The COVID-19 pandemic has been accompanied by mental stress in children and families, as has been shown by numerous meta-analyses and the nationwide COPSY (COVID-19 and Psychological Health) Study (1– 3). Furthermore, long COVID symptoms are increasingly gaining attention (4). The longitudinal COPSY study has investigated in four survey waves so far (W1: 05–06/2020, W2: 12/2020–01/2021, W3: 09–10/2021, W4: 02/2022) how the mental health and quality of life of children and adolescents developed during the first two years of the pandemic, and which risk factors and resources affected the trend.
Footnotes
Conflict of interest statement The authors declare that no conflict of interest exists.
Translated from the original German by Birte Twisselmann, PhD.
Methods
A total of 2319 families with children aged 7–17 participated in the study; the study is based on self reports from 11–17 year olds (n=1602) and from one parent (7–17 years, n=2319), respectively. The families were selected randomly by Infratest Dimap and invited to participate. The sample reflects the structure of the German baseline total of parents with 7–17 year old children according to the most recent microcensus (2018). The longitudinal participation was high in all survey waves, at more than 80% (wave four: 83.6%, initial response rate: 45.8%). We used internationally validated scales (Figure, Table). The health data were analyzed by means of descriptive statistics, chi square tests, and logistic regression in order to calculate the associations (odds ratio, OR) between a defined risk group and the outcomes were adjusted for age, sex, and the interaction between age and sex. The data were compared with pre-pandemic reference values of the BELLA Study (5), which was the methodological basis for the COPSY Study and whose design, sample selection, and survey instruments were almost identical.
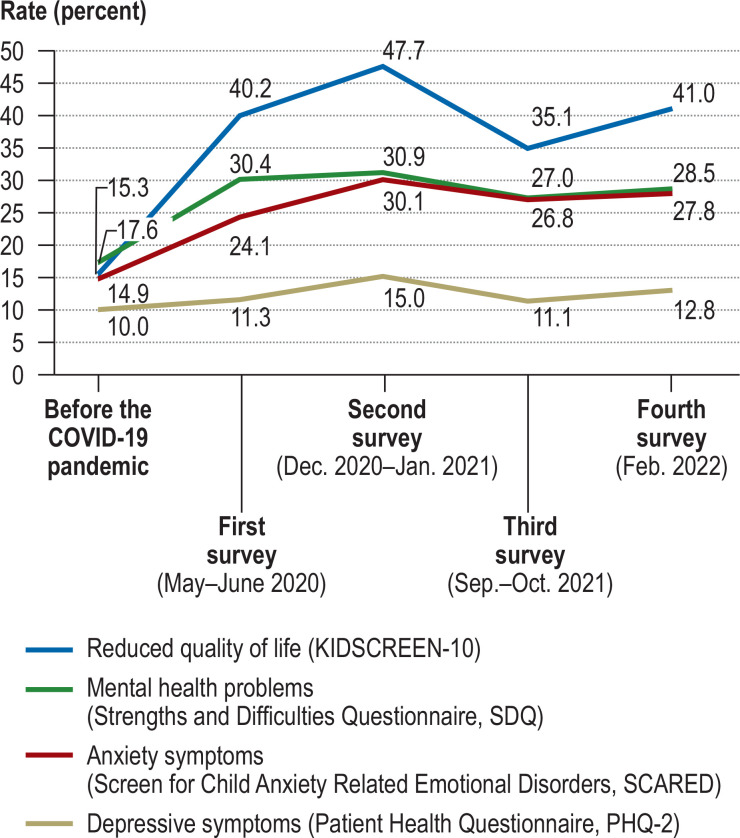
Figure.
Quality of life (somatic, mental, and social quality of life in the KIDSCREEN-10) and mental abnormalities (emotional, behavioral, hyperactivity, and peer problems in theSDQ; generalized anxiety in the SCARED, depressive symptoms in the PHQ-2) in children and adolescents before and during the COVID-19 pandemic overall
Table. Psychosomatic complaints in children and adolescents during the COVID-19 pandemic.
|
BELLA before
the pandemic |
COPSY
W1 |
COPSY
W2 |
COPSY
W3 |
COPSY
W4 |
|
| n = self reports (children) | 1040 | 1073 | 1019 | 1173 | 1119 |
| n = reports by others (parents) | 1552 | 1586 | 1625 | 1618 | 1668 |
| Psychosomatic complaints*3 (at least once in the preceding week) | |||||
| Headache Stomachache Backache Feeling low Irritability Nervousness Sleeping problems Dizziness/daze |
28.3 % 21.3 % 25.9 % 23.0 % 39.8 % 23.6 % 39.2 % 16.4 % |
40.5 % 30.5 % 26.4 % 33.8 % 53.2 % 27.9 % 43.3 % 11.9 % |
46.4 % 36.4 % 33.0 % 43.4 % 57.2 % 33.3 % 47.4 % 17.3 % |
48.7 % 39.2 % 32.8 % 41.2 % 57.0 % 35.3 % 46.0 % 16.9 % |
53.7 % 40.9 % 32.1 % 44.5 % 56.5 % 35.5 % 50.1 % 17.6 % |
| With at least 3 symptoms*2 | 36.9 % | 48.4 % | 53.0 % | 54.6 % | 58.4 % |
*1 HBSC symptom checklist; *2 children and adolescents ticked in the HBSC questionnaire at least 3 of the 8 symptoms listed in the table as present at least once a week
Results
At the start of the COPSY Study (wave 1), the children and adolescents were on average 11.9 years old (50% girls, 17.2% with a migration background), the parents were 43.1 years old (56.4% mothers, 57.5% medium-level education). In survey wave 4, one in every five children (20.4%) had already had COVID –19 once. The question “How difficult/stressful were changes associated with the corona crisis for you overall?” was answered by 40.8%/28.8%/10.7% with “somewhat”/“quite”/“extremely.” The proportion of children and adolescents with a low quality of life rose from 15.3% before the pandemic to 35.1–47.7%. The proportion of children with mental health problems rose during the pandemic to almost one third until survey wave 2, fell slightly by the time of survey wave 3, and has stagnated since, at 27.0–28.5%. For self-reported symptoms of anxiety or depression, the trend was similar (figure). The reported values were self-reported symptoms of mental health problems, not diagnosed mental disorders.
Psychosomatic complaints rose continually throughout the pandemic, among children and adolescents with prior COVID-19 infection, 60.8% (W4) and 77.5% (W3) experienced at least three symptoms (table). 14.0–16.7% of children and adolescents were affected by a combination of the following:
Either
One of the parents has a mental disorder or
The parents were severely stressed as a result of the pandemic or
The parents had low-level education and a very restricted living space (<20 sq m/person) or had a migration background.
Children and adolescents with this risk cluster conceptualized a priori were across the four survey waves had a 1.2–4.3 higher chance or risk (OR) of a low quality of life (OR: 1.2–2.8; p<0.001–0.004), of having mental health problems (OR: 2.6–4.3; p<0.001), symptoms of anxiety (OR: 1.2–2.8; p<0.001–0.453) or symptoms of depression (OR: 2.1–3.8; p<0.001) or of developing psychosomatic complaints (OR: 1.5–3.2; p< 0.001–0.013).
Almost all children and adolescents coped with the stress and risks thanks to a positive family atmosphere, more than three quarters thanks to strong personal resources, and about half thanks to good social support. Children with this combined resource cluster (in each resource variable above the 20th percentile) had a 0.1–0.2 reduced chance/risk (OR) for a poor quality of life (p<0.001); mental health problems (OR: 0.1–0.2; p< 0.001), symptoms of anxiety (OR: 0.2–0.3; p<0.001), depressive symptoms (OR: 0.1–0.2; p<0.001), and psychosomatic complaints (OR: 0.4–0.5; p<0.001).
Discussion
Even two years after the onset of the pandemic, at the start of 2022, a large proportion of children were affected by mental stress. Especially psychosomatic symptoms slightly increased once again. This is consistent with international meta-analyses (2, 3). For the pre-pandemic comparison, the data of the methodologically comparable BELLA Study were used. Even though the COPSY Study is the first to show a trend over two years of the pandemic, no causal conclusions can be drawn and it is unclear whether the results are associated with a notable increase in COVID-19 infections/post- or long COVID, the winter season, the cumulative stress of the pandemic or other factors. Most of the children and adolescents had good resources to cope with this experience of stress. Even though the effect sizes overall are small, a substantial proportion of children and adolescents still had mental health problems(28.5%) or were in the risk group (14.0%) two years after the onset of the pandemic. These adolescents need support in order to strengthen their mental health.
References
- 1.Schlack R, Neuperdt L, Junker S, et al. Veränderungen der psychischen Gesundheit in der Kinder- und Jugendbevölkerung in Deutschland während der COVID-19-Pandemie—Ergebnisse eines Rapid Reviews. PsyArXiv. 2022 [Google Scholar]
- 2.Ravens-Sieberer U, Kaman A, Devine J, et al. The mental health and health-related behavior of children and parents during the COVID-19 pandemic Findings of the longitudinal COPSY study. Dtsch Arztebl Int. 2022;119:436–437. doi: 10.3238/arztebl.m2022.0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma L, Mazidi M, Li K, et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;293:78–89. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez-Leon S, Wegman-Ostrosky T, Ayuzo Del Valle NC, et al. Long-COVID in children and adolescents: a systematic review and meta-analyses. Sci Rep. 2022;12 doi: 10.1038/s41598-022-13495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Otto C, Reiss F, Voss C, et al. Mental health and well-being from childhood to adulthood: design, methods and results of the 11-year follow-up of the BELLA study. Eur Child Adolesc Psychiatry. 2021;30:1559–1577. doi: 10.1007/s00787-020-01630-4. [DOI] [PMC free article] [PubMed] [Google Scholar]