Summary
Background
The digitization of the primary care system provides an opportunity to evaluate the current use of statins in secondary prevention populations (myocardial infarction or stroke).
Methods
We conducted a cross-sectional study (ClinicalTrials.gov, NCT05285085), analysing anonymised data routinely collected by community health workers (CHW) in Brazil between May 2016 and September 2021 to assess the proportion of self-reported statins use and associated factors.
Findings
From the 2,133,900 individuals on the database, 35,103 (1.6%), mean age 66.2 years (SD14.6), 49.5% (17,382/35,103) male sex, 50.5% (17,721/35,103) female sex, and 29.6% (10,381/34,975) Caucasians, had a previous myocardial infarction (MI) (n = 11,628; 33.1%) or stroke (n = 25,925; 73.9%). Approximately 50% (17,020/35,103) were from the Northeast region, 78.7% (27,605) from urban zones, and 39.4% (13,845) with social development index (SDI) >0.7. Overall, 6.7% (2346) and 0.6% (212) reported statins and high dose statins use, respectively. Age over 60 years old (OR 1.32 [95% CI 1.19–1.47), living in the Southern region (OR 4.53 [95% CI 3.66–5.60]), having a previous diagnosis of MI (OR 4.53 [95% CI 3.66–5.60]), heart failure (OR 2.29 [95% CI 1.13–1.47]), diabetes (OR 1.50 [95% CI 1.37–1.64]), dyslipidaemia (OR 2.90 [95% CI 2.55–3.29]), chronic kidney disease (OR 1.27 [95% CI 1.08–1.48]) and use of anti-hypertensives (OR 5.47 [95% CI 4.60–6.47]) were associated with statin use.
Interpretation
The analysis of a real-world database from a digitized primary care system, allowed us to identify a very low use of statins in secondary prevention Brazilian patients, mostly influenced by socio-demographic factors and co-morbidities.
Funding
Novartis Biociências, Brazil.
Keywords: Primary care, Digital health, Statins use, Dyslipidaemia
Research in context.
Evidence before this study
We searched PubMed on April 5, 2021, without language or date restrictions using the search terms “statin use” and “low- and middle-income countries”. We identified three large important studies. The WHO study on Prevention of REcurrences of Myocardial Infarction and StrokE (WHO-PREMISE) was a cross-sectional study performed in ten LMICs from 2002 to 2003, in which 20% of patients with a previous history of cardiovascular disease reported using statins. The Prospective Urban Rural Epidemiology (PURE) cohort study was performed in 20 high-income, middle-income, and low-income countries, in which the reported use of statins for secondary prevention between 2003 and 2009 was 3.3% in low- and middle-income countries. And the Marcus et al. study carried out in 41 LMICs showed that statins were used by about one in five eligible people for secondary prevention.
Added value of this study
To our knowledge, this is the first and largest study assessing statins use from a populational routinely collected data digitized system in LMICs. Our study adds value through important findings. First, in a nationally representative cross-sectional analysis from routinely collected data, we could observe a very low use (6.7%) of statins. Second, in assessing factors associated with statin use, we observed more statin use in older individuals and with other previous cardiovascular conditions and risk factors; and less statin use mostly influenced by racial/ethnic, geographic, and behavioural aspects.
Implications of all the available evidence
Our study highlights both the role of multimorbidity in the use of statins and the role of social, demographic, and behavioural aspects in statins nonuse. Therefore, the need to scale up statin therapy to prevent and control cardiovascular disease by tailoring appropriate interventions is imperative. Initiatives that build on digitized systems, particularly in primary care, should be assessed. A potential approach to increasing statin use in LMICs would build on embedding health services research into clinical practice by evaluating the effect of tailored interventions through adequate methods while treating patients, thus creating a virtuous learning-doing cycle.
Introduction
Ischemic heart disease and stroke are responsible for more than a fifth of all deaths worldwide, especially in low and middle-income countries (LMICs), where 80% of these deaths occur.1 Considering their low cost, high safety and efficacy in lowering pro-atherogenic lipoproteins, the use of statins is an important strategy for health systems to reduce the population burden of cardiovascular diseases.2 Indeed current guidelines recommend the use of high-dose high-potency statins with the aim of reducing LDL-cholesterol by at least 50%, targeting values <50–55 mg/dL, for those individuals with previous manifestations of atherosclerotic cardiovascular disease.3, 4, 5 However, despite robust evidence-based recommendations for cholesterol lowering, most high and very high-risk individuals are not treated accordingly in different regions of the world.6, 7, 8 Recently, a cross-sectional analysis of pooled, individual-level data from nationally representative health surveys done in forty-one LMICs between 2013 and 2019 showed that only one in five eligible secondary prevention patients were taking statins.9
Myocardial infarction and stroke consist of the leading causes of death in Brazil.10, 11, 12 For the last two decades, Brazilian prevention guidelines have recommended statins and more recently high doses of these medications with the aim of reducing the burden of cardiovascular disease.3,13,14 Few studies with a relatively small number of patients indicate; however, that LDL-cholesterol levels are not adequately controlled in high-risk Brazilian patients.6,15,16 So far there is no robust and representative information on the use of statins in patients undergoing secondary prevention due to previous myocardial infarction or stroke in Brazil.
Officially, Brazil provides healthcare through two care systems: the public system, characterized by the SUS (Unified Health System), which according to the Constitution is the duty of the State; and the private system, characterized by the Supplementary Health System (comprising the health insurances) whose freedom of action was guaranteed by the Constitution and regulated by the creation of the Agência Nacional de Saúde–ANS.17 In 2020, 22.4% of the Brazilian population was assisted by the Supplementary Health System.18 Within the public system, primary care includes the Family Health Strategy (Estratégia de Saúde da Família, ESF),12 from the Brazilian Ministry of Health. This consists of a program in which community health workers (CHWs) perform home visits in primary care. The ESF currently assists 62.6% (over 131 million people) of the Brazilian population, covering 54.6% of the population in the Southeast region, 60.1% in the Midwest, 62.2% in the North, 67.6% in the South and 73.3% in the Northeast.19 Among the many health-promotion routine activities performed, CHWs check medication prescriptions and if patients are filling the latter. Therefore, this brings an opportunity to investigate how a representative part of the Brazilian population is using statins. The primary objective of this study was to evaluate if statins and other lipid lowering therapies were being used by patients that had a history of previous myocardial infarction or stroke and are assisted by CHW using a free application (ACS Lite®) for data collection at the ESF. The use of high-dose high-potency statins, or their equivalents (statins associated with ezetimibe) and factors associated with their use were investigated. In addition, we have accessed the use of other preventive therapies, specifically antihypertensive as well as antiplatelet medications.
Methods
Study design, procedures and participants
In our cross-sectional retrospective study, we analysed individual-level anonymized data extracted from a real-world database generated by a free application used by registered CHW in the context of the ESF Program in Brazil between May 2016 and September 2021. Through this application, CHWs can collect compulsory demographic and health information required by the Brazilian Ministry of Health (that is subsequently transferred to its database) as well as additional information, such as medications in use, during routine home visits.20 The nature of the ESF program, the free application, the data anonymization process as well data extraction and transfer procedures are described in the Supplementary Material.
Our study population consisted of adult individuals (age >18 years old) from both sex categorized as secondary prevention by having a history of self-reported established atherosclerotic cardiovascular disease (ASCVD) including myocardial infarction (MI), and/or stroke.
This study was approved by the Hospital Israelita Albert Einstein Ethical Committee (CAAE 53194121.0.0000.0071) and a waiver of individual consent was granted. The study was also registered on ClinicalTrials.gov (NCT05285085).
Variables of interest and outcomes
The primary outcome consisted of the proportion of MI and stroke individuals self-reporting using any statins in any dose by the data extraction date. We defined statin use based on the answer to the standard question: “Do you use any medication?” asked by the CHWs during the routine home visits. It was considered as “yes” for statins use in the case of answering yes to any of the following statins: lovastatin, simvastatin, pravastatin, fluvastatin, pitavastatin, atorvastatin, rosuvastatin; or any of the aforementioned statins and ezetimibe. Secondary outcomes included: 1) the proportion of MI and stroke patients using statins in high doses (we defined high dose statins use based on the use of atorvastatin 40–80 mg or, rosuvastatin 20–40 mg, or any dose atorvastatin, rosuvastatin, simvastatin, lovastatin, pravastatin, fluvastatin, pitavastatin associated with ezetimibe) by the data extraction date and, 2) the proportion of patients using protein convertase subtilisin kexin type 9 (PCSK9) inhibitors.
Statistical analysis
Quantitative variables were reported as a function of descriptive statistics such as: minimum, maximum, 1st and 3rd quartiles, median, mean, and standard deviation. Qualitative variables were presented in tables of crude frequencies and percentages. Missing data were counted in percentages. We performed a logistic regression model to investigate factors associated with the use of statins. The factors assessed included self-reported data on age, sex, race, or ethnicity (yellow, white, indigenous, black—as per definitions in the national CENSO), geographic region, household location (rural zone or urban zone), physical activity, smoking habit, alcohol, consumption, use of illicit drugs, use of PCSK9 inhibitors, hypertension, diabetes, dyslipidaemia, MI, stroke, use of antihypertensives, chronic kidney disease (CKD), cancer, respiratory diseases. The social development index-SDI (Índice de Desenvolvimento Humano Municipal, IDHM) was obtained from the municipal SDI available at the Instituto Brasileiro de Geografia e Estatística (IBGE) website.21 The variance inflation factor (VIF) was assessed to verify multicollinearity. Because of the high multicollinearity observed in the pre-specified model, which could have been producing parameter estimates of the “incorrect sign” we have chosen to combine two independent variables into a single index.22 Thus, “SDI” and “race or ethnicity” were combined based on the high VIF values observed (see Supplementary Material). Following this adjustment, all values for the VIF were satisfactory. Variables describing body mass index (BMI), literacy and family income were not included in the models due to the very high rate of missing values. Nevertheless, SDI represents an index that also considers the aforementioned factors. For the verification of the quality of the model, we assessed the ROC Curve. We presented the logistic regression results as odds ratios (OR) with their respective Wald 95% confidence interval (CI) and p-values (a two-sided p-value of <0.05 was considered statistically significant). All analyses and summaries were performed using R software, version 4.1.1 (R Foundation).
Role of the funding source
Members of the sponsors’ medical affairs department have contributed to the study design, results interpretation, and manuscript review.
Results
Table 1, Table 2 show the sociodemographic and clinical characteristics of MI and stroke individuals. Of the 2,133,900 individuals on the database, 35,103 (1.64%–mean age 66 years [SD 14.6], 49.5% (17,382/35,103) male sex, 50.5% (17,721/35,103) female sex, and 29.6% (10,381/34,975) Caucasians, were considered as being at secondary prevention with 11,628/35,103 (33.1%) and 25,925/35,103 (73.9%) describing a previous MI and/or stroke, respectively. Of importance, almost 50% (17,020/35,103) were from the Northeast region, 78.7% (27,605/35,103) from urban zones, with 39.4% (13,845/35,103) with social development index >0.7, 60.8% (21,343/35,103) literate and only 3.6% (1157/32,076) with income ≥4 salaries. Overall, 95.7% (33,598/35,103) reported being sedentary, 12.3% (4304/35,103) smoked, 77.3% (27,133/35,103) had hypertension, 29.2% (10,245/35,103) diabetes, 6.3% (2228/35,103) chronic kidney disease, 6.2% (2179/35,103) dyslipidaemia, 3.4% (975/35,103) neoplasms and 5.8% (2020/35,103) respiratory diseases.
Table 1.
Baseline characteristics of secondary prevention individuals.
| Secondary prevention (N = 35,103) | Complete data base (N = 2,133,900) | |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 66.2 (14.6) | 43.9 (17.8) |
| Median (Q1, Q3) | 67 (57, 77) | 42 (29, 57) |
| Min–Max | 18–115 | 18–121 |
| Age group | ||
| 18–35 years | 1064 (3.0%) | 807,751 (37.9%) |
| 36–50 years | 3903 (11.1%) | 592,793 (27.8%) |
| 51–65 years | 10,863 (30.9%) | 438,328 (20.5%) |
| 66–80 years | 13,528 (38.5%) | 228,851 (10.7%) |
| >80 years | 5745 (16.4%) | 66,177 (3.1%) |
| Missing | 0 | 0 |
| Ethnicity | ||
| Yellow | 243 (0.7%) | 15,167 (0.7%) |
| Caucasian | 10,381 (29.6%) | 531,949 (24.9%) |
| Indigenous | 81 (0.2%) | 4360 (0.2%) |
| Brown | 20,673 (58.9%) | 1,405,199 (65.9%) |
| Black | 3597 (10.2%) | 164,331 (7.7%) |
| No information | 128 (0.4%) | 12,894 (0.6%) |
| Sex | ||
| Female | 17,721 (50.5%) | 1,168,247 (54.7%) |
| Male | 17,382 (49.5%) | 965,653 (45.3%) |
| Body Mass Index (BMI) (kg/m2) | ||
| Mean (SD) | 27.2 (5.2) | 26.2 (5.1) |
| Median (Q1, Q3) | 26.5 (23.7, 30.0) | 25.4 (22.8, 29.0) |
| Min–Max | 13.2–62.6 | 7.4–68.9 |
| Missing | 29,751 | 1,826,502 |
| Body Mass Index (BMI) (kg/m2) | ||
| <18.5 | 119/5352 (2.2%) | 9125/307,398 (3.0%) |
| 18.5–24.9 | 1889/5352 (35.3%) | 133,979/307,398 (43.6%) |
| 25–29.9 | 2014/5352 (37.6%) | 103,219/307,398 (33.6%) |
| 30–34.9 | 939/5352 (17.5%) | 43,056/307,398 (14.0%) |
| 35–39.9 | 273/5352 (5.1%) | 12,967/307,398 (4.2%) |
| >40 | 118/5352 (2.2%) | 5052/307,398 (1.6%) |
| Missing | 29,751 | 1,826,502 |
Table 2.
Demographic characteristics of secondary prevention individuals.
| Secondary prevention individuals (N = 35,103) | Complete data base (N = 2,133,900) | |
|---|---|---|
| Geographic region | ||
| North | 7122/35,102 (20.3%) | 486,435/2,133,893 (22.8%) |
| South | 2162/35,102 (6.2%) | 94,609/2,133,893 (4.4%) |
| Northeast | 17,020/35,102 (48.5%) | 1,046,003/2,133,893 (49.0%) |
| Southeast | 7700/35,102 (21.9%) | 421,535/2,133,893 (19.8%) |
| Midwest | 1098/35,102 (3.1%) | 85,311/2,133,893 (4.0%) |
| Missing | 1 | 7 |
| Household location | ||
| Rural zone | 7458/35,063 (21.3%) | 526,360/2,131,460 (24.7%) |
| Urban area | 27,605/35,063 (78.7%) | 1,605,100/2,131,460 (75.3%) |
| Missing | 40 | 2440 |
| Social Development Index (SDI) | ||
| 0–0.29 | 0/35,103 (0%) | 0/2,133,816 (0%) |
| 0.3–0.49 | 263/35,103 (0.7%) | 22,632/2,133,816 (1.1%) |
| 0.5–0.69 | 20,995/35,103 (59.8%) | 1,349,538/2,133,816 (63.2%) |
| 0.7–1.0 | 13,845/35,103 (39.4%) | 761,646/2,133,816 (35.7%) |
| Missing | 0 | 84 |
| Literate | ||
| Yes | 21,343/35,103 (60.8%) | 1,530,590/2,133,900 (71.7%) |
| No | 8064/35,103 (23.0%) | 235,184/2,133,900 (11.0%) |
| Family income | ||
| ≤01 salary | 14,178/32,076 (44.2%) | 1,016,644/1,931,567 (52.6%) |
| 02–03 salaries | 12,698/32,076 (39.6%) | 574,177/1,931,567 (29.7%) |
| ≥04 salaries | 1157/32,076 (3.6%) | 56,070/1,931,567 (2.9%) |
| Not informed | 4043/32,076 (12.6%) | 284,676/1,931,567 (14.7%) |
| Missing | 3027 | 20,2333 |
| Lifestyle habits | ||
| Sedentarism | 33,598/35,103 (95.7%) | 2,045,885/2,133,900 (95.9%) |
| Smoking | 4304/35,103 (12.3%) | 166,329/2,133,900 (7.8%) |
| Alcohol use | 2552/35,103 (7.3%) | 186,085/2,133,900 (8.7%) |
| Illicit drugs use | 287/35,103 (0.8%) | 13,943/2,133,900 (0.7%) |
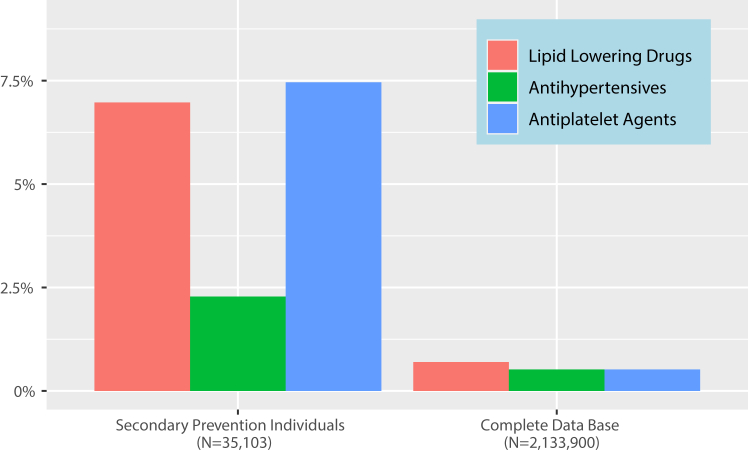
Fig. 1 shows the frequency of lipid-lowering, blood pressure and antiplatelet drugs in the study population. Overall, 6.7% (2346/35,103) and 0.6% (212/35,103) reported the use of statins and high dose statins, respectively. Only 0.4% (133/35,103) referred to use ezetimibe in association with statins and none PCSK9 inhibitors. Of those taking statins, simvastatin was the most reported (1830/2346–78%).
Fig. 1.
Lipid lowering agents and cardiovascular prevention drugs in secondary prevention individuals.
Of those with a previous MI diagnosis (n = 11,628), 9.8% (n = 1140) and 1.2% (n = 140) were in use of statins and high dose statins, respectively. For those with a previous stroke diagnosis (n = 25,925), 5.5% (1434/25,925) were in use of statins and 0.36% (94/25,925) of high doses of the latter. The use of antihypertensive and antiplatelet medications was reported by 2.3% (801/35,103) and 7.5% (2619/35,103) of these individuals with previous MI and/or stroke, respectively.
Table 3 shows the multivariable associations with statin use in the study population. Age over 60 years old (OR 1.32 [95% CI 1.19–1.47), not living in the North region of Brazil (especially in the South region (OR 4.53 [95% CI 3.66–5.60])), having a previous diagnosis of myocardial infarction (OR 4.53 [95% CI 3.66–5.60]), heart failure (OR 2.29 [95% CI 1.13–1.47]), diabetes (OR 1.50 [95% CI 1.37–1.64]), dyslipidaemia (OR 2.90 [95% CI 2.55–3.29]), chronic kidney disease (OR 1.27 [95% CI 1.08–1.48]) and use of anti-hypertensive medications (OR 5.47 [95% CI 4.60–6.47]) were independently associated with statin use. On the other hand, being non-Caucasian independently of living in high or not-high social development index regions (OR 0.78 [95% CI 0.69–0.88), living in urban areas (OR 0.85 [95% CI 0.77–0.95), sedentary lifestyle (OR 0.64 [95% CI 0.54–0.78) and smoking (OR 0.86 [95% CI 0.75–0.99) were independently associated with non-use of statins. No associations were encountered for sex or previous stroke.
Table 3.
Multivariable associations with statin use in secondary prevention individual (n = 34,934).
| Secondary prevention individuals using statins (N = 2332)a | Secondary prevention individuals not using statins (N = 32,602)a | OR (95% CI) | p-value | |
|---|---|---|---|---|
| Age group (vs. <60 years) | ||||
| ≥60 years | 1793 (76.9%) | 22,645 (69.5%) | 1.32 [1.19–1.47] | <0.0001 |
| Ethnicity/SDI (vs. Caucasian and Not High) | ||||
| Caucasian∗high | 430 (18.4%) | 4877 (15.0%) | 1.00 [0.86–1.16] | >0.95 |
| Non-caucasianb,∗ not high | 995 (42.7%) | 15,147 (46.5%) | 0.78 [0.69–0.88] | <0.001 |
| Non-caucasianb,∗ high | 434 (18.6%) | 7989 (24.5%) | 0.85 [0.73–0.98] | 0.031 |
| Gender (vs. Female) | ||||
| Male | 1200 (51.5%) | 16,103 (49.4%) | 1.08 [0.99–1.18] | 0.091 |
| Geographic region (vs. North) | ||||
| South | 275 (11.8%) | 1878 (5.8%) | 4.53 [3.66–5.60] | <0.001 |
| Northeast | 1359 (58.3%) | 15,616 (47.9%) | 3.13 [2.66–3.71] | <0.001 |
| Southeast | 453 (19.4%) | 7155 (21.9%) | 2.29 [1.91–2.76] | <0.001 |
| Midwest | 70 (3.0%) | 1025 (3.1%) | 2.48 [1.84–3.30] | <0.001 |
| Household location (vs. Rural Zone) | ||||
| Urban area | 1749 (75.0%) | 25,738 (78.9%) | 0.85 [0.77–0.95] | 0.0003 |
| Sedentary lifestyle (vs. No) | ||||
| Yes | 2181 (93.5%) | 31,256 (95.9%) | 0.64 [0.54–0.78] | <0.0001 |
| Smoking (vs. No) | ||||
| Yes | 252 (10.8%) | 4023 (12.3%) | 0.86 [0.75–0.99] | 0.042 |
| Use of antihypertensives (vs. No) | ||||
| Yes | 220 (9.4%) | 577 (1.8%) | 5.47 [4.60–6.47] | <0.001 |
| Stroke (vs. No) | ||||
| Yes | 1429 (61.3%) | 24,394 (74.8%) | 0.91 [0.78–1.07] | 0.30 |
| Myocardial infarction (vs. No) | ||||
| Yes | 1130 (48.5%) | 10,420 (32.0%) | 1.58 [1.35–1.85] | <0.0001 |
| Heart failure (vs. No) | ||||
| Yes | 337 (14.5%) | 2664 (8.2%) | 1.29 [1.13–1.47] | <0.0001 |
| Diabetes (vs. No) | ||||
| Yes | 946 (40.6%) | 9241 (28.3%) | 1.50 [1.37–1.64] | <0.0001 |
| Dyslipidaemia | ||||
| Yes | 371 (15.9%) | 1800 (5.5%) | 2.90 [2.55–3.29] | <0.0001 |
| Respiratory diseases (vs. No) | ||||
| Yes | 144 (6.2%) | 1761 (5.4%) | 0.95 [0.79–1.14] | 0.60 |
| Chronic kidney disease (vs. No) | ||||
| Yes | 214 (9.2%) | 2004 (6.1%) | 1.27 [1.08–1.48] | 0.0003 |
Acronyms and Abbreviations: OR, Odds ratio; CI, Confidence interval.
Area under the curve for the model (95% CI): 0.72 [0.71–0.73].
Reflects the actual sample size with complete data for the included variables.
Non-Caucasian includes people from Brown, Black and Yellow Ethnicity.
Table 4 shows that male sex (OR 1.59 [95% CI 1.20–2.12), not living in the Southern region (OR 6.71 [95% CI 3.05–16.4), those with previous myocardial infarction (OR 2.38 [95% CI 1.42–3.84), diabetes (OR 1.51 [95% CI 1.13–2.01), dyslipidaemia (OR 2.87 [95% CI 1.97–4.08) and using antihypertensives (OR 5.39 [95% CI 3.43–8.16) were more likely to use high-dose statins. On the contrary, a sedentary lifestyle (OR 0.53 [95% CI 0.33–0.90) and smoking (OR 0.51 [95% CI 0.29–0.84) were associated with lower odds of using high dose statins. No associations were encountered with sex, ethnicity, social development index, living or not in urban zones and previous stroke.
Table 4.
Multivariable associations with use of high dose statins in secondary prevention individuals (n = 34,934).
| Secondary prevention individuals using high-dose statins (N = 210)a | Secondary prevention individuals not using high-dose statins (N = 34,724)a | OR (95% CI) | p-value | |
|---|---|---|---|---|
| Age group (vs. <60 years) | ||||
| ≥60 years | 159 (75.7%) | 24,279 (69.9%) | 1.17 [0.85–1.63] | 0.30 |
| Ethnicity/SDI (vs. Caucasian and Not High) | ||||
| Caucasian∗high | 47 (22.4%) | 5260 (15.1%) | 1.29 [0.82–2.05] | 0.30 |
| -Not caucasianb,∗ not high | 90 (42.9%) | 16,052 (46.2%) | 0.91 [0.62–1.36] | 0.60 |
| Not caucasianb,∗ high | 32 (15.2%) | 8391 (24.2%) | 0.85 [0.52–1.39] | 0.50 |
| Gender (vs. Female) | ||||
| Male | 131 (62.4%) | 17,172 (49.5%) | 1.59 [1.20–2.12] | 0.0001 |
| Geographic region (vs. North) | ||||
| South | 26 (12.4%) | 2127 (6.1%) | 6.71 [3.05–16.4] | <0.0001 |
| Northeast | 126 (60.0%) | 16,849 (48.5%) | 5.29 [2.72–11.9] | <0.0001 |
| Southeast | 49 (23.3%) | 7559 (21.8%) | 4.59 [2.26–10.6] | <0.0001 |
| Midwest | 1 (0.5%) | 1094 (3.2%) | 0.64 [0.03–3.51] | 0.70 |
| Household location (vs. Rural Zone) | ||||
| Urban area | 153 (72.9%) | 27,334 (78.7%) | 0.76 [0.55–1.06] | 0.10 |
| Sedentary lifestyle (vs. No) | ||||
| Yes | 192 (91.4%) | 33,245 (95.7%) | 0.53 [0.33–0.90] | 0.012 |
| Smoking (vs. No) | ||||
| Yes | 15 (7.1%) | 4260 (12.3%) | 0.51 [0.29–0.84] | 0.014 |
| Use of antihypertensives (vs. No) | ||||
| Yes | 26 (12.4%) | 771 (2.2%) | 5.39 [3.43–8.16] | <0.0001 |
| Stroke (vs. No) | ||||
| Yes | 94 (44.8%) | 25,729 (74.1%) | 0.72 [0.44–1.12] | 0.20 |
| Myocardial infarction (vs. No) | ||||
| Yes | 138 (65.7%) | 11,412 (32.9%) | 2.38 [1.42–3.84] | <0.0001 |
| Heart failure (vs. No) | ||||
| Yes | 41 (19.5%) | 2960 (8.5%) | 1.40 [0.96–1.99] | 0.073 |
| Diabetes (vs. No) | ||||
| Yes | 89 (42.4%) | 10,098 (29.1%) | 1.51 [1.13–2.01] | 0.005 |
| Dyslipidaemia (vs. No) | ||||
| Yes | 39 (18.6%) | 2132 (6.1%) | 2.87 [1.97–4.08] | <0.0001 |
| Respiratory diseases (vs. No) | ||||
| Yes | 11 (5.2%) | 1894 (5.5%) | 0.78 [0.40–1.39] | 0.40 |
| Chronic kidney disease (vs. No) | ||||
| Yes | 19 (9.0%) | 2199 (6.3%) | 1.08 [0.64–1.72] | 0.80 |
Acronyms and Abbreviations: OR =Odds ratio; CI = Confidence interval.
Area under the curve for the model (95% CI): 0.81 [0.78, 0.83].
Reflects the actual sample size with complete data on the included variables.
Non-Caucasian includes people from Brown, Black and Yellow Ethnicity.
Discussion
This study shows a very low use of either statins or high doses of these medications as well as other lipid lowering combination therapies in very high ASCVD risk Brazilian patients followed in primary care. Socio-demographic factors as well as previous co-morbidities were associated with statin use. In addition to that, severe deficiencies were seen in the use of antiplatelet and blood pressure medications despite previous diagnoses of myocardial infarction and stroke as well as an elevated frequency of hypertension.
Statins are recommended by guidelines to intensively reduce LDL-cholesterol in people with previous manifestations of ASCVD however previous studies had shown that recommended LDL-cholesterol goals were seldom attained by Brazilian patients.6,15,16,23,24 The findings of this study performed in a broad sample of patients from different Brazilian regions visited by CHW in both rural and urban areas, indicate that absence or inadequate statin use may explain the latter. In addition, subjects reported low use of combination therapy with ezetimibe and no use of PCSK9 inhibitors, medications that reduce not only LDL-cholesterol but prevent ASCVD events.25 Important previous studies assessing the use of statins in multiple LMICs include the WHO study on Prevention of REcurrences of Myocardial Infarction and StrokE (WHO-PREMISE) and the Prospective Urban Rural Epidemiology (PURE) study.26, 27, 28 WHO-PREMISE results from ten LMICs show that 20% of patients with a previous history of cardiovascular disease reported using statins.29 PURE results show that statin use for secondary prevention was reported by 3.3% of individuals in low-income countries, 4.3% in lower-middle-income countries, 17.6% in upper-middle-income countries, and 66.5% in high-income countries.26 The socioeconomic position was associated with variations in statin use.27 Even though this study aimed at evaluating the use of lipid-lowering therapies, an alarming low use of antiplatelet and anti-hypertensive medications was also encountered in this population. This was more shocking when almost 8 in 10 individuals reported having hypertension. Similarly to PURE,26 this study suggests an overall low use of preventive therapies for this population.
As previously shown for primary care populations in upper-middle-income countries including Brazil, statin use was associated with older age, presence of co-morbidities, and use of medications for blood pressure.26 Indeed, a previous diagnosis of myocardial infarction was independently associated with statin use while the one of stroke was not. This finding is also in accordance with the results from the REACT registry developed in both tertiary and primary care settings.30 In our study, the greater frequency of previous stroke (approximately three-quarters of the population), its greater association with hypertension rather than dyslipidaemia, and a possible misperception of lack of statin benefit for stroke and consequently lower use in this situation (in this study comprising only in 5.5% of study subjects) might have influenced our findings. Indeed, previous evidence shows a low use of statins in patients with previous stroke despite proven benefits of the latter in reducing ASCVD events in these subjects.26,31 However, it is important to emphasize that, even in those with a previous diagnosis of myocardial infarction, in this study, less than one in ten and one in 100 received statins and high dose statins, respectively.
Brazil is a continental country with several social inequalities that are extended to health systems in different regions. More than 70% of participants were of non-Caucasian ethnicity and came from less resourceful country regions (Northeast, North and Midwest). Moreover, 96.4% of study subjects received less than 4 minimum wages a situation that may put them in line of poverty. Even in this context, socio-demographic or social factors indicating less privileged individuals and less adequate care were independently associated with lower use of statins. Being of non-Caucasian ethnicity independently of the SDI and living in the North region of Brazil were negatively associated with statin use. Results are in accordance with previous evidence, indicating that Black individuals and those with other social deprivations have higher morbidity, hospital admissions and mortality in Brazil.32 On the other hand, a positive association was encountered for those living in rural rather than urban zones. These results differed from the PURE study, where approximately 6000 individuals from Brazil were included and a higher use of statins was seen in those living in urban rather than rural zones.26 However, the current study enrolled a six-fold greater number of subjects than PURE, and this might explain these differences. The unique approach of the Brazilian Family Health Strategy, where the poorest municipalities in Brazil have particularly benefited from the program,12 and a possible greater activity of CHW33 in those rural areas vs. urban that needs to be ascertained, could also contribute to explaining this finding. Additionally, there is a need for further research on the impact of the ESF program coverage by region. While there is evidence of decreased hospitalizations for conditions such as heart failure and stroke in regions with broader ESF coverage,34 there is also a considerable opportunity for improvement in the dispensation of medications for non-communicable diseases (including cardiovascular diseases) as per regional ESF coverage.35
A severe deficiency was seen not only in the overall use of statins but also high dose or combination therapies aimed at reducing LDL cholesterol by at least 50%, as recommended by more recent Brazilian guidelines.3 Associate factors for high dose statins or combination dose use were similar to those for overall statin use. However, this may reflect a lack of prescription by attending physicians but also a lack or low availability of atorvastatin or rosuvastatin as well as ezetimibe and PCSK9 inhibitors in the Brazilian public health system.36
More recently, in a geographically and economically diverse sample of nationally representative surveys from low-income and middle-income countries, statins were used by approximately one in ten eligible people for the primary prevention of cardiovascular disease and one in five eligible people for the secondary prevention of cardiovascular disease.9 The WHO target of at least 50% of eligible individuals receiving statin therapy to prevent cardiovascular disease was achieved by only one country (and just for secondary prevention patients), and this target was not achieved by entire regions nor income groups in this set of LMICs. At the individual level, there was generally lower statin use among men (primary prevention only) and individuals who were younger, less educated or lived in rural areas.9
Our study adds to the evidence previously provided by WHO-Premise,29 PURE26 and Marcus et al.9 to substantially advance the understanding of statin use in a real-world setting of one of the most unequal upper-middle-income countries. First, to our knowledge, this is the first and largest study assessing cardiovascular secondary prevention from a nationally representative population. This study provides a unique observation of the reality of the majority Brazilian population which consists of the ones relying solely on the public health care system. Second, the present study provides a unique approach by generating evidence from data obtained from CHWs. This approach support not only the transition of workflow from a paper-based system to a digitized system,37 improving workflow and quality of services,38 but also generate insights on possible quality improvement strategies that could take advantage of this approach. This strategy strengthens the potential of CHW-derived data as an important contributing data source to be encouraged and improved.
Our study also has limitations. First, we rely on self-reported measures of a previous history of cardiovascular disease and statin use. We justify using these self-reported measures as they are the recommended methodology in the WHO non-communicable disease Monitoring Framework,39 they were considered reliable with 89% accuracy in the PURE study26 and, as they represent a more generalisable finding. Additionally, although further research is still needed to investigate agreement between self-reported conditions in multimorbidity patients and physician-reported data, previous studies demonstrated good and moderate agreement for cardiovascular conditions such as the ones assessed in the present study (i.e., diabetes, stroke, dyslipidaemia, coronary disease).40 Self-reports for cardiovascular disease medications have also been found to be highly accurate in previous studies.41,42 Second, we observed a lower prevalence of myocardial infarction than expected. This could be related to the need for improvements in disease awareness and identification in the primary care system. Third, we are not assessing data from higher-income levels of assistance in Brazil where most of the primary care attention is provided by the private system, thus extrapolations to this scenario should be cautious. Finally, we did not assess statin use by target lipid concentrations because low-density lipoprotein cholesterol data are not collected by the CHW.
In conclusion, our results emphasise the urgent need to scale up statin use in LMICs, where most of the global cardiovascular risk burden occurs. Enabling tailored quality improvement and care pathway interventions that suit local needs is key not only to increase the usage of evidence-based treatments but also to prevent care delivery discontinuation, especially between multiple settings. Policies and programmes that allow for the integrated assessment of statins use from prescription to actual use, therefore facilitating the successful implementation of strategies comprising the primary health care systems, must be investigated in future research and advocacy.
Contributors
MJMC, KS, FF, PR, FR, OB and RDS conceived the study. MJMC and PMP obtained funding. ANG and PMP extracted data. ANG, PMP, FM and JN had full access to the data. JN and FM performed the statistical analysis. MJMC and RDS drafted the first version of the manuscript. All academic authors had access and validated the data independently and Novartis representatives had access only to aggregated results. All authors reviewed the manuscript and provided inputs for the final approved version. MJMC and RDS were responsible for the decision of submitting the article.
Data sharing statement
Data used in this study was available for the purpose of a specific project and might be available for further analysis on a case-by-case basis at the discretion of the authors’ representatives.
Declaration of interests
MJMC received research grants from Amgen, GSK, Ipsen and Novartis. FF has stock options from Novartis Biociências. PMP has received research grants from Ipsen and Takeda; honoraria for presentations from Swiss Basel Area; travel support from Astra Zeneca; PR has contracts and has received travel support from Novartis Biociências. OB received research grants from Astra Zeneca, Bayer, Servier and Amgen. RDS received research grants from Amgen, Sanofi, Novartis, Kowa and Esperion; consulting fees from Amgem, Astra, Zeneca, Abbot, Amryt, Pfizer, Hypera, Libbs, Novo-Nordisk, Novartis; honoraria for lectures, speakers bureaus, presentations from Abbott, Amgen, Astra Zeneca, Biolab, Libbs, Pfizer, Novo Nordisk, Eli-Lilly, Sanofi; has received travel support from Novo Nordisk and has played a leadership role in the International Atherosclerosis Society.
Acknowledgements
This study was funded by Novartis Biociências, Brazil.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100534.
Appendix A. Supplementary data
References
- 1.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wirtz V.J., Kaplan W.A., Kwan G.F., Laing R.O. Access to medications for cardiovascular diseases in low- and middle-income countries. Circulation. 2016;133(21):2076–2085. doi: 10.1161/CIRCULATIONAHA.115.008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faludi A.A., Izar M.C.O., Saraiva J.F.K., et al. Atualização da diretriz brasileira de dislipidemias e prevenção da aterosclerose – 2017. Arq Bras Cardiol. 2017;109(2 Supl 1):1–76. doi: 10.5935/abc.20170121. [DOI] [PubMed] [Google Scholar]
- 4.Grundy S.M., Stone N.J., Bailey A.L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;73(24):3168–3209. doi: 10.1016/j.jacc.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Mach F., Baigent C., Catapano A.L., et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–188. doi: 10.1093/eurheartj/ehz455. [DOI] [PubMed] [Google Scholar]
- 6.Danchin N., Almahmeed W., Al-Rasadi K., et al. Achievement of low-density lipoprotein cholesterol goals in 18 countries outside Western Europe: the international ChoLesterol management practice study (ICLPS) Eur J Prev Cardiol. 2018;25(10):1087–1094. doi: 10.1177/2047487318777079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ray K., Molemans B., Schoonen W., et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol. 2020;28(11):1279–1289. doi: 10.1093/eurjpc/zwaa047. [DOI] [PubMed] [Google Scholar]
- 8.Arnold S.V., Cannon C.P., de Lemos J.A., et al. What do US physicians and patients think about lipid-lowering therapy and goals of treatment? Results from the GOULD registry. J Am Heart Assoc. 2021;10(16) doi: 10.1161/JAHA.120.020893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marcus M.E., Manne-Goehler J., Theilmann M., et al. Use of statins for the prevention of cardiovascular disease in 41 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data. Lancet Glob Health. 2022;10(3):e369–e379. doi: 10.1016/S2214-109X(21)00551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oliveira G.M.M., Brant L.C.C., Polanczyk C.A., et al. Cardiovascular statistics - Brazil 2021. Arq Bras Cardiol. 2022;118(1):115–373. doi: 10.36660/abc.20211012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oliveira G.M.M., Brant L.C.C., Polanczyk C.A., et al. Cardiovascular statistics - Brazil 2020. Arq Bras Cardiol. 2020;115(3):308–439. doi: 10.36660/abc.20200812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macinko J., Harris M.J. Brazil's family health strategy--delivering community-based primary care in a universal health system. N Engl J Med. 2015;372(23):2177–2181. doi: 10.1056/NEJMp1501140. [DOI] [PubMed] [Google Scholar]
- 13.Santos R.D., Sociedade Brasileira de C III Brazilian guidelines on dyslipidemias and guideline of Atherosclerosis prevention from Atherosclerosis department of sociedade brasileira de Cardiologia. Arq Bras Cardiol. 2001;77(Suppl 3):1–48. [PubMed] [Google Scholar]
- 14.Sociedade Brasileira de C. Xavier H.T., Izar M.C., et al. V Brazilian guidelines on dyslipidemias and prevention of Atherosclerosis. Arq Bras Cardiol. 2013;101(4 Suppl 1):1–20. doi: 10.5935/abc.2013S010. [DOI] [PubMed] [Google Scholar]
- 15.Lotufo P.A., Santos R.D., Figueiredo R.M., et al. Prevalence, awareness, treatment, and control of high low-density lipoprotein cholesterol in Brazil: baseline of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) J Clin Lipidol. 2016;10(3):568–576. doi: 10.1016/j.jacl.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 16.Bernardi A., Olandoski M., Erbano L.O., Guarita-Souza L.C., Baena C.P., Faria-Neto J.R. Achievement of LDL-cholesterol goals after acute myocardial infarction: real-world data from the city of curitiba public health system. Arq Bras Cardiol. 2022;118(6):1018–1025. doi: 10.36660/abc.20210328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gandra A. 2022. Em 2022, beneficiários de planos de saúde somavam 47,7 milhões - Dados são da Agência de Saude Suplementar.https://agenciabrasil.ebc.com.br/saude/noticia/2022-08/em-2020-beneficiarios-de-planos-de-saude-somavam-474-milhoes [Google Scholar]
- 18.Ziroldo R., Gimenes R.O., Castelo Junior C. The importance of supplementary health in the demand for assistance services supply in Brazil. O Mundo da Saúde. 2013;37(2):5. [Google Scholar]
- 19.Giovanella L., Bousquat A., Schenkman S., Almeida P.F., Sardinha L.M.V., Vieira M. The family health strategy coverage in Brazil: what reveal the 2013 and 2019 national health surveys. Cien Saude Colet. 2021;26(suppl 1):2543–2556. doi: 10.1590/1413-81232021266.1.43952020. [DOI] [PubMed] [Google Scholar]
- 20.ePHealth ePHealth. 2020. http://www.ephealth.com.br/2020)
- 21.Estatística IBdGe . 2017. Índice de Desenvolvimento Humano dos municípios. [Google Scholar]
- 22.O'Brien R. A caution regarding rules of thumb for variance inflation factors. Qual Quantity. 2007;41:673–690. [Google Scholar]
- 23.Waters D.D., Brotons C., Chiang C.W., et al. Lipid treatment assessment project 2: a multinational survey to evaluate the proportion of patients achieving low-density lipoprotein cholesterol goals. Circulation. 2009;120(1):28–34. doi: 10.1161/CIRCULATIONAHA.108.838466. [DOI] [PubMed] [Google Scholar]
- 24.Faria-Neto J.R., Yarleque C., Vieira L.F., Sakane E.N., Santos R.D. Challenges faced by patients with dyslipidemia and systemic arterial hypertension in Brazil: a design of the patient journey. BMC Cardiovasc Disord. 2022;22(1):237. doi: 10.1186/s12872-022-02669-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang N., Fulcher J., Abeysuriya N., et al. Intensive LDL cholesterol-lowering treatment beyond current recommendations for the prevention of major vascular events: a systematic review and meta-analysis of randomised trials including 327 037 participants. Lancet Diabetes Endocrinol. 2020;8(1):36–49. doi: 10.1016/S2213-8587(19)30388-2. [DOI] [PubMed] [Google Scholar]
- 26.Yusuf S., Islam S., Chow C.K., et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378(9798):1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 27.Murphy A., Palafox B., O'Donnell O., et al. Inequalities in the use of secondary prevention of cardiovascular disease by socioeconomic status: evidence from the PURE observational study. Lancet Glob Health. 2018;6(3):e292–e301. doi: 10.1016/S2214-109X(18)30031-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chow C.K., Nguyen T.N., Marschner S., et al. Availability and affordability of medicines and cardiovascular outcomes in 21 high-income, middle-income and low-income countries. BMJ Glob Health. 2020;5(11) doi: 10.1136/bmjgh-2020-002640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mendis S., Abegunde D., Yusuf S., et al. WHO study on prevention of REcurrences of myocardial infarction and StrokE (WHO-PREMISE) Bull World Health Organ. 2005;83(11):820–829. [PMC free article] [PubMed] [Google Scholar]
- 30.Berwanger O., Piva e Mattos L.A., Martin J.F., et al. Evidence-based therapy prescription in high-cardiovascular risk patients: the REACT study. Arq Bras Cardiol. 2013;100(3):212–220. doi: 10.5935/abc.20130062. [DOI] [PubMed] [Google Scholar]
- 31.Albright K.C., Howard V.J., Howard G., et al. Age and sex disparities in discharge statin prescribing in the stroke belt: evidence from the reasons for geographic and racial differences in stroke study. J Am Heart Assoc. 2017;6(8) doi: 10.1161/JAHA.117.005523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hone T., Stokes J., Trajman A., et al. Racial and socioeconomic disparities in multimorbidity and associated healthcare utilisation and outcomes in Brazil: a cross-sectional analysis of three million individuals. BMC Public Health. 2021;21(1):1287. doi: 10.1186/s12889-021-11328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Santos A.D.F.D., Rocha H.A.D., Lima Â.M.L.D., et al. Contribution of community health workers to primary health care performance in Brazil. Rev Saude Publica. 2020;54:143. doi: 10.11606/s1518-8787.2020054002327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cavalcante D.F.B., Brizon V.S.C., Probst L.F., Meneghim M.D.C., Pereira A.C., Ambrosano G.M.B. Did the Family Health Strategy have an impact on indicators of hospitalizations for stroke and heart failure? Longitudinal study in Brazil: 1998-2013. PLoS One. 2018;13(6) doi: 10.1371/journal.pone.0198428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alves K.C.G., Guimarães R.A., de Souza M.R., de Morais Neto O.L. Evaluation of the primary care for chronic diseases in the high coverage context of the family health strategy. BMC Health Serv Res. 2019;19(1):913. doi: 10.1186/s12913-019-4737-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.do Nascimento R., Guerra A.A., Jr., Alvares J., et al. Statin use in Brazil: findings and implications. Curr Med Res Opin. 2018;34(10):1809–1817. doi: 10.1080/03007995.2018.1451312. [DOI] [PubMed] [Google Scholar]
- 37.Agarwal S., Perry H.B., Long L.A., Labrique A.B. Evidence on feasibility and effective use of mHealth strategies by frontline health workers in developing countries: systematic review. Trop Med Int Health. 2015;20(8):1003–1014. doi: 10.1111/tmi.12525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feroz A., Jabeen R., Saleem S. Using mobile phones to improve community health workers performance in low-and-middle-income countries. BMC Public Health. 2020;20(1):49. doi: 10.1186/s12889-020-8173-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization . 2017. The WHO global monitoring framework on noncommunicable diseases.https://www.euro.who.int/data/assets/pdf_file/0003/340869/Report-3.pdf [Google Scholar]
- 40.Hansen H., Schäfer I., Schön G., et al. Agreement between self-reported and general practitioner-reported chronic conditions among multimorbid patients in primary care - results of the MultiCare Cohort Study. BMC Fam Pract. 2014;15(1):39. doi: 10.1186/1471-2296-15-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Richardson K., Kenny R.A., Peklar J., Bennett K. Agreement between patient interview data on prescription medication use and pharmacy records in those aged older than 50 years varied by therapeutic group and reporting of indicated health conditions. J Clin Epidemiol. 2013;66(11):1308–1316. doi: 10.1016/j.jclinepi.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 42.Hafferty J.D., Campbell A.I., Navrady L.B., et al. Self-reported medication use validated through record linkage to national prescribing data. J Clin Epidemiol. 2018;94:132–142. doi: 10.1016/j.jclinepi.2017.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.