Abstract
Background:
Hindfoot coronal alignment is an important factor in the assessment of patients with many different foot and ankle complaints. A number of clinical and radiographic techniques have been described to measure hindfoot coronal alignment, but none of them are widely accepted. The purpose of the present study was to assess the correlation between clinical and radiographic hindfoot alignment measures and to evaluate the reproducibility of each.
Methods:
We evaluated 85 patients with foot and/or ankle symptoms. Hindfoot clinical alignment was measured from photographs. Each patient was placed at a distance of 1 m from the observer, with both feet placed parallel. Four photographs were taken, at a height of 40 cm: a posterior view of both lower limbs including knees, a posterior view focalized on the studied hindfoot, an anterior view of the foot, and the last view of the medial aspect of the foot. Radiographic alignment was quantified on long axial view radiographs. Patients were lying over the film cassette with a focus distance of 1 m and the beam pointed to the ankle joint. The inclination angle of the beam was 45 degrees to the floor. Measurements were independently made by 2 observers, who were asked to classify pictures into 3 categories: varus, neutral, and valgus. Radiographic measurements were made using the angle measurement tool on the radiograph viewer. The intraclass correlation coefficients (ICCs) and the 95% confidence interval (CI) of the ICC were used to quantify the inter- and intraobserver reliability for clinical assessment. Radiographic parameters were correlated by calculating the Pearson correlation coefficient (r).
Results:
The intraobserver ICC for clinical analysis was good for both observers, while the interobserver ICC was moderate for both measurements. Regarding radiographic assessment, there was significant intra- and interobserver reliability. The correlation between both methods was weak for both observers.
Conclusions:
We found only weak intra- and interobserver correlations between the clinical and radiographic assessment of hindfoot coronal alignment. It is therefore necessary to complement the clinical evaluation of hindfoot alignment with an objective measurement method such as a long axial view radiograph. Further studies comparing different measurement methods need to be performed to establish the most objective evaluation.
Level of Evidence:
Level III, diagnostic study.
Keywords: hindfoot coronal alignment, hindfoot assessment
Commentary: A study comparing the clinical and radiographic (long calcaneal view) evaluation of hindfoot alignment in 85 patients. They found that there was a high correlation between observers, but not between clinical and radiographic evaluation. They concluded that it is important to supplement clinical evaluation with objective radiographic measures.
Hindfoot coronal alignment should be considered in the assessment of patients with foot and ankle complaints, since it affects treatment decision making for many foot and ankle problems (eg, ankle instability, 27 fifth metatarsal base fractures8,18).
When assessing hindfoot alignment, both clinical and radiographic evaluation should be considered to make a complete appraisal of the pathology. Multiple techniques have been described for each analysis (visual examination,12 -14 goniometry,2,12 -14 drawing lines on the skin, 22 employing measurement devices,17,22 modified radiographs,6,9,16 3-dimension biplanar radiographic assessment, 26 weight-bearing computed tomography 7 and magnetic resonance imaging,5,11 ellipsis superimposition, 15 lowest contact point, 23 lateral wall of the calcaneus,22,24 bisecting lines,17,26,28 and the 40% to 60% division 21 ), but none of them are widely accepted. Therefore, there is not an established algorithm for how to evaluate hindfoot coronal alignment.
Clinical hindfoot coronal alignment assessment (CHCAA) has the advantage of being performed at the office without the need for any devices; however, it may be influenced by individual features and by observers’ experience, becoming a great source of bias. 19 Measuring hindfoot alignment in the coronal plane radiographically is difficult because of the superimposition of the calcaneus with the mid- and forefoot. Although many radiographic techniques have been described to address this particular issue, 21 controversies still exist around selection of the ideal radiograph and measurement method.
The literature is scarce regarding comparison between clinical and radiographic evaluation. The purpose of the present study was to assess the correlation between clinical and radiographic hindfoot alignment measures and to evaluate the reproducibility of both methods.
Materials and Methods
The institutional review board approved the study protocol, and written informed consent was obtained from all patients prior to the study. We evaluated 85 consecutive patients who presented to our clinic with foot and/or ankle symptoms, other than rearfoot complaints. Hindfoot clinical alignment was evaluated through photographs taken at the time of presentation, and radiographic alignment was quantified on long axial view (LAV) 16 radiographs in a neutral rotation position. Measurements were made by 2 observers, different from the one who took the photographs (a foot and ankle surgeon, with 10 years’ experience, and a foot and ankle fellow), with a 30-day period between both measurements.
Clinical Evaluation
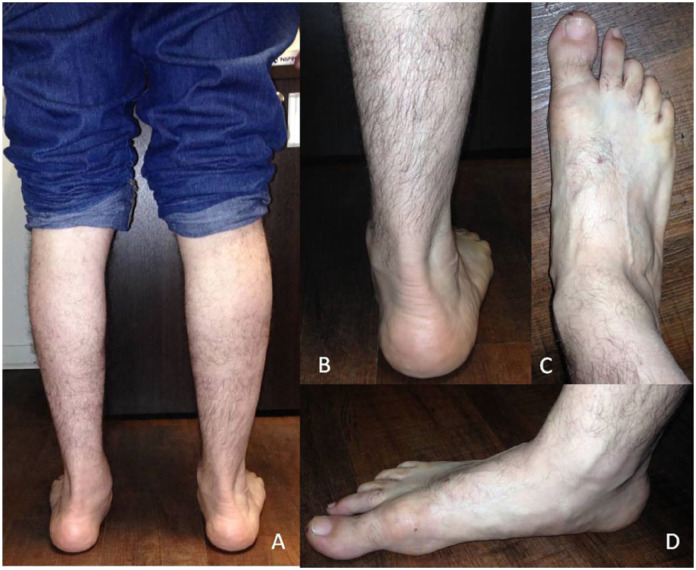
Each patient was placed at a distance of 1 m from the observer, with both feet placed parallel. Four photographs were taken, at a height of 40 cm. The first was a posterior view of both lower limbs including knees; the second one was also a posterior view focused on the studied hindfoot. These rear views were aimed to evaluate the lower limb’s global alignment and hindfoot alignment, which were better at identifying valgus deformity. The third view, an anterior view of the foot, was used to look for the “peek-a-boo heel” 18 thought to assess subtle varus deformity. The last view was a photograph of the medial aspect of the foot, important for ruling out midfoot pronation and medial hindfoot deformities, which may become a source of bias (Figure 1). Information regarding the physical examination was not provided, and observers were asked to limit their interpretation to the visual examination of the photographs.
Figure 1.
Photographic evaluation of foot alignment. (A) Posterior view of both lower limbs including knees. (B) Posterior view focalized on the studied hindfoot. (C) Anterior view of the foot. (D) Medial aspect of the foot.
Radiographic Technique
As described in the original publication of the LAV technique, 16 patients laid over the film cassette. The settings for the radiation source were 4 mAs and 50 kV, with a focus distance of 1 m, with the beam pointed at the ankle joint. The inclination angle of the beam was 45 degrees to the floor. The film cassette size was 35 by 43 cm (Figure 2).
Figure 2.
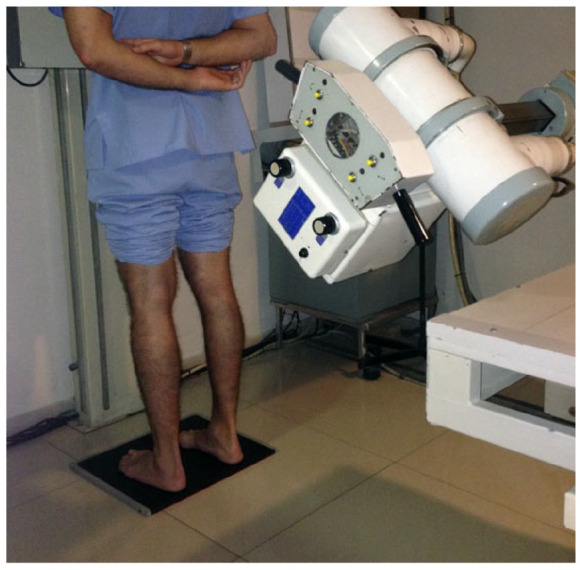
Long axial view radiographic technique.
Patients were placed in the bilateral stance with feet positioned 10 cm apart in a predefined foot position: the second metatarsal longitudinal axis aligned with the hindfoot.4,10
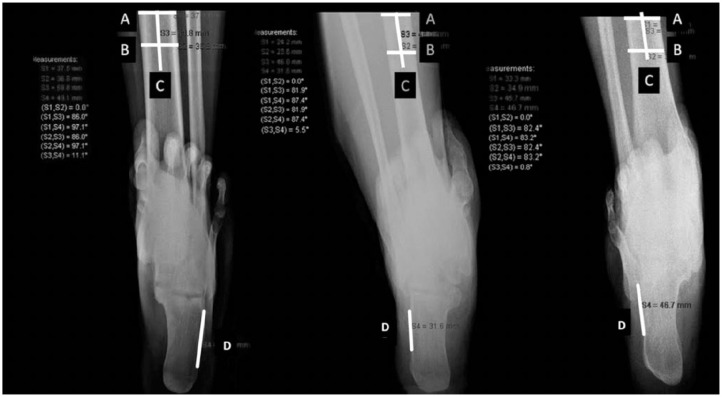
Measurement Methods
Photographic evaluation was made twice by each observer with images randomized, with a 30-d period between measurements. Observers were asked to classify pictures into 3 categories: varus, neutral, and valgus. Radiographic measurements were made using the angle measurement tool on the radiograph viewer (AGFA SE Media Viewer, version 3.7.0.0) Instructions on how to measure the LAV were provided to each observer. For tibial axis assessment, observers were instructed to bisect the tibia into 2 mid-diaphyseal points (lines A and B) 30 mm apart and extend this line distally (line C). 4 For the calcaneal axis, a line was drawn parallel to the calcaneus lateral wall (line D)13,24 (Figure 3). Results were classified as neutral for angles up to 5 degrees, as valgus for angles greater than 5.1 degrees, and as varus for negative angles. Each observer made 2 separate measurements independently, with the order of images randomized.
Figure 3.
For tibial axis assessment the tibia was bisected into two mid-diaphyseal points (lines A and B) 30 mm apart and extended this line distally (line C). For calcaneal axis a line was drawn parallel to the calcaneus lateral wall (line D).
Statistical Analysis
To quantify the inter- and intraobserver reliability for clinical assessment, the intraclass correlation coefficient (ICC) and 95% confidence interval (CI) of the ICC were used. ICC values were interpreted as follows: ICC 0.81 to 1 meant excellent agreement; 0.61 to 0.80, good agreement; 0.41 to 0.60, moderate agreement; 0.21 to 0.40, weak agreement; and less than 0.20, poor agreement. For radiographic parameter correlation, the Pearson correlation coefficient (r) was calculated. The significance level of r was corrected for multiple testing by dividing the significance level of .05 by the number of tests. Finally, for clinical and radiographic correlation analysis, results were categorized into 3 groups: varus, neutral, and valgus, as previously described. A 95% CI was applied. SPSS version 15.0 (SPSS Inc, Chicago, IL, USA) was used for every analyses.
To define the sample size, Epidat 4.1 (Ministry of Health, Xunta de Galicia, Spain; PAHO WHO; CES University, Colombia), was used. Sampling was applied to contrast hypotheses about the correlation coefficient; with 95% CI and 0.90 power, a minimum sample of 50 patients was needed.
Results
Intraobserver ICC for CHCAA was good for both observers (ICC of 0.78 for each one). Interobserver ICC was moderate for both measurements. Regarding radiographic assessment, there was statistically significant intraobserver reliability on each observer measurement (observer 1: r = 0.95 and observer 2: r = 0.99; P < .0001). The interobserver reliability was also statistically significant.
The correlation between both methods was weak for both observers: observer 1, ICC 0.072, P = .24 for the first measurement and ICC 0.167, P = .029, for the second measurement (Table 1); observer 2, ICC 0.23, P < .001, for the first measurement and ICC 0.137, P = .021, for the second measurement (Table 2).
Table 1.
Correlation Between Both Methods in Both Measurements, Observer 1 a .
| Cl, Obs1.1 | ||||||
|---|---|---|---|---|---|---|
| Varus | Neutral | Valgus | Total | P Value | ||
| Rx- Obs1.1 | Varus | 14 | 29 | 6 | 49 | |
| Neutral | 1 | 12 | 17 | 30 | ||
| Valgus | 0 | 2 | 4 | 6 | ||
| Total | 15 | 43 | 27 | 85 | .24 | |
| Cl, Obs1.2 | ||||||
| Rx- Obs1.2 | Varus | 14 | 25 | 8 | 47 | |
| Neutral | 1 | 15 | 15 | 31 | ||
| Valgus | 0 | 2 | 5 | 7 | ||
| Total | 15 | 42 | 28 | 85 | .029 | |
Bold indicates diagnostic agreement between the two evaluations.
Table 2.
Correlation Between Both Methods in Both Measurements, Observer 2 a .
| Cl, Obs2.1 | ||||||
|---|---|---|---|---|---|---|
| Varus | Neutral | Valgus | Total | p value | ||
| Rx- Obs2.1 | Varus | 20 | 18 | 12 | 50 | |
| Neutral | 1 | 10 | 13 | 24 | ||
| Valgus | 0 | 2 | 9 | 11 | ||
| Total | 21 | 30 | 34 | 85 | <.001 | |
| Cl, Obs2.2 | ||||||
| Rx- Obs2.2 | Varus | 18 | 22 | 12 | 52 | |
| Neutral | 0 | 6 | 18 | 24 | ||
| Valgus | 1 | 0 | 8 | 9 | ||
| Total | 19 | 28 | 38 | 85 | .021 | |
Bold indicates diagnostic agreement between the two evaluations.
Discussion
CHCAA is a great challenge for orthopedists, and the optimal method of evaluation is yet to be defined.1,8,20,27 It is influenced by patient and observer factors. On the patient side, the lack of feasible landmarks and many individual features (obesity, edema, Haglund’s deformity, heel shape, level of flaring of the calcaneal fat pad, length and width of the Achilles tendon insertion, midfoot pronation, metatarsus adductus) decreases evaluation accuracy. On the observer side, reliability may be affected by experience, training, and techniques of measurement employed. Many efforts were made to make clinical assessment more objective: goniometry,2,12 -14 drawing lines on the skin, 22 and developing measurement devices.17,22 However, estimations remain essentially subjective, and the observer’s bias is still present because of individual practitioner dexterity, skin movement when the marker is applied, and even the thickness of the marker pen itself. 19 Simple bisection of the posterior surface of the calcaneus also failed to represent a central bisection of this bone. 22 Another study group examined the reliability of weight-bearing hindfoot alignment assessment as used in clinical practice; despite the fact that they obtained acceptable intraobserver reliability for clinical use, interobserver results were not reliable even between experienced examiners (Table 3). 14
Table 3.
Clinical Evaluation Methods Previously Published.
| Reference | Method | Observations |
|---|---|---|
| Ball and Johnson 2 | Electrogoniometer | Non–weight-bearing Subtalar joint movement |
| Frigg et al 12 | Goniometer Visual examination Dynamic pedobarography HAV radiography | Weight-bearing Ankle or TTC arthrodesis |
| Frigg et al 13 | Goniometer Visual examination Dynamic pedobarography HAV radiography | Weight-bearing Total ankle replacement |
| Haight et al 14 | Goniometer Visual examination | Weight-bearing Standing tibiocalcaneal angle |
| Lamm et al 17 | Goniometer Radiographs Malleolar valgus index jig Plexiglas platform with a flatbed scanner | Non–weight-bearing subtalar joint alignment Resting calcaneal stance position Malleolar valgus index |
| Robinson et al 22 | Examination platform Calliper Goniometer | Weight-bearing Drawing lines on the skin Relaxed calcaneal stance position Neutral calcaneal stance position |
Abbreviations: HAV, hindfoot alignment view; TTC, tibio talo calcaneal.
Radiographic assessment is also difficult. Currently, both the radiographic technique and measurement methods are controversial. Despite the many methods that were proposed,5,7,11 we chose to perform the LAV, a modified radiographic technique, which was developed to allow placement of the hindfoot axis in relation to the tibia. 21 When comparing it with the hindfoot alignment view (HAV),6,9 another modified radiograph, LAV proved to have better interobserver reliability and to be less susceptible to rotational misplacement of the foot.4,21 It is our perspective that this technique also has some practical advantages, such as not requiring the use of specific devices and the fact that technicians found it less difficult to perform.
Regarding measurement method, we agree with authors who sustain that the amount of hindfoot deformity should be expressed as an angular measurement, especially when planning for corrective treatment.15,21 The weight-bearing axis of the lower leg is routinely determined by the mid-diaphyseal axis of the tibia.21,23,26,28 But problems arise when calcaneal axis has to be defined. Methods described for this purpose are ellipsis superimposition, 15 lowest contact point, 23 bisecting lines,17,26,28 the 40% to 60% division, 21 and lateral wall of the calcaneus22,24 (Table 4). There are different anatomical factors that affect this axis measurement, for instance, calcaneal orientation on varus-valgus foot, cuboidal body shape, concavely curved medial surface, and the medial tuberosity. Instead, the lateral wall of the calcaneus is an easily identifiable flat surface of the bone22,24 and probably the most reproducible parameter.
Table 4.
Summary of Previously Presented Radiographic Evaluation Techniques.
| Reference | Radiographic Technique | Tibial Axis | Calcaneal Axis |
|---|---|---|---|
| Johnson et al 15 | Modified HAV | Not given | A series of ellipses with increasing size were printed on a transparent sheet. These ellipses were laid over the x-rays, and the ellipse that best approximated the shape of the cortical condensation of the posterior calcaneal tuberosity was used to determine the axis of the calcaneus. |
| Lamm et al 17 | AP and L weight-bearing foot radiographs, LAV and HAV | Not given | The calcaneal bisection line was obtained from the bisector of the radiographic silhouette of the calcaneus. |
| Reilingh et al 21 | HAV and LAV | The authors bisect the tibia into 2 mid-diaphyseal points 30 mm apart and extend the line distally. | 40% to 60% method: at a distance of 7 mm from the most distal part of the calcaneus, a horizontal line was drawn; the width of the calcaneus at this level was divided into a 40%:60% ratio, where the length of 40% extended from the lateral side. A second line was drawn horizontally at 20 mm from the most distal part of the calcaneus in the HAV and 30 mm in the LAV. The width of the calcaneus at this second level was bisected equally. The calcaneus axis was drawn by a line connecting the 40% mark at the first level and the bisecting mark at the second level. |
| Saltzman et al 23 | HAV | The authors bisect the tibia 10 and 15 cm above the medial tibial plafond. | The most inferior aspect of the calcaneus was identified by finding the point under the calcaneus closest to the image of a lead marker line (a line positioned perpendicular to the long axis of the foot and film plate, which represent the plane of the floor in the coronal plane). |
| Sutter et al 26 | LAV radiographs and low-dose biplanar radiographs of a phantom | Was defined by the line connecting the midpoints of 2 pairs of points on the cortex of the distal tibia. A minimum distance of 3 cm was maintained between these 2 pairs of points. | Was defined as the line connecting the midpoint between the lateral edge of the calcaneus at the level of the subtalar joint and the corner at the inferior aspect of the sustentaculum base, and the midpoint between the medial and lateral contour of the posterior calcaneal process. |
| Williamson et al 28 | HAV | The authors bisect 2 pairs of points on the tibial shaft cortex drawn 100 mm and 150 mm proximal to the tibial plafond. A line connecting the bisection marks was extended inferiorly and was defined as the tibial axis. | The authors bisect 2 transversals between 2 lines adapted to the lateral and medial osseous contours of the calcaneus. Line of the lateral osseous contour was drawn between the most lateral aspect of the lateral process on the calcaneal tuberosity and the most superior and lateral discernable aspect of the calcaneus. Line of the medial osseous contour was drawn from the most medial aspect of the medial process of the calcaneal tuberosity to the most inferomedial discernable aspect of the sustentaculum tali. The transversals were drawn with equal consecutive interior angles. |
Abbreviations: HAV, hindfoot alignment view; AP, anteroposterior; L, lateral; LAV, long axial view.
We observed, in agreement with several studies, that clinical and radiographic assessments do not correlate.3,12,13,17,22,25 In a study evaluating tibiotalocalcaneal fusion patients, the authors found that visual judgment predicted radiographic alignment in only 48% of the patients 12 ; similar results were obtained when evaluating the clinical relevance of HAV in total ankle replacement. 13
We found a weak clinical-radiographic correlation in our sample of patients, although when evaluating each method separately, they showed acceptable reproducibility. Despite the fact that we did not include it in the analysis, we detected that greater deformities were easier to be identified, and observers were better at identifying varus malalignment.
This study has some limitations. First, is the inaccuracy of performing a clinical assessment through photographs, Second, the measurement method is not validated, although there is no validated tool for this radiographic method. Finally, the evaluation was performed by only 2 observers, even though this is similar to what is used in many published articles.
In conclusion, the correlation between clinical and radiographic assessment was weak and not statistically significant for both observers in our series. We believe that this reflects the need for complementing the clinical evaluation with a standardized radiographic examination, including a reproducible technique and measurement method, to better understand the complex triplanar hindfoot alignment. Further studies comparing different measurement methods need to be performed to establish the most objective evaluation.
Footnotes
This article was originally published as: Slullitel G, Álvarez V, Lopez V, Calvi JP, Calvo AB. How accurate is clinical evaluation in hindfoot coronal alignment? Foot Ankle Orthop. 2017 Oct 17;2(4):2473011417731563. doi:10.1177/2473011417731563.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Al-Nammari S, Myerson M. The use of tibial osteotomy (ankle plafondplasty) for joint preservation of ankle deformity and early arthritis. Foot Ankle Clin. 2016;21(1):15–26. [DOI] [PubMed] [Google Scholar]
- 2. Ball P, Johnson GR. Reliability of hindfoot goniometry when using a flexible electrogoniometer. Clin Biomech. 1993;8(1):13–19. [DOI] [PubMed] [Google Scholar]
- 3. Barg A, Harris MD, Henninger HB, et al. Medial distal tibial angle: comparison between weightbearing mortise view and hindfoot alignment view. Foot Ankle Int. 2012;33(8):655–661. [DOI] [PubMed] [Google Scholar]
- 4. Buck FM, Hoffmann A, Mamisch-Saupe N, Espinosa N, Resnick D, Hodler J. Hindfoot alignment measurements: rotation-stability of measurement techniques on hindfoot alignment view and long axial view radiographs. AJR Am J Roentgenol. 2011;197(3):578–582. [DOI] [PubMed] [Google Scholar]
- 5. Buck FM, Hoffmann A, Mamisch-Saupe N, et al. Diagnostic performance of MRI measurements to assess hindfoot malalignment: an assessment of four measurement techniques. Eur Radiol. 2013;23(9):2594–25601. [DOI] [PubMed] [Google Scholar]
- 6. Buck P, Morrey BF, Chao EY. The optimum position of arthrodesis of the ankle: a gait study of the knee and ankle. J Bone Joint Surg Am. 1987;69(7):1052–1062. [PubMed] [Google Scholar]
- 7. Burssens A, Peeters J, Buedts K, Victor J, Vandeputte G. Measuring hindfoot alignment in weight bearing CT: a novel clinical relevant measurement method. Foot Ankle Surg. 2016;22(4):233–238. [DOI] [PubMed] [Google Scholar]
- 8. Carreira DS, Sandilands SM. Radiographic factors and effect of fifth metatarsal Jones and diaphyseal stress fractures on participation in the NFL. Foot Ankle Int. 2013;34(4):518–522. [DOI] [PubMed] [Google Scholar]
- 9. Cobey JC. Posterior roentgenogram of the foot. Clin Orthop Relat Res. 1976;118:202–207. [PubMed] [Google Scholar]
- 10. Cobey JC, Sella E. Standardizing methods of measuring foot shape by including the effects of subtalar rotation. Foot Ankle. 1981;2(1):230–236. [DOI] [PubMed] [Google Scholar]
- 11. Donovan A, Rosenberg ZS. Extraarticular lateral hindfoot 224 impingement with posterior tibial tendon tear: MRI correlation. AJR Am J Roentgenol. 2009;193(3):672–678. [DOI] [PubMed] [Google Scholar]
- 12. Frigg A, Nigg B, Davis E, Pederson B, Valderrabano V. Does alignment in the hindfoot radiograph influence dynamic foot-floor pressures in ankle and tibiotalocalcaneal fusion? Clin Orthop Relat Res. 2010;468(12):3362–3370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Frigg A, Nigg B, Hinz L, Valderrabano V, Russell I. Clinical relevance of hindfoot alignment view in total ankle replacement. Foot Ankle Int. 2010;31(10):871–879. [DOI] [PubMed] [Google Scholar]
- 14. Haight HJ, Dahm DL, Smith J, Krause DA. Measuring standing hindfoot alignment: reliability of goniometric and visual measurements. Arch Phys Med Rehabil. 2005;86(3):571–575. [DOI] [PubMed] [Google Scholar]
- 15. Johnson JE, Lamdan R, Granberry WF, Harris GF, Carrera GF. Hindfoot coronal alignment: a modified radiographic method. Foot Ankle Int. 1999;20(12):818–825. [DOI] [PubMed] [Google Scholar]
- 16. Kleiger B, Mankin HJ. A roentgenographic study of the development of the calcaneus by means of the posterior tangential view. J Bone Joint Surg Am. 1961;43(7):961–969. [Google Scholar]
- 17. Lamm BM, Mendicino RW, Catanzariti AR, Hillstrom HJ. Static rearfoot alignment: a comparison of clinical and radiographic measures. J Am Podiatr Med Assoc. 2005;95(1):26–33. [DOI] [PubMed] [Google Scholar]
- 18. Manoli A II, Graham B, Ped C. The subtle cavus foot, “the underpronator.”’ Foot Ankle Int. 2005;26(3):256–263. [DOI] [PubMed] [Google Scholar]
- 19. Menz HB. Clinical hindfoot measurement: a critical review of the literature. Foot. 5(2):57–64. [Google Scholar]
- 20. Norton A, Callaghan JJ, Amendola A, et al. Correlation of knee and hindfoot deformities in advanced knee OA: compensatory hindfoot alignment and where it occurs. Clin Orthop Relat Res. 2015;473(1):166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reilingh ML, Beimers L, Tuijthof GJ, Stufkens SA, Maas M, van Dijk C. Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view. Skeletal Radiol. 2010;39(11):1103–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Robinson I, Dyson R, Halson-Brown S. Reliability of clinical and radiographic measurement of rearfoot alignment in a patient population. Foot. 2001;11(1):2–9. [Google Scholar]
- 23. Saltzman CL, el-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16(9):572–576. [DOI] [PubMed] [Google Scholar]
- 24. Sensiba PR, Coffey MJ, Williams NE, Mariscalco M, Laughlin RT. Inter- and intraobserver reliability in the radiographic evaluation of adult flatfoot deformity. Foot Ankle Int. 2010;31(2):141–145. [DOI] [PubMed] [Google Scholar]
- 25. Strash W, Berardo P. Radiographic assessment of the hindfoot and ankle. Clin Podiatr Med Surg. 2004;21:295–304. [DOI] [PubMed] [Google Scholar]
- 26. Sutter R, Pfirrmann CW, Espinosa N, Buck FM. Three-dimensional hindfoot alignment measurements based on biplanar radiographs: comparison with standard radiographic measurements. Skeletal Radiol. 2013;42(4):493–498. [DOI] [PubMed] [Google Scholar]
- 27. Van Bergeyk A, Younger A, Carson B. CT analysis of hindfoot alignment in chronic lateral ankle instability. Foot Ankle Int. 2002;23(1):37–42. [DOI] [PubMed] [Google Scholar]
- 28. Williamson ER, Chan JY, Burket JC, Deland JT, Ellis SJ. New radiographic parameter assessing hindfoot alignment in stage II adult-acquired flatfoot deformity. Foot Ankle Int. 2015;36(4):417–423. [DOI] [PubMed] [Google Scholar]