Abstract
Objectives
To perform a systematic review on the use of magnetic resonance imaging (MRI) of the abdomen to evaluate clinically suspected appendicitis in the general adult population. We examined the diagnostic accuracy, the reported trends of MRI use, and the factors that affect the utility of MRI abdomen, including study duration and cost-benefits.
Methods
We conducted a systematic literature search on PubMed, MEDLINE, Embase, Web of Science, and Cochrane Library databases. We enrolled primary studies investigating the use of MRI in diagnosing appendicitis in the general adult population, excluding studies that predominantly reported on populations not representative of typical adult appendicitis presentations, such as those focusing on paediatric or pregnant populations.
Results
Twenty-seven eligible primary studies and 6 secondary studies were included, totaling 2,044 patients from eight countries. The sensitivity and specificity of MRI for diagnosing appendicitis were 96% (95% CI: 93–97%) and 93% (95% CI: 80–98%), respectively. MRI can identify complicated appendicitis and accurately propose alternative diagnoses. The duration of MRI protocols in each primary study ranged between 2.26 and 30 minutes, and only one study used intravenous contrast agents in addition to the non-contrast sequences. Decision analysis suggests significant benefits for replacing computed tomography (CT) with MRI and a potential for cost reduction. Reported trends in MRI usage showed minimal utilisation in diagnostic settings even when MRI was available.
Conclusions
MRI accurately diagnoses appendicitis in the general adult population and improves the identification of complicated appendicitis or alternative diagnoses compared to other modalities using a single, rapid investigation.
Keywords: MRI, Magnetic resonance imaging, Appendicitis, Appendicectomy, Appendix, Systematic review
Introduction
General surgeons encounter clinically suspected appendicitis most commonly in adults,1 with an estimated 87% of appendicitis cases occurring in individuals aged over 15.2 Surgeons reviewing patients suspected of acute appendicitis often utilise imaging to enhance diagnostic certainty and prevent unnecessary invasive procedures.3 The rate of imaging use and the choice of modality varies according to local practice.4–7
Traditionally, imaging has been sparingly used for suspected appendicitis in the UK and Australia.4,5 In one Australian report, only 25% of patients received imaging, with this figure being mostly ultrasound.8 Although reliance on the clinical acumen of surgeons can help avoid the issues surrounding the routine use of CT scans, minimal use of imaging results in an increased length of stay5 and a higher negative appendicectomy rate.9 Clinical scoring systems can improve outcomes such as length of stay,10 but still result in a negative appendicectomy rate of 10%.11
In some countries, such as the USA or the Netherlands, imaging is routinely employed for assessing possible appendicitis cases in the general adult population with imaging rates reported at 99%.6,7 Computed tomography (CT) is a popular modality for diagnosing acute appendicitis, due to its high sensitivity (95%; 95% CI: 93–96%) and specificity (94%; 95% CI: 92–95%).12 However, ionising radiation from CT scans increases the cumulative risk of carcinogenesis in patients.13,14 The incidence rate ratio of leukaemia and myelodysplasia for patients that have undergone CT of the abdomen and pelvis is 3.24 (95% CI: 2.17–4.84).15 Furthermore, the incidence of contrast-induced nephropathy nears 25% in patients with pre-existing renal impairments.16 Intravenous contrast is a common allergic and anaphylactic reaction trigger, and can also cause fluid extravasation and hazardous interactions with common medications such as metformin.17 Ultrasound is an alternative, radiation-free imaging modality also commonly employed to detect acute appendicitis, with superior safety when compared to CT.18,19 However, ultrasound is limited by a low sensitivity (69%; 95% CI: 59–78%) and specificity (81%; 95% CI: 73–88%) when evaluating suspected appendicitis, with inconclusive results in nearly 48% of cases.20,21
A US study reported a system-wide trend towards significantly increased use of CT in emergency departments (ED) for assessing patients with abdominal pain, without a corresponding increase in detecting surgical emergencies.22 Clinicians and patients are understandably keen to reduce the number of missed appendicitis cases and improve the diagnosis of other conditions. However, the increasing use of CT inevitably increases patient exposure to ionising radiation and intravenous contrast agents. An ideal alternative imaging modality would be affordable and rapid with high sensitivity and specificity for all common causes of abdominal pain whilst not exposing patients to ionising radiation and contrast agents.
Magnetic resonance imaging (MRI) has been widely used as an alternative imaging modality for diagnosing acute appendicitis in paediatric or pregnant patients where avoiding ionising radiation is a priority.23,24 The benefit of avoiding radiation exposure and contrast agents can be extended to the general adult population, although the relatively high cost and limited availability of MRI have historically remained as impediments to widespread use for these purposes.25,26
A 2021 Cochrane Review reported that rapid MRI abdomen (with a total study time lasting 30 minutes or less) may entail numerous additional advantages that may help overcome its perceived high cost, including a low false-positive rate and a low negative appendicectomy rate.26 Appendicitis is a high incidence condition, estimated at 100 (95% CI: 91–110) per 100,000 person-years,27 so substituting contrast-enhanced CT with MRI in this patient population has the potential for significant system-wide improvements in patient safety and outcomes.
Existing literature about MRI use for suspected appendicitis often includes high proportions of pregnant and paediatric patients, well above their proportions of the overall population, which is understandable given that these populations have led the way in the use of MRI. The anatomical and physiological differences between demographic groups may cause significant bias if the results from those subgroups are generalised to the adult population. The assessment of the utility of abdominal MRI outside these groups requires a dedicated study of the general (non-pregnant) adult population. The 2021 Cochrane Review examined the diagnostic accuracy of MRI for appendicitis26 in a population including large numbers of pregnant and paediatric patients, as well as reporting on the general adult subgroup. However, the scope of this meta-analysis was limited to reporting the pooled sensitivity and specificity of MRI, and two additional primary studies have been published since. We aimed to provide an updated systematic review on the use of MRI to assess clinically suspected appendicitis in the general adult population by reviewing the diagnostic accuracy and other knowledge gaps, such as the ability of MRI to identify complicated appendicitis, to identify alternative diagnoses, the reported trends of use, time requirements, cost-benefits, and potential impact on decision analyses.
Method
We conducted our literature search in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines28 using PubMed, Ovid MEDLINE, Ovid Embase + Embase Classic, Web of Science, and Cochrane Library with the search keywords “magnetic resonance imaging”, “MRI”, “appendicitis”, “appendix”, “appendicectomy”, and “appendectomy”. The studies were compiled and merged using the Zotero reference management software, and then duplicates, retractions, and studies lacking abstracts were removed. The remaining articles were screened for relevance to the use of MRI for detecting appendicitis.
After the initial screening, we excluded articles that met the exclusion criteria, formulated a priori. Studies were excluded if full texts could not be found, if they were case reports (1–2 patients), if they lacked explicit patient inclusion and exclusion criteria, or if they were written in languages other than English. Review articles, opinion pieces, book reviews, and study protocols were also excluded. Secondary studies were not excluded and their bibliographies were reviewed as an ancestral search to identify any further primary studies.
Two authors reviewed the remaining list of potentially eligible studies to determine which studies satisfied the inclusion criteria, formulated a priori. Studies were included if they reported the results of MRI scans evaluating suspected appendicitis cases in populations predominated by non-pregnant adults. Studies that reported only on pregnant or paediatric patients were excluded by this method.
The following information was then extracted from each study: name of the first author, year published, national location, study type, study duration, study setting, reference standard, the total number of patients, number of patients that underwent appendicectomy, prevalence of appendicitis, proportion of women, mean age, age range, number of subgroup patients, true positives, false positives, false negatives, true negatives, sensitivity, specificity, number of histologically proven appendicitis, number of alternative diagnoses from MRI results, number of cases with alternative diagnosis as final diagnosis, MRI sequence, and MRI scanning time. If available or possible, the positive predictive value (PPV) and the negative predictive value (NPV) of reported MRI features for discrimination of complicated from simple appendicitis were extracted or calculated.
The Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) was employed to assess the validity and applicability of the included studies reporting on diagnostic outcomes.29
Results
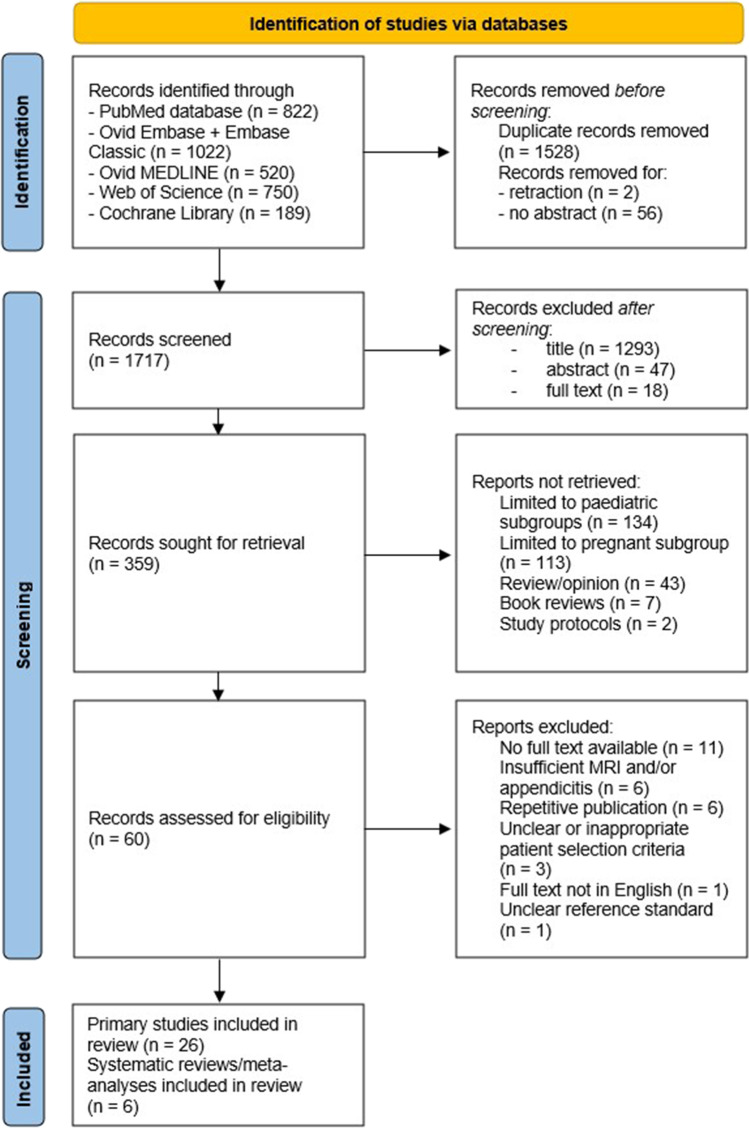
The literature search identified a total of 3,303 studies from across PubMed, EMBASE, MEDLINE, Web of Science, and Cochrane Library databases. Twenty-six primary studies and six secondary studies were selected, as shown in the PRISMA flowchart in Fig. 1. One new primary study was identified in the ancestral searching of the bibliographies of the identified secondary studies, as shown in Fig. 2. In total, there were 33 studies identified by our systematic review.5,26,30–60
Fig. 1.
PRISMA flowchart detailing the literature search results
Fig. 2.
PRISMA flowchart detailing the ancestral search from bibliographies of secondary studies identified
There were no randomised controlled trials (RCT) identified. Of the 33 studies identified in our systematic review, there were 16 primary cohort studies that examined the diagnostic accuracy of MRI for appendicitis with a total of 2,044 patients.30–46 Table 1 summarises the characteristics of these 16 studies, including their study designs, demographic information, and reference standards. All 16 studies employed non-contrast MRI sequences and only one study added a gadolinium contrast sequence to their multiple non-contrast sequences.43 Table 2 shows the MRI characteristics and diagnostic outcomes, which also shows that all the published MRI protocols required no more than 30 minutes for all sequences and that half the published MRI protocols required no more than 15 minutes.
Table 1.
Characteristics of the included primary studies identified in the systematic review that reported on diagnostic outcomes
| First author | Year | Location | Study type | Study duration (months) | Total patients | Mean age (range) (years) | Proportion of women | Number of operative patients | Reference Standard | Reference standard positive appendicitis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S Serinsoz30 | 2021 | Turkey | Retrospective, centre unknown | 24 | 70 | 32 (11–71) | 63% | 40 | Surgical results; unclear for non-operated patients | 37/70 (53%) | ||||||||||
| G Islam31 | 2021 | India | Prospective, single-centre | 18 | 67 | 24 (6–70) | 37% | 39 | Histopath; or clinical follow-up | 45/67 (67%) | ||||||||||
| A Inoue32 | 2019 | Japan | Retrospective, single-centre | 10 | 51 | 35 (6–90) | 53% | 25 | Surgery; or clinical follow-up and CT | 35/51 (69%) | ||||||||||
| M Repplinger33 | 2018 | USA | Prospective, single-centre | 30 | 198 | 32 (12–81) | 58% | Not reported | Expert panel; Histopath or clinical follow-up | 64/198 (32%) | ||||||||||
| S Byott34 | 2016 | England | Prospective, single-centre | 60 | 468 | Median 27 (7–59) | 74% | 116 | Surgical, histological, and clinical follow-up | 38/468 (8%) | ||||||||||
| I Petkovska35 | 2016 | USA | Retrospective, single-centre | 24 | 253 | Not reported | Not reported | Not reported | Expert panel; surgical results; or clinical follow-up | 35/253 (14%) | ||||||||||
| H Gielkens36 | 2016 | Netherlands | Prospective, single-centre | 18 | 112 | Median 22 (12–55) | 100% | 51 | Histopath; or clinical follow-up | 29/112 (26%) | ||||||||||
| M Leeuwenburgh37 | 2014 | Netherlands | Prospective, multi-centre | 6 | 223 | 35 (18–84) | 62% | 128 | Expert panel; surgical findings, histopath, and clinical-follow-up | 117/223 (52%) | ||||||||||
| S Avcu38 | 2013 | Turkey | Prospective, single-centre | 12 | 55 | 36 (17–83) | 43% | 40 | Histopath; unclear for non-operated patients | 40/55 (73%) | ||||||||||
| First Author | Year | Location | Study type | Study duration (months) | Total patients | Mean age (range) (years) | Proportion of women | Number of operative patients | Reference Standard | Reference standard positive appendicitis | ||||||||||
| B Zhu39 | 2012 | China | Prospective, single-centre | 24 | 41 | 42 (range not reported) | 56% | 41 | Surgery/histopath | 36/41 (88%) | ||||||||||
| E Inci40 | 2011 | Turkey | Prospective, single-centre | 11 | 119 | 27 (17–72) | 36% | 92 | Histopath; unclear for non-operated patients | 79/119 (66%) | ||||||||||
| E Chabanova41 | 2011 | Denmark | Prospective, single-centre | Not reported | 48 | 37 (18–70) | 60% | 48 | Surgery/histopath | 30/48 (63%) | ||||||||||
| L Cobben42 | 2009 | Netherlands | Prospective, single-centre | 22 | 138 |
Not reported (6–80) |
58% | 64 | Histopath; or clinical follow-up | 62/138 (44.9%) | ||||||||||
| A Singh43 | 2008 | USA | Retrospective, multi-centre | 72 | 67 | 34 (11–69) | 91% | Not reported | Surgical results; unclear for non-operated patients | 12/67 (18%) | ||||||||||
| N Nitta44 | 2005 | Japan | Prospective, single-centre | Not reported | 37 | 37 (16–69) | 51% | 31 | Surgery/histopath; clinical follow-up | 29/37 (43%) | ||||||||||
| L Incesu46 | 1997 | Turkey | Prospective, single-centre | 22 | 60 | 20 (14–71) | 55% | 39 | Surgery/histopath; or clinical follow-up | 34/60 (57%) | ||||||||||
Table 2.
MRI Characteristics and diagnostic outcomes reported by included primary studies
| First author | MRI Sequences | MRI duration (min) | Number of histopatho-logically proven appendicitis | Number of cases of alternative diagnoses from pre-treatment MRI | Number of cases of alternative diagnoses after definitive treatment | TP | FP | FN | TN | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| S Serinsoz30 | DWI ssEPI + FS, T2 TSE, T2 STIR/TIRM | 7 | 37 (52.9%) | Not reported | Not reported | 37 | 3 | 0 | 30 | 100 | 90.9 |
| G Islam31 | T2 and DWI | 14 | 34 (50.7%) | 6 (9.0%) | 6 (9.0%) | 42 | 3 | 3 | 19 | 93.3 | 86.4 |
| A Inoue32 | T2 HASTE and DWI | Not reported | 25 (49.0%) | Not reported | 16 (31.4%) | 31 | 6 | 4 | 10 | 88.6 | 62.5 |
|
M Repplinger (J Harringa)33 |
T2-SS FSE, T1 3D spoiled GRE, DWI | 30 | Not reported | 51 (25.8%) | 54 (27.3%) | 62 | 14 | 2 | 120 | 96.9 | 89.6 |
| S Byott34 a | HASTE | 15 | 36 (7.7%) | 82 (17.5%) | 82 (17.5%) | 34 | 3 | 3 | 428 | 91.9 | 99.3 |
| I Petkovska35 b | multiplanar single-shot T2 ± SPAIR FS | 14 (mean) | Not reported | Not reported | Not reported | 34 | 1 | 1 | 217 | 97.1 | 99.5 |
| H Gielkens36 c | T2 TSE, T1 GRE | 22 | 29 (28.2%) | 22 (21.4%) | Not reported | 25 | 0 | 3 | 75 | 89.3 | 100 |
| M Leeuwenburgh37 | T2 FSE ± FS, DWI | 15 | 114 (51.1%) | 27 (12.1%) | Not reported | 113 | 7 | 4 | 99 | 96.6 | 93.4 |
| S Avcu38 | DWI, bSSFP, STIR | 2.26 | 40 (72.7%) | 0 (0%) | 0 (0%) | 39 | 0 | 1 | 15 | 97.5 | 100 |
| B Zhu39 | T2 FSE, bSSFP + FS | 2.7 | 36 (87.8%) | 5 (12.2%) | 5 (12.2%) | 33 | 0 | 3 | 5 | 91.7 | 100 |
| E Inci40 | T1 FSE, T2 FSE ± FS, DWI | 4 | 79 (66.4%) | Not reported | 7 (5.9%) | 78 | 0 | 1 | 40 | 98.7 | 100 |
| E Chabanova41 d | T1 SE, T2 FSE, STIR | 20 | 30 (62.5%) | 15 (31.3%) | 14 (29.2%) | 25 | 3 | 5 | 15 | 83.3 | 83.3 |
| L Cobben42 | T1 SGRE, T2 FSE, T2 FSE + FS | 20 | 62 (44.9%) | 41 (29.7%) | 42 (30.4%) | 62 | 1 | 0 | 75 | 100 | 98.7 |
| A Singh43 e | T2 SSFSE + FS, T2 FSE + FS, STIR, pre-GAD T1, post-GAD T1 | <25 | 12 (30.0%) | 36 (90.0%) | 37 (92.5%) | 12 | 1 | 0 | 27 | 100 | 96.4 |
| N Nitta44 | T1 SE, T2 FSE, T2 + FS | 20 | 29 (78.4%) | 1 (2.7%) | 8 (21.6%) | 29 | 1 | 0 | 7 | 100 | 87.5 |
| L Incesu46 | T1 SE, T1 CE FS, T2 FS FSE | 25 | 34 (56.7%) | 9 (15.0%) | 11 (18.3%) | 33 | 2 | 1 | 24 | 97.1 | 92.3 |
ssEPI, single-shot echo-planar imaging; bSSFP, balanced steady-state free precession; RARE, rapid acquisition with relaxation enhancement; SPAIR, spectral selection attenuated inversion recovery; SENSE, sequence, sensitivity encoding; BTFE, balanced turbo field echo; SPIR, spectral pre-saturation and inversion recovery; SS-FSE, single shot fast spin echo; FSE, fast spin echo; STIR, short tau inversion recovery; SE, spin echo; DWI, diffusion-weighted imaging; True-FISP, T2-weighted true-fast imaging with steady-state precession; TIRM, turbo inversion-recovery in magnitude; TSE, turbo spin echo; HF, half Fourier; GRE, gradient echo; FLASH, fast low-angle shot; FS, fat-suppressed; HASTE, half-Fourier acquisition single-shot turbo spin echo; GAD, gadolinium
aThe values for sensitivity and specificity were calculated based on the TP, FP, FN, and TN, and are different to the values reported by the study that were calculated with a restriction to the 90 operative patients
bResults restricted to adults aged over 18
cThis study had nine patients with equivocal MRI results, which were excluded from this table
dThe values of sensitivity and specificity for this study are based on MRI interpretations by a surgeon who had 3 years of experience with abdominal MRI
eResults restricted to patients clinically suspected of appendicitis
Six secondary studies were identified26,45,47–50 and all but one50 examined the diagnostic accuracy of MRI in appendicitis—the results of these five secondary studies are summarised in Table 3. The largest of these was the 2021 Cochrane meta-analysis on the diagnostic accuracy of MRI for appendicitis, which calculated the pooled sensitivity (96%; 95% CI: 93–97%) and specificity (93%; 95% CI: 80–98%) for the subgroup of the general non-pregnant adult population.26
Table 3.
Results of meta-analyses on the diagnostic accuracy of MRI for appendicitis
| Author name | Year | Number of total patients | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| N D'Souza26 | 2021 | 7,492 (overall) | 95 (95% CI: 94–97) | 96 (95% CI: 95–97) |
| 1,088 (non-pregnant adults) | 96 (95% CI: 93–97) | 93 (95% CI: 80–98) | ||
| 2,794 (paediatric patients) | 96 (95% CI: 95–97) | 96 (95% CI: 92–98) | ||
| 2,282 (pregnant patients) | 96 (95% CI: 88–99) | 97 (95% CI: 95–98) | ||
| K Eng45 | 2018 | 287 | 89.9 (95% CI: 84.8–93.5) | 93.6 (95% CI: 90.9–95.5) |
| M Repplinger47 | 2016 | 838 | 96.6 (95% CI: 92.3–98.5) | 95.9 (95% CI: 89.4–98.4) |
| E Duke48 | 2016 | 2,665 a | 96 (95% CI: 95–97) | 96 (95% CI: 95–97) |
| R Barger49 | 2010 | 363 | 97 (95% CI: 92–99) | 97 (CI: 94–99) |
aResults combining all paediatric, pregnant, and non-pregnant adults
We identified 12 studies that reported on topics unrelated to diagnostic accuracy.5,50–60 These studies are summarised in Table 4: three reported on trends of MRI use,51,53,55 two were reports about visualisation of the normal appendix,58,59 two were analyses of financial implications,5,60 one was a secondary study comparing simple versus perforated appendicitis using different imaging modalities,50 one reported on MRI to assess treatment response in non-operatively managed appendicitis,52 one was a decision analysis,56 one was a radiologist training report,57 and one was a survey of imaging prioritisation.54
Table 4.
Summary of the studies identified in the systematic review that investigated topics other than the diagnostic accuracy of MRI
| Author | Year | Topic | Finding |
|---|---|---|---|
| W Bom50 | 2020 | The diagnostic accuracy of different imaging modalities for discriminating complicated from simple appendicitis a | The available evidence was not sufficient for conducting a meta-analysis |
| A Agathis51 | 2019 | The trend of MRI use according to the American College of Surgeons database | Of the 11,841 patients that received an appendicectomy in 2016, only 36 adult patients had received MRI |
| O Ozdemir52 | 2018 | The utility of MRI in follow-up assessment | MRI was useful in the follow-up assessment of simple appendicitis cases after initial medical management |
| N D'Souza5 | 2018 | Financial implications of imaging use for suspected appendicitis | The reduction in healthcare cost due to routine imaging was 68% less when using MRI instead of CT |
| V Tan53 | 2017 | The trends of MRI use at 16 Canadian centres | MRI was generally not used for assessing appendicitis in non-pregnant adults in Canada, even at centres having MRI available 24 hours a day |
| M Agapova54 | 2017 | Imaging preferences of U.S. physicians | Radiologists generally preferred contrast-enhanced CT over MRI to assess suspected appendicitis, whilst ED physicians had minimal preference in choosing between contrast-enhanced CT and MRI |
| M Repplinger55 | 2016 | The trend of MRI use at one U.S. academic centre | MRI was never used for evaluating adults suspected of appendicitis between 1992 and 2014 |
| S Kiatpongsan56 | 2014 | Decision analysis on the benefits of MRI use | The advantage of MRI in minimising radiation exposure is substantial only if MRI demonstrates a minimum sensitivity of 91% when specificity is 100%, or minimum specificity of 62% when sensitivity is 100% |
| M Leeuwenburgh57 | 2012 | Training of radiologists for interpreting MRI | Training of radiologists can improve the diagnostic accuracy of MRI for appendicitis |
| J Horowitz58 | 2011 | Visualising normal appendixes | T2-weighted MRI could visualise 80% of normal appendixes |
| P Nikolaidis59 | 2006 | Visualising normal appendixes | The reliability of MRI in visualising normal appendixes was variable |
| M Beinfield60 | 2005 | Costs of MRI use | The costs of MRI varied significantly between 1996 and 2002 |
aThis was a secondary study that investigated MRI, CT, and ultrasound. However, due to the insufficient evidence regarding MRI and ultrasound, meta-analysis was conducted only for CT
Three primary cohort studies were identified that reported on the diagnostic accuracy of MRI in identifying perforated appendicitis, reporting a sensitivity of 57–100% and a specificity 86–100%, respectively.38,46,61 The PPV and NPV of MRI features for discriminating complicated from simple appendicitis are shown in Table 5.
Table 5.
PPV and NPV of individual MRI features for discriminating complicated from simple appendicitis, as identified in the systematic review; for the data reported by Leeuwenburgh et al.,61 the PPV and NPV were calculated to exclude cases without appendicitis, based on the reported values; the data reported by Zhu et al.39 was excluded due to an unusually high prevalence of complicated appendicitis
| MRI feature | PPV | NPV |
|---|---|---|
| Appendiceal diameter > 7 mm61 | 26.3 (30/114) | 100 (2/2) |
| Periappendiceal fat infiltration61 | 26.4 (29/110) | 83.3 (5/6) |
| Periappendiceal fluid61 | 30.7 (27/88) | 89.3 (25/28) |
| Absence of intraluminal air61 | 24.5 (26/106) | 60 (6/10) |
| Appendicolith61 | 30.8 (16/52) | 78.1 (50/64) |
| Extraluminal appendicolith32 | 100 (1/1) | 73.5 (25/34) |
| Appendiceal wall defect32 | 75~85.7 (6/8 ~ 6/7) | 85.2~85.7 (23/27 ~ 24/28) |
| Appendiceal wall destruction61 | 51.9 (14/27) | 82.0 (73/89) |
| Phlegmon32 | 40.9~42.9 (9/22 ~ 9/21) | 92.3~92.9 (12/13 ~ 13/14) |
| Abscess32,61 | 55.6 (10/18), 85.7~100 (6/7 ~ 6/6) | 79.8 (79/99), 85.7~86.2 (24/28 ~ 25/29) |
| Extraluminal free air32,61 | 100 (1/1), 100 (2/2) | 75 (87/116), 75.8 (25/33) |
| Restricted diffusion of appendiceal wall61 | 27.3 (27/99) | 86.7 (13/15) |
| Restricted diffusion of appendiceal lumen61 | 27.9 (24/86) | 82.1 (23/28) |
| Restricted diffusion of focal collections61 | 55.6 (15/27) | 83.9 (73/87) |
Eight primary cohort studies were identified that compared MRI and the reference standard with respect to their ability to identify alternative diagnoses when appendicitis was clinically suspected.31,34,39,42,43,46,62,63 The sensitivity and specificity of MRI for alternative diagnoses ranged between 77.0–100%34,62 and 94.9–100%,34,43 respectively. Seven of these studies additionally reported the data with a restriction to gynaecological pathologies, with the values of sensitivity and specificity ranging between 57.1–100%34,63 and 95.3–100%,34,43 respectively.
Four studies were identified that directly compared MRI with other assessment methods within homogenous populations. Repplinger et al. compared between MRI (sensitivity 96.9%, 95% CI: 88.2–99.5%; specificity 89.6%, 95% CI: 82.8–94.0%) and contrast-enhanced CT (sensitivity 98.4%, 95% CI: 90.5–99.9%; specificity 93.3%, 95% CI: 87.3–96.7%).33 Leeuwenburgh et al. compared between MRI (sensitivity 97%; specificity 93%) and ultrasound with selective use of contrast-enhanced CT (sensitivity 97%; specificity 91%).37 Incesu et al. compared between MRI (sensitivity 97%; specificity 92%) and ultrasound (sensitivity 76%; specificity 88%).46 Inci et al. compared between MRI (sensitivity 99%; specificity 100%) and the Alvarado scoring system (sensitivity 84.2%; specificity 66.7%).64
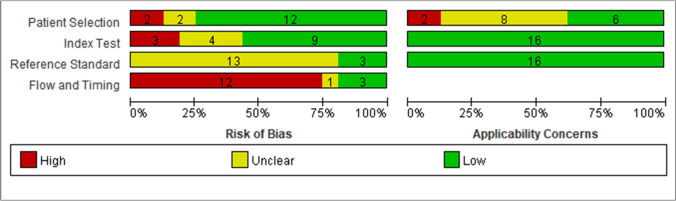
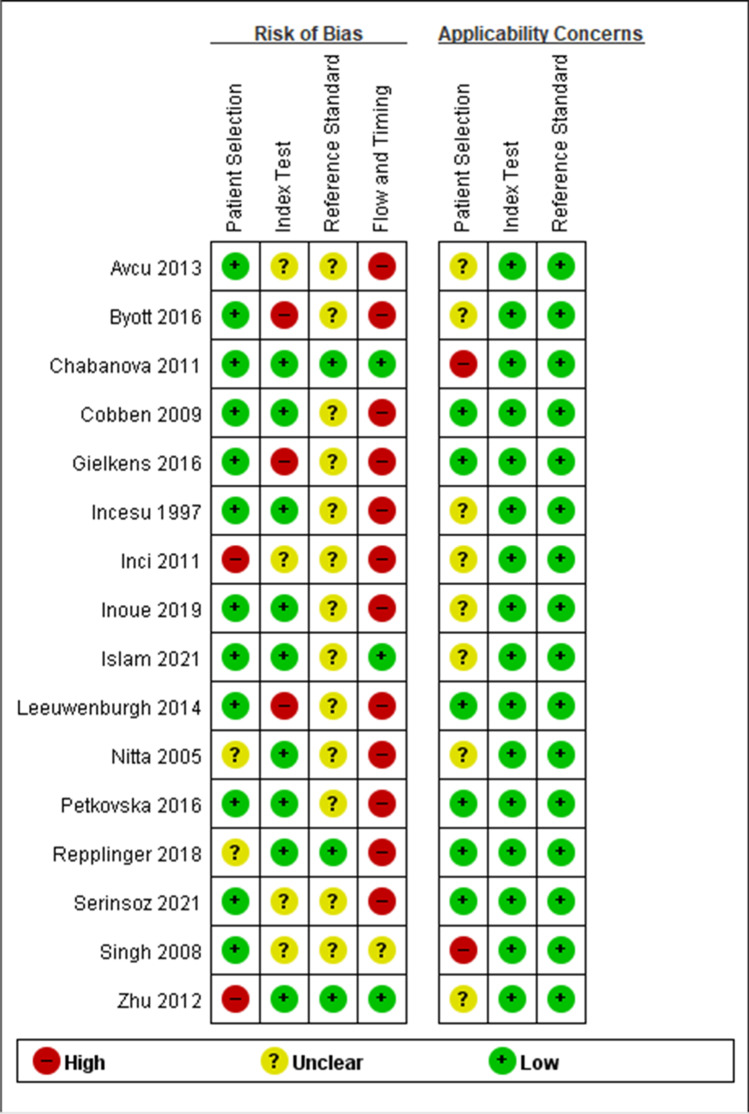
Quality assessment results of the diagnostic accuracy studies are displayed in Figs. 3 and 4. The limitations of primary studies included insufficient descriptions of the reference standard, the employment of composite reference standards, and a significant portion of patients comprising paediatric, pregnant, or both subgroups.
Fig. 3.
QUADAS-2 assessment findings for each domain represented as percentages
Fig. 4.
QUADAS-2 assessment findings for each domain of the diagnostic outcomes studies
Discussion
In this study, we conducted a systematic review of the published literature concerning the use of MRI for evaluating possible appendicitis presentations in the general adult population. To our knowledge, this systematic review is the first to extend beyond the diagnostic accuracy of MRI and provides clinicians with an overview of the value of MRI for diagnosing appendicitis in the general adult population. Not only does MRI have high sensitivity and specificity for diagnosing appendicitis, but it also has a potential role in differentiating simple from complicated appendicitis and in identifying alternative diagnoses that are commonly seen when appendicitis is suspected, such as gynaecological diagnoses.
MRI has a promising diagnostic accuracy for acute appendicitis in the general adult population,26 with clinical parameters similar to CT (sensitivity 95%; 95% CI: 93–96%; specificity 94%; 95% CI: 92–95%)12 and superior to ultrasound (sensitivity 69%; 95% CI: 59–78%; specificity 81%; 95% CI: 73–88%).20 Direct comparisons within homogeneous populations suggested that the diagnostic accuracy of MRI is comparable to contrast-enhanced CT33 or ultrasound with selective use of contrast-enhanced CT,37 and superior to ultrasound46 or the Alvarado scoring system.64 No statistically significant difference exists when comparing MRI with CT or ultrasound for the visualisation of a normal appendix,65 likely due to the paucity of data published.
Five meta-analyses have been published on the diagnostic accuracy of MRI in appendicitis26,45,47–49 with the largest being the 2021 Cochrane Review.26 This study reported the pooled sensitivity and specificity of abdominal MRI separately in three distinct population groups: the pregnant, the paediatric, and the non-pregnant adult population.26 The headline overall (non-subgrouped) results reported on a population that is unrepresentative of the typical population presenting with appendicitis, with large numbers of paediatric patients (2,794), pregnant patients (2,282), and an uncategorised group of mixed patients (1,298). These patient groups combined to far exceed the size of the non-pregnant adult population (1,088 patients), though the diagnostic accuracy of MRI was similar across all subgroups. However, the Cochrane review was limited to the issue of diagnostic accuracy, whereas our paper also aims to cover the other knowledge domains regarding MRI in appendicitis.
The discrimination between simple and complicated appendicitis has significant ramifications on management, as surgeons can choose to medically manage simple appendicitis safely with antibiotics alone.66 Our results show conflicting values of sensitivity and specificity of MRI for identifying complicated appendicitis. This possibly reflects the variations in MRI interpretation criteria used in each study, as certain individual MRI features demonstrated a favorable ability to identify or exclude complicated appendicitis.32,39,44 Still, little evidence currently exists to support the use of MRI to identify perforated appendicitis, as also noted by a 2018 systematic review.50 The sensitivity and specificity of CT for identifying complicated appendicitis range between 28~95% and 71~100%, respectively.50
Our results suggest that the sensitivity of MRI for proposing alternative diagnoses is variable, despite the high specificity of MRI. The range of the reported values of sensitivity was greater when the alternative diagnoses were restricted to gynaecological pathologies. Using MRI to investigate gynaecological pathologies illustrated a significant advantage over CT, given the underwhelming performance of CT for the initial evaluation of adnexal pathologies.67 The variable results on the sensitivity of MRI may be partially attributable to the varying levels of MRI experience of the interpreting radiologists in different studies,34,63 as the sensitivity of MRI interpretation can improve with training.62
The amount of time needed to perform imaging has an obvious impact on the time it takes to diagnose and treat appendicitis. All but one of our studies reported an MRI duration of 25 minutes or less, with half of them reporting 15 minutes or less. Three studies used MRI protocols lasting four minutes or less, demonstrating that MRI for appendicitis can be performed rapidly. Preparation for a typical non-contrast MRI is minimal,68 whereas preparing a patient for CT (typically contrast-enhanced) often takes at least 30 to 60 minutes in clinical practice,69 for reasons such as intravenous cannulation for radiocontrast injection and administration and progression of oral contrast (commonly 1.5 to 2 hours).68,70 The use of contrast agents is common in most CT practices, with at least one contrast agent used over 80% of the time.71,72 By comparison, the MRI protocols used by the primary studies in our systematic review all used non-contrast sequences, with only one study adding a gadolinium contrast sequence, suggesting that contrast use is unnecessary in MRI of the appendix. The literature suggests that MRI is not significantly slower than CT in daily clinical practice, and indeed may be quicker in some scenarios, as was demonstrated with paediatric patients.73 Also, the use of MRI can avoid the need for contrast agents, which are well-recognised as a source of patient morbidity.16,17
Decision analysis shows substantial long-term patient benefit of receiving MRI over CT56 by virtue of avoiding the adverse effects of ionising radiation.26 Routine use of imaging including MRI significantly lowers healthcare costs by reducing the negative appendicectomy rate,42 though this cost reduction is 68% less when using MRI instead of CT.5 The improved identification of simple (versus complicated) appendicitis using MRI38,46 may allow risk stratification and more effective use of non-operative management, thus hypothetically reducing hospital costs, although this has yet to be formally studied. Similarly, MRI detection of gynaecological pathologies avoids the need to use both CT and ultrasound to identify these common differential diagnoses, making MRI potentially less costly in females. However, the exact financial implication of using MRI to assess suspected appendicitis is unclear due to the lack of a direct cost-benefit analysis.
Despite these advantages, an extremely small proportion of non-pregnant adult patients with suspected appendicitis receive MRI imaging in the USA and Canada,51,53,55 even at institutions that have MRI available 24 hours a day.53
Several limitations underlie the published meta-analyses, including the 2021 Cochrane Review. Firstly, the results of these meta-analyses generally do not extend beyond investigating sensitivity, specificity, and heterogeneity. Secondly, the meta-analyses published to date are subject to bias due to the lack of RCTs. A lack of RCTs introduces bias through unmitigated inter-cohort variability and the lack of randomisation or blinding. Thirdly, the generally poor reporting standards of the primary studies compromise the validity of the meta-analyses, as described by the 2021 Cochrane Review.26 Nevertheless, it is arguable that RCTs are unlikely to be funded or conducted given the currently available evidence.
Our systematic review contains multiple limitations. Heterogeneity of patient characteristics and study designs exists between individual primary studies. The presumed greater likelihood of publication of studies with positive conclusions about MRI would bring publication bias. Because the MRI experience of radiologists impacts diagnostic accuracy,74 our conclusions may not be generalised to centres where access to experienced MRI radiologists is limited.
Possible directions for future research may include cost-benefit analysis of MRI for appendicitis and the visualisation rate of the normal appendix given the lack of data in the current literature. More reports on the use of MRI to identify complicated appendicitis or propose alternative diagnoses would help better define the role of MRI in streamlining surgical decision-making in clinical practice.
Conclusion
The diagnostic accuracy of MRI for appendicitis has already been shown to be excellent. Our systematic review identifies the evolving ability of MRI to help differentiate simple and complicated appendicitis or to identify alternative diagnoses, whilst avoiding the adverse effects of CT, such as the use of ionising radiation and the contrast agents. Whether MRI is less costly remains uncertain; however our systematic review demonstrates that MRI can be performed rapidly. Despite these benefits, MRI is rarely used in current clinical practice for the investigation of abdominal pain in adults, but our study suggests it has great potential to markedly benefit the pre-operative decision-making of surgeons treating appendicitis.
Acknowledgements
The following person was involved in reviewing the methodology of this work: Dr. Danette Wright; Department of Surgery, Blacktown and Mount Druitt Hospitals, N.S.W., Australia.
The article processing charge is funded by the Western Sydney University.
Author Contribution
D Kim: project development, data collection & analysis, manuscript writing & editing
Dr. B Woodham: project development, data analysis, manuscript writing & editing
K Chen: data collection, manuscript editing
V Kuganathan: data collection, manuscript editing
Professor M Edye: manuscript editing
Funding
Open Access funding enabled and organised by CAUL and its Member Institutions.
Declarations
Ethical Approval
As this systematic review was a secondary review of studies that were already published, it was exempt from ethical approval of our local institution or the institutional review board (IRB). For the same reason, patient consents were not applicable.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Dongchan Kim, Email: donny.kim100@gmail.com.
Benjamin Luke Woodham, Email: b.woodham@westernsydney.edu.au.
References
- 1.Zingone F, Sultan A, Humes D, West J. Risk of acute appendicitis in and around pregnancy: a population-based cohort study from England. Ann Surg. 2015;261(2):332–7. doi: 10.1097/SLA.0000000000000780. [DOI] [PubMed] [Google Scholar]
- 2.Lin K, Lai K, Yang N, Chan C, Liu Y, Pan R, et al. Epidemiology and socioeconomic features of appendicitis in Taiwan: a 12-year population-based study. World J Emerg Surg. 2015;10:42. doi: 10.1186/s13017-015-0036-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charfi S, Sellami A, Affes A, Yaich K, Mzali R, Boudawara T. Histopathological findings in appendectomy specimens: a study of 24,697 cases. Int J Colorectal Dis. 2014;29(8):1009–12. doi: 10.1007/s00384-014-1934-7. [DOI] [PubMed] [Google Scholar]
- 4.Campbell G, Fletcher D, Glasson W, Horsburgh B, Johnson M, Malisano L. Surgical interventions. In Duggan A, ed. The Second Australian Atlas of Healthcare Variation, vol. 1, 1st ed. Sydney: Australian Commission on Safety and Quality in Healthcare, 2017, pp293-304.
- 5.D’Souza N, Marsden M, Bottomley S, Nagarajah N, Scutt F, Toh S. Cost-effectiveness of routine imaging of suspected appendicitis. Ann R Coll Surg Engl. 2018;100(1):47–51. doi: 10.1308/rcsann.2017.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lahaye M, Lambregts D, Mutsaers E, Beets-Tan R, Essers B, Breukink S, et al. Mandatory imaging cuts costs and reduces the rate of unnecessary surgeries in the diagnostic work-up of patients suspected of having appendicitis. Eur Radiol. 2015;25(5):1464–70. doi: 10.1007/s00330-014-3531-0. [DOI] [PubMed] [Google Scholar]
- 7.Tseng J, Cohen T, Melo N, Alban R. Imaging utilization affects negative appendectomy rates in appendicitis: An ACS-NSQIP study. Am J Surg. 2019;217(6):1094–8. doi: 10.1016/j.amjsurg.2018.12.072. [DOI] [PubMed] [Google Scholar]
- 8.Brockman S, Scott S, Guest G, Stupart D, Ryan S, Watters D. Does an acute surgical model increase the rate of negative appendicectomy or perforated appendicitis? ANZ J Surg. 2013;83(10):744–7. doi: 10.1111/ans.12211. [DOI] [PubMed] [Google Scholar]
- 9.Boonstra P, van Veen R, Stockmann H. Less negative appendectomies due to imaging in patients with suspected appendicitis. Surg Endosc. 2015;29(8):2365–70. doi: 10.1007/s00464-014-3963-2. [DOI] [PubMed] [Google Scholar]
- 10.Coleman J, Carr W, Rogers T. The Alvarado score should be used to reduce emergency department length of stay and radiation exposure in select patients with abdominal pain. J Traum Acute Care Surg. 2018;84(6):946–50. doi: 10.1097/TA.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 11.Memon Z, Irfan S, Fatima K, Iqbal M, Sami W. Acute appendicitis: Diagnostic accuracy of Alvarado scoring system. Asian J Surg. 2013;36(4):144–9. doi: 10.1016/j.asjsur.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Rud B, Vejborg T, Rappeport E, Reitsma J, Willie-Jorgensen P. Computed tomography for diagnosis of acute appendicitis in adults. Cochrane Database Syst Rev. 2019;2019(11):009977. doi: 10.1002/14651858.CD009977.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith-Bindman R, Lipson J, Marcus R, Kim K, Mahesh M, Gould R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078–86. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miglioretti D, Johnson E, Williams A, Greenlee R, Weinmann S, Solberg L, et al. Pediatric computed tomography and associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700–7. doi: 10.1001/jamapediatrics.2013.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matthews J, Forsythe A, Brady Z, Butler M, Goergen S, Byrnes G, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. doi: 10.1136/bmj.f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simone B, Ansaloni L, Sartelli M, Gaiani F, Leandro G, Angelis G, et al. Is the risk of contrast-induced nephropathy a real contraindication to perform intravenous contrast enhanced computed tomography for non-traumatic acute abdomen in emergency surgery department?. Acta Biomed 2018;89(9-S):158–72. [DOI] [PMC free article] [PubMed]
- 17.Rose T, Choi J. Intravenous imaging contrast media complications: The basics that every clinician needs to know. Am J Med. 2015;128(9):943–9. doi: 10.1016/j.amjmed.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 18.Gorter R, Eker H, Gorter-Stam M, Abis G, Acharya A, Ankersmit M, et al. Diagnosis and management of acute appendicitis EAES consensus development conference 2015. Surg Endosc. 2016;30(11):4668–90. doi: 10.1007/s00464-016-5245-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mostbeck G, Adam E, Nielsen M, Claudon M, Clevert D, Nicolau C, et al. How to diagnose acute appendicitis: ultrasound first. Insights Imaging. 2016;7(2):255–63. doi: 10.1007/s13244-016-0469-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giljaca V, Nadarevic T, Poropat G, Nadarevic V, Stimac D. Diagnostic accuracy of abdominal ultrasound for diagnosis of acute appendicitis: systematic review and meta-analysis. World J Surg. 2017;41(3):693–700. doi: 10.1007/s00268-016-3792-7. [DOI] [PubMed] [Google Scholar]
- 21.Pelin M, Paquette B, Revel L, Landecy M, Bouveresse S, Delabrousse E. Acute appendicitis: Factors associated with inconclusive ultrasound study and the need for additional computed tomography. Diagn Interv Imaging. 2018;99(12):809–14. doi: 10.1016/j.diii.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Pines J. Trends in the rates of radiography use and important diagnoses in emergency department patients with abdominal pain. Med Care. 2009;47(7):782–6. doi: 10.1097/MLR.0b013e31819748e9. [DOI] [PubMed] [Google Scholar]
- 23.Moore M, Kulaylat A, Hollenbeak C, Engbrecht B, Dillman J, Methratta S. Magnetic resonance imaging in pediatric appendicitis: a systematic review. Pediatr Radiol. 2016;46(6):928–39. doi: 10.1007/s00247-016-3557-3. [DOI] [PubMed] [Google Scholar]
- 24.Dewhurst C, Beddy P, Pedrosa I. MRI evaluation of acute appendicitis in pregnancy. J Magn Reson Imaging. 2013;37(3):566–75. doi: 10.1002/jmri.23765. [DOI] [PubMed] [Google Scholar]
- 25.Siewert R. Availability and accessibility of diagnostic imaging equipment around Australia. Canberra: Parliament of Australia: Senate Community Affairs References Committee, 2018.
- 26.D’Souza N, Hicks G, Beable R, Higginson A, Rud B. Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis. Cochrane Database Syst Rev. 2021;12(12):CD012028. doi: 10.1002/14651858.CD012028.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferris M, Quan S, Kaplan B, Molodecky N, Ball C, Chernoff G, et al. The global incidence of appendicitis: A systematic review of population-based studies. Ann Surg. 2017;266(2):237–41. doi: 10.1097/SLA.0000000000002188. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):1000097. [PMC free article] [PubMed] [Google Scholar]
- 29.Whiting P, Rutjes A, Westwood M, Mallett S, Deeks J, Reitsma J, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 30.Serinsoz S, Akturk R. Can diffusion-weighted imaging be a gold standard method for acute appendicitis? A comparative study. Iran J Radiol. 2021;18(3):e113603. [Google Scholar]
- 31.Islam G, Yadav T, Khera P, Sureka B, Garg P, Elhence P, et al. Abbreviated MRI in patients with suspected acute appendicitis in emergency: a prospective study. Abdom Radiol (NY) 2021;46(11):5114–24. doi: 10.1007/s00261-021-03222-5. [DOI] [PubMed] [Google Scholar]
- 32.Inoue A, Furukawa A, Nitta N, Takaki K, Ota S, Zen Y, et al. Accuracy, criteria, and clinical significance of visual assessment on diffusion-weighted imaging and apparent diffusion coefficient quantification for diagnosing acute appendicitis. Abdom Radiol (NY) 2019;44(10):3235–45. doi: 10.1007/s00261-019-02180-3. [DOI] [PubMed] [Google Scholar]
- 33.Repplinger M, Pickhardt P, Robbins J, Kitchin D, Ziemlewicz T, Hetzel S, et al. Prospective comparison of the diagnostic accuracy of MR imaging versus CT for acute appendicitis. Radiology. 2018;288(2):467–75. doi: 10.1148/radiol.2018171838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Byott S, Harris I. Rapid acquisition axial and coronal T2 HASTE MR in the evaluation of acute abdominal pain. Eur J Radiol. 2016;85(1):286–90. doi: 10.1016/j.ejrad.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Petkovska I, Martin D, Covington M, Urbina S, Duke E, Daye Z, et al. Accuracy of unenhanced MR imaging in the detection of acute appendicitis: Single-institution clinical performance review. Radiology. 2016;279(2):451–60. doi: 10.1148/radiol.2015150468. [DOI] [PubMed] [Google Scholar]
- 36.des Plantes C, van Veen M, van der Palen J, Klaase J, Gielkens H, Geelkerken R. The effect of unenhanced MRI on the surgeons’ decision-making process in females with suspected appendicitis. World J Surg. 2016;40(12):2881–7. doi: 10.1007/s00268-016-3626-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leeuwenburgh M, Wiarda B, Wiezer M, Vrouenraets B, Gratama J, Spilt A, et al. Comparison of imaging strategies with conditional contrast-enhanced CT and unenhanced MR imaging in patients suspected of having appendicitis: A multicenter diagnostic performance study. Radiology. 2013;268(1):135–43. doi: 10.1148/radiol.13121753. [DOI] [PubMed] [Google Scholar]
- 38.Avcu S, Cetin F, Arslan H, Kemik O, Dulger A. The value of diffusion-weighted imaging and apparent diffusion coefficient quantification in the diagnosis of perforated and nonperforated appendicitis. Diagn Interv Radiol. 2013;19(2):106–10. doi: 10.4261/1305-3825.DIR.6070-12.1. [DOI] [PubMed] [Google Scholar]
- 39.Zhu B, Zhang B, Li M, Xi S, Yu D, Ding Y. An evaluation of a superfast MRI sequence in the diagnosis of suspected acute appendicitis. Quant Imaging Med Surg. 2012;2(4):280–7. doi: 10.3978/j.issn.2223-4292.2012.12.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Inci E, Kilickesmez O, Hocaoglu E, Aydin S, Bayramoglu S, Cimilli T. Utility of diffusion-weighted imaging in the diagnosis of acute appendicitis. Eur Radiol. 2011;21(4):768–75. doi: 10.1007/s00330-010-1981-6. [DOI] [PubMed] [Google Scholar]
- 41.Chabanova E, Balslev I, Achiam M, Nielsen Y, Adamsen S, Gocht-Jensen P, et al. Unenhanced MR imaging in adults with clinically suspected acute appendicitis. Eur J Radiol. 2011;79(2):206–10. doi: 10.1016/j.ejrad.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 42.Cobben L, Groot I, Kingma L, Coerkamp E, Puylaert J, Blickman J. A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on outcome of appendectomy. Eur Radiol. 2009;19(5):1175–83. doi: 10.1007/s00330-008-1270-9. [DOI] [PubMed] [Google Scholar]
- 43.Singh A, Desai H, Novelline R. Emergency MRI of acute pelvic pain: MR protocol with no oral contrast. Emerg Radiol. 2009;16(2):133–41. doi: 10.1007/s10140-008-0748-8. [DOI] [PubMed] [Google Scholar]
- 44.Nitta N, Takahashi M, Furukawa A, Murata K, Mori K, Fukushima M. MR imaging of the normal appendix and acute appendicitis. J Magn Reson Imaging. 2005;21(2):156–65. doi: 10.1002/jmri.20241. [DOI] [PubMed] [Google Scholar]
- 45.Eng K, Abadeh A, Ligocki C, Lee Y, Moineddin R, Adams-Webber T, et al. Acute appendicitis: A meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology. 2018;288(3):717–27. doi: 10.1148/radiol.2018180318. [DOI] [PubMed] [Google Scholar]
- 46.Incesu L, Coskun A, Selcuk MB, Akan H, Sozubir S, Bernay F. Acute appendicitis: MR imaging and sonographic correlation. AJR Am J Roentgenol. 1997;168(3):669–74. doi: 10.2214/ajr.168.3.9057512. [DOI] [PubMed] [Google Scholar]
- 47.Repplinger M, Levy J, Peethumnongsin E, Gussick M, Svenson J, Golden S, et al. Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J Magn Reson Imaging. 2016;43(6):1346–54. doi: 10.1002/jmri.25115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Duke E, Kalb B, Arif-Tiwari H, Daye Z, Gilbertson-Dahdal D, Keim S, et al. A systematic review and meta-analysis of diagnostic performance of MRI for evaluation of acute appendicitis. AJR Am J Roentgenol. 2016;206(3):508–17. doi: 10.2214/AJR.15.14544. [DOI] [PubMed] [Google Scholar]
- 49.Barger R, Nandalur K. Diagnostic performance of magnetic resonance imaging in the detection of appendicitis in adults: A meta-analysis. Acad Radiol. 2010;17(10):1211–6. doi: 10.1016/j.acra.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 50.Bom W, Bolmers M, Gans S, van Rossem C, van Geloven A, Bossuyt P, et al. Discriminating complicated from uncomplicated appendicitis by ultrasound imaging, computed tomography or magnetic resonance imaging: systematic review and meta-analysis of diagnostic accuracy. BJS Open. 2021;5(2):zraa030. doi: 10.1093/bjsopen/zraa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Agathis A, Miller M, Divino C. National trends in diagnostic imaging for appendicitis: A cross-sectional analysis using NSQIP. Am Surg. 2019;85(6):625–30. [PubMed] [Google Scholar]
- 52.Ozdemir O, Metin N, Metin Y, Kalcan S, Kupeli A. Contribution of diffusion-weighted magnetic resonance imaging in the follow-up of uncomplicated acute appendicitis: Initial results. Iran J Radiol. 2018;15(1):e56033. [Google Scholar]
- 53.Tan V, Patlas M, Katz D. Imaging trends in suspected appendicitis-a Canadian perspective. Emerg Radiol. 2017;24(3):249–54. doi: 10.1007/s10140-016-1472-4. [DOI] [PubMed] [Google Scholar]
- 54.Agapova M, Bresnahan B, Linnau K, Garrison L, Higashi M, Kessler L, et al. Using the analytic hierarchy process for prioritizing imaging tests in diagnosis of suspected appendicitis. Acad Radiol. 2017;24(5):530–7. doi: 10.1016/j.acra.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 55.Repplinger M, Weber A, Pickhardt P, Rajamanickam V, Svenson J, Ehlenbach W, et al. Trends in the use of medical imaging to diagnose appendicitis at an academic medical center. J Am Coll Radiol. 2016;13(9):1050–6. doi: 10.1016/j.jacr.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kiatpongsan S, Meng L, Eisenberg J, Herring M, Avery L, Kong C, et al. Imaging for appendicitis: Should radiation-induced cancer risks affect modality selection? Radiology. 2014;273(2):472–82. doi: 10.1148/radiol.14132629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leeuwenburgh M, Wiarda B, Bipat S, Nio C, Bollen T, Kardux J, et al. Acute appendicitis on abdominal MR images: Training readers to improve diagnostic accuracy. Radiology. 2012;264(2):455–63. doi: 10.1148/radiol.12111896. [DOI] [PubMed] [Google Scholar]
- 58.Horowitz J, Nikolaidis P, Hammond N, Wood C, Gabriel H, Miller F. Taking advantage of chemical shift imaging: Using opposed-phase images to locate the normal appendix on MR. Clin Imaging. 2011;35(6):424–30. doi: 10.1016/j.clinimag.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 59.Nikolaidis P, Hammond N, Marko J, Miller F, Papanicolaou N, Yaghmai V. Incidence of visualization of the normal appendix on different MRI sequences. Emerg Radiol. 2006;12(5):223–6. doi: 10.1007/s10140-006-0489-5. [DOI] [PubMed] [Google Scholar]
- 60.Beinfeld M, Gazelle G. Diagnostic imaging costs: Are they driving up the costs of hospital care? Radiology. 2005;235(3):934–9. doi: 10.1148/radiol.2353040473. [DOI] [PubMed] [Google Scholar]
- 61.Leeuwenburgh M, Wiezer M, Wiarda B, Bouma W, Phoa S, Stockmann H, et al. Accuracy of MRI compared with ultrasound imaging and selective use of CT to discriminate simple from perforated appendicitis. Br J Surg. 2014;101(1):e147–55. doi: 10.1002/bjs.9350. [DOI] [PubMed] [Google Scholar]
- 62.Harringa J, Bracken R, Davis J, Mao L, Kitchin D, Robbins J. Prospective evaluation of MRI compared with CT for the etiology of abdominal pain in emergency department patients with concern for appendicitis. J Magn Reson Imaging. 2019;50(5):1651–8. doi: 10.1002/jmri.26728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Harringa J, Bracken R, Markhardt B, Ziemlewicz T, Lubner M, Chiu A, et al. Magnetic resonance imaging versus computed tomography and ultrasound for the diagnosis of female pelvic pathology. Emerg Radiol. 2021;28(4):789–96. doi: 10.1007/s10140-021-01923-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Inci E, Hocaoglu E, Aydin S, Palabiyik F, Cimilli T, Turhan A, et al. Efficiency of unenhanced MRI in the diagnosis of acute appendicitis: Comparison with Alvarado scoring system and histopathological results. Eur J Radiol. 2011;80(2):253–8. doi: 10.1016/j.ejrad.2010.06.037. [DOI] [PubMed] [Google Scholar]
- 65.Kim D, Suh C, Yoon H, Kim J, Jung A, Lee J, et al. Visibility of normal appendix on CT, MRI, and sonography: A systematic review and meta-analysis. AJR Am J Roentgenol. 2018;211(3):W140–50. doi: 10.2214/AJR.17.19321. [DOI] [PubMed] [Google Scholar]
- 66.Sallinen V, Akl E, You J, Agarwal A, Shoucair S, Vandvik P, et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656–67. doi: 10.1002/bjs.10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Iyer V, Lee S. MRI, CT, and PET/CT for ovarian cancer detection and adnexal lesion characterization. AJR Am J Roentgenol. 2010;194(2):311–21. doi: 10.2214/AJR.09.3522. [DOI] [PubMed] [Google Scholar]
- 68.Streit U, Uhlig J, Lotz J, Panahi B, Hosseini A. Analysis of core processes of the MRI workflow for improved capacity utilization. Eur J Radiol. 2021;138:109648. doi: 10.1016/j.ejrad.2021.109648. [DOI] [PubMed] [Google Scholar]
- 69.Mun S, Ernst R, Chen K, Oto A, Shah S, Mileski W. Rapid CT diagnosis of acute appendicitis with IV contrast material. Emerg Radiol. 2006;12(3):99–102. doi: 10.1007/s10140-005-0456-6. [DOI] [PubMed] [Google Scholar]
- 70.Macari M, Balthazar E. The acute right lower quadrant: CT evaluation. Radiol Clin North Am. 2003;41(6):1117–36. doi: 10.1016/s0033-8389(03)00101-5. [DOI] [PubMed] [Google Scholar]
- 71.O’Malley M, Halpern E, Mueller P, Gazelle G. Helical CT protocols for the abdomen and pelvis: a survey. AJR Am J Roentgenol. 2000;175(1):109–13. doi: 10.2214/ajr.175.1.1750109. [DOI] [PubMed] [Google Scholar]
- 72.Hill B, Johnson S, Owens E, Gerber J, Senagore A. CT scan for suspected acute abdominal process: impact of combinations of IV, oral, and rectal contrast. World J Surg. 2010;34(4):699–703. doi: 10.1007/s00268-009-0379-6. [DOI] [PubMed] [Google Scholar]
- 73.Martin J, Mathison D, Mullan P, Otero H. Secondary imaging for suspected appendicitis after equivocal ultrasound: time to disposition of MRI compared to CT. Emerg Radiol. 2018;25(2):161–8. doi: 10.1007/s10140-017-1570-y. [DOI] [PubMed] [Google Scholar]
- 74.Leeuwenburgh M, Wiarda B, Jensch S, van Es H, Hein Stockmann, Gratama J, et al. Accuracy and interobserver agreement between MR-non-expert radiologists and MR-experts in reading MRI for suspected appendicitis. Eur J Radiol. 2014;83:103–10. doi: 10.1016/j.ejrad.2013.09.022. [DOI] [PubMed] [Google Scholar]