Abstract
Background
Constipation is a digestive disorder with a high global prevalence, with approximately 20–25% of the population suffering from constipation, and the majority of constipated patients experience functional constipation (FC). Although abdominal massage is an effective intervention, there is a lack of analysis of the efficacy of abdominal massage in the treatment of functional constipation. Objective: To evaluate the clinical efficacy of abdominal massage in the treatment of functional constipation.
Methods
A computerized retrieval of randomized controlled trials on abdominal massage for functional constipation was conducted on China National Knowledge Infrastructure (CNKI), Wanfang, VIP Chinese Science and Technology Periodical Database, Chinese BioMedical Literature Database, Cochrane Database, PubMed, Embase, and Web of Science until October 1, 2022. Meta-analysis was performed using RevMan 5.3 software after the initial screening and re-screening of the literature.
Results
A total of 13 papers involving 830 patients were included. The results of the meta-analysis showed that abdominal massage had better efficacy in the treatment of functional constipation. Constipated patients in the treatment group showed greater improvement in the frequency of defecation, difficulty in defecation, stool properties, and PAC-QOL scores than those in the control group. The SMD/MD values and 95% CI of each score were: SMD = 1.05, 95%CI (0.63,1.46); SMD = −1.51, 95%CI (−2.35,-0.68); SMD = 0.95, 95%CI (0.31,1.59); MD = −13.24, 95%CI (−25.83, −0.65).
Conclusion
Abdominal massage can increase the frequency of defecation, reduce the symptoms of difficulty in defecation, improve stool properties, and positively affect the quality of life of patients with constipation. Hence, abdominal massage therapy shows definite therapeutic efficacy for functional constipation, providing a more specific plan for clinical treatment.
Keywords: Functional constipation, Abdominal massage, Other therapies, Meta-analysis
1. Introduction
Functional constipation (FC) is a common clinical condition and a digestive disorder with a high global prevalence that is mainly induced by non-systemic diseases or organic changes in the intestinal tract and characterized by difficulty in defecation, reduced frequency of defecation or a sense of incomplete defecation [1,2]. A study by Chen et al. [3] suggests that approximately 20–25% of the population is affected by constipation, with more female victims and a male-to-female ratio of 1:2.2. The prevalence of functional constipation in China is about 6% [4]. Chronic constipation not only reduces the quality of life of patients and causes problems in the genitourinary system, circulatory system, nervous system, and other systems [[5], [6], [7]], but also poses a significant physical and psychological risk to patients [8]. Due to the long treatment period, multiple causes of constipation, poor clinical efficacy, recurrent symptoms, and difficulty in eradicating constipation, a large number of medical resources are used [9].
Currently, the traditional treatment options for functional constipation include dietary interventions, habit development, biofeedback training, and other lifestyle education and pharmacological treatment such as volumetric laxatives, oil-based lubricants, and intestinal pro-secretory drugs [10]. However, a study by Silva et al. [11] indicates that the cure rate of traditional treatment plans is only 50–60%. Moreover, long-term use of laxatives can cause contraction of intestinal smooth muscle, resulting in loss of bowel sensation and increased rectal tension due to fecal obstruction [12]. Excessive use of laxatives, enemas, or suppositories can aggravate constipation and even lead to intractable constipation without laxatives [13]. Dietary interventions, habit development, biofeedback training, and other lifestyle education have no side effects but require long-term adherence to be effective. Nonetheless, most patients are unable to adhere to them regularly due to their dietary habits, and work and life demands. Therefore, finding a protocol that does not require long-term adherence and is free of side effects with good efficacy has become an urgent need for the treatment of constipation. Zhi et al. [14] proved through a meta-analysis that pediatric massage is highly effective and safe in treating functional constipation in children, and it can effectively improve constipation symptoms, relieve defecation difficulties and have many other advantages. However, the studies are limited to infants and children, and there is a lack of analysis of the efficacy of abdominal massage in the treatment of functional constipation in adults. In summary, by collecting clinical literature on abdominal massage for functional constipation, we conducted a meta-analysis of its clinical efficacy in order to provide a basis for choosing a more reasonable treatment for functional constipation.
2. Data and method
2.1. Retrieval strategy
The systematic evaluation was registered on PROSPERO (CRD42023388539) and was conducted according to the recommendations in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15].
Computer retrieval of clinical literature on abdominal massage for functional constipation published up to October 1, 2022 was conducted in China National Knowledge Infrastructure (CNKI), Wanfang, VIP Chinese Science and Technology Periodical Database, Chinese BioMedical Literature Database, Cochrane Database, PubMed, Embase, and Web of Science.
Chinese and English literature were retrieved using a combination of subject terms and free words. Chinese retrieval terms included abdomen, Tuina + massage, randomized, constipation, and English retrieval terms included masso therapy, massotherapy, sports massage, Massage, Massage Therapies, Massage Therapy, Zone Therapies, Zone Therapy, constipation, rectal constipation, slow transit constipation, Colonic Inertia, Dyschezia, obstipation.
A cross-retrieval was conducted to screen the literature that met the inclusion criteria.
2.2. Inclusion and exclusion criteria
2.2.1. Literature inclusion criteria
(1) Study type: RCT of abdominal massage for functional constipation; (2) Study subjects: patients with functional constipation with clearly recognized diagnostic criteria; (3) Age ≥18 years old, no restrictions on case source, number of cases, duration of disease, or gender; (4) Interventions: the observation group used massage therapy combined with basic therapy, or massage therapy combined with other therapies, with unlimited time and duration of massage therapy, and the treatment site was abdomen. Other therapies include oral Western medicine, intestinal care, lifestyle education, and physical therapy. The control group used basic therapy or other therapies without massage therapy (the basic therapy or other therapies were the same in both groups).
2.2.2. Literature exclusion criteria
(1) Non-RCT studies, such as conference abstracts, review papers, dissertations, registration documents, clinical experience summary analysis, clinical case reports, animal experiments, etc.; (2) Lack of clearly recognized diagnostic criteria; (3) Other treatments such as the combination of drugs, acupuncture, acupoint application, etc. in the observation and control groups; (4) Incorrect or incomplete case data.
2.3. Outcome measures
The evaluation indexes included frequency of defecation, total score, and four dimensional scores (somatic discomfort, psychosocial discomfort, anxiety/worries, satisfaction) of the PAC-QOL (Patient-Assessment of Constipation Quality of Life), total score of the Constipation Assessment Scale (CAS), total score of severity of defecation, difficulty in defecation, score of stool properties, duration of defecation, a sense of incomplete defecation, abdominal distension, and pain.
2.4. Literature screening and data extraction
The literature retrieval was conducted independently by 2 researchers, and the retrieved literature was imported into the End-Note ×9 software for management. All papers were screened according to preset inclusion/exclusion criteria; repeated papers from different databases were excluded, and then any obviously irrelevant papers were excluded according to their titles and abstracts. Lastly, the full text of the remaining literature was read closely, and those papers that met the requirements were included. The final data were cross-checked. Any disagreements were resolved by discussion or arbitration by a third researcher. Extracted data included the name of the first author, year of publication, sample size, gender of participants, interventions in the observation and control groups, duration of treatment, and evaluation of the quality of the literature.
2.5. Quality evaluation
The quality of the literature was evaluated using the “bias risk assessment” tool recommended by the Cochrane Handbook of Systematic Reviews, which involved 7 domains: random sequence generation, random allocation concealment, double-blinding of performers and subjects, blinding in outcome assessment, data integrity, selective outcomes, and other biases. Each domain was assessed at a high, unclear, or low risk of bias. Disagreement between two researchers on the conclusions of the literature could be discussed or determined by a third researcher for inclusion. Using RevMan software, a bias risk assessment chart and a bias risk assessment table were developed to show the evaluation results of all included literature.
2.6. Statistical analysis
A spreadsheet was created to extract data. The differences in outcome indicators between the observation and control groups before and after treatment were calculated, and the differences between the treatment and control groups and their standard deviations were entered into RevMan 5.3 software by two researchers independently for meta-analysis. Mean squared differences (MD) were used to combine effect sizes when quantitative information was collected using the same scale, and standardized mean squared differences (SMD) were used to combine effect sizes when quantitative information was collected using different scales. Estimates and 95% confidence intervals (CIs) are given for each effect size. Heterogeneity tests were performed for each study. If the heterogeneity test results were P ≥ 0.1 and I2 ≤ 50%, which indicated good consistency or low heterogeneity among the included studies, a fixed-effect model was used for meta-analysis; if the heterogeneity test results were P < 0.1 and I2 >50%, which indicated high heterogeneity among the included studies, a random-effects model was selected for meta-analysis. For higher heterogeneity, subgroup analyses were performed to explore the source of the heterogeneity. Sensitivity analyses were performed on all outcomes to evaluate the stability of the study. A publication bias test was performed on outcomes reported in ≥10 studies. The presence of publication bias was evaluated by Begg's test and Egger's test in the StataSE15 software. Statistical differences were considered to exist at a two-sided P < 0.05.
2.7. Grading of evidence (GRADE level evaluation)
The evidence levels of the results of the meta-analysis in this paper were determined using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines [16], as shown in the Appendix.
3. Results
3.1. Literature retrieval results
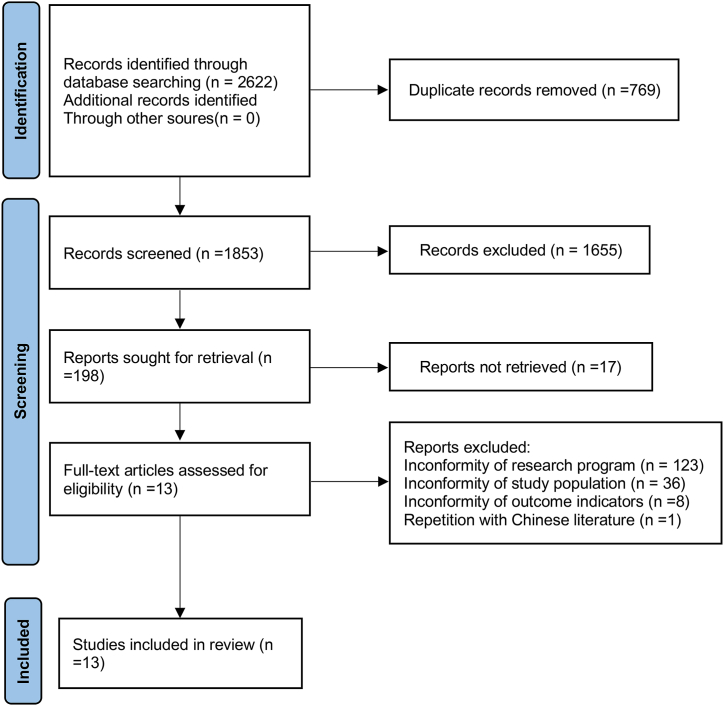
A total of 2622 papers were retrieved in the 8 databases without using other means such as manual retrieval, including 1269 papers in Chinese and 1353 papers in English. After eliminating repeated papers, reading titles and abstracts, 198 papers were initially screened out, including 91 papers in Chinese and 107 papers in English. The full text was read, and those that did not meet the inclusion criteria were screened out, including 17 papers (10 in English and 7 in Chinese) whose full text was not available. Lastly, 13 studies were finally included, among which 3 were published in Chinese [[17], [18], [19]], 9 in English [[20], [21], [22], [23], [24], [25], [26], [27], [28]], and 1 in Korean [29]. The literature screening process is shown in Fig. 1.
Fig. 1.
Literature screening process and results.
3.2. Basic characteristics of the included studies
The 13 eligible studies were all single-center clinical RCTs, with the number of patients ranging from 32 to 101, and a total of 830 patients involved. Of these, 262 patients were male and 407 were female. The gender of the remaining 161 patients was unknown, as the gender was not reported in 2 studies. The included studies were published between 2013 and 2022. The basic characteristics of the included literature are shown in Table 1.
Table 1.
Basic characteristics of the included literature.
| Study | Number of cases (T/C) | Gender (M/F) | Intervention time | Interventions |
Random method | Blinding method | Allocation concealment | Baseline consistency | |
|---|---|---|---|---|---|---|---|---|---|
| Intervention group | Control group | ||||||||
| Baran et al., 2019 | 30/30 | Unclear | 4 weeks | Abdominal massage | No specific treatment | Random allocation in individual bags | No | Reported | Consistent |
| Orhan et al., 2022 | 20/20 | 5/35 | 4 weeks | Abdominal massage + usual care | Usual care | Computer randomization | No | Reported | Consistent |
| Dogan et al., 2022 | 37/37 | 14/60 | 4 weeks | Abdominal massage + lifestyle advice | Placebo therapeutic ultrasound + lifestyle advice | Computer randomization | No | Unclear | Consistent |
| Faghihi et al., 2021 | 18/18 | 21/15 | 5 days | Abdominal massage | No specific treatment | Computer randomization | Single-blinding | Reported | Consistent |
| Faghihi et al., 2022 | 27/26 | 24/29 | 2 weeks | Abdominal Massage + oral administration of sweet almond oil | Oral administration of sweet almond oil | Computer randomization | No | Unclear | Consistent |
| Fan Ming Na et al., 2020 | 38/38 | 32/44 | 2 weeks | Abdominal massage + conventional treatment and nursing | Conventional treatment and nursing (diet, exercise, blood sugar control, gastrointestinal motility promotion, etc.) | Random number table | No | Unclear | Consistent |
| Fekri et al., 2021 | 29/34 | 19/44 | 10 days | Abdominal massage + lifestyle training | Lifestyle training | Random number table | No | Reported | Consistent |
| Lee Young Ae et al., 2013 | 20/20 | 16/24 | 3 days | Abdominal massage | No specific treatment | Assigned according to discharge date | No | Unclear | Consistent |
| Liang Bing Lian et al., 2020 | 50/50 | 64/36 | 7 days | Abdominal massage + usual care of traditional Chinese medicine | Usual care of traditional Chinese medicine | Random number table | No | Unclear | Consistent |
| Liu Wen Xia et al., 2017 | 51/50 | Unclear | 4 weeks | Abdominal Massage + oral administration of bisacodyl | Oral administration of bisacodyl | Mentioned but not described | No | Unclear | Consistent |
| McClurg et al., 2016 | 16/16 | 15/17 | 6 weeks | Abdominal massage + lifestyle advice | Lifestyle advice | Mentioned but not described | No | Unclear | Consistent |
| Mokhtare et al., 2020 | 48/47 | 32/63 | 2 weeks | Abdominal massage + polyethylene glycol | Polyethylene glycol | Computer randomization | No | Unclear | Consistent |
| Olgun et al., 2022 | 30/30 | 20/40 | 4 weeks | Abdominal massage | No specific treatment | Computer randomization | No | Unclear | Consistent |
3.3. Quality evaluation of the included studies
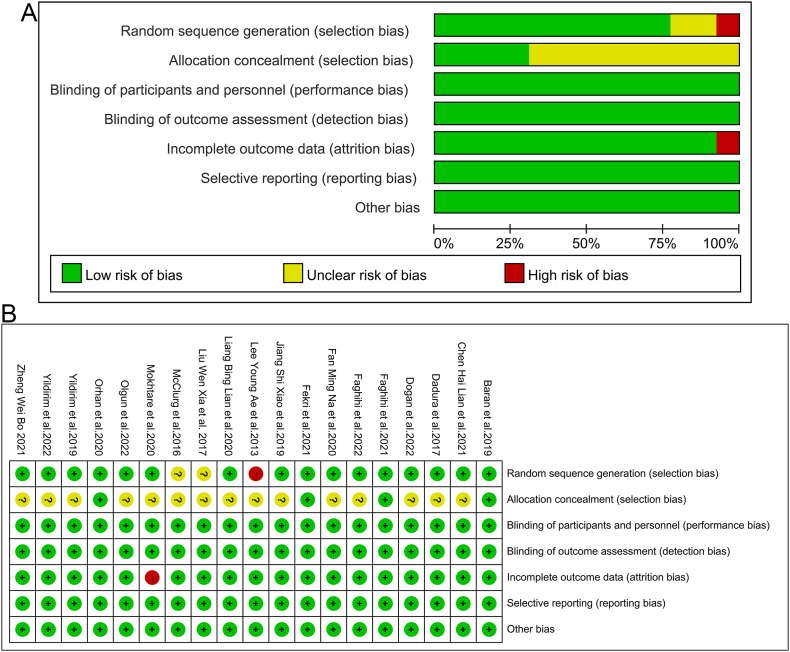
Generation of random sequences: three studies [18,19,27] used random number tables for random grouping; six studies [20,[23], [24], [25], [26],28] used computers for random grouping; one study [21] used individual bags for random assignment; one study [29] used access time for randomization, and two studies [17,22] only mentioned random grouping but did not specify the specific grouping method. Allocation concealment: a total of four studies [20,21,24,27] used allocation concealment. Investigator/subject blinding: one study [20] used single blinding and the remaining studies were unblinded, but it is unlikely that systematic reviewers were affected by the lack of blinding. Blinding of outcome evaluators: no blinding, but systematic reviewers judged that outcome measures were unlikely to be affected by the lack of blinding. Incomplete outcome data: None of the included studies had missing outcome data. Selective outcome reporting: Outcome indicators of interest to systematic reviewers were inadequately reported in one study [25]. Other sources of bias: All included studies appeared to have no other sources of bias. Fig. 2A and B summarize the detailed results of the bias risk assessment.
Fig. 2.
Risk of bias. A: graph; B: summary.
3.4. Meta-analysis results
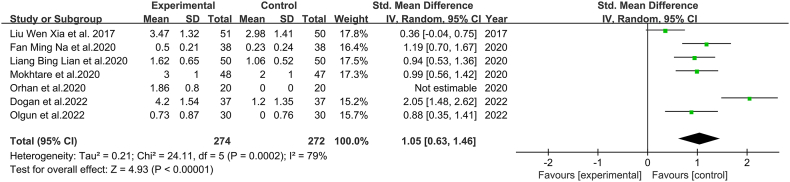
3.4.1. Comparison of scores of defecation frequency
A total of 7 papers [[17], [18], [19],[23], [24], [25],28] were included, involving 546 patients. Since different scales were used to evaluate the frequency of defecation in the included studies, SMD was used to pool effect size. Since the scoring criteria of the evaluation tools used in each study were inconsistent, a lower score in 2 studies [18,19] indicates a higher frequency of defecation and a higher score in 5 studies [17,[23], [24], [25],28] indicates a higher frequency of defecation. Therefore, the evaluation standard is the lower the score, the more frequent the defecation, and the results of the former were processed by multiplying the scale scores by −1 to ensure that the scales were evaluated in the same direction [30]. The results of the heterogeneity test showed that the heterogeneity among the studies was large (P = 0.0002, I2 = 79%). Meta-analysis using a random-effects model showed that: the improvement in the frequency of defecation was more significant in patients in the observation group than those in the control group, with a statistically significant difference [SMD = 1.05, 95%CI (0.63, 1.46), P < 0.00001], as shown in Fig. 3. The evidence classification of defecation frequency should be considered as moderate (Appendix).
Fig. 3.
Meta-analysis comparing the defecation frequency between the two groups.
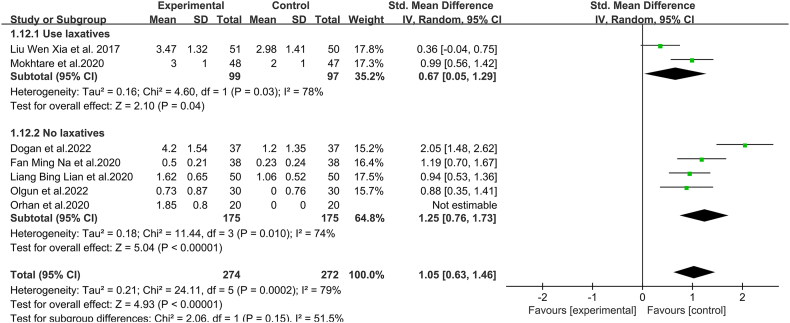
Due to I2 = 79%, a subgroup analysis was performed on the defecation frequency of patients using laxatives and not using laxatives. The heterogeneity results show that there is considerable heterogeneity between the included studies (P = 0.0002, I2 = 79%); thus, a random-effects model was used for meta-analysis. The results showed that the defecation frequency of both subgroups of patients with functional constipation treated with abdominal massage was higher than the control measures [laxative-using group: SMD = 0.67, 95%CI (0.05, 1.29), P = 0.03]; non-laxative-using group: SMD = 1.25, 95%CI (0.76, 1.73), P = 0.010], as shown in Fig. 4.
Fig. 4.
Subgroup analysis of defecation frequency in functional constipation patients treated with abdominal massage using laxatives and not using laxatives.
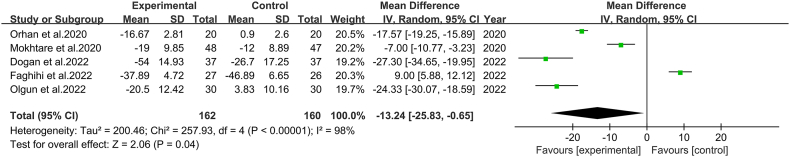
3.4.2. Comparison of total scores of PAC-QOL
A total of 5 papers [[23], [24], [25], [26],28] were included, involving 322 patients. The same scale was used to evaluate the quality of life of patients with constipation in the included studies, so MD was used to combine effect size. The results of the heterogeneity test showed that the heterogeneity between studies was large (P < 0.00001, I2 = 98%). A random-effects model was adopted for meta-analysis, and the results showed that the PAC-QOL score was higher in the observation group than those in the control group, and the difference was statistically significant [MD = −13.24, 95%CI (−25.83, −0.65), P = 0.04]. A sensitivity analysis was done, and heterogeneity was still high after elimination one by one. The cause of the increased heterogeneity could not be determined. We suggest that the higher heterogeneity may be related to a variety of factors, such as sample size, duration of treatment, different diseases of subjects included in each study, and different massage practices in the observation group (as shown in Fig. 5). Due to the high total score of PAC-QOL for constipation patients, the evidence grading of the quality of life for constipation patients should be considered high (Appendix).
Fig. 5.
Meta-analysis comparing the quality of life between two groups of constipated patients.
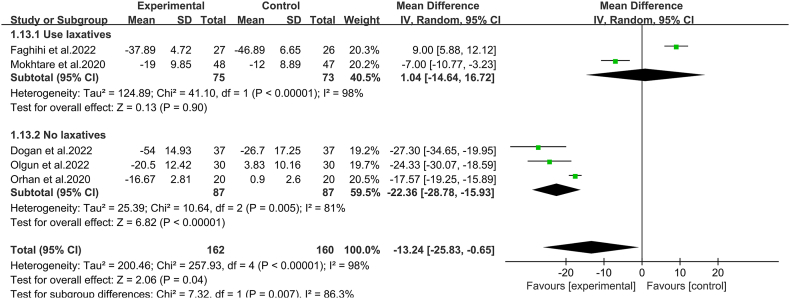
Due to I2 = 98%, a subgroup analysis was performed on the PAC-QOL of patients using laxatives and not using laxatives. The heterogeneity results show significant heterogeneity between the included studies (P < 0.00001, I2 = 98%); thus, a random-effects model was used for meta-analysis. The results showed that the PAC-QOL of both subgroups of patients with functional constipation treated with abdominal massage was higher than the control measures [laxative-using group: MD = 1.04, 95%CI (−14.64, 16.72), P < 0.00001]; non-laxative-using group: MD = −22.36, 95%CI (−28.78, −15.93), P < 0.00001], as depicted in Fig. 6.
Fig. 6.
Subgroup analysis of PAC-QOL in functional constipation patients treated with abdominal massage using laxatives and not using laxatives.
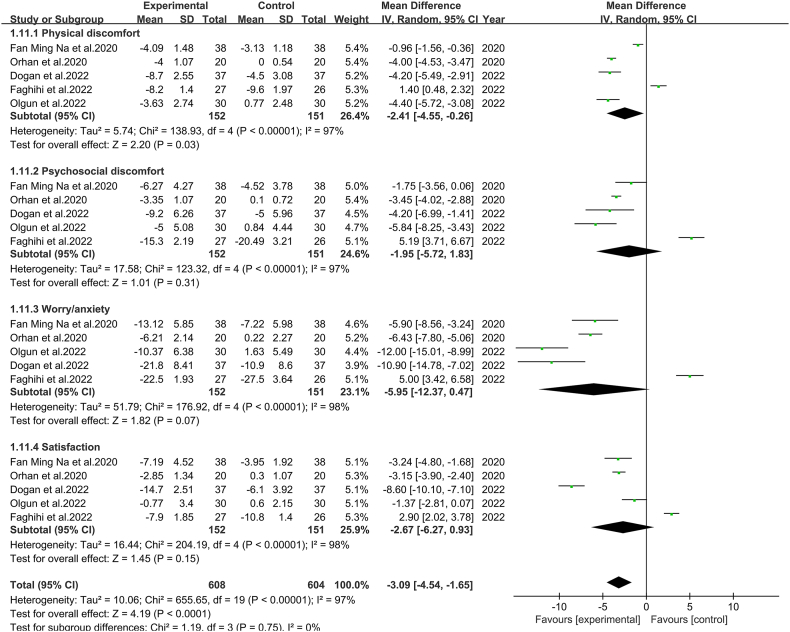
Different dimensional analyses were performed according to the PAC-QOL subscales; 5 studies [[23], [24], [25], [26],28] evaluated the effect of somatic discomfort on the quality of life of patients with constipation. 5 studies [[23], [24], [25], [26],28] evaluated the effect of psychosocial discomfort on the quality of life of patients with constipation. 5 studies [[23], [24], [25], [26],28] evaluated the effect of anxiety/worry on the quality of life of patients with constipation. 5 studies [[23], [24], [25], [26],28] evaluated satisfaction. The results of the test for heterogeneity in the somatic discomfort group showed that: the heterogeneity between studies was large (P < 0.00001, I2 = 97%). A random-effects model was used for meta-analysis, and the results showed a statistically significant difference in somatic discomfort in the observation group compared with the control group [MD = −2.41, 95%CI (−4.55, −0.26), P = 0.03]. The results of the test for heterogeneity in the psychosocial discomfort group showed that the heterogeneity between studies was large (P < 0.00001, I2 = 97%). Meta-analysis using a random-effects model showed that there was a statistically significant difference in the psychosocial discomfort of patients in the observation group compared with the control group [MD = −1.95, 95%CI (−5.72, 1.83), P = 0.31]. The results of the test for heterogeneity in the anxiety/worry group showed that: the heterogeneity between studies was large P < 0.00001, I2 = 98%). Meta-analysis using a random-effects model showed that there was a statistically significant difference in the improvement of anxiety/worry in the observation group compared with the control group [MD = −5.95, 95%CI (−12.37, 0.47), P = 0.07]. The results of the test for heterogeneity of satisfaction groups showed that: the heterogeneity between studies was large P < 0.00001, I2 = 98%). One stud y [26] had a scale with a higher score indicating higher satisfaction, and 4 studies [18,23,24,28] had a scale with a lower score indicating higher satisfaction. Therefore, the results of the scales in which the evaluation criterion was that higher scores indicate higher satisfaction were processed by multiplying the scale scores by −1 to ensure that the scales were evaluated in the same direction [30]. Meta-analysis using a random-effects model showed that the difference between patient satisfaction in the observation group and the control group was statistically significant [MD = −2.67, 95%CI (−6.27, 0.93), P = 0.15]. Due to the high heterogeneity, sensitivity analysis was performed, and the results showed that disease outcomes were not affected by the intervention and were not consistent with the overall results. The reasons for the increased heterogeneity could not be determined. Influencing factors may be sample size, duration of treatment, different diseases of subjects included in each study, different massage practices in the observation group, and different criteria for judging efficacy. The results are illustrated in Fig. 7.
Fig. 7.
Meta-analysis comparing different dimensions of PAC-QOL between the two groups.
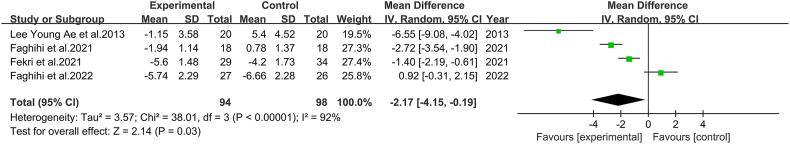
3.4.3. Comparison of total scores of Constipation Assessment Scale (CAS)
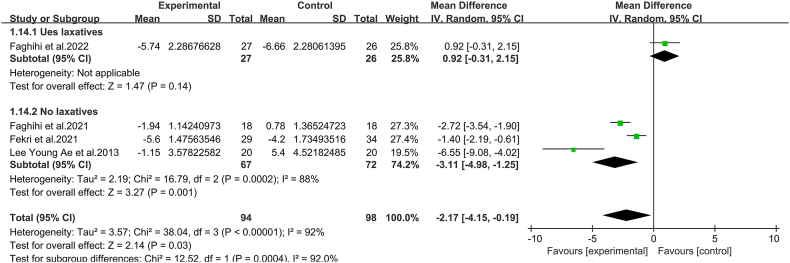
A total of 4 papers [20,26,27,29] involving 192 patients were included. The MD was used to combine effect size because the same scale was used to evaluate the included studies. The results of the heterogeneity test showed that the heterogeneity between studies was large (P < 0.00001, I2 = 92%). Meta-analysis using a random-effects model showed that patients in the observation group had better CAS scores than those in the control group, with a statistically significant difference [MD = −2.17, 95%CI (−4.15, −0.19), P = 0.03] (as shown in Fig. 8). Evidence grading for the comparison of the total scores of CAS should be considered as moderate (Appendix).
Fig. 8.
Meta-analysis comparing the total scores of the Constipation Assessment Scale (CAS) between the two groups.
Owing to I2 = 92%, a subgroup analysis was carried out on the CAS scores of patients who used laxatives and did not use laxatives. The heterogeneity results indicate substantial heterogeneity among the included studies (P < 0.00001, I2 = 92%). Hence, a random-effects model was applied for the meta-analysis. The results demonstrate that the CAS of both groups of functional constipation patients treated with abdominal massage was higher than that of the control measures [non-laxative-using group: MD = −3.11, 95%CI (−4.98, −1.25), P = 0.001], as shown in Fig. 9.
Fig. 9.
Subgroup analysis of CAS in functional constipation patients treated with abdominal massage using laxatives and not using laxatives.
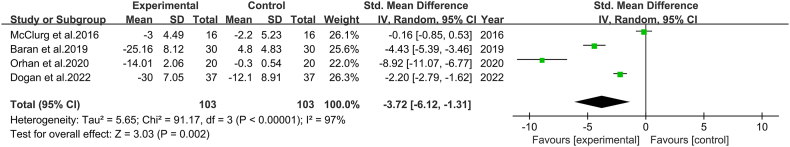
3.4.4. Comparison of the total scores of constipation severity
A total of 4 papers [[21], [22], [23], [24]] involving 206 patients were included. Different scales were used to evaluate the severity of constipation in the included studies, so the SMD combined effect size was used. The results of the heterogeneity test showed that the heterogeneity between studies was large (P < 0.00001, I2 = 97%). Meta-analysis using a random-effects model showed that the improvement in constipation severity scores was better in the observation group than in the control group, and the difference was statistically significant [SMD = −3.72, 95%CI (−6.12, −1.31), P = 0.002]. (as shown in Fig. 10). Evidence grading for the comparison of the total scores of constipation severity should be considered as high (Appendix).
Fig. 10.
Meta-analysis comparing the constipation severity between the two groups.
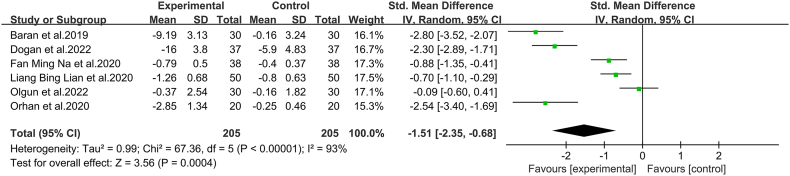
3.4.5. Comparison of scores of difficulty in defecation
A total of 6 papers [18,19,21,23,24,28] were included, involving 410 patients. Different scales were used to evaluate defecation difficulties in the included studies, so the SMD was used to combine effect size. The results of the heterogeneity test showed that the heterogeneity between studies was large (P < 0.00001, I2 = 93%). Meta-analysis using a random-effects model showed that the improvement in the score of defecation difficulties was greater in the observation group than in the control group, and the difference was statistically significant [SMD = −1.51, 95%CI (−2.35, −0.68), P=0.0004]. The heterogeneity remained high after sensitivity analysis of eliminating each study, which could be due to the specificity of the intervention measure of abdominal massage (techniques or acupoints). As shown in Fig. 11, the evidence classification for the comparison of defecation difficulty scores should be considered as moderate (Appendix).
Fig. 11.
Meta-analysis comparing the difficulty in defecation between the two groups.
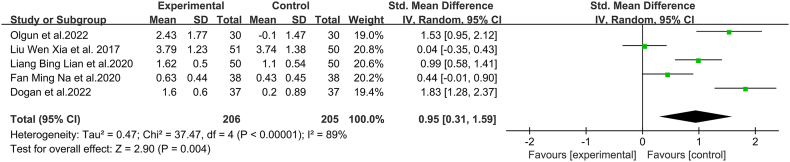
3.4.6. Comparison of scores of stool properties
A total of 5 papers [[17], [18], [19],22,28] were included, involving 411 patients. Since different scales were used to evaluate stool properties in the included studies, the SMD was used to combine effect size. Because of the inconsistent scoring criteria of the evaluation tools used in the studies, 3 studies [[17], [18], [19]] had a lower score indicating better stool properties, and 1 studies [28] had a score closer to 3–4 indicating better stool properties. Therefore, the results of studies with a lower score indicating better stool properties were processed by multiplying the scale scores by −1 to ensure that the scale evaluations pointed in the same direction [30]. The results of the heterogeneity test showed that the heterogeneity between studies was large (P < 0.00001, I2 = 89%). Meta-analysis using a random-effects model showed that patients in the observation group showed more significant improvement in stool properties than those in the control group, with a statistically significant difference [SMD = 0.95, 95%CI (0.31, 1.59), P = 0.004] (as shown in Fig. 12). Due to the high heterogeneity of scores of stool properties, the different efficacies may be obtained with different massage techniques in the intervention group, and the effect size was low, so the evidence grading should be considered moderate (Appendix).
Fig. 12.
Meta-analysis comparing the stool properties between the two groups.
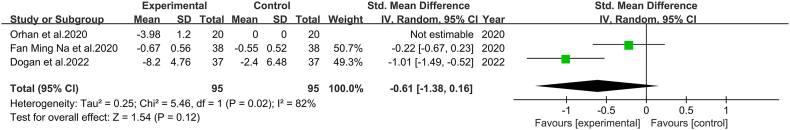
3.4.7. Comparison of scores of duration of defecation
A total of 3 papers [18,23,24] involving 190 patients were included. Different scales were used to evaluate the duration of defecation in the included studies, so the SMD combined effect size was used. The results of the heterogeneity test showed that the heterogeneity between studies was large (P = 0.02, I2 = 82%). Meta-analysis using a random-effects model showed that patients in the observation group showed more significant improvement in the scores of duration of defecation than those in the control group, with no statistically significant difference [SMD = −0.61, 95%CI (−1.38, 0.16), P = 0.12] (As depicted in Fig. 13). The evidence classification for the comparison of defecation time scores should be considered as moderate (Appendix).
Fig. 13.
Meta-analysis comparing the duration of defecation between the two groups.
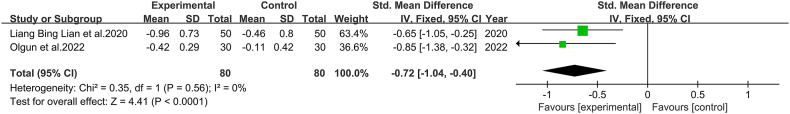
3.4.8. Comparison of scores of the sense of incomplete defecation
A total of 2 papers [19,28] involving 160 patients were included. Different scales were used in the included studies to evaluate the sense of incomplete defecation, so SMD was used to combine effect size. The heterogeneity test results show minor heterogeneity between studies (P = 0.56, I2 = 0%). A fixed-effects model was used for the meta-analysis. The results showed that the score improvement for the sensation of incomplete evacuation in the observation group was superior to the control group, and the difference was statistically significant [SMD = −0.72, 95%CI (−1.04,-0.40), P < 0.0001] (as shown in Fig. 14). Although there was little heterogeneity and the included studies lacked blinding, it didn't significantly affect the interpretation of the observers and the measured results. Thus, the evidence classification of the score for the sensation of incomplete evacuation should be considered as moderate (Appendix).
Fig. 14.
Meta-analysis comparing the sense of incomplete defecation between the two groups.
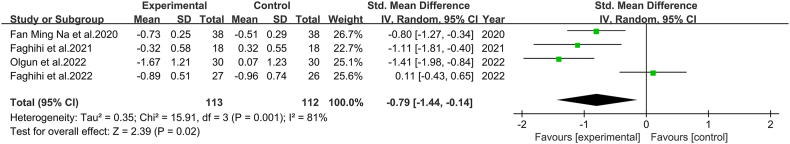
3.4.9. Comparison of abdominal distension scores
A total of 4 papers [18,20,26,28] involving 225 patients were included. Different scales were used to evaluate abdominal distension in the included studies, so SMD was used to combine effect size. The results of the heterogeneity test showed a large heterogeneity between studies (P = 0.001, I2 = 81%). Meta-analysis using a random-effects model showed that patients in the observation group improved their abdominal distension scores more significantly than those in the control group, with a statistically significant difference [SMD = −0.79, 95%CI (−1.44, −0.14), P = 0.02] (as shown in Fig. 15). Due to the large heterogeneity and the lack of blinding involved in the study, the evidence grading of the abdominal distension score should be considered as low (Appendix).
Fig. 15.
Meta-analysis comparing the scores of abdominal distension between the two groups.
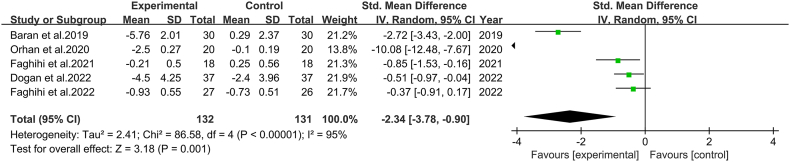
3.4.10. Comparison of pain scores
A total of 5 papers [20,21,23,24,26] were included, involving 263 patients. Different scales were used to evaluate pain in the included studies, so the SMD combined effect size was used. The results of the heterogeneity test showed that the heterogeneity between studies was large (P < 0.00001, I2 = 95%). Meta-analysis using a random-effects model showed that the improvement in pain scores was greater in the observation group than in the control group, with a statistically significant difference [SMD = −2.34, 95%CI (−3.78,-0.90), P = 0.001] (as shown in Fig. 16). Due to the large heterogeneity and the lack of blinding in the included studies, the evidence grading of the pain score should be considered as moderate (Appendix).
Fig. 16.
Meta-analysis comparing the scores of pain between two groups.
3.4.11. Publication bias detection
As the number of studies included in the outcome indicators of this study is all less than 10, no publication bias test was conducted.
4. Discussion
This meta-analysis of 13 pieces of literature shows that abdominal massage therapy for functional constipation outperforms the control measure in defecation frequency, CAS total score, total score of defecation severity, defecation difficulty, stool properties score, defecation time, sensation of incomplete evacuation, bloating, and pain. In addition, we analyzed the total PAC-QOL score and the specific four-item scores. This score assesses the impact of functional constipation on patients' quality of life in four major areas: somatic discomfort, psychosocial discomfort, anxiety/worry, and satisfaction, based on patient-related symptoms and signs. The PAC-QOL total score and the specific four-item scores of the abdominal massage group were better than those of the control group, indicating that abdominal massage therapy for functional constipation has certain clinical efficacy, and has a positive impact on the quality of life of patients. The included studies are largely heterogeneous, mainly likely due to the specificity of massage interventions (techniques/acupoints, etc.), and this specificity, like other traditional Chinese medicine interventions (acupuncture), is not uniform. However, this article focuses on population characteristics and research methodology similarities, so we believe this heterogeneity is acceptable.
Ten separate studies have shown that abdominal massage can increase defecation frequency and relieve difficulty in defecation. The earliest symptom of functional constipation is reduced frequency of defecation with difficulty in defecation. Liu Yanping et al. [31] that massage has the effect of regulating gastrointestinal function and helps to strengthen gastrointestinal motility, with effects and mechanisms similar to those of intestinal motility drugs, and is an important external treatment for functional constipation. Li Huanan et al. [32] found that abdominal massage may improve the functional area of the brain effectively by means of the brain-gut axis, while using the plasma neurotransmitters SP and VIP as bridging links to feed back the signals integrated by the brain, thus regulating and improving the contraction of smooth muscle cells through the activation of ion channels, and exerting its regulatory role in intestinal motility. It was demonstrated that abdominal massage can effectively stimulate intestinal peristalsis and improve intestinal dynamics, thus increasing the frequency of defecation and alleviating difficulty in defecation. Boonruab et al. [33] showed that there was no significant difference in terms of defecation frequency between massage therapy and Senokot therapy in statistical analysis, but the stool properties of massage therapy were better than those of Senokot therapy, and massage therapy led to more continuous defecation management, with an ideal defecation frequency reaching 75%, while the ideal defecation frequency of Senokot group was only 25%. Consideration may be given to the influence of the medication factor in Senokot therapy. Although there was no significant difference in the frequency of defecation, the massage therapy showed significantly better stool properties than the Senokot therapy.
Seven studies have shown that abdominal massage is effective in improving stool properties in patients with functional constipation. Hard stools are one of the causes of difficulty in defecation. In abdominal massage, mechanical and reflexive effects on the intestine are produced by manual pressure on the anterior abdominal wall, which promotes bowel motility and increases contractility by increasing the movement of substances in the intestine, shortening the transition period of feces in the intestine, thus softening feces and facilitating its movement in the colon [23,28] Lamas et al. [34] found no significant changes in stool properties in patients treated with abdominal massage. In this study protocol, the use of laxatives was not discontinued in the massage and control groups during the eight-week-long course of treatment. The lack of significant change in stool properties may be related to the prolonged use of laxatives.
Seven studies evaluated the effect of abdominal massage on the quality of life of patients with constipation in different dimensions. The results all showed that abdominal massage was effective in improving the quality of life of patients. Studies have shown [9,35] that patients with functional constipation have more psychosocial problems than normal individuals, with anxiety and depression being the most prevalent. Abdominal massage improves the anxiety of constipated patients by relieving the symptoms of constipation. Walker et al. [36] found that the majority of participants in the intervention group felt that abdominal massage improved physical symptoms (including improving intestinal function, shortened the duration of defecation, reduced tension and abdominal distension, increased completeness of emptying, and reducing dependence on laxatives), and relieved emotional symptoms.
In conclusion, abdominal massage is effective in improving the symptoms of patients with constipation and can have a positive impact on the quality of life of patients.
There are some limitations in this study. First, the underlying diseases of the subjects in this study varied, except for functional constipation, which may have an impact on the study results. Second, the assessment scales used for some of the outcome indicators in the included studies were different, and there may be some measurement bias. Third, most included studies did not specify the allocation concealment, which may have influenced the evaluation results.
5. Conclusion
Currently, no meta-analyses concerning abdominal massage treatment for functional constipation are found in various databases. This meta-analysis includes recent RCTs on abdominal massage treatment for FC and analyzes multiple evaluation outcome indicators, providing valuable references for clinical treatment. The results of this study show that abdominal massage treatment can increase defecation frequency, reduce defecation time, improve stool properties, alleviate symptoms such as defecation difficulty, pain, bloating, and sensation of incomplete evacuation, and positively impact the quality of life of constipation patients. Therefore, in clinical practice, abdominal massage might be an effective and safe method to treat FC. However, these findings need to be proved by future high-quality studies.
Author contributions
Xinxin Gu and Lei Zhang wrote the main manuscript text. Haiguang Yuan and Min Zhang collected and analyzed data. All authors have read and approved the final version of the manuscript.
Funding
Scientific Research Project of Affiliated Hospital of Shaanxi University of Chinese Medicine (2020ZWBKF007).
The fund was not involved in any study design, data collection, analysis and interpretation, report writing, and article submission for publication.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Supplementary content related to this article has been publish online at [URL].
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e18098.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Wang F., Sun S., Yin Z., et al. Acupuncture point patching for functional constipation: digging into the rules of acupuncture point selection and medication use. Chinese Acupunc. 2021;41:5. doi: 10.13703/j.0255-2930.20200823-k0003. [DOI] [Google Scholar]
- 2.Kassolik K., Andrzejewski W., Wilk I., et al. The effectiveness of massage based on the tensegrity principle compared with classical abdominal massage performed on patients with constipation. Arch. Gerontol. Geriatr. 2015;61:202–211. doi: 10.1016/j.archger.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Chen H., Tan P.S., Li C.P., et al. Acupoint massage therapy alters the composition of gut microbiome in functional constipation patients, evidence-based complementary and alternative medicine. eCAM. 2021;2021 doi: 10.1155/2021/1416236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J., Chen J., Ke X. Consensus opinion on the combined diagnosis and treatment of functional constipation in Chinese and Western medicine. Chinese J. Integrat. Gastroenterol. 2017;26(2018):9. doi: 10.3969/j.issn.1671-038X.2018.01.03. [DOI] [Google Scholar]
- 5.Zhang B., Wei A., Chen X., et al. Investigation of the relationship between constipation and Alzheimer's disease. Chinese J. Gerontol. 2009;29:3. doi: 10.3969/j.issn.1005-9202.2009.22.043. [DOI] [Google Scholar]
- 6.Wang L. Southern Medical University; 2013. Correlation between Post-stroke Constipation and Cognitive Function and its Intervention Study. [Google Scholar]
- 7.Zeng T. Constipation - a common and unrecognized cause of enuresis. Int. J. Urol. 1987;6:41–42. [Google Scholar]
- 8.Durmuş İskender M., Çalışkan N. Effect of acupressure and abdominal massage on constipation in patients with total knee arthroplasty: a randomized controlled study. Clin. Nurs. Res. 2022;31:453–462. doi: 10.1177/10547738211033917. [DOI] [PubMed] [Google Scholar]
- 9.Wang H., Chen J., Yao S. Progress in the study of socio-demographic characteristics and psycho-psychological conditions of patients with functional constipation. Med. Rev. 2019;25 [Google Scholar]
- 10.Sun Y., Li Y., Liang H., et al. Data mining based study on the dosing pattern of Lujinguen's formula for functional constipation. Shanghai J. Tradit. Chin. Med. 2022;56:21–28. [Google Scholar]
- 11.Silva C.A., Motta M.E. The use of abdominal muscle training, breathing exercises and abdominal massage to treat paediatric chronic functional constipation, Colorectal disease. Off. J. Assoc. Coloproctol. Great Britain and Ireland. 2013;15:e250–e255. doi: 10.1111/codi.12160. [DOI] [PubMed] [Google Scholar]
- 12.Ho M.H., Chang H.C.R., Liu M.F., et al. Effectiveness of acupoint pressure on older people with constipation in nursing homes: a double-blind quasi-experimental study. Contemp. Nurse. 2020;56:417–427. doi: 10.1080/10376178.2020.1813042. [DOI] [PubMed] [Google Scholar]
- 13.Li M., Chen Y., Ge B., et al. Clinical efficacy of Ten Treasure Bowel Formula in the treatment of laxative-dependent constipation of Qi-Yin type and its effect on the barrier function of intestinal mucosa. Mod. J. Integrat. Chinese West. Med. 2021;30:1627–1631+1636. [Google Scholar]
- 14.Liu Z., Gang L., Yunwei M., et al. Clinical efficacy of infantile massage in the treatment of infant functional constipation: a Meta-analysis. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.663581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. (Clinical research ed.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Su X., Qian H., Chen B., et al. Acupuncture for acute low back pain: a systematic review and meta-analysis. Ann. Palliat. Med. 2021;10:3924–3936. doi: 10.21037/apm-20-1998. [DOI] [PubMed] [Google Scholar]
- 17.Liu W., Liu Z. The efficacy of abdominal acupressure in the treatment of functional constipation in the elderly. Gastroenterology. 2017;22:367–369. doi: 10.3969/j.issn.1008-7125.2017.06.009. [DOI] [Google Scholar]
- 18.Fan M., Chang L., Yang X. Clinical study on abdominal tuina for the treatment of diabetic constipation in the elderly. New Chinese Med. 2020;52:4. doi: 10.13457/j.cnki.jncm.2020.16.039. [DOI] [Google Scholar]
- 19.Liang B., Feng L., Zhang M., et al. The effect of "Fu Yuan Tong Qi" abdominal massage method on the care of constipation after stroke. J. Clin. Nurs. 2020;19:3. doi: 10.3969/j.issn.1671-8933.2020.03.030. [DOI] [Google Scholar]
- 20.Faghihi A., Najafi S.S., Hashempur M.H., et al. The effect of abdominal massage with extra-virgin olive oil on constipation among elderly individuals: a randomized controlled clinical trial. Int. J. Commun. Base. Nurs. Midwifery. 2021;9:268–277. doi: 10.30476/ijcbnm.2021.88206.1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baran A., Ates S. The effects of abdominal massage in the management of constipation in elderly people: a randomized controlled study. Top. Geriatr. Rehabil. 2019;35:134–140. [Google Scholar]
- 22.McClurg D., Hagen S., Jamieson K., et al. Abdominal massage for the alleviation of symptoms of constipation in people with Parkinson's: a randomised controlled pilot study. Age Ageing. 2016;45:299–303. doi: 10.1093/ageing/afw005. [DOI] [PubMed] [Google Scholar]
- 23.Doğan İ G., Gürşen C., Akbayrak T., et al. Abdominal massage in functional chronic constipation: a randomized placebo-controlled trial. Phys. Ther. 2022;102 doi: 10.1093/ptj/pzac058. [DOI] [PubMed] [Google Scholar]
- 24.Orhan C., Özgül S., Baran E., et al. Comparison of connective tissue manipulation and abdominal massage combined with usual care vs usual care alone for chronic constipation: a randomized controlled trial. J. Manipulative Physiol. Therapeut. 2020;43:768–778. doi: 10.1016/j.jmpt.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 25.Mokhtare M., Karimi S., Bahardoust M., et al. How adding the abdominal massage to polyethylene glycol can improve symptom and quality of life in patients with functional constipation in comparison with each one of the treatment modalities alone: a randomized clinical trial. Compl. Ther. Med. 2020;52 doi: 10.1016/j.ctim.2020.102495. [DOI] [PubMed] [Google Scholar]
- 26.Faghihi A., Zohalinezhad M.E., Najafi Kalyani M. Comparison of the effects of abdominal massage and oral administration of sweet almond oil on constipation and quality of life among elderly individuals: a single-blind clinical trial. BioMed Res. Int. 2022;2022 doi: 10.1155/2022/9661939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fekri Z., Aghebati N., Sadeghi T., et al. The effects of abdominal "I LOV U" massage along with lifestyle training on constipation and distension in the elderly with stroke. Compl. Ther. Med. 2021;57 doi: 10.1016/j.ctim.2021.102665. [DOI] [PubMed] [Google Scholar]
- 28.Ismet Eser R. The effect of abdominal massage on chronic constipation and constipation quality of life in elderly: a randomized controlled trial. Int. J. Caring Sci. 2022;15:316–324. [Google Scholar]
- 29.Lee Y., Choi H.J., Jo Y.M., et al. Effects of abdominal massage or lactic acid fermented milk for constipation in patients following spinal surgery. J. Korean Clinic. Nurs. Res. 2013;19:208–217. [Google Scholar]
- 30.Xue Y., Ding Y., Yu J., et al. Meta-analysis of the effects of a cognitive-behavioral intervention on fear of falling and balance in older adults. Nurs. Res. 2021;35:6. doi: 10.12102/j.issn.1009-6493.2021.10.004. [DOI] [Google Scholar]
- 31.Fang Y., Huang Y., Chen D., et al. 2021. Systematic Evaluation and Meta-Analysis of the Effectiveness and Safety of Tui Na in the Treatment of Functional Constipation; p. 8. Chinese Acupuncture 41. [DOI] [Google Scholar]
- 32.Li H., Wang J., Zhang W., et al. Study on the regulation mechanism of colon dynamics in rabbit model of irritable bowel syndrome with constipation by abdominal massage therapy. Liaoning J. Tradit. Chin. Med. 2022;49:210–213. doi: 10.13192/j.issn.1000-1719.2022.03.058. [DOI] [Google Scholar]
- 33.Boonruab J., Poonsuk P., Damjuti W. Effect of court-type Thai traditional massage versus Senokot treatment on chronic constipation: a randomized controlled trial. J. Evid.-Base. Integrat. Med. 2020;25 doi: 10.1177/2515690x20960644. 2515690x20960644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lämås K., Lindholm L., Stenlund H., et al. Effects of abdominal massage in management of constipation-a randomized controlled trial. Int. J. Nurs. Stud. 2009;46:759–767. doi: 10.1016/j.ijnurstu.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Ding M., Lin Z., Wang M., et al. Study on the correlation between symptoms, psychosomatic status and autonomic function in patients with functional constipation. J. Nurs. 2010;17:4. doi: 10.3969/j.issn.1008-9969.2010.07.002. [DOI] [Google Scholar]
- 36.McClurg D., Walker K., Aitchison P., et al. 2016. Abdominal Massage for the Relief of Constipation in People with Parkinson's: A Qualitative Study, Parkinson's Disease 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.