Summary
Background
This study addressed the limited understanding of suicide risk and patterns among migrants in Australia. It examined national-level suicide rates and trends in the Australian population to identify migrant groups which are disproportionately affected by suicide.
Methods
The National Coronial Information System was used to identify suicide cases from 2006 to 2019. Incident rate ratios (IRR) with 95% confidence intervals (CI) evaluated suicide risk for migrant groups compared to Australian-born and migrants from English-speaking countries. Age-standardised suicide rates (ASR) per 100,000 and average annual percentage change (AAPC) were calculated to compare suicide rates and trends.
Findings
Compared to the Australian-born population, all migrant males and females had significantly lower suicide risk, except females from Oceania countries. Females from European (IRR 1.28, 95% CI 1.13, 1.14) and Oceanian countries (IRR 1.25; 95% CI 0.95, 1.66) had an elevated suicide risk compared to female migrants from English-speaking countries. Male migrants from Oceania (ASR 20.4, AAPC 1.0 (−3.6, 5.8)) and Africa (ASR 18.0, AAPC −0.4 (−5.5, 4.9)) have high ASR with no significant changes in trend over the study duration. Female African migrants had an ASR of 5.3 per 100,000, which increased by 8% (95% CI 1.4, 15.0) between 2006 and 2019.
Interpretation
Migrants from Oceania and African countries are disproportionately affected by suicide mortality compared to other migrant groups in Australia. Further research is needed to identify the risk factors and develop suicide prevention strategies for these groups.
Funding
Suicide Prevention Australia, Australian Research Council.
Keywords: Suicide, Migrant, First-generation, Acculturation, Australia
Research in context.
Evidence before this study
We conducted a search of Medline and PubMed databases for studies published up to December 2022, using three tiers of search terms: migrant (keywords included migration, migrant, immigrant, immigration, skilled worker, refugee, foreign worker, ethnicity, racial, race) (anywhere in the text), suicide (anywhere in the text), and name of 38 Organisation for Economic Co-operation and Development (OECD countries) in the title and abstracts, with no language restrictions. Our final search yielded 664 studies related to the project in OECD countries. Most of the recent literature on this topic from OECD countries came from the United States and England, with only 26 primary studies (both qualitative and quantitative) from Australia. Current evidence suggests that suicide mortality among migrant groups in their host countries depends on various factors, including visa status, country of origin, acculturation stress, and perceived discrimination. Countries of origin can be a significant predictor of suicide mortality, and some migrant groups from countries with lower suicide rates continue to show lower suicide rates in their host countries.
Added value of this study
The existing Australian literature on the suicide mortality of migrant populations is limited, with the latest update available until 2007. This study contributes to the field by offering an updated analysis (covering the period of 2006–2019) of suicide rates and trends among migrant groups in Australia for both males and females. The study identifies migrants from Oceania and African countries as high-risk groups, evidenced by their elevated suicide risk and observed trends.
Implications of all the available evidence
Our study findings indicate that migrants from Oceania and African countries face a disproportionate burden of suicide compared to other migrants in Australia. We also noted some elevated parameters of female suicide (higher risk or increasing suicide rate over time) in migrant groups, which can indicate an emerging problem. Our study also highlighted the lack of ethnicity and migration-related data associated with individual cases, which is one of the limitations of our interpretation. We support calls for police and coronial data collection to report ethnicity and migration-related data to enhance our knowledge of high-risk groups for suicide in migrant communities across Australia. Future suicide prevention interventions should use an intersectionality approach, considering sex, migration status, and countries of birth to determine factors associated with migrant suicide in Australia and develop effective prevention strategies.
Introduction
Migration is recognised as a social determinant of health.1,2 With the increase in global migration in diverse contexts, understanding health inequities as a consequence of migration is increasingly important. Optimal health is an essential selection criterion for skilled/economic migrants in many countries. For example, in Australia, irrespective of skill requirements, a certain level of health is required to contemplate and engage in the migration process.3 Migrants, therefore, tend to have a health advantage over the local-born population in their destination countries, a phenomenon commonly referred to as the healthy migrant effect.4,5 However, a recent systematic review shows that the evidence of migrant mental health advantages over the local-born is inconsistent and that some evidence suggests a decline in migrant mental health over time, especially for migrants in North American and European countries.6 Several factors may contribute to this decline, migrant status (refugee vs economic),7 the ability to secure suitable employment in the host country field,8 unemployment,9,10 and individual factors that affect the process of assimilation in their destination countries such as sex, age at migration, language proficiency, and personality traits.11
Suicide is a significant public health concern worldwide. The suicidal behaviour of an individual is often the result of psychological, environmental, and cultural factors that place some individuals at a greater risk of suicide than others.12 For migrants, their country of origin, which is often used as a proxy measure for their ethnic or cultural backgrounds, has been found to be highly correlated with suicide mortality in destination countries.13, 14, 15 This could partly be explained by the perception of suicide in different cultural groups, where acceptable attitudes towards suicide generally exhibit higher suicide rates than in those cultures where suicide is considered forbidden or sinful.16 Some studies suggest that the cultural protection against suicide lessens as migrants assimilate into host cultures, with some adopting risky health behaviours like alcoholism, or substance abuse, thereby increasing their risk of suicidal behaviour.16,17 Understanding the complex interplay among migration, countries of origin, and suicide is critical, as personal and political circumstances in destination countries can either increase or decrease the risk of suicidal behaviour and mortality among migrants.
Acculturation stress is a predictor of suicidal ideation and poor mental health in migrant communities in their destination countries.18, 19, 20 Acculturation is the process through which individuals adapt and acquire the host society's social norms, culture and beliefs.16 Acculturation stress is the psychological reaction resulting directly from the acculturation process and includes feelings of marginality and alienation, psycho-somatic symptoms, or identity confusion.18 Hence, the closer an immigrant's values are to the dominant culture, the lower the potential acculturation stress will be, protecting against poor mental health and suicide mortality. Individuals who migrate from collectivist to individualistic societies may be at a greater risk of experiencing acculturation stress than others. This can result in an actual or perceived lack of adequate social support, a disparity between expectations and reality, and low self-esteem.18,21 Many migrants experience a drastic change in social status upon migration and disruption in social networks.22 Language and cultural factors, intensified by racial and ethnic prejudice in the host country, may also contribute to immigrants' sense of isolation.23 The combination of these stressors, along with the absence of culturally-sensitive and easily accessible mental health services, and the stigma surrounding seeking help for mental health issues,24 can lead to an elevated risk of suicide mortality among migrants in their destination countries.
Australia is a highly diverse nation, with over 25% of its population being born overseas and 72% of them speaking a language other than English at home.25 In recent years, there has been a surge in migration from countries such as India, Nepal, the Philippines, China, and Vietnam.25 Despite its cultural diversity, Australian suicide literature has a limited understanding of the risk and patterning among migrants from various countries of origin. Two national-level studies have examined suicide mortality among migrants. Ide et al.26 analysed suicide rates from 1974 to 2006 among migrant groups based on their countries of origin. In contrast, Anikeea et al.27 examined various mortality indicators, including intentional self-harm, from 1981 to 2007. Ide et al. found that all migrant groups had a lower suicide risk than the Australian-born population. However, they observed that European regions, specifically Eastern Europe (33.2 per 100,000) and Western Europe (42.1 per 100,000), had higher suicide rates than the Australian-born population as well as other migrant groups.26 Anieeka et al. (2006) reported that during 1981–2007, the suicide rate among Eastern Europeans increased by 3%. Conversely, migrants from Asian (−6.31%), West European (−1.75%), and Southern European (−1.92%) countries showed a significant decline in suicide rates.27 Both studies have confirmed that migrants from Asian, African, and Middle Eastern countries demonstrate a reduced risk of suicide and maintain consistently low and non-increasing suicide rates. However, considering the evolving migration landscape in Australia, characterised by an increasing number of individuals migrating from these regions, Ide et al.26 recommended ongoing monitoring of suicide trends and patterns within these specific groups.
The most recent national-level analysis of migrant suicide mortality used suicide data until 2007, and little has been done since.26,27 One possible explanation is that it is perceived to be less of a problem, given that suicide rates among migrant groups are typically lower than those among the locally-born population. To address this research gap, our study examined national-level suicide rates and trends between 2006 and 2019 across different population groups in Australia. The main objectives of this study were as follows:
-
1)
Assess the suicide risk among migrant groups by sex, with reference to Australian-born and migrants from English-speaking countries.
-
2)
Analyse suicide mortality rates and trends among Australian migrants and Australian-born males and females to identify high-risk migrant groups in Australia.
Methods
Study design
Using intentional self-harm data from the National Coronial Information System (NCIS),28 a retrospective mortality study design was used to compare suicide rates across first-generation migrant groups and those born in Australia and examined changes in suicide mortality over time and across groups.
Database
Data were extracted from the National Coronial Information System (NCIS), a web-based repository of coronial data from Australia and New Zealand (NCIS, 2000). The NCIS holds online records of coronial briefs created as part of the investigation conducted by a coroner into the death of an individual. They provide restricted access to academics and researchers for research purposes after ethics approval. Data is available in both coded and non-coded forms.
Ascertainment of cases
The query builder program of the NCIS online database was used for searching closed cases (for which a coronial investigation was completed) of intentional self-harm deaths between 2001 and 2019. We extracted demographic data on sex, age, country of birth, usual country of residence, place of birth, and year of death. The analytic sample included people 15 years and older at the time of death.
Ascertainment of country of birth
To identify first-generation migrants in our study, we used country of birth and usual country of residence as proxy measures. The NCIS uses the Standard Australian Classification of Countries (SACC)29 to code countries. To ascertain foreign migrants who live permanently in Australia, we only included cases where Australia was noted as the usual country of residence.30 For the country of birth, the NCIS database provides information in two fields 1) country of birth reported by coroners and 2) and place of birth provided by the Births, Deaths and Marriages (BDM) registries in each Australian jurisdiction. Both fields provided similar information, but in some cases, only information was available in one field. The researchers used both fields to minimise missing data on this field. The country of birth was missing in 28% of Coroners' records and 26% from BDM. We substituted missing coroners' data on country of birth with BDM data on the same variable; as a result, the proportion of missing values was decreased to 9%. Data on the country of birth was missing in almost 34% of the cases between 2001 and 2005; for that reason, we restricted our analytical sample to 2006–2019, where missing data on country of birth affected 0.55% of cases. Appendix 1 describes the case inclusion process.
Defining countries of origin
We used the Standard Australian Classification of Countries (SACC) to categorise migrant groups based on their countries of origin.29 The SACC classification is endorsed by the Australian Bureau of Statistics to use when collecting, aggregating and disseminating data relating to characteristics such as birthplace and country of residence.29 The classification structure has a three-level hierarchy based on geographical proximity and has been previously used in studies measuring suicide outcomes in the Australian population.26,27 Using a country of birth or corresponding geographical region is considered an acceptable approach and is particularly useful for studying migrant populations31 as it accounts for the migration context and, to some extent, individual migrant characteristics (refugee vs skilled migrants). In countries like Australia, where previous migration waves have been associated with the countries of origin (migration from UK, China, Europe, Asia, Middle East), country of birth provides a useful migration context. In our study, we used the major groups of SAAC, with some modifications noted below.
Specifically, we separated out English-speaking countries, judging that migrants from these countries would not experience acculturation stress (a predictor of suicidality in migrants) as other migrant groups. The Australian Bureau of Statistics defines English-speaking countries as those from which Australia receives its migrants who primarily speak English as a first language.32
Suicide rates can be susceptible to unstable estimates with wide confidence intervals when based on a low number of cases, making it challenging to draw meaningful conclusions. In the case of migrant groups, several countries of origin correspond to a small number of suicide deaths, which makes it difficult to calculate reliable rates. The Australian Institute of Health and Welfare33 recommends reporting age-standardised mortality rates for a minimum of 20 cases (i.e., the number of deaths or cases). Given that part of our analysis involved using annual suicide data by countries of origin, grouping was necessary to avoid small numbers. It is for this reason that we merged three major SACC groups5, 6, 7 to form one major group for Asia (North-east, south-east, Central and South Asia), and "North Africa" and "Sub-Saharan Africa" to create a major group for migrants from African countries. We also separated the Middle East and South Africa from the African region to minimise the heterogeneity within categorise. Below are the categories used for analysis.
-
1.
Australia
-
2.
English-speaking countries—(including Canada, New Zealand, Ireland, United States, South Africa, UK and Ireland)
-
3.
European countries (excluding Ireland and UK)
-
4.
Asia (including North-East, South-East, and Southern and Central Asia)
-
5.
Africa (excluding South Africa, and Middle East)
-
6.
South and Central America (including the US-Caribbean region)
-
7.
Oceania (excluding Australia and New Zealand)
-
8.
Middle East
Population estimates
Population-level data on sex, age (15 & above), and SACC four-digit codes were obtained from the Australian Census information. Census data (counting persons and places of usual residence) for the years 2006, 2011 and 2016 were used as population estimates. The Census tool of Table Builder was used to obtain age-specific, sex-stratified populations for all countries of birth (SACC countries-Four digits). Population data for Census 2006 was used as the reference year for suicide cases for 2006, Census 2011 as the reference year for suicide cases between 2007 and 2011, and Census 2016 as the reference year for suicide cases between 2012 and 2019.
Analysis
Age-standardised suicide rates per 100,000
Age-standardised suicide rates (ASR) were calculated using the population census data for 2006, 2011, and 2016 by age groups (15–24 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years, 65–74 years and 75 & above years) for Australian migrant (groups) and Australian-born. Since the study aimed to make an international comparison, we used the world population's data (15 and above) for age standardisation.34
Regression model
To determine the relative risk of suicide among Australian migrant males and females, compared to Australian-born and those English-speaking countries, we used Negative binomial regression models. The use of negative binomial regression was chosen over Poisson regression following the identification of over-dispersion in the regression models. Separate regression models were fitted for males and females, and both models were controlled for age and year of death. The regression coefficients were transformed into Incidence rate ratios (IRR) to aid interpretation, and analysis was undertaken in Stata 16.0.
Joinpoint regression
For the study's second objective, joinpoint regression was used to analyse the trend of suicide mortality over a period of 13 years. The joinpoint analysis produces two measures of trends: the annual percentage change (APC) and the average annual percentage change (AAPC).35 The APC shows significant changes in the trend (at P < 0.05) corresponding to each time segment (also known as the joinpoint segment), while the AAPC provides a summary measure of the trend change for the study duration. The AAPC is calculated as a weighted average of the APCs, with the weights based on the length of the joinpoint segments, accounting for trend transitions during the study time.
Unlike the APC, which assumes a linear rate change over time, the AAPC assumes that the change in age-adjusted rates is constant within each joinpoint but varies across different joinpoints.35 When there are no significant trend transitions, the AAPC is similar to the APC. The AAPC measure is a more reliable way to compare two groups over a similar time period than the APC measure. This is because it takes into account all significant changes in trend between the joinpoints for each group.35 The joinpoint analysis was conducted using the joinpoint software provided by the US National Cancer Institute's Surveillance Research Program (Version 4.9.0.1).36
Ethics approval
The study was approved by the Justice Human Research Ethics Committee (reference, C.F./18/22468) and the Human Ethics Advisory Group (2022-23605-29220-3), School of Population and Global Health, University of Melbourne.
Role of funding source
The funding agency had no role in the study design, data collection, data analysis, interpretation, or writing of the report.
Results
Table 1 shows the total number of suicides between 2006 and 2019 based on countries of origin. It also identifies countries that accounted for 50% of migrants' suicide from their respective regions within Australia. From the total sample of 36,086, about 79% were born in Australia, 8% were born in English-speaking countries, and 13% were from other regions. The ASR of Australian-born persons was 18.2 per 100,000. Amongst migrants, those from Oceania countries had the highest suicide rate of 14.3 per 100,000, followed by migrants from English-speaking countries and European regions.
Table 1.
Suicide in Australia between 2006 and 2019 (by countries of origin).
| Region | Total number of suicidea | Average suicide rate per 100,000 | Countries contributing at least 50% of migrant suicides in Australia (Chronological order) |
|---|---|---|---|
| Australia | 28,520 | 18.2 (18.0, 18.4) | Australia |
| English-speaking countries (ESC) | 3010 | 13.0 (12.4, 13.5) | New Zealand, England, Scotland |
| European region (excluding ESC) | 2113 | 12.4 (11.5, 13.3) | Germany, Italy, Netherlands, Poland, Croatia |
| Asia | 1633 | 7.2 (6.8, 7.5) | China, India, Vietnam, Korea |
| Africa (excluding ESC) | 261 | 11.6 (10.1, 13.0) | Zimbabwe, Ethiopia, Sudan, Mauritius |
| South and Central America (excluding ESC) | 131 | 8.6 (6.9, 10.3) | Chile, Argentina, Columbia, Brazil |
| Oceania (excluding ESC) | 221 | 14.3 (12.1, 16.5) | Fiji, Papa New Guinea, Samoa |
| Middle East | 197 | 6.0 (5.1, 6.9) | Iran, Turkey, Lebanon |
| Total | 36,086 |
Including cases with a known country of birth, where Australia was noted as a usual country of residence.
Table 2 shows the IRR of suicide in male and female migrants with reference to their Australian-born counterparts. Male migrants from all categories had a lower risk of suicide compared to Australian-born males. Female migrants from European, Asian, South and Central American, African, and Middle Eastern countries had a lower risk of suicide relative to Australian-born females. There was insufficient evidence to reject the null hypothesis that the suicide risk for females from Oceania countries was not different from their Australian-born counterparts.
Table 2.
Negative binomial regression models assessing relative risk of suicide of migrant groups with reference to Australian-born.
| Suicides |
IRR |
P > z |
[95% Conf. interval] |
Suicides |
IRR |
P > z |
[95% Conf. interval] |
|---|---|---|---|---|---|---|---|
| Males (Model 1) | Females (Model 2) | ||||||
| Countries of origin | Countries of origin | ||||||
| Australia | Reference | Australia | Reference | ||||
| English-speaking countries | 0.73 | <0.001 | 0.68, 0.79 | English-speaking countries | 0.66 | <0.001 | 0.61, 0.71 |
| Europea | 0.90 | 0.01 | 0.84, 0.98 | Europea | 0.90 | 0.03 | 0.82, 0.99 |
| Asia | 0.33 | <0.001 | 0.3, 0.36 | Asia | 0.65 | <0.001 | 0.60, 0.71 |
| Africaa | 0.66 | <0.001 | 0.57, 0.77 | Africaa | 0.59 | <0.001 | 0.46, 0.76 |
| South & Central America | 0.50 | <0.001 | 0.4, 0.61 | South & Central America | 0.47 | <0.001 | 0.33, 0.68 |
| Oceaniaa | 0.72 | <0.001 | 0.61, 0.85 | Oceaniaa | 0.79 | 0.09 | 0.60, 1.03 |
| Middle East | 0.40 | <0.001 | 0.34, 0.47 | Middle East | 0.28 | <0.001 | 0.21, 0.38 |
| Age groups | Age groups | ||||||
| 15–24 | Reference | 15–24 | Reference | ||||
| 25–34 | 1.14 | 0.02 | 1.02, 1.26 | 25–34 | 1.21 | <0.001 | 1.13, 1.31 |
| 35–44 | 1.17 | 0.003 | 1.05, 1.30 | 35–44 | 1.43 | <0.001 | 1.33, 1.54 |
| 45–54 | 1.15 | 0.009 | 1.04, 1.28 | 45–54 | 1.46 | <0.001 | 1.35, 1.57 |
| 55–64 | 1.09 | 0.11 | 0.98, 1.21 | 55–64 | 1.22 | <0.001 | 1.12, 1.32 |
| 65–74 | 0.94 | 0.29 | 0.84, 1.05 | 65–74 | 0.91 | 0.06 | 0.83, 1.01 |
| 75 and above | 1.07 | 0.26 | 0.95, 1.20 | 75 and above | 1.36 | <0.001 | 1.24, 1.5 |
| Years | Years | ||||||
| 2006 | 1.00 | 2006 | Reference | ||||
| 2007 | 1.06 | 0.41 | 0.92, 1.23 | 2007 | 1.06 | 0.37 | 0.94, 1.19 |
| 2008 | 1.14 | 0.09 | 0.98, 1.31 | 2008 | 0.98 | 0.71 | 0.86, 1.1 |
| 2009 | 1.15 | 0.06 | 1.00, 1.33 | 2009 | 1.06 | 0.33 | 0.94, 1.2 |
| 2010 | 1.05 | 0.47 | 0.91, 1.22 | 2010 | 1.03 | 0.60 | 0.92, 1.18 |
| 2011 | 0.99 | 0.90 | 0.86, 1.14 | 2011 | 0.99 | 0.83 | 0.87, 1.11 |
| Suicides | IRR | P > z | [95% Conf. interval] | Suicides | IRR | P > z | [95% Conf. interval] |
| Males (Model 1) | Females (Model 2) | ||||||
| 2012 | 1.06 | 0.45 | 0.92, 1.22 | 2012 | 1.1 | 0.11 | 0.98, 1.24 |
| 2013 | 1.04 | 0.57 | 0.9, 1.2 | 2013 | 1.14 | 0.02 | 1.02, 1.28 |
| 2014 | 1.1 | 0.19 | 0.95, 1.26 | 2014 | 1.18 | 0.01 | 1.05, 1.33 |
| 2015 | 1.19 | 0.02 | 1.03, 1.37 | 2015 | 1.25 | 0.00 | 1.11, 1.4 |
| 2016 | 1.05 | 0.51 | 0.91, 1.21 | 2016 | 1.14 | 0.03 | 1.01, 1.27 |
| 2017 | 1.13 | 0.09 | 0.98, 1.3 | 2017 | 1.24 | 0.00 | 1.11, 1.39 |
| 2018 | 1.11 | 0.13 | 0.97, 1.28 | 2018 | 1.16 | 0.01 | 1.04, 1.3 |
| 2019 | 1.13 | 0.08 | 0.98, 1.3 | 2019 | 1.15 | 0.01 | 1.03, 1.29 |
Exluding English-speaking countries.
To investigate variation in suicide patterning across migrant groups, we examined rates relative to migrants from English-speaking countries (Table 2). Male migrants from Asia, South and Central America and the Middle East had a lower suicide risk than their male counterparts from English-speaking countries. For females, European migrants had 30% more suicide risk than females from English-speaking countries. There was insufficient evidence to reject the null hypothesis that there is no difference in the suicide risk of females from other countries or origins (except the Middle East) compared to that of their English-speaking counterparts.
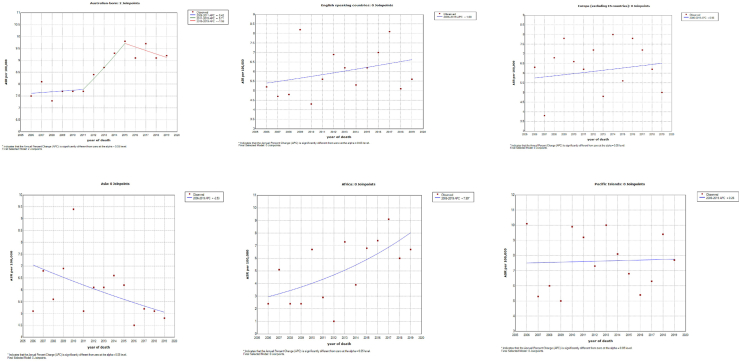
Table 3 shows the average age-standardised rates of both Australian-born and Australian migrant men and women based on their countries of origin. Additionally, the table provides AAPC measures for each group. Overall, we found that most groups showed no significant trend transitions during the study period (2006–2013), as indicated by the AAPC measures based on 0 joinpoints (see Figs. 1 and 2). The only exception was observed in the suicide trends of Australian-born females, where we identified two significant trend transitions that occurred in 2006–2011 and 2012–2016 (refer to Fig. 2 for details).
Table 3.
Negative binomial regression models assessing relative risk of suicide of migrant groups with reference to migrants from English-speaking countries.
| Suicides |
IRR |
P > z |
[95% Conf. interval] |
Suicides |
IRR |
P > z |
[95% Conf. interval] |
|---|---|---|---|---|---|---|---|
| Males (Model 1) | Females (Model 2) | ||||||
| Countries of origin | Countries of origin | ||||||
| English-speaking countries | Reference | English-speaking countries | Reference | ||||
| Europea | 1.18 | <0.001 | 1.09, 1.28 | Europe | 1.28 | 0.00 | 1.13, 1.14 |
| Asia | 0.45 | <0.001 | 0.41, 0.50 | Asia | 1.06 | 0.35 | 0.94, 1.19 |
| Africaa | 0.93 | 0.32 | 0.79, 1.08 | Africa | 0.92 | 0.55 | 0.71, 1.20 |
| South & Central America | 0.71 | 0.001 | 0.58, 0.87 | South & Central America | 0.75 | 0.13 | 0.52, 1.09 |
| Oceaniaa | 1.03 | 0.74 | 0.87, 1.21 | Oceaniaa | 1.25 | 0.12 | 0.95, 1.66 |
| Middle East | 0.56 | <0.001 | 0.48, 0.67 | Middle East | 0.44 | 0.00 | 0.32, 0.61 |
| Age groups | Age groups | ||||||
| 15–24 | Reference | 15–24 | Reference | ||||
| 25–34 | 0.90 | 0.11 | 0.79, 1.03 | 25–34 | 1.14 | 0.19 | 0.94, 1.40 |
| 35–44 | 0.91 | 0.16 | 0.8, 1.04 | 35–44 | 1.36 | 0.00 | 1.12, 1.65 |
| 45–54 | 0.94 | 0.36 | 0.83, 1.07 | 45–54 | 1.46 | 0.00 | 1.20, 1.77 |
| 55–64 | 1.01 | 0.89 | 0.89, 1.15 | 55–64 | 1.29 | 0.01 | 1.05, 1.57 |
| 65–74 | 0.96 | 0.61 | 0.84, 1.11 | 65–74 | 1.11 | 0.34 | 0.89, 1.38 |
| 75 and above | 1.18 | 0.02 | 1.03, 1.36 | 75 and above | 1.77 | 0.00 | 1.43, 2.19 |
| Years | Years | ||||||
| 2006 | 1.00 | 2006 | Reference | ||||
| 2007 | 1.08 | 0.40 | 0.90, 1.29 | 2007 | 1.02 | 0.91 | 0.78, 1.32 |
| 2008 | 1.17 | 0.08 | 0.98, 1.40 | 2008 | 1.00 | 1.00 | 0.77, 1.30 |
| 2009 | 1.22 | 0.03 | 1.03, 1.46 | 2009 | 1.22 | 0.13 | 0.94, 1.57 |
| 2010 | 1.02 | 0.81 | 0.85, 1.23 | 2010 | 1.11 | 0.42 | 0.86, 1.44 |
| 2011 | 1.00 | 0.97 | 0.84, 1.19 | 2011 | 0.88 | 0.36 | 0.68, 1.15 |
| 2012 | 1.03 | 0.70 | 0.87, 1.23 | 2012 | 1.07 | 0.57 | 0.84, 1.38 |
| Suicides | IRR | P > z | [95% Conf. interval] | Suicides | IRR | P > z | [95% Conf. interval] |
| Males (Model 1) | Females (Model 2) | ||||||
| 2013 | 1.01 | 0.90 | 0.85, 1.21 | 2013 | 1.12 | 0.37 | 0.87, 1.44 |
| 2014 | 1.04 | 0.67 | 0.87, 1.24 | 2014 | 1.03 | 0.81 | 0.80, 1.33 |
| 2015 | 1.16 | 0.10 | 0.97, 1.38 | 2015 | 1.09 | 0.51 | 0.85, 1.40 |
| 2016 | 1.00 | 0.97 | 0.84, 1.19 | 2016 | 0.99 | 0.93 | 0.77, 1.27 |
| 2017 | 1.03 | 0.74 | 0.87, 1.22 | 2017 | 1.10 | 0.43 | 0.86, 1.41 |
| 2018 | 1.03 | 0.71 | 0.87, 1.23 | 2018 | 0.98 | 0.90 | 0.77, 1.26 |
| 2019 | 1.07 | 0.46 | 0.9, 1.27 | 2019 | 0.99 | 0.95 | 0.77, 1.27 |
Excluding English-speaking countries.
Fig. 1.
AAPC graphs showing suicide trends in males across migrant groups.
Fig. 2.
AAPC graphs showing suicide trends in females across migrant groups.
To identify high-risk groups for suicide, we used the ASR and AAPC measures in combination, focusing on one of the following three possibilities: 1) a high ASR that increases over time, 2) a low ASR that increases over time, or 3) a high ASR that remains consistent over time (see Table 4). Australian-born males have the highest average ASR (27.2 per 100,000). The suicide trends of Australian-born males have also increased between 2006 and 2019 by 1.8 times, making them a high-risk group. Male migrants from Oceania countries had the highest suicide rates (20.4 per 100,000) among all migrant groups, which did not show significant changes during the study period (AAPC 1.0). Similarly, male migrants from African countries demonstrated relatively large ASR (18.0 per 100,000) compared to other groups, but their suicide rates did not change over the study duration (AAPC −0.4). In contrast, male migrants from Asian countries not only had lower suicide rates compared to their Australian-born and other migrant counterparts, but their rates also showed a declining trend.
Table 4.
Age-standardised suicide rate and AAPC measure (2006–2019).
| Suicide | Age-standardised rates per 100,000 | Average annual percentage change | P-value | |
|---|---|---|---|---|
| Males (2006–2019) | ||||
| Australian-born | 21,929 | 27.7 (27.3, 28) | 1.8 (1.1–2.5) | <0.001 |
| English-speaking countries | 2307 | 20.1 (19.1, 21.1) | 1.2 (−0.1, 2.5) | 0.06 |
| Europea | 1616 | 18.1 (16.5, 19.7) | −1.0 (−3.0, 1.0) | 0.29 |
| Asia | 1021 | 8.5 (8.0, 9.1) | −1.0 (−3.4, 1.5) | 0.40 |
| Africaa | 200 | 18.0 (15.4, 20.6) | −0.4 (−5.5, 4.9) | 0.86 |
| South & Central Americaa | 102 | 13.1 (10.1, 16.1) | −1.3 (−5.6, 3.3) | 0.55 |
| Oceaniaa | 167 | 20.4 (16.9, 24.0) | 1.0 (−3.6, 5.8) | 0.65 |
| Middle East | 156 | 10.2 (8.5, 12.0) | −1.4 (−7.1, 4.6) | 0.60 |
| Females (2006–2019) | ||||
| Australian-born | 6591 | 8.5 (8.3, 8.8) | 1.4 (−0.7, 3.6) | 0.20 |
| English-speaking countries | 703 | 6.0 (5.4, 6.5) | 1.6 (−1.2, 4.5) | 0.23 |
| Europea | 497 | 6.5 (5.6, 7.4) | 1.0 (−2.3, 4.3) | 0.52 |
| Asia | 612 | 5.7 (5.3, 6.2) | −2.5 (−5.1, 0.1) | 0.06 |
| Africaa | 61 | 5.3 (3.9, 6.6) | 8.0 (1.4, 15.0) | 0.02 |
| South & Central Americaa | 29 | 3.7 (2.2, 5.1) | N.A.b | – |
| Oceaniaa | 54 | 7.5 (5.2, 9.8) | 0.3 (−3.6, 4.3) | 0.89 |
| Middle East | 41 | 2.2 (1.5, 3.0) | N.A.b | – |
Excluding English-speaking countries.
AAPC could not be calculated.
A similar trend was observed for females, where Australian-born females show the highest suicide rates compared to migrants from other countries. Fig. 2 shows that after a significant increase in Australian-born female suicide death between the year 2011 and 2015, it is now showing a declining trend. The most noticeable change in suicide rates was observed in female migrants from African countries, which increased by 8% between 2006 and 2019. While their ASR (5.3 per 100,000) is low relative to other migrant groups, the rapid increase in the last 13 years can make them high-risk. Similar to males, female migrants from Oceania countries also have high ASR, with no significant change over time. Suicide rates for females from Asian countries showed a lower ASR (5.3 per 100,000), with a decline of 2.5% during the study period.
Discussion
Our study provides current evidence on suicide mortality of Australian residents based on their countries of origin. Given the heterogeneity of Australian migrant population groups, we reported suicide rates, risk and trends based on countries of origin as well as by sex. We found that suicide mortality in migrants from Oceania countries is of concern. Not only are their suicide rates the highest amongst other migrant groups but there has also been little to no change in their suicide rates across the study period (2006–2019). This was similarly observed in males from African countries. An increasing suicide trend was also noted in female African migrants during the study period. Furthermore, an increasing trend in suicide rates of Australian-born males was also noted during the study time period—a pattern not observed in Australian-born females. Overall, the suicide rates and trends of Australian-born and migrants from English-speaking countries showed similar results. We noted that while male migrants from non-English-speaking countries have significantly lower suicide risk compared to their counterparts from English-speaking countries, this was not the case for females, where except for the Middle East, all migrants from non-English-speaking countries had similar or higher rates compared to females from English-speaking countries.
Individuals from Oceania countries, also known as Pacific Islands, have one of the highest suicide mortality rates in the world.37,38 The country of origin phenomenon may, to some extent, explain their higher suicide rates in Australia as a migrant; however, more research is needed to understand whether migrating to Australia exacerbates or lowers the risk of suicide in this group. Our study also noted that the suicide trend of Oceania migrants (both males and females) has not changed since 2006. The consistently high suicide rate in this group is indicative that the current interventions may not have been effective for them. As climate change continues to impact many small islands in the Pacific region, we can anticipate an increase in migration from these islands to countries like Australia, New Zealand and the USA.39 Australia also offers special migration streams for individuals from Pacific Island to address the Australian labour force shortage.40 This highlights the political and strategic importance of this region to Australia. It is, therefore, important to understand what other factors (apart from country of origin) are associated with higher suicide rates of Oceania migrants and identify tailored suicide prevention strategies for this group.
African migrants are a relatively new migrant group in Australia, with the majority migrating on humanitarian visas from 2006 onwards, noting that earlier waves of this group arrived in the 1980s.41 Given that refugee status is the single most important predictor of PTSD and suicidal ideation, it is possible that this may explain the higher suicide rates in this group.17 Our study observed a significant increase in female suicide mortality in this group between 2006 and 2019. Despite having a lower average ASR, an eight-fold increase in the suicide rate among female migrants from Africa in just 13 years indicates an emerging issue that warrants further research. A qualitative study from South Australia42 has identified poor mental health and suicide deaths of young African migrants stemming from intergenerational conflicts with their parents. Notably, young African females were particularly vulnerable to navigating these differences. Although our study did not focus on the suicide mortality of young migrants, future studies should investigate whether being a young migrant is a risk factor for suicide mortality in migrant groups. In a recent Australian study, Mihtsintu et al.43 examined attitudes and knowledge about suicide among African migrants and showed that negative views on suicide and a limited connection between community resources and support services might impede their access to lifesaving interventions. Considering the alarming increase in suicide mortality within this group, concerted efforts are needed to address suicide mortality among African migrants.
Our study noted some elevated parameters related to female suicide in migrant groups (higher risk or increasing suicide rate over time, as discussed above), which can be indicative of an emerging problem. For example, migrant females from Oceania, European, and Asian countries exhibited an elevated or similar risk of suicide compared to migrant females from English-speaking countries. Similarly, Oceania and European female migrants also had comparable suicide risk to Australian-born females. Recognising this pattern and identifying factors contributing to this elevated risk is important. We speculate that acculturation stress may explain some of the elevated suicide risks of female migrants. Previous literature has linked migrant women's experience of acculturation stress to feelings of loneliness,44 loss of family ties and social networks,45 intimate partner violence,46 and marital conflict47; all of these factors are associated with poor mental health and increased risk of suicidal behaviours. These findings underscore the importance of adopting a gender lens when developing suicide prevention initiatives for the migrant population. Furthermore, in some migrant groups, mental health service use may be limited due to the stigma around mental health48 or negative attitudes towards suicide.43 Therefore, It is important to incorporate culturally competent approaches in developing effective suicide prevention programs.
Our study noted the low average ASR of Asian migrants with a substantial decline in female suicide rates over time. A declining trend was also noted in Asian males. We argue that declining trends may partly be explained by their countries of origin also having lower suicide rates. This was similarly noted in other studies from Australia26,27 and England,49, 50, 51 where migrants from Asian countries tend to show lower suicide rates than the host population. Anikeeva et al. (2015) also noted a decline in suicide rates of Asian migrants between 1981 and 2007.27 Australia's migration from Asia has changed from refugees in the early '70s to predominately skilled and family migrants since 2000.52 We speculate that the decline may be explained by the "healthy migrant effect"15 from newer Asian migrants, who are often selected based on age, optimal health, high English proficiency, and matching skills with the Australian labour market. However, it's important to recognise that not all refugees or skilled migrants have an easy transition to Australia. Studies have also shown that the mental health of migrants worsens over time in their respective host countries.6 Considering that future studies should monitor suicide trends among this group and identify risk and protective factors of suicide in Asian migrants.
European migrants from non-English-speaking countries have always been noted as high-risk migrant groups in England and Sweden,49,53 including Australia26,27,54 continued to show high ASR with some decline over time. Despite being one of the oldest migrant groups in Australia, their steady suicide rates suggest that current prevention initiatives have not been effective for this group.
Strengths and limitations
Our study provides the latest insights into suicide mortality among migrant groups in Australia using national-level data, making it useful for policy and program planning. We note that earlier data from 2001 to 2005 is not included due to missing information on countries of birth. The study may underestimate suicide cases due to misclassification or delayed classification. However, recent improvements by the Australian Bureau of Statistics in revising the cause of death for open coroners' cases have reduced underreporting of suicides, especially after 2006.55 We also performed sensitivity analysis examining cases of 'undetermined intent' with respect to the country of birth. We found no such evidence that country of birth was associated with 'undetermined intent' in the NCIS data; therefore, we restrict our analysis to cases classified as intentional self-harm in the NCIS data.
The small number of cases prevented us from analysing country-specific suicide rates and trends, and grouping countries based on regional proximity may not reflect the diversity within sub-regions and cultures. As our research focused on countries of origin, we were unable to consider indigenous status. We acknowledge that indigenous status is a significant predictor of suicide mortality, and future research should investigate how the intersection of migration and indigenous status can impact suicide mortality in Australia.
At present, coroners do not regularly collect migration-related data, such as ethnicity, language skills proficiency, visa status, and length of residence. These variables are known to be linked to poor mental health, acculturation stress, and, in turn, suicidal behaviour. To better understand suicide risk factors in migrant communities, we argue that national data collection should capture ethnicity and migration-related information. We support calls for police and coronial data collection to report ethnicity and migration-related data to enhance our knowledge of high-risk groups for suicide in migrant communities across Australia.
Conclusion
Our study provided evidence that suicide mortality among males and females varies across different migrant groups in Australia. To effectively tackle suicidality in Australia, further research is required to identify the factors contributing to suicide among Australian migrants and to develop tailored suicide prevention strategies. Given the substantial changes in Australia's population demographics due to migration over the years, and the likelihood of further changes, evaluating suicide mortality over time is crucial.
Contributors
Dr Humaira Maheen had complete access to all the data in the study and assumed responsibility for maintaining the data's integrity and ensuring the accuracy of the data analysis. Additionally, Dr Maheen contributed to the conceptualisation, methodology, formal analysis, and initial drafting of the manuscript. Dr Tania King contributed to the analysis process and provided critical revisions to the manuscript for important intellectual content.
Data sharing statement
The datasets analysed during the current study are not publicly available due to confidentiality reasons. The corresponding author can provide deidentified aggregated data per the NCIS guidelines to someone authorised by the Victorian Justice Human Research Ethics Committee and NCIS for access to the data.
Declaration of interests
All authors declare that they have no competing interests.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100845.
Appendix A. Supplementary data
References
- 1.Davies A.A., Basten A., Frattini C. Migration: a social determinant of the health of migrants. Eurohealth. 2009;16(1):10–12. [Google Scholar]
- 2.Ingleby D. Ethnicity, migration and the 'social determinants of health' agenda∗. Psychosoc Interv. 2012;21(3):331–341. [Google Scholar]
- 3.Department of Home Affairs Australian Government Who needs health examinations 2022. https://immi.homeaffairs.gov.au/help-support/meeting-our-requirements/health/who-needs-health-examinations Available from:
- 4.Salas-Wright C.P., Vaughn M.G., Goings T.C., Miller D.P., Schwartz S.J. Immigrants and mental disorders in the United States: new evidence on the healthy migrant hypothesis. Psychiatry Res. 2018;267:438–445. doi: 10.1016/j.psychres.2018.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dhadda A., Greene G. 'The healthy migrant effect' for mental health in England: propensity-score matched analysis using the EMPIRIC survey. J Immigr Minor Health. 2018;20:799–808. doi: 10.1007/s10903-017-0570-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elshahat S., Moffat T., Newbold K.B. Understanding the healthy immigrant effect in the context of mental health challenges: a systematic critical review. J Immigr Minor Health. 2021;24(6):1564–1579. doi: 10.1007/s10903-021-01313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nørredam M. Migration and health: exploring the role of migrant status through register-based studies. Dan Med J. 2015;62(4) [PubMed] [Google Scholar]
- 8.Dean J.A., Wilson K. 'Education? It is irrelevant to my job now. It makes me very depressed ...': exploring the health impacts of under/unemployment among highly skilled recent immigrants in Canada. Ethn Health. 2009;14(2):185–204. doi: 10.1080/13557850802227049. [DOI] [PubMed] [Google Scholar]
- 9.Disney L. The impact of employment on immigrant mental health: results from a national survey. Soc Work. 2021;66(2):93–100. doi: 10.1093/sw/swab005. [DOI] [PubMed] [Google Scholar]
- 10.Maheen H., King T. Employment-related mental health outcomes among Australian migrants: a 19-year longitudinal study. Aust N Z J Psychiatry. 2023 doi: 10.1177/00048674231174809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choy B., Arunachalam K., Gupta S., Taylor M., Lee A. Systematic review: acculturation strategies and their impact on the mental health of migrant populations. Public Health Pract. 2021;2 doi: 10.1016/j.puhip.2020.100069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai D.W., Li L., Daoust G.D. Factors influencing suicide behaviours in immigrant and ethno-cultural minority groups: a systematic review. J Immigr Minor Health. 2017;19(3):755–768. doi: 10.1007/s10903-016-0490-3. [DOI] [PubMed] [Google Scholar]
- 13.Voracek M., Loibl L.M. Consistency of immigrant and country-of-birth suicide rates: a meta-analysis. Acta Psychiatr Scand. 2008;118(4):259–271. doi: 10.1111/j.1600-0447.2008.01238.x. [DOI] [PubMed] [Google Scholar]
- 14.Spallek J., Reeske A., Norredam M., Nielsen S.S., Lehnhardt J., Razum O. Suicide among immigrants in Europe—a systematic literature review. Eur J Public Health. 2015;25(1):63–71. doi: 10.1093/eurpub/cku121. [DOI] [PubMed] [Google Scholar]
- 15.Kolves K., De Leo D. Are immigrants responsible for the recent decline in Australian suicide rates? Epidemiol Psychiatr Sci. 2015;24(3):241–248. doi: 10.1017/S2045796014000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ratkowska K.A., De Leo D. Suicide in immigrants: an overview. Open J Med Psychol. 2013;2:124–133. [Google Scholar]
- 17.Forte A., Trobia F., Gualtieri F., et al. Suicide risk among immigrants and ethnic minorities: a literature overview. Int J Environ Res Public Health. 2018;15(7):1438. doi: 10.3390/ijerph15071438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hovey J.D. Acculturative stress, depression, and suicidal ideation among Central American immigrants. Suicide Life Threat Behav. 2000;30(2):125–139. [PubMed] [Google Scholar]
- 19.Khawaja N.G., Milner K. Acculturation stress in South Sudanese refugees: impact on marital relationships. Int J Intercult Relat. 2012;36(5):624–636. [Google Scholar]
- 20.Yun S., Ahmed S.R., Hauson A.O., Al-Delaimy W.K. The relationship between acculturative stress and postmigration mental health in Iraqi refugee women resettled in San Diego, California. Community Ment Health J. 2021;57(6):1111–1120. doi: 10.1007/s10597-020-00739-9. [DOI] [PubMed] [Google Scholar]
- 21.Liebkind K., Jasinskaja-Lahti I. The influence of experiences of discrimination on psychological stress: a comparison of seven immigrant groups. J Community Appl Soc Psychol. 2000;10(1):1–16. [Google Scholar]
- 22.Kirmayer L.J. Suicide in cultural context: an ecosocial approach. Transcult Psychiatry. 2022;59(1):3–12. doi: 10.1177/13634615221076424. [DOI] [PubMed] [Google Scholar]
- 23.Friis R., Yngve A., Persson V. Review of social epidemiologic research on migrants' health: findings, methodological cautions, and theoretical perspectives. Scand J Soc Med. 1998;26(3):173–180. doi: 10.1177/14034948980260030601. [DOI] [PubMed] [Google Scholar]
- 24.Wood J., Newbold K.B. Provider perspectives on barriers and strategies for achieving culturally sensitive mental health services for immigrants: a Hamilton, Ontario case study. J Int Migr Integr. 2012;13:383–397. [Google Scholar]
- 25.Australian Bureau of Statistics . 2021. Cultural diversity: census. Australia.https://www.abs.gov.au/statistics/people/people-and-communities/cultural-diversity-census/latest-release Avaiable from: [Google Scholar]
- 26.Ide N., Kõlves K., Cassaniti M., De Leo D. Suicide of first-generation immigrants in Australia, 1974–2006. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1917–1927. doi: 10.1007/s00127-012-0499-4. [DOI] [PubMed] [Google Scholar]
- 27.Anikeeva O., Bi P., Hiller J.E., Ryan P., Roder D., Han G.-S. Trends in migrant mortality rates in Australia 1981–2007: a focus on the National Health Priority Areas other than cancer. Ethn Health. 2015;20(1):29–48. doi: 10.1080/13557858.2014.883368. [DOI] [PubMed] [Google Scholar]
- 28.NCIS National coronial information system 2001. https://www.ncis.org.au/ Available from:
- 29.Australian Bureau of Statistics . 2nd ed. 2016. 1269.0 - Standard Australian classification of countries (SACC)https://www.abs.gov.au/ausstats/abs@.nsf/0/C8B8914F6C683351CA25744D00818CED?opendocument Available from: [Google Scholar]
- 30.Australian Bureau of Statistics . 2012. Place of usual residence (PURP, IFPURP)https://www.abs.gov.au/websitedbs/censushome.nsf/home/statementspersonpurp?opendocument&navpos=430 Available from: [Google Scholar]
- 31.Khan T., Abimbola S., Kyobutungi C., Pai M. How we classify countries and people—and why it matters. BMJ Glob Health. 2022;7 doi: 10.1136/bmjgh-2022-009704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Australian Bureau of Statistics Migrant data metrics 2013. https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/3415.0Glossary12013?OpenDocument Available from:
- 33.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; 2011. Principles on the use of direct age-standardisation in administrative data collections Canberra.https://www.aihw.gov.au/getmedia/95237794-4b77-4683-9f00-77c4d33e0e7c/13406.pdf.aspx?inline=true Available from: [Google Scholar]
- 34.Ahmad O.B., Boschi-Pinto C., Lopez A.D., Murray C.J., Lozano R., Inoue M. World Health Organization; Geneva: 2001. Age standardisation of rates: a new WHO standard. 9(10):1–14. [Google Scholar]
- 35.Clegg L.X., Hankey B.F., Tiwari R., Feuer E.J., Edwards B.K. Estimating average annual per cent change in trend analysis. Statistics Med. 2009;28(29):3670–3682. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.NIH . NIH; 2004. National Cancer Institute.https://surveillance.cancer.gov/ Available from: [Google Scholar]
- 37.Mathieu S., De Leo D., Koo Y.W., Leske S., Goodfellow B., Kõlves K. Suicide and suicide attempts in the Pacific Islands: a systematic literature review. Lancet Reg Health West Pac. 2021;17 doi: 10.1016/j.lanwpc.2021.100283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease study 2016. BMJ. 2019;364 doi: 10.1136/bmj.l94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Constable A.L. Climate change and migration in the Pacific: options for Tuvalu and the Marshall Islands. Reg Environ Change. 2017;17(4):1029–1038. [Google Scholar]
- 40.Australian Government . 2022. Pacific Australia labour mobility (PALM)https://www.palmscheme.gov.au/ Available from: [Google Scholar]
- 41.Jakubowicz A. 2010. Australia's migration policies: African dimensions.https://humanrights.gov.au/our-work/african-australians-project-australias-migration-policies-african-dimensionsaustralias Available from: [Google Scholar]
- 42.Mwanri L., Okyere E., Pulvirenti M. Intergenerational conflicts, cultural restraints and suicide: experiences of young African people in Adelaide, South Australia. J Immigr Minor Health. 2018;20:479–484. doi: 10.1007/s10903-017-0557-9. [DOI] [PubMed] [Google Scholar]
- 43.Mihtsintu Y., Yohannes K., Gebrat A. Knowledge, attitudes and practices towards suicide among immigrants from the horn of Africa in Victoria, Australia. Int J Soc Psychiatry. 2023 doi: 10.1177/00207640231167075. [DOI] [PubMed] [Google Scholar]
- 44.Yakushko O., Watson M., Thompson S. Stress and coping in the lives of recent immigrants and refugees: considerations for counselling. Int J Adv Couns. 2008;30(3):167–178. [Google Scholar]
- 45.Lumley M., Katsikitis M., Statham D. Depression, anxiety, and acculturative stress among resettled Bhutanese refugees in Australia. J Cross Cult Psychol. 2018;49(8):1269–1282. [Google Scholar]
- 46.O'Connor M., Colucci E. Exploring domestic violence and social distress in Australian-Indian migrants through community theatre. Transcult Psychiatry. 2016;53(1):24–44. doi: 10.1177/1363461515599327. [DOI] [PubMed] [Google Scholar]
- 47.Negy C., Hammons M.E., Reig-Ferrer A., Marino Carper T. The importance of addressing acculturative stress in marital therapy with Hispanic immigrant women. Int J Clin Health Psychol. 2010;10(1):5–21. [Google Scholar]
- 48.Slewa-Younan S., Rioseco P., Guajardo M.G.U., Mond J. Predictors of professional help-seeking for emotional problems in Afghan and Iraqi refugees in Australia: findings from the building a new life in Australia database. BMC Public Health. 2019;19(1):1485. doi: 10.1186/s12889-019-7673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shah A., Lindesay J., Dennis M. Suicides by country of birth groupings in England and Wales: age-associated trends and standardised mortality ratios. Soc Psychiatry Psychiatr Epidemiol. 2011;46(3):197–206. doi: 10.1007/s00127-010-0188-0. [DOI] [PubMed] [Google Scholar]
- 50.McKenzie K., Bhui K., Nanchahal K., Blizard B. Suicide rates in people of South Asian origin in England and Wales: 1993–2003. Br J Psychiatry. 2008;193(5):406–409. doi: 10.1192/bjp.bp.107.042598. [DOI] [PubMed] [Google Scholar]
- 51.Bhui K.S., Dinos S., McKenzie K. Ethnicity and its influence on suicide rates and risk. Ethn Health. 2012;17(1–2):141–148. doi: 10.1080/13557858.2011.645151. [DOI] [PubMed] [Google Scholar]
- 52.Scanlon Foundation Research Institute . 2021. Australian migration and population dashboard.https://scanloninstitute.org.au/publications/migrationdashboard Available from: [Google Scholar]
- 53.Westman J., Sundquist J., Johansson L.M., Johansson S.-E., Sundquist K. Country of birth and suicide: a follow-up study of a national cohort in Sweden. Arch Suicide Res. 2006;10(3):239–248. doi: 10.1080/13811110600582471. [DOI] [PubMed] [Google Scholar]
- 54.Pavloviæ E., Marušiè A. Suicide in Croatia and in Croatian immigrant groups in Australia and Slovenia. Croat Med J. 2001;42:669–672. [PubMed] [Google Scholar]
- 55.Australian Institute of Health and Welfare Deaths by suicide over time 2022. https://www.aihw.gov.au/suicide-self-harm-monitoring/data/deaths-by-suicide-in-australia/suicide-deaths-over-time Available from:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.