Abstract
The purpose of this study was to provide information on cysts of the anterior cruciate ligament (ACL) of the knee. This included an anatomical and radio-anatomical reminder of the cruciate ligaments of the knee, along with details of the epidemiology, etiopathogenesis, anatomical risk factors, clinical presentation, differential diagnosis, and treatment of ACL cysts. A retrospective analysis was conducted, involving the review of 7 radioclinical records from the medical imaging department of Ibn Sina University Hospital in Rabat, covering a period of 3 years (2018-2020), during which 7 cases of ACL cysts were diagnosed. The results revealed that ACL cysts are a rare condition, frequently detected incidentally during the assessment of meniscal lesions. Symptoms commonly include knee pain and limited mobility, and MRI is considered the diagnostic modality of for distinguishing between simple fluid-filled cysts and infiltrative cysts, as well as for ruling out other differential diagnoses. Treatment options include radio-guided infiltration puncture and arthroscopic resection.
Keywords: Knee, Anterior cruciate ligament, Cyst, Rare condition
Introduction
Intra-articular cystic formations affecting the knee joint are considered a rare condition [1]. These cysts can be intra-synovial, such as meniscal cysts, or extra-synovial, like cysts of the cruciate ligaments and Hoffa's fat pad cysts [2]. Cruciate ligament mucoid cysts are a particularly rare form, with an incidence of less than 1% [3]. They mainly affect the anterior cruciate ligament (ACL) [4] and were first described by Caan in 1924 through dissection studies [5]. While the prevalence of ACL cysts ranges from 0.2% to 1.2% [6,7], they often remain asymptomatic and often go unnoticed [4]. When symptoms do occur, they typically manifest as gradual-onset knee pain and limited mobility [8]. Various etiopathogenic theories have been put forward, but none has been definitively validated [6]. The diagnosis is generally established using MRI, which enables differentiation between infiltrative lesions, also known as mucoid degeneration, and purely cystic lesions [9]. Treatment options vary depending on the nature of the cyst [8] and may involve arthroscopic surgery or scan/ultrasound-guided aspiration [7]. In a retrospective study, 7 cases of ACL cysts were recorded over a 3-year period (2018-2020). The objective of our study is to demonstrate the MRI features of ACL cystic formations and to clarify the role of this imaging modality in the diagnostic management of these cysts.
Cases presentation
Patient 1
A 30-year-old patient, with no previous history, presented with 5 months of mechanical pain in the left knee, with no evidence of trauma (Fig. 1). Clinical examination revealed pain on active and passive mobilization of the knee. No patellar shock was noted, meniscal signs were negative and the Lachman test was negative. The standard radiograph was normal, and a complementary MRI showed the presence of a mucoid cyst of the ACL in hypersignal with multilocular cystic expansion at the level of its femoral insertion.
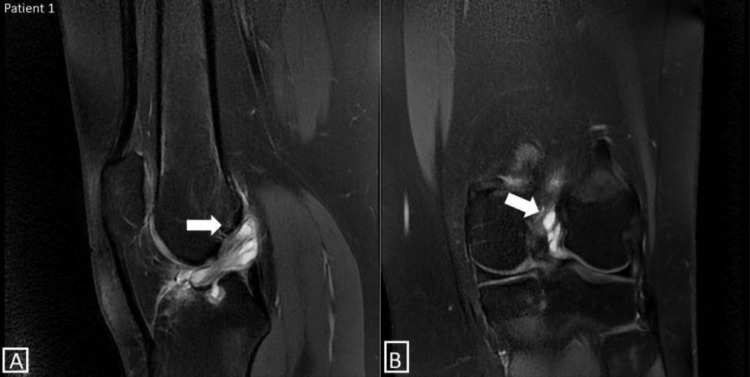
Fig. 1.
Sagittal (A) and coronal (B) proton density MRI images with fat saturation show a mucocele cyst of the anterior cruciate ligament (ACL) with hyperintense signal and multilocular cystic expansion at its femoral insertion.
Patient 2
A 52-year-old patient, type 2 diabetic on treatment, consulted 8 months after a trauma to the left knee causing chronic mechanical pain (Fig. 2). The patient had been on analgesic treatment, but when his symptoms did not improve, he came for a consultation. Clinical examination revealed tenderness on palpation of the joint space, with pain on flexion-extension, particularly on hyperflexion. Patellar impingement was felt, but ligament testing was normal. MRI showed taut, continuous ligament fibers with the presence of a mucoid cyst.
Fig. 2.
MRI of the right knee. (A) Sagittal proton density-weighted MRI slice showing a swollen ACL with an overall hyperintense signal. The fibers are stretched from the tibia to the femur, each maintaining their physiological signal, discreetly individualized in PD fat sat hypo-intensity, showing the “celery stalk sign.” Note the presence of an associated mucocele cyst. (B) Coronal proton density MRI slice showing the ACL with an overall hyperintense signal, without discontinuity of its fibers, consistent with mucoid degeneration. Note the lateral femoral notch sign, related to the mucoid inclusion at the point of ligament insertion.
Patient 3
A 49-year-old patient with no previous history presented with posterior pain in the left knee, which had been present for 12 months (Fig. 3). Clinical examination revealed slight tenderness of the joint space; flexion-extension was preserved and painless; and ligament testing was normal. A standard radiograph was ordered and found to be unremarkable, followed by an MRI scan showing a small cystic formation in the ACL tent in T1 hyposignal and fat sat PD hypersignal.
Fig. 3.
Sagittal MRI slices in T1-weighted (A) and proton density with fat saturation (B) sequences showing a small cystic formation in the ACL with T1 hypointensity and PD fat sat hyperintensity. (C) Coronal proton density MRI section with fat saturation showing a cyst in the ACL with a hyperintense signal.
Patient 4
A 25-year-old patient suffering from chronic mechanical pain in the left knee following trauma during a soccer match (Fig. 4). Clinical examination revealed a meniscal syndrome with possible but painful extension. Ligament testing was normal. No specific abnormalities were noted on standard radiography. On MRI, however, there was a cystic formation of the ACL tent in T1 hyposignal and PD fat sat hypersignal.
Fig. 4.
Sagittal MRI slices in T1-weighted (A) and proton density with fat saturation (B) sequences showing a cystic formation in the ACL with T1 hypointensity and PD fat sat hyperintensity. (C) Coronal proton density MRI slice with fat saturation showing the ACL cyst with a hyperintense signal. Note: a poorly defined hyperintense signal abnormality in the femoral shaft, suggesting a unicameral bone cyst.
Patient 5
A 29-year-old patient with no previous history consulted for a meniscus syndrome that had been evolving for 10 months, following a trauma sustained during a soccer match (Fig. 5). After initial consultation, a standard radiograph was ordered, which proved normal, and the patient was put on analgesic medication. The evolution was marked by the absence of improvement, which motivated the patient to consult again. Clinical examination revealed painful hyperextension with a preserved flexion-extension arc. There was no patellar impingement and ligament testing was normal. On MRI, a cystic formation was found in hyposignal T1, hypersignal PD fat sat, above the tibial insertion of the ACL, associated with patellar chondropathy.
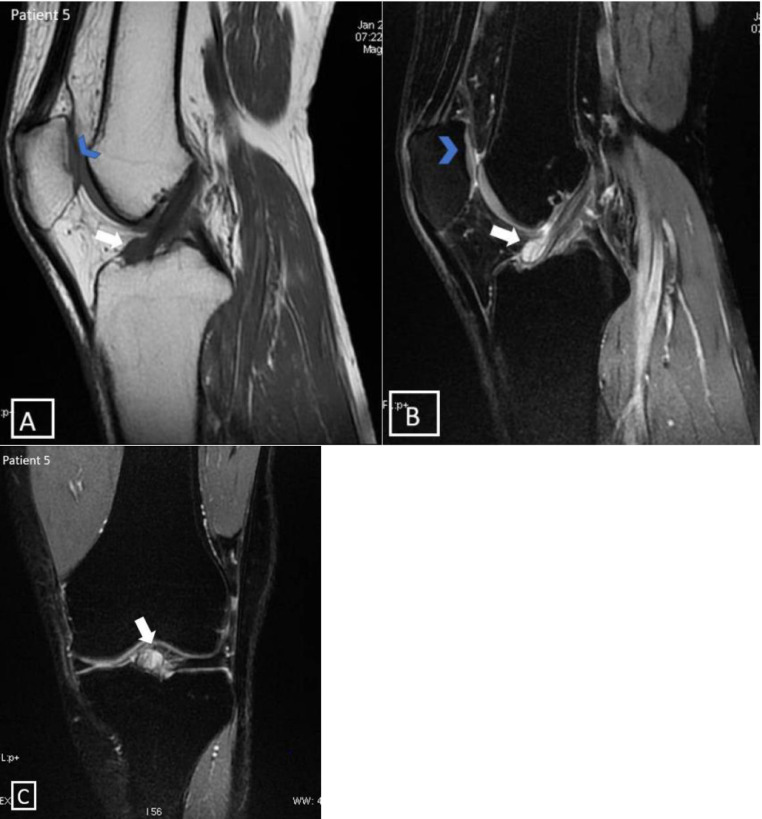
Fig. 5.
MRI of the left knee. Sagittal MRI slices in T1-weighted sequence (A) and proton density with fat saturation (B), showing a small cystic formation in T1 low signal intensity and PD fat sat high signal intensity, located above the tibial insertion of the ACL. Note: T1 low signal intensity, PD fat sat high signal intensity in the patellar cartilage reflecting patellar chondropathy. (C) Coronal MRI slice in proton density-weighted sequence with fat saturation showing hyperintense signal of the LCA cyst.
Patient 6
A 68-year-old woman, treated for hypertension and left gonarthrosis, presented with a meniscal syndrome with recent locked knee, associated with increased gonalgia (Fig. 6). Clinical examination revealed diffuse pain on palpation of the joint space, with possible extension that became painful at 150°. Ligament testing was normal and patellar impingement was absent. The standard radiograph showed a pinched joint space associated with osteophytes and geodes related to his gonarthrosis. Additional MRI was ordered, showing an ACL tent cyst in T1 hyposignal and fat sat PD hypersignal.
Fig. 6.
MRI of the right knee. Sagittal MRI slices in T1-weighted sequence (A) and proton density with fat saturation (B) showing a cyst in the ACL with T1 low intensity signal and PD fat sat high-intensity signal. Note: Bone spurs of the patella with subchondral geodes.
Patient 7
A 56-year-old patient presented with chronic gonalgia of the posterior aspect of the right knee (Fig. 7). Clinical examination revealed tenderness on palpation of the posterior aspect of the knee, with no limitation of flexion-extension. There was no meniscal syndrome, and ligament evaluation was normal. Standard radiography revealed a pinched of the femorotibial joint space with bone spurs. MRI revealed fusiform thickening of the ACL associated with a popliteal cyst and a femoral notch due to mucoid inclusion.
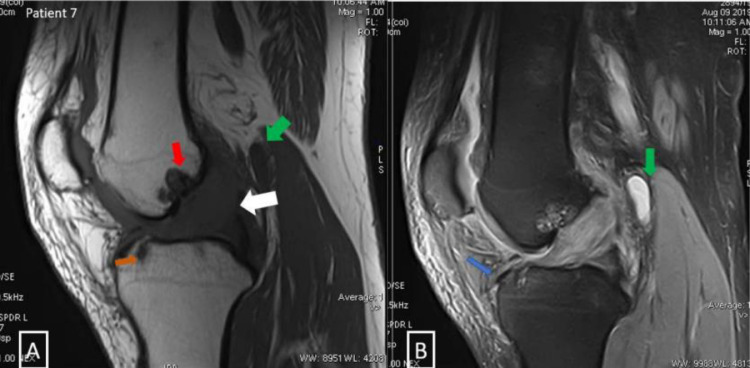
Fig. 7.
(A) Sagittal MRI slice in T1-weighted sequence showing a spindle-shaped thickening of the ACL with an intermediate signal. (B) Sagittal MRI slice in proton density with fat saturation showing a swollen LCA in high-intensity signal with a few fibers in low-intensity signal.
Discussion
Two types of cystic lesions of the ACL can be distinguished by MRI: purely cystic lesions, which include mucoid cysts; and infiltrative lesions, also known as hypertrophy, mucoid degeneration, or infiltrative pseudocyst of the ACL [9]. Mucoid cysts of the knee are neo-formed cystic lesions consisting of one or multiple cavities containing highly viscous mucoid fluid and surrounded by a pauci-cellular fibro-conjunctive wall [10,11].
Mucoid degeneration of the ACL is a poorly known degenerative condition characterized by diffuse infiltration of mucoid-like substance interspersed within the ACL tissue.
This condition is distinct from pure cystic lesions such as synovial cysts and mucoid cysts [12].
ACL cysts are rare and their etiopathogenesis is not well understood [13], although several theories have been suggested [6]. Two hypotheses have been put forward, both suggesting an association with prior trauma [9,14], as these cysts tend to develop in areas exposed to continuous mechanical stress, often in patients with a history of knee trauma [13].
The first hypothesis suggests that the cyst is formed from synovial tissue and joint fluid through the dehiscence of ligament fibers [8]. The second theory holds that the cyst develops as a result of a degenerative process in the connective tissue, involving mucoid degeneration and the formation of micro-cysts, which are secondary to partial ruptures of the ACL [8].
ACL cysts are generally asymptomatic. However, when symptoms do occur, they tend to develop gradually and are nonspecific [15]. Common clinical symptoms associated with ACL cysts include deep knee pain and limited joint movement [4].
Magnetic resonance imaging (MRI) is considered the gold standard for diagnosing and evaluating of ACL cyst lesions [16]. The characteristic features of an ACL mucoid cyst on MRI include a well-defined fusiform formation with regular contours, which can be located either inside or on the surface of the ligament [17], [18], [19]. These cysts may appear as unilocular or multilocular structures and exhibit a fluid signal with T1 hypo-intensity, T2 hyperintensity, and fat suppression (PD fat sat) [4].
The identification of mucoid degeneration of the ACL using MRI is based on diagnostic criteria defined by Bergin et al. [20]: an overall T1-T2 hyperintensity of the ACL, an overall increase in the volume of the ACL, clear T2 visualization of ligament fibers, continuing from the tibial to the femoral insertion.
There are 2 potential treatment options for ACL cysts: a conservative approach consisting of an aspiration with infiltration guided by CT or ultrasound, or a surgical approach involving arthroscopic resection [7].
MRI distinction between fluid-filled and infiltrative forms of ACL cyst is crucial in determining the appropriate therapeutic strategy [8]. Puncture is recommended for well-localized, unilocular cystic forms. However, it may not be suitable for deep localization [21]. In the case of infiltrative cysts, surgery is recommended, including complete excision of the cyst and, if necessary, total resection of the ACL.
Conclusion
ACL cysts are rare and usually cause knee pain and limited mobility. MRI is considered the gold standard due to its high sensitivity and specificity. It plays a crucial role in distinguishing between simple cysts and infiltrative cysts, as well as ruling out other potential differential diagnoses like a partial tear in the ACL.
Treatment options for ACL cysts include imagery-guided infiltrative puncture, which is recommended for fluid-filled cysts, and arthroscopic resection, which is typically performed for infiltrative cysts. The choice of treatment method will depend on the specific characteristics of the cyst and the patient's condition. The prognosis and outcome of ACL cysts are influenced by the selected treatment approach, as well as individual factors.
Authors’ contributions
All authors have read and approved the final manuscript.
Availability of data and materials
The datasets used and analyzed during the study are available from the corresponding author.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Footnotes
Acknowledgment: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing Interests: The authors declare that there is no conflict of interest.
References
- 1.Fillingham YA, Coe MP, Hellman M, Haughom B, Adeniran AO, Sparks MB. Report of ganglion cyst in the anterior cruciate ligament of a 6-year-old child. Knee. 2013;20(2):144–147. doi: 10.1016/j.knee.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Marin F, Albert J-D, Jrad Z, Le Nouvel J-B, Guénard C, Duvauferrier R. Imagerie des kystes synoviaux et mucoides des genoux de l'adulte. Rev Rhumat. 2006;73:633–641. [Google Scholar]
- 3.McLaren DB, Buckwalter KA, Vahey TN. The prevalence and significance of cyst-like changes at the cruciate ligament attachments in the knee. Skelet Radiol. 1992;21:365–369. doi: 10.1007/BF00241814. [DOI] [PubMed] [Google Scholar]
- 4.Jamal L, Cherrad T, Bousbaa H, Zejjari H, Ouahidi M, Amhajji L, Rachid K. Kyste mucoïde du ligament croisé antérieur: à propos d'un cas. Pan Afr Med J. 2016;24:331. doi: 10.11604/pamj.2016.24.331.10196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caan P. Zystenbildung (ganglion) im Ligamentum cruciatum ant genus. Deut Zeitschr Z Chir. 1924;186:403–408. [Google Scholar]
- 6.Bui-Mansfield LT, Youngberg RA. Intra-articular ganglion in the knee: prevalence, presentation, etiology and management. Am J Roentgenol. 1997;168:123–127. doi: 10.2214/ajr.168.1.8976934. [DOI] [PubMed] [Google Scholar]
- 7.Kim MG, Kim BH, Choi JA, Lee NJ, Chung KB, Choi YS, et al. Intra-articular ganglion cysts of the knee: clinical and MR imaging features. Eur Radiol. 2001;11:834–840. doi: 10.1007/s003300000713. [DOI] [PubMed] [Google Scholar]
- 8.Demey G., Servien E., Aït Si Selmi T., Neyret P. Les kystes du ligament croisé antérieur : à propos de 24 cas. J Traumatol Sport. 2007;24:11–17. [Google Scholar]
- 9.Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: coexistence and clinical correlation. AJR Am J Roentgenol. 2004;182(5):1283–1287. doi: 10.2214/ajr.182.5.1821283. [DOI] [PubMed] [Google Scholar]
- 10.Ouali Idrissi M, Che´rif Idrissi El ganouni N, Basraoui D, Abkari I. Imagerie de la pathologie synoviale du genou. J Traumatol Sport. 2011;28:174–184. [Google Scholar]
- 11.Courroy JB, Folinais D, Thelen PH. Le kyste infiltrant du ligament croise´ antérieur : a` propos de 23 cas. J Traumatol Sport. 2002;19:68–75. [Google Scholar]
- 12.Moricea A., Couprya A., Lintzb F., Roberta H. ∗ Plastie de réduction de la dégénérescence mucoïde du ligament croisé antérieur : résultats cliniques et laximétriques : à propos de 23 cas. Rev Chir Orthop Traumatol. 2013;99:579–583. [Google Scholar]
- 13.Vilchez F, Erquicia J, Pelfort X, Carlos Monllau J. Symptomatic ganglions in the knee joint, report of three cases and literature review. Acta Orthop Mex. 2009;23(4):223–227. [PubMed] [Google Scholar]
- 14.Krudwig WK, Schulte KK, Heinemann C. Intra-articular ganglion cysts of the knee joint: a report of 85 cases and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2004;12:123–129. doi: 10.1007/s00167-003-0372-9. [DOI] [PubMed] [Google Scholar]
- 15.Sumen Y, Ochi M, Deie M, Adachi N, Ikuta Y. Ganglion cysts of the cruciate ligaments detected by MRI. Int Orthop. 1999;23:58–60. doi: 10.1007/s002640050305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ouali Idrissi M., Alga S., Cherif Idrissi El Ganouni N. Aspects IRM du kyste mucoide du ligament croise´ antérieur. Feuill Radiol. 2013;53:386–387. [Google Scholar]
- 17.Liu SH, Osti L, Mirzayan R. Ganglion cysts of the anterior cruciate ligament: a case report and review of the literature. Arthroscopy. 1994;10:110–112. doi: 10.1016/s0749-8063(05)80303-2. [DOI] [PubMed] [Google Scholar]
- 18.Kang CN, Lee SB, Kim SW. Symptomatic ganglion cyst within the substance of the anterior cruciate ligament. Arthroscopy. 1995;11:612–615. doi: 10.1016/0749-8063(95)90141-8. [DOI] [PubMed] [Google Scholar]
- 19.Roeser WM, Tsai E. Ganglion cysts of the anterior cruciate ligament. Arthroscopy. 1994;10:574–575. doi: 10.1016/s0749-8063(05)80017-9. [DOI] [PubMed] [Google Scholar]
- 20.Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: coexistence and clinical correlation. AJR Am J Roentgenol. 2004;182:1283–1287. doi: 10.2214/ajr.182.5.1821283. [DOI] [PubMed] [Google Scholar]
- 21.Antonacci VP, Foster T, Fenlon H, Harper K, Eustace S. Technical report: CT-guided aspiration of anterior cruciate ligament ganglion cysts. Clin Radiol. 1998;53(10):771–773. doi: 10.1016/s0009-9260(98)80323-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the study are available from the corresponding author.