Abstract
PURPOSE
Girls and women with Down syndrome (DS) and their caregivers may have more difficulties in dealing with puberty, menstruation, and sexuality than those without DS. Our aim was to understand the concerns of these caregivers about gynecological aspects, including menstruation, contraception, and sexual practice.
METHODS
We performed a cross-sectional study that included caregivers of females with DS aged 9 years or older and both in pre- and post-menarche. The caregivers answered a questionnaire about their concerns regarding puberty, menstruation, sexuality, and contraception methods.
RESULTS
We enrolled 100 caregivers of females with DS. Caregivers’ major concern was menstrual bleeding. Most caregivers (57%) would not prohibit romantic relationships, including sexual relationships. Of the care recipients, 78 had reached menarche and their most common complaints were pain and behavioral changes. Regarding sexual behavior, 2% had already had sexual intercourse. Contraception was used by 14 of the 78 (17.9%) post-menarche females with weight gain as the most common side effect (43%).
CONCLUSIONS
In our sample, females with DS had sexual development comparable to those without the syndrome. As these females become increasingly independent, it is necessary to guide caregivers and primary care physicians, especially gynecologists, about the difficulties related to the menstrual period.
Key words: caregivers, down syndrome, gynecology, menstrual cycle, primary healthcare
INTRODUCTION
Down syndrome (DS) is the most common aneuploidy in live births and the most common genetic cause of cognitive impairment, affecting 1 in 319 to 1,000 live births.1,2 Some authors have stated that girls with DS have similar pubertal development to their peers without the syndrome. The age at menarche, menstrual cycles, genital anatomy, and sex hormone profiles are similar between females with and without DS. However, menstrual hygiene, premenstrual disorders, and contraception may be more difficult to manage in those with DS.3
Understanding the changes related to menstrual cycles and the use of contraception may be difficult due to the cognitive deficit in girls and women with DS.3,4 Females with DS may struggle using contraception methods because of communication and organizational difficulties native to this population. These issues make situations that require decision making, such as deciding to use oral contraception or even barrier methods, difficult to navigate.5 Side effects such as weight gain, drug interactions, irregular bleeding, and risk of thromboembolism should be taken into account when using contraception in this population. Patients with mild cognitive impairment can manage and adapt to their sexual impulses and social relationships.4 Females with DS face barriers such as inadequate gynecological guidance, lack of sexual education, and being considered by some parents and caregivers to be asexual.6 This occurs as a result of protection provided to girls considered incapable of dealing with sexuality and also to the myth that they have increased sexuality.7,8 Functional and physical limitations, medication, and comorbidities can also be limiting factors of sexuality development in this population.8 These girls need sexual education, especially from caregivers and family members, who also need to provide information about their concerns to health professionals.
There is insufficient medical knowledge about the gynecological needs of patients with DS. Medical professionals need to acquire more knowledge to provide proper care for this population.6-9 Our aim was to understand the concerns of the caregivers of Brazilian girls and women with DS-related gynecological issues.
METHODS
Overview
This is a cross-sectional study of the caregivers of girls and women (aged 9 years and older) diagnosed with DS who brought their care recipients to the Outpatient Clinic of the Hospital das Clínicas da Universidade Federal do Paraná. This multidisciplinary clinic was founded in 1997 and is dedicated to care of patients with Down syndrome. It offers consultations performed by a team of health professionals with skills in pediatrics, odontology, nutrition, psychology, nursing, and social work. All consultations and procedures are free of charge under Brazil’s public health system. Caregivers of patients with primary genital and sexual development disorders or deformities were excluded.
The patients with DS were not directly questioned as recommended by the ethics committee; they could not sign the consent form. Due to varying severity in cognitive deficits, some patients with DS may have difficulty understanding changes related to menstrual cycles and contraception and could be embarrassed.
Questionnaire
A literature review did not yield studies with validated questions that addressed the gynecological aspects of DS. Hence, the authors prepared the questionnaire in consultation with 3 parents of females with DS who were also health professionals and with expert input from other members of the clinic team (Table 1).
Table 1.
Questions About Gynecological Care of Patients With Down Syndrome
| How long does the caregiver stay with the patient? |
| What is your main concern or difficulty regarding puberty? |
| Have there been secondary sexual characteristics? (breasts, hair, vaginal bleeding) If yes, at what age? |
| How often does menstruation occur? |
| Do you notice pain with menstruation? Changes in behavior? |
| Does the patient use any medication to delay the onset of menstruation? |
| Would you like some medication to be used to delay the onset of menstruation? |
| Does the patient use any medication to control menstrual symptoms? |
| Do you think it is necessary to use any method or medication to control bleeding/menstruation? |
| What type of treatment to prevent pregnancy and/or reduce/abolish menstrual bleeding would you like the patient to use? |
| Does the patient use any method of contraception? If so which type? Did you notice side effects? Have you had to stop using it? What reason? |
| Does the occurrence of menstruation make it impossible or has already made it impossible for the patient to attend school, work, or other social activities? |
| Would you allow/not allow a loving relationship (dating, without sex)? |
| Would you allow/not allow intimate relationships, consensual sexual relations? |
| Do you think there is a need for guidance on STDs (sexually transmitted diseases)? |
| Do you agree to perform a surgical method to sterilize the patient? |
| Has the patient ever consulted with a doctor or gynecologist? |
| Has the patient ever had sexual intercourse in her life? |
| Has the patient ever had treatment for vaginal infection/discharge? |
| Does the patient perform personal hygiene alone? |
Recruitment
Caregivers attending the clinic with their daughters or care recipients from July 2018 to July 2019 were approached about participating in a study. The nature of the questionnaire (its focus on gynecologic issues) was explained and they were asked to participate. If they agreed, informed written consent was obtained. None of the patients with DS were directly asked the questions as the authors were concerned that many did not have the cognitive ability to respond, and the research ethics committee, (following Brazilian national legislation) did not allow it.
The questionnaire was administered face-to-face to caregivers. Questions were asked orally and the interviewer wrote down the answers. The caregivers’ demographic details were obtained, including date of birth, age, sex, kinship, education, and occupation. For the patients with DS, age, weight, height, and associated diseases were recorded from health records.
Data were analyzed using descriptive statistics including medians and interquartile ranges (IQR), means and standard deviations, or frequencies and percentages.
Ethical Approval
This study was approved by the local Committee of Ethics in Research (number 1.598.369). All caregivers of girls and woman with DS were informed about the study and signed consent. All procedures performed involving participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
RESULTS
During the study period, 100 caregivers of females with DS were approached and all agreed to participate.
Caregiver Data
The mean age of caregivers was 50 years (SD = 8.7), 89 were mothers, 1 was a father, and 10 were other relatives. Caregiver education level attained was college level for 34, high school completion or partial attendance for 39, and primary school level for 26. Nearly all (95%) caregivers lived with their daughter or care recipient and had daily contact.
Patient Data
Among the 100 patients with DS, the mean age was 17 years (SD = 8.4); 22 were children (aged less than 12 years old, 45 were adolescents (aged 13 to 17 years), and 33 were adults (aged 18 years or older).
A majority of patients (60%) had other diagnosed diseases. The most common were hypothyroidism (42%) and cardiac disease (9%), with a low numbers having diabetes mellitus (3%), depression (3%), rhinitis (2%), autism (2%), and lupus (1%).
Table 2 shows the demographic and clinical characteristics of the patients with DS. Most (78%) had reached menarche. Of those 78, 45% reported that menstruation had already interfered with activities such as attending school, work, or other social activities.
Table 2.
Characteristics of Patients (N = 100)
| Characteristic (No.) | Mean (SD) | Range |
|---|---|---|
| Age (n = 100), y | 17.4 (8.4) | 9-47 |
| Weight (n = 98), kg | 50.5 (14.8) | 28-88 |
| Height (n = 95), m | 1.42 (0.1) | 1.1-1.6 |
| Thelarche (n = 77), y | 11.1 (1.7) | 8-15 |
| Pubarche (n = 82), y | 10.9 (1.6) | 7-15 |
| Menarche (n = 78), y | 11.8 (1.5) | 9-15 |
Table 3 shows the proportion of menstrual-related symptoms reported, frequency of menstruation, and use of medications for control of symptoms. Pain was a common complaint and when managed with drugs, antispasmodics and nonsteroidal anti-inflammatory drugs were used most often. Behavioral changes and bleeding were also troublesome. Personal hygiene was a concern for 12%, but caregivers reported that 78% could manage their personal hygiene.
Table 3.
Characteristics Related to Menstruation (N = 78)
| Symptoms related to menstruation, % | |
| Behavior changes | 74.0 |
| Pain | 62.3 |
| Pain and behavior changes | 44.1 |
| Did not answer | 6.0 |
| Frequency of menstruation, % | |
| Monthly | 88.3 |
| Unpredictable | 9.1 |
| Twice a month | 2.6 |
| Medications to control menstrual symptoms, % | |
| Antispasmodics | 13.0 |
| NSAIDs | 11.0 |
| Hormones | 7.0 |
| Analgesics | 4.0 |
| Others | 3.0 |
NSAID = nonsteroidal anti-inflammatory drug.
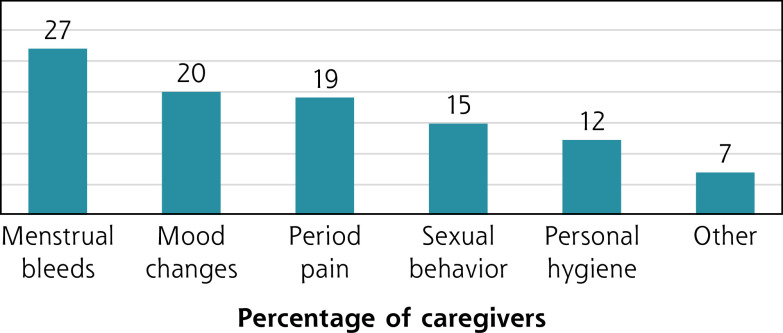
Figure 1 displays the caregiver’s concerns related to the monthly menstrual cycle in females with DS. All of the caregivers of patients who had reach menarche had concerns about menstruation, and the main concerns included menstrual bleeds, mood changes, pain, and hygiene.
Figure 1.
Caregiver concerns about menstrual cycles.
Further, regarding the use of methods to prevent or reduce menstrual bleeding, 41% of caregivers were not interested in their care recipients using any method, 15% would like methods that allow menstruation to occur at predictable intervals, and 36% would like a non-surgical method to stop menstruation. Most caregivers (78%) did not agree with use of a surgical sterilization method, but 14% were in favor of tubal ligation and 8% preferred hysterectomy.
Two caregivers reported that their care recipients who had reached menarche had had sexual intercourse, while 94 denied any sexual intercourse and 4 did not respond. Most caregivers (57%) reported that they would not prohibit romantic relationships, including sexual relationships. It should be noted that 33% of the patients were adults aged 18 or over. For 84%, caregivers felt it was necessary for patients to be educated about sexually transmitted diseases.
Table 4 summarizes findings associated with use of contraception. The use of contraception was reported for 14 patients; 4 used injectable medroxyprogesterone acetate (3 used it quarterly, 1 used it monthly), 9 used oral contraception, and 1 used an intrauterine device. Weight gain was the most common side effect, affecting 43% of patients using birth control.
Table 4.
Contraception Methods and Side Effects (N = 14)
| Contraception Method | No. (%) | Side Effects | No. |
|---|---|---|---|
| Oral pills | |||
| With interval | 7 (50.0) | Weight gain | 4 |
| Without interval | 2 (14.4) | Skin changesa | 1 |
| Quarterly injectable (MPA) | 3 (21.4) | Weight gain | 1 |
| Monthly injectable (MPA) | 1 (7.2) | Did not answer | 1 |
| Intrauterine device | 1 (7.2) | Weight gain | 1 |
MPA = medroxyprogesterone acetate.
Oily, acne, spots on the skin.
Consultation with a gynecologist was reported for 52% of patients. Caregivers reported that 4% of patients had had a vaginal infection or vaginal discharge at least once.
DISCUSSION
This is the first study that addresses gynecological concerns reported by caregivers of girls and women with DS in Latin America. The caregivers interviewed were predominantly mothers with a mean age of 50 years who spent most of the day with their daughters. This was a common finding in other studies10,11 and demonstrates that the caregivers were familiar with their daughter’s daily routines and concerns.
The mean age at menarche, pubarche, and thelarche of our DS women was similar to that reported in other studies of women with developmental disabilities.12,13 Pain and sexual behavior change were the most frequent complaints reported in our study. The American College of Gynecologists have opined behavioral changes in patients with cognitive impairment may be an expression of pain.13 Thus, it is important that behavioral changes are interpreted appropriately.
Most caregivers were concerned about menstrual bleeding in patients with DS, followed by changes in behavior. This is in line with other articles that reported the main complaints of patients with DS and caregivers are related to menstruation.14-18 Menarche imposes new care routines on caregivers, as they help the adolescents manage their monthly cycles. This raises the anxiety for both caregivers and the girls. Health professionals must be encouraged to give adequate guidance to both parties. Further work is needed to understand if physicians and other health professionals have adequate training to meet these needs.
Regarding associated diseases in our patients with DS, hypothyroidism was the most common (42%) which is corroborated in the literature.19,20 Hence, screening for thyroid disorders is important in individuals with DS, especially in girls, because thyroid dysfunction affects menses including both oligomenorrhea and menorrhagia.21,22
We inquired about the ability of the girls and women with DS to perform personal hygiene without the help of the caregiver and tasks that require autonomy. While most patients were reportedly able to perform their hygiene activities, it is essential that health care professionals encourage caregivers to help the girls to develop this capacity.6
Although 57% of caregivers reported that they allowed girls with DS under their care to have romantic relationships, including sexual intercourse, only 2% reported that this had actually occurred. While parents and caregivers want their daughters to have the greatest independence possible, they reported fear about sexuality, a concern documented in other studies.23,24
Many caregivers and families of girls with DS treat their girls as “eternal children,” without sexuality.13,25,26 There is also the myth that sexuality in people with DS is exacerbated.27 In most cases this is due to parents or caregivers not properly guiding their children on these topics, as sexuality in girls with DS is thought to be similar to that of the general population.24 Good guidance on the subject is essential so that they can live with independence and fullness.24,28
In our sample, about 18% of the girls who had already had menarche used contraception, with 1 of them using an intrauterine device. Caregivers often ask attending physicians to control menstruation or even induce amenorrhea. It is prudent to investigate the reason for requests to suppress menstruation in patients with DS, particularly to determine if the request comes directly from the patient or is demanded by her caregivers.23 The reasons for this demand must be documented (convenience, prevention of unwanted pregnancies, control of menstrual bleeding).23
Of those using contraception, 4 patients used injectable and 9 used oral. The contraception method’s route of administration must be evaluated in the context of the patient’s cognitive ability.13 Other factors that may influence the type of contraception method used are the potential side effects. The most common side effect (weight gain) observed in our study was the same as that found in the general population.28 There were 3 patients using medroxyprogesterone acetate (injectible) quarterly. Due to its potential side effects, such as bone mineral density loss and weight gain in obese teens, this medication should be used with caution in young girls.28
In our sample, 8% of caregivers would like the patients to have a hysterectomy to eliminate vaginal bleeding. Hysterectomy for the purpose of sterilization is inadequate, however, and for elimination of bleeding it can only be considered as a last resort and in cases of extreme necessity. The procedure does not reduce the risk of sexual abuse and does not improve the behavioral changes associated with monthly hormonal cycles. It should be performed exclusively for medical reasons, after taking into account ethical and legal aspects inherent to the issue.17 Brazil has specific legislation on this subject, indicating that the sterilization of legally incapable people can only be carried out with judicial authorization.29 However, this law does not establish levels of disability. In our understanding, it is necessary for the government to potentially provide the most needy families with the hormone implants free of charge, which we believe is the most suitable solution for those women who need it.
It’s possible that some patients with cognitive deficit have greater difficulty understanding menarche and its symptoms, so the patient’s physician (gynecologist or not) must be able to help the family. Most demands will be presented in their offices, health centers, or even emergency services. The education of health professionals involved in these services is important. They must be aware of the peculiarities of gynecological care for girls and women with DS and know how to instruct the patient and her caregiver about these topics.
The limitations of the present study are inherent to its descriptive design and lack of comparison with a caregiver group of females without DS. We believe that the people who answered the questionnaire are well informed about DS in general, since they attend our Outpatient Clinic whose purpose is to assist people with DS. Possibly, caregivers who do not have such assistance find greater difficulty in the gynecological care of patients with DS. Our study was conducted in Brazil, with patients served by a public health system, and some of our results may not be applicable to other regions of the world, due to the cultural aspects, particularly related to sexuality. Although some data about gynecological issues found in our study certainly correspond to those observed in girls and women with DS worldwide. In addition, factors that could cause biases such as autonomy, degree of cognition, and other associated gynecological diseases such as myomatosis and endometriosis were not evaluated.
In conclusion, our data may contribute to better understanding the needs of these patients regarding gynecological care and the main concerns of the caregivers. Also, our study serves to sensitize physicians, whether gynecologists or not, who may at some point attend to a patient with DS and may not be well equipped to answer the family’s questions or address their concerns.
Footnotes
Conflicts of interest: authors report none.
Disclaimer: The views expressed are solely those of the authors and do not necessarily represent official views of the authors’ affiliated institutions.
REFERENCES
- 1.Gardiner K, Herault Y, Lott IT, Antonarakis SE, Reeves RH, Dierssen M.. Down syndrome: from understanding the neurobiology to therapy. J Neurosci. 2010; 30(45): 14943-14945. 10.1523/JNEUROSCI.3728-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holmes G. Gastrointestinal disorders in Down syndrome. Gastroenterol Hepatol Bed Bench. 2014; 7(1): 6-8. [PMC free article] [PubMed] [Google Scholar]
- 3.Paransky OI, Zurawin RK.. Management of menstrual problems and contraception in adolescents with mental retardation: a medical, legal, and ethical review with new suggested guidelines. J Pediatr Adolesc Gynecol. 2003; 16(4): 223-235. 10.1016/s1083-3188(03)00125-6 [DOI] [PubMed] [Google Scholar]
- 4.Gokgoz C, Deliktas Demirci A, Kabukcuoglu K.. Sexual behaviours and education in adolescents and young adults with Down syndrome: a grounded theory study of experiences and opinions of their mothers in Turkey. Res Dev Disabil. 2021; 112: 103907. 10.1016/j.ridd.2021.103907 [DOI] [PubMed] [Google Scholar]
- 5.Scola PS, Pueschel SM.. Menstrual cycles and basal body temperature curves in women with Down syndrome. Obstet Gynecol. 1992; 79(1): 91-94. [PubMed] [Google Scholar]
- 6.Grover SR. Gynaecological issues in adolescents with disability. J Paediatr Child Health. 2011; 47(9): 610-613. 10.1111/j.1440-1754.2011.02163.x [DOI] [PubMed] [Google Scholar]
- 7.Atkinson E, Bennett MJ, Dudley J, et al. ; Australian Society of Paediatric and Adolescent Gynaecology Working Party . Consensus statement: menstrual and contraceptive management in women with an intellectual disability. Aust N Z J Obstet Gynaecol. 2003; 43(2): 109-110. 10.1046/j.0004-8666.2003.00046.x [DOI] [PubMed] [Google Scholar]
- 8.Murphy GH. Capacity to consent to sexual relationships in adults with learning disabilities. J Fam Plann Reprod Health Care. 2003; 29(3): 148-149. 10.1783/147118903101197520 [DOI] [PubMed] [Google Scholar]
- 9.Zurawin RK, Paransky OI.. The role of surgical techniques in the treatment of menstrual problems and as contraception in adolescents with disabilities. J Pediatr Adolesc Gynecol. 2003; 16(1): 51-54. 10.1016/s1083-3188(02)00214-0 [DOI] [PubMed] [Google Scholar]
- 10.Barros ALO, Barros AO, Barros GLM, Santos MTBR.. Burden of caregivers of children and adolescents with Down Syndrome. Cien Saude Colet. 2017; 22(11): 3625-3634. 10.1590/1413-812320172211.31102016 [DOI] [PubMed] [Google Scholar]
- 11.Silva M, Trovó de Marqui AB.. Síndrome de Down: caracterização dos pacientes, seus cuidadores e percepção dos pais [Down syndrome: characterization of patients, their caregivers and parents’ perception]. Multitemas. 2020; 21(59): 27-50. 10.20435/multi.v21i59.2677 [DOI] [Google Scholar]
- 12.Kirkham YA, Allen L, Kives S, et al. Trends in menstrual concerns and suppression in adolescents with developmental disabilities. Journal Adolesc Health. 2013; 53(3): 407–412. 10.1016/j.jadohealth.2013.04.014 [DOI] [PubMed] [Google Scholar]
- 13.American College of Obstetricians and Gynecologists’ Committee on Adolescent Health Care . Committee Opinion No. 668: menstrual manipulation for adolescents with physical and developmental disabilities. Obstet Gynecol. 2016; 128(2): e20-e25. 10.1097/AOG.0000000000001585 [DOI] [PubMed] [Google Scholar]
- 14.Grover SR. Menstrual and contraceptive management in women with an intellectual disability. Med J Aust. 2002; 176(3): 108-110. 10.5694/j.1326-5377.2002.tb04315.x [DOI] [PubMed] [Google Scholar]
- 15.Dizon CD, Allen LM, Ornstein MP.. Menstrual and contraceptive issues among young women with developmental delay: a retrospective review of cases at the Hospital for Sick Children, Toronto. J Pediatr Adolesc Gynecol. 2005; 18(3): 157-162. 10.1016/j.jpag.2005.03.002 [DOI] [PubMed] [Google Scholar]
- 16.Albanese A, Hopper NW.. Suppression of menstruation in adolescents with severe learning disabilities. Arch Dis Child. 2007; 92(7): 629-632. 10.1136/adc.2007.115709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quint EH. Menstrual issues in adolescents with physical and developmental disabilities. Ann N Y Acad Sci. 2008; 1135: 230-236. 10.1196/annals.1429.020 [DOI] [PubMed] [Google Scholar]
- 18.Burke LM, Kalpakjian CZ, Smith YR, Quint EH.. Gynecologic issues of adolescents with Down syndrome, autism, and cerebral palsy. J Pediatr Adolesc Gynecol. 2010; 23(1): 11-15. 10.1016/j.jpag.2009.04.005 [DOI] [PubMed] [Google Scholar]
- 19.Chaker L, Razvi S, Bensenor IM, Azizi F, Pearce EN, Peeters RP.. Hypothyroidism. Nat Rev Dis Primers. 2022; 19; 8(1): 30. 10.1038/s41572-022-00357-7 [DOI] [PubMed] [Google Scholar]
- 20.Whooten R, Schmitt J, Schwartz A.. Endocrine manifestations of Down syndrome. Curr Opin Endocrinol Diabetes Obes. 2018; 25(1): 61-66. 10.1097/MED.0000000000000382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krassas GE, Pontikides N, Kaltsas T, et al. Disturbances of menstruation in hypothyroidism. Clin Endocrinol (Oxf). 1999; 50(5): 655-659. 10.1046/j.1365-2265.1999.00719.x [DOI] [PubMed] [Google Scholar]
- 22.Joshi JV, Bhandarkar SD, Chadha M, et al. Irregularidades menstruais e falha na lactação podem preceder a disfunção da tireoide ou bócio [Menstrual irregularities and lactation failure may precede thyroid dysfunction or goitre]. Jornal de medicina de pós-graduação. 1993; 39(3): 137-141. [PubMed] [Google Scholar]
- 23.Quint EH. Menstrual and reproductive issues in adolescents with physical and developmental disabilities. Obstet Gynecol. 2014; 124(2 Pt 1): 367-375. 10.1097/AOG.0000000000000387 [DOI] [PubMed] [Google Scholar]
- 24.Bernert DJ. Sexuality and disability in the lives of women with intellectual disabilities. Sex Disabil. 2010; 29(2): 129-141. 10.1007/s11195-010-9190-4 [DOI] [Google Scholar]
- 25.Esmail S, Darry K, Walter A, Knupp H.. Attitudes and perceptions towards disability and sexuality. Disabil Rehabil. 2010; 32(14): 1148-1155. 10.3109/09638280903419277 [DOI] [PubMed] [Google Scholar]
- 26.Manor-Binyamini I, Schreiber-Divon M.. Parental perceptions of the sexuality of adolescents with intellectual disabilities. Sex Disabil. 2019; 37: 599-612. 10.1007/s11195-019-09586-3 [DOI] [Google Scholar]
- 27.Bononi BM, Sant’Anna MJ, de Oliveira AC, et al. Sexualidade e pessoas com síndrome de Down: Um estudo do Brasil [Sexuality and persons with Down syndrome: a study from Brazil]. Revista Internacional de Medicina e Saúde do Adolescente. 2009; 21(3): 319-326. 10.1515/ijamh.2009.21.3.319 [DOI] [PubMed] [Google Scholar]
- 28.Quint EH. Adolescents with special needs: clinical challenges in reproductive health care. J Pediatr Adolesc Gynecol. 2016; 29(1): 2-6. 10.1016/j.jpag.2015.05.003 [DOI] [PubMed] [Google Scholar]
- 29.Brasil, Presidência da República, Lei no 9.263 . Regula o § 7° do art. 226 da Constituição Federal, que trata do planejamento familiar, estabelece penalidades e dá outras providências [Regulates § 7 of art. 226 of the Federal Constitution, which deals with family planning, establishes penalties and takes other measures]. Casa Civil [Civil House], Brasilia. Published 1996. https://www.camara.leg.br/proposicoesWeb/prop_mostrarintegra;jsessionid=1585CB40CB70F16A655332E4B7D84995.proposicoesWeb1?codteor=490199&filename=LegislacaoCitada+-PL+1686/2007