Abstract
Purpose
To investigate the association between changes in individual (anterior, lateral, and posterior) and overall deltoid compartment pressures and postoperative opioid consumption up to 14 days after primary double-row arthroscopic rotator cuff repair (ARCR).
Methods
In 113 consecutive patients undergoing primary double-row ARCR, anterior, lateral, and posterior deltoid compartment pressures were measured prior to incision and immediately after closure with a manometer. Postoperatively, all patients were provided with an identical rehabilitation protocol, quantity and dose of opioid tablets, and pain journal in which to record daily opioid consumption and visual analog scale pain scores for 14 days after surgery. The pain journals were collected at the first postoperative visit, and opioid consumption was calculated based on morphine equivalents. Statistical analysis was performed to determine the association between deltoid compartment pressures and opioid consumption postoperatively.
Results
Sixty-nine percent of patients who met the inclusion criteria (74 of 107) returned the pain journals. The mean age at the time of surgery was 57.4 ± 8.8 years (range, 30-75 years), with female patients being significantly older (P = .03). The mean length of surgery was 71.7 ± 16.3 minutes. No significant association between increase in individual (anterior, lateral, or posterior) or mean overall compartment pressures and morphine equivalents of opioid consumption was appreciated on any postoperative day.
Conclusions
No significant correlation between increase in individual or overall deltoid compartment pressures after ARCR and postoperative opioid consumption in the immediate postoperative period was found in this study.
Level of Evidence
Level II, prospective cohort study.
Opioid consumption in the United States has increased dramatically over the past 3 decades, leading the US Centers for Disease Control and Prevention to label opioid abuse as an epidemic.1, 2, 3 The opioid epidemic presents a substantial concern for all medical specialties, particularly orthopaedic surgeons, who represent the third highest prescribers of opioid pain medication in the United States.4,5 Successful postsurgical outcomes have become increasingly complicated in the setting of the opioid epidemic, necessitating a balance between achieving adequate pain control and avoiding opioid tolerance and potential dependence after the treatment of orthopaedic injuries.4,6 As such, given the substantial burden of musculoskeletal pain after surgery5,7 and the high volume of opioid prescriptions, orthopaedic surgeons are in a position to have a substantial influence on helping control the current opioid crisis.
One of the most frequently performed operations associated with the potential for considerable postoperative pain requiring prolonged opioid use is arthroscopic rotator cuff repair (ARCR).8,9 As the national incidence of primary rotator cuff repair has increased over the past 2 decades,10 the rate of ARCR has similarly increased when compared with traditional open or mini-open rotator cuff repair.11,12 ARCR is characterized as a minimally invasive procedure, with the benefit of smaller incisions, less trauma to the deltoid musculature, and the ability to address concomitant lesions in the shoulder, while theoretically producing less postoperative pain compared with open procedures.13,14 However, the benefit of ARCR in reducing pain in the early postoperative period has been disputed in multiple investigations.15, 16, 17, 18, 19 As such, identifying variables influencing postoperative pain requiring opioid consumption after ARCR is critical to combat the current opioid epidemic while improving patient satisfaction and postoperative outcomes.
Prior investigations have examined the association between postoperative pain and opioid consumption in terms of both patient-related (preoperative pain levels, preoperative opioid use, patient age, sex, nicotine abuse, tear size, and range of motion)9,20, 21, 22, 23, 24, 25, 26, 27 and surgeon-related (duration of surgery and surgical approach) factors.19,26 When examining deltoid pressures, in their investigation of 40 patients undergoing arthroscopic subacromial decompression with or without distal clavicle resection, De Wachter et al.28 reported that soft-tissue pressure in the deltoid was elevated during surgery and did not drop to baseline levels within 10 minutes after discontinuation of fluid irrigation into the shoulder. However, the influence of increased deltoid compartment pressures due to fluid extravasation from fluid pump pressure during ARCR on postoperative opioid consumption remains unknown.
The purpose of this study was to investigate the association between changes in individual (anterior, lateral, and posterior) and overall deltoid compartment pressures and postoperative opioid consumption up to 14 days after primary double-row ARCR. We hypothesized that patients with greater increases in postoperative deltoid compartment pressures when compared with preoperative values would consume more opioids postoperatively.
Methods
Prior to patient enrollment, approval was obtained from the institutional review board at the senior author’s (R.J.G.) institution. Prospective patients were scheduled to undergo ARCR with subacromial decompression performed by 1 of 4 (M.J.S., B.N.V., J.E.V., R.J.G.) fellowship-trained orthopaedic surgeons who all participated equally for the duration of the investigation. The inclusion criteria consisted of patients undergoing primary arthroscopic double-row repair with suture anchors, age 18 to 80 years, and capability of providing consent and following a standardized postoperative rehabilitation protocol. Patients using opioid pain medication at the time of surgery, patients with active pain disorders (fibromyalgia or complex regional pain syndrome), pregnant patients, and patients undergoing single-row repair, open repair, or revision surgery were excluded. A state-based prescription drug monitoring program was used to confirm the absence of active opioid consumption prior to surgery while tracking any prescription refills provided postoperatively by other providers. During the 50-month study period, a total of 113 patients were identified as potentially meeting the inclusion criteria and provided consent for study participation.
Surgical Technique
After the administration of a single-shot interscalene block by a fellowship-trained anesthesiologist, induction of general anesthesia, and positioning in the beach-chair position, deltoid compartment pressures were measured using a Stryker manometer needle (Kalamazoo, MI). Measurements were performed by placing the needle within the chamber, calibrating the monitor, and inserting the needle in the anterior, lateral, and posterior deltoid compartments with care to ensure needle placement within the musculature. The measurement locations were standardized using anatomic landmarks, with the anterior compartment needle placed 1 cm lateral to the coracoid and 1 cm inferior to the anterior aspect of the acromion. The lateral deltoid was measured 2 cm inferior to the lateral aspect of the acromion, whereas the posterior deltoid needle was inserted 1 cm inferior and 1 cm medial to the posterolateral tip of the acromion. Compartment pressures were recorded on an intraoperative data sheet. ARCR was then performed with concomitant subacromial decompression and biceps tenodesis when clinically indicated. Two types of pumps (DePuy Synthes, Raynham, MA, and Arthrex, Naples, FL) were used among the 3 surgeons, with the application of comparable pump pressures during each surgical procedure. Immediately after portal closure, deltoid compartment pressures were remeasured using the same procedure in the anterior, lateral, and posterior deltoid musculature, and these measurements were recorded. Patients were discharged with a standardized postoperative rehabilitation protocol consisting of sling immobilization with a supporting abduction pillow to be worn at all times for 4 weeks except when showering and during rehabilitation, which consisted of passive range of motion of the shoulder according to patient tolerance. Patients were also supplied with a prescription for 1 to 2 tablets of oxycodone/acetaminophen, 5/325 mg (42 tablets), to be taken every 4 to 6 hours as needed for pain control. No refill prescriptions were provided by the treating surgeons.
Pain Journal
After surgery, patients not excluded owing to the performance of an open or single-row repair were instructed to track their daily pain level and opioid consumption. Patients were asked to record their mean overall pain level over the duration of the day on a visual analog scale (VAS) prior to bed, whereas opioid consumption was recorded as the total quantity of tablets consumed each day. On the basis of prior studies, analgesic use was normalized to morphine-equivalent (MEQ) dosage.18,29 Pain journals with daily entries were kept by patients for a total of 14 days and returned during their first postoperative visit approximately 2 weeks after surgery.
Statistical Analysis
On the basis of previously published studies, an a priori sample size calculation was performed to identify the necessary number of patients for this analysis.13,17, 18, 19,30,31 Assuming an α probability of .05 and a target β value of .8, for an estimated large effect size (d = 0.8), the necessary sample size would be 84, whereas a medium effect size (d = 0.5) would require a sample size of 210.
Mean patient age and length of surgery were calculated, and the Student t test was used to compare differences between men and women. Mean preoperative compartment pressures overall and in each compartment (anterior, lateral, and posterior) were calculated and compared with postoperative compartment pressures similarly using the Student t test. Unique linear models were estimated for each of the following outcomes: MEQs of opioids consumed on day 1, day 2, day 3, day 4, day 5, day 6, day 7, and day 14 postoperatively. We first tested whether postoperative pressures in each compartment (anterior, middle, and posterior) were associated with MEQs of opioids consumed on each of the aforementioned postoperative days. Under the hypothesis that the change in compartment pressure may be associated with the consumption of opioids postoperatively, we tested whether preoperative-to-postoperative changes in each compartment pressure were associated with MEQs of opioids consumed on each of the days previously described. We also analyzed the association with preoperative-to-postoperative change in average compartment pressure, with the hypothesis that changes in overall pressure would influence opioid consumption more than changes in the pressure of any single compartment. To assess the relation between pain scores and MEQs of opioids consumed preoperatively, we estimated a unique linear model for each postoperative day that used MEQs of opioids consumed on that day as the dependent variable and used VAS pain score on that same day as the independent variable (while also adjusting for age and sex). We further hypothesized that opioid consumption may alternatively relate to the pain experienced on the previous day rather than the present day, and we tested this hypothesis by introducing a 1-day lag in VAS pain score relative to opioid consumption. Prior studies have documented an association between postoperative pain and MEQs of opioids consumed after rotator cuff repair.26,32 We therefore also estimated all of our models using pain scores specific to each postoperative day as a covariate. We did not find that including postoperative pain scores changed our estimates of the association between deltoid compartment pressures and postoperative opioid consumption in a clinically meaningful way. We therefore present estimates of the more parsimonious models that include only age and sex as covariates. A prespecified α of .05 was used to determine statistical significance. All analyses were conducted in R (version 3.6.2; R Foundation for Statistical Computing, Vienna, Austria) using the Hmisc, rms, ggplot2, ggpubr, gridExtra, and tidyverse packages.
Results
Of the 113 patients identified preoperatively for study inclusion, 6 required open repair and were excluded; no patients underwent single-row repair. After surgery, 69% of patients (74 of 107) returned completed pain journals; the remaining 31% of patients (33 of 107) did not return the pain journals and were excluded from further analysis. Among the patients who returned completed pain journals, the mean overall age at the time of surgery was 57.4 ± 8.8 years (range, 30-75 years), with female patients being significantly older (P = .03) (Table 1). The mean length of surgery was 71.7 ± 16.3 minutes and was longer in male patients (P = .06). Biceps tenodesis was performed in 77% of patients (58 of 74), of whom 71% (41 of 58) underwent these procedures prior to ARCR. Subacromial decompression was performed in all patients. No complications were reported during short-term patient follow-up.
Table 1.
Overview of Study Population
| Male Patients | Female Patients | P Value | |
|---|---|---|---|
| Patients, n | 51 | 23 | — |
| Age at surgery, mean ± SD, yr | 56.0 ± 9.0 | 60.4 ± 7.7 | .03 |
| Length of surgery, mean ± SD, min | 73.8 ± 17.5 | 66.6 ± 12.1 | .06 |
SD, standard deviation.
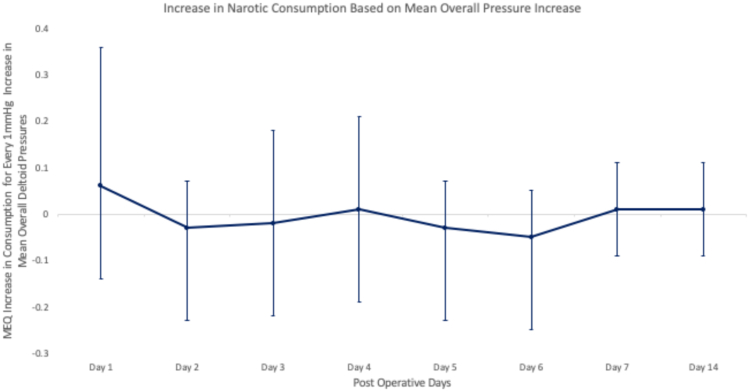
The mean deltoid pressure in each compartment (anterior, lateral, and posterior) and the mean overall deltoid compartment pressure were significantly elevated when comparing postoperative and preoperative pressures (P < .001 for all) (Table 2). No significant association between increase in individual compartment pressure (anterior, lateral, or posterior) (Fig 1) or mean overall increase (Fig 2) in compartment pressures and MEQs of opioid consumption was appreciated on any day through postoperative day 14 (Fig 3). No significant difference in opioid consumption was appreciated on any postoperative day in patients who underwent biceps tenodesis versus those who did not (P > .05 for all days).
Table 2.
Comparison of Mean Preoperative and Postoperative Deltoid Compartment Pressures
| Compartment Pressure, Mean ± SD, mm Hg |
P Value | ||
|---|---|---|---|
| Preoperative | Postoperative | ||
| Individual | |||
| Anterior | 9.5 ± 2.7 | 18.5 ± 6.0 | <.001 |
| Lateral | 10.4 ± 2.6 | 20.3 ± 6.5 | <.001 |
| Posterior | 9.2 ± 2.6 | 20.0 ± 6.8 | <.001 |
| Overall | 9.74 ± 2.7 | 19.7 ± 6.5 | <.001 |
SD, standard deviation.
Fig 1.
Graph showing association between increased opioid consumption (based on morphine equivalents [MEQ]) and increase in each deltoid compartment (anterior, lateral, and posterior) after arthroscopic rotator cuff repair with standard error.
Fig 2.
Graph showing association between increased opioid consumption (based on morphine equivalents [MEQ]) and overall mean increase in all deltoid compartments after arthroscopic rotator cuff repair with standard error.
Fig 3.
Scatter-plot graphs showing absence of association between opioid consumption (based on morphine equivalents [MEQ]) and average (Avg) overall postoperative (Post-Op) compartment pressures measured immediately after surgery from postoperative day (POD) 1 to POD 14.
Discussion
The most important finding of this study is that the individual and mean overall increases in deltoid compartment pressures after ARCR were not associated with statistically significant changes in postoperative opioid consumption. We initially hypothesized that during ARCR, the extravasation of the fluid into the deltoid musculature would significantly contribute to postoperative opioid consumption. However, our results do not support a relation between the increases in overall or individual compartment pressures and postoperative opioid consumption. Whereas some investigations have cited less postoperative pain as a reported benefit of ARCR when compared with open repair,13,14 other studies have challenged this assertion. Notably, when analyzing 102 patients undergoing ARCR (50 patients) versus open repair (52 patients), Williams et al.19 found no difference in days to zero pain, residual pain, cumulative pain, or opioid consumption when patients were evaluated up to 6 weeks postoperatively. As such, further investigations are necessary to identify other surgeon-controlled factors inherent to ARCR accounting for postoperative pain and subsequent opioid consumption to further elucidate the benefits of ARCR over open repair.
Patients who were actively consuming opioids at the time of surgery were excluded from this investigation because of the concern for greater opioid consumption in the postoperative period, thereby excluding a potential confounding variable in our analysis. Multiple prior investigations have shown that active opioid use prior to surgery has a substantial impact on postoperative outcomes and pain after ARCR. Williams et al.26 retrospectively analyzed 200 patients undergoing ARCR, of whom 44 self-reported opioid consumption preoperatively or were determined to be actively consuming opioids preoperatively. The authors found that patients using opioids prior to surgery required both a significantly greater number of opioids postoperatively (1.91 times more; 95% confidence interval, 1.31-2.78) and a longer duration of postoperative opioid therapy (2.73 times longer; 95% confidence interval, 1.62-4.59) compared with those without not consuming opioids prior to surgery. Meanwhile, Westermann et al.9 retrospectively analyzed 29,827 ARCR patients to identify variables associated with prolonged opioid consumption postoperatively. They found that patients prescribed opioids less than 1 month prior to surgery were 3.04 times more likely to require opioids up to 3 months postoperatively whereas those prescribed opioids 1 to 3 months prior to surgery were 7.45 times more likely to require opioids at 3 months. Although preoperative opioid consumption is likely related to the increased prevalence of pre-existing medical conditions causing pain, it remains imperative that the orthopaedic surgeon inquire about potential opioid tolerance or dependence in selecting appropriate patients for elective ARCR.22
Patients reporting higher preoperative VAS scores have been found to have greater postoperative pain and opioid consumption after surgery.19,20,21,32 Kim et al.21 found that high initial VAS scores were associated with higher-than-average pain scores 12 months after ARCR. On the contrary, in their evaluation of 181 patients undergoing ARCR, Cuff et al.20 found that preoperative subjective pain tolerance, namely patient-reported high pain tolerance, was the most significant predictor of high VAS scores on postoperative days 1 and 7. As such, determination of preoperative pain levels may be valuable in predicting postoperative pain tolerance, warranting further investigations identifying and intervening on factors associated with high preoperative VAS scores as a means of decreasing postoperative opioid consumption.
Inherent within the patient-physician relation is the value of direct communication. As such, controlling the opioid epidemic may rely considerably on the ability of the treating surgeon to communicate with patients regarding the indications for and expected duration of opioid consumption after ARCR. Syed et al.32 evaluated 134 patients undergoing ARCR at a single institution, randomized into those receiving opioid-related education preoperatively (68 patients) and those not receiving any education on opioid usage, side effects, dependence, or addiction (66 patients). All patients were provided with the same standardized postoperative pain management protocol and prospectively followed up for 3 months. The authors found that patients receiving preoperative education consumed significantly fewer opioids at the 3-month follow-up assessment and were 2.2 times (odds ratio, 2.19; P = .03) more likely to have discontinued opioids by the end of the follow-up period compared with patients receiving no education. As such, as the surgical specialists with the highest odds of prescribing a narcotic for a noncancer diagnosis,33,34 orthopaedic surgeons have a critical role in alleviating the opioid epidemic. Providing patient education while setting expectations regarding opioid consumption remains a critical component of the preoperative workup as it relates to determining appropriate patient selection.
Limitations
This study was not without limitations. On the basis of our power analysis, this investigation was underpowered to detect even a large effect size, which we largely attribute to funding, as well as patient compliance with completing and returning the pain journals. Prior investigations have shown a history of smoking,20,23 psychiatric conditions,9,24 and osteoporosis35 to affect rotator cuff healing in patients undergoing ARCR, leading to potentially higher pain levels in the postoperative period and prolonged opioid use. Patients with these conditions were not excluded from our investigation. As such, the presence of these factors may have confounded our results. Patients were asked to complete the pain journals on a daily basis to minimize recall bias. However, as all pain scores and opioid consumption were patient reported, there is the potential for under- or over-reporting of pain or opioid consumption, and this cannot be ruled out as a further confounding variable affecting our analysis. Finally, given the scrutiny placed on opioid consumption and the potential for tolerance and abuse, it is possible that patients were inclined to consume fewer tablets, resulting in less variability in the quantity of opioids that would otherwise be consumed.
Conclusions
No significant correlation between increase in individual or overall deltoid compartment pressures after ARCR and postoperative opioid consumption in the immediate postoperative period was found in this study.
Acknowledgment
The authors thank Sunita R. P. Mengers, M.D., for her assistance with data collection and study coordination.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: This study was funded by a grant provided by the Department of Orthopaedic Surgery at University Hospitals Cleveland Medical Center. D.M.K. receives grant support from Arthrex, outside the submitted work; is a paid speaker for DJ Orthopaedics; and receives educational support from Smith & Nephew and Elite Orthopaedics. M.J.S. is a consultant for Stryker and Smith & Nephew, outside the submitted work. J.E.V. is a consultant for Arthrex and DePuy Synthes, outside the submitted work. R.J.G. is a consultant for Stryker, Shoulder Innovations, DJ Orthopaedics, Encore Medical, Wright Medical Technologies, and Tornier, outside the submitted work; receives royalties from Shoulder Innovations; owns stock in Accumed and Genesis Innovation Group; and receives educational support from Rock Medical Orthopaedics. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Chakravarthy B., Shah S., Lotfipour S. Prescription drug monitoring programs and other interventions to combat prescription opioid abuse. West J Emerg Med. 2012;13:422–425. doi: 10.5811/westjem.2012.7.12936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frieden T.R., Houry D. Reducing the risks of relief—The CDC opioid-prescribing guideline. N Engl J Med. 2016;374:1501–1504. doi: 10.1056/NEJMp1515917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manchikanti L., Helm S., II, Fellows B., et al. Opioid epidemic in the United States. Pain Physician. 2012;15(suppl):ES9–ES38. [PubMed] [Google Scholar]
- 4.Morris B.J., Mir H.R. The opioid epidemic: Impact on orthopaedic surgery. J Am Acad Orthop Surg. 2015;23:267–271. doi: 10.5435/JAAOS-D-14-00163. [DOI] [PubMed] [Google Scholar]
- 5.Volkow N.D., McLellan T.A., Cotto J.H., Karithanom M., Weiss S.R. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305:1299–1301. doi: 10.1001/jama.2011.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kidner C.L., Mayer T.G., Gatchel R.J. Higher opioid doses predict poorer functional outcome in patients with chronic disabling occupational musculoskeletal disorders. J Bone Joint Surg Am. 2009;91:919–927. doi: 10.2106/JBJS.H.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morris B.J., Zumsteg J.W., Archer K.R., Cash B., Mir H.R. Narcotic use and postoperative doctor shopping in the orthopaedic trauma population. J Bone Joint Surg Am. 2014;96:1257–1262. doi: 10.2106/JBJS.M.01114. [DOI] [PubMed] [Google Scholar]
- 8.Uquillas C.A., Capogna B.M., Rossy W.H., Mahure S.A., Rokito A.S. Postoperative pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25:1204–1213. doi: 10.1016/j.jse.2016.01.026. [DOI] [PubMed] [Google Scholar]
- 9.Westermann R.W., Anthony C.A., Bedard N., et al. Opioid consumption after rotator cuff repair. Arthroscopy. 2017;33:1467–1472. doi: 10.1016/j.arthro.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Colvin A.C., Egorova N., Harrison A.K., Moskowitz A., Flatow E.L. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94:227–233. doi: 10.2106/JBJS.J.00739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang R., Wang S., Wang Y., Qin X., Sun Y. Systematic review of all-arthroscopic versus mini-open repair of rotator cuff tears: A meta-analysis. Sci Rep. 2016;6 doi: 10.1038/srep22857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly B.C., Constantinescu D.S., Vap A.R. Arthroscopic and open or mini-open rotator cuff repair trends and complication rates among American Board of Orthopaedic Surgeons Part II examinees (2007-2017) Arthroscopy. 2019;35:3019–3024. doi: 10.1016/j.arthro.2019.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Buess E., Steuber K.U., Waibl B. Open versus arthroscopic rotator cuff repair: A comparative view of 96 cases. Arthroscopy. 2005;21:597–604. doi: 10.1016/j.arthro.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Kang L., Henn R.F., Tashjian R.Z., Green A. Early outcome of arthroscopic rotator cuff repair: A matched comparison with mini-open rotator cuff repair. Arthroscopy. 2007;23:573–582. doi: 10.1016/j.arthro.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Cho N.S., Ha J.H., Rhee Y.G. Patient-controlled analgesia after arthroscopic rotator cuff repair: Subacromial catheter versus intravenous injection. Am J Sports Med. 2007;35:75–79. doi: 10.1177/0363546506291632. [DOI] [PubMed] [Google Scholar]
- 16.Ciccone W.J., II, Busey T.D., Weinstein D.M., Walden D.L., Elias J.J. Assessment of pain relief provided by interscalene regional block and infusion pump after arthroscopic shoulder surgery. Arthroscopy. 2008;24:14–19. doi: 10.1016/j.arthro.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Kasten P., Keil C., Grieser T., Raiss P., Streich N., Loew M. Prospective randomised comparison of arthroscopic versus mini-open rotator cuff repair of the supraspinatus tendon. Int Orthop. 2011;35:1663–1670. doi: 10.1007/s00264-011-1262-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warner J.J., Tetreault P., Lehtinen J., Zurakowski D. Arthroscopic versus mini-open rotator cuff repair: A cohort comparison study. Arthroscopy. 2005;21:328–332. doi: 10.1016/j.arthro.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Williams G., Jr., Kraeutler M.J., Zmistowski B., Fenlin J.M., Jr. No difference in postoperative pain after arthroscopic versus open rotator cuff repair. Clin Orthop Relat Res. 2014;472:2759–2765. doi: 10.1007/s11999-014-3715-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cuff D.J., O'Brien K.C., Pupello D.R., Santoni B.G. Evaluation of factors affecting acute postoperative pain levels after arthroscopic rotator cuff repair. Arthroscopy. 2016;32:1231–1236. doi: 10.1016/j.arthro.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 21.Kim C.W., Kim J.H., Kim D.G. The factors affecting pain pattern after arthroscopic rotator cuff repair. Clin Orthop Surg. 2014;6:392–400. doi: 10.4055/cios.2014.6.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menendez M.E., Ring D., Bateman B.T. Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res. 2015;473:2402–2412. doi: 10.1007/s11999-015-4173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naimark M., Robbins C.B., Gagnier J.J., et al. Impact of smoking on patient outcomes after arthroscopic rotator cuff repair. BMJ Open Sport Exerc Med. 2018;4 doi: 10.1136/bmjsem-2018-000416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ravindra A., Barlow J.D., Jones G.L., Bishop J.Y. A prospective evaluation of predictors of pain after arthroscopic rotator cuff repair: Psychosocial factors have a stronger association than structural factors. J Shoulder Elbow Surg. 2018;27:1824–1829. doi: 10.1016/j.jse.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 25.Sabesan V.J., Petersen-Fitts G.R., Sweet M.C., Katz D.L., Lima D.J.L., Whaley J.D. The impact of preoperative opioid use on outcomes after arthroscopic rotator cuff repair. JSES Open Access. 2018;2:155–158. doi: 10.1016/j.jses.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams B.T., Redlich N.J., Mickschl D.J., Grindel S.I. Influence of preoperative opioid use on postoperative outcomes and opioid use after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28:453–460. doi: 10.1016/j.jse.2018.08.036. [DOI] [PubMed] [Google Scholar]
- 27.Wylie J.D., Suter T., Potter M.Q., Granger E.K., Tashjian R.Z. Mental health has a stronger association with patient-reported shoulder pain and function than tear size in patients with full-thickness rotator cuff tears. J Bone Joint Surg Am. 2016;98:251–256. doi: 10.2106/JBJS.O.00444. [DOI] [PubMed] [Google Scholar]
- 28.De Wachter J.D., Glabbeek F.V., van Riet R., Van Leemput W., Vermeyen K., Somville J. Surrounding soft tissue pressuring during shoulder arthroscopy. Acta Orthop Belg. 2005;71:521–527. [PubMed] [Google Scholar]
- 29.Svendsen K., Borchgrevink P., Fredheim O., Hamunen K., Mellbye A., Dale O. Choosing the unit of measurement counts: The use of oral morphine equivalents in studies of opioid consumption is a useful addition to defined daily doses. Palliat Med. 2011;25:725–732. doi: 10.1177/0269216311398300. [DOI] [PubMed] [Google Scholar]
- 30.Kose K.C., Tezen E., Cebesoy O., et al. Mini-open versus all-arthroscopic rotator cuff repair: Comparison of the operative costs and the clinical outcomes. Adv Ther. 2008;25:249–259. doi: 10.1007/s12325-008-0031-0. [DOI] [PubMed] [Google Scholar]
- 31.Pearsall A.W.I.V., Ibrahim K.A., Madanagopal S.G. The results of arthroscopic versus mini-open repair for rotator cuff tears at mid-term follow-up. J Orthop Surg Res. 2007;2:24. doi: 10.1186/1749-799X-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Syed U.A.M., Aleem A.W., Wowkanech C., et al. Neer Award 2018: The effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: A prospective, randomized clinical trial. J Shoulder Elbow Surg. 2018;27:962–967. doi: 10.1016/j.jse.2018.02.039. [DOI] [PubMed] [Google Scholar]
- 33.Levy B., Paulozzi L., Mack K.A., Jones C.M. Trends in opioid analgesic-prescribing rates by specialty, U.S., 2007-2012. Am J Prev Med. 2015;49:409–413. doi: 10.1016/j.amepre.2015.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ringwalt C., Gugelmann H., Garrettson M., et al. Differential prescribing of opioid analgesics according to physician specialty for Medicaid patients with chronic noncancer pain diagnoses. Pain Res Manag. 2014;19:179–185. doi: 10.1155/2014/857952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chung S.W., Oh J.H., Gong H.S., Kim J.Y., Kim S.H. Factors affecting rotator cuff healing after arthroscopic repair: Osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39:2099–2107. doi: 10.1177/0363546511415659. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.