Abstract
Background:
Total knee arthroplasty (TKA) is associated with tremendous postoperative pain, and pain relief should concisely be considered. This study aims to compare the efficacy of preemptive periarticular multimodal drug injection versus placebo and oral celecoxib on postoperative pain control after TKA.
Materials and Methods:
This study is a randomized clinical trial on 146 patients candidate for TKA who were randomly allocated to three treatment groups, including (1) a cocktail consisting of bupivacaine, morphine, epinephrine, and ketorolac (n = 48), (2) only epinephrine (placebo group) (n = 49), and (3) 400 mg celecoxib orally (control group) (n = 49) using the Random Allocation software. The injections and oral therapy were performed within 15 min before the surgical procedure. The study's primary outcome was the Knee Society Score (KSS) calculated at baseline, within 6 weeks and 6 months postoperatively. Range of motion (ROM) and Visual Analog Scale (VAS) to assess pain intensity as the other primary outcomes were evaluated before the procedure, within 24 h, 48 h, and 6 weeks postoperatively.
Results:
The three studied groups were similar regarding demographic characteristics, including age (P = 0.33), gender distribution (P = 0.65), and involved knee side (P = 0.94). Baseline comparison of KSS (P = 0.39), VAS (P = 0.24), and ROM (P = 0.37) among the groups revealed insignificant differences. All the studied groups showed a statistically significant trend of improvement in KSS, VAS, and ROM (P < 0.001), while the comparison of the three groups in terms of KSS (P = 0.001), VAS (P < 0.001), and ROM (P < 0.001) revealed remarkable superiority of multimodal injection to the other treatments.
Conclusion:
Preemptive periarticular multimodal drug injection, including bupivacaine, morphine, epinephrine, and ketorolac, can cause considerable postoperative pain relief and better ROM achievement in comparison to placebo or oral celecoxib.
Keywords: Multimodal analgesia, pain, range of motion, total knee arthroplasty
INTRODUCTION
Total knee arthroplasty (TKA) is a painful but efficient orthopedic procedure used to treat patients suffering from degenerative disease, osteoarthritis in particular.[1,2] TKA, which is mostly performed on the elderly, may cause considerable postoperative pain that can lead to an increased hospital stay, disability to take part in rehabilitation programs, poor outcomes, and increased rate of referral to health-care centers as well as chronic pain in up to 35% of patients.[3,4]
The concept of pain turned into a significant issue to the extent that it has been declared as the fifth parameter of the vital sign by the Joint Commission on Accreditation of Health-care Organizations (JCAHO).[5] Accordingly, varieties of pain-relieving approaches have been provided to manage postoperative pain.[6] Nevertheless, the old age of the patients who are the majority of patients requiring TKA can limit the alternatives for this aim.[7]
The traditional methods include the use of analgesic agents such as nonsteroidal analgesic agents (NSAIDs), acetaminophen, gabapentin, and pregabalin, which not only has short-term effects but also may cause drug-related adverse effects and are mostly required to be administered for a long time.[8] Nevertheless, preoperative use of NSAIDS, cyclooxygenases-2 inhibitors, in particular, has shown promising outcomes as it can reduce the amount of retrieved inflammatory factors at the site of surgery in addition to its opioid-sparing effect, which can reduce opioid-related side effects, including nausea and vomiting, which contribute to the postoperative morbidity associated with TKA.[7]
Using opioids for postoperative pain management is a common and useful option but has complications such as nausea and vomiting, respiratory depression, drowsiness, decreased gut motility, and urinary retention.[9] Other postoperative pain relief strategies with acceptable outcomes are continuous epidural, lumbar plexus, femoral, and sciatic nerve blocks. These approaches can effectively control postoperative pain and decrease narcotic consumption, though have several side effects such as epidural bleeding, less muscle strength, urinary retention, and neuronal damages.[10]
The use of multimodal local analgesics at the surgical site during or by the end of the procedure is another optimal option for reducing postoperative pain with minimal side effects in TKA. Intra-articular injection of mixed analgesics following TKA surgery has been accompanied by decrease in further requirements for analgesia and led to earlier hospital discharge;[11,12] however, studies in this regard have not achieved unified outcomes.[13,14]
Despite various introduced strategies for postprocedural pain management among patients undergoing TKA, limited comparative evidence is available to assess the best pain controlling approach. Besides, numerous patients are suffering from chronic postoperative pain worldwide to the extent that they are dissatisfied with their procedure.[15,16] Therefore, the current study is raised to assess the efficacy of periarticular multimodal injections versus placebo and oral analgesic therapy for post-TKA pain relief.
METHODS
Participants and study design
This is a randomized clinical trial conducted on 146 patients undergone TKA in orthopedic hospitals affiliated at Isfahan University of Medical Science (IUMS) in 2016.
The presence of osteoarthritis, making the patients candidate for primary unilateral TKA, and body mass index of 20–30 kg/m2 were determined as inclusion criteria for participation in this study.
Abnormal renal function test (Cr clearance <60 ml/min), abnormal liver function test, myofascial pain syndrome or fibromyalgia, and patient's unwillingness for participation in the study were considered as unmet criteria. Patients with allergy, drug and/or alcohol abuse, inflammatory arthritis, history of previous major knee surgery, and those who were a candidate for bilateral TKA were the other conditions defined as unmet criteria, as well.[17] American College of Rheumatology Preliminary Diagnostic Criteria were used to diagnose fibromyalgia and myofascial pain syndrome.[18]
Failure to refer for follow-up assessments and more than 20% defects in medical records were the current study's exclusion criteria.
The study was approved in the Ethics Committee of IUMS (ethical code: IR.mui.rec. 1396.3.048), and the study protocol was registered in the ClinicalTrials.gov (NCT05324995) and also was explained entirely for the patients, they were reassured about their information confidentiality, and written consent was obtained.
This study was designed as a census study; therefore, all the patients who met the criteria for participation in this study were recruited. Participants were randomly divided into three groups using the Random Allocation software, so each patient was provided with a specific number from 1 to 146 by the software and allocated to one of the groups.
The investigator who performed the baseline and follow-up assessments and the patients were unaware of the study group; as the investigator was absent at the time of the surgery and all the patients administered a pill before the surgical procedure (one group was treated with celecoxib and the other two ones administered placebo similar in shape and color with celecoxib).
The surgical technique
All TKA surgeries were performed under spinal anesthesia using 10–15 mg Marcaine (bupivacaine). About 1 g cefazoline (EXIR®, Boroujerf, Iran) was administered for patients within an hour before the surgery.
TKA surgery was performed for all participants by a reference skilled orthopedic surgeon electively using knee prosthesis (Zimmer®, Warsaw, IN, USA).
After proper sterilization, a preemptive periarticular injection was done for participants in the first and second groups. Then, an anterior midline skin incision was done within 8 cm above the patella to 2 cm distal to the tibial tubercle.
A pneumatic tourniquet was pumped up before incision and collapsed before the soft tissue repair at the end of surgery. A low vacuum intraarticular drain was used during soft tissue repairing for postoperative wound drainage and then removed 48 h after surgery.[19]
For pain control following the surgery, meloxicam (15 mg daily), celecoxib (400 mg daily), acetaminophen (1000 mg every 8 h), tramadol (50 mg every 8 h), ketorolac (30 mg slow IV every 8 h, 4-dose max), and morphine (5–10 mg slow IV, PRN) were prescribed for the patients.
On the 1st day after surgery, all patients were mobilized, and daily 60 mg subcutaneous enoxaparin (Clexane®, Prefilled syringes Sanofi, Seine Martine, France) was used for deep-vein thrombosis (DVT) prophylaxis for 14 days. Prophylactic treatment of patients with a higher risk of DVT was continued with bridging therapy of warfarin, and then, warfarin was merely prescribed for a further 3 months.[20]
After that, the patients were discharged within 3 days after the surgery if they were appropriately mobilized and had dry clean wounds. After discharge, standard rehabilitation methods were used for patients at home or in physiotherapy centers. The rehabilitation schedule consisted of strengthening lower extremity muscles by concentration on the quadriceps, and gait training with weight bearings was allowed by the reconstructed knee to perform the necessary daily life.[21]
The interventions
The first group was treated using a preemptive periarticular injection of multimodal drugs. Therefore, a combination of drugs consisted of 50 mg bupivacaine hydrochloride 0.5% (AstraZeneca, Cenexi, France), 1 ml morphine sulfate 10 mg/ml (DarouPakhsh, Tehran, Iran), 300 mcg epinephrine (1:1000) (DarouPakhsh, Tehran, Iran), and 30 mg ketorolac (Caspian Tamin, Rasht, Iran) diluted by 0.9% sodium chloride solution to make a total 100 ml of injection drug was injected in the periarticular area. The injections were done within 15 min before the incision in seven areas of the joint as followed: 15 ml in posterolateral soft tissue and lateral femoral periosteum, 15 ml posteromedial soft tissue and medial femoral periosteum, 20 ml inferomedial capsule, 20 ml superomedial capsule, 10 ml lateral capsule, 10 ml medial subcutaneous tissues, and 10 ml lateral subcutaneous tissue.
The second group received 300 mcg epinephrine (1:1000) (DarouPakhsh, Tehran, Iran) peri-articulary, similar to the first group.
The third group administered celecoxib (200 mg) orally immediately before the surgery initiation.
Outcomes
Before the surgical procedure, patients’ age, gender, and the operated knee side were recorded in the study checklist.
The study's primary outcomes included measurements of Knee Society Score (KSS) and range of motion (ROM) as the determinant of knee function and Visual Analog Scale (VAS) as the means for pain assessment.
The KSS is an assessment of the knee that comprises two arms, the functional ability and clinical examination scores, each with a 100-point denominator. One-hundred points are allocated to the functional capacity, including walking distance, stair-climbing ability, and the use of walking aids. The latter 100 points are used to assess knee motion, stability, and pain. This scoring is divided into two subscales, 50 points for evaluating motion, stability, and alignment. The remained 50 points for pain intensity assessment.[22] According to the scores 160–200, 140–159, 120–139, and <120, the KSS total score was defined as excellent, good, fair, and poor, respectively.[19] KSS was at baseline, and then, within 6 weeks and 6 months postoperatively.
In addition, the knee ROM was evaluated using a standard goniometer.[23]
VAS was used to evaluate the patient's postoperative pain intensity with a 0–10 rating scoring scale.[16]
The patient's postoperative pain intensity and ROM were evaluated in the preoperative visit (baseline), within 24 h, 48 h, and 6 weeks following surgery.
Statistical analysis
The obtained data were entered into the Statistical Package for the Social Sciences (version 22, IBM Corporation, Armonk, NY, USA). The descriptive data were presented in mean, standard deviation, absolute numbers, and percentages. In order to assess the normality of data, the Kolmogorov–Smirnov test was administered. The Chi-square test was utilized to compare the categorical variables, and the quantitative variables were compared using independent t-test for two variables and ANOVA for more than two variables. Tukey post hoc test was utilized to detect the difference between two independent variables evaluated by ANOVA test. Repeated-measure ANOVA assessments were performed to compare independent quantitative variables in repeated measurements. P < 0.05 was considered statistically significant level.
RESULTS
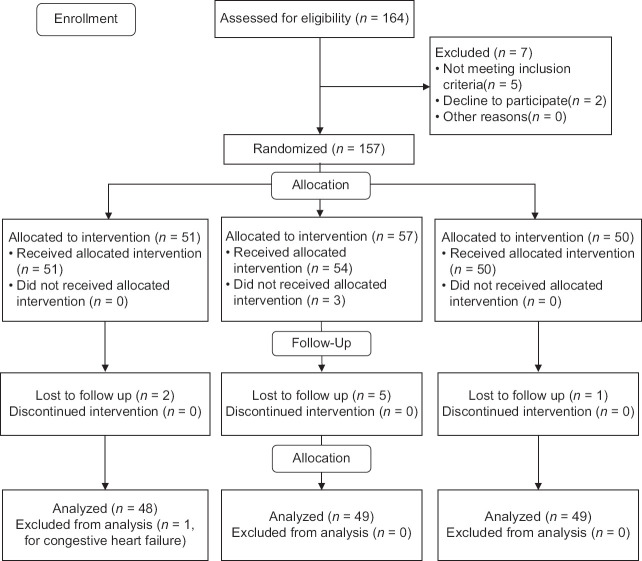
In this clinical trial, 170 patients undergone unilateral TKA were assessed, among which 164 ones were eligible to participate in the study. Five patients did not meet inclusion criteria, and two ones refused to participate in this study. During the study, three patients in the second group did not receive the intervention because of unwillingness to participate in the study, and eight ones did not refer for follow-ups (2 in the first, 5 in the second, and 1 in the third group) and thus were excluded from the study. The information of one patient in the first group was excluded because of having congestive heart failure. Eventually, data about 146 patients were analyzed [Figure 1].
Figure 1.
The flow diagram of randomization of patients
One-hundred and forty-six patients with a mean age of 63.38 ± 5.486 years (37–81) and female gender predominance 92.5% (n = 135) were assessed.
The comparison of demographic factors, including age (P = 0.33), gender distribution (P = 0.33), and side of the operated knee (P = 0.94), was not statistically different among the three groups. Detailed information is provided in Table 1.
Table 1.
Demographic data of participants
| Variable | Multimodal injection, n (%) | Placebo group, n (%) | Control group, n (%) | P |
|---|---|---|---|---|
| Age (mean±SD) | 63.44±6.164 | 64.18±4.902 | 62.53±5.319 | 0.330* |
| Gender | ||||
| Male | 5 (10.4) | 3 (6.1) | 3 (6.1) | 0.65** |
| Female | 43 (89.6) | 46 (93.9) | 46 (93.9) | |
| Side | ||||
| Right | 26 (54.2) | 28 (57.1) | 28 (57.1) | 0.94** |
| Left | 22 (54.8) | 21 (42.9) | 21 (42.9) |
*One-way ANOVA test did not show significant differences, **Chi-square test did not show significant differences. SD=Standard deviation
Baseline KSS (P = 0.39), ROM (P = 0.24), and VAS (P = 0.37) assessments of the three groups revealed insignificant differences; however, further comparison of KSS measurements within 6 weeks (P < 0.001) and 6 months (P < 0.001) postoperatively represented significant differences among the groups. Post hoc evaluations revealed multimodal injection superiority to the other two techniques (P < 0.001), whereas the control and placebo groups, were similar (P > 0.05). The VAS and ROM assessments within 24 and 48 h after the surgical procedure, as well as within the next 6 months, were accompanied by remarkable better statuses of multimodal injection than the two other interventions (P < 0.05) in all the assessments. The post hoc measurements showed remarkable better outcomes of multimodal injection than the other two interventions in all assessments (P < 0.05), while generally, the other two groups were similar, but not in all measurements demonstrated in Table 2. The repeated measurements of KSS, VAS, and ROM revealed statistically significant improvements in all the interventions (P < 0.001 for all three groups represented as P1); however, the comparison of the groups revealed remarkable superiority of multimodal injection to the other two techniques in terms of higher KSS scores (P < 0.001 represented as P3), less pain intensity based on VAS (P < 0.001 represented as P3), and better ROM (P < 0.001 represented as P3).
Table 2.
Total contents of knee society score, visual analog scale and range of motion in three groups
| Variable | Mean±SD | P * | P** (between multimodal injection and placebo) | P** (between multimodal injection and control group) | P** (between placebo group and control group) | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Multimodal injection | Placebo group | Control group | |||||
| KSS | |||||||
| Baseline | 1.49±24.894 | 1.94±23.942 | 6.84±13.801 | 0.39 | 0.918 | 0.224 | 0.26 |
| Within 6 weeks | 113.15±14.89 | 100.24±17.97 | 102.02±7.91 | <0.001 | <0.001 | <0.001 | 0.53 |
| Within 6 months | 115.96±13.49 | 101.20±16.62 | 98.53±6.97 | <0.001 | <0.001 | <0.001 | 0.31 |
| P1 (time) | <0.001 | <0.001 | <0.001 | ||||
| P3 (intervention) | 0.001 | ||||||
| VAS | |||||||
| Baseline | 7±1.22 | 7.39±1.07 | 7.27±1.09 | 0.24 | 0.098 | 0.25 | 0.59 |
| Within 24 h | 6.39±1.45 | 8.80±0.88 | 8.10±0.65 | <0.001 | <0.001 | <0.001 | 0.001 |
| Within 48 h | 5.02±1.25 | 6.20±1.22 | 6.18±0.80 | <0.001 | <0.001 | <0.001 | 0.92 |
| Within 6 weeks | 3.46±1.14 | 4.15±1.25 | 3.67±0.65 | 0.006 | 0.002 | 0.31 | 0.028 |
| P1 (time) | <0.001 | <0.001 | <0.001 | ||||
| P3 (intervention) | <0.001 | ||||||
| ROM | |||||||
| Baseline | 87.89±10.41 | 90.10±10.02 | 90±3.68 | 0.37 | 0.21 | 0.23 | 0.95 |
| Within 24 h | 107.56±6.36 | 94.49±3.57 | 95±2.88 | <0.001 | <0.001 | <0.001 | 0.57 |
| Within 48 h | 113.44±5.09 | 96.12±4.11 | 98.16±2.83 | <0.001 | <0.001 | <0.001 | 0.015 |
| Within 6 weeks | 128.33±13.18 | 119.80±8.16 | 122.65±4.57 | <0.001 | <0.001 | 0.003 | 0.12 |
| P1 (time) | <0.001 | <0.001 | <0.001 | ||||
| P3 (intervention) | <0.001 | ||||||
*ANOVA, **Post hoc Tukey test. P1, P2, P3 at the 5% level error of repeated measures. KSS=Knee society score; VAS=Visual Analogue Scale; ROM=Range of motion; SD=Standard deviation
DISCUSSION
This study's study population was not statistically different regarding age, gender, and side of the knee under TKA. Therefore, demographic variables could not influence the outcomes of the study. This study demonstrated that using the preemptive periarticular injection of multimodal medications, including bupivacaine hydrochloride, morphine, epinephrine, and ketorolac, can efficiently tranquilize postoperative pain. However, the two other techniques were accompanied by promising outcomes, as well. Nevertheless, the three groups’ general comparison revealed the superiority of the preemptive periarticular injection of multimodal medications to the other two techniques.
Surgery trauma during TKA decreases afferent nociceptive neuron thresholds and increases spinal neuron excitability. This is a somatic pain that may be present for months.[24] Postoperative pain management in TKA is critical and includes systemic, local, and regional methods.[25] Local injection of analgesic agents in the site of surgery is appropriate for controlling postoperative pain after TKA with limited side effects.[7,24] Limited studies have demonstrated the efficacy of preemptive periarticular injection in controlling postoperative pain in TKA.
A reviewed study reported that periarticular injection of morphine in TKA surgery could significantly decrease postoperative pain compared to placebo.[13] Another study used the preemptive periarticular injection of opioid, ketorolac, ropivacaine, and epinephrine and evaluated postoperative pain within 6 and 12 h after surgery and showed that this method could significantly decrease self-reported pain score and improve self-satisfactory presentation.[17] Studies demonstrated that a mixture of opioids, NSAIDs, epinephrine, and long-acting local anesthetics could cause proper analgesia after TKA.[7,26] Yue et al. presented that receiving a periarticular injection of multimodal drugs consisted of corticosteroids can cause earlier rehabilitation and hospital discharge, although pain relief was not positively affected by cocktails containing corticosteroids in comparison to those without steroids.[27] The further study presented that periarticular injection of multimodal medications had fewer side effects, caused the reduced incidence of nausea and vomiting, and also decreased the risk of wound infections.[28]
The efficacy of multimodal medications may be attributed to its consistency. Opioid receptors are located in peripheral inflamed tissues and are expressed after surgical trauma. Mentioned receptors are responsible for sensory input to the central nervous system.[29] NSAIDs can decrease peripheral sensitization and activation of nociceptors.[30] Bupivacaine can block afferent peripheral nociceptive activity and also has anti-inflammatory effects.[31] The epinephrine used in periarticular multimodal injections causes decreased local blood flow leading to local anesthesia toxicity reduction.[32]
Several studies evaluated the effects of celecoxib on postoperative pain after TKA in comparison to placebo. However, there is no study compared this medication with the periarticular injection of multimodal medications. One study prescribed 400 mg celecoxib before surgery for patients undergoing TKA and then continued with 200 mg celecoxib for 12 days postoperatively. This method significantly improved postoperative knee ROM and decreased postoperative morphine requirement compared with the placebo.[33] Another study showed that perioperative use of celecoxib was accompanied by less time to achieve maximal ROM and improved knee function within a year after surgical procedure.[34]
Studies have presented the superiority of 400 mg celecoxib to the 200 mg doses.[35] Moreover, our study results may have occurred due to ketorolac's use, as an NSAID, in our cocktail. Therefore, we want to recommend further studies prescribing preoperative 400 mg of oral celecoxib.
Limitations
Despite the appropriate population of this study, a significant limitation in the current report is to follow the patients for a short period; therefore, further studies with a larger sample population and more extended follow-up periods are strongly recommended. Another limitation was lacking hospitalization duration and postoperative opioid requirement assessment. The third limitation of this study may be attributed to the assessment of probable confounders. It is still possible that unmeasured confounders interfere with a part of the associations have been missed. Among the probable confounder, the patients’ job, smoking, physical activity, and dietary status can be named that has not been assessed in the current report.
CONCLUSION
Preemptive periarticular multimodal drug injection, including bupivacaine, morphine, epinephrine, and ketorolac, can cause considerable postoperative pain relief and better ROM achievement in comparison to placebo or oral celecoxib. Thus, periarticular multimodal drug injection is recommended for patients who are candidates for TKA.
Further studies with a more extensive study population and considering more variables affecting the study outcomes are strongly recommended.
Financial support and sponsorship
Isfahan University of Medical Sciences has funded the current study.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to Kashani Hospital's head office, nurses, and employees. In addition, we want to acknowledge Dr. Ali Safaei for his efforts to prepare the current manuscript.
REFERENCES
- 1.Bastos Filho R, Magnussen RA, Duthon V, Demey G, Servien E, Granjeiro JM, et al. Total knee arthroplasty after high tibial osteotomy: A comparison of opening and closing wedge osteotomy. Int Orthop. 2013;37:427–31. doi: 10.1007/s00264-012-1765-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mousavian A, Kachooie AR, Ali Birjandinejad MK, Ebrahimzadeh MH. Translation and cross-cultural adaptation of the hip disability and osteoarthritis score into Persian language: Reassessment of validity and reliability. Int J Prev Med. 2018;9:23. doi: 10.4103/ijpvm.IJPVM_359_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puolakka PA, Rorarius MG, Roviola M, Puolakka TJ, Nordhausen K, Lindgren L. Persistent pain following knee arthroplasty. Eur J Anaesthesiol. 2010;27:455–60. doi: 10.1097/EJA.0b013e328335b31c. [DOI] [PubMed] [Google Scholar]
- 4.Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2:e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009;467:1418–23. doi: 10.1007/s11999-009-0728-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Derakhshan P. What is the role of erythropoietin prolotherapy on pain relief of knee osteoarthritis? J Res Med Sci. 2018;23:50. doi: 10.4103/jrms.JRMS_802_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCartney CJ, Nelligan K. Postoperative pain management after total knee arthroplasty in elderly patients: Treatment options. Drugs Aging. 2014;31:83–91. doi: 10.1007/s40266-013-0148-y. [DOI] [PubMed] [Google Scholar]
- 8.Gaffney CJ, Pelt CE, Gililland JM, Peters CL. Perioperative pain management in hip and knee arthroplasty. Orthop Clin North Am. 2017;48:407–19. doi: 10.1016/j.ocl.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Essving P, Axelsson K, Åberg E, Spännar H, Gupta A, Lundin A. Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: A randomized controlled trial. Anesth Analg. 2011;113:926–33. doi: 10.1213/ANE.0b013e3182288deb. [DOI] [PubMed] [Google Scholar]
- 10.Baratta JL, Gandhi K, Viscusi ER. Perioperative pain management for total knee arthroplasty. J Surg Orthop Adv. 2014;23:22–36. doi: 10.3113/jsoa.2014.0022. [DOI] [PubMed] [Google Scholar]
- 11.Kelley TC, Adams MJ, Mulliken BD, Dalury DF. Efficacy of multimodal perioperative analgesia protocol with periarticular medication injection in total knee arthroplasty: A randomized, double-blinded study. J Arthroplasty. 2013;28:1274–7. doi: 10.1016/j.arth.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Teng Y, Jiang J, Chen S, Zhao L, Cui Z, Khan MS, et al. Periarticular multimodal drug injection in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22:1949–57. doi: 10.1007/s00167-013-2566-0. [DOI] [PubMed] [Google Scholar]
- 13.Kalso E, Tramèr MR, Carroll D, McQuay HJ, Moore RA. Pain relief from intra-articular morphine after knee surgery: A qualitative systematic review. Pain. 1997;71:127–34. doi: 10.1016/s0304-3959(97)03344-7. [DOI] [PubMed] [Google Scholar]
- 14.Klasen JA, Opitz SA, Melzer C, Thiel A, Hempelmann G. Intraarticular, epidural, and intravenous analgesia after total knee arthroplasty. Acta Anaesthesiol Scand. 1999;43:1021–6. doi: 10.1034/j.1399-6576.1999.431009.x. [DOI] [PubMed] [Google Scholar]
- 15.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient dissatisfaction following total knee arthroplasty: A systematic review of the literature. J Arthroplasty. 2017;32:3854–60. doi: 10.1016/j.arth.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 16.Burns LC, Ritvo SE, Ferguson MK, Clarke H, Seltzer Z, Katz J. Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: A systematic review. J Pain Res. 2015;8:21–32. doi: 10.2147/JPR.S64730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Busch CA, Shore BJ, Bhandari R, Ganapathy S, MacDonald SJ, Bourne RB, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am. 2006;88:959–63. doi: 10.2106/JBJS.E.00344. [DOI] [PubMed] [Google Scholar]
- 18.Wolfe F, Simons DG, Fricton J, Bennett RM, Goldenberg DL, Gerwin R, et al. The fibromyalgia and myofascial pain syndromes: A preliminary study of tender points and trigger points in persons with fibromyalgia, myofascial pain syndrome and no disease. J Rheumatol. 1992;19:944–51. [PubMed] [Google Scholar]
- 19.Obaid-Ur-Rahman, Hafeez S, Amin MS, Ameen J, Adnan R. Early release of tourniquet in total knee arthroplasty: Is it worthwhile? J Pak Med Assoc. 2015;65(11 Suppl 3):S77–81. [PubMed] [Google Scholar]
- 20.Warwick D. Prevention of venous thromboembolism in total knee and hip replacement. Circulation. 2012;125:2151–5. doi: 10.1161/CIRCULATIONAHA.111.055731. [DOI] [PubMed] [Google Scholar]
- 21.Canale ST, Beaty JH. Campbell's Operative Orthopaedics E-Book. Amsterdam: Elsevier Health Sciences; 2012. [Google Scholar]
- 22.Ghanem E, Pawasarat I, Lindsay A, May L, Azzam K, Joshi A, et al. Limitations of the Knee Society Score in evaluating outcomes following revision total knee arthroplasty. J Bone Joint Surg Am. 2010;92:2445–51. doi: 10.2106/JBJS.I.00252. [DOI] [PubMed] [Google Scholar]
- 23.Sancheti KH, Sancheti PK, Shyam AK, Joshi R, Patil K, Jain A. Factors affecting range of motion in total knee arthroplasty using high flexion prosthesis: A prospective study. Indian J Orthop. 2013;47:50–6. doi: 10.4103/0019-5413.106901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsukada S, Wakui M, Hoshino A. Postoperative epidural analgesia compared with intraoperative periarticular injection for pain control following total knee arthroplasty under spinal anesthesia: A randomized controlled trial. J Bone Joint Surg Am. 2014;96:1433–8. doi: 10.2106/JBJS.M.01098. [DOI] [PubMed] [Google Scholar]
- 25.Motififard M, Omidian A, Badiei S. Pre-emptive injection of peri-articular-multimodal drug for post-operative pain management in total knee arthroplasty: A double-blind randomized clinical trial. Int Orthop. 2017;41:939–47. doi: 10.1007/s00264-016-3357-2. [DOI] [PubMed] [Google Scholar]
- 26.Kim TW, Park SJ, Lim SH, Seong SC, Lee S, Lee MC. Which analgesic mixture is appropriate for periarticular injection after total knee arthroplasty? Prospective, randomized, double-blind study. Knee Surg Sports Traumatol Arthrosc. 2015;23:838–45. doi: 10.1007/s00167-014-3366-x. [DOI] [PubMed] [Google Scholar]
- 27.Yue DB, Wang BL, Liu KP, Guo WS. Efficacy of multimodal cocktail periarticular injection with or without steroid in total knee arthroplasty. Chin Med J (Engl) 2013;126:3851–5. [PubMed] [Google Scholar]
- 28.Andersen KV, Nikolajsen L, Haraldsted V, Odgaard A, Søballe K. Local infiltration analgesia for total knee arthroplasty: Should ketorolac be added? Br J Anaesth. 2013;111:242–8. doi: 10.1093/bja/aet030. [DOI] [PubMed] [Google Scholar]
- 29.Stein C. Peripheral Mechanisms of Opioid Analgesia. Opioids II: Springer. 1993:91–103. doi: 10.1213/00000539-199301000-00031. [DOI] [PubMed] [Google Scholar]
- 30.McCormack K, Brune K. Dissociation between the antinociceptive and anti-inflammatory effects of the non-steroidal anti-inflammatory drugs. Drugs. 1991;41:533–47. doi: 10.2165/00003495-199141040-00003. [DOI] [PubMed] [Google Scholar]
- 31.Martinsson T, Haegerstrand A, Dalsgaard CJ. Effects of ropivacaine on eicosanoid release from human granulocytes and endothelial cells in vitro. Inflamm Res. 1997;46:398–403. doi: 10.1007/s000110050210. [DOI] [PubMed] [Google Scholar]
- 32.Solanki DR, Enneking FK, Ivey FM, Scarborough M, Johnston RV. Serum bupivacaine concentrations after intraarticular injection for pain relief after knee arthroscopy. Arthroscopy. 1992;8:44–7. doi: 10.1016/0749-8063(92)90134-w. [DOI] [PubMed] [Google Scholar]
- 33.Liu J, Wang F. Preoperative celecoxib analgesia is more efficient and equally tolerated compared to postoperative celecoxib analgesia in knee osteoarthritis patients undergoing total knee arthroplasty: A randomized, controlled study. Medicine (Baltimore) 2018;97:e13663. doi: 10.1097/MD.0000000000013663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin J, Zhang L, Yang H. Perioperative administration of selective cyclooxygenase-2 inhibitors for postoperative pain management in patients after total knee arthroplasty. J Arthroplasty. 2013;28:207–13.e2. doi: 10.1016/j.arth.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 35.Rømsing J, Møiniche S. A systematic review of COX-2 inhibitors compared with traditional NSAIDs, or different COX-2 inhibitors for post-operative pain. Acta Anaesthesiol Scand. 2004;48:525–46. doi: 10.1111/j.0001-5172.2004.00379.x. [DOI] [PubMed] [Google Scholar]