Abstract
This cross-sectional study examines emergency department use among older adults with Alzheimer disease and related dementias.
Individuals with Alzheimer disease and related dementias (ADRDs) face challenges that may lead to higher reliance on emergency department (ED) care.1 Although previous studies have examined hospitalization among patients with ADRDs, less is known about ED use.1,2 To reduce potentially inappropriate ED use, a first step is to understand the characteristics of ED visits.
Methods
This cross-sectional study used data on ED visits among older adults (aged ≥65 years) from the 2016-2019 National Hospital Ambulatory Medical Care Survey (NHAMCS).3 The NHAMCS collects data from a random sample of ED visits, and trained reviewers collect data including ADRD status, race, and ethnicity from medical record review (eAppendix in Supplement 1). We examined primary reason for visit (chief complaint) as reported by the patient and/or proxy and coded according to NHAMCS; diagnoses were classified according to ICD-10-CM codes.3 Data were analyzed from May 2, 2022, to January 17, 2023. This study was deemed exempt by the Michigan Medicine Institutional Review Board. We followed the STROBE reporting guideline.
We examined diagnostic testing results and medications administered focused on central nervous system–active medications. Generalized linear models were used to adjust for differences between the groups, and the associations between ADRD status and visit characteristics were expressed as rate ratios. Complex survey design methods were used to make annual estimates by appending 2016-2019 NHAMCS data. All analyses were conducted using Stata 16 with 2-sided tests (α = .05).
Results
Among 20 359 190 annual ED visits by older adults, an estimated 1 378 940 visits were among patients with ADRDs. Among all visits, patients had a mean (SE) age of 76.5 (0.14) years; 57.3% were men, 42.7% were women, 8.0% were Hispanic, 14.6% were non-Hispanic Black, and 74.1% were non-Hispanic White. ADRD ED visits were more common among those 85 years or older, female patients, and medical comorbidity. Common reasons for ADRD visits included accidents (7.9%) and behavioral disturbances (7.4%), which were twice as likely compared with non-ADRD visits (accidents: adjusted rate ratio [ARR], 2.1 [95% CI, 1.3-3.3]; behavioral disturbances: ARR, 2.0 [95% CI, 1.3-3.2]; Figure 1). Common diagnoses among ADRD visits included dementia with or without behavioral disturbances, symptoms involving cognitive function and awareness, and urinary tract infection. After adjusting for differences, diagnostic testing, including urinalysis (43.3% ADRD vs 33.5% non-ADRD visits; P < .001) and head computed tomography (30.1% ADRD vs 17.0% non-ADRD visits; P < .001), was more common among ADRD visits (Figure 2A). Antipsychotic administration was more common among patients with ADRDs (2.8% vs 1.1%; P = .003); opioid administration was less likely among patients with ADRDs (16.5% vs 24.1%; P = .002; Figure 2B).
Figure 1. Top 10 Primary Reasons for Visit and Diagnoses Associated With Emergency Department (ED) Visits Among Older Adults Living With Alzheimer Disease and Related Dementias (ADRDs) vs Those Without ADRDs.
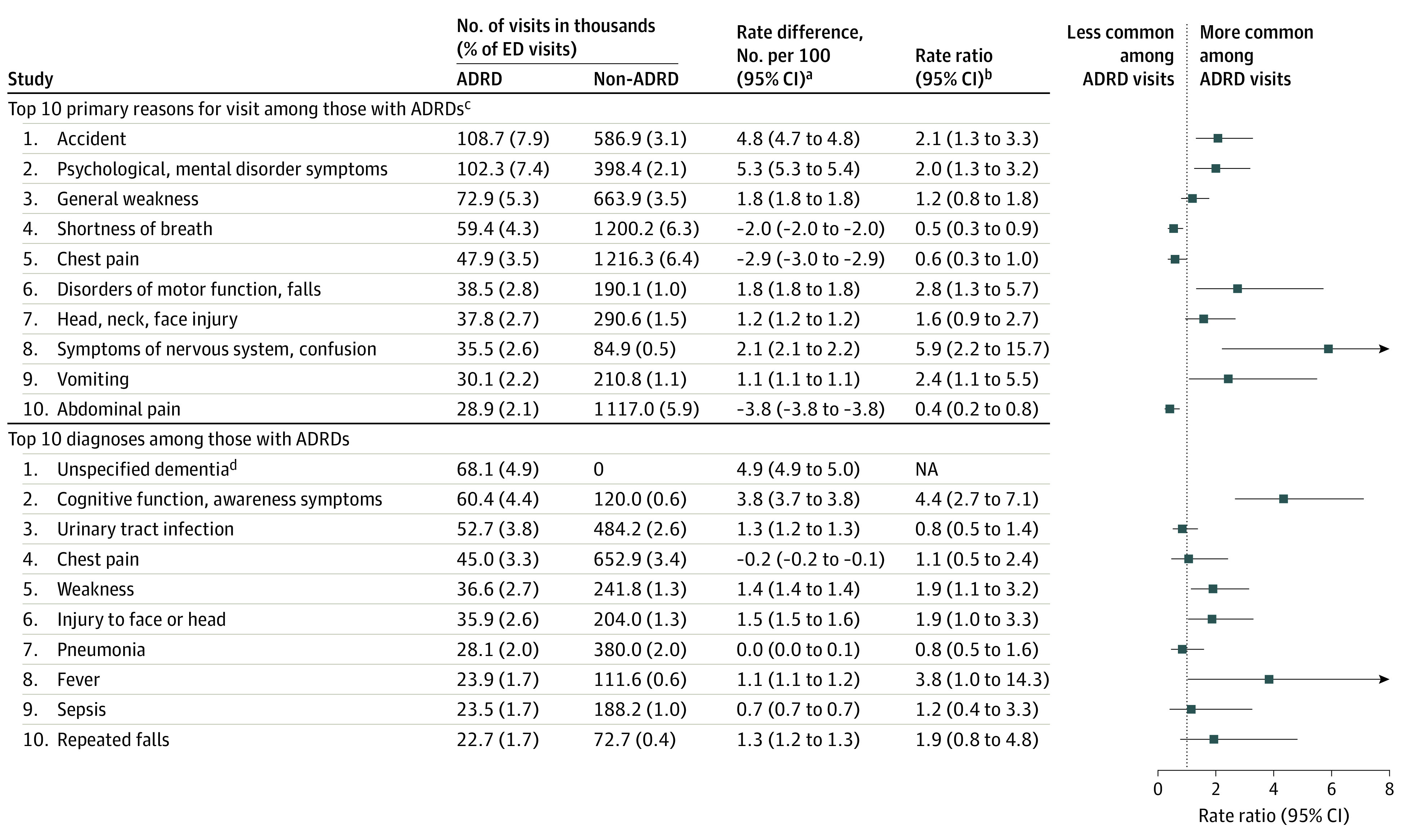
All analyses are weighted to represent the US population.
aNumber of visits among the ADRD group minus number of visits among non-ADRD group per 100 visits.
bAdjusted for age (continuous), sex, race and ethnicity, number of comorbidities (continuous), rurality, and residency type.
cPrimary reasons for visit represents the chief complaint of the patient and/or proxy coded according to the 2016-2019 National Hospital Ambulatory Medical Care Survey.
dWith or without behavioral symptoms, rate ratio omitted due to 0 outcomes in non-ADRD group.
Figure 2. Diagnostic Tests and Central Nervous System–Active Medications Associated With Emergency Department Visits for Older Adults Living With Alzheimer Disease and Related Dementias (ADRDs) vs Those Without ADRDs.
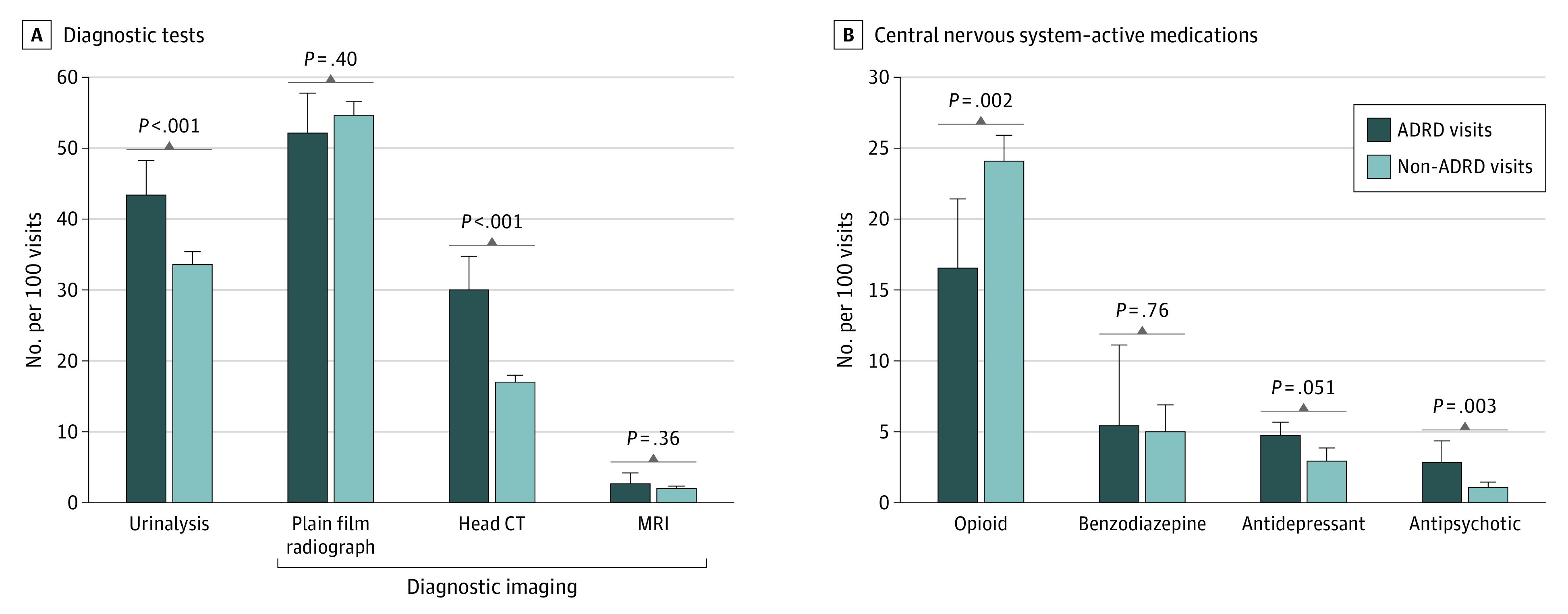
All analyses are weighted to represent the US population and adjusted for age (continuous), sex, race and ethnicity, number of comorbidities (continuous), rurality, and residency types. Whiskers represent upper bound of the 95% CI. CT indicates computed tomography; MRI, magnetic resonance imaging.
Discussion
In this national study of ED visits, nearly 1.4 million visits were made by patients with ADRDs annually. Following accidents, behavioral disturbances (eg, day-night reversal and mood fluctuations)4 were the primary reason for ADRD ED visits, which may reflect caregiver difficulty in managing behaviors. As the ED is not an optimal treatment setting for ADRD care, findings highlight the need for caregiver support services to better manage ADRD care in ambulatory settings.
We found that those with ADRD ED visits were more likely to undergo a head computed tomography scan and/or urinalysis. Difficulty in the ability of patients with ADRDs to communicate symptoms may lead to differences in diagnostic testing to rule out reversible causes or even indiscriminate testing. Given the high rates of ED visits for behavioral disturbances, it is perhaps unsurprising that those with ADRD visits were twice as likely to receive antipsychotic agents. Such use is concerning given the increased mortality risk associated with antipsychotic agents and potential for transition to long-term use.5
Among our study’s limitations, there may be misclassification of patients with ADRD who are not identified from NHAMCS medical record review. Although the ED is an important care location for an increasing number of patients with ADRDs, our findings highlight the need for better ways to evaluate and manage ADRD care in outpatient settings to reduce potentially avoidable and harmful visits.6
eAppendix. Description of the National Hospital Ambulatory Medical Care Survey (NHAMCS) Procedures
Data Sharing Statement
References
- 1.LaMantia MA, Stump TE, Messina FC, Miller DK, Callahan CM. Emergency department use among older adults with dementia. Alzheimer Dis Assoc Disord. 2016;30(1):35-40. doi: 10.1097/WAD.0000000000000118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bynum JP, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, Medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187-194. doi: 10.1111/j.1532-5415.2004.52054.x [DOI] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics, Center for Disease Control and Prevention . National Ambulatory Medical Care Survey: ambulatory health care data. Accessed January 23, 2023. https://www.cdc.gov/nchs/ahcd/index.htm
- 4.Lyketsos CG, Steinberg M, Tschanz JT, Norton MC, Steffens DC, Breitner JC. Mental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in Aging. Am J Psychiatry. 2000;157(5):708-714. doi: 10.1176/appi.ajp.157.5.708 [DOI] [PubMed] [Google Scholar]
- 5.Maust DT, Kim HM, Seyfried LS, et al. Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiatry. 2015;72(5):438-445. doi: 10.1001/jamapsychiatry.2014.3018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kales HC, Gitlin LN, Lyketsos CG; Detroit Expert Panel on Assessment and Management of Neuropsychiatric Symptoms of Dementia . Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. J Am Geriatr Soc. 2014;62(4):762-769. doi: 10.1111/jgs.12730 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Description of the National Hospital Ambulatory Medical Care Survey (NHAMCS) Procedures
Data Sharing Statement


