Abstract
Purpose
Siblings of probands with depressive and anxiety disorders are at increased risk for psychopathology, but little is known about how risk factors operate within families to increase psychopathology for siblings. We examined the additional impact of psychosocial risk factors in probands—on top of or in combination with those in siblings—on depressive/anxious psychopathology in siblings.
Methods
The sample included 636 participants (Mage = 49.7; 62.4% female) from 256 families, each including a proband with lifetime depressive and/or anxiety disorders and their sibling(s) (N = 380 proband-sibling pairs). Sixteen psychosocial risk factors were tested. In siblings, depressive and anxiety disorders were determined with standardized psychiatric interviews; symptom severity was measured using self-report questionnaires. Analyses were performed with mixed-effects models accounting for familial structure.
Results
In siblings, various psychosocial risk factors (female gender, low income, childhood trauma, poor parental bonding, being single, smoking, hazardous alcohol use) were associated with higher symptomatology and likelihood of disorder. The presence of the same risk factor in probands was independently associated (low income, being single) with higher symptomatology in siblings or moderated (low education, childhood trauma, hazardous alcohol use)—by reducing its strength—the association between the risk factor and symptomatology in siblings. There was no additional impact of risk factors in probands on likelihood of disorder in siblings.
Conclusion
Our findings demonstrate the importance of weighing psychosocial risk factors within a family context, as it may provide relevant information on the risk of affective psychopathology for individuals.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00127-023-02432-0.
Keywords: Siblings, Familial clustering, Depression, Anxiety, Psychosocial risk
Introduction
One of the strongest risk factors for the onset of depressive and anxiety disorders is a family history of these disorders [1, 2]. A two- to three-fold increased risk of the disorders is found for siblings of probands with depressive and anxiety disorders as compared to individuals without affected relatives [3–5]. However, despite their increased risk for psychopathology, siblings from the same at-risk family can differ substantially from one another in psychological functioning [6, 7]. Consistent with this, we showed in a previous study that proband-sibling resemblance in several psychopathology-related features (i.e. symptoms, social/cognitive vulnerabilities, personality traits) was only mild to moderate [8]. Although a large body of evidence exists for the association between several psychosocial risk factors (e.g. female gender, socioeconomic deprivation, social isolation, poor parental bonding, adverse events, smoking, alcohol (ab)use, physical inactivity) and high risk for depressive and anxiety disorders [9–21], little is known about how these risk factors operate within families to increase psychopathology for at-risk siblings. Siblings’ increased risk for psychopathology may depend on the presence of such risk factors in their affected proband, either by also being present in the proband (e.g. an additional ‘vicarious’ effect) [22] or by being absent in the proband while being present in the sibling (e.g. the feeling of ‘being the black sheep’ in the family) [23–25]. This may even extend to sociodemographic risk factors such as higher age and female gender: for instance, rumination seems to be ‘contagious’ especially among older and same-sex female sibling pairs potentially due to the stronger emotional bonds and social learning/sharing [26–29]. Co-rumination, in turn, has been found to be associated with affective psychopathology [30, 31]. Identifying how psychosocial risk factors of poor mental health in siblings of affected probands operate within families may help identifying potential mechanisms explaining why some siblings develop a depressive and anxiety disorder, whereas others do not.
While a large number of studies have investigated the familial aggregation of depressive and anxious psychopathology, only a few have examined the impact of not only considering psychosocial risk factors within at-risk siblings, but also within their affected proband, on increasing psychopathology in at-risk siblings. Findings were mixed as to whether the individual risk for psychopathology is increased if risk factors in a relative are also present or if risk factors in a relative are absent. A larger neighborhood socioeconomic deprivation [32], higher childhood emotional maltreatment [33], and poorer parental bonding [34–37] in an individual as compared to their sibling(s) was found to be associated with more severe depressive symptoms of that individual. Results were mixed for age and gender, with some studies finding associations of similarity (vs. dissimilarity) in female gender and age with similarity in depressive/anxious psychopathology [4, 38], while other studies found no added impact of taking into account the gender/age of an individual’s sibling for their risk for psychopathology [5, 39, 40]. Moreover, available studies have mainly been limited to investigate the degree but not the direction of proband-sibling (dis)similarity of risk factors [4, 5, 38, 40, 41] and mainly focused on sociodemographic and early life adversity risk factors, but not on a wider variety of psychosocial risk factors (e.g. also including recent life adversity and lifestyle-related factors).
The present study examined how a broad range of established psychosocial risk factors for depression/anxiety operate within families to explain interindividual differences in psychopathology between siblings of probands with depressive/anxiety disorders. The main aim was to disentangle and quantify the effect of the presence of a risk factor in the proband, by testing whether this (i) had a unique contribution for psychopathology in the sibling, over-and-above the presence of this risk factor in the sibling, and/or (ii) modified the association between this risk factor and psychopathology in the sibling.
Methods
Study sample
Participants were from the Netherlands Study of Depression and Anxiety (NESDA), an ongoing longitudinal cohort study (2004-present) investigating the long-term course and consequences of depressive and anxiety disorders. A detailed description of the NESDA study design and sampling procedure has been reported elsewhere [42]. During the 9-year follow-up (2014–2017), full-biological siblings of NESDA participants with a lifetime depressive and/or anxiety disorder were additionally recruited for the NESDA family study (see Van Sprang et al. [8] for inclusion criteria and sampling procedure). The study sample included 636 participants from 256 unique families: 256 lifetime affected probands and their 380 siblings (N = 380 proband-sibling pairs). The present study used data for probands assessed at the 9-year follow-up of NESDA, at the time of recruitment and assessment of siblings. The study protocol was approved by the ethical committee of participating universities, and all respondents provided written informed consent.
Measurements
Outcome measures in sibling
The presence of lifetime DSM-IV-TR [43] diagnoses of depressive (i.e. major depressive disorder and dysthymia) and anxiety disorders (i.e. generalized anxiety disorder, panic disorder with or without agoraphobia, social phobia, and agoraphobia only) was determined using the Composite Interview Diagnostic Instrument (CIDI, lifetime version 2.1) [44].
Past week severity and number of symptoms was measured with the Inventory of Depressive Symptomatology-Self Report (IDS) [45] for depression and with the Beck Anxiety Inventory (BAI) [46] for anxiety. As the IDS and BAI showed a large overlap (multilevel1 correlation r = 0.71, 95% CI 0.67–0.75, t(623) = 25.28, p < 0.001), IDS and BAI scores were standardized and averaged into an overall IDS/BAI score to reflect number and severity of current depressive and/or anxiety symptoms.
Psychosocial risk factors in probands and siblings
Sociodemographics
Sociodemographic risk factors included higher age (in years; i.e. longer exposure time-frame) [47, 48], female gender, low education (i.e. reversed years of education), and low income defined as gross annual income ≤ €33,600 (i.e. income below average in 2014–2017 in the Netherlands) [49].
Life adversity and lifestyle
Early life adversity included childhood trauma and poor parental bonding. The Childhood Trauma Questionnaire-Short Form2 (CTQ) [50] was used to assess childhood trauma before the age of 16 (subscales: sexual, physical, and emotional abuse, and physical and emotional neglect). The perception of the relationship between participants and their mother (i.e. maternal bonding) and father (i.e. paternal bonding) before the age of 16 was assessed using the shortened 16-item version of the Parental Bonding Instrument (PBI) [51].
Recent life adversity and lifestyle-related risk factors included current unemployment, living alone, being single (i.e. not married or in a steady relationship), small social network, past-year negative life events, smoking status (yes/no), hazardous alcohol use, and physical inactivity. Participants were considered to have a small social network if the total number of relatives, friends, and close acquaintances with whom they have regular and important contact was ≤ 5. The List of Threatening Experiences (LTE) was used to assess the total number of past-year exposures to two types of negative life events: (i) independent events, which are unlikely to be influenced by the person (e.g. death of a loved one) and (ii) dependent events, which are likely, but do not have to be, influenced by a person (e.g. job loss) [52, 53]. Following the WHO guidelines [54] for the Alcohol Use Disorders Identification Test (AUDIT) [55], hazardous alcohol use was defined as having an AUDIT sum-score ≥ 8 for participants aged < 65 years and, given that the effects of alcohol vary with average body weight and differences in metabolism, as having an AUDIT sum-score ≥ 7 for participants aged ≥ 65 years. Physical activity was measured using the Metabolic Equivalent of Task (MET) score, which was derived from the International Physical Activity Questionnaire (IPAQ) [56], and represented the total number of MET-minutes per week of walking, moderate, and vigorous activities divided by 1000. In the analyses, reversed MET-scores were used reflecting risk associated with physical inactivity.
Statistical analyses
The associations between outcomes in sibling and explanatory variables in siblings and probands were estimated with linear (current symptom severity) and logistic (presence of lifetime psychiatric diagnosis) mixed-effects regressions. All models included a random intercept of ‘Family-ID’ to account for within-family clustering (34.4% of families included more than one proband-sibling pair) [8]. Models with symptom severity in sibling as the outcome were additionally adjusted for symptom severity in the proband.3
Analyses were divided in three main steps, separately for each of the 16 risk factors. In Step 1, main effects of risk factors measured in siblings were included as explanatory variables. In Step 2, main effects of the same risk factors measured in probands were added to examine whether there was a unique contribution of this risk in the proband for psychopathology in their sibling(s), over-and-above individual-level sibling risk factors. In Step 3, sibling × proband risk factor interaction terms were added to corresponding Step 2 models to evaluate whether the association between a risk factor and psychopathology in the sibling was moderated by the presence/degree of this risk in the proband. In logistic models the coefficient of the interaction term estimates departure from multiplicativity, rather than departure from additivity as is the case in linear models. Since interaction on the additive scale may reflect biological/psychological interaction better than interaction on the multiplicative scale [57], we additionally tested departure from additivity using the relative excess risk due to interaction (RERI) measure as proposed by Knol et al. [58] for logistic models (information on the calculation of the RERI measure can be found in the supplementary methods). To facilitate the evaluation of the clinical relevance of also taking into account risk factors in probands, percentages of additional explained variance (ΔR2) were reported for risk factors showing a significant proband main effect in Step 2 or a significant sibling × proband interaction in Step 3, as compared to Step 1 (in which only individual-level sibling risk factors were included). In line with recommendations by Nakagawa et al. [59] for R2 in mixed-effects models, both marginal (i.e. additional variance explained by fixed effects) and conditional ΔR2 (i.e. additional variance explained by both fixed and random effects) were reported.
All analyses were performed in R version 3.6.1 [60]. Statistical tests were two-sided and considered to be statistically significant at p < 0.05. False discovery rate (FDR) [61] q-values4 were additionally reported taking into account multiple testing for the total number of tests performed within each analytical step. Proband-sibling pairs with missing data on a variable were deleted listwise from the analyses including that variable.
Deviations of pre-registration
This paper was pre-registered on the Open Science Framework; here, the R code for the analyses and a detailed description of the deviations from the pre-registered plan can be found as well (https://www.osf.io/kzq3p/?view_only=a65ae8fac4154d65857773212ede73e5). Briefly, we had initially planned on using proband-sibling difference scores for explanatory variables and outcomes. However, during analyses, we realized several problems with this approach with regard to interpretation (e.g. for continuous data, difference scores around zero could mean both high and both low risk for the sibling and their proband, which would likely have different implications for risk for psychopathology). With our new approach, we were able to assess the impact of individual-level sibling and proband risk factors and whether their combination was related to sibling psychopathology.
Results
The mean age of the sample (N = 636) was 49.7 years (SD = 13.2, range 20–78), mean years of education was 13.3, and 62.4% were female. Sample characteristics for probands and siblings separately can be found in Table 1. Of the 380 siblings, 191 (50.3%) had a lifetime depressive and/or anxiety disorder diagnosis. Missing data on study variables was small (Supplementary Table 1). Pairwise multilevel correlations between psychosocial risk factor variables can be found in Supplementary Table 2.
Table 1.
Sample characteristics of probands and siblings
| Probands N = 256 | Siblings N = 380 | |
|---|---|---|
| Sociodemographics | ||
| Age (years), M (SD) | 48.52 (13.10) | 50.46 (13.25) |
| Female gender, % | 73.4 | 55.0 |
| Education (years), M (SD) | 13.42 (2.99) | 13.17 (3.22) |
| Low income, % | 52.9 | 47.5 |
| Life adversity and lifestyle | ||
| Early life | ||
| Childhood trauma, M (SD) | 38.59 (10.64) | 37.18 (9.54) |
| Poor parental bonding—maternal, M (SD) | 31.70 (8.88) | 30.63 (8.26) |
| Poor parental bonding—paternal, M (SD) | 31.90 (8.57) | 31.20 (8.26) |
| Recent life | ||
| Unemployment, % | 36.7 | 29.6 |
| Living alone, % | 28.9 | 20.8 |
| Being single, % | 25.4 | 21.3 |
| Small social network, % | 38.6 | 24.5 |
| Negative life events—independent, M (SD) | 0.30 (0.60) | 0.45 (0.67) |
| Negative life events—dependent, M (SD) | 0.21 (0.54) | 0.27 (0.59) |
| Smoking status, % | 20.3 | 24.3 |
| Hazardous alcohol use, % | 30.8 | 28.5 |
| Physical activity, M (SD) | 3.58 (2.92) | 4.15 (3.48) |
| Mental health | ||
| Current depressive symptom severity, M (SD) | 16.45 (10.49) | 13.15 (9.72) |
| Current anxiety symptom severity, M (SD) | 9.22 (8.11) | 5.73 (6.09) |
| Current depressive and/or anxiety disorder diagnosis, % | 37.5 | 26.8 |
| Lifetime depressive and/or anxiety disorder diagnosis, % | 100.0 | 50.3 |
Sample sizes vary slightly due to marginally missing data on psychosocial risk factors (Supplementary Table 1)
M mean, SD standard deviation
Associations of explanatory variables in siblings and probands and outcomes in siblings are reported in Table 2 (current symptom severity; linear mixed models) and Table 3 (lifetime psychiatric diagnosis; logistic mixed models). Analyses with individual-level sibling risk factors only (Step 1; Table 2) showed that more severe symptoms in the sibling were associated with female gender (γ = 0.33, SE = 0.08, p < 0.001), low income (γ = 0.39, SE = 0.08, p < 0.001), unemployment (γ = 0.32, SE = 0.09, p < 0.001), being single (γ = 0.24, SE = 0.10, p = 0.020), smoking (γ = 0.21, SE = 0.10, p = 0.030), hazardous alcohol use (γ = 0.26, SE = 0.09, p = 0.006), higher levels of childhood trauma (γ = 0.34, SE = 0.04, p < 0.001), and poorer maternal (γ = 0.25, SE = 0.04, p < 0.001) and paternal bonding (γ = 0.27, SE = 0.04, p < 0.001). These risk factors were also significantly associated with an increased likelihood of lifetime psychiatric diagnosis in the sibling (all p < 0.05; Step 1; Table 3), except for unemployment (OR = 1.64, SE = 0.42, p = 0.051).
Table 2.
Adjusteda associations of psychosocial risk factors with current depressive and/or anxious symptoms in the sibling: Step 1 (sibling individual-level associations), Step 2 (sibling and proband individual-level associations), and Step 3 (sibling × proband interactionsb) (N = 380)
| Psychosocial risk factors | Step 1 | Step 2 | Step 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| coeff | SEcoeff | p | q | coeff | SEcoeff | p | q | coeff | SEcoeff | p | q | |
| Sociodemographics | ||||||||||||
| Age | ||||||||||||
| Sibling | − 0.06 | 0.04 | 0.166 | 0.241 | − 0.23 | 0.10 | 0.026 | 0.069 | ||||
| Proband | 0.19 | 0.10 | 0.071 | 0.134 | ||||||||
| Sibling × proband interaction | 0.0002 | 0.0003 | 0.496 | 0.661 | ||||||||
| Female gender | ||||||||||||
| Sibling | 0.33 | 0.08 | < 0.001 | < 0.001 | 0.32 | 0.08 | < 0.001 | < 0.001 | ||||
| Proband | 0.06 | 0.10 | 0.532 | 0.655 | ||||||||
| Sibling × proband interaction | 0.25 | 0.19 | 0.182 | 0.416 | ||||||||
| Low educationc | ||||||||||||
| Sibling | 0.08 | 0.04 | 0.054 | 0.086 | 0.08 | 0.05 | 0.099 | 0.167 | ||||
| Proband | 0.02 | 0.05 | 0.714 | 0.762 | ||||||||
| Sibling × proband interaction | − 0.01 | 0.004 | 0.028 | 0.149 | ||||||||
| Low income | ||||||||||||
| Sibling | 0.39 | 0.08 | < 0.001 | < 0.001 | 0.39 | 0.08 | < 0.001 | < 0.001 | ||||
| Proband | 0.17 | 0.08 | 0.045 | 0.094 | ||||||||
| Sibling × proband interaction | 0.07 | 0.16 | 0.676 | 0.773 | ||||||||
| Life adversity and lifestyle | ||||||||||||
| Early life | ||||||||||||
| Childhood trauma | ||||||||||||
| Sibling | 0.34 | 0.04 | < 0.001 | < 0.001 | 0.37 | 0.04 | < 0.001 | < 0.001 | ||||
| Proband | − 0.10 | 0.04 | 0.023 | 0.067 | ||||||||
| Sibling × proband interaction | − 0.001 | 0.0004 | 0.006 | 0.048 | ||||||||
| Poor parental bonding—maternal | ||||||||||||
| Sibling | 0.25 | 0.04 | < 0.001 | < 0.001 | 0.30 | 0.05 | < 0.001 | < 0.001 | ||||
| Proband | − 0.12 | 0.05 | 0.013 | 0.042 | ||||||||
| Sibling × proband interaction | − 0.0004 | 0.001 | 0.418 | 0.634 | ||||||||
| Poor parental bonding—paternal | ||||||||||||
| Sibling | 0.27 | 0.04 | < 0.001 | < 0.001 | 0.31 | 0.04 | < 0.001 | < 0.001 | ||||
| Proband | − 0.14 | 0.05 | 0.003 | 0.014 | ||||||||
| Sibling × proband interaction | − 0.001 | 0.001 | 0.124 | 0.360 | ||||||||
| Recent life | ||||||||||||
| Unemployment | ||||||||||||
| Sibling | 0.32 | 0.09 | < 0.001 | 0.002 | 0.32 | 0.09 | < 0.001 | 0.003 | ||||
| Proband | 0.02 | 0.09 | 0.863 | 0.891 | ||||||||
| Sibling × proband interaction | − 0.15 | 0.19 | 0.436 | 0.634 | ||||||||
| Living alone | ||||||||||||
| Sibling | 0.09 | 0.10 | 0.405 | 0.438 | 0.08 | 0.10 | 0.450 | 0.600 | ||||
| Proband | 0.16 | 0.10 | 0.092 | 0.164 | ||||||||
| Sibling × proband interaction | − 0.36 | 0.23 | 0.111 | 0.360 | ||||||||
| Being single | ||||||||||||
| Sibling | 0.24 | 0.10 | 0.020 | 0.040 | 0.21 | 0.10 | 0.033 | 0.081 | ||||
| Proband | 0.27 | 0.10 | 0.008 | 0.028 | ||||||||
| Sibling × proband interaction | − 0.001 | 0.22 | 0.996 | 0.996 | ||||||||
| Small social network | ||||||||||||
| Sibling | 0.12 | 0.10 | 0.216 | 0.288 | 0.10 | 0.10 | 0.444 | 0.470 | ||||
| Proband | 0.18 | 0.09 | 0.054 | 0.108 | ||||||||
| Sibling × proband interaction | − 0.12 | 0.20 | 0.550 | 0.677 | ||||||||
| Negative life events—independent | ||||||||||||
| Sibling | 0.005 | 0.04 | 0.909 | 0.909 | 0.02 | 0.04 | 0.704 | 0.762 | ||||
| Proband | − 0.07 | 0.05 | 0.161 | 0.999 | ||||||||
| Sibling × proband interaction | 0.003 | 0.08 | 0.969 | 0.996 | ||||||||
| Negative life events—dependent | ||||||||||||
| Sibling | 0.04 | 0.04 | 0.359 | 0.438 | 0.04 | 0.04 | 0.337 | 0.470 | ||||
| Proband | − 0.02 | 0.04 | 0.657 | 0.751 | ||||||||
| Sibling × proband interaction | 0.08 | 0.10 | 0.422 | 0.634 | ||||||||
| Smoking | ||||||||||||
| Sibling | 0.21 | 0.10 | 0.030 | 0.053 | 0.20 | 0.10 | 0.039 | 0.089 | ||||
| Proband | 0.06 | 0.11 | 0.590 | 0.699 | ||||||||
| Sibling × proband interaction | − 0.27 | 0.23 | 0.241 | 0.482 | ||||||||
| Hazardous alcohol use | ||||||||||||
| Sibling | 0.26 | 0.09 | 0.006 | 0.014 | 0.25 | 0.09 | 0.007 | 0.028 | ||||
| Proband | 0.09 | 0.09 | 0.338 | 0.470 | ||||||||
| Sibling × proband interaction | − 0.53 | 0.19 | 0.005 | 0.048 | ||||||||
| Physical inactivityd | ||||||||||||
| Sibling | 0.03 | 0.04 | 0.411 | 0.438 | 0.05 | 0.04 | 0.283 | 0.453 | ||||
| Proband | − 0.03 | 0.04 | 0.500 | 0.640 | ||||||||
| Sibling × proband interaction | 0.01 | 0.004 | 0.135 | 0.360 | ||||||||
Estimates and standard errors were retrieved from linear mixed-effects models with a random intercept of ‘Family-ID’ to account for within-family clustering. Sample sizes vary slightly due to marginally missing data on psychosocial risk factors (Supplementary Table 1). Significant associations (p < 0.05) are presented in bold. False discovery rate (FDR) q-values [61] presented here take into account multiple testing for the total number of tests per outcome performed within each analytical step: 16 tests per outcome in Step 1 and Step 3, and 32 tests per outcome in Step 2
SEcoeff standard error of coefficient
aAll linear mixed-effects regression models were adjusted for current severity of depressive and/or anxious symptoms in the proband
bAdditive interactions
cTotal years of education was multiplied by − 1 (reversed) to reflect low education
dMET-scores were multiplied by − 1 (reversed) to reflect physical inactivity and divided by 1000 to prevent very large estimates
Table 3.
Associations of psychosocial risk factors with lifetime depressive and/or anxious psychopathology in the sibling: Step 1 (sibling individual-level associations), Step 2 (sibling and proband individual-level associations), and Step 3 (sibling × proband interactionsa) (N = 380)
| Psychosocial risk factors | Step 1 | Step 2 | Step 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | SEOR | p | q | OR | SEOR | p | q | OR | SEOR | p | q | |
| Sociodemographics | ||||||||||||
| Age | ||||||||||||
| Sibling | 0.96 | 0.11 | 0.746 | 0.796 | 0.78 | 0.21 | 0.345 | 0.552 | ||||
| Proband | 1.28 | 0.35 | 0.372 | 0.567 | ||||||||
| Sibling × proband interaction | 1.00 | 0.001 | 0.914 | 0.994 | ||||||||
| Female gender | ||||||||||||
| Sibling | 2.44 | 0.58 | < 0.001 | < 0.001 | 2.36 | 0.56 | < 0.001 | 0.003 | ||||
| Proband | 1.54 | 0.41 | 0.105 | 0.336 | ||||||||
| Sibling × proband interaction | 1.77 | 0.90 | 0.262 | 0.645 | ||||||||
| Low educationb | ||||||||||||
| Sibling | 1.10 | 0.12 | 0.403 | 0.513 | 1.13 | 0.14 | 0.309 | 0.520 | ||||
| Proband | 0.92 | 0.11 | 0.515 | 0.687 | ||||||||
| Sibling × proband interaction | 0.99 | 0.01 | 0.211 | 0.645 | ||||||||
| Low income | ||||||||||||
| Sibling | 2.00 | 0.44 | 0.002 | 0.006 | 1.96 | 0.43 | 0.002 | 0.015 | ||||
| Proband | 1.28 | 0.29 | 0.274 | 0.487 | ||||||||
| Sibling × proband interaction | 1.34 | 0.59 | 0.511 | 0.956 | ||||||||
| Life adversity and lifestyle | ||||||||||||
| Early life | ||||||||||||
| Childhood trauma | ||||||||||||
| Sibling | 2.21 | 0.32 | < 0.001 | < 0.001 | 2.20 | 0.35 | < 0.001 | < 0.001 | ||||
| Proband | 1.01 | 0.14 | 0.942 | 0.972 | ||||||||
| Sibling × proband interaction | 1.00 | 0.001 | 0.064 | 0.645 | ||||||||
| Poor parental bonding—maternal | ||||||||||||
| Sibling | 1.89 | 0.25 | < 0.001 | < 0.001 | 1.86 | 0.27 | < 0.001 | < 0.001 | ||||
| Proband | 1.08 | 0.15 | 0.550 | 0.704 | ||||||||
| Sibling × proband interaction | 1.00 | 0.002 | 0.168 | 0.645 | ||||||||
| Poor parental bonding—Paternal | ||||||||||||
| Sibling | 1.76 | 0.23 | < 0.001 | < 0.001 | 1.88 | 0.27 | < 0.001 | < 0.001 | ||||
| Proband | 0.82 | 0.11 | 0.161 | 0.429 | ||||||||
| Sibling × proband interaction | 1.00 | 0.002 | 0.619 | 0.956 | ||||||||
| Recent life | ||||||||||||
| Unemployment | ||||||||||||
| Sibling | 1.64 | 0.42 | 0.051 | 0.091 | 1.63 | 0.42 | 0.057 | 0.203 | ||||
| Proband | 1.10 | 0.27 | 0.704 | 0.802 | ||||||||
| Sibling × proband interaction | 1.46 | 0.76 | 0.462 | 0.914 | ||||||||
| Living alone | ||||||||||||
| Sibling | 1.25 | 0.34 | 0.417 | 0.329 | 1.24 | 0.34 | 0.432 | 0.601 | ||||
| Proband | 1.23 | 0.31 | 0.416 | 0.601 | ||||||||
| Sibling × proband interaction | 0.50 | 0.29 | 0.232 | 0.645 | ||||||||
| Being single | ||||||||||||
| Sibling | 1.95 | 0.53 | 0.014 | 0.028 | 1.92 | 0.52 | 0.017 | 0.078 | ||||
| Proband | 1.34 | 0.35 | 0.274 | 0.487 | ||||||||
| Sibling × proband interaction | 0.97 | 0.59 | 0.954 | 0.994 | ||||||||
| Small social network | ||||||||||||
| Sibling | 1.38 | 0.36 | 0.226 | 0.329 | 1.34 | 0.35 | 0.261 | 0.487 | ||||
| Proband | 1.13 | 0.27 | 0.595 | 0.717 | ||||||||
| Sibling × proband interaction | 1.42 | 0.76 | 0.514 | 0.914 | ||||||||
| Negative life events—independent | ||||||||||||
| Sibling | 0.87 | 0.10 | 0.220 | 0.513 | 0.87 | 0.10 | 0.239 | 0.487 | ||||
| Proband | 0.97 | 0.12 | 0.826 | 0.881 | ||||||||
| Sibling × proband interaction | 1.00 | 0.21 | 0.994 | 0.994 | ||||||||
| Negative life events—dependent | ||||||||||||
| Sibling | 1.01 | 0.11 | 0.941 | 0.941 | 1.00 | 0.11 | 0.993 | 0.993 | ||||
| Proband | 1.06 | 0.12 | 0.605 | 0.717 | ||||||||
| Sibling × proband interaction | 0.95 | 0.25 | 0.859 | 0.994 | ||||||||
| Smoking | ||||||||||||
| Sibling | 2.18 | 0.58 | 0.004 | 0.011 | 2.09 | 0.56 | 0.007 | 0.037 | ||||
| Proband | 1.49 | 0.44 | 0.179 | 0.441 | ||||||||
| Sibling × proband interaction | 0.51 | 0.32 | 0.282 | 0.645 | ||||||||
| Hazardous alcohol use | ||||||||||||
| Sibling | 1.79 | 0.47 | 0.013 | 0.028 | 1.74 | 0.43 | 0.028 | 0.112 | ||||
| Proband | 1.34 | 0.33 | 0.244 | 0.487 | ||||||||
| Sibling × proband interaction | 0.57 | 0.30 | 0.279 | 0.645 | ||||||||
| Physical inactivityc | ||||||||||||
| Sibling | 0.95 | 0.11 | 0.674 | 0.770 | 0.96 | 0.11 | 0.727 | 0.802 | ||||
| Proband | 1.19 | 0.14 | 0.126 | 0.367 | ||||||||
| Sibling × proband interaction | 1.00 | 0.01 | 0.958 | 0.994 | ||||||||
Odds ratios and standard errors were retrieved from logistic mixed-effects models with a random intercept of ‘Family-ID’ to account for within-family clustering. Sample sizes vary slightly due to marginally missing data on psychosocial risk factors (Supplementary Table 1). Significant associations (p < 0.05) are presented in bold. False discovery rate (FDR) q-values [61] presented here take into account multiple testing for the total number of tests per outcome performed within each analytical step: 16 tests per outcome in Step 1 and Step 3, and 32 tests per outcome in Step 2
OR odds ratio, SEOR standard error of odds ratio
aMultiplicative interactions. Results for additive interactions as estimated by the relative excess risk due to interaction (RERI) can be found in Supplementary Table 3
bTotal years of education was multiplied by − 1 (reversed) to reflect low education
cMET-scores were multiplied by − 1 (reversed) to reflect physical inactivity and divided by 1000 to prevent very large estimates
In Step 2, we added the same risk factors assessed in probands as additional explanatory variables. For the outcome of current symptomatology in sibling, main effects of several proband individual-level risk factors were found (Step 2; Table 2): on top of the presence/degree of the risk factor in the sibling, proband low income (γ = 0.17, SE = 0.08, p = 0.045, ΔR2marginal = 0.4%, ΔR2conditional = 0.7%), being single (γ = 0.27, SE = 0.10, p = 0.008, ΔR2marginal = 1.8%, ΔR2conditional = 3.4%), and lower levels of childhood trauma (γ = − 0.10, SE = 0.04, p = 0.023, ΔR2marginal = 0.2%, ΔR2conditional = 2.7%), and more optimal maternal (γ = − 0.12, SE = 0.05, p = 0.013, ΔR2marginal = 1.5%, ΔR2conditional = 1.5%) and paternal bonding (γ = − 0.14, SE = 0.05, p = 0.003, ΔR2marginal = 2.1%, ΔR2conditional = 1.2%) were associated with more severe symptoms in the sibling. No significant main effects of proband risk factors on the outcome of lifetime psychiatric diagnosis in sibling were found (all p > 0.05; Step 2; Table 3).
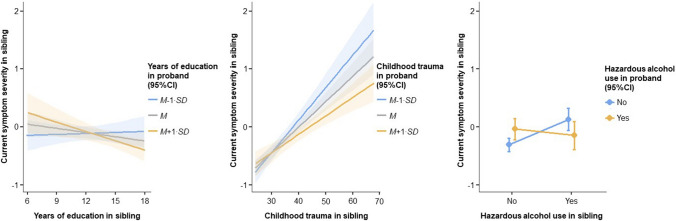
The additional effect of sibling × proband interactions in risk factors was tested in Step 3. For the additive interaction effect on current symptomatology in the sibling (Step 3; Table 2), significant sibling × proband interactions were found for low education (γ = − 0.01, SE = 0.004, p = 0.028, ΔR2marginal = 1.3%, ΔR2conditional = 1.1%), childhood trauma (γ = − 0.001, SE = 0.0004, p = 0.006, ΔR2marginal = 1.8%, ΔR2conditional = 0.7%), and hazardous alcohol use (γ = − 0.53, SE = 0.19, p = 0.005, ΔR2marginal = 2.2%, ΔR2conditional = 2.4%). Figure 1 shows the association between a risk factor and symptoms in the sibling for different values of that risk factor in the proband for low education (left panel), childhood trauma (middle panel), and hazardous alcohol use (right panel). Consistently, when the risk factor was also present in the proband (lower years of education, higher levels of childhood trauma, and hazardous alcohol use), the strength of the association between the same risk factor and symptoms in their sibling was reduced. No significant (multiplicative) sibling × proband interactions were found for the outcome of lifetime psychiatric diagnosis in sibling (all p > 0.05; Step 3; Table 3), nor when the coefficient of the interaction term estimated departure from additivity (Supplementary Table 3).
Fig. 1.
Fixed effects (with 95% confidence intervals) of sibling × proband interaction effects of years of education (left panel), childhood trauma (middle panel), and hazardous alcohol use (right panel) on current depressive and/or anxiety symptom severity in the sibling, while controlling for current symptomatology in the proband. Current depressive and/or anxiety symptom severity was measured as standardized and averaged overall IDS/BAI score. Estimates of simple effects (γ) were retrieved from linear mixed-effects models with a random intercept of ‘Family-ID’ to account for within-family clustering and indicate the (presence/absence and direction of) association between a risk factor and current symptomatology in the sibling for different values of that risk factor in the proband. Low years of education (left panel) was associated with more severe symptoms in the sibling when the proband had high years of education (M + 1∙SD: γ = − 0.05, SE = 0.02, p = 0.007); no associations were found when the proband had average (M: γ = − 0.02, SE = 0.01, p = 0.104) or low years of education (M−1∙SD: γ = 0.01, SE = 0.02, p = 0.781). Higher childhood trauma (middle panel) was associated with more severe symptoms in the sibling and the strength of this association increases for decreasing trauma levels in the proband (M + 1∙SD: γ = 0.03, SE = 0.01, p < 0.001; M: γ = 0.04, SE = 0.005, p < 0.001; M−1∙SD: γ = 0.05, SE = 0.01, p < 0.001). Hazardous alcohol use (right panel) was associated with more severe symptoms in the sibling when the proband was not a user (No: γ = 0.44, SE = 0.11, p < 0.001); no association was found when the proband was a user (Yes: γ = − 0.11, SE = 0.15, p = 0.473). M mean, SD standard deviation, SE standard error
Discussion
In siblings of probands with lifetime depressive and anxiety disorders, we confirmed the association of a wide range of established psychosocial risk factors with psychopathology symptoms and disorders. However, the major finding of our study is that the presence of the same risk factors in affected probands, explained additional interindividual differences in psychopathology in at-risk siblings. For instance, siblings having low income and who were single had higher symptoms; intriguingly, the presence of the same risk factor in the proband was additionally associated with higher symptoms in their sibling, independently of the sibling’s individual risk factor. Furthermore, for other risk factors (low education, childhood trauma, hazardous alcohol use), the presence in the proband moderated the association between the risk factor and symptoms in the sibling: when the risk factor was also present in the proband, the strength of the association between the risk factor and symptoms in the sibling was reduced. Thus, when similar levels of a risk factor were shared between probands and siblings, the impact of the risk factor on siblings’ symptoms was buffered. Of note, we only confirmed these additional family effects of risk factors for the continuous outcome of psychopathology symptoms but not for binary clinical diagnoses, possibly due to the reduced statistical power or loss of information when using a dichotomous classification.
Besides showing an additive impact of probands’ low income, which is in line with findings from a previous community-based twin study [32], we extend the current literature by showing that when a proband was single, on top of the presence of the risk in their sibling, this was associated with more severe symptomatology in the sibling. This additive impact of also having low income and being single present in the proband may arise from additional familial clustering between these risk factors and psychopathology (i.e. a more genetic form of the disorders that tends to be co-inherited with these risk factors). In line with this reasoning, twin and genome-wide association studies have shown substantial genetic correlations of income (− 0.30 to − 0.44) [62, 63] and avoidant/anxious romantic attachment (0.48–0.58) [64], which might increase the probability of being single, with depressive and anxiety disorders. The additive impact of the presence of a risk factor in the proband may also be a reflection of the degree of (and/or other additional) problems within their family. That is, both proband and sibling having low income and being single may indicate a more substantial degree of a family’s socioeconomic deprivation and romantic relationship problems, which likely results from or leads to more severe affective problems [9, 65].
We also found several risk factors for which the additional presence or higher levels in the proband were associated with less severe symptomatology in their sibling(s). These factors included poor parental bonding and childhood trauma, which were also identified in previous studies [33–37, 41], and low education and hazardous alcohol use. Independently of parental bonding levels in the sibling, poorer parental bonding in the proband was associated with less severe symptomatology in the sibling. For childhood trauma, low education, and hazardous alcohol use, the individual-level risk in the proband moderated the impact of the risk factor on symptomatology in their sibling(s): when these factors were similarly present in both proband and sibling, the impact of the factor on sibling symptomatology appeared to be buffered. Conversely, a sibling’s symptoms were higher when these risk factors were not shared with or were of lower level in their proband. This may reflect a ‘black sheep effect’, in which the feeling of having been worse off than your sibling may arise from (perceived) differential parenting (for early life adversity) [66, 67], differences in innate abilities and/or unequal parental resource investment (for education) [68], and sibling deidentification in the proband (i.e. actively seeking to differentiate themself from their sibling; for alcohol use) [69]. Siblings may use each other as a reference point, which in the case of upward social comparisons (i.e. comparisons to a perceived ‘superior’ other) may lead to experiences of unfairness and inequity [24]. Such upward social comparisons have been shown to have the most detrimental effects on depressive and anxious psychopathology by feeding into dysfunctional beliefs about the self [25]. Of note, among risk factors for which we found significant additional impact of considering proband levels, evidence was less strong for low income/education given that these associations were not significant after correcting for multiple testing.
We did not find evidence for an added effect of taking into account proband risk over-and-above or in combination with a sibling’s individual risk for any of the other psychosocial risk factors that we tested, which is in line with previous findings (age, gender) [5, 39, 40]. For instance, recent negative life events, for which we reported moderate proband-sibling resemblance in a previous study [8], were not associated with sibling psychopathology. One possible reason for that is that we measured recent life events in a sample of relatively older aged adults, in which factors beyond the family environment (such as individual, rather than familial, recent negative life events) may have a larger impact. As such cross-sibling effects of recent negative life events on affective psychopathology may be less likely. This is in line with evidence from behavioral-genetic research [6, 7] suggesting an increased role across the lifespan for individual environments and unique risk and protective factors in shaping behavioral, psychological, and personality features.
Overall, results were highly similar between the two outcomes with regard to the direction of associated risk factors, but lifetime diagnosis (dichotomous) showed fewer associated factors within siblings and no associated proband main effects or sibling × proband interaction effects for any of the risk factors, as compared to current symptomatology (continuous). This suggests that the continuous outcome may have provided deeper resolution and/or higher statistical power. This is particularly the case with regard to recent life risk factors and the dichotomous outcome, since we investigated associations between a risk factor that occurred in current/recent life (e.g. unemployment) with a disorder that may have occurred years before the time of assessment, whereas the continuous outcome referred to current symptoms. This may have reduced power to detect proband main effects and/or sibling × proband interaction effects of recent life risk factors and the dichotomous outcome by diluting effects in both siblings and probands.
Strengths of the present study include the sibling structure of the data, which has the advantage that sibling relationships contain a higher shared proportion of (early) environmental factors as compared to parent–offspring relationships; the relatively older age of the sample, which allows for the examination of siblings’ more definite clinical profiles and interindividual discrepancies between siblings that emerged across the lifespan; and the wide variety of assessed psychosocial risk factors. However, the present study is not without limitations. First, as this study only used cross-sectional data, no conclusion can be drawn with regard to the ordering of effects. In particular with regard to some of the lifestyle risk factors, such as smoking or hazardous alcohol use, the association with depressive and anxious psychopathology may be bidirectional [19, 20, 70]. Second, although this study used a relatively large clinically relevant sibling sample of 380 proband-sibling pairs, we may have had insufficient power to detect the examined sibling × proband risk factor interaction effects: based on the assumption that the interaction effect is half size of the main effects, 16 times the sample size is required to estimate an interaction than to estimate a main effect [71]. Third, retrospective self-report measures of life adversity may have been confounded by participants’ differential recall accuracy and current mood. However, we deem the impact low because previous NESDA and other studies showed that these measures had adequate temporal stability and were not critically affected by respondents’ current mood [72–78]. Fourth, this study explored as a ‘bench-mark’ the added impact of individual psychosocial risk factors in probands, over-and-above or in combination with risk factors in siblings. Given the relatively exploratory nature of our study and the fact that several of the studied risk factors were correlated and may, therefore, explain overlapping portions of the symptom variance, we used separate analytical models for each risk factor. For future research, it would definitely be worthwhile to investigate the impact of individual risk factors in probands on top of a broad set of risk factors in siblings. Fifth, the fact that the present study was designed to include a high-risk sample of probands with a lifetime depressive and/or anxiety disorder and their siblings limits the generalizability of the findings to the general population.
To conclude, this study confirmed the association of a broad range of psychosocial risk factors with depressive and anxiety symptoms and disorders in siblings of probands with a lifetime depressive or anxiety disorder. However, importantly, we demonstrated that not only the risk factors within these at-risk individuals are important, but also those within their relatives: the individual-level risk factor in the proband, in itself or in combination with the individual-level risk factor in their sibling, had additional value for siblings’ psychopathology over only considering the individual-level risk factor in the sibling. Even though percentages of additional explained variance were small, previous research [79] has argued that small effects are the norm, rather than the exception, and form an indispensable foundation for cumulative psychological science: small effects may still have substantial direct consequences for individual mental well-being, especially for effects that accumulate over time and at scale such as childhood trauma [80, 81] and low income [82]. Our findings underscore the importance of weighing risk factors within a family context, as whether or not risk factors are shared with other siblings in the family may provide relevant information on the individual risk of depressive/anxious psychopathology. Future studies are needed to identify the exact mechanisms explaining the additive impact of weighing risk factors within all siblings in the family. Moreover, given the recent findings of little specificity in familial transmission in specific classes of psychiatric disorders [83–85], future studies may want to examine whether our findings extend to other risk factors and/or psychiatric conditions.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
BWJHP developed the NESDA study concept and design. Together with BWJHP, BME and AMvH were closely involved in the design of the NESDA family study. EDvS and MK prepared the data for the analyses. EDvS performed the data analysis and interpretation under supervision of DFM, YM and BWJHP. EDvS drafted the manuscript, and BWJHP, DFM, YM, MK, CAH, BME, and AMvH provided critical revisions. All authors approved the final version of the paper for submission.
Funding
The Netherlands Study of Depression and Anxiety (NESDA) is funded through the Geestkracht program of the Netherlands Organization for Scientific Research and Development (ZonMw, Grant number 10-000-1002) and financial contributions by participating universities and mental health care organizations (Amsterdam University Medical—Vrije Universiteit VU, GGZ ingeest, Leiden University Medical Center, Leiden University, GGZ Rivierduinen, University Medical Center Groningen, University of Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Rob Giel Onderzoekscentrum).
Data availability
The data that support the findings of this study are available via the website of NESDA (https://www.nesda.nl/pro-index/), which will be provided after handing in a data request. This paper was pre-registered on the Open Science Framework; here, the R code for the analyses can be found as well (https://www.osf.io/kzq3p/?view_only=a65ae8fac4154d65857773212ede73e5).
Declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
The NESDA study protocol was approved by the ethical committee of participating universities. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Footnotes
Unlike a normal Pearson correlation coefficient, a multilevel Pearson correlation coefficient takes into account the within-family clustering of the IDS and BAI data (34.4% of families in the present study included more than one proband-sibling pair) [8].
For probands, CTQ was administered at the 6-year follow-up.
This was done to rule out the possibility that associations were not simply due to familial clustering of depressive/anxious psychopathology. Applying a similar adjustment procedure on models with presence of psychiatric diagnosis in sibling as the outcome was not possible as there was no variance in psychiatric diagnosis in probands (i.e. all probands were lifetime affected).
Given the number of statistical comparisons performed within each analytical step (Step 1 and Step 3: 16 comparisons, one for each risk factor, per outcome; Step 2: 32 comparisons, two for each risk factor, per outcome), we deemed it necessary to additionally report FDR-corrected q-values. However, uncorrected p-values were used as leading in the analyses of this paper: following reasoning by Althouse [86] we believe that adjustment for multiple testing is too strict given the strong prior credibility of the 16 tested risk factors in terms of their association with depressive/anxious psychopathology based on prior research [9–21, 47, 48]. Therefore, uncorrected p-values were used as leading, with the sidenote that associations with p < 0.05 with but with FDR-corrected q ≥ 0.05 should be interpreted with caution.
References
- 1.Lawrence PJ, Murayama K, Creswell C. Systematic review and meta-analysis: anxiety and depressive disorders in offspring of parents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2019;58:46–60. doi: 10.1016/j.jaac.2018.07.898. [DOI] [PubMed] [Google Scholar]
- 2.Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk studies. Schizophr Bull. 2014;40:28–38. doi: 10.1093/schbul/sbt114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steinhausen H-C, Foldager L, Perto G, Munk-Jørgensen P. Family aggregation of mental disorders in the nationwide Danish three generation study. Eur Arch Psychiatry Clin Neurosci. 2009;259:270–277. doi: 10.1007/s00406-008-0865-0. [DOI] [PubMed] [Google Scholar]
- 4.Li X, Sundquist J, Sundquist K. Sibling risk of anxiety disorders based on hospitalizations in Sweden. Psychiatry Clin Neurosci. 2011;65:233–238. doi: 10.1111/j.1440-1819.2011.02199.x. [DOI] [PubMed] [Google Scholar]
- 5.Li X, Sundquist J, Hemminki K, Sundquist K. Familial risks for depression among siblings based on hospitalizations in Sweden. Psychiatry Genet. 2008;18:80–84. doi: 10.1097/YPG.0b013e3282f08ac9. [DOI] [PubMed] [Google Scholar]
- 6.Plomin R. Commentary: why are children in the same family so different? Non-shared environment three decades later. Int J Epidemiol. 2011;40:582–592. doi: 10.1093/ije/dyq144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Plomin R, Daniels D. Why are children in the same family so different from one another? Behavioral Brain Sci. 1987;10:1–16. doi: 10.1017/S0140525X00055941. [DOI] [Google Scholar]
- 8.van Sprang ED, Maciejewski DF, Milaneschi Y, et al. Familial resemblance in mental health symptoms, social and cognitive vulnerability, and personality: a study of patients with depressive and anxiety disorders and their siblings. J Affect Disord. 2021;294:420–429. doi: 10.1016/j.jad.2021.06.072. [DOI] [PubMed] [Google Scholar]
- 9.Ridley MW, Rao G, Schilbach F, Patel VH. Poverty, depression, and anxiety: causal evidence and mechanisms. J Chem Inf Model. 2017;53:21–25. doi: 10.1126/science.aay0214. [DOI] [PubMed] [Google Scholar]
- 10.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4:146–158. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 11.Frasquilho D, Matos MG, Salonna F, et al. Mental health outcomes in times of economic recession: a systematic literature review health behavior, health promotion and society. BMC Public Health. 2016;16:115. doi: 10.1186/s12889-016-2720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lorant V, Deliège D, Eaton W, et al. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 13.Lund C, Breen A, Flisher AJ, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med. 2010;71:517–528. doi: 10.1371/journal.pone.0156939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norman RE, Byambaa M, De R, et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9:e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marshall M, Shannon C, Meenagh C, et al. The association between childhood trauma, parental bonding and depressive symptoms and interpersonal functioning in depression and bipolar disorder. Ir J Psychol Med. 2018;35:23–32. doi: 10.1017/ipm.2016.43. [DOI] [PubMed] [Google Scholar]
- 16.Roca M, Gili M, Garcia-Campayo J, et al. Stressful life events severity in patients with first and recurrent depressive episodes. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1963–1969. doi: 10.1007/s00127-013-0691-1. [DOI] [PubMed] [Google Scholar]
- 17.Andrade L, Caraveo-Anduaga JJ, Berglund P, et al. The epidemiology of major depressive episodes: results from the international consortium of psychiatric epidemiology (ICPE) surveys. Int J Methods Psychiatr Res. 2003;12:3–21. doi: 10.1002/mpr.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levula A, Harré M, Wilson A. The association between social network factors with depression and anxiety at different life stages. Commun Ment Health J. 2018;54:842–854. doi: 10.1007/s10597-017-0195-7. [DOI] [PubMed] [Google Scholar]
- 19.Fluharty M, Taylor AE, Grabski M, Munafò MR. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob Res. 2017;19:3–13. doi: 10.1093/ntr/ntw140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schuch F, Vancampfort D, Firth J, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J Affect Disord. 2017;210:139–150. doi: 10.1016/j.jad.2016.10.050. [DOI] [PubMed] [Google Scholar]
- 21.Li J, Wang H, Li M, et al. Effect of alcohol use disorders and alcohol intake on the risk of subsequent depressive symptoms: a systematic review and meta-analysis of cohort studies. Addiction. 2020;115:1224–1243. doi: 10.1111/add.14935. [DOI] [PubMed] [Google Scholar]
- 22.Spano R. We are family: specifying the unique contribution of abuseand neglect of siblings on the prevalence, severity, and chronicity of maltreatment in the household. J Interpers Violence. 2018;33:2420–2438. doi: 10.1177/0886260515625908. [DOI] [PubMed] [Google Scholar]
- 23.Jensen AC, Whiteman SD, Fingerman KL, Birditt KS. “Life still isn’t fair”: parental differential treatment of young adult siblings. J Marriage Fam. 2013;75:438–452. doi: 10.1111/jomf.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Festinger L. A theory of social comparison processes. Hum Relat. 1954;7:117–140. doi: 10.1177/001872675400700202. [DOI] [Google Scholar]
- 25.McCarthy PA, Morina N. Exploring the association of social comparison with depression and anxiety: a systematic review and meta-analysis. Clin Psychol Psychother. 2020;27:640–671. doi: 10.1002/cpp.2452. [DOI] [PubMed] [Google Scholar]
- 26.Rose AJ. The costs and benefits of co-rumination. Child Dev Perspect. 2021;15:176–181. doi: 10.1111/cdep.12419. [DOI] [Google Scholar]
- 27.Spendelow JS, Simonds LM, Avery RE. The relationship between co-rumination and internalizing problems: a systematic review and meta-analysis. Clin Psychol Psychother. 2017;24:512–527. doi: 10.1002/cpp.2023. [DOI] [PubMed] [Google Scholar]
- 28.Her YC, Batur ZZ, Vergauwen J, Mortelmans D. Siblings’ similarities and dissimilarities: a review of theoretical perspectives and empirical insights. J Fam Theory Rev. 2021;13:447–462. doi: 10.1111/jftr.12436. [DOI] [Google Scholar]
- 29.Felton JW, Cole DA, Havewala M, et al. Talking together, thinking alone: relations among co-rumination, peer relationships, and rumination. J Youth Adolesc. 2019;48:731–743. doi: 10.1007/s10964-018-0937-z.Talking. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ames-Sikora AM, Donohue MR, Tully EC. Nonlinear associations between co-rumination and both social support and depression symptoms. J Psychol. 2017;151:597–612. doi: 10.1080/00223980.2017.1372345. [DOI] [PubMed] [Google Scholar]
- 31.Calmes CA, Roberts JE. Rumination in interpersonal relationships: does co-rumination explain gender differences in emotional distress and relationship satisfaction among college students? Cognit Ther Res. 2008;32:577–590. doi: 10.1007/s10608-008-9200-3. [DOI] [Google Scholar]
- 32.Cohen-Cline H, Beresford SAA, Barrington WE, et al. Associations between neighbourhood characteristics and depression: a twin study. J Epidemiol Commun Health (1978) 2018;72:202–207. doi: 10.1136/jech-2017-209453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kullberg M-L, van Schie C, van Sprang E, et al. It is a family affair: Individual experiences and sibling exposure to emotional, physical and sexual abuse and the impact on adult depressive symptoms. Psychol Med. 2020 doi: 10.1017/S0033291720000823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kullberg M-L, van Schie CC, van Sprang ED, et al. Why some siblings thrive whereas others struggle: a within-family study on recollections of childhood parental bonding and current adult depressive and anxiety symptoms. J Affect Disord. 2021;281:413–421. doi: 10.1016/j.jad.2020.12.045. [DOI] [PubMed] [Google Scholar]
- 35.Boyle MH, Jenkins JM, Georgiades K, et al. Differential-maternal parenting behavior: estimating within- and between-family effects on children. Child Dev. 2004;75:1457–1476. doi: 10.1111/j.1467-8624.2004.00751.x. [DOI] [PubMed] [Google Scholar]
- 36.Long EC, Aggen SH, Gardner C, Kendler KS. Differential parenting and risk for psychopathology: a monozygotic twin difference approach. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1569–1576. doi: 10.1007/s00127-015-1065-7.Differential. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feinberg M, Hetherington EM. Differential parenting as a within-family variable. J Fam Psychol. 2001;15:22–37. doi: 10.1037/0893-3200.15.1.22. [DOI] [PubMed] [Google Scholar]
- 38.Moskvina V, Farmer A, Jones IR, et al. Sex differences in symptom patterns of recurrent major depression in siblings. Depress Anxiety. 2008;25:527–534. doi: 10.1002/da.20372. [DOI] [PubMed] [Google Scholar]
- 39.Olino TM, Lewinsohn PM, Klein DN. Sibling similarity for MDD: evidence for shared familial factors. J Affect Disord. 2006;94:211–218. doi: 10.1016/j.jad.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 40.Boomsma DI, van Beijsterveldt CEM, Hudziak JJ. Genetic and environmental influences on anxious/depression during childhood: a study from the Netherlands twin register. Genes Brain Behav. 2005;4:466–481. doi: 10.1111/j.1601-183X.2005.00141.x. [DOI] [PubMed] [Google Scholar]
- 41.Shanahan L, Mchale SM, Crouter AC, Osgood DW. Linkages between parents’ differential treatment, youth depressive symptoms, and sibling relationships. J Marriage Fam. 2008;70:480–494. doi: 10.1111/j.1741-3737.2008.00495.x. [DOI] [Google Scholar]
- 42.Penninx BWJH, Eikelenboom M, Giltay EJ, et al. Cohort profile of the longitudinal Netherlands study of depression and anxiety (NESDA) on etiology, course and consequences of depressive and anxiety disorders. J Affect Disord. 2021;287:69–77. doi: 10.1016/j.jad.2021.03.026. [DOI] [PubMed] [Google Scholar]
- 43.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 44.Wittchen H-U. Reliability and validity studies of the WHO-composite international diagnostic interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 45.Rush AJ, Gullion CM, Basco MR, et al. The inventory of depressive symptomatology (IDS): psychometric properties. Psychol Med. 1996;26:477–486. doi: 10.1017/S0033291700035558. [DOI] [PubMed] [Google Scholar]
- 46.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psycometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- 47.Essau CA, Lewinsohn PM, Xin J, et al. Incidence, recurrence and comorbidity of anxiety disorders in four major developmental stages. J Affect Disord. 2018;228:248–253. doi: 10.1016/j.jad.2017.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beesdo K, Höfler M, Leibenluft E, et al. Mood episodes and mood disorders: patterns of incidence and conversion in the first three decades of life. Bipolar Disord. 2009;11:637–649. doi: 10.1111/j.1399-5618.2009.00738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Centraal Planbureau (2014) Kortetermijnraming december 2014. SDU, Den Haag. Available online at .https://www.cpb.nl/cijfer/kortetermijnraming-december-2014
- 50.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. 2003;27:169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 51.Parker G, Tupling H, Brown LB. A parental bonding instrument. Br J Med Psychol. 1979;52:1–10. doi: 10.1111/j.2044-8341.1979.tb02487.x. [DOI] [Google Scholar]
- 52.Maciejewski DF, van Sprang ED, Spinhoven P, Penninx BWJH. Longitudinal associations between negative life events and depressive symptoms—a 9-year longitudinal study on between-person and within-person effects and the role of family history. J Personal Soc Psychol. 2021;121:707–721. doi: 10.1037/pspp0000381. [DOI] [PubMed] [Google Scholar]
- 53.Brugha TS, Bebbington P, Tennant C, Hurry J. The list of threatening experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychol Med. 1985;15:189–194. doi: 10.1017/S003329170002105X. [DOI] [PubMed] [Google Scholar]
- 54.World Health Organization . AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. 2. Geneva: World Health Organization; 2001. [Google Scholar]
- 55.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 56.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-Country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 57.Andersson T, Alfredsson L, Källberg H, et al. Calculating measures of biological interaction. Eur J. 2005;20:575–579. doi: 10.1007/s10654-005-7835-x. [DOI] [PubMed] [Google Scholar]
- 58.Knol MJ, van der Tweel I, Grobbee DE, et al. Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int J Epidemiol. 2007;36:1111–1118. doi: 10.1093/ije/dym157. [DOI] [PubMed] [Google Scholar]
- 59.Nakagawa S, Johnson PCD, Schielzeth H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface. 2017;14:20170213. doi: 10.1098/rsif.2017.0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.R Core Team (2018) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. Available online at .https://www.R-project.org/
- 61.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc: Ser B (Methodol) 1995;57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 62.Marees AT, Smit DJA, Abdellaoui A, et al. Genetic correlates of socio-economic status influence the pattern of shared heritability across mental health traits. Nat Hum Behav. 2021;5:1065–1073. doi: 10.1038/s41562-021-01053-4.Genetic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hill WD, Hagenaars SP, Marioni RE, et al. Molecular genetic contributions to social deprivation and household income in UK biobank report. Curr Biol. 2016;26:3083–3089. doi: 10.1016/j.cub.2016.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Franz CE, York TP, Eaves LJ, et al. Adult romantic attachment, negative emotionality, and depressive symptoms in middle aged men: a multivariate genetic analysis. Behav Genet. 2011;41:488–498. doi: 10.1007/s10519-010-9428-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Joosten DHJ, Nelemans SA, Meeus W, Branje S. Longitudinal associations between depressive symptoms and quality of romantic relationships in late adolescence. J Youth Adolesc. 2022;51:509–523. doi: 10.1007/s10964-021-01511-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Avinun R, Knafo A. Parenting as a reaction evoked by children’s genotype: a meta-analysis of children-as-twins studies. Pers Soc Psychol Rev. 2014;18:87–102. doi: 10.1177/1088868313498308. [DOI] [PubMed] [Google Scholar]
- 67.Jenkins JM, McGowan P, Knafo-Noam A. Parent-offspring transaction: mechanisms and the value of within family designs. Horm Behav. 2016;77:53–61. doi: 10.1016/j.yhbeh.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 68.Grätz M. Competition in the family: Inequality between siblings and the intergenerational transmission of educational advantage. Sociol Sci. 2018;5:246–269. doi: 10.15195/v5.a11. [DOI] [Google Scholar]
- 69.Whiteman SD, Jensen AC, Maggs JL. Similarities in adolescent siblings’ substance use: testing competing pathways of influence. J Stud Alcohol Drugs. 2013;74:104–113. doi: 10.15288/jsad.2013.74.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pacek LR, Martins SS, Crum RM. The bidirectional relationships between alcohol, cannabis, co-occurring alcohol and cannabis use disorders with major depressive disorder: results from a national sample. J Affect Disord. 2013;148:188–195. doi: 10.1016/j.jad.2012.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gelman A, Hill J, Vehtari A. Regression and other stories. Cambridge: Cambridge University Press; 2020. [Google Scholar]
- 72.Spinhoven P, Elzinga BM, Hovens JGFM, et al. The specificity of childhood adversities and negative life events across the life span to anxiety and depressive disorders. J Affect Disord. 2010;126:103–112. doi: 10.1016/j.jad.2010.02.132. [DOI] [PubMed] [Google Scholar]
- 73.Kullberg M-L, Maciejewski D, van Schie CC, et al. Parental bonding: psychometric properties and association with lifetime depression and anxiety disorders. Psychol Assess. 2020;32:780–795. doi: 10.1037/pas0000864. [DOI] [PubMed] [Google Scholar]
- 74.Burns RA, Loh V, Byles JE, Kendig HL. The impact of childhood parental quality on mental health outcomes in older adults. Aging Ment Health. 2018;22:819–825. doi: 10.1080/13607863.2017.1317331. [DOI] [PubMed] [Google Scholar]
- 75.Reuben A, Moffitt TE, Caspi A, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry. 2016;57:1103–1112. doi: 10.1111/jcpp.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Goltermann J, Meinert S, Hülsmann C, et al. Temporal stability and state-dependence of retrospective self-reports of childhood maltreatment in major depression: a two-year longitudinal analysis of the childhood trauma questionnaire. medRxiv. 2021 doi: 10.1101/2021.08.31.21262884. [DOI] [Google Scholar]
- 77.Rosmalen JGM, Bos EH, de Jonge P. Validation of the long-term difficulties inventory (LDI) and the list of threatening experiences (LTE) as measures of stress in epidemiological population-based cohort studies. Psychol Med. 2012;42:2599–2608. doi: 10.1017/S0033291712000608. [DOI] [PubMed] [Google Scholar]
- 78.Murphy E, Wickramaratne P, Weissman M. The stability of parental bonding reports: a 20-year follow-up. J Affect Disord. 2010;125:307–315. doi: 10.1016/j.jad.2010.01.003.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Götz FM, Gosling SD, Rentfrow PJ. Small effects: the indispensable foundation for a cumulative psychological science. Perspect Psychol Sci. 2022;17:205–215. doi: 10.1177/1745691620984483. [DOI] [PubMed] [Google Scholar]
- 80.McCutcheon VV, Heath AC, Nelson EN, et al. Accumulation of trauma over time and risk for depression in a twin sample. Psychol Med. 2009;39:431–441. doi: 10.1017/S0033291708003759.Accumulation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Infurna FJ, Rivers CT, Reich J, Zautra AJ. Childhood trauma and personal mastery: their influence on emotional reactivity to everyday events in a community sample of middle-aged adults. PLoS ONE. 2015;10:1–21. doi: 10.1371/journal.pone.0121840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Evans GW, de France K. Childhood poverty and psychological well-being: the mediating role of cumulative risk exposure. Dev Psychopathol. 2022;34:911–921. doi: 10.1017/S0954579420001947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dean K, Green MJ, Laurens KR, et al. The impact of parental mental illness across the full diagnostic spectrum on externalising and internalising vulnerabilities in young offspring. Psychol Med. 2018;48:2257–2263. doi: 10.1017/S0033291717003786. [DOI] [PubMed] [Google Scholar]
- 84.Martel MM, Pan PM, Hoffmann MS, et al. A general psychopathology factor (P Factor) in children: structural model analysis and external validation through familial risk and child global executive function. J Abnorm Psychol. 2017;126:137–148. doi: 10.1037/abn0000205. [DOI] [PubMed] [Google Scholar]
- 85.McLaughlin KA, Gadermann AM, Hwang I, et al. Parent psychopathology and offspring mental disorders: results from the WHO world mental health surveys. Br J Psychiatry. 2012;200:290–299. doi: 10.1192/bjp.bp.111.101253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Althouse AD. Adjust for multiple comparisons? It’s not that simple. Ann Thorac Surg. 2016;101:1644–1645. doi: 10.1016/j.athoracsur.2015.11.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available via the website of NESDA (https://www.nesda.nl/pro-index/), which will be provided after handing in a data request. This paper was pre-registered on the Open Science Framework; here, the R code for the analyses can be found as well (https://www.osf.io/kzq3p/?view_only=a65ae8fac4154d65857773212ede73e5).