 192. 10.1186/s12875-021-01543-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garfan S, Alamoodi AH, Zaidan BB, et al. Telehealth utilization during the Covid-19 pandemic: a systematic review. Comput Biol Med. 2021; 138: 104878. 10.1016/j.compbiomed.2021.104878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughes LS, Cohen DJ, Phillips RL Jr.. Strengthening primary care to improve health outcomes in the US. JAMA Health Forum. 2022; 3(9): e222903-e222903. 10.1001/jamahealthforum.2022.2903 [DOI] [PubMed] [Google Scholar]
- 23.National Academies of Sciences, Engineering, and Medicine . Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. The National Academies Press; 2021. [PubMed] [Google Scholar]


