Abstract
Background
Vestibular migraine (VM) is a common cause of dizziness that is underrecognized, underdiagnosed, and challenging to effectively treat. The prevalence, appropriate diagnostic workup, and therapies for VM in low- and lower-middle-income countries (LLMICs) remain understudied. The objective of this scoping review is to evaluate the current state of VM research in LLMICs.
Methods
PubMed, Embase, and Web of Science databases were searched to execute a scoping review of VM. Keywords “vestibular diseases” and “vertigo” were used in combination with terms referring to LLMICs as defined by the World Bank. Title and abstract screening, full-text review, and data collection were conducted by two authors independently.
Results
Twenty-six studies were included in the scoping review. Most studies were cross-sectional (57.7%) or case studies/series (23.1%) and were conducted in urban settings only (92.3%). Geographic distribution of studies was skewed, with 65.4% of articles originating from India. The prevalence of VM among clinic patients ranged from 0.3% to 33.3%. VM most frequently presented as headache, nausea and vomiting, and photophobia. Radiographic imaging, audiometry, and electronystagmography/videonystagmography were the three most commonly utilized diagnostic modalities in the dizziness workup. The most studied pharmacotherapies included calcium channel blockers, followed by beta-blockers and antiepileptics. Case studies and series discussed less common VM pharmacotherapies, such as ayurvedic medicine.
Conclusions
There is a need for more VM research in LLMICs, including innovative diagnostic approaches and therapies that can improve VM care globally. Equitable partnerships between LLMIC and high-income country researchers must expand vestibular research capacity and productivity in LLMICs.
Keywords: Vestibular migraine, Migraine, Global, Otolaryngology, Scoping review
1. Introduction
Vestibular migraine (VM) is a highly prevalent, relatively new, and poorly understood disease entity with diagnostic and treatment challenges (Formeister et al., 2018; Hsu et al., 2011; Lempert et al., 2012; Sargent, 2013; Strupp et al., 2010). In the Global Burden of Disease Study (2019) date, migraine had a prevalence rate of 14.0% (Stovner et al., 2022; Vos et al., 2012). Migraine has been associated with various vestibular symptoms, including vertigo, motion intolerance, nausea, and imbalance (Akdal et al., 2015). Although there is no specific data on the global burden of VM, one can extrapolate from studies conducted in high-income countries (HICs) that a large and significant subset of migraineurs may also have VM, potentially numbering in the millions globally (Akdal et al., 2013, 2015). VM symptoms can be debilitating and often result in substantial social and functional impacts on quality of life; a large proportion of individuals with VM report that their symptoms interfere with their daily activities and seek out healthcare services ranging from clinic visits to emergency departments (Formeister et al., 2018).
VM remains a diagnostic and therapeutic challenge for clinicians. The symptomatology of VM widely varies, overlaps with other vestibular disorders, and is exacerbated by comorbid depression and anxiety (Huang et al., 2020; Strupp et al., 2010). The lack of diagnostic markers further compounds this issue (Mallampalli et al., 2022). Furthermore, there are no clear recommendations for specific VM therapies, so empiric treatment is borrowed from treatment strategies employed in managing patients with migraine headaches. For these reasons, many have posited that this debilitating disease is underdiagnosed and its impact underestimated (Formeister et al., 2018; Mallampalli et al., 2022; Sargent, 2013).
To better understand the global impact of VM, a multidisciplinary panel of experts recommended creating a global VM registry, highlighting the need for more high-quality data and research on VM from all areas of the world (Mallampalli et al., 2022). Currently, however, the vast majority of the research on VM originates from HICs or upper-middle income countries (UMICs), but not low- and lower-middle income countries (LLMICs). LLMICs, home to billions of people, are particularly underrepresented in the medical literature and face some of the world's most severe healthcare disparities (Yao et al., 2022). An appraisal of the current state of VM research in LLMICs is needed to assess the existing evidence, which can inform future directions of VM research in LLMICs and identify potential areas for cross-cultural collaboration and partnership to advance the field. The aims of this scoping review were to identify publications on prevalence, clinical presentation, diagnosis, and treatment of VM in LLMICs and identify gaps in knowledge that could guide future VM research.
2. Methods
A scoping review using Arksey and O'Malley's framework and followed the guidelines of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) Extension for Scoping Reviews was conducted (Arksey and O’Malley, 2005; Tricco et al., 2018). Eligibility criteria were:
-
1.
Population: Individuals with vestibular migraine.
-
2.
Setting: Research conducted in LLMICs, as defined by the World Bank (World Bank Country and Lending Groups – World Bank Data Help Desk, 2022).
-
3.
Intervention: Studies that discussed the prevalence, clinical presentation, diagnosis, and treatment/rehabilitation of VM, migrainous vertigo, and migraine-associated vertigo were included.
-
4.
Outcomes: Study characteristics (last name of the first author, journal, publication year, journal, study type), context (population, age, urban vs. rural setting, level of healthcare) and key findings. Because of the heterogeneity in the studies' scope, setting, and outcomes, we grouped the findings into the following categories: prevalence, clinical presentation, diagnostic methods, and treatment.
-
5.
Study design: Original research of any kind was included. Abstracts, basic science or animal studies, narrative reviews, those conducted in upper-middle-income countries or high-income countries, and unavailable articles were excluded. Studies of migraine without associated vertigo were also excluded.
-
6.
Language: English.
PubMed, Embase, and Web of Sciences databases for studies published from January 1st, 2002 to February 11th, 2022 in English were searched. An update search to find any new articles published between November 2, 2022 and 8/29/2022 was also performed. Until 2012, there were no consensus diagnostic criteria for VM (Lempert et al., 2012); thus, a broader search spanning vestibular diseases and vertigo was utilized. Key terms “vestibular diseases” and “vertigo” were combined with a set of terms that refer to LLMICs (full search strategy available in Appendix A).
Relevant gray literature was identified using snowball sampling of the reference lists of included articles, Google Scholar, and African Journals Online (AJOL) using the same key terms. All searches were uploaded into Covidence (Veritas Health Innovation Ltd, Melbourne). If the articles were not readily available, we attempted to obtain them by contacting the corresponding authors by email.
In the title/abstract screening, two independent authors screened each article to determine eligibility. At least two authors independently extracted data from the included articles and resolved any discrepancies through discussion and consensus. Ethics or institutional review board approval was not obtained, as this study did not involve human subjects and utilized only published data.
3. Results
3.1. Search results
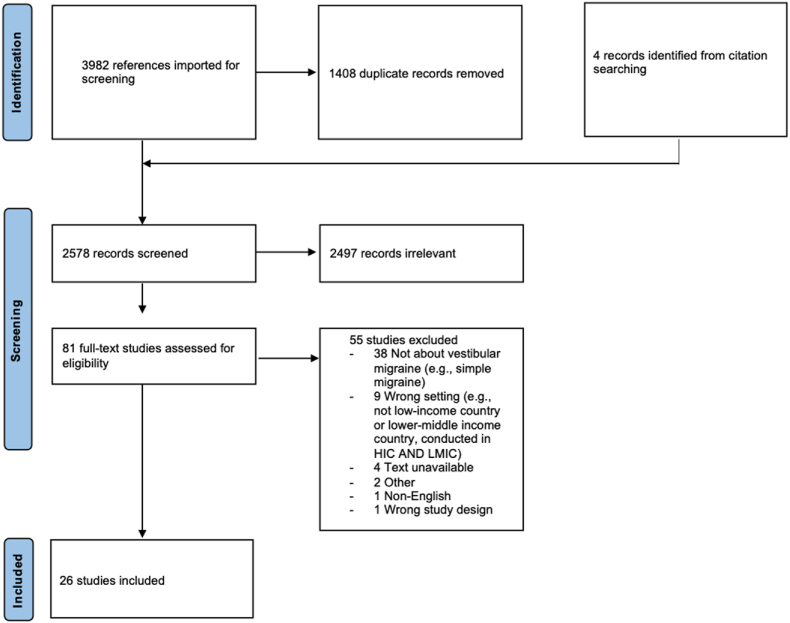
Our search on February 11th, 2022 yielded 3,982 references, with 4 additional studies included from citation searching. After 1,408 duplicates were removed, 2,578 records were screened. Of these, 2,497 articles were removed, and the full texts of 81 articles were assessed for eligibility. A total of 26 studies met the inclusion criteria (PRISMA diagram shown in Fig. 1). No additional studies were identified on the update search. The details of the included studies are in Table 1.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses diagram for included studies.
Table 1.
Summary of included articles.
| First author, publication year | Study Title | Aim of study | Study design | Country in which study conducted | Practice setting | Ages of patients | Total number of participants (including controls) | Number of patients with vestibular migraine |
|---|---|---|---|---|---|---|---|---|
| Adegbiji et al., 2014 | Vertigo presentation in developing country, Nigeria | To determine clinical and epidemiological features of vertigo in Ado Ekiti | Cross-sectional | Nigeria | Tertiary/referral hospital | Both children and adults | 178 | 12 |
| Anshul et al., 2020 | Ayurvedic management of chronic migraine through mashbaladi pachan kashaya nasya: A case study | To evaluate the effect of two Indian traditional systems of medicine on migraine | Case study/Case series | India | Other: Ayurveda clinic | Adults (18+) | 1 | 1 |
| Ashish et al., 2017 | Subjective Visual Vertical and Horizontal in Vestibular Migraine | To compare results of static and dynamic subjective visual vertical and horizontal testing in patients with vestibular migraine with those of healthy individuals | Cross-sectional | India | Tertiary/referral hospital | Adults (18+) | 148 | 66 |
| Bansal, 2016 | Common causes of vertigo and dizziness in Gujarat | To report common causes of dizziness and vertigo in Gujarat | Cross-sectional | India | Tertiary/referral hospital | Adults (18+) | 35 | 3 |
| Das et al., 2017 | Dizziness in a Tertiary Care Centre in Sikkim: Our Experience and Limitations | To investigate the causes of dizziness and the limitations and challenges in the diagnosis | Cross-sectional | India | Tertiary/referral hospital | Both children and adults | 75 | 3 |
| Dash et al., 2008 | Migraine and audiovestibular dysfunction: is there a correlation? | To study audiovestibular functions in cases of migraine with or without vertigo | Prospective cohort | India | Tertiary/referral hospital | Adults (18+) | 50 | 38 |
| El-Badry et al., 2017 | Clinical criteria of positional vertical nystagmus in vestibular migraine | To identify key diagnostic criteria for positional vertical nystagmus caused by vestibular migraine | Case study/Case series | Egypt | Tertiary/referral hospital | Adults (18+) | 13 | 13 |
| ElSherif et al., 2020 | Eye movements and imaging in vestibular migraine | To evaluate eye movement using videonystagmography and video head impulse test and to study the occipital lobe metabolic profile in vestibular migraine patients | Case control study | Egypt | Tertiary/referral hospital | Adults (18+) | 45 | 25 |
| Haripriya et al., 2021 | Prevalence, clinical profile, and diagnosis of pediatric dizziness in a tertiary care hospital | To ascertain the prevalence of pediatric vertigo in children presenting to the otolaryngology clinic of a tertiary care hospital | Cross-sectional | India | Tertiary/referral hospital | Children (<18) | 89 | 25 |
| Ky et al., 2021 | Study of the features of systemic dizziness in patients with chronic and recurrent migraine | To determine the type of vertigo in patients with chronic migraine and episodic migraine | Cross-sectional | Vietnam | Tertiary/referral hospital | Adults (18+) | 113 | 66 |
| Lepcha et al., 2014 | Flunarizine in the prophylaxis of migrainous vertigo: a randomized controlled trial | To evaluate efficacy of flunarizine in patients with migrainous vertigo when compared to non-specific vestibular treatment of betahistine and vestibular exercise | Randomized controlled trial | India | Tertiary/referral hospital | Adults (18+) | 52 | 52 |
| Mamindla et al., 2020 | A descriptive epidemiological study on migraine | To conduct an observational study in migraine patients | Cross-sectional | India | Other: epidemiological or database study | Both children and adults | 415 | 2 |
| Mostafa et al., 2014 | Central vestibular dysfunction in an otorhinolaryngological vestibular unit: incidence and diagnostic strategy | To determine the incidence of central vestibular disorders in patients presenting to a vestibular unit in a tertiary referral academic center | Cross-sectional | Egypt | Tertiary/referral hospital | Adults (18+) | 100 | 4 |
| Mouelhi et al., 2020 | Sparse classification of discriminant nystagmus features using combined video-oculography tests and pupil tracking for common vestibular disorder recognition | To propose a novel automated approach to achieve both selection and classification of nystagmus parameters in vestibular disorders | Diagnostic test accuracy study | Tunisia | Tertiary/referral hospital | Adults (18+) | 120 | 30 |
| Ogah, 2017 | Etiology of Vertigo as Seen at the Federal Medical Center Lokoja, North Central Nigeria | To determine the prevalence and causes of vertigo in Federal Medical Center Lokoja, North Central Nigeria | Cross-sectional | Nigeria | Tertiary/referral hospital | Both children and adults | 50 | 1 |
| Olusesi, 2016 | 10 years of Vertigo Clinic at National Hospital Abuja, Nigeria: what have we learned? | To report management outcomes of peripheral vestibular diseases from Africa | Cross-sectional | Nigeria | Tertiary/referral hospital | Adults (18+) | 561 | 32 |
| Prakash et al., 2008 | Headaches related to triptans therapy in patients of migrainous vertigo | To report 3 female patients in which administration of triptan was associated with induction or exacerbation of headache with disappearance of vertigo | Case study/Case series | India | Tertiary/referral hospital | Adults (18+) | 3 | 3 |
| Prakash et al., 2009 | Migrainous vertigo responsive to intravenous methylprednisolone: case reports | To report 4 patients with migrainous vertigo who showed response to intravenous methylprednisolone | Case study/Case series | India | Tertiary/referral hospital | Adults (18+) | 4 | 4 |
| Prakash et al., 2021 | Bilateral persistent ophthalmoplegia in a patient with migraine: persistent migraine aura without infarction? | To report a patient who had an attack of a headache with diplopia, vertigo and tinnitus | Case study/Case series | India | Tertiary/referral hospital | Adults (18+) | 1 | 1 |
| Sen et al., 2016 | The vertigo spectrum: A retrospective analysis in 149 walk-in patients at a specialised neurotology clinic | To assess the frequencies of different kinds of vertigo patients in a vertigo clinic | Cross-sectional | India | Tertiary/referral hospital | Adults (18+) | 149 | 31 |
| Sunitha et al., 2019 | Vertigo: Incidences, Diagnosis and Its Relations with Hearing Loss | To evaluate the various causes of vertigo based on the vertigo attacks and hearing loss | Cross-sectional | India | Tertiary/referral hospital | Adults (18+) | 150 | 4 |
| Swain et al., 2018 | Vertigo among elderly people: Our experiences at a tertiary care teaching hospital of Eastern India | To evaluate the etiology, clinical profile, morbidity, diagnosis, and management of vertigo among elderly patients at a tertiary care teaching hospital of Eastern India | Cross-sectional | India | Tertiary/referral hospital | Adults (18+) | 72 | 19 |
| Swain et al., 2020 | Vertigo in Children: Our Experiences at a Tertiary Care Teaching Hospital of Eastern India | To evaluate vertigo among pediatric age presenting to the vertigo clinic | Cross-sectional | India | Tertiary/referral hospital | Children (<18) | 108 | 36 |
| Syed et al., 2020 | Clinico-aetiological profile of patients with vertigo: A cross-sectional observational study | To study the clinical profile and various aetiological factors for vertigo in patients with actual sensation of rotatory motion | Cross-sectional | India | Tertiary/referral hospital | Adults (18+) | 110 | 4 |
| Taghdiri et al., 2014 | Cinnarizine for the prophylaxis of migraine associated vertigo: a retrospective study | To assess efficacy and safety of cinnarizine for prophylaxis of migraine associated vertigo | Retrospective cohort | Iran | Tertiary/referral hospital | Adults (18+) | 40 | 24 |
| Udagatti et al., 2017 | Migraine Related Vertigo | To report a case of vestibular migraine and outline a protocol for management | Case study/Case series | India | Tertiary/referral hospital | Adults (18+) | 1 | 1 |
3.2. Characteristics of included studies
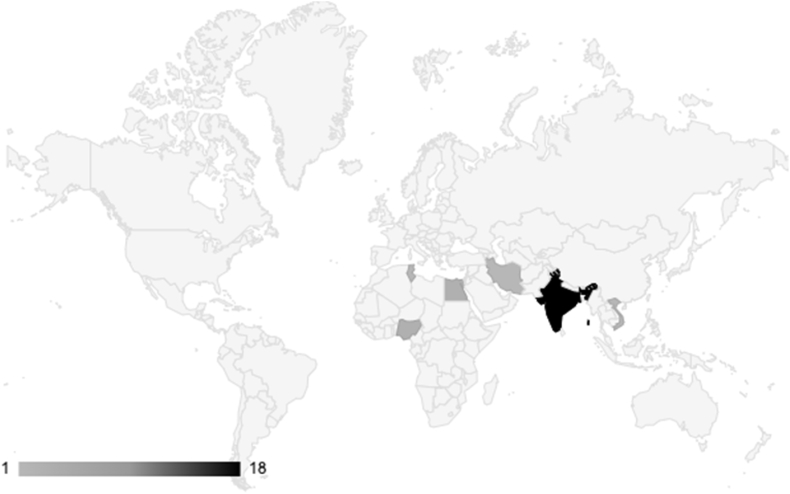
Most of the articles originated from India (n = 17, 65.4%) (Anshul et al., 2020; Ashish et al., 2017; Bansal, 2016; Das et al., 2017; Dash et al., 2008; Haripriya et al., 2021; Lepcha et al., 2014; Mamindla et al., 2020; Prakash et al., 2008, 2021; Prakash and Shah, 2009; Sen et al., 2016; Sunitha et al., 2019; Swain et al., 2018, 2020; Syed et al., 2020; Udagatti and Dinesh Kumar, 2017), followed by Egypt (n = 3, 11.5%) (El-Badry et al., 2017; ElSherif et al., 2020; Mostafa et al., 2014), Nigeria (n = 3, 11.5%) (Adegbiji et al., 2014; Ogah, 2017; Olusesi and Abubakar, 2016), Iran (n = 1, 3.8%) (Taghdiri et al., 2014), Tunisia (n = 1, 3.8%) (Mouelhi et al., 2020), and Vietnam (n = 1, 3.8%) (Ky et al., 2021) as represented by the heat map (Fig. 2). Twenty-four studies (92.3%) were conducted in urban and tertiary care settings. The majority of the studies were cross-sectional studies (n = 15, 57.7%) and case studies/series (n = 6, 23.1%). Other study designs included case-control study, randomized controlled trial, retrospective cohort study, prospective cohort study, and evaluation of a novel diagnostic test (all n = 1, 3.7%). Except for two that only reported on pediatric populations (Haripriya et al., 2021; Swain et al., 2020) and four that reported on both adult and pediatric patients (Adegbiji et al., 2014; Das et al., 2017; Mamindla et al., 2020; Ogah, 2017), all other studies examined only adults.
Fig. 2.
Location of studies as represented by a heat map. Darker colors represent a higher number of included citations from the country.
3.3. Terminology
There was wide variability in the terminology used to describe VM among studies. Many variations of “migrainous vertigo,” such as “migraine-associated vertigo,” “migraine with vertigo,” and “migraine related vertigo,” were used (n = 10, 38.5%) (Adegbiji et al., 2014; Das et al., 2017; Dash et al., 2008; Haripriya et al., 2021; Lepcha et al., 2014; Olusesi and Abubakar, 2016; Prakash et al., 2008; Prakash and Shah, 2009; Syed et al., 2020; Udagatti and Dinesh Kumar, 2017). “Vestibular migraine” was used in eight studies (n = 8, 30.8%) (Ashish et al., 2017; El-Badry et al., 2017; ElSherif et al., 2020; Mamindla et al., 2020; Sunitha et al., 2019; Swain et al., 2018, 2020; Taghdiri et al., 2014). Five studies used the term “migraine” and described vertigo and/or dizziness in its clinical presentation (n = 5, 19.2%) (Anshul et al., 2020; Ky et al., 2021; Mouelhi et al., 2020; Ogah, 2017; Prakash et al., 2021). “Migraine vestibulopathy” was utilized in one study (n = 1, 3.7%) (Mostafa et al., 2014). Two studies simultaneously used more than one of the aforementioned terms (n = 2, 7.4%) (Bansal, 2016; Sen et al., 2016).
3.4. Prevalence of VM in clinics
Prevalence of VM was reported in 13 studies (50%), ranging from 0.3% to 33.3% (Adegbiji et al., 2014; Bansal, 2016; Das et al., 2017; Haripriya et al., 2021; Mamindla et al., 2020; Mostafa et al., 2014; Ogah, 2017; Olusesi and Abubakar, 2016; Sen et al., 2016; Sunitha et al., 2019; Swain et al., 2018, 2020; Syed et al., 2020). Five of the studies were conducted specifically in vertigo or dizziness clinics (Bansal, 2016; Mostafa et al., 2014; Sen et al., 2016; Swain et al., 2018; Udagatti and Dinesh Kumar, 2017), whereas five others were conducted at otolaryngology clinics (Adegbiji et al., 2014; Das et al., 2017; Haripriya et al., 2021; Sunitha et al., 2019; Syed et al., 2020), another at a headache clinic (Taghdiri et al., 2014), and one which did not specify (Mamindla et al., 2020).
More than a quarter of pediatric patients with chief complaints of vertigo at dizziness clinics were diagnosed with VM (Haripriya et al., 2021; Swain et al., 2020). VM was present among 26.4% of elderly adults (above the age of 60) at a vertigo clinic (Swain et al., 2018). Among adults only, the prevalence of VM was more variable and ranged from 0.3% to 15.4% (Bansal, 2016; Mostafa et al., 2014; Olusesi and Abubakar, 2016; Sen et al., 2016; Sunitha et al., 2019). In studies of both adults and children, the prevalence ranged from 2% to 6.7% (Adegbiji et al., 2014; Das et al., 2017; Ogah, 2017).
3.5. Clinical presentation
Seventeen studies reported the symptomatology of VM (65.4%), excluding studies that either did not report the clinical presentation or reported symptoms of all vestibulopathies in aggregate (Table 2) (Ashish et al., 2017; Dash et al., 2008; ElSherif et al., 2020; Haripriya et al., 2021, 2021; Ky et al., 2021; Lepcha et al., 2014; Mostafa et al., 2014; Ogah, 2017; Prakash et al., 2008, 2021; Prakash and Shah, 2009; Sen et al., 2016; Sunitha et al., 2019; Syed et al., 2020; Udagatti and Dinesh Kumar, 2017). Dizziness and/or vertigo were reported in all studies. Headache was the second most commonly reported clinical presentation (n = 15 studies, 88.2%) (Anshul et al., 2020; Ashish et al., 2017; Dash et al., 2008; ElSherif et al., 2020; Haripriya et al., 2021; Ky et al., 2021; Lepcha et al., 2014; Ogah, 2017; Prakash et al., 2008, 2021; Prakash and Shah, 2009; Sen et al., 2016; Sunitha et al., 2019; Taghdiri et al., 2014; Udagatti and Dinesh Kumar, 2017), followed by nausea/vomiting (n = 7 studies, 41.2%) (Anshul et al., 2020; Haripriya et al., 2021; Lepcha et al., 2014; Mostafa et al., 2014; Prakash et al., 2008; Prakash and Shah, 2009; Udagatti and Dinesh Kumar, 2017), photophobia (n = 6 studies, 41.2%) (Anshul et al., 2020; Dash et al., 2008; Haripriya et al., 2021; Lepcha et al., 2014; Prakash et al., 2008; Prakash and Shah, 2009), phonophobia (n = 6 studies, 35.3%) (Anshul et al., 2020; Haripriya et al., 2021; Lepcha et al., 2014; Prakash et al., 2008; Prakash and Shah, 2009; Sunitha et al., 2019), and tinnitus (n = 3 studies, 17.6%) (Ashish et al., 2017; Lepcha et al., 2014; Sen et al., 2016). Other less common symptoms included head movement intolerance (Mostafa et al., 2014), sweating and giddiness (Udagatti and Dinesh Kumar, 2017), decreased consciousness (Lepcha et al., 2014), and hearing change and aural fullness (Dash et al., 2008).
Table 2.
Clinical presentation of vestibular migraine in the included studies.
| Reported clinical presentation of vestibular migraine | Number of studies that report the symptom, n (%) |
|---|---|
| Dizziness/vertigo | 17 (100) |
| Headache | 15 (88.2) |
| Nausea/vomiting | 7 (41.2) |
| Photophobia | 7 (41.2) |
| Phonophobia | 6 (35.3) |
| Tinnitus | 3 (17.6) |
| Head movement intolerance | 1 (5.9) |
| Sweating and giddiness | 1 (5.9) |
| Decreased consciousness | 1 (5.9) |
| Aural fullness and hearing change | 1 (5.9) |
3.6. Diagnostic workup
The most commonly used diagnostic methods for dizziness workup included radiographic imaging (n = 16 studies, 61.5%) (Adegbiji et al., 2014; Ashish et al., 2017; Bansal, 2016; Dash et al., 2008; ElSherif et al., 2020; Haripriya et al., 2021; Lepcha et al., 2014; Mostafa et al., 2014; Olusesi and Abubakar, 2016; Prakash et al., 2008, 2021; Prakash and Shah, 2009; Sen et al., 2016; Sunitha et al., 2019; Swain et al., 2020; Udagatti and Dinesh Kumar, 2017), audiometry (n = 13 studies, 50%) (Adegbiji et al., 2014; Ashish et al., 2017; Bansal, 2016; Dash et al., 2008; ElSherif et al., 2020; Haripriya et al., 2021; Mostafa et al., 2014; Olusesi and Abubakar, 2016; Sen et al., 2016; Sunitha et al., 2019; Swain et al., 2020; Syed et al., 2020; Udagatti and Dinesh Kumar, 2017), electronystagmography/videonystagmography (n = 11 studies, 46.2%) (Adegbiji et al., 2014; El-Badry et al., 2017; ElSherif et al., 2020; Haripriya et al., 2021; Ky et al., 2021; Mostafa et al., 2014; Mouelhi et al., 2020; Sen et al., 2016; Swain et al., 2018; Syed et al., 2020; Udagatti and Dinesh Kumar, 2017), positional testing (n = 11 studies, 42.3%) (Adegbiji et al., 2014; Bansal, 2016; El-Badry et al., 2017; ElSherif et al., 2020; Mostafa et al., 2014; Prakash and Shah, 2009; Sen et al., 2016; Sunitha et al., 2019; Swain et al., 2018, 2020; Syed et al., 2020), oculomotor examination (n = 8 studies, 30.8%) (Adegbiji et al., 2014; Bansal, 2016; ElSherif et al., 2020; Prakash and Shah, 2009; Sunitha et al., 2019; Swain et al., 2020; Syed et al., 2020; Udagatti and Dinesh Kumar, 2017), and an otologic exam (n = 8 studies, 30.8%) (Adegbiji et al., 2014; Bansal, 2016; Haripriya et al., 2021; Lepcha et al., 2014; Sen et al., 2016; Swain et al., 2018, 2020; Udagatti and Dinesh Kumar, 2017) (see Table 3). A smaller percentage of studies used various hematologic tests (e.g., complete blood count, metabolic panel, thyroid function test, inflammatory markers) (Haripriya et al., 2021; Prakash et al., 2021; Prakash and Shah, 2009; Syed et al., 2020; Udagatti and Dinesh Kumar, 2017), psychiatric examination (Haripriya et al., 2021), electromyography and nerve conduction test (Prakash et al., 2021), fistula test (Syed et al., 2020), electrocochleogram (Haripriya et al., 2021), and brainstem audiometry evoked response (Udagatti and Dinesh Kumar, 2017). Vertebral artery screening test and vertebrobasilar doppler were used to exclude other pathologies, such as vertebral artery dissection (Mostafa et al., 2014). Aside from more traditional diagnostic methods, Mouelhi et al. (2020) designed a novel automated program to recognize vestibular disorders based on nystagmus patterns. Additionally, Bansal et al. utilized a novel program called CADINO (Computer-Aided Diagnosis In Neurotology), which used patient history, physical exam findings, and other results to determine the etiology of dizziness (Bansal, 2016).
Table 3.
Diagnostic workup utilized in the included studies.
| Diagnostic modality | Number of studies that utilize the diagnostic method, n (%) |
|---|---|
| Radiographic imaging | 16 (61.5) |
| Magnetic Resonance Imaging, n = 15 | |
| Computed Tomography, n = 3 | |
| Unspecified imaging, n = 1 | |
| Audiometry | 13 (50) |
| Electronystagmography/Videonystagmography | 11 (42.3) |
| Positional testing (e.g., Dix-Hallpike, Supine Roll Test) | 11 (42.3) |
| Oculomotor examination (nystagmus, saccades, smooth pursuit) | 8 (30.8) |
| Ear exam | 8 (30.8) |
| Functional vestibular examination (head impulse test, head shake test) | 7 (26.9) |
| Caloric exam | 7 (26.9) |
| Cranial nerve exam | 6 (23.1) |
| Romberg/Unteberger exam | 6 (23.1) |
| Gait exam | 5 (19.2) |
| Cerebellar exam (finger-to-nose, rapid alternating movements) | 5 (19.2) |
| Tympanometry | 4 (15.4) |
| Auditory brainstem response | 4 (15.4) |
| Video head impulse test | 3 (11.5) |
| Vestibular evoked myogenic potential | 3 (11.5) |
| Subjective visual vertical/horizontal | 2 (7.7) |
3.7. Treatment
Nine studies discussed treatment for VM (Table 4) (Anshul et al., 2020; El-Badry et al., 2017; Lepcha et al., 2014; Prakash et al., 2008, 2021; Prakash and Shah, 2009; Sunitha et al., 2019; Taghdiri et al., 2014; Udagatti and Dinesh Kumar, 2017). Except for one randomized controlled trial (Lepcha et al., 2014), one prospective study (Sunitha et al., 2019), and one retrospective study (Taghdiri et al., 2014), the rest were case reports or case series (Anshul et al., 2020; El-Badry et al., 2017; Prakash et al., 2008, 2021; Prakash and Shah, 2009; Udagatti and Dinesh Kumar, 2017). Taghdiri et al. (2014) showed that prophylactic cinnarizine reduced the frequency of vertigo and headaches. Lepcha et al. (2014) demonstrated that prophylactic flunarizine reduced the frequency and severity of vertigo episodes. Sunitha et al. (2019) discussed the role of therapeutic flunarizine, although they did not report its efficacy. El-Badry et al. (2017) saw a 92% cure rate of positional vertigo among 13 VM patients with either cinnarizine or topiramate, which may indicate an improvement in motion sensitivity symptoms with anti-migraine therapy. One study mentioned mashbaladi pachana kashaya and pana, a form of Indian ayurvedic medicine (Anshul et al., 2020). Other treatments included prophylactic beta blockers (Prakash et al., 2008; Sunitha et al., 2019), dimenhydrinate (Udagatti and Dinesh Kumar, 2017), paracetamol (Prakash et al., 2008; Prakash and Shah, 2009), promethazine (Prakash and Shah, 2009), methylprednisolone (Prakash and Shah, 2009), and triptans (Prakash et al., 2008). Nonpharmacologic treatments included avoidance of triggers (Anshul et al., 2020) and vestibular therapy (Lepcha et al., 2014).
Table 4.
Management for vestibular migraine in the included studies.
| First author, year of study | Prophylactic or abortive? | Medical treatment of study | Additional management | Effect of treatment |
|---|---|---|---|---|
| Anshul et al., 2020 | Prophylactic | Mashbaladi pachana kashaya nasya (nasal administration) and pana BID for 1 month | Avoidance to dust, smoke, sunshine, anger, excess fatty and liquid diet, day sleeping, cold water | Patient reported complete relief of symptoms during 4-month follow-up period |
| El-Badry et al., 2017 | Prophylactic | 37.5-mg cinnarizine, BID or 50-mg topiramate daily | N/A | Cured positional vertigo in 92% of study group |
| Lepcha et al., 2014,a | Prophylactic | 10-mg flunarizine daily | Vestibular therapy | Frequency of vertigo differed between flunarizine treatment group and control group (p = 0.010); no difference in headache frequency and severity |
| Prakash et al., 2008,b | Both | Prophylactic 50-mg sumatriptan, 10-mg rizatriptan, 40- or 60-mg propranolol BID | N/A | Triptan was associated with reduction or resolution of vertigo symptoms; their effect on migraines is less clear |
| Abortive 50-mg sumatriptan, 10-mg rizatriptan, 500-mg paracetamol | ||||
| Prakash et al., 2009),c | Abortive | 1000-mg IV methylprednisolone, 50-mg topiramate BID, paracetamol-domperidon, 6-mg subcutaneous sumatriptan, 25-mg intramuscular promethazine | N/A | Termination or near complete resolution of vertigo |
| Prakash et al., 2021 | Both | 500-mg IV sodium valproate acutely and prophylactic 50-mg oral lamotrigine BID for 2–3 months | N/A | Patient was symptom-free for 2 years |
| Sunitha et al., 2019 | Both | Prophylactic beta blocker, flunarizine for acute attacks | N/A | N/A |
| Taghdiri et al., 2014 | Prophylactic | 37.5-mg cinnarizine tablet at night for the first 3 days, then 75-mg tablet daily for the remaining 12-week treatment period | N/A | Mean frequency of vertigo and mean frequency, duration, and intensity of migraines decreased after 3 months of cinnarizine (p < 0.001) |
| Udagatti et al., 2017 | Prophylactic | 10-mg flunarizine and/or cinnarizine and 50-mg dimenhydrinate | N/A | Patient was symptom-free for over 9 years |
Abbreviation: BID: twice a day; IV: intravenous; TID: three times a day.
A: This study was a randomized controlled trial. Both arms received 16-mg betahistine three times a day for 48 h after onset of vertigo and 1-g paracetamol for acute attacks of headaches. The treatment arm received flunarizine.
B: This study was a case series of three patients. Sumatriptan and rizatriptan were used sometimes prophylactically and sometimes abortively.
C: This study was a case series of four patients. All patients received intravenous methylprednisolone. In addition to methylprednisolone, one patient received topiramate, and another patient received paracetamol-domperidone, sumatriptan, and promethazine.
4. Discussion
This scoping review includes 26 studies from six countries and overall demonstrates very limited research on VM from LLMICs. The reported prevalence of VM at clinics ranged from 0.3% to 33.3%. The most common clinical presentations included headache, nausea, and photophobia. Diagnostic workup was broad and heterogeneous, with imaging, audiometry, and nystagmography as the three most widely utilized modalities. Only a third of studies discussed VM therapies, including calcium channel blockers such as flunarizine and cinnarizine, triptans, and paracetamol.
The health disparities in otolaryngology-head and neck surgery (OHNS) between high-income countries (HICs) and low- and middle-income countries are well-documented for certain conditions such as hearing loss (Leach et al., 2020; Waterworth et al., 2022) and head and neck cancer (Patterson et al., 2020), yet potential disparities in vestibular disease remain understudied. Although research surrounding the prevalence and social challenges of dizziness in LLMICs exists (Lasisi and Gureje, 2010, 2014), few are focused solely on VM. Given that this condition has been shown to be underdiagnosed in HICs, more focused research efforts are needed globally.
This review identified significant gaps in the VM research conducted in LLMICs. The majority of the studies were cross-sectional and aimed at capturing the frequency of various vestibulopathies seen in clinics. The second most common study design was the case study or series, which has limited generalizability. Prospective and randomized studies of novel or integrative medical treatments (e.g., ayurvedic medicine) can be a unique contribution of researchers from LLMICs and bolster the body of evidence for treatment efficacy of these interventions. The geographic spread of the included articles was also uneven, with two-thirds of the studies coming from India. Notably, few studies originated from Africa, where the majority of the LLMICs are located and the otolaryngology workforce is scarce (Fagan, 2018). The low number of articles reflects the reality that VM is not a major research priority in LLMICs, where non-communicable diseases are only recently starting to gain prominence (Jailobaeva et al., 2021).
The variability of terms used by the included studies is likely attributable to the fact that vestibular migraine was not an established entity until the relatively recent publication of a consensus statement by the Barany Society and the International Headache Society in 2012 (Lempert et al., 2012). While the condition was first described as early as 1917, it is only in the past two decades that significant efforts to characterize this condition were made (Multidisciplinary experts consensus for assessment and management of vestibular migraine, 2019). Even after 2012, however, several studies used a variety of terms other than vestibular migraine to refer to the condition. To facilitate research dissemination and avoid confusion, researchers should be encouraged to use the name “vestibular migraine” and utilize the Barany Society's diagnostic criteria (Lempert et al., 2012).
The dizziness workup utilized in the studies was widely heterogeneous. Unlike other vestibular diseases that may require equipment for diagnosis, VM is a purely clinical diagnosis with no pathognomonic test results (Huang et al., 2020). This can come as an advantage to providers in LLMICs, where vestibular and imaging diagnostic capacity may be limited. Most studies used a routine battery of testing for vertigo, which spanned hematologic workup and vestibular tests, and did not focus solely on diagnosing VM. The most utilized diagnostic modality was radiographic imaging, which is surprising given its low availability in LLMICs (Frija et al., 2021). Its high utilization among the included studies in our review, however, is likely because these studies took place in well-equipped tertiary clinics, with little representation from primary care, community, or rural settings. This may be also due to the limited availability of specialist training and equipment in vestibular diagnostics, and so the use of available imaging to rule out the presence of an identifiable central pathology may have been promoted instead. The large variability with respect to diagnostic approach to vertiginous patients in the included studies reflects heterogeneity of patients presenting with dizziness or vertigo to clinics in LLMICs, a setting in which other “must-not-miss” diagnoses such as stroke or brain tumors must be ruled out. Teaching how to quickly and effectively diagnose VM based on presenting symptoms in LLMICs could potentially avert the use of expensive and unnecessary diagnostic testing modalities.
The clinical manifestations of VM reported in the LLMIC literature closely matches the presentation of VM as described in the HIC literature. As expected, headache, the hallmark symptom of VM, was reported by most articles, although studies did not present details of headaches or the temporality between headaches and vertigo. Photophobia and phonophobia, also well-known features of VM, were observed. All findings were aligned with the expected phenotype of VM (Huang et al., 2020).
VM therapies used in LLMICs included conventional migraine pharmacotherapies, although some studies suggested less common treatments, such as ayurvedic medicine. Calcium channel inhibitors, such as flunarizine and cinnarizine, were the most studied. While studies in our review demonstrated these medications’ efficacy, other studies have shown mixed results (Bikhazi et al., 1997; Maione, 2006; Rashid et al., 2022). Triptans, beta-adrenergic blockers, and antiepileptics were also discussed, which have been shown to be effective in the literature (Bikhazi et al., 1997; Huang et al., 2020; Maione, 2006). Case studies and series demonstrated the effects of medications that are not typically used for VM, such as methylprednisolone (Prakash and Shah, 2009). One case study examined mashbaladi pachana kashaya nasya, a nasally delivered ayurvedic medication that is known to improve aggravated vata (a force responsible for all body functions) (Anshul et al., 2020; Yadav et al., 2022). Integrative medicine, which brings together traditional therapies and complementary medicine, may be a critical contribution by LLMIC researchers, as alternative interventions such as mindfulness exercises and tai chi have been shown to help dizzy patients (Formeister, 2022; Huang et al., 2019).
This review lays out several future directions for VM research in LLMICs. First, future investigations can examine VM in community settings. The data in our review is mostly limited to dizziness or otolaryngology clinics, which doesn't reflect the true prevalence in the general population or the clinical practices of community providers. Second, little is reported on the impact of VM on the life of this population in LLMICs. Third, there should be greater focus on innovative approaches to diagnosis and therapies that stem from LLMICs. Reverse innovation, or an intervention derived from low-resource settings that can be implemented in high-resource settings, can improve vestibular care in HICs (Ahmed et al., 2017). Two studies shared the results of innovative systems designed to aid the diagnostic process for vestibular disease, which show promise in diagnosing VM (Bansal, 2016; Mouelhi et al., 2020). In addition to encouraging LLMIC researchers to pursue further work in innovation, institutions of HICs can engage in equitable partnerships to support more VM research in these countries (Patterson et al., 2021). The broader scientific community can greatly benefit from better adoption of techniques that providers of LLMICs have developed and refined to provide high quality care for VM patients despite resource constraints.
This study has several notable limitations. First, the scoping review is limited to LLMICs and does not include research from UMICs. While UMICs also face significant barriers to research and dissemination, our review intentionally focused on LLMICs because we sought to capture the current state of VM research in the countries that are most underrepresented in scientific literature. Second, there was considerable variability in the terminology of VM. While some studies specifically used the term “vestibular migraine,” not all studies used this terminology or referenced specific criteria used to make the diagnosis of VM. For maximum inclusivity, we adopted a broader definition of VM and included any articles that referred to VM, migraine-associated vertigo, or migraine accompanied by vertigo. Third, our study only searched for articles in English because of the authors’ language abilities. Future works can examine articles in other common research languages, such as French and Spanish.
5. Conclusion
In this scoping review, 26 studies on VM conducted in LLMICs in the last 20 years were identified. There was an overall low volume of evidence related to diagnosis and treatment of VM, and many studies were limited in scope because of low sample size. Future directions include diversifying study design, exploring innovative diagnostic and therapeutic modalities, and studying the prevalence and impact of VM in community settings. Supporting VM research in LLMICs can yield new insights into VM management and improve the lives of VM patients globally.
Ethics approval
All study data were collected from published journal articles, so no ethics approval was obtained for this scoping review.
Funding
Authors did not receive any funding for this work.
Authors’ contributions
EK, AJ, and CW were involved in study conception and design. EK, AJ, PT, and CW designed the search strategy. EK, AS, MT, and AJ were involved in data collection. EK, AS, MT, CW, EF, AJ, and PT analyzed the data and were involved with manuscript preparation and critical revision.
Declaration of competing interest
Authors have no disclosures.
Acknowledgment
On behalf of the Global OHNS Initiative, we would like to thank the following collaborators for their contribution: Chee Yang Tan, Rolvix H. Patterson, and Mary Jue Xu.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
Appendix 1. Full search strategy
PubMed search #2:
("Vestibular Diseases/diagnosis"[Mesh] "Vestibular Diseases/diagnostic imaging"[Mesh] OR "Vestibular Diseases/drug therapy"[Mesh] OR "Vestibular Diseases/prevention and control"[Mesh] OR "Vestibular Diseases/rehabilitation"[Mesh] OR "Vestibular Diseases/surgery"[Mesh] OR "Vestibular Diseases/therapy"[Mesh] OR "Vestibular Neuronitis/diagnosis"[Mesh] OR "Vestibular Neuronitis/diagnostic imaging"[Mesh] OR "Vestibular Neuronitis/drug therapy"[Mesh] OR "Vestibular Neuronitis/rehabilitation"[Mesh] OR "Vestibular Neuronitis/surgery"[Mesh] OR "Vestibular Neuronitis/therapy"[Mesh] OR (“vestibular disease” OR “vestibular diseases” OR “vestibular neuronitis” OR vertigo OR "Bilateral Vestibulopathy” OR "Semicircular Canal Dehiscence" OR "Endolymphatic Hydrops"[Mesh] OR "Endolymphatic Hydrops" OR "Meniere Disease" OR "Labyrinthitis"[Mesh] OR labyrinthitis) AND (diagnosis OR “diagnostic imaging” OR “drug therapy” OR “drug treatment” OR “prevention-and-control” OR surgery OR therapy))
AND ("developing countries"[mesh] OR “developing countries” OR “developing country” OR LMIC OR “low income countries” OR “low income country” OR “low and middle income countries” OR “low middle income countries” OR “middle income countries” OR “middle income country” OR “low resource setting” OR “resource-limited” OR “resource poor” OR “Central America” OR “Central America”[Mesh] OR “Costa Rica” OR “El Salvador” OR Guatemala OR Honduras OR Nicaragua OR Panama OR “Latin America” OR “Latin America”[Mesh] OR “South America” OR “South America”[Mesh] OR Argentina OR Bolivia OR Brazil OR Chile OR Colombia OR Ecuador OR Guyana OR Paraguay OR Peru OR Uruguay OR Venezuela OR “Mexico”[mesh] OR Mexico OR “Cuba”[mesh] OR Cuba OR “Puerto Rico”[mesh] OR “Puerto Rico” OR “Dominican Republic”[mesh] OR “Dominican Republic” OR “democratic people's republic of Korea” OR "Democratic People's Republic of Korea"[Mesh] OR Cambodia OR "Cambodia"[Mesh] OR Kiribati OR Lao-PDR OR "Laos"[Mesh] OR Micronesia OR “Micronesia”[mesh] OR Mongolia OR “Mongolia”[mesh] OR Myanmar OR “Myanmar”[mesh] OR “Papua New Guinea” OR "Papua New Guinea"[Mesh] OR Philippines OR "Philippines"[Mesh] OR Melanesia OR “Melanesia”[mesh] OR “Solomon Islands” OR “Timor-Leste” OR "Timor-Leste"[Mesh] OR Vanuatu OR "Vanuatu"[Mesh] OR Vietnam OR "Vietnam"[Mesh] OR Tajikistan OR "Tajikistan"[Mesh] OR “Kyrgyz Republic” OR "Kyrgyzstan"[Mesh] OR Moldova OR "Moldova"[Mesh] OR Ukraine OR "Ukraine"[Mesh] OR Uzbekistan OR “Uzbekistan”[mesh] OR Haiti OR "Haiti"[Mesh] OR “Syrian Arab Republic” OR "Syria"[Mesh] OR Yemen OR "Yemen"[Mesh] OR Algeria OR "Algeria"[Mesh] OR Djibouti OR "Djibouti"[Mesh] OR Egypt OR "Egypt"[Mesh] OR Morocco OR “Morocco”[mesh] OR Tunisia OR "Tunisia"[Mesh] OR “West Bank and Gaza” OR “Gaza Strip” OR Afghanistan OR “Afghanistan”[mesh] OR Bangladesh OR "Bangladesh"[Mesh] OR Bhutan OR "Bhutan"[Mesh] OR India OR "India"[Mesh] OR Nepal OR "Nepal"[mesh] OR Pakistan OR "Pakistan"[Mesh] OR “Sri Lanka” OR "Sri Lanka"[Mesh] OR “Burkina Faso” OR "Burkina Faso"[Mesh] OR Burundi OR "Burundi"[Mesh] OR “Central African Republic” OR "Central African Republic"[Mesh] OR Chad OR "Chad"[Mesh] OR “Democratic Republic of the Congo” OR "Democratic Republic of the Congo"[Mesh] OR Eritrea OR "Eritrea"[Mesh] OR Ethiopia OR "Ethiopia"[Mesh] OR Gambia OR “Gambia”[mesh] OR Guinea OR "Guinea"[Mesh] OR “Guinea-Bissau” OR "Guinea-Bissau"[Mesh] OR Liberia OR "Liberia"[Mesh] OR Madagascar OR "Madagascar"[Mesh] OR Malawi OR "Malawi"[Mesh] OR Mali OR "Mali"[Mesh] OR Mozambique OR "Mozambique"[Mesh] OR Niger OR "Niger"[Mesh] OR Rwanda OR "Rwanda"[Mesh] OR “Sierra Leone” OR "Sierra Leone"[Mesh] OR Somalia OR "Somalia"[Mesh] OR “South Sudan” OR "South Sudan"[Mesh] OR Sudan OR "Sudan"[Mesh] OR Togo OR “Togo”[mesh] OR Uganda OR “Uganda”[mesh] OR Angola OR “Angola”[mesh] OR Benin OR “Benin”[mesh] OR “Cabo Verde” OR "Cabo Verde"[Mesh] OR Cameroon OR “Cameroon”[mesh] OR Comoros OR "Comoros"[Mesh] OR Congo OR “Congo”[mesh] OR “Côte d'Ivoire” OR "Cote d'Ivoire"[Mesh] OR Eswatini OR “Eswatini”[mesh] OR Ghana OR “Ghana”[mesh] OR Kenya OR “Kenya”[mesh] OR Lesotho OR “Lesotho”[mesh] OR Mauritania OR "Mauritania"[Mesh] OR Nigeria OR “Nigeria”[mesh] OR “São Tomé and Principe” OR "Sao Tome and Principe"[Mesh] OR Senegal OR “Senegal”[mesh] OR Tanzania OR “Tanzania”[mesh] OR Zambia OR “Zambia”[mesh] OR Zimbabwe OR “Zimbabwe”[mesh] OR Belize OR "Belize"[Mesh] OR Aruba OR "Aruba"[Mesh] OR “British Virgin Islands” OR "British Virgin Islands"[Mesh] OR Curacao OR "Curacao"[Mesh] OR Grenada OR "Grenada"[Mesh] OR Jamaica OR "Jamaica"[Mesh] OR Indonesia OR "Indonesia"[Mesh] OR Africa OR "Africa"[Mesh] OR Caribbean OR "Caribbean Region"[Mesh])
NOT (“guinea pig” OR “guinea pigs”)
Refs = 1,727
WoS search #2:
Use the search boxes on the main search screen and follow these instructions. Don't add or remove any parenthesis:
Copy and paste this search hedge into the first search box:
(“vestibular disease” OR “vestibular diseases” OR “vestibular neuronitis” OR vertigo OR "Bilateral Vestibulopathy” OR "Semicircular Canal Dehiscence" OR “Endolymphatic Hydrops" OR "Meniere Disease" OR labyrinthitis) AND (diagnosis OR “diagnostic imaging” OR “drug therapy” OR “drug treatment” OR “prevention-and-control” OR rehabilitation OR surgery OR therapy)
Copy and paste this search hedge into the second search box; also, change the drop-down menu to the left of the search box from ALL FIELDS to TOPIC:
(“developing countries” OR “developing country” OR LMIC OR “low income countries” OR “low income country” OR “low and middle income countries” OR “low middle income countries” OR “middle income countries” OR “middle income country” OR “low resource setting” OR “resource-limited” OR “resource poor” OR “Central America” OR “Costa Rica” OR “El Salvador” OR Guatemala OR Honduras OR Nicaragua OR Panama OR “Latin America” OR “South America” OR Argentina OR Bolivia OR Brazil OR Chile OR Colombia OR Ecuador OR Guyana OR Paraguay OR Peru OR Uruguay OR Venezuela OR Mexico OR Cuba OR “Puerto Rico” OR “Dominican Republic” OR “democratic people's republic of Korea” OR Cambodia OR Kiribati OR Lao-PDR OR Laos OR Micronesia OR Mongolia OR Myanmar OR “Papua New Guinea” OR Philippines OR Melanesia OR “Solomon Islands” OR “Timor-Leste” OR Vanuatu OR Vietnam OR Tajikistan OR “Kyrgyz Republic” OR Kyrgyzstan OR Moldova OR Ukraine OR Uzbekistan OR Haiti OR “Syrian Arab Republic” OR Syria OR Yemen OR Algeria OR Djibouti OR Egypt OR Morocco OR Tunisia OR “West Bank and Gaza” OR “Gaza Strip” OR Afghanistan OR Bangladesh OR Bhutan OR India OR Nepal OR Pakistan OR “Sri Lanka” OR “Burkina Faso” OR Burundi OR “Central African Republic” OR Chad OR “Democratic Republic of the Congo” OR Eritrea OR Ethiopia OR Gambia OR Guinea OR “Guinea-Bissau” OR Liberia OR Madagascar OR Malawi OR Mali OR Mozambique OR Niger OR Rwanda OR “Sierra Leone” OR Somalia OR “South Sudan” OR Sudan OR Togo OR Uganda OR Angola OR Benin OR “Cabo Verde” OR Cameroon OR Comoros OR Congo OR “Côte d'Ivoire” OR Eswatini OR Ghana OR Kenya OR Lesotho OR Mauritania OR Nigeria OR “São Tomé and Principe” OR Senegal OR Tanzania OR Zambia OR Zimbabwe OR Belize OR Aruba OR “British Virgin Islands” OR Curacao OR Grenada OR Jamaica OR Indonesia OR Africa OR Caribbean)
Copy and paste this into the 3rd search box, and change the drop down menu to the left from AND to NOT:
“guinea pig” OR “guinea pigs”
Refs = 125
Embase search #2:
('vestibular disorder'/exp/dm_di,dm_dt,dm_pc,dm_su,dm_th,dm_rh OR 'vestibular neuronitis'/exp/dm_di,dm_dt,dm_pc,dm_rh,dm_su,dm_th OR 'vertigo'/exp/dm_di,dm_dt,dm_pc,dm_su,dm_th,dm_rh OR 'bilateral vestibulopathy'/exp/dm_di,dm_dt,dm_pc,dm_su,dm_th,dm_rh OR 'semicircular canal dehiscence'/exp/dm_di,dm_dt,dm_pc,dm_su,dm_th,dm_rh OR 'meniere disease'/exp/dm_di,dm_dt,dm_pc,dm_su,dm_th,dm_rh OR 'labyrinthitis'/exp/dm_di,dm_dt,dm_pc,dm_su,dm_th,dm_rh OR 'vestibular disorder':ab,ti OR 'vestibular neuronitis':ab,ti OR 'vertigo':ab,ti OR 'bilateral vestibulopathy':ab,ti OR 'semicircular canal dehiscence':ab,ti OR 'meniere disease':ab,ti OR 'labyrinthitis':ab,ti) AND ('diagnosis':ab,ti OR ‘diagnostic imaging’:ab,ti OR 'drug therapy':ab,ti OR 'prevention':ab,ti OR 'surgery':ab,ti OR 'therapy':ab,ti OR ‘rehabilitation’:ab,ti)
AND ('developing country'/exp OR 'developing country' OR lmic OR 'low income country'/exp OR 'low income country' OR 'low and middle income country'/exp OR 'low and middle income country' OR 'low and middle income countries'/exp OR 'low and middle income countries' OR 'low middle income country'/exp OR 'low middle income country' OR 'low middle income countries' OR 'middle income country'/exp OR 'middle income country' OR 'low resource setting'/exp OR 'low resource setting' OR 'resource-limited' OR 'resource limited setting'/exp OR 'resource limited setting' OR 'resource poor' OR 'central america'/exp OR 'central america' OR 'costa rica'/exp OR 'costa rica' OR 'el salvador'/exp OR 'el salvador' OR 'guatemala'/exp OR 'guatemala' OR 'honduras'/exp OR 'honduras' OR 'nicaragua'/exp OR 'nicaragua' OR 'panama'/exp OR 'panama' OR 'south and central america'/exp OR 'south and central america' OR 'south america'/exp OR 'south america' OR 'argentina'/exp OR 'argentina' OR 'bolivia'/exp OR 'bolivia' OR 'brazil'/exp OR 'brazil' OR 'chile'/exp OR 'chile' OR 'colombia'/exp OR 'colombia' OR 'ecuador'/exp OR 'ecuador' OR 'guyana'/exp OR 'guyana' OR 'paraguay'/exp OR 'paraguay' OR 'peru'/exp OR 'peru' OR 'uruguay'/exp OR 'uruguay' OR 'venezuela'/exp OR 'venezuela' OR 'mexico'/exp OR 'mexico' OR 'cuba'/exp OR 'cuba' OR 'puerto rico'/exp OR 'puerto rico' OR 'dominican republic'/exp OR 'dominican republic' OR 'korea'/exp OR 'korea' OR 'south korea'/exp OR 'south korea' OR 'cambodia'/exp OR 'cambodia' OR 'laos'/exp OR 'laos' OR 'kiribati'/exp OR 'kiribati' OR 'federated states of micronesia'/exp OR 'federated states of micronesia' OR 'mongolia'/exp OR 'mongolia' OR 'myanmar'/exp OR 'myanmar' OR 'papua new guinea'/exp OR 'papua new guinea' OR 'philippines'/exp OR 'philippines' OR 'melanesia'/exp OR 'melanesia' OR 'solomon islands'/exp OR 'solomon islands' OR 'timor-leste'/exp OR 'timor-leste' OR 'vanuatu'/exp OR 'vanuatu' OR 'viet nam'/exp OR 'viet nam' OR 'tajikistan'/exp OR 'tajikistan' OR 'kyrgyzstan'/exp OR 'kyrgyzstan' OR 'moldova'/exp OR 'moldova' OR 'ukraine'/exp OR 'ukraine' OR 'uzbekistan'/exp OR 'uzbekistan' OR 'haiti'/exp OR 'haiti' OR 'syrian arab republic'/exp OR 'syrian arab republic' OR 'yemen'/exp OR 'yemen' OR 'algeria'/exp OR 'algeria' OR 'djibouti'/exp OR 'djibouti' OR 'egypt'/exp OR 'egypt' OR 'morocco'/exp OR 'morocco' OR 'tunisia'/exp OR 'tunisia' OR 'gaza strip'/exp OR 'gaza strip' OR 'gaza strip palestine'/exp OR 'gaza strip palestine' OR 'afghanistan'/exp OR 'afghanistan' OR 'bangladesh'/exp OR 'bangladesh' OR 'bhutan'/exp OR 'bhutan' OR 'india'/exp OR 'india' OR 'nepal'/exp OR 'nepal' OR 'pakistan'/exp OR 'pakistan' OR 'sri lanka'/exp OR 'sri lanka' OR 'burkina faso'/exp OR 'burkina faso' OR 'burundi'/exp OR 'burundi' OR 'central african republic'/exp OR 'central african republic' OR 'chad'/exp OR 'chad' OR 'democratic republic congo'/exp OR 'democratic republic congo' OR 'eritrea'/exp OR 'eritrea' OR 'ethiopia'/exp OR 'ethiopia' OR 'gambia'/exp OR 'gambia' OR 'guinea'/exp OR 'guinea' OR 'guinea-bissau'/exp OR 'guinea-bissau' OR 'liberia'/exp OR 'liberia' OR 'madagascar'/exp OR 'madagascar' OR 'malawi'/exp OR 'malawi' OR 'mali'/exp OR 'mali' OR 'mozambique'/exp OR 'mozambique' OR 'niger'/exp OR 'niger' OR 'rwanda'/exp OR 'rwanda' OR 'sierra leone'/exp OR 'sierra leone' OR 'somalia'/exp OR 'somalia' OR 'south sudan'/exp OR 'south sudan' OR 'sudan'/exp OR 'sudan' OR 'togo'/exp OR 'togo' OR 'uganda'/exp OR 'uganda' OR 'angola'/exp OR 'angola' OR 'benin'/exp OR 'benin' OR 'cape verde'/exp OR 'cape verde' OR 'cameroon'/exp OR 'cameroon' OR 'comoros'/exp OR 'comoros' OR 'congo'/exp OR 'congo' OR 'eswatini'/exp OR 'eswatini' OR 'ghana'/exp OR 'ghana' OR 'kenya'/exp OR 'kenya' OR 'lesotho'/exp OR 'lesotho' OR 'mauritania'/exp OR 'mauritania' OR 'nigeria'/exp OR 'nigeria' OR 'sao tome and principe'/exp OR 'sao tome and principe' OR 'senegal'/exp OR 'senegal' OR 'tanzania'/exp OR 'tanzania' OR 'zambia'/exp OR 'zambia' OR 'zimbabwe'/exp OR 'zimbabwe' OR 'belize'/exp OR 'belize' OR 'aruba'/exp OR 'aruba' OR 'virgin islands (british)'/exp OR 'virgin islands (british)' OR 'curacao'/exp OR 'curacao' OR 'grenada'/exp OR 'grenada' OR 'jamaica'/exp OR 'jamaica' OR 'indonesia'/exp OR 'indonesia' OR 'africa'/exp OR 'africa' OR 'caribbean islands'/exp OR 'caribbean islands' OR 'caribbean'/exp OR 'caribbean' OR 'cote d'ivoire'/exp OR 'cote d'ivoire') NOT ('guinea pig'/exp OR 'guinea pig') AND [2002-2022]/py
Refs = 2,239 (of these, 1050 are unique to Embase, and of the 1050, 360 are conference abstracts)
References
- Adegbiji W.A., Aremu S.K., Alabi B.S., Nwawolo C.C., Olajuyin O.A. Vertigo presentation in developing country, Nigeria. Am J Res Commun. 2014;5:258–271. [Google Scholar]
- Ahmed F., Ahmed N., Briggs T.W.R., Pronovost P.J., Shetty D.P., Jha A.K., et al. Can reverse innovation catalyse better value health care? Lancet Global Health. 2017;5:e967–e968. doi: 10.1016/S2214-109X(17)30324-8. [DOI] [PubMed] [Google Scholar]
- Akdal G., Baykan B., Ertaş M., Zarifoğlu M., Karli N., Saip S., et al. Population-based study of vestibular symptoms in migraineurs. Acta Otolaryngol. 2015;135:435–439. doi: 10.3109/00016489.2014.969382. [DOI] [PubMed] [Google Scholar]
- Akdal G., Ozge A., Ergör G. The prevalence of vestibular symptoms in migraine or tension-type headache. J Vestib Res Equilib Orientat. 2013;23:101–106. doi: 10.3233/VES-130477. [DOI] [PubMed] [Google Scholar]
- Anshul Srivastava A., Mohanty D., Mehta A. Ayurvedic management of chronic migraine through mashbaladi pachan kashaya nasya: a case study. Int. J. Res. Ayurveda Pharm. 2020;11:1–3. doi: 10.7897/2277-4343.110477. [DOI] [Google Scholar]
- Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Ashish G., Augustine A.M., Tyagi A.K., Lepcha A., Balraj A. Subjective visual vertical and horizontal in vestibular migraine. J Int Adv Otol. 2017;13:254–258. doi: 10.5152/iao.2017.4056. [DOI] [PubMed] [Google Scholar]
- Bansal M. Common causes of vertigo and dizziness in Gujarat. Int J Clin Trials. 2016;3:250–253. doi: 10.18203/2349-3259.ijct20163964. [DOI] [Google Scholar]
- Bikhazi P., Jackson C., Ruckenstein M.J. Efficacy of antimigrainous therapy in the treatment of migraine-associated dizziness. Am. J. Otol. 1997;18:350–354. [PubMed] [Google Scholar]
- Das S., Chakraborty S., Shekar S. Dizziness in a tertiary care centre in Sikkim: our experience and limitations. Indian J. Otolaryngol. Head Neck Surg. 2017;69:443–448. doi: 10.1007/s12070-017-1221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dash A.K., Panda N., Khandelwal G., Lal V., Mann S.S. Migraine and audiovestibular dysfunction: is there a correlation? Am. J. Otolaryngol. 2008;29:295–299. doi: 10.1016/j.amjoto.2007.09.004. [DOI] [PubMed] [Google Scholar]
- El-Badry M.M., Samy H., Kabel A.M., Rafat F.M., Sanyelbhaa H. Clinical criteria of positional vertical nystagmus in vestibular migraine. Acta Otolaryngol. 2017;137:720–722. doi: 10.1080/00016489.2017.1318220. [DOI] [PubMed] [Google Scholar]
- ElSherif M., Reda M.I., Saadallah H., Mourad M. Eye movements and imaging in vestibular migraine. Acta Otorrinolaringol. Esp. 2020;71:3–8. doi: 10.1016/j.otorri.2018.10.001. [DOI] [PubMed] [Google Scholar]
- Fagan J.J. Workforce considerations, training, and diseases in africa. Otolaryngol. Clin. 2018;51:643–649. doi: 10.1016/j.otc.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Formeister E.J. 2022. Mindfulness-Based Stress Reduction for the Treatment of Vestibular Migraine. [Google Scholar]
- Formeister E.J., Rizk H.G., Kohn M.A., Sharon J.D. The epidemiology of vestibular migraine: a population-based survey study. Otol. Neurotol. 2018;39:1037–1044. doi: 10.1097/MAO.0000000000001900. [DOI] [PubMed] [Google Scholar]
- Frija G., Blažić I., Frush D.P., Hierath M., Kawooya M., Donoso-Bach L., et al. How to improve access to medical imaging in low- and middle-income countries. EClinicalMedicine. 2021;38 doi: 10.1016/j.eclinm.2021.101034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haripriya G.R., Lepcha A., Augustine A.M., John M., Philip A., Mammen M.D. Prevalence, clinical profile, and diagnosis of pediatric dizziness in a tertiary care hospital. Int. J. Pediatr. Otorhinolaryngol. 2021;146 doi: 10.1016/j.ijporl.2021.110761. [DOI] [PubMed] [Google Scholar]
- Hsu L.-C., Wang S.-J., Fuh J.-L. Prevalence and impact of migrainous vertigo in mid-life women: a community-based study. Cephalalgia. 2011;31:77–83. doi: 10.1177/0333102410373152. [DOI] [PubMed] [Google Scholar]
- Huang H.-W., Nicholson N., Thomas S. Impact of tai chi exercise on balance disorders: a systematic review. Am. J. Audiol. 2019;28:391–404. doi: 10.1044/2018_AJA-18-0115. [DOI] [PubMed] [Google Scholar]
- Huang T.-C., Wang S.-J., Kheradmand A. Vestibular migraine: an update on current understanding and future directions. Cephalalgia. 2020;40:107–121. doi: 10.1177/0333102419869317. [DOI] [PubMed] [Google Scholar]
- Jailobaeva K., Falconer J., Loffreda G., Arakelyan S., Witter S., Ager A. An analysis of policy and funding priorities of global actors regarding noncommunicable disease in low- and middle-income countries. Glob. Health. 2021;17:68. doi: 10.1186/s12992-021-00713-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ky L.M., Uyen N.T.T., Van N.T.K., Xuong N.T., Thanh C.M., Tuan N.T., et al. Study of the features of systemic dizziness in patients with chronic and recurrent migraine. 2021. 20. [DOI]
- Lasisi A.O., Gureje O. Prevalence and correlates of dizziness in the ibadan study of ageing. Ear Nose Throat J. 2014;93:E37–E44. [PMC free article] [PubMed] [Google Scholar]
- Lasisi A.O., Gureje O. Disability and quality of life among community elderly with dizziness: report from the Ibadan study of ageing. J. Laryngol. Otol. 2010;124:957–962. doi: 10.1017/S0022215110000538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach A.J., Homøe P., Chidziva C., Gunasekera H., Kong K., Bhutta M.F., et al. Panel 6: otitis media and associated hearing loss among disadvantaged populations and low to middle-income countries. Int. J. Pediatr. Otorhinolaryngol. 2020;130(Suppl. 1) doi: 10.1016/j.ijporl.2019.109857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lempert T., Olesen J., Furman J., Waterston J., Seemungal B., Carey J., et al. Vestibular migraine: diagnostic criteria. J Vestib Res Equilib Orientat. 2012;22:167–172. doi: 10.3233/VES-2012-0453. [DOI] [PubMed] [Google Scholar]
- Lepcha A., Amalanathan S., Augustine A.M., Tyagi A.K., Balraj A. Flunarizine in the prophylaxis of migrainous vertigo: a randomized controlled trial. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. 2014;271:2931–2936. doi: 10.1007/s00405-013-2786-4. [DOI] [PubMed] [Google Scholar]
- Maione A. Migraine-related vertigo: diagnostic criteria and prophylactic treatment. Laryngoscope. 2006;116:1782–1786. doi: 10.1097/01.mlg.0000231302.77922.c5. [DOI] [PubMed] [Google Scholar]
- Mallampalli M.P., Rizk H.G., Kheradmand A., Beh S.C., Abouzari M., Bassett A.M., et al. Care gaps and recommendations in vestibular migraine: an expert panel summit. Front. Neurol. 2022;12 doi: 10.3389/fneur.2021.812678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamindla P., Mogilicherla S., Enumula D., Prasad P. A descriptive EpidemiologicalStudy on migraine. 2020. 13. [DOI]
- Mostafa B.E., Kahky A.O.E., Kader H.M.A., Rizk M. Central vestibular dysfunction in an otorhinolaryngological vestibular unit: incidence and diagnostic strategy. Int. Arch. Otorhinolaryngol. 2014;18:235–238. doi: 10.1055/s-0034-1370884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouelhi A., Ben Slama A., Marrakchi J., Trabelsi H., Sayadi M., Labidi S. Sparse classification of discriminant nystagmus features using combined video-oculography tests and pupil tracking for common vestibular disorder recognition. Comput. Methods Biomech. Biomed. Eng. 2020;24:400–418. doi: 10.1080/10255842.2020.1830972. [DOI] [PubMed] [Google Scholar]
- Multidisciplinary experts consensus for assessment and management of vestibular migraine. Chin. Med. J. 2019;132:183–189. doi: 10.1097/CM9.0000000000000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogah S.A. Aetiology of vertigo as seen at the federal medical center lokoja, north Central Nigeria. Sudan J Med Sci. 2017;12:19–24. doi: 10.4314/sjms.v12i1. [DOI] [Google Scholar]
- Olusesi A.D., Abubakar J. 10 years of vertigo clinic at national hospital abuja, Nigeria: what have we learned? Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. 2016;273:3567–3572. doi: 10.1007/s00405-016-3969-6. [DOI] [PubMed] [Google Scholar]
- Patterson R.H., Fischman V.G., Wasserman I., Siu J., Shrime M.G., Fagan J.J., et al. Global burden of head and neck cancer: economic consequences, health, and the role of surgery. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2020;162:296–303. doi: 10.1177/0194599819897265. [DOI] [PubMed] [Google Scholar]
- Patterson R.H., Xu M.J., Okerosi S., Bhutta M.F., Der C., Alkire B., et al. Research equity in otolaryngology–head and neck surgery. OTO Open. 2021;5 doi: 10.1177/2473974X211024145. 2473974X211024145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakash S., Chavda B.V., Mandalia H., Dhawan R., Padmanabhan D. Headaches related to triptans therapy in patients of migrainous vertigo. J. Headache Pain. 2008;9:185–188. doi: 10.1007/s10194-008-0035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakash S., Prakash A., Lodha D. Bilateral persistent ophthalmoplegia in a patient with migraine: persistent migraine aura without infarction? BMJ Case Rep. 2021;14 doi: 10.1136/bcr-2021-242099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakash S., Shah N.D. Migrainous vertigo responsive to intravenous methylprednisolone: case reports. Headache. 2009;49:1235–1239. doi: 10.1111/j.1526-4610.2009.01474.x. [DOI] [PubMed] [Google Scholar]
- Rashid S.M.U., Sumaria S., Koohi N., Arshad Q., Kaski D. Patient experience of flunarizine for vestibular migraine: single centre observational study. Brain Sci. 2022;12:415. doi: 10.3390/brainsci12040415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargent E.W. The challenge of vestibular migraine. Curr. Opin. Otolaryngol. Head Neck Surg. 2013;21:473–479. doi: 10.1097/MOO.0b013e3283648682. [DOI] [PubMed] [Google Scholar]
- Sen K., Sarkar A., Raghavan A. The vertigo spectrum: a retrospective analysis in 149 walk-in patients at a specialised neurotology clinic. Astrocyte. 2016;3 [Google Scholar]
- Stovner L.J., Hagen K., Linde M., Steiner T.J. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23(1):34. doi: 10.1186/s10194-022-01402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strupp M., Versino M., Brandt T. Vestibular migraine. Handb. Clin. Neurol. 2010;97:755–771. doi: 10.1016/S0072-9752(10)97062-0. [DOI] [PubMed] [Google Scholar]
- Sunitha M., Asokan L., Sambandan A.P. Vertigo: incidences, diagnosis and its relations with hearing loss. Indian J. Otolaryngol. Head Neck Surg. 2019;71:1282–1286. doi: 10.1007/s12070-018-1315-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swain S.K., Baliarsingh D., Sahu M.C. Vertigo among elderly people: our experiences at a tertiary care teaching hospital of Eastern India. Ann Indian Acad Otorhinolaryngol Head Neck Surg. 2018;2:5. doi: 10.4103/aiao.aiao_11_18. [DOI] [Google Scholar]
- Swain S.K., Munjal S., Shajahan N. Vertigo in children: our experiences at a tertiary care teaching hospital of eastern India. J Sci Soc. 2020;47:74–78. doi: 10.4103/jss.JSS_20_20. [DOI] [Google Scholar]
- Syed S., Mittal H.K., Bist S., Agarwal V., Kumar L. 2020. Clinico-Aetiological Profile of Patients with Vertigo: A Cross-Sectional Observational Study. [DOI] [Google Scholar]
- Taghdiri F., Togha M., Razeghi Jahromi S., Refaeian F. Cinnarizine for the prophylaxis of migraine associated vertigo: a retrospective study. SpringerPlus. 2014;3:231. doi: 10.1186/2193-1801-3-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Udagatti V.D., Dinesh Kumar R. Migraine related vertigo. Indian J. Otolaryngol. Head Neck Surg. 2017;69:563–567. doi: 10.1007/s12070-017-1101-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T., Flaxman A.D., Naghavi M., Lozano R., Michaud C., Ezzati M., et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet Lond Engl. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waterworth C.J., Marella M., O'Donovan J., Bright T., Dowell R., Bhutta M.F. Barriers to access to ear and hearing care services in low- and middle- income countries: a scoping review. Global Publ. Health. 2022:1–25. doi: 10.1080/17441692.2022.2053734. [DOI] [PubMed] [Google Scholar]
- World Bank Country and Lending Groups – World Bank Data Help Desk 2022. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups n.d.
- Yadav M., Singh A., Meena J., Sankar J.M. A systematic review and meta-analysis of otorhinolaryngological manifestations of coronavirus disease 2019 in paediatric patients. J. Laryngol. Otol. 2022;136:588–603. doi: 10.1017/s0022215122000536. [DOI] [PubMed] [Google Scholar]
- Yao J., Nguyen A.X.-L., Xiang L., Li A., Wu A.Y. Geography, gender, and collaboration trends among global health authors. J Glob Health Rep. 2022;6 doi: 10.29392/001c.33616. [DOI] [Google Scholar]