Abstract
PURPOSE
As the average level of medical education indebtedness rises, physicians look to programs such as Public Service Loan Forgiveness (PSLF) and National Health Service Corps (NHSC) to manage debt burden. Both represent service-dependent loan repayment programs, but the requirements and program outcomes diverge, and assessing the relative uptake of each program may help to inform health workforce policy decisions. We sought to describe variation in the composition of repayment program participant groups and measure relative impact on patient access to care.
METHODS
In this bivariate analysis, we analyzed data from 10,677 respondents to the American Board of Family Medicine’s National Graduate Survey to study differences in loan repayment program uptake as well as the unique participant demographics, scope of practice, and likelihood of practicing with a medically underserved or rural population in each program cohort.
RESULTS
The rate of PSLF uptake tripled between 2016 and 2020, from 7% to 22% of early career family physicians, while NHSC uptake remained static at 4% to 5%. Family physicians reporting NHSC assistance were more likely than those reporting PSLF assistance to come from underrepresented groups, demonstrated a broader scope of practice, and were more likely to practice in rural areas (23.3% vs 10.8%) or whole-county Health Professional Shortage Areas (12.5% vs 3.7%) and with medically underserved populations (82.2% vs 24.2%).
CONCLUSIONS
Although PSLF supports family physicians intending to work in public service, their peers who choose NHSC are much more likely to work in underserved settings. Our findings may prompt a review of the goals of service loan forgiveness programs with potential to better serve health workforce needs.
Key words: primary care workforce, student loan repayment, physician demographics, health equity, scope of practice, access to care, delivery of health care, health planning, health policy, vulnerable populations, medically underserved area, rural population
INTRODUCTION
The total debt incurred during medical education continues to increase year over year, now topping $200,000 for the average graduating medical student beginning postgraduate training.1,2 As average indebtedness rises, medical trainees, particularly those interested in lower-paying specialties, increasingly look to student loan repayment programs to facilitate their entry into the physician workforce.3-5 Previous studies indicate that high educational indebtedness may impact the choice of careers in academic medicine and public service including Federally Qualified Health Centers, rural health clinics, and the Indian Health Service.6,7
For those who seek financial assistance to repay medical education debt, federal loan forgiveness and scholarship programs include the Indian Health Service, the Health Professions Scholarship Program (serving the US Army, Navy, and Air Force), the National Health Service Corps (NHSC), and the Public Service Loan Forgiveness (PSLF) program. There are also countless smaller loan forgiveness and scholarship programs, executed at the level of states, municipalities, or health care delivery systems. Although NHSC also offers a tuition reimbursement option, we focus on the NHSC loan repayment program, which provides up to $25,000 in annual loan repayment for early career professionals working with very disadvantaged communities determined by Health Professional Shortage Area (HPSA) score.8,9 The PSLF program, established under the College Cost Reduction and Access Act of 2007, allows forgiveness of the remaining loan balance for direct loan borrowers who make 120 qualifying payments in the setting of qualified employment, and has been expanded to individuals in a wider variety of repayment plans (Temporary Expanded PSLF), and to borrowers with Federal Family Education loan or Federal Perkins loan that are consolidated into Direct loans (limited PSLF waiver).10,11
In 2021, nearly 15,000 practicing health professionals had received NHSC funding, of whom 2,500 are currently in training, and the program’s budget totals $430 million or roughly $225,000 for each scholarship recipient and up to $110,000 for each student who received loan repayment assistance.12,13 Previous economic impact analyses have suggested that NHSC support generates a greater than 2:1 return on investment in the form of economic output, and creates 3 additional support jobs for each NHSC-supported clinician.14 Recent studies suggest that only about 13% of early career physicians involved in loan forgiveness programs participate in the NHSC.15
Heavily indebted early career physicians appear to be increasingly drawn to PSLF and the possibility of unlimited forgiveness as a debt mitigation strategy. Because an estimated 68% of health system employers qualify as nonprofit for PSLF purposes, this mechanism is broadly available to medical graduates regardless of practice specialty, geographic location, or practice pattern.16 Data on recent medical school graduates suggest that the intention to pursue PSLF is 3 times more common among those students in the highest one-third of debt burden, who owe more than $246,000, of whom 48% intend to pursue PSLF.17 Of those in the lowest one-third of debt burden, who owe less than $160,000, only 16% plan to pursue PSLF.17 The intention to engage in NHSC or other federal service-based repayment, on the other hand, appears to be independent of amount owed, consistent at 2% to 3% across all groups.17 Notably, our study set out to investigate whether these reported intentions are confirmed in graduate behaviors, and to further understand the downstream relationships of these loan repayment programs with physician workforce composition, including geographic distribution and scope of practice of early career physicians.
METHODS
Data Source
We used data from the American Board of Family Medicine (ABFM) National Graduate Survey (NGS) for the years 2016-2020 to investigate the relationship between early career physicians’ loan repayment choices and workforce outcomes.18 The survey, administered on a voluntary basis to ABFM-certified physicians 3 years after residency graduation, asks about current practice location and organization, scope of services provided, and participation in loan repayment programs.18 Basic demographic data on the physician cohort were obtained from the ABFM residency matriculation database and board certification database, both of which contain data on 100% of early career physicians who have graduated from a residency program and have attempted initial family medicine board certification.
We included all respondents to the NGS for 2016-2020 in our study. Respondents to the survey numbered as follows: 2016 (2,069 physicians), 2017 (2,159 physicians), 2018 (2,255 physicians), 2019 (2,511 physicians), and 2020 (1,683 physicians), representing response rates of 66% to 74%. We matched demographic and debt data from these respondents from their responses on an initial certification examination questionnaire taken at the point of residency graduation (100% response rate). To measure scope of practice, we calculated an individual scope of practice (iSOP) score for each respondent from data available in the NGS. This score is determined by the number of clinical services provided and ranges from 0 to 30 with a higher score indicating a broader scope.19 An NGS question on loan repayment allowed respondents to choose more than 1 option, including PSLF, NHSC, Military, or Other (write-in option). We designated work with medically underserved populations based on practice type: Federally Qualified Health Center, rural health clinic, Indian Health Services location, non–federal government clinic, or prison location. Practice addresses were also geocoded to determine county-level rurality (with rural defined by a Rural-Urban Continuum Code of 4 or greater) and primary care HPSA status (whole-county or partial), and each respondent was linked with geocoded data on residency program and practice location. Using Health Resources and Services Administration data, we defined these locations as falling within a rural area and either a whole-county or partial primary care Health Professional Shortage Area.
This study was approved by the American Academy of Family Physicians Institutional Review Board.
Statistical Analysis
We computed descriptive statistics for our NGS sample using age, gender, race, ethnicity, degree type, and international graduate status, and conducted bivariate analysis by loan repayment mechanism to compare scope of practice and likelihood of working with a medically underserved population or in a rural area. We conducted bivariate analysis of practice location and population served by loan repayment mechanism used. All analyses were performed in Stata version 17.0 (StataCorp LLC).
RESULTS
Uptake of Loan Repayment Programs
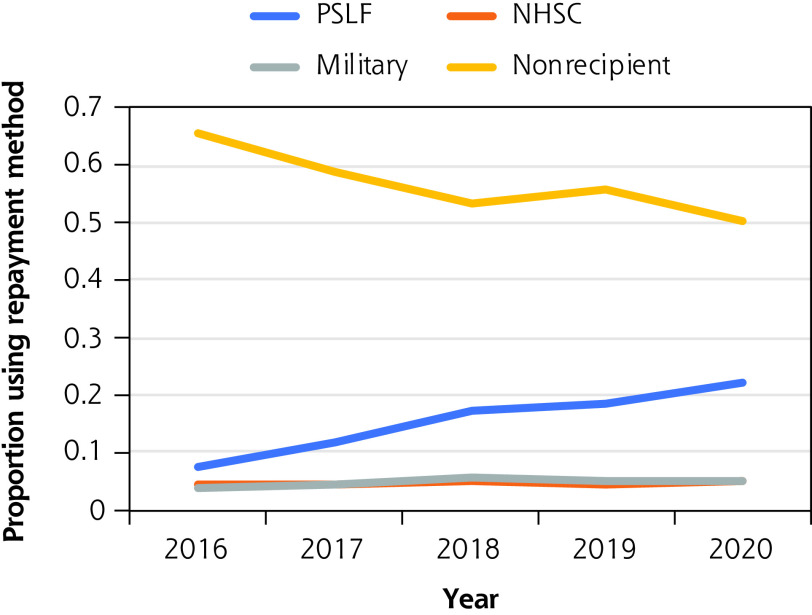
Of the 10,677 family physicians in the 2016-2020 sample, surveyed approximately 3 years into unsupervised practice, more than one-half (56%) reported using no loan repayment mechanism. About 15% reported pursuing PSLF and 10% reported a federal loan repayment mechanism other than PSLF, including NHSC. Roughly 22% of the overall sample reported they would take advantage of a hospital, state, private, or other loan repayment program. The proportion of recent family medicine residency graduates receiving NHSC repayment assistance remained consistent between 4% and 5%, but the proportion reporting engagement with PSLF tripled from 7% to 22% between 2016 and 2020 (Figure 1).
Figure 1.
Trends in the use of loan repayment programs among early career family physicians, 2016-2020.
NHSC = National Health Service Corps; PSLF = Public Service Loan Forgiveness.
Note: Data are from the American Board of Family Medicine National Graduate Survey, 2016-2020.
Program Use by Physician Demographics
Several important demographic findings distinguished NHSC recipients from their peers. The NHSC recipients were significantly more likely than average to be female (62.7% vs 56.3% of the overall population, P = .003) and less likely to be international medical graduates (12.3% vs 32.8%, P <.001) (Table 1). NHSC recipients were also less likely than the overall population to be Asian (7.7% vs 17.1%, P <.01), but more likely to be Black/African American (9.5% vs 5.6%, P <.002) or White (57.5% vs 51.9%, P = .009).
Table 1.
Demographics of Early Career Family Physicians, Overall and by Loan Repayment Program
| Demographic | Value (P Value) | |||||
|---|---|---|---|---|---|---|
| Overall (N = 10,677) | PSLF (n = 1,653) | NHSC (n = 504) | IHS (n = 32) | Military (n = 525) | Other (n = 2,360) | |
| Age, mean, y | 35.8 | 35.2 (<.001) | 35.8 (.88) | 36.4 (.40) | 36.0 (.37) | 35.3 (<.001) |
| Gender, % | ||||||
| Female | 56.3 | 57.4 (.34) | 62.7 (.003) | 78.2 (.01) | 35.1 (<.001) | 55.3 (.30) |
| Male | 43.7 | 42.7 | 37.3 | 21.9 | 65.0 | 44.7 |
| Medical degree, % | ||||||
| MD | 81.8 | 71.0 (<.001) | 80.8 (.55) | 96.9 (.03) | 61.3 (<.001) | 82.2 (.49) |
| DO | 18.2 | 29.0 | 19.3 | 3.1 | 38.7 | 17.8 |
| International medical graduate, % | ||||||
| Yes | 32.8 | 18.1 (<.001) | 12.3 (<.001) | 0 (<.002) | 4.4 (<.001) | 29.6 (<.001) |
| No | 67.2 | 81.9 | 87.7 | 100.0 | 95.6 | 40.5 |
| Race, %a | ||||||
| Asian | 17.1 | 9.3 (<.001) | 7.7 (<.001) | 3.1 (.04) | 6.9 (<.001) | 12.8 (<.001) |
| Black or African American | 5.6 | 5.6 (.93) | 9.5 (<.002) | 0 (.17) | 4.8 (.40) | 5.0 (.20) |
| White | 51.9 | 70.3 (<.001) | 57.5 (.009) | 18.8 (<.002) | 68.6 (<.001) | 66.7 (<.002) |
| Other | 2.3 | 1.6 (.051) | 2.8 (.46) | 53.1 (<.001) | 1.5 (.23) | 1.5 (.005) |
| Ethnicity, %a | ||||||
| Hispanic | 8.4 | 5.9 (<.002) | 9.7 (.33) | 4.2 (.46) | 8.2 (.86) | 6.5 (<.002) |
| Non-Hispanic | 91.6 | 94.1 | 90.3 | 95.8 | 91.8 | 93.5 |
DO = doctor of osteopathy; IHS = Indian Health Service; MD = doctor of medicine; NHSC = National Health Service Corps; PSLF = Public Service Loan Forgiveness.
Notes: Data are from the American Board of Family Medicine National Graduate Survey, 2016-2020. A total of 5,603 family physicians reported using no loan repayment program. P values are for comparison of the program group vs the overall sample.
Available for the 2017-2020 cohorts only.
As a population, PSLF recipients were more likely than the cohort overall to be graduates of osteopathic schools (29.0% vs 18.2%, P <.001), less likely to be international medical graduates (18.1% vs 32.8%, P <.001) or Asian (9.3% vs 17.1%, P <.001), and more likely to be White (70.3% vs 51.9%, P <.001). They were not statistically more likely than average to be female or Black/African American, however.
Program Use by Physician Practice Geography and Patient Population
Although 82.2% of early career NHSC recipients practiced in an underserved setting, just 24.2% of PSLF recipients did so, a value only slightly higher than average (19.5%, P <.001 for both) (Table 2). Those with NHSC assistance were significantly more likely to practice in a rural setting (23.3% vs 12.0% overall, P <.001), but this was not true for those pursuing PSLF. Both NHSC recipients and PSLF recipients reported earning less than the mean respondent annual salary, but this difference was greater for NHSC recipients, who averaged $191,344 as compared with the $203,995 earned by PSLF recipients and the $208,646 mean salary for the respondents overall (P <.001 and P = .02 vs overall, respectively).
Table 2.
Practice Scope and Setting of Early Career Family Physicians, Overall and by Loan Repayment Program
| Practice Attribute | Value (P Value) | |||||
|---|---|---|---|---|---|---|
| Overall | PSLF | NHSC | IHS | Military | Other | |
| iSOP score, meana | 16.1 | 16.4 (<.001) | 17.2 (<.001) | 18.6 (<.001) | 17.3 (<.001) | 16.8 (<.001) |
| Rural area (RUCC ≥4), % | 12.0 | 10.8 (.11) | 23.3 (<.001) | 43.8 (<.001) | 8.2 (.009) | 28.9 (<.001) |
| Primary care HPSA in 2020 | ||||||
| Whole county or partial, % | 89.7 | 90.7 (.43) | 96.6 (.03) | 100.0 (.41) | 88.9 (.82) | 91.0 (.32) |
| Whole county only, % | 4.5 | 3.7 (.42) | 12.5 (<.002) | 0 (.60) | 4.9 (.83) | 8.2 (<.001) |
| Medically underserved practice setting, % | 19.5 | 24.2 (<.001) | 82.2 (<.001) | 100.0 (<.001) | 2.6 (<.001) | 30.4 (<.001) |
| Annual income, mean, $ | 208,646 | 203,995 (.02) | 191,344 (<.001) | 203,726 (.74) | 148,711 (<.001) | 223,757 (<.001) |
HPSA = Health Professional Shortage Area; IHS = Indian Health Service; iSOP = individual scope of practice; NHSC = National Health Service Corps; PSLF = Public Service Loan Forgiveness; RUCC = Rural-Urban Continuum Code.
Notes: Data are from the American Board of Family Medicine National Graduate Survey, 2016-2020. A total of 5,603 family physicians reported using no loan repayment program. P values are for comparison of the program group vs the overall sample.
Reflects the number of clinical services provided; possible range is 0 to 30, with a higher score indicating a broader scope.
Scope of Practice by Repayment Program
A higher iSOP score indicates a broader range of services offered by a primary care physician, including obstetrical care and deliveries, pediatric care, geriatric care, and substance use disorder treatment, among others. Out of a possible maximum of 30 points on the iSOP scale, NHSC respondents had the highest mean at 17.2 compared with the means of 16.4 for PSLF respondents and 16.1 for the family physicians overall.
These findings point to an NHSC cohort distinct in its scope, geographic dispersion, and focus on underserved patients.
DISCUSSION
Key Findings and Implications
Our study suggests that the share of early career family physicians pursuing PSLF more than tripled between 2016 and 2020, while participation in the NHSC remained constant. Although NHSC loan repayment is offered at $25,000 per year and generally does not exceed 5 years, the average level of early career physician indebtedness is more than $200,000 and the uncapped forgiveness of PSLF makes it an appealing option for those with greater debt.9,10,11 We found distinct demographic profiles of family physicians pursuing PSLF vs NHSC loan repayment. For example, compared with the average family physician, PSLF enrollees were more likely to be trained in osteopathic medicine, White, and US medical graduates, and less likely to be Hispanic. By contrast, NHSC recipients were more likely to be female, Black, White, and US medical graduates relative to the average family physician. Asian American physicians were less likely to engage in any loan repayment mechanism.
These findings raise the question of whether the PSLF repayment mechanism provides more support to demographically overrepresented groups than to those who are underrepresented in medicine amid national calls to increase their inclusion in the physician workforce.20 The precise mechanism remains important to investigate further, but previous work suggests that information asymmetry in a complex repayment landscape may magnify existing disparities in access to education, training, and professional opportunities.21 Despite recent attention to diversity, inclusion, and health equity as a critical factor in expanding access to health careers and improving patient satisfaction with care and outcomes, investment in workforce change still lags.22 In a nation where a disproportionately low share of medical students hail from rural backgrounds and only 7% of physicians identify as Black or Hispanic/Latine, it is critically important to understand the contributions of medical education debt reduction to addressing these equity gaps.23
Focusing on issues of patient access to care, we found that physicians pursuing PSLF were no more likely than their broader peer group to work with an underserved patient population, to practice a broader scope of primary care, or to locate in a rural area. Although the absolute magnitude of difference in practice scope was modest at the physician level (17.2 for NHSC vs 16.4 for PSLF and 16.1 for the overall population), the national impact across family physicians should be considered. This difference raises important questions about the role of service-based loan repayment programs in the medical field, suggesting that PSLF may do no better than average at producing family physicians who practice in ways that extend health care to Americans regardless of geography or ability to pay, and setting it apart from NHSC as a mechanism to encourage public service in the medical field.
Limitations
Our study has several limitations. First, the ABFM data source includes self-reported data on student loan repayment and lacks detailed information on why respondents selected their given loan repayment program(s). Physicians also self-select their student loan repayment mechanisms, and there may be underlying differences between the populations engaging in NHSC and in PSLF; however, we believe this speaks to the importance of distinguishing outcomes between the 2 repayment programs. In the ABFM data set, scope of practice data, practice setting, practice address (from which rurality is derived), and demographic information are also self-reported by diplomates.
Given the cross-sectional nature of our analysis, we cannot make causal inferences about the relationship between demographics, loan burden, loan repayment mechanism selection, and practice patterns in early postgraduate careers. Future research could investigate the directionality of these associations while digging deeper into the level of financial support provided by various loan repayment and scholarship streams to physicians from groups traditionally underrepresented in medicine.
Additionally, HPSA designations are a nuanced tool for assessing the degree to which certain populations or communities are considered medically underserved. We did not distinguish between whole- or partial-county primary care HPSAs, which reduces the applicability of our findings in areas where this distinction is particularly important. Finally, this analysis is at the level of the physician survey respondent and does not, for instance, model the impact of type of graduate medical education training program (eg, Teaching Health Center).
Conclusions
The scope of PSLF is wide, encompassing loan repayment to medical professionals as well as a host of other employees with an intention of incentivizing careers in public service. Within the field of family medicine in particular, our analysis suggests that PSLF may be less likely to support physicians from underrepresented backgrounds, encourage broader scope of practice, and direct physicians to underserved settings, as compared with service-based loan repayment programs such as NHSC. These findings should prompt further discussion of the ways in which alignment of service-based loan repayment incentives with workforce policy goals could increase equity within the physician workforce and improve patient access to care.
Footnotes
Conflicts of interest: authors report none.
Previous presentation: Student Loan Repayment Options for Family Physicians: Impact on Practice Scope, Geography, and Vulnerable Populations Served; presented at the Society of Teachers of Family Medicine Annual Conference; April 30-May 4, 2022; Indianapolis, Indiana.
References
- 1.Driessen J, Zaloom C, Shrank WH.. Medical student debt reform: a proposed value-based loan repayment policy. J Gen Intern Med. 2020; 35(5): 1576-1578. 10.1007/s11606-020-05759-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friedman AB, Grischkan JA, Dorsey ER, George BP.. Forgiven but not relieved: US physician workforce consequences of changes to public service loan forgiveness. J Gen Intern Med. 2016; 31(10): 1237-1241. 10.1007/s11606-016-3767-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phillips JP, Morgan ZJ, Bazemore AW, Peterson LE.. Debt of family medicine residents continues to grow. J Am Board Fam Med. 2021; 34(3): 663-664. 10.3122/jabfm.2021.03.200567 [DOI] [PubMed] [Google Scholar]
- 4.Scheckel CJ, Richards JR, Newman JR, Fangman BD, Poole KG.. How trainees finance their medical education: implications of Higher Education Act reform. J Am Osteopath Assoc. 2020; 120(6): 370-379. 10.7556/jaoa.2020.058 [DOI] [PubMed] [Google Scholar]
- 5.Youngclaus JA, Koehler PA, Kotlikoff LJ, Wiecha JM.. Can medical students afford to choose primary care? An economic analysis of physician education debt repayment. Acad Med. 2013; 88(1): 16-25. 10.1097/ACM.0b013e318277a7df [DOI] [PubMed] [Google Scholar]
- 6.Phillips JP, Petterson SM, Bazemore AW, Phillips RL.. A retrospective analysis of the relationship between medical student debt and primary care practice in the United States. Ann Fam Med. 2014; 12(6): 542-549. 10.1370/afm.1697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Phillips JP, Peterson LE, Fang B, Kovar-Gough I, Phillips RL.. Debt and the emerging physician workforce: the relationship between educational debt and family medicine residents’ practice and fellowship intentions. Acad Med. 2019; 94(2): 267-273. 10.1097/ACM.0000000000002468 [DOI] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services Health Resources and Services Administration . National Health Service Corps loan repayment program. Published 2021. Accessed Oct 9, 2022. https://nhsc.hrsa.gov/sites/default/files/nhsc/loan-repayment/nhsc-lrp-fact-sheet.pdf
- 9.US Department of Health and Human Services, Health Resources and Services Administration . Students to service (S2S) loan repayment program. Published 2020. Accessed Oct 9, 2022. https://nhsc.hrsa.gov/sites/default/files/nhsc/loan-repayment/s2s-lrp-fact-sheet.pdf
- 10.US Department of Education, Federal Student Aid . Public service loan forgiveness data. Published 2022. Accessed Oct 9, 2022. https://studentaid.gov/data-center/student/loan-forgiveness/pslf-data
- 11.US Department of Education, Federal Student Aid . PSLF waiver offers way to get closer to loan forgiveness. Published 2022. Accessed Oct 9, 2022. https://studentaid.gov/announcements-events/pslf-limited-waiver
- 12.US Department of Health and Human Services . Fiscal year 2021. Justifications of estimates for appropriations committees. Published 2021. Accessed Feb 7, 2022. https://oig.hhs.gov/documents/root/8/hhs-oig-2021budget.pdf
- 13.National Health Service Corps . National Health Service Corps factsheet: building healthier communities. Accessed Feb 7, 2022. https://nhsc.hrsa.gov/sites/default/files/nhsc/about-us/nhsc-builds-healthy-communities.pdf
- 14.Kamerow DB. Is the National Health Service Corps the answer? (for placing family doctors in underserved areas). J Am Board Fam Med. 2018; 31(4): 499-500. 10.3122/jabfm.2018.04.180153 [DOI] [PubMed] [Google Scholar]
- 15.Nagaraj M, Coffman M, Bazemore A.. 30% of recent family medicine graduates report participation in loan repayment programs. J Am Board Fam Med. 2018; 31(4): 501-502. 10.3122/jabfm.2018.04.180002 [DOI] [PubMed] [Google Scholar]
- 16.American Hospital Association . Fast facts on U.S. hospitals, 2021. Published 2021. Accessed Feb 7, 2022. https://www.aha.org/system/files/media/file/2021/01/Fast-Facts-2021-table-FY19-data-14jan21.pdf
- 17.Association of American Medical Colleges . AAMC medical school graduation questionnaire (GQ). Published 2021. Accessed Feb 7, 2022. https://www.aamc.org/data-reports/students-residents/report/graduation-questionnaire-gq
- 18.Weidner AKH, Chen FM, Peterson LE.. Developing the National Family Medicine Graduate Survey. J Grad Med Educ. 2017; 9(5): 570-573. 10.4300/JGME-D-17-00007.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Neill T, Peabody MR, Blackburn BE, Peterson LE.. Creating the Individual Scope of Practice (I-SOP) scale. J Appl Meas. 2014; 15(3): 227-239. [PubMed] [Google Scholar]
- 20.Redford G; Association of American Medical Colleges . AAMC releases framework to address and eliminate racism. Published Oct 6, 2020. Accessed May 30, 2022. https://www.aamc.org/news/aamc-releases-framework-address-and-eliminate-racism
- 21.Bergh DD, Ketchen DJ, Orlandi I, Heugens PPMAR, Boyd BK.. Information asymmetry in management research: past accomplishments and future opportunities. J Manage. 2019; 45(1): 122-158. 10.1177/0149206318798026 [DOI] [Google Scholar]
- 22.Jacobs CK, Douglas M, Ravenna P, et al. Diversity, inclusion, and health equity in academic family medicine. Fam Med. 2022; 54(4): 259-263. 10.22454/FamMed.2022.419971 [DOI] [PubMed] [Google Scholar]
- 23.Jafee A, Associated Press . Harris announces $1.5B investment in healthcare workforce. US News & World Report. Published Nov 22, 2021. https://www.usnews.com/news/health-news/articles/2021-11-22/harris-to-announce-1-5b-investment-in-health-care-workforce