This case series describes clinical, socioeconomic, and occupational characteristics of patients diagnosed with silicosis associated with occupational exposure to engineered stone in California.
Key Points
Question
What are the characteristics of patients in California with silicosis from occupational exposure to dust from engineered stone (quartz), a popular material that is high in silica content and that is used to fabricate countertops?
Findings
In this case series of 52 patients, the median age was 45 years at diagnosis, and nearly all were Latino immigrant men. Diagnosis was delayed in 58%, with 38% presenting with advanced disease (progressive massive fibrosis), and 19% died.
Meaning
In California, silicosis associated with occupational exposure to dust from engineered stone primarily occurred among young Latino immigrant men; many patients presented with severe disease, and some cases were fatal.
Abstract
Importance
Silicosis associated with inhalation of respirable crystalline silica among engineered stone countertop fabrication workers is an emerging health concern.
Objective
To describe clinical, socioeconomic, and occupational characteristics of patients diagnosed with silicosis associated with engineered stone in California.
Design, Setting, and Participants
This case series included reported cases of silicosis associated with fabrication of engineered stone countertops, as identified by statewide surveillance by the California Department of Public Health (2019-2022). Data analysis was performed from October 2022 to March 2023.
Exposures
Patient interviews and medical record abstractions were used to assess occupational exposure to respirable crystalline silica, including duration of work tenure and preventive measures undertaken.
Main Outcomes and Measures
Demographics, clinical characteristics, health care utilization, and clinical outcomes were obtained, including vital status, hypoxia, and lung transplant.
Results
This case series identified 52 male patients meeting inclusion criteria; median (IQR) age was 45 (40-49) years, and 51 were Latino immigrants. Ten (19%) were uninsured, and 20 (39%) had restricted-scope Medi-Cal; 25 (48%) presented initially to an emergency department. A delay in diagnosis occurred in 30 (58%) patients, most commonly due to alternative initial diagnoses of bacterial pneumonia (9 [30%]) or tuberculosis (8 [27%]). At diagnosis, 20 (38%) patients had advanced disease (progressive massive fibrosis) with severely or very severely reduced forced expiratory volume in 1 second in 8 (18%) and 5 (11%), respectively. Of the cases, 10 (19%) were fatal; median (IQR) age at death was 46 (38-51) years, and 6 patients (12%) were alive with chronic resting hypoxia. Eleven were referred for lung transplant: 3 underwent transplant with 1 fatality; 7 were declined transplant, with 6 fatalities; and 1 died prior to listing. Median (IQR) work tenure was 15 (10-20) years; 23 (45%) reported use of water suppression for dust mitigation, and 25 (48%) continued to fabricate stone after being diagnosed with silicosis.
Conclusions and Relevance
In this case series performed in California, silicosis associated with occupational exposure to dust from engineered stone primarily occurred among young Latino immigrant men. Many patients presented with severe disease, and some cases were fatal.
Introduction
Silicosis is the most prevalent pneumoconiosis worldwide. It is a fibrotic interstitial lung disease resulting from the occupational inhalation of respirable crystalline silica over decades. With exposure to higher dust levels, the disease can also occur in acute and accelerated forms over shorter periods of time.1,2 Initially, patients are often asymptomatic. Subsequently, they may develop worsening respiratory symptoms and end-stage lung disease. As there are no effective treatments, silicosis may lead to premature death or lung transplant. Although deaths from silicosis have declined in the US,3,4 workers in certain industries continue to be exposed to silica dust.1,2
Recently, reported clusters of silicosis among engineered stone countertop workers in countries other than the US have called attention to an accelerated and rapidly fatal form of silicosis.5,6,7,8 Engineered (artificial, synthetic, or quartz conglomerate) stone is manufactured in large facilities via mechanical crushing of quartz with polymer resins, dyes, and glass at high heat to produce a damage-resistant alternative to marble or granite kitchen countertops. In contrast to natural stone products, engineered stone contains more than 3 times the silica content (90% vs 3%-30%).9,10 Driven by new construction, consumer taste, and imported slabs of engineered stone that are less expensive than other countertop materials, demand has increased 23% annually over the past decade.11 At present, engineered stone is the most popular countertop material in the US,12 with a global market value of more than $20 billion in 2020.13 Manufacturers deliver slabs to shops where fabricators cut, sand, and polish the material and generate levels of crystalline silica dust that may be hazardous. Fabrication is frequently performed in shops where ventilation, dust control methods, and personal protective equipment are inadequate.14,15
Despite a comprehensive Occupational Safety and Health Administration standard for exposure to silica dust,16 there are concerns about exposure and disease burden among people who work with engineered stone. During workplace inspections by California’s Division of Occupational Safety and Health, air sampling found levels above the permissible exposure limit of 50 µg/m3 among 25% of employees and 51% of workplaces.14 Water suppression can reduce crystalline silica dust exposure by 10-fold17 but is often insufficient to reduce exposure below the permissible exposure limit without local exhaust ventilation and appropriate personal protective equipment.17,18 In Queensland, Australia, a comprehensive government screening program found a silicosis prevalence of 19.5% among 1053 workers who were screened.19 An estimated 100 000 stone fabricators in the US are at potential risk for silicosis associated with exposure to respirable crystalline silica.20
In the US, a case of silicosis associated with engineered stone was reported in Texas in 2015,21 followed by 18 cases from 4 states in 2019 (6 from California).22 In California, a sentinel (fatal) case led to discovery of 2 others in the same workplace, which prompted workplace screening enforcement and identification of 5 additional cases (3 reported in 2019 and 2 discovered subsequently). The present case series, which includes the 8 California cases that were previously reported,23 aims to describe silicosis associated with engineered stone in California workers through 2022, focusing on clinical presentation.
Methods
Case Identification
We identified cases from 2019 to 2022 through multiple methods: statewide hospital-based patient discharge data (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision code for silicosis [J62.X] from 2006 to 2021; if age younger than 50 years, requested and reviewed medical records for engineered stone exposure); direct reporting by physicians or community members to the California Department of Public Health Occupational Health Branch; and public health follow-up of mandated medical testing following worksite investigations. We defined silicosis based on the definition of Occupational Respiratory Disease Surveillance from the National Institute for Occupational Safety and Health (NIOSH): history of occupational exposure to airborne silica and either imaging or pathological findings characteristic of silicosis.24 We only included participants with a primary occupation of stone countertop fabricator and who regularly worked with engineered stone. The institutional review boards at the California Department of Public Health and the Olive View-UCLA Medical Center Education and Research Institute approved the study. Informed consent was waived owing to use of deidentified data.
Medical Record Abstraction
We abstracted medical records and called patients or next of kin to obtain further medical and occupational information if necessary. Demographic data included date of birth, sex, race and ethnicity, and birthplace and year immigrated to the US. Self-reported occupational history included number of years worked in stone fabrication (work tenure), current employment status, and employer. To assess respirator use, we asked, “How often do/did you wear a respirator”: never, sometimes, or always. Type of respirator was not mutually exclusive and was recorded as any use of N-95, half-face respirator with filters, or full-face respirator with filters. This information was not easily standardized due to inconsistent interviews and use of electronic medical record data. We obtained information about whether workers regularly used water suppression for dust mitigation and recorded it as a binary outcome (yes/no). Workshop size was designated as small, medium, or large if less than 10, 10 to 50, or greater than 50 workers, respectively.
Dates of initial presentation, diagnosis, and death were collected to the month. Symptoms at presentation recorded were shortness of breath, cough, wheezing, fever, weight loss, and chest/back pain. Additionally, we recorded if a patient had ever had a pneumothorax. Delayed diagnosis was defined as a case where an alternative initial diagnosis for abnormal chest imaging and/or symptoms was assigned prior to documentation of a presumed or confirmed diagnosis of silicosis. Time to diagnosis of silicosis was quantified by subtracting presentation date from date of diagnosis. Smoking status was defined as greater than 20 packs of cigarettes over a lifetime expressed in pack-years. We recorded comorbidities, specifically autoimmune and pulmonary diseases. We coded computed tomography imaging findings closest to time of diagnosis as simple silicosis (small nodular areas of fibrosis) or progressive massive fibrosis (coalescent fibrotic masses greater than 1 cm). We recorded lung transplant referrals, if any, and whether the patient was declined, underwent transplant, or died prior to listing. We obtained outcomes: death due to silicosis (time from diagnosis to death in months, and age at death) and alive with or without hypoxia, determined by need for long-term supplemental oxygen.
We analyzed the pulmonary function test (PFT) results closest to time of diagnosis based on American Thoracic Society and European Respiratory Society criteria.25 We defined obstruction as the ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) below the lower limit of normal, and restriction as the total lung capacity below the lower limit of normal. If total lung capacity was unavailable, we used FVC as a proxy. Severity of limitation was graded using FEV1. Air trapping was defined as abnormal spirometry with total lung capacity above the upper limit of normal. We defined diffusion impairment as reduced diffusing capacity of lung for carbon monoxide (DLCO) lower than the lower limit of normal and graded based on American Thoracic Society and European Respiratory Society guidelines.25 We calculated the predicted values for spirometry using the global lung initiative other race equations and global lung initiative equations for lung volumes and DLCO.26 Lung biopsy data included biopsy or explant done (yes/no), biopsy type, and presence/absence of pathologic characteristics known to be consistent with silicosis.27
We recorded health insurance as none/self-pay, full-scope Medi-Cal (California’s Medicaid program), restricted Medi-Cal, private insurance, workers’ compensation, or Medicare. California has incrementally increased access to full-scope Medi-Cal for the oldest (age >50 years [2020]) and youngest (age <26 years [2022]) undocumented immigrants.28 As those aged 26 to 49 years only qualify for restricted Medi-Cal benefits, we used restricted-scope Medi-Cal or uninsured as a proxy for undocumented immigration status.29 Full-scope Medi-Cal provides medical, dental, and vision insurance to eligible low-income California residents, while restricted Medi-Cal limits coverage to emergency and pregnancy-related care for low-income individuals with undocumented immigration status.30 We obtained health care utilization data: location of initial presentation (urgent care/clinic or emergency department), if and how many emergency department visits or hospitalizations due to respiratory symptoms, and cumulative hospital length of stay, if applicable.
Statistical Analysis
We calculated standard descriptive statistics for categorical data (counts and percentage) and continuous data (median and IQR) using R Studio, version 4.0.2 (R Foundation for Statistical Computing).31 This study followed the reporting guideline for case series.
Results
Case Demographics
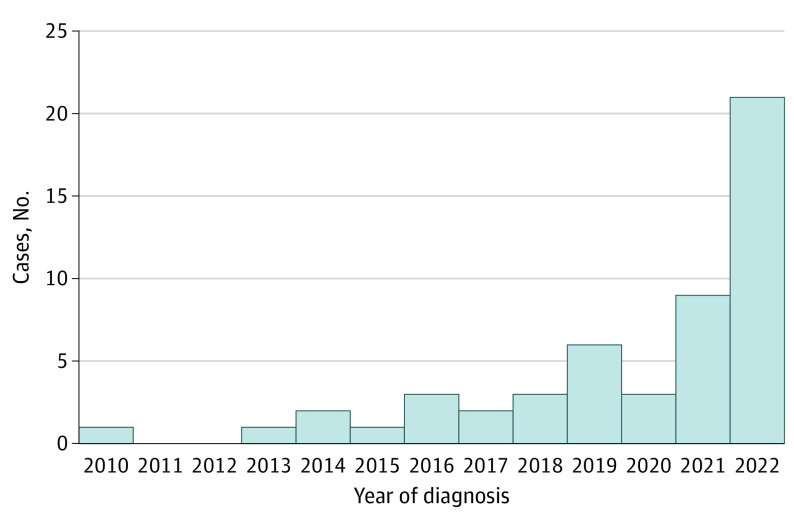
Between 2019 and 2022, we identified 52 patients in California with silicosis associated with engineered stone. Diagnosis dates ranged from 2010 to 2022; most of the diagnoses were in 2019 or later (Figure 1). Seven cases were identified from hospital discharge data, 37 from direct reporting, and 8 through workplace medical testing and public health follow-up. Thirty-seven cases (71%) were identified in Los Angeles County, 30 of whom sought care at Olive View-UCLA Medical Center, one of the county’s 3 safety net hospitals. Cases were reported in an additional 9 counties and represented 22 unique workplaces among 35 participants with known employment location. The median (IQR) age at diagnosis was 45 (40-49) years; all but 1 patient were Spanish-speaking Latino immigrant men from Mexico (32 [62%]), El Salvador (14 [27%]), and elsewhere in Central America (5 [10%]) (Table 1), with median (IQR) time from immigration to diagnosis of 18 (15-22) years.
Figure 1. Yearly Case Counts for 52 Patients With Engineered Stone–Associated Silicosis in California, 2010-2022.
There were no reported cases of silicosis associated with engineered stone in California prior to 2010.
Table 1. Demographic Characteristics and Self-Reported Occupational History of 52 Patients From California With Engineered Stone–Associated Silicosis.
| Demographic or occupational characteristic (No. with data available) | Overall (n = 52), No. (%) |
|---|---|
| Demographic characteristics | |
| Age at diagnosis (52), median (IQR), y | 45 (40-49) |
| Male sex (52) | 52 (100) |
| Race and ethnicity (52) | |
| Latino | 51 (98) |
| Othera | 1 (2) |
| Country of birth (52) | |
| Mexico | 32 (62) |
| El Salvador | 14 (27) |
| Central America, other | 5 (10) |
| Othera | 1 (2) |
| Occupational history | |
| Years of work in engineered stone industry (51), median (IQR) | 15 (10-20) |
| Continued working after diagnosis (52) | |
| Still working | 25 (48) |
| Not working | 18 (35) |
| Unknown | 9 (18) |
| Engineering controls: water suppression methods (51) | 23 (45) |
| Respirator use (47) | |
| Sometimes | 35 (74) |
| Always | 12 (26) |
| Type of respirator (37) | |
| N-95 | 33 (89) |
| Half-face respirator | 17 (46) |
| Full-face respirator | 2 (5) |
| No. of employees in workshop (35) | |
| <10 | 17 (49) |
| 10-50 | 17 (49) |
| >50 | 1 (2) |
Further detail on the “Other” category cannot be disclosed due to small cell size and protection of privacy.
Occupational Exposure History
Median (IQR) work tenure was 15 (10-20) years, with 25 (48%) patients continuing to fabricate stone after diagnosis at the time the occupational history was obtained (Table 1). Water suppression for silica dust control was reported among 45% (23 of 51). Of 47 patients with available data, respiratory personal protective equipment was used “always” by 12 (26%) or “sometimes” by 35 (74%), with none indicating “never” (Table 1). Workshop size was reported as small, medium, or large among 49% (17 of 35), 49% (17 of 35), or 2% (1 of 35), respectively.
Clinical Findings and Health Care Utilization
Forty-five patients (87%) reported at least 1 initial presenting symptom (all with shortness of breath) (Table 2), which led to chest imaging. Median (IQR) time to diagnosis was 3 (0-8) months. A delay in diagnosis occurred in 30 patients (58%), among whom the alternative initial diagnosis was most commonly bacterial pneumonia (9 [30%]), active pulmonary tuberculosis (8 [27%]), and nontuberculous mycobacterial infection (3 [10%]). Of 5 patients with comorbid nontuberculous mycobacterial infection and silicosis, the diagnosis of silicosis was delayed in the 3 patients where the mycobacterial infection was diagnosed first. Of the 8 patients with initial presumed active pulmonary tuberculosis, only 1 was confirmed to have tuberculosis.
Table 2. Clinical Characteristics and Outcomes of Patients With Engineered Stone–Associated Silicosis.
| Clinical characteristic (No. with data available) | Overall (n = 52), No. (%) |
|---|---|
| Presenting symptoms (52) | |
| Asymptomatic | 7 (13) |
| Shortness of breath | 45 (87) |
| Cough | 38 (73) |
| Chest/back pain | 25 (48) |
| Weight loss | 18 (35) |
| Fevers | 10 (19) |
| Wheezing | 8 (15) |
| Pneumothorax | 5 (10) |
| Delayed diagnosis (52) | |
| Initial delay in diagnosis | 30 (58) |
| Time to correct diagnosis, median (IQR), mo | 3 (0-8) |
| Alternative initial diagnosis (30) | |
| Pulmonary tuberculosis | 8 (27) |
| Nontuberculous mycobacterial infection | 3 (10) |
| Sarcoidosis | 2 (7) |
| Asthma | 2 (7) |
| Bacterial pneumonia | 9 (30) |
| Other | 6 (20) |
| Tobacco use (52) | |
| Current or former smoker | 18 (36) |
| Pack-years among tobacco users, median (IQR) | 3.5 (1.25-6) |
| Comorbidities (52) | |
| Autoimmune disease | 6 (12) |
| Myositis | 1 (2) |
| Rheumatoid arthritis | 4 (8) |
| Systemic sclerosis or CREST syndrome | 1 (2) |
| Nontuberculous mycobacterial infection | 5 (10) |
| History of active pulmonary TB | 1 (2) |
| Other lung disease (COPD/asthma) | 2 (4) |
| Imaging (52) | |
| Predominant CT pattern | |
| Simple silicosis | 32 (62) |
| Progressive massive fibrosis | 20 (38) |
| Lung zone distribution | |
| Upper | 34 (65) |
| Lower | 5 (10) |
| Diffuse | 13 (25) |
| Lymphadenopathy (52) | |
| None | 6 (12) |
| Hilar only | 4 (8) |
| Mediastinal only | 12 (23) |
| Hilar and mediastinal | 30 (58) |
| Calcified lymphadenopathy (52) | 17 (33) |
| Ground glass opacities (51) | 19 (37) |
| Bronchiectasis (52) | 6 (12) |
| Cavitary lesions (51) | 5 (10) |
| Pleural effusion (52) | 6 (13) |
| Pleural thickening (52) | 4 (8) |
| Emphysema (52) | 2 (4) |
| Cardiomegaly (50) | 3 (6) |
| PFTs (44) | |
| PFT pattern (44) | |
| Normal | 13 (30) |
| Restriction | 24 (55) |
| Mixed | 6 (14) |
| Obstruction | 1 (2) |
| Severity of FEV1 reduction (44) | |
| Normal | 13 (20) |
| Mild | 9 (23) |
| Moderate | 8 (18) |
| Moderate-severe | 1 (2) |
| Severe | 8 (18) |
| Very severe | 5 (11) |
| Severity of DLCO reduction (43) | |
| Normal | 23 (54) |
| Mild | 5 (12) |
| Moderate | 11 (26) |
| Severe | 4 (9) |
| Air trapping (30) | 11 (37) |
| Lung biopsy (34) | |
| Bronchoscopic | |
| Transbronchial | 29 (85) |
| Lymph node | 16 (47) |
| Surgical (video assisted) | 5 (15) |
| Percutaneous needle | 2 (6) |
| Lung explant | 1 (3) |
| Pathologic features | |
| Characteristic findings of silicosis | 26 (76) |
| Birefringent crystals | 19 (58) |
| Granulomas | 14 (41) |
| Dust particles | 15 (46) |
| Fibrotic nodules | 12 (36) |
| Pulmonary alveolar proteinosis | 3 (9) |
| Outcomes (52) | |
| Deceased due to silicosis | 10 (19) |
| Time from diagnosis to death, median (IQR), mo (9) | 35 (19-52) |
| Age at death, median (IQR), years (9) | 46 (38-51) |
| Alive with hypoxia | 6 (12) |
| Alive without hypoxia | 35 (67) |
| Referred for lung transplant | 11 (21) |
| Formally declined | 7 (13) |
| Underwent transplant | 3 (6) |
Abbreviations: COPD, chronic obstructive pulmonary disease; CREST, calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia; CT, computed tomography; FEV1, forced expiratory volume in 1 second; DLCO, diffusion capacity of the lung for carbon monoxide; PFT, pulmonary function test; TB, tuberculosis.
Chest computed tomography imaging demonstrated progressive massive fibrosis in 20 (38%) patients and simple silicosis in 32 (62%) patients; representative cross-sectional imaging is shown in Figure 2, and detailed imaging characteristics are presented in Table 2. Among 44 patients with available PFT results, 13 (30%) were normal, 24 (55%) restrictive (2 based on FVC alone), 6 (14%) were mixed, and 1 (2%) was obstructive. In those with abnormal PFT results, air trapping was observed in 11 (37%) patients. Results for DLCO were normal in 23 (54%) but reduced mildly in 5 (12%), moderately in 11 (26%), and severely in 4 (9%).
Figure 2. Representative Chest Imaging From 2 Patients With Engineered Stone–Associated Silicosis in Different Stages of Disease.

Noncontrast computed tomography chest images demonstrate a case of early simple silicosis with scattered micronodules (A and B) and a case of complicated silicosis with progressive massive fibrosis, indicative of advanced disease (C and D).
Of the patients, 34 had a lung biopsy; 26 (77%) biopsy results were consistent with a diagnosis of silicosis. Eight (24%) patients were without characteristic findings of silicosis but diagnosed based on clinical and imaging findings after alternative diagnoses were excluded (Table 2). Rheumatologic disease was seen in 6 (12%) patients: rheumatoid arthritis in 4 (8%), and 1 case each had scleroderma and myositis. Concurrent infection with nontuberculous mycobacterial infection was present in 5 (10%) patients, 4 with Mycobacterium kansasii. Autoimmune serologies were collected with a positive result for antinuclear antibody in 11 of 19 (58%) patients and rheumatoid factor in 4 of 16 (25%) patients. As of June 2023, at least 10 (19%) had died due to silicosis: among 9 with available data, median (IQR) time from diagnosis to death was 35 (19-52) months, and median (IQR) age at death was 46 (38-51) years. Six (12%) were alive with resting hypoxia, 1 posttransplant. Thirty-five (67%) remained alive without hypoxia. Additionally, 11 patients were referred for lung transplant; 1 died before listing, 7 were formally declined (6 deceased as of May 2023), and 3 underwent transplant.
Of the cases, 25 (48%) initially presented to the emergency department, and 19 (37%) presented to a primary or urgent care clinician (Table 3). Ten patients (19%) were uninsured, 20 (38%) had restricted-scope Medi-Cal, 7 (13%) had Medi-Cal, 8 (15%) had private insurance, and 7 (13%) had workers’ compensation. None had Medicare. Of 51 patients with available health care utilization data, 42 (82%) had 1 or more respiratory-related emergency department visits, with a median (IQR) of 2.5 (1-4) visits. Hospitalization for respiratory symptoms occurred among 31 (61%) patients with median (IQR) cumulative length of stay of 9.5 (4.3-19.8) days.
Table 3. Health Care Utilization of Patients With Engineered Stone–Associated Silicosis.
| Health care utilization characteristic (No. with data available) | Overall (n = 52), No. (%) |
|---|---|
| Health insurance (52) | |
| Uninsured or self-pay | 10 (19) |
| Restricted-scope Medi-Cal | 20 (38) |
| Full-scope Medi-Cal | 7 (13) |
| Private insurance | 8 (15) |
| Medicare | 0 (0) |
| Workers’ compensation | 7 (13) |
| Location of initial presentation (52) | |
| Emergency department | 25 (48) |
| Outpatient clinic | 19 (37) |
| Medical surveillance | 8 (15) |
| Emergency department (52) | |
| Ever visited emergency department (52) | 42 (82) |
| No. of emergency department visits (42), median (IQR) | 2.50 (1.00-4) |
| Hospitalization (51) | |
| Ever hospitalized for breathing | 31 (61) |
| No. of times hospitalized (31), median (IQR) | 2.0 (1-3.5) |
| Cumulative hospital length of stay per patient (30), median (IQR), d | 9.5 (4.3-19.8) |
Discussion
The case series of 52 patients from California confirms clinical findings of silicosis in engineered stone countertop fabrication workers that are similar to the clinical findings identified in other countries in recent years.5,6,7 Silicosis was diagnosed in men in their mid-40s with an average work tenure of 15 years. Patients typically had delays in diagnosis and presented after symptoms developed, with abnormal PFT results and progressive massive fibrosis.32
To diagnose silicosis, a detailed occupational history should be obtained in the patient’s native language, specifically asking about work in stone countertop fabrication and explicitly asking about work with engineered stone. Duration of exposure should be assessed in terms of years worked and hours per week, type of work done (eg, cutting large slabs, which is more readily done with wet cutting, vs fabrication, which involves grinding and shaping edges and is more often done dry, thus posing increased risk), engineering controls used (ie, wet cutting methods), and type and regularity of respirator used and whether the respirator was fit-tested.33 Imaging and history alone are sufficient for diagnosis24; however, if the diagnosis is uncertain, pulmonary consultation and bronchoscopic lung biopsy may be warranted.34 Management includes serial monitoring with PFTs and imaging and evaluation for signs and symptoms of associated conditions, including rheumatologic disease and mycobacterial infections.35 Clinicians should report cases to the local state or federal Occupational Safety and Health Administration office,36 notify their state health department occupational health program,37 and provide patient resources from the California Department of Public Health or other agencies.38
Our findings highlight the importance of timely access to care for early diagnosis. The mainstay of managing patients with silicosis is minimizing further exposure. This can be challenging, as inadequate dust suppression and poor compliance with respiratory protection regulations are common in this industry.14,15 The NIOSH hierarchy of controls for worker safety prioritizes the elimination of hazardous exposure, followed by use of engineering controls; personal protective equipment is least effective.39 In this case series, 48% of workers continued working in the industry after diagnosis, posing a risk of ongoing silica exposure. Less than half reported working in shops regularly using water suppression; respiratory protection was inconsistently used.
Limitations
This study has limitations. First, as we describe cases identified through clinician reporting, the findings may not be generalizable to all cases of silicosis associated with engineered stone in California. Second, the mean time to diagnosis of 3 months should be interpreted cautiously, as over half of the cases were identified at Olive View-UCLA Medical Center, where heightened clinician awareness led to earlier diagnosis. Third, self-report of occupational data may have resulted in recall bias. Fourth, cross-sectional health utilization data provide only a limited snapshot and may underestimate services used throughout a patient’s lifetime. Fifth, although many of the patients in the case series may have been working as independent contractors, data on employment status were not formally collected. Sixth, although a substantial number of the patients, including some of those who were uninsured or with restricted-scope Medi-Cal, likely had an undocumented immigration status, we did not directly collect information about whether individuals were undocumented immigrants. Finally, some patients may have received more medical care than we were able to document, resulting in an underestimate of health care utilization.
Conclusions
In this case series from California, silicosis associated with occupational exposure to dust from engineered stone primarily occurred among young Latino immigrant men. Many presented with severe disease, and some cases were fatal. The findings highlight the urgent need for clinicians and public health officials to fully address the emerging issue of silicosis among engineered stone countertop fabrication workers through measures such as protecting workers from exposure to silica dust in the workplace, timely diagnosis of disease, provision of needed medical care, and medical surveillance programs.
Data Sharing Statement
References
- 1.Leung CC, Yu ITS, Chen W. Silicosis. Lancet. 2012;379(9830):2008-2018. doi: 10.1016/S0140-6736(12)60235-9 [DOI] [PubMed] [Google Scholar]
- 2.Barnes H, Goh NSL, Leong TL, Hoy R. Silica-associated lung disease: an old-world exposure in modern industries. Respirology. 2019;24(12):1165-1175. doi: 10.1111/resp.13695 [DOI] [PubMed] [Google Scholar]
- 3.Silicosis mortality, prevention, and control—United States, 1968–2002. Accessed April 27, 2023. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5416a2.htm [PubMed]
- 4.Harris K. Forty years of falling manufacturing employment: beyond the numbers. US Bureau of Labor Statistics. Accessed April 27, 2023. https://www.bls.gov/opub/btn/volume-9/forty-years-of-falling-manufacturing-employment.htm
- 5.Kramer MR, Blanc PD, Fireman E, et al. Artificial stone silicosis [corrected]: disease resurgence among artificial stone workers. Chest. 2012;142(2):419-424. doi: 10.1378/chest.11-1321 [DOI] [PubMed] [Google Scholar]
- 6.Hoy RF, Baird T, Hammerschlag G, et al. Artificial stone-associated silicosis: a rapidly emerging occupational lung disease. Occup Environ Med. 2018;75(1):3-5. doi: 10.1136/oemed-2017-104428 [DOI] [PubMed] [Google Scholar]
- 7.Leso V, Fontana L, Romano R, Gervetti P, Iavicoli I. Artificial stone associated silicosis: a systematic review. Int J Environ Res Public Health. 2019;16(4):568. doi: 10.3390/ijerph16040568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu N, Xue C, Yu S, Ye Q. Artificial stone-associated silicosis in China: a prospective comparison with natural stone-associated silicosis. Respirology. 2020;25(5):518-524. doi: 10.1111/resp.13744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DuPont . Material safety data sheet: Zodiaq quartz surfaces. Accessed December 11, 2022. https://www.parliament.nsw.gov.au/lcdocs/other/12562/Tabled%20Document%20-%20Du%20Pont%20Material%20Safety%20Data%20Sheet%20-%20regarding%20Zodiaq%20Quartz%20Surfaces.pdf
- 10.Simcox NJ, Lofgren D, Leons J, Camp J. Silica exposure during granite countertop fabrication. Appl Occup Environ Hyg. 1999;14(9):577-582. doi: 10.1080/104732299302350 [DOI] [PubMed] [Google Scholar]
- 11.Freedonia Group . Engineered stone countertops: market size, market share, market leaders, demand forecast, sales, co profiles, market research, industry trends and companies. Accessed April 27, 2023. https://www.freedoniagroup.com/industry-study/engineered-stone-countertops-4395.htm
- 12.Research and Markets . US countertops market 2022-2026. Accessed May 17, 2023. https://www.researchandmarkets.com/reports/4995479/us-countertops-market-2022-2026
- 13.Grand View Research . Engineered stone market size report, 2021-2028. Accessed April 27, 2023. https://www.grandviewresearch.com/industry-analysis/engineered-stone-market
- 14.Surasi K, Ballen B, Weinberg JL, et al. Elevated exposures to respirable crystalline silica among engineered stone fabrication workers in California, January 2019-February 2020. Am J Ind Med. 2022;65(9):701-707. doi: 10.1002/ajim.23416 [DOI] [PubMed] [Google Scholar]
- 15.Spiegel A, Cummings KJ, Flattery J, Harrison R, Heinzerling A. Self-reported silica exposures and workplace protections among engineered stone fabrication workers in California. Am J Ind Med. 2022;65(12):1022-1024. doi: 10.1002/ajim.23432 [DOI] [PubMed] [Google Scholar]
- 16.Occupational Safety and Health Administration (OSHA), Department of Labor . Occupational exposure to respirable crystalline silica: final rule. Fed Regist. 2016;81(58):16285-16890. [PubMed] [Google Scholar]
- 17.Cooper JH, Johnson DL, Phillips ML. Respirable silica dust suppression during artificial stone countertop cutting. Ann Occup Hyg. 2015;59(1):122-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson DL, Phillips ML, Qi C, Van AT, Hawley DA. Experimental evaluation of respirable dust and crystalline silica controls during simulated performance of stone countertop fabrication tasks with powered hand tools. Ann Work Expo Health. 2017;61(6):711-723. doi: 10.1093/annweh/wxx040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silicosis. WorkSafe.qld.gov.au. Published September 11, 2020. Accessed December 10, 2022. https://www.worksafe.qld.gov.au/claims-and-insurance/work-related-injuries/types-of-injury-or-illness/work-related-respiratory-diseases/silicosis
- 20.Wise R. QCEW industry codes and titles (for NAICS coded data). US Bureau of Labor Statistics. Accessed December 11, 2022. https://www.bls.gov/cew/classifications/industry/industry-titles.htm
- 21.Friedman GK, Harrison R, Bojes H, Worthington K, Filios M; Centers for Disease Control and Prevention (CDC) . Notes from the field: silicosis in a countertop fabricator - Texas, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(5):129-130. [PMC free article] [PubMed] [Google Scholar]
- 22.Rose C, Heinzerling A, Patel K, et al. Severe silicosis in engineered stone fabrication workers - California, Colorado, Texas, and Washington, 2017-2019. MMWR Morb Mortal Wkly Rep. 2019;68(38):813-818. doi: 10.15585/mmwr.mm6838a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heinzerling A, Cummings KJ, Flattery J, Weinberg JL, Materna B, Harrison R. Radiographic screening reveals high burden of silicosis among workers at an engineered stone countertop fabrication facility in California. Am J Respir Crit Care Med. 2021;203(6):764-766. doi: 10.1164/rccm.202008-3297LE [DOI] [PubMed] [Google Scholar]
- 24.ORDS: silicosis state reporting guidelines. Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. Published August 2, 2021. Accessed December 6, 2022. https://www.cdc.gov/niosh/topics/surveillance/ords/statesurveillance/reportingguidelines-silicosis.html
- 25.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948-968. doi: 10.1183/09031936.05.00035205 [DOI] [PubMed] [Google Scholar]
- 26.Cooper BG, Stocks J, Hall GL, et al. The Global Lung Function Initiative (GLI) Network: bringing the world’s respiratory reference values together. Breathe (Sheff). 2017;13(3):e56-e64. doi: 10.1183/20734735.012717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gibbs A, Wagner J. Diseases due to silica. In: Churg A, Green FHY, eds. Pathology of Occupational Lung Disease. 2nd ed. Williams & Wilkins; 1998:209-234. [Google Scholar]
- 28.What is the difference between full scope and restricted scope benefits? Marin Health and Human Services. Accessed January 31, 2023. https://www.marinhhs.org/faq/what-difference-between-full-scope-restricted-scope-benefits
- 29.Ro A, Yang HW, Du S, Hanlon CL, Young AS. Severity of inpatient hospitalizations among undocumented immigrants and Medi-Cal patients in a Los Angeles, California, hospital: 2019. Am J Public Health. 2021;111(11):2019-2026. doi: 10.2105/AJPH.2021.306485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Immigrant access to Medi-Cal. Mental Health Advocacy Services. Published December 2014. Accessed May 25, 2023. https://www.mhas-la.org/medi-cal-benefits/immigrant-access-to-medi-cal
- 31.R Core Team . R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Accessed June 14, 2023. https://www.R-project.org/
- 32.Hua JT, Zell-Baran L, Go LHT, et al. Demographic, exposure and clinical characteristics in a multinational registry of engineered stone workers with silicosis. Occup Environ Med. 2022;79(9):586-593. doi: 10.1136/oemed-2021-108190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Banerjee D, Kuschner WG. Diagnosing occupational lung disease: a practical guide to the occupational pulmonary history for the primary care practitioner. Compr Ther. 2005;31(1):2-11. doi: 10.1385/COMP:31:1:002 [DOI] [PubMed] [Google Scholar]
- 34.Shitrit D, Adir Y, Avriel A, et al. EBUS-TBNA is sufficient for successful diagnosis of silicosis with mediastinal lymphadenopathy. Lung. 2018;196(4):441-445. doi: 10.1007/s00408-018-0129-3 [DOI] [PubMed] [Google Scholar]
- 35.Perret JL, Miles S, Brims F, et al. Respiratory surveillance for coal mine dust and artificial stone exposed workers in Australia and New Zealand: a position statement from the Thoracic Society of Australia and New Zealand. Respirology. 2020;25(11):1193-1202. doi: 10.1111/resp.13952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.OSHA offices by state. Occupational Safety and Health Administration. Accessed April 28, 2023. https://www.osha.gov/contactus/bystate
- 37.State and territorial health departments—STLT Gateway. Centers for Disease Control and Prevention. Published January 23, 2023. Accessed April 28, 2023. https://www.cdc.gov/publichealthgateway/healthdirectories/healthdepartments.html
- 38.Silica safety resources for stone fabricators. California Department of Public Health Occupational Health Branch. Published February 8, 2023. Accessed March 8, 2023. https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/OHB/Pages/SilicaStoneFabricators.aspx
- 39.Hierarchy of controls. Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. Published January 17, 2023. Accessed February 10, 2023. https://www.cdc.gov/niosh/topics/hierarchy/default.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement