Abstract
True intrathoracic subclavian artery aneurysms (SCAAs) are rare and have various etiologies. Right intrathoracic SCAAs pose specific anatomic challenges to repair. We present three different operative approaches, open, endovascular, and hybrid repair, for the repair of a right intrathoracic SCAA in three patients with genetic arteriopathy: Marfan syndrome, vascular Ehlers-Danlos syndrome, and unspecified Ehlers-Danlos syndrome, respectively. These cases demonstrate an individualized operative approach based on the genetic diagnosis for each patient presenting with a right intrathoracic SCAA.
Keywords: Subclavian artery aneurysm, Intrathoracic aneurysm, Peripheral artery aneurysm, Marfan syndrome, Vascular Ehlers Danlos syndrome
Nontraumatic subclavian artery aneurysms (SCAAs) are rare and can present with pain, Horner’s syndrome, hoarseness, or distal embolization.1, 2, 3, 4, 5, 6 Genetic arteriopathy conditions such as Marfan syndrome (MFS), vascular Ehlers-Danlos syndrome (VEDS), and Loeys-Dietz syndrome are known risk factors for SCAAs.2,7, 8, 9, 10 We report the surgical approaches for right intrathoracic SCAA repair in three patients with genetic arteriopathy to demonstrate tailored operative approaches. The institutional review board approved the study, and patients consented to publication.
Case 1
A 40-year-old never-smoker woman with MFS (FBN1 c.841_842insT p.Glu281Valfs∗7, heterozygous null variant) presented with an asymptomatic, enlarging 4.1-cm right intrathoracic SCAA (Fig 1, A and B). Her history included lens subluxation, recurrent pneumothoraces, ascending aorta interposition graft for a type A aortic dissection at age 26, extent II thoracoabdominal aortic aneurysm repair at age 29, aortic root replacement with a mechanical valve at age 34, and left supraclavicular SCAA repair at age 40.
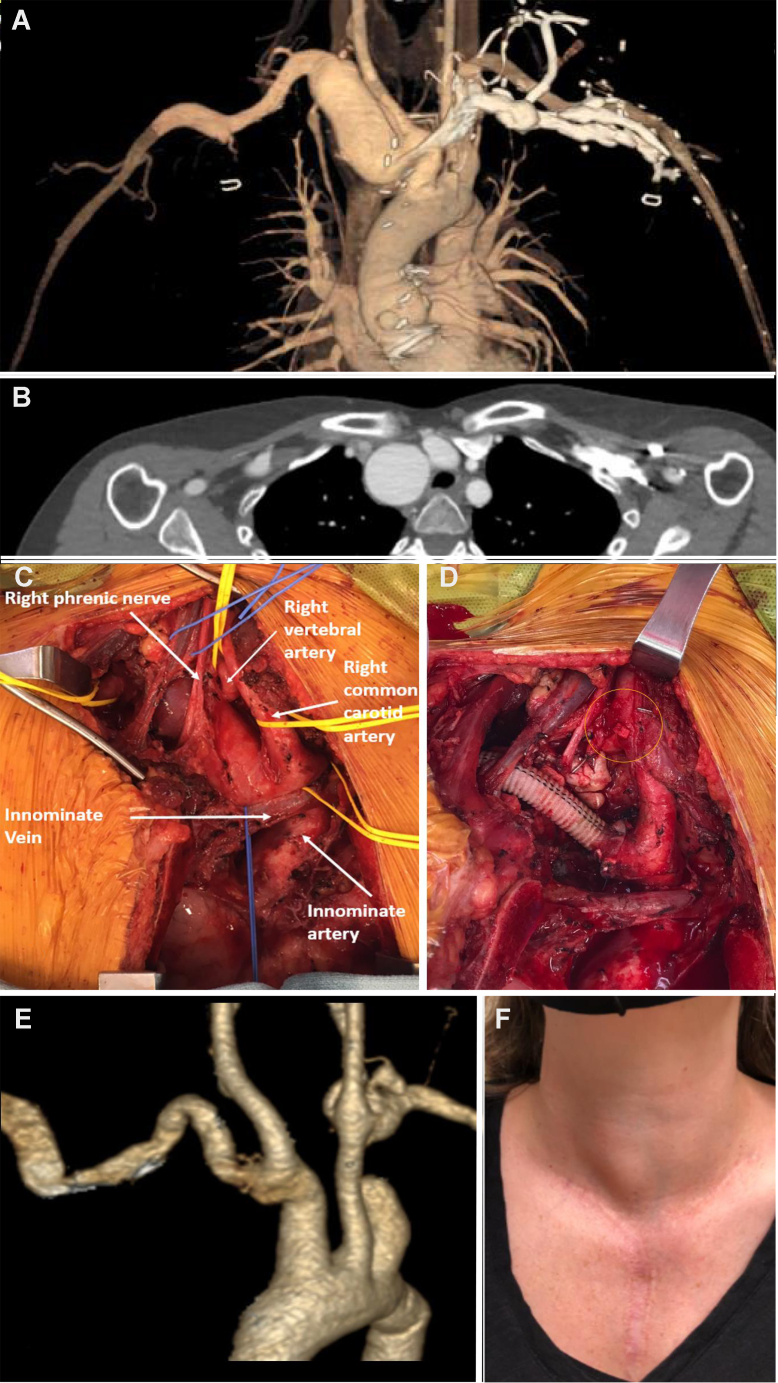
Fig 1.
(A) A three-dimensional image postprocessing and (B) axial computed tomography (CT) imaging of an intrathoracic right subclavian artery aneurysm in a 44-year-old woman with Marfan syndrome. C, Intraoperative photographs of the open surgical repair of the aneurysm with the subclavian artery exposed via a median sternotomy with a right supraclavicular extension. (D) 10 mm interposition Dacron graft between the innominate to the right proximal axillary artery with reimplantation of the right vertebral artery to the right common carotid artery (circle). E, Postprocessing three-dimensional reconstruction of the 1-year follow-up CT imaging of the right subclavian artery repair. F, A 2-year postoperative picture of the patient’s neck. Notice the small right bulge at the base of the neck consistent with the repair that was pulsatile in clinic.
Repair was performed via a redo median sternotomy with a right supraclavicular extension to expose the innominate, right SCA, internal mammary artery (IMA), vertebral artery (VA), and common carotid artery (CCA) while protecting the vagus and phrenic nerves (Fig 1, C). After systemic heparinization, the VA was clamped and transected. The VA had excellent back bleeding. Vascular clamps were applied proximally and distally to the right SCA and proximal axillary artery, respectively. The IMA was ligated. After opening the SCAA sac and ligating the back bleeding arteries, a beveled 10 mm Dacron interposition bypass was anastomosed proximally to the SCA origin and distally to the proximal axillary artery in an end-to-end manner. The anastomoses were reinforced with 0.8 × 8 cm bovine pericardium strips to support the tensile strength of the fragile tissues. The right VA was transposed to the right CCA (Fig 1, D). Estimated blood loss was 2 L. The patient was extubated at the end of the case and discharged home 6 days later. The patient has been followed for 3 years and has a patent bypass graft on imaging (Fig 1, E and F).
Case 2
A 39-year-old never-smoker man with VEDS (COL3A1 c.755G>T p.Gly252Val, missense variant) presented with an asymptomatic 5.1-cm intrathoracic right SCAA with a proximal SCA dissection and thrombosed right 2.5 cm axillary artery (Fig 2, A and B) without malperfusion or distal embolization. The patient’s history included a family history of dissection, club foot at birth, a right V4 segment VA dissection with thrombosis at age 29, splenic artery dissection at age 30, and a left proximal 2.2 cm SCAA with dissection at age 31 and unchanged over 8 years.
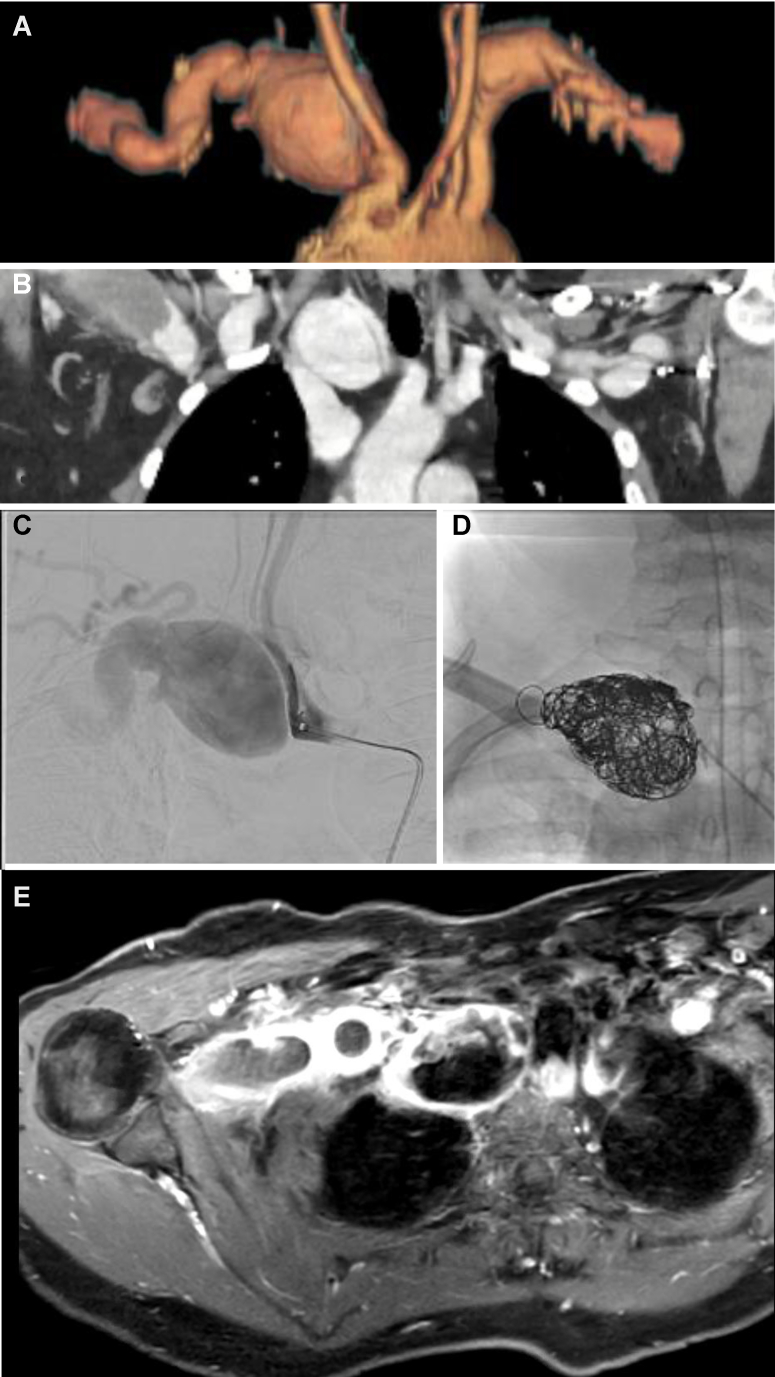
Fig 2.
(A) A three-dimensional image postprocessing and (B) coronal computed tomography imaging of an intrathoracic right subclavian artery aneurysm in a 39-year-old man with vascular Ehlers-Danlos syndrome associated with subclavian artery dissection, a thrombosed distal vertebral artery, and a thrombosed aneurysmal axillary artery. C, Selective angiography of the right subclavian artery demonstrating the dissection flap and thrombosed axillary artery. D, Coil embolization of the right subclavian artery. E, Axial magnetic resonance imaging showing inflammation of the thrombosed right intrathoracic subclavian artery and the axillary artery.
The thrombosis of the right axillary and distal VA with adequate collateralization eliminated the need for revascularization of these arteries. Given the concern over prohibitive risk of open surgical repair (OSR) in VEDS, an endovascular solution was chosen. In preparation for repair, he was started on 2 g of oral vitamin C to support collagen production. Under general anesthesia, the right common femoral artery (CFA) was exposed to allow direct access with a 15-cm 7F sheath. A 55-cm 5F Raabe sheath was advanced over a 0.035 J wire into the descending thoracic aorta, and then a glide catheter and wire were used to select the innominate artery and traverse the dissection flap. The Raabe and a Renegade catheter were placed into the SCAA sac. The sac was embolized with a combination of Concerto Helix detachable (Medtronic) and Nester (Cook Medical) coils (Fig 2, C and D). Detachable coils were chosen for precise deployment and to prevent deployment into the CCA. The CFA was repaired primarily with a pledgeted 5.0 Prolene suture and circumferentially wrapped with a 0.8 × 8 cm bovine pericardium strip to prevent the risk of pseudoaneurysm formation. Estimated blood loss was minimal. The patient recovered in the intensive care unit overnight and discharged the following day. He returned with severe right shoulder pain and, on repeat imaging, had extensive inflammatory reaction identified (Fig 2, E). The pain resolved over the following month while managed with gabapentin and acetaminophen. The patient has been followed for 2 years with imaging confirming satisfactory embolization and no endoleaks.
Case 3
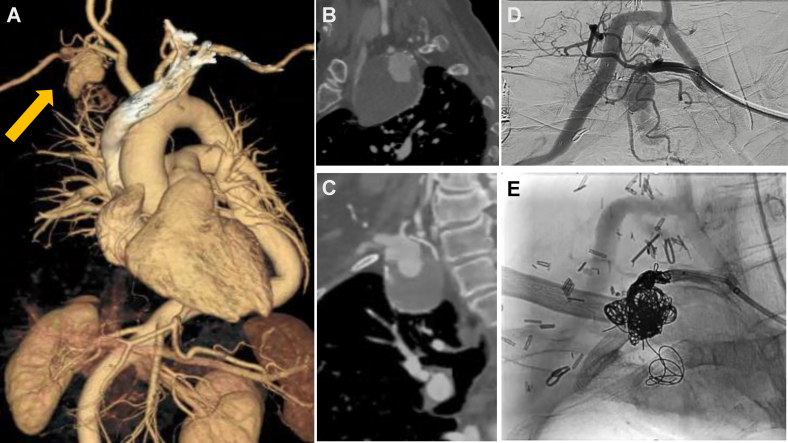
A 60-year-old never-smoker man with an unspecified type of Ehlers-Danlos syndrome (EDS) presented with a 5-week history of right neck pain and a 5-cm partially thrombosed intrathoracic right SCAA (Fig 3, A-C) without distal embolization. His history included a severe scoliosis and velvety-textured skin. His family history was negative for aneurysms or dissections. Genetic testing was negative for known genetic arteriopathies including MFS, Loeys-Dietz syndrome, or VEDS. Given that he did not have VEDS, an OSR via right supraclavicular and infraclavicular incisions was performed. An 8-mm ringed polytetrafluoroethylene graft bypass was anastomosed end-to-side to the distal CCA and end-to-end to the proximal axillary artery. The right VA was reimplanted into the bypass. The SCAA neck could not be dissected safely deep into the clavicle to allow clamp placement due to dense inflammatory adhesions. Thus, subsequent endovascular coil embolization of the sac with Concerto Helix detachable (Medtronic) and Nester (Cook Medical) coils was performed via percutaneous CFA access (Fig 3, D and E). The patient has been followed for 3 years and has a patent bypass graft and thrombosed SCAA sac on imaging.
Fig 3.
A, Three-dimensional postprocessing imaging of a computed tomography (CT) angiography examination of an intrathoracic right subclavian artery aneurysm (arrow) in a 60-year-old man with a clinical diagnosis of Ehlers-Danlos syndrome. Note the severe thoracic and abdominal aortic tortuosity associated with the known scoliosis. (B) Sagittal and (C) coronal CT angiography imaging showing the right intrathoracic subclavian artery aneurysm. D, Selective angiography of the right subclavian artery demonstrating the luminal filling and a patent right common carotid artery to axillary artery bypass and patent right vertebral artery jump graft. E, Coil embolization of the right subclavian artery aneurysm sac.
Discussion
Intrathoracic right SCAAs pose a significant technical challenge due to the complexities of exposure. These three cases illustrate the different operative approaches to an anatomically challenging aneurysm and decision-making tailored to the anticipated operative risks based on the underlying genetic etiology. Specifically, VEDS is associated with arterial friability compared with MFS and other EDS subtypes due to the defective type III collagen production; thus, minimally invasive approaches are advocated.8,11,12 Although there are no agreed-upon size criteria for SCAA repair, repair is indicated if SCAA is symptomatic, rapidly expanding, or ruptured.4 Rupture was reported in 9% of 381 SCAA cases in a 2010 literature review.2
Surgical resection of SCAAs and an interposition bypass graft is the standard treatment2,3,5,13 with some cases of necessitating ligation without reconstructions.2,5 When the aneurysm neck is short, a median sternotomy with a right supraclavicular extension is required for exposure, whereas a focal aneurysm with a longer proximal neck can be reached via a supraclavicular approach alone.1, 2, 3,5,13 Either approach carries the risk of Horner’s syndrome and vocal cord palsy.5 The distal bypass graft anastomosis is dictated by the extent of the SCAAs. When focal, an extrathoracic bypass between the CCA and SCA distal to the aneurysm and ligation of the SCA origin is an option.1,2,5 Extensive aneurysms may require a distal anastomosis to the axillary artery such as in cases 1 and 3.2 The right VA is managed by reimplantation when it arises from the aneurysm sac into the right CCA or the bypass, while the IMA and thoracoacromial branches can be ligated. Another planning consideration for OSR includes whether concomitant aortic arch replacement is needed.5 This consideration was discussed in case 1 because the arch was the only remaining portion of the aorta. Because the arch was normal in size and there were potential risks of cardiopulmonary bypass, repair was deferred.
Endovascular stent grafts are a minimally invasive treatment option.2,6,14,15 This approach is limited by stent graft compression and fracture between the clavicle and first rib.2 In addition, anatomic limitations exist when the aneurysm has a short proximal landing zone and when the SCAA involves the right VA origin.6,14,15 CCA and SCA kissing stenting techniques are a solution for the inadequate proximal landing zone.6 Embolization of the aneurysm sac was used in case 2 similar to a reported case of a large right CCA aneurysm embolization in a patient with VEDS.8 Hybrid approaches have also been reported including the combination of a right CCA to SCA bypass and placement of stent grafts in the innominate artery to cover the right SCA origin2,16 or reimplantation of the right VA to the CCA and then stenting the SCA.17
Ligation (or embolization) of the SCA without revascularization is reserved for circumstances in which revascularization is not possible and can be tolerated because of the collateral network to the upper extremity. A large body of experience with left SCA coverage during thoracic endovascular aortic repair reports a 9% risk of upper extremity ischemia.18
Lastly, intrathoracic SCAAs are rare. We identified 15 among 394 patients with MFS cared for at our health care system and 7 among 282 patients enrolled in the VEDS Collaborative Research Study19 accounting for 3.8% and 2.5% of the MFS and VEDS population, respectively (unpublished data). Because of the rarity of intrathoracic SCAAs, we recommend considering a genetic etiology during workup.20
Conclusions
Intrathoracic right SCAA repair is technically challenging because of the complexities of exposure. Repair approaches are variable and dictated by anatomy and the underlying genetic etiology.
Footnotes
This work was partially funded by gifts to the vascular Ehlers-Danlos syndrome (VEDS) Collaborative Research Study by the Adventuresinlove4Andie Memorial Fund, Bella's Fight for Cure, the DEFY Foundation, the Lauren Tenney Memorial Fund, funds in memory of John DeMasi, the Semanoff family, the VEDS warriors unite, and the Women & Infants Hospital of Rhode Island NICU RNs among many others who generously gifted funds to support VEDS research.
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Davidovic L.B., Markovic D.M., Pejkic S.D., Kovacevic N.S., Colic M.M., Doric P.M. Subclavian artery aneurysms. Asian J Surg. 2003;26:7–11. doi: 10.1016/S1015-9584(09)60206-2. discussion: 12. [DOI] [PubMed] [Google Scholar]
- 2.Vierhout B.P., Zeebregts C.J., van den Dungen J.J., Reijnen M.M. Changing profiles of diagnostic and treatment options in subclavian artery aneurysms. Eur J Vasc Endovasc Surg. 2010;40:27–34. doi: 10.1016/j.ejvs.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Bin H.G., Kim M.S., Kim S.C., Keun J.B., Lee J.H., Kim S.S. Intrathoracic aneurysm of the right subclavian artery presenting with hoarseness: a case report. J Korean Med Sci. 2005;20:674–676. doi: 10.3346/jkms.2005.20.4.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cury M., Greenberg R.K., Morales J.P., Mohabbat W., Hernandez A.V. Supra-aortic vessels aneurysms: diagnosis and prompt intervention. J Vasc Surg. 2009;49:4–10. doi: 10.1016/j.jvs.2008.08.088. [DOI] [PubMed] [Google Scholar]
- 5.Coselli J.S., Crawford E.S. Surgical treatment of aneurysms of the intrathoracic segment of the subclavian artery. Chest. 1987;91:704–708. doi: 10.1378/chest.91.5.704. [DOI] [PubMed] [Google Scholar]
- 6.Gao X., Li L., Gu Y., Guo L., Cui S., Qi L., et al. Endovascular repair of subclavian artery aneurysms: results from a single-center experience. Perfusion. 2017;32:670–674. doi: 10.1177/0267659117720988. [DOI] [PubMed] [Google Scholar]
- 7.Sobh M., Voges I., Attmann T., Scheewe J. Prosthetic graft replacement of a large subclavian aneurysm in a child with Loeys-Dietz syndrome: a case report. Eur Heart J Case Rep. 2020;4:1–4. doi: 10.1093/ehjcr/ytaa163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shalhub S., Black J.H., 3rd, Cecchi A.C., Xu Z., Griswold B.F., Safi H.J., et al. Molecular diagnosis in vascular Ehlers-Danlos syndrome predicts pattern of arterial involvement and outcomes. J Vasc Surg. 2014;60:160–169. doi: 10.1016/j.jvs.2014.01.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beaulieu R.J., Lue J., Ehlert B.A., Grimm J.C., Hicks C.W., Black J.H., 3rd Surgical management of peripheral vascular manifestations of Loeys-Dietz syndrome. Ann Vasc Surg. 2017;38:10–16. doi: 10.1016/j.avsg.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Banning S.K., Ur R., Malleis J., Hamlat C.A., Byers P.H., Shalhub S. Extrathoracic subclavian artery aneurysm in a patient with suspected genetic arteriopathy. J Vasc Surg Cases Innov Tech. 2021;7:46–50. doi: 10.1016/j.jvscit.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shalhub S., Byers P.H., Hicks K.L., Charlton-Ouw K., Zarkowsky D., Coleman D.M., et al. A multi-institutional experience in the aortic and arterial pathology in individuals with genetically confirmed vascular Ehlers-Danlos syndrome. J Vasc Surg. 2019;70:1543–1554. doi: 10.1016/j.jvs.2019.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brooke B.S., Arnaoutakis G., McDonnell N.B., Black J.H., 3rd Contemporary management of vascular complications associated with Ehlers-Danlos syndrome. J Vasc Surg. 2010;51:131–138. doi: 10.1016/j.jvs.2009.08.019. discussion: 8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mizoguchi H., Miura T., Inoue K., Iwata T., Tei K., Horio Y. Surgical reconstruction for intrathoracic aneurysm originating from proximal part of the right subclavian artery. Ann Vasc Dis. 2012;5:194–198. doi: 10.3400/avd.cr.11.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoder M., Cejna M., Holzenbein T., Bischof G., Lomoschitz F., Funovics M., et al. Elective and emergent endovascular treatment of subclavian artery aneurysms and injuries. J Endovasc Ther. 2003;10:58–65. doi: 10.1177/152660280301000113. [DOI] [PubMed] [Google Scholar]
- 15.Li L., Zhang J., Wang R., Li J., Gu Y., Yu H. Endovascular repair of a right subclavian artery aneurysm with coil embolization and stent graft: case report and literature review. Ann Vasc Surg. 2016;36:290.e1–290.e5. doi: 10.1016/j.avsg.2016.02.041. [DOI] [PubMed] [Google Scholar]
- 16.Van Leemput A., Maleux G., Heye S., Nevelsteen A. Combined open and endovascular repair of a true right subclavian artery aneurysm without proximal neck. Interact Cardiovasc Thorac Surg. 2007;6:406–408. doi: 10.1510/icvts.2006.149088. [DOI] [PubMed] [Google Scholar]
- 17.D'Oria M., Pipitone M., Chiarandini S., Calvagna C., Riccitelli F., Rotelli A., et al. Hybrid treatment of a true right subclavian artery aneurysm involving the vertebral artery using a covered stent. Ann Vasc Surg. 2018;53:273.e7–273.e11. doi: 10.1016/j.avsg.2018.05.074. [DOI] [PubMed] [Google Scholar]
- 18.Batubara E.A.D., Nugraha R.A., Amshar M., Siddiq T., Indriani S., Adiarto S. Ischemic complications following thoracic endovascular aortic repair with and without revascularization of left subclavian artery: a systematic review and meta-analysis. Ann Vasc Surg. 2022;86:417–427. doi: 10.1016/j.avsg.2022.04.037. [DOI] [PubMed] [Google Scholar]
- 19.Sage L., Russo M.L., Byers P.H., Demasi J., Morris S.A., Puryear L.N., et al. Setting a research agenda for vascular Ehlers-Danlos syndrome using a patient and stakeholder engagement model. J Vasc Surg. 2020;72:1436–1444.e2. doi: 10.1016/j.jvs.2019.12.043. [DOI] [PubMed] [Google Scholar]
- 20.Shalhub S., Wallace S., Okunbor O., Newhall K. Genetic aortic disease epidemiology, management principles, and disparities in care. Semin Vasc Surg. 2021;34:79–88. doi: 10.1053/j.semvascsurg.2021.02.012. [DOI] [PubMed] [Google Scholar]