Abstract
Introduction:
Zimbabwe introduced human papillomavirus (HPV) vaccine nationally in May 2018, targeting multiple cohorts (girls aged 10–14 years) through a school-based vaccination campaign. One year later, the second dose was administered to the multiple cohorts concurrently with the first dose given to a new single cohort of girls in grade 5. We conducted cross-sectional surveys among health workers, school personnel, and community members to assess feasibility of implementation, training, social mobilization, and community acceptability.
Methods:
Thirty districts were selected proportional to the volume of the HPV vaccine doses delivered in 2018; two health facilities were randomly selected within each district. One health worker, school health coordinator, village health worker, and community leader were surveyed at each selected health facility and surrounding area during January-February 2020, using standard questionnaires. Descriptive analysis was completed across groups.
Results:
There were 221 interviews completed. Over 60% of health workers reported having enough staff to carry out vaccination sessions in schools while maintaining routine vaccination services in health facilities. All school health coordinators felt the HPV vaccine should be delivered in schools in the future. Knowledge of the correct target cohort eligibility decreased from 91% in 2018 to 50% in 2020 among health workers. Understanding of HPV infection and use of HPV vaccine for cervical cancer prevention was above 90% for all respondents. Forty-two percent of respondents reported hearing rumors about the HPV vaccine, primarily regarding infertility and safety.
Conclusions:
Findings demonstrate the presence of highly knowledgeable staff at health facilities and schools, strong community acceptance, and a school-based HPV program considered feasible to implement in Zimbabwe. However, misunderstandings regarding target eligibility and rumors persist, which can impact vaccine uptake and coverage. Continued social mobilization efforts to maintain community demand and training on eligibility were recommended. Integration, partnerships, and resource mobilization are also needed to ensure program sustainability.
Keywords: Human papillomavirus (HPV) vaccine, Vaccine introduction, Multiple cohort, Zimbabwe, School-based vaccination
1. Introduction
In May 2018, the Government of Zimbabwe Ministry of Health, in collaboration with the Ministry of Education, introduced the HPV vaccine nationwide following a successful pilot program in two districts [1,2]. In accordance with the World Health Organization (WHO) recommendations, the campaign targeted multiple cohorts during the first year of the introduction for the greatest public health impact [3]. The primarily school-based campaign targeted all girls aged 10–14 years with the first dose of the HPV vaccine. The second dose was administered to this cohort one year later, concurrently with a first dose being administered to a new single cohort of all grade 5 girls in-school and out-of-school girls aged 10 years [4]. From 2020 onward, the single cohort (grade 5 girls in-school and out-of-school girls aged 10 years) will receive the first dose annually at the same time as the previous cohort’s second dose.
The first vaccination campaign in May 2018 achieved 83% administrative coverage for the first dose targeting multiple cohorts [5] through primarily school-based vaccination sessions taking place over one week. According to WHO/United Nations International Children’s Emergency Fund (UNICEF) estimates, the second vaccination campaign in May 2019 achieved 67% coverage for the second dose of the multiple cohort and 91% coverage for the first dose of the single cohort [5]. Both campaigns were carried out by teams of health workers in partnership with school health coordinators (teachers from each school trained in basic health topics); village health workers helped identify out-of-school girls [4,6]. A stand-alone training was provided to health workers, school health coordinators and village health workers prior to the 2018 campaign only. Eligibility for vaccination was determined by school health coordinators and health workers, using the information on grade, current age, or birth year. Strong political commitment and good cooperation between the health and education sectors contributed to high administrative coverage; however, challenges with transitioning between cohorts, funding shortages, and concerns about sustainability were reported [30].
Evaluating program feasibility, assessing knowledge of HPV and the HPV vaccine, and understanding community and stakeholder acceptability can support program improvements to maintain community demand and improve vaccine uptake. We conducted feasibility and acceptability surveys among health workers, school personnel, and community members to understand their perceptions of community awareness, implementation, training, and social mobilization. Lessons, best practices, and challenges from the community-level can inform the programmatic success of Zimbabwe’s HPV vaccination program in the future. Experiences in Zimbabwe, a resource-constrained and complex environment with economic, infrastructure, and healthcare access challenges, may be useful for HPV vaccine introduction planning in similar settings.
2. Methods
Cross-sectional surveys were administered to health workers, school health coordinators, village health workers, and community leaders in January and February 2020. The surveys took place after two HPV vaccination campaigns were completed in Zimbabwe, in May 2018 and May 2019.
2.1. Sampling
We used a two-stage cluster sampling approach for the survey, following WHO coverage survey guidance [7] and the costing evaluation for a simultaneously-administered nationally-representative HPV vaccination program at the district and health facility level. We stratified districts by urban or rural and made selections, using probability proportional to size, with the volume of the HPV vaccine doses delivered in the 2018 campaign as the size variable. Thirty districts were selected; two health facilities were randomly selected within each district, totaling 60 health facilities. Within each health facility, we selected one health worker purposively based on involvement with HPV vaccination in that setting. Data collectors selected one school health coordinator, one village health worker, and one community leader within the health facility catchment area, using convenience sampling. Health facility staff assisted data collectors to identify appropriate respondents who were involved with the HPV vaccination program. This allowed data collectors to interview a range of participants from each sampled health facility’s catchment area within a suitable time frame at each geographic location.
2.2. Data collection
Surveys included questions on respondent demographics, vaccine delivery and program feasibility, understanding of target age and eligibility, knowledge of HPV and the HPV vaccine, social mobilization, community acceptability, and program challenges. Data collectors interviewed respondents, using standard questionnaires available on android-based electronic devices (e.g. tablets) via Open Data Kit (ODK) software (www.opendatakit.org). Data collectors administered village health worker and community leader questionnaires in Shona and Ndebele languages, if needed. To the extent possible, translated terminology was standardized among data collectors during the training and field-testing process prior to data collection.
2.3. Data analysis
We analyzed data, using SAS version 9.4 (SAS Institute, Inc., Cary, North Carolina, USA) and calculated descriptive analysis (numbers and proportions) for all variables across each respondent group.
2.4. Ethical approval
The study was determined to be non-research by the CDC’s Human Subjects Office and the Medical Research Council of Zimbabwe issued a waiver. Oral informed consent was obtained by data collectors before conducting surveys and no personally identifiable information was collected.
3. Results
3.1. Respondent demographics
A total of 221 interviews were completed across the following respondent groups: health workers (56), school health coordinators (55), village health workers (55), and community leaders (55) (Table 1). Of the 55 schools visited, 46 (84%) were primary schools (grade 1–7). Among respondents, most health workers (75%), school health coordinators (62%), and village health workers (84%) were female, whereas 18% of the community leaders surveyed were female. Forty-five percent of the health workers interviewed were primary care nurses, 36% were registered general nurses, and others were nurses-in-charge (7%), community health nurses (7%), or other professions (6%). Almost all (98%) school personnel were school health coordinators. Community leaders were administrative (30%), political (20%), or religious leaders (6%), members of the health center committee (16%), or other influential community members (28%).
Table 1.
Demographics of the health workers, school health coordinators, village health workers, and community leaders surveyed for the HPV vaccination program feasibility and acceptability surveys, Zimbabwe, January–February 2020.
| Health workers* (N = 56) |
School health coordinators* (N = 55) |
Village health workers* (N = 55) |
Community leaders* (N = 55) |
|||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Type of school | ||||||||
| Primary (Grade 1–7) | – | – | 46 | (84) | – | – | – | – |
| Secondary (Form 1–5) | – | – | 9 | (16) | – | – | – | – |
| Gender | ||||||||
| Male | 14 | (25) | 21 | (38) | 9 | (16) | 45 | (82) |
| Female | 42 | (75) | 34 | (62) | 46 | (84) | 10 | (18) |
| Age of respondent | ||||||||
| Under 25 | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| 25–34 | 7 | (13) | 4 | (7) | 5 | (9) | 1 | (2) |
| 35–44 | 21 | (38) | 21 | (38) | 8 | (15) | 11 | (20) |
| 45–54 | 23 | (41) | 23 | (42) | 32 | (58) | 21 | (38) |
| 55 and over | 5 | (9) | 7 | (13) | 10 | (18) | 22 | (40) |
| Profession of respondent | ||||||||
| Primary Care Nurse | 25 | (45) | – | – | – | – | – | – |
| Registered General Nurse (RGN) | 20 | (36) | – | – | – | – | – | – |
| Nurse-in-charge/Sister-in-charge | 4 | (7) | – | – | – | – | – | – |
| Community Health Nurse | 4 | (7) | – | – | – | – | – | – |
| Other** | 3 | (5) | ||||||
| School Health Coordinator/School Health Master | – | – | 54 | (98) | – | – | – | – |
| School Administrator | – | – | 1 | (2) | – | – | – | – |
| Village Health Worker | – | – | – | – | 55 | (100) | – | – |
| Administrative representative (e.g. Councilor) | – | – | – | – | – | – | 15 | (30) |
| Influential community member (e.g. lead mother in women’s group) | – | – | – | – | – | – | 14 | (28) |
| Political community leader | – | – | – | – | – | – | 10 | (20) |
| Health Center Committee (HCC) chairperson or member | – | – | – | – | – | – | 8 | (16) |
| Religious community leader | – | – | – | – | – | – | 3 | (6) |
Five health facilities in the initial sample were not visited by data collectors because they had closed or did not participate in the HPV vaccination program.
Other includes midwife, environmental health technician, and primary counselor.
3.2. Feasibility of vaccine delivery
All school health coordinators surveyed felt the HPV vaccine should continue to be delivered in schools in the future. Among health workers, 66% reported having enough staff to conduct HPV vaccination in schools; 61% reported having enough staff to maintain routine immunization services in health facilities (Table 2). Many health workers (75%) and school health coordinators (53%) indicated that their workload had “somewhat or greatly increased”. Eighty percent of the health workers reported having adequate time for each vaccination session, and 77% reported acquiring additional support when needed.
Table 2.
Feasibility of the HPV vaccine delivery and its impact on workload, reported by the health workers and school health coordinators surveyed for the HPV vaccination program feasibility and acceptability surveys, Zimbabwe, January–February 2020.
| Health workers (N = 56) |
School health coordinators (N = 55) |
|||
|---|---|---|---|---|
|
|
|
|||
| n | (%) | n | (%) | |
| Felt HPV vaccine should be delivered in schools in the future | – | – | 55 | (100) |
| Reported having enough staff to carry out vaccination activities in schools during the most recent campaign (2019) | 37 | (66) | – | – |
| Reported having enough staff to maintain routine vaccination services in health facilities during the most recent campaign (2019) | 34 | (61) | – | – |
| Reported adequate amount of time for each vaccination session | 45 | (80) | – | – |
| Reported ability to get additional support when needed | 43 | (77) | – | – |
| Impact of the HPV vaccine introduction on workload | ||||
| Greatly or somewhat increased | 42 | (75) | 29 | (53) |
| No effect | 14 | (25) | 26 | (47) |
| Greatly or somewhat decreased | 0 | (0) | 0 | (0) |
Several programmatic challenges were identified by the respondents overall, including inadequate social mobilization activities or materials (28%), insufficient transportation of staff and supplies (26%) and inadequate training (18%). Challenges varied somewhat by respondent group (Table 3). The top three challenges reported by the health workers included transporting staff and supplies (38%), lack of funds for delivering the vaccine (34%), and staff shortages to conduct vaccination sessions (25%).
Table 3.
Challenges with the HPV vaccination program reported by the health workers, school health coordinators, village health workers, and community leaders surveyed for the HPV vaccination program feasibility and acceptability surveys, Zimbabwe, January–February 2020.
| Health workers (N = 56) |
School health coordinators (N = 55) |
Village health workers (N = 55) |
Community leaders (N = 55) |
|||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Reported biggest challenge related to the HPV program | ||||||||
| Transportation of staff and supplies (fuel shortages/cost, the lack of vehicles) | 21 | (38) | 9 | (16) | 14 | (25) | 13 | (24) |
| Lack of funds for delivering vaccine (health worker per diem, etc.) | 19 | (34) | 5 | (9) | 8 | (15) | 6 | (11) |
| Staff shortages to conduct vaccination sessions | 14 | (25) | 7 | (13) | 1 | (2) | 5 | (9) |
| Inadequate training | 9 | (16) | 12 | (22) | 14 | (25) | 4 | (7) |
| Inadequate social mobilization activities/materials | 9 | (16) | 20 | (36) | 15 | (27) | 17 | (31) |
| Lack of registers, tally sheets, cards, etc. | 8 | (14) | 5 | (9) | 4 | (7) | 2 | (4) |
| Increased workload | 5 | (9) | 3 | (5) | 1 | (2) | 0 | (0) |
| Community resistance | 5 | (9) | 16 | (29) | 9 | (16) | 7 | (13) |
| Tracking girls/recording/reporting | 4 | (7) | 2 | (4) | 1 | (2) | 4 | (7) |
| Lack of understanding of the delivery model/eligibility criteria | 2 | (4) | 13 | (24) | 14 | (25) | 19 | (36) |
| HPV vaccine stock outs | 1 | (2) | 2 | (4) | 0 | (0) | 0 | (0) |
| Difficulty identifying eligible girls (out-of-school) | 1 | (2) | 1 | (2) | 0 | (0) | 2 | (4) |
| Geographic accessibility | 1 | (2) | 0 | (0) | 1 | (2) | 4 | (7) |
| Other | 0 | (0) | 5 | (9) | 4 | (7) | 4 | (7) |
| No challenges reported | 7 | (13) | 11 | (20) | 12 | (22) | 16 | (29) |
3.3. Target age group and eligibility
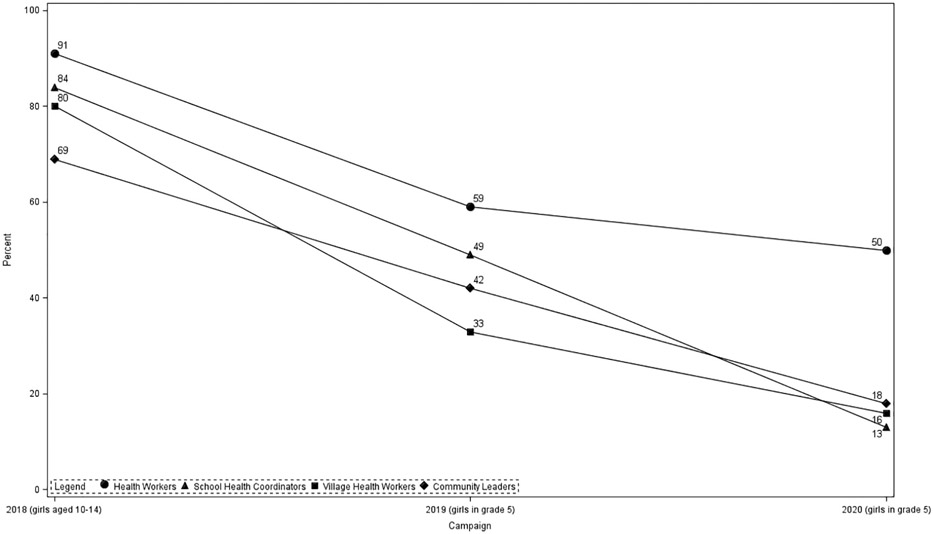
Most respondents correctly identified that girls aged 10–14 years were eligible for vaccination in 2018, the first year of introduction (91% of health workers, 84% of school health coordinators, 80% of village health workers, and 69% of community leaders, Fig. 1). Fewer respondents correctly identified grade 5 girls as eligible for first dose in 2019, the second year of vaccination (59% of health workers, 49% of school health coordinators, 33% of village health workers, and 42% of community leaders). Less than half of the respondents correctly identified grade 5 girls as being eligible for the first dose of HPV vaccination in 2020, the upcoming year (50% of health workers, 13% of school health coordinators, 16% of village health workers, and 18% of community leaders). Twenty-three percent of health workers, 62% of school health coordinators, 49% of village health workers, and 51% of community leaders indicated that they were not informed about the HPV vaccine target eligibility for 2020.
Fig. 1.
Percent of respondents correctly identifying HPV vaccination first dose target eligibility criteria for 2018, 2019, and 2020 campaigns among the health workers, school health coordinators, village health workers, and community leaders surveyed for the HPV vaccination program feasibility and acceptability surveys, Zimbabwe, January–February 2020.
3.4. Awareness, communication, and social mobilization
Most respondents (89% of health workers, 60% of school health coordinators, 96% of village health workers, and 96% of community leaders) reported that parents and caregivers were the primary decision-maker for girls’ receipt of the HPV vaccine (Table 4). Some (36%) school health coordinators also mentioned girls as being the primary decision-maker. Word-of-mouth communication (i.e., teachers, village health workers, community leaders, and health workers) was identified by respondents as being the most effective at reaching caregivers and girls. Almost all (96% of health workers, 96% of school health coordinators 84% village health workers, and 84% of community leaders) respondents felt prepared to answer questions from the community about the HPV vaccine. Thirty-six percent of health workers, 47% of school health coordinators 56% of village health workers, and 29% of community leaders reported hearing rumors about the HPV vaccine. Common rumors included “HPV vaccine will affect a girl’s fertility”, “HPV vaccine is not safe”, “HPV vaccine is experimental”, and “HPV vaccine will cause severe side effects”.
Table 4.
HPV vaccine perceptions on decision-making, communication channels, and rumors among the health workers, school health coordinators, village health workers, and community leaders surveyed for the HPV vaccination program feasibility and acceptability surveys, Zimbabwe, January–February 2020.
| Health workers (N = 56) |
School health coordinators (N = 55) |
Village health workers (N = 55) |
Community leaders (N = 55) |
|||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Primary decision-maker for girls’ receipt of HPV vaccine according to respondent | ||||||||
| Parent(s) | 50 | (89) | 33 | (60) | 53 | (96) | 53 | (96) |
| Health worker | 0 | (0) | 0 | (0) | 1 | (2) | 1 | (2) |
| Girl | 6 | (11) | 20 | (36) | 1 | (2) | 0 | (0) |
| Teacher/school health coordinator | 0 | (0) | 1 | (2) | 0 | (0) | 1 | (2) |
| Other | 0 | (0) | 1 | (2) | 0 | (0) | 0 | (0) |
| Communication channels identified to be most effective in reaching caregivers and girls about the HPV vaccination | ||||||||
| Health Worker recommendation | 14 | (25) | 8 | (15) | 6 | (11) | 3 | (6) |
| Village Health Workers | 10 | (18) | 3 | (5) | 18 | (33) | 8 | (16) |
| Schools/Teachers/School Health Coordinator | 10 | (18) | 14 | (25) | 5 | (9) | 13 | (25) |
| Flyers/pamphlets/leaflets | 6 | (11) | 3 | (5) | 2 | (4) | 3 | (6) |
| Community Leaders | 5 | (9) | 9 | (16) | 7 | (13) | 16 | (31) |
| Town criers/Megaphones | 5 | (9) | 4 | (7) | 6 | (11) | 1 | (2) |
| Other | 3 | (5) | 6 | (11) | 3 | (5) | 4 | (7) |
| Radio | 1 | (2) | 5 | (9) | 2 | (4) | 3 | (6) |
| Posters/Banners | 1 | (2) | 2 | (4) | 4 | (7) | 1 | (2) |
| Churches/Religious Leaders | 1 | (2) | 0 | (0) | 2 | (4) | 3 | (6) |
| TV | 0 | (0) | 1 | (2) | 0 | (0) | 0 | (0) |
| Felt prepared to answer questions about HPV/recommending the HPV vaccine | 54 | (96) | 53 | (96) | 46 | (84) | 46 | (84) |
| Heard rumors on the HPV vaccine | 20 | (36) | 26 | (47) | 31 | (56) | 16 | (29) |
| Type of rumors heard | ||||||||
| HPV vaccine will affect a girl’s fertility | 11 | (55) | 19 | (73) | 23 | (74) | 9 | (56) |
| HPV vaccine is not safe | 7 | (35) | 12 | (46) | 11 | (35) | 9 | (56) |
| HPV vaccine will cause cervical cancer | 5 | (25) | 1 | (4) | 1 | (3) | 0 | (0) |
| HPV vaccine is experimental | 5 | (25) | 12 | (46) | 16 | (52) | 7 | (44) |
| HPV vaccine will promote early sexual onset | 4 | (20) | 2 | (8) | 4 | (13) | 1 | (6) |
| HPV vaccine will cause severe side effects | 3 | (15) | 12 | (46) | 11 | (35) | 8 | (50) |
| Other | 2 | (10) | 2 | (8) | 4 | (13) | 0 | (0) |
| HPV vaccine costs money | 1 | (5) | 0 | (0) | 1 | (3) | 0 | (0) |
Most respondents reported attending a training or orientation before the first HPV vaccination campaign (82% of health workers, 67% of school health coordinators, 95% of village health workers, and 85% of community leaders). Most respondents (93% of health workers, 76% of school health coordinators, 62% of village health workers, and 85% of community leaders) reported having received written materials on the HPV. Among village health workers and community leaders, “disease HPV vaccine protects against”, “HPV vaccine is for girls 10–14 years of age” and “HPV vaccine is safe” were the top messages received during the training/orientation.
Almost all stakeholders stated that the HPV infection can cause cervical cancer (98% of health workers, 95% of school health coordinators, 91% of village health workers, 82% of community leaders). A few stakeholders identified other cancers (9% of health workers, 9% of school health coordinators, 20% of village health workers, 15% of community leaders) or genital warts (5% of health workers, 4% of school health coordinators, 5% of village health workers and 5% of community leaders) as being caused by the HPV infection. Nearly all health workers (96%) and school health coordinators (98%) identified the HPV vaccination as the primary method of cervical cancer prevention. Over half (55%) of health workers also mentioned screening (visual inspection with acetic acid, pap smear for HPV testing). Other methods of prevention identified included education on the risks associated with cervical cancer, avoiding multiple partners, abstaining from sexual activity, treatment of pre-cancerous lesions, and male circumcision. Most (93%) health workers, 73% of school health coordinators, and 55% of village health workers correctly identified that two doses of the HPV vaccine are needed to complete the series. Similarly, 86% of health workers, 87% of school health coordinators, and 67% of village health workers correctly identified the one-year interval schedule for the HPV vaccine administration in Zimbabwe.
Most (>=78%) respondents stated cervical cancer was “very serious”. Twenty-nine to fifty-two percent of the respondents felt that cervical cancer was a “big problem” in their communities; less than 20% of the respondents felt that cervical cancer was “not a problem” (Table 5). The respondents “strongly agreed” (>= 98%) that the HPV vaccine is important for girls, and over 90% of health workers, school health coordinators, and village health workers felt “very comfortable” recommending the HPV vaccine. Almost all village health workers (95%) and community leaders (82%) reported the HPV vaccine was “very accepted” in their community.
Table 5.
Perceptions around cervical cancer and the HPV vaccination among the health workers, school health coordinators, village health workers, and community leaders surveyed for HPV vaccination program feasibility and acceptability surveys, Zimbabwe, January–February 2020.
| Health workers (N = 56) |
School health coordinators (N = 55) |
Village health workers (N = 55) |
Community leaders (N = 55) |
|||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Perception of seriousness of cervical cancer | ||||||||
| Very serious | 55 | (98) | 51 | (93) | 43 | (78) | 44 | (80) |
| Somewhat serious | 1 | (2) | 3 | (5) | 8 | (15) | 5 | (9) |
| Not very serious | 0 | (0) | 1 | (2) | 3 | (5) | 6 | (11) |
| Don’t know | 0 | (0) | 0 | (0) | 1 | (2) | 0 | (0) |
| Perception of cervical cancer as a problem | ||||||||
| Big problem | 29 | (52) | 23 | (42) | 18 | (33) | 16 | (29) |
| Minor problem | 21 | (38) | 17 | (31) | 31 | (56) | 27 | (49) |
| Not a problem | 4 | (7) | 10 | (18) | 6 | (11) | 11 | (20) |
| Don’t know | 2 | (4) | 5 | (9) | 0 | (0) | 1 | (2) |
| Perception that the HPV vaccine is important | ||||||||
| Strongly agree | 56 | (100) | 55 | (100) | 54 | (98) | 54 | (98) |
| Somewhat agree | 0 | (0) | 0 | (0) | 1 | (2) | 1 | (2) |
| Somewhat disagree | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| Strongly disagree | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| Comfort level recommending the HPV vaccine | ||||||||
| Very comfortable | 56 | (100) | 54 | (98) | 51 | (93) | – | – |
| Somewhat comfortable | 0 | (0) | 1 | (2) | 4 | (7) | – | – |
| Not very comfortable | 0 | (0) | 0 | (0) | 0 | (0) | – | – |
| Perception of acceptance of the HPV vaccine in community | ||||||||
| Very accepted | – | – | – | – | 52 | (95) | 45 | (82) |
| Somewhat accepted | – | – | – | – | 3 | (5) | 8 | (15) |
| Not very accepted | – | – | – | – | 0 | (0) | 2 | (4) |
4. Discussion
The HPV vaccine introduction in Zimbabwe was effective at reaching large numbers of eligible girls with 751,367 doses delivered in the 2018 campaign and 801,887 doses delivered in the 2019 campaign, as reported through the WHO/UNICEF joint reporting process [8]. The HPV vaccine introduction was considered a success by the national-level stakeholders due to political commitment, strong collaborations, and careful preparation [30]. In our evaluation conducted at the health facility and community level, respondents identified funding gaps, lack of transportation, and staff shortages as key challenges faced in the implementation of the HPV vaccination program.
The extended and complex economic situation in Zimbabwe, exacerbated by Cyclone Idai in March 2019 and a severe drought, has led to numerous downstream effects, including inflated prices of goods, limited fuel availability, decreased access to electricity and water, and increased food insecurity [9]. Infrastructure challenges, supply stockouts, and staffing shortages have negatively impacted access to health services and patient care [10]. Despite these complicated obstacles, health workers found the HPV vaccine delivery feasible and the program was well accepted by the school and community respondents. Prioritizing sustained funding for the HPV vaccination in Zimbabwe will help maintain gains achieved in the HPV vaccination so far and will contribute to a sustainable future for the program.
School-based vaccination has been shown to result in high coverage, and programs incorporating health facility vaccination into this strategy have shown most effective at reaching the target population [11-14]. Findings support that the school-based campaign was feasible and well-accepted in Zimbabwe. Despite some challenges identified, health workers and teachers were well informed about the HPV vaccination program and indicated having the capacity to deliver services to the target population while maintaining routine immunization services. This suggests school-based HPV vaccination in similar low-resource settings is possible, provided necessary funding is available. Moving forward, reaching out-of-school girls through engagement with the community health workers or by using other strategies will ensure equity in the HPV vaccination program in Zimbabwe.
The introduction of the HPV vaccine presents an opportunity for many low- and middle-income country immunization programs to target a population that is not typically reached by routine immunization services. Questions remain as to the ideal target group selection for the HPV vaccination, and the decision is largely based on country preference and context. While Zimbabwe achieved high coverage (83%) in the initial age-based HPV vaccination of a multiple cohort, findings from this survey illustrate that the transition from the 10–14-year-old age-based multiple cohort to the grade 5 single cohort was not well understood among the respondents. Improper identification of eligible girls can lead to missed opportunities for vaccination, vaccination outside the target group, or inaccuracies in recording and reporting—potentially resulting in coverage inaccuracies. Further, different criteria for in-school girls (grade-based) and out-of-school girls (age-based) can lead to additional confusion among health workers and the community. As Zimbabwe continues the HPV vaccination program with grade-based, primarily in-school vaccination, this confusion is likely to reduce; however, the continuation of trainings and communication to the public on eligibility is essential.
Nearly half of the respondents in the survey reported having heard negative rumors related to the HPV vaccine. Concerns about the HPV vaccine possibly causing severe side effects or having a negative effect on future fertility have commonly been reported during the HPV vaccine introductions elsewhere [15]. Vaccine hesitancy has been reported in pockets of the population in Zimbabwe, primarily among religious groups [16-18]. Fortunately, overall high coverage for the HPV vaccination has been seen in the administrative records and a coverage survey [6,19] suggesting that rumors have not negatively impacted vaccine uptake thus far. However, Zimbabwe should monitor these rumors and work to maintain community acceptability as vaccine hesitancy and rumors have derailed the HPV vaccination programs in other countries [20-23]. Continued training and sensitization around rumor management as well as maintenance of a risk communication plan will be important in the coming years, especially as access to the internet, social media, and other information sources become more widespread in Zimbabwe.
Coverage for the HPV vaccination programs is higher in low- and middle-income countries when compared to high-income countries [13]. Vaccination programs are often well-trusted in low-resource settings where the impact of vaccines has been seen with the reduction of vaccine-preventable diseases over time [24,25]. Low hesitancy and good uptake of the HPV vaccine has been observed in resource-constrained settings where the burden of cervical cancer is often high and screening and treatment capabilities are limited [25-27]. Survey respondents from all groups considered cervical cancer to be a very serious disease, which is consistent with previous reports by health workers of concerns related to cervical cancer among young people and the presence of general support for the HPV vaccination programs in Zimbabwe [28,29]. Almost all respondents felt that receiving the HPV vaccine is important; additionally, village health workers and community leaders indicated a high level of acceptance in their communities.
There are several limitations to this survey. Within each health facility catchment area, one school health coordinator, one village health worker, and one community leader were selected, using convenience sampling by the data collection team. While this allowed for the selection of stakeholders from a range of geographic and urban/rural communities, it was not random. Health workers assisted in the referral of nearby individuals available for interviews at the time of the visit, and they may have recommended respondents more familiar with and knowledgeable about the HPV program.
All questionnaires were written and displayed on tablets in English. While Shona and Ndebele translations were available within the tablet interface for data collectors for village health worker and community leader questionnaires, variability in the interpretation of specific questions within the survey is possible. Lastly, the survey was administered more than one year after the vaccine was introduced; therefore, participants may have had difficulty recalling experiences related to certain questions pertaining directly to the introduction period.
5. Conclusion
Findings from this survey supported evidence of a strong nationwide HPV vaccine introduction in Zimbabwe. It was feasible for the health system to implement and was well accepted within the community. Challenges in determining target eligibility were seen within the first year of introduction and the lack of full understanding of the target eligibility criteria may have led to missed opportunities for vaccination, vaccinating outside the target group, and recording and reporting challenges. The Zimbabwe immunization program should strive to maintain gains achieved so far, continue fostering high demand for the HPV vaccine and advocate for additional resources from the government, partners, and donors to ensure the sustainability of the HPV program in the future.
Acknowledgements
We acknowledge the Government of Zimbabwe, including the Ministry of Health and Child Care, the Ministry of Primary and Secondary Education, and ZIMSTAT; global partners, including John Snow International, Inc. (particularly Ernest Ndlela and Adelaide Shearley), WHO, and PATH. Additional acknowledgements include Anna Hidle and Anyie Li.
Funding
This work was supported by Gavi, the Vaccine Alliance [“Evaluation of Human Papilloma Virus (HPV) Vaccine National Introduction in Low-and-Lower-Middle Income Countries” - Contract No. ME 9422 12 20].
Footnotes
CRediT authorship contribution statement
Julie R. Garon: Conceptualization, Methodology, Project administration, Data curation, Formal analysis, Writing - original draft, Writing - review & editing. Aluwisio Mukavhi: Project administration, Writing - review & editing. Maxwell Rupfutse: Methodology, Writing - review & editing. Shakia Bright: Investigation, Writing - review & editing. Timothy Brennan: Data curation, Writing - review & editing. Portia Manangazira: Conceptualization, Writing - review & editing. Qian An: Methodology, Writing - review & editing. Anagha Loharikar: Conceptualization, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Disclaimer
The authors alone are responsible for the views expressed in this article, which do not necessarily represent the views, decisions, or policies of the institutions with which the authors are affiliated.
This article was published as part of a supplement supported by Centers for Disease Control and Prevention Global Immunization Division. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or World Health Organization. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors.
Data statement
Data associated with this manuscript is unsuitable to post
Data is country owned
Authors do not have permission to share.
References
- [1].Hidle A, Gwati G, Abimbola T, Pallas SW, Hyde T, Petu A, et al. Cost of a human papillomavirus vaccination project, Zimbabwe. Bull World Health Organ 2018;96:834–42. 10.2471/BLT.18.211904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Government of Zimbabwe. Proposal for HPV Support 2017: Zimbabwe 2017.
- [3].Meeting of the Strategic Advisory Group of Experts on immunization, October 2016 - conclusions and recommendations. World Health Organization; 2016. [Google Scholar]
- [4].Lessons Learned - HPV Vaccine Nationwide Introduction in Zimbabwe n.d.:19. [Google Scholar]
- [5].WHO/UNICEF Human papillomavirus (HPV) vaccine coverage estimates. World Health Organization/UNICEF; 2020. [Google Scholar]
- [6].HPV Vaccination Program. Senegal: 2019. [Google Scholar]
- [7].Vaccination Coverage Cluster Surveys: Reference Manual. Geneva: World Health Organization; 2018. [Google Scholar]
- [8].WHO/UNICEF country reported HPV doses administered. World Health Organization/UNICEF; 2020. [Google Scholar]
- [9].WorldBank Zimbawe Overview. World Bank n.d. https://www.worldbank.org/en/country/zimbabwe/overview (accessed October 30, 2020).
- [10].Mangundu M, Roets L, van Rensberg EJ. Accessibility of healthcare in rural Zimbabwe: The perspective of nurses and healthcare users. Afr J Prim Health Care Fam Med 2020;12. 10.4102/phcfm.v12i1.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Watson-Jones D, Baisley K, Ponsiano R, Lemme F, Remes P, Ross D, et al. Human papillomavirus vaccination in tanzanian schoolgirls: cluster-randomized trial comparing 2 vaccine-delivery strategies. J Infect Dis 2012;206:678–86. 10.1093/infdis/jis407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].WHO ∣ Human papillomavirus vaccine delivery strategies that achieved high coverage in low- and middle-income countries. WHO; n.d. https://www.who.int/bulletin/volumes/89/11/11-089862/en/ (accessed June 25, 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Paul Proma, and Fabio Anthony. “Literature Review of HPV Vaccine Delivery Strategies: Considerations for School- and Non-School Based Immunization Program.” Vaccine 32, no. 3 (January 9, 2014): 320–26. 10.1016/j.vaccine.2013.11.070. [DOI] [PubMed] [Google Scholar]
- [14].Ladner J, Besson M-H, Hampshire R, Tapert L, Chirenje M, Saba J. Assessment of eight HPV vaccination programs implemented in lowest income countries. BMC Public Health 2012;12:370. 10.1186/1471-2458-12-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kabakama S, Gallagher KE, Howard N, Mounier-Jack S, Burchett HED, Griffiths UK, et al. Social mobilisation, consent and acceptability: a review of human papillomavirus vaccination procedures in low and middle-income countries. BMC Public Health 2016;16. 10.1186/s12889-016-3517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Machekanyanga Z, Ndiaye S, Gerede R, Chindedza K, Chigodo C, Shibeshi ME, et al. Qualitative Assessment of Vaccination Hesitancy Among Members of the Apostolic Church of Zimbabwe: A Case Study. J Relig Health 2017;56:1683–91. 10.1007/s10943-017-0428-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gerede R, Machekanyanga Z, Ndiaye S, Chindedza K, Chigodo C, Shibeshi ME, et al. How to Increase Vaccination Acceptance Among Apostolic Communities: Quantitative Results from an Assessment in Three Provinces in Zimbabwe. J Relig Health 2017;56:1692–700. 10.1007/s10943-017-0435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ha W, Salama P, Gwavuya S, Kanjala C. Is religion the forgotten variable in maternal and child health? Evidence from Zimbabwe. Soc Sci Med 1982;2014 (118):80–8. 10.1016/j.socscimed.2014.07.066. [DOI] [PubMed] [Google Scholar]
- [19].Zimbabwe HPV Vaccination Coverage Survey Report (Unpublished). n.d.
- [20].Gallagher KE, LaMontagne DS, Watson-Jones D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine 2018. 10.1016/j.vaccine.2018.02.003. [DOI] [PubMed] [Google Scholar]
- [21].Larson HJ, Wilson R, Hanley S, Parys A, Paterson P. Tracking the global spread of vaccine sentiments: The global response to Japan’s suspension of its HPV vaccine recommendation. Hum Vaccines Immunother 2014;10:2543–50. 10.4161/21645515.2014.969618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Larson HJ, Brocard P, Garnett G. The India HPV-vaccine suspension. The Lancet 2010;376:572–3. [DOI] [PubMed] [Google Scholar]
- [23].Mølbak K, Hansen ND, Valentiner-Branth P. Pre-Vaccination Care-Seeking in Females Reporting Severe Adverse Reactions to HPV Vaccine. A Registry Based Case-Control Study. PLOS One 2016;11:e0162520. 10.1371/journal.pone.0162520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Turner HC, Thwaites GE, Clapham HE. Vaccine-preventable diseases in lower-middle-income countries. Lancet Infect Dis 2018;18:937–9. 10.1016/S1473-3099(18)30478-X. [DOI] [PubMed] [Google Scholar]
- [25].Brotherton JML, Bloem PJN. HPV Vaccination: Current Global Status. Curr Obstet Gynecol Rep 2015;4:220–33. 10.1007/s13669-015-0136-9. [DOI] [Google Scholar]
- [26].Vermandere H, Naanyu V, Mabeya H, Vanden Broeck D, Michielsen K, Degomme O. Determinants of Acceptance and Subsequent Uptake of the HPV Vaccine in a Cohort in Eldoret. Kenya. PLoS One 2014;9:e109353. 10.1371/journal.pone.0109353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Gallagher KE, Howard N, Kabakama S, Mounier-Jack S, Burchett HED, LaMontagne DS, et al. Human papillomavirus (HPV) vaccine coverage achievements in low and middle-income countries 2007–2016. Papillomavirus Res Amst Neth 2017;4:72–8. 10.1016/j.pvr.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Crann SE, Barata PC, Mitchell R, Mawhinney L, Thistle P, Chirenje ZM, et al. Healthcare providers’ perspectives on the acceptability and uptake of HPV vaccines in Zimbabwe. J Psychosom Obstet Gynecol 2016;37:147–55. 10.1080/0167482X.2016.1199544. [DOI] [PubMed] [Google Scholar]
- [29].Mapanga W, Girdler-Brown B, Singh E. Knowledge, attitudes and practices of young people in Zimbabwe on cervical cancer and HPV, current screening methods and vaccination. BMC Cancer 2019;19:845. 10.1186/s12885-019-6060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Garon Julie. Nationwide Introduction of HPV Vaccine in Zimbabwe 2018–2019: Experiences with Multiple Cohort Vaccination Delivery. Unpublished results. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data associated with this manuscript is unsuitable to post
Data is country owned
Authors do not have permission to share.