Abstract
Objectives
The aim of this meta-analysis was to compare the efficacy and safety of unilateral curved and bilateral straight percutaneous vertebral augmentation (PVA) in the treatment of osteoporotic vertebral compression fractures (OVCFs).
Materials and methods
We performed a comprehensive literature search from electronic databases including Springer, Web of Science, PubMed, Cochrane Library databases and ScienceDirect up to July 2022. Three randomized-controlled trials (RCTs) and one retrospective study which met the inclusion criteria were analyzed.
Results
There were significant differences in the operative time, injected bone cement volume, bone cement leakage rate and X-ray frequency between the bilateral straight PVA and unilateral curved PVA. No significant differences were found regarding postoperative Cobb angle, Visual Analog Scale or Oswestry Disability Index between the two groups.
Conclusion
Compared to bilateral straight PVA, unilateral curved PVA may decrease operative time, injected bone cement volume, bone cement leakage rate, and X-ray frequency in the treatment of OVCFs. However, the Cobb angle, pain, and clinical scores are comparable. Due to the limited quality and data of the evidence currently available, more high-quality RCTs are required.
Keywords: Meta-analysis, osteoporotic vertebral fractures, percutaneous, vertebral augmentation.
Introduction
Osteoporotic vertebral compression fractures (OVCFs) are common in the aging population, and there are approximately 1.7 million cases of OVCF in the United States (US) and Europe annually.[1] These fractures often lead to low back pain, spinal deformity, neurological dysfunction, and even impaired quality of life.[2] Percutaneous vertebral augmentation (PVA), including percutaneous kyphoplasty (PKP) and percutaneous vertebroplasty (PVP), is a minimally invasive interventional technique and have been proven to be a successful surgical procedure for patients with OVCFs to provide rapid pain control, correct deformity, and improve postoperative function.[3]
Using conventional straight PVA, puncture approaches include unipedicular puncture and bipedicular puncture.[4] Traditionally, the standard technique for PVA is a bipedicular approach and it has been shown to be associated with uniform cement distribution in the vertebral body.[5] However, bipedicular puncture approach can increase operating time, surgical trauma to the patients, risk of bone cement leakage and X-ray exposure.[6] During unipedicular percutaneous puncture approach, bone cement can often only fill the ipsilateral vertebral bone, leaving the contralateral vertebral bone poorly filled. The non-uniform distribution of the bone cement is likely to increase the risk of re-collapse of the non-augmented contralateral vertebral bone, particularly during lateral bending.[7] Moreover, the unipedicular puncture requires a more aggressive, lateral-to-medial approach as compared to the bipedicular approach, which increases the risk of injury to paravertebral nerves or vessels.[8]
In recent years, an improved PVA with curved device has been introduced and applied through unipedicular puncture, achieving uniform distribution of bone cement in the vertebral body.[9] To date, several studies[8,10-12] have compared unilateral curved and bilateral straight PVA in treating OVCFs. However, whether unilateral curved PVA is superior to bilateral straight PVA still remains controversial. In the present study, we, therefore, performed a metaanalysis with a large sample to compare the efficacy and safety of unilateral curved and bilateral straight PVA in treating OVCFs.
Patients and Methods
Search strategy
This meta-analysis was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We performed a comprehensive literature search from electronic databases such as Springer, Web of Science, PubMed, Cochrane Library databases and ScienceDirect up to July 2022. We also checked the references of the identified articles to find other relevant articles. The language of identified articles was not restricted. The keywords used for the search strategy included: “osteoporotic vertebral compression fractures”, “percutaneous”, “vertebral augmentation” and “curved”.
Inclusion criteria
Studies were selected for inclusion if they met the following criteria: (i) the sample included OVCFs patients treated with PVA; (ii) the test group was unilateral curved PVA and the control group was bilateral straight PVA; (iii) the clinical outcomes included operative time, X-ray frequency, injected bone cement volume, postoperative functional score, the Visual Analog Scale (VAS) score, Cobb angle, cement leakage or other complications; and (iv) the study was a published comparative trial, including randomized-controlled trials (RCTs) and non-RCTs. Two independent reviewers assessed the eligibility of identified articles. A third reviewer resolved any disagreement between the reviewers.
Exclusion criteria
Studies were excluded for following reasons: (i) duplicate articles or articles including the same patients, content and results; (ii) theoretical research, case reports, meta-analyses, systematic reviews, expert comments, economic analyses and conference reports; and (iii) studies with non-relevant outcome.
Data extraction
Data extraction was performed independently from the included articles by two reviewers. The following information was extracted: the first author’s name, the publication year, country conducted in, the size of the sample, intervention, the comparable baselines, the follow-up time and the computed endpoints in each study. Endpoints include operative time, X-ray frequency, injected bone cement volume, postoperative functional score, the VAS score, Cobb angle, bone cement leakage or other complications. Other relevant data were also extracted from the included studies. If there were incomplete data, we contacted the corresponding author through e-mail for details.
Quality assessment
The methodological quality of the RCTs were assessed with a modification of the generic evaluation tool described in the Cochrane Handbook for Systematic Reviews of Interventions.[13] The methodological quality of non-RCTs was evaluated by the methodological index for non-randomized studies (MINORS).[14] Two authors independently performed the methodological quality assessment. Disagreements in methodological assessment were solved by discussion, and a third reviewer was consulted if necessary.
Data analysis and statistical analysis
Statistical analysis was performed using the RevMan version 5.1 software (The Cochrane Collaboration, Oxford, UK). The I2 values and p values were used to estimate the level of heterogeneity. When I2 <50%, p>0.1, heterogeneity could be accepted and the fixed-effects model was used for data analysis. Otherwise, significant heterogeneity was considered, and a random-effects model was used for the data analysis. Subgroup analysis was performed to investigate the sources of significant heterogeneity. For continuous variables, mean differences (MDs) and 95% confidence intervals (CIs) were calculated. For dichotomous outcomes, odds ratios (ORs) and 95% CIs were calculated.
Results
Search results
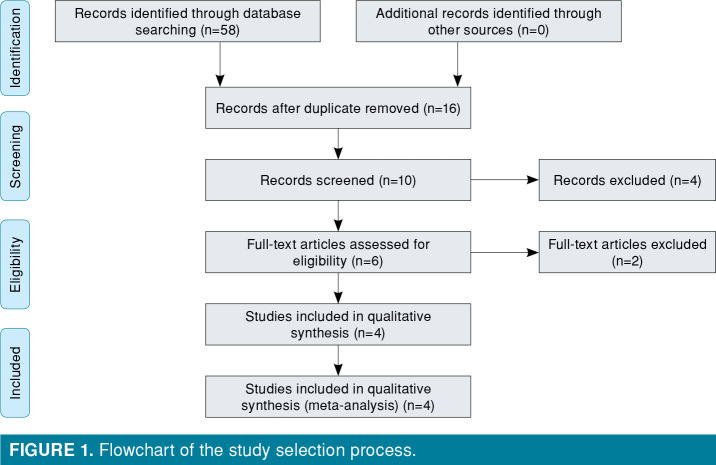
A total of 58 studies were retrieved from the selected data base search. No additional study was identified through other sources. After carefully reviewing the titles and abstract, 54 studies were excluded. Finally, three RCTs and one non-RCTs were included for data extraction and meta-analysis. The detailed search process is summarized in Figure 1.
Figure 1. Flowchart of the study selection process.
Characteristics of the included studies
General information of included studies is summarized in Table I. The baseline characteristics of two groups in all studies were comparable.
Table 1. Characteristics of included studies.
| Authors | Year | Study design | PVA type | Group | Cases (n) | Female (n) | Mean age (year) | Preoperative VAS | Preoperative ODI | Follow-up (months) |
| Curved | 30 | 18 | 71.8+11.2 | 8.0+1.1 | - | 3 | ||||
| Cheng and Liu[11] | 2019 | RCT | PVP | Straight | 22 | 12 | 69.8±12.1 | 8.3±0.7 | - | 3 |
| Curved | 25 | 17 | 70.7+6.8 | 7.9+0.6 | 40.1+3.5 | 3 | ||||
| Geng et al.[12] | 2021 | RCT | PVP | Straight | 31 | 21 | 70.4±6.6 | 7.9±0.5 | 40.1±4.7 | 3 |
| Curved | 36 | 26 | 75.6+6.1 | 7.6+1.3 | 70.8+10.0 | 6 | ||||
| Wang et all10! | 2021 | RCT | PKP | Straight | 36 | 24 | 76.5±6.2 | 7.4±1.0 | 72.6±9.4 | 6 |
| Curved | 29 | 26 | 70.7+7.5 | 8.3+1.0 | 75.0+11.1 | 12 | ||||
| Zhong et al.[8] | 2019 | RCS | PVP | Straight | 75 | 63 | 73.8±8.2 | 8.2±0.8 | 73.4±11.7 | 12 |
| PVA: Percutaneous vertebral augmentation; RCT: Randomized-controlled trial; RCS: Retrospective, controlled study; PVP: Percutaneous vertebroplasty; PKP: Percutaneous kyphoplasty; VAS: Visual Analog Scale; ODI: Oswestry Disability Index. | ||||||||||
Risk of bias assessment
The methodological quality of the RCTs is shown in Figure 2. The inclusion and exclusion criteria were clearly stated in all RCTs. All RCTs reported randomized sequence generation. None of RCTs reported allocation concealment and blinding method. Unclear bias was not found due to incomplete outcome data or selective outcomes. The MINORS of the non-RCTs was 20 (Table II). The non-RCTs did not prospectively perform prospective calculation of the sample size and data collection.
Figure 2. The summary of bias risk of randomized controlled trials.
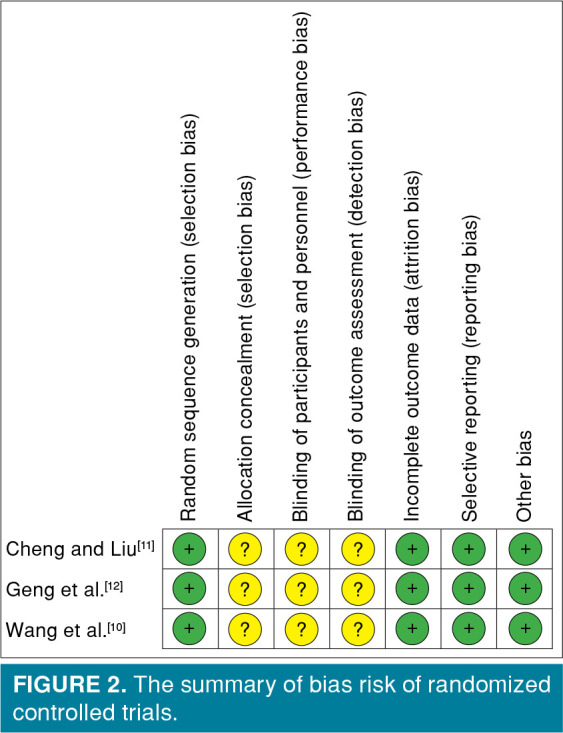
Table 2. Quality assessment for non-randomized trials.
| Quality assessment for non-randomized trials | Zhong et al.[8] 2019 |
| A clearly stated aim | 2 |
| Inclusion of consecutive patients | 2 |
| Prospective data collection | 0 |
| Endpoints appropriate to the aim of the study | 2 |
| Unbiased assessment of the study endpoint | 2 |
| A follow-up period appropriate to the aims of study | 2 |
| Less than 5% loss to follow-up | 2 |
| Prospective calculation of the sample size | 0 |
| An adequate control group 2 Contemporary groups | 2 |
| Baseline equivalence of groups | 2 |
| Adequate statistical analyses | 2 |
| Total score | 20 |
Outcomes of the meta-analysis
Operative time
Operative time was recorded in four studies. Figure 3 shows that operative time in the curved group was lower than that in the straight group (MD= -13.51, 95% CI: -17.29 to -9.733; p<0.00001).
Figure 3. Forest plot showing operative time. SD: Standard deviation; CI: Confidence interval.
X-ray frequency
X-ray frequency was reported in three studies. Figure 4 depicts that X-ray frequency in the curved group was less than that in the straight group (MD= -8.57, 95% CI: -10.34 to -6.81; p<0.00001).
Figure 4. Forest plot showing X-ray frequency. SD: Standard deviation; CI: Confidence interval.
Injected bone cement volume
Injected bone cement volume was reported in four studies. Figure 5 shows that injected bone cement volume in the curved group was less than that in the straight group (MD= -1.13, 95% CI: -1.63 to -0.62; p<0.0001).
Figure 5. Forest plot showing injected bone cement volume. SD: Standard deviation; CI: Confidence interval.
Postoperative Oswestry Disability Index (ODI)
Postoperative ODI was documented in three studies. Figure 6 shows that postoperative ODI in the curved group was similar to that in the straight group (MD= -0.78, 95% CI: -2.28 to 0.72; p=0.31).
Figure 6. Forest plot showing postoperative ODI. SD: Standard deviation; CI: Confidence interval.
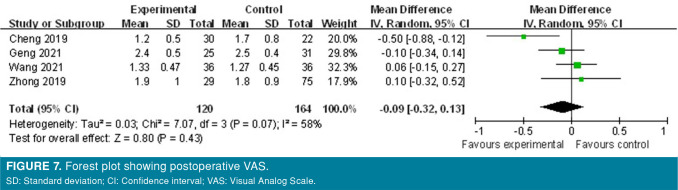
Postoperative VAS
Postoperative VAS scores were assessed in four studies. Figure 7 depicts that postoperative VAS in the curved group was similar to that in the straight group (MD= -0.09, 95% CI: -0.32 to 0.13; p=0.43).
Figure 7. Forest plot showing postoperative VAS. SD: Standard deviation; CI: Confidence interval; VAS: Visual Analog Scale.
Postoperative Cobb angle
Postoperative Cobb angle was available in two studies. Figure 8 shows that postoperative Cobb angle in the curved group was similar to that in the straight group (MD= 0.17, 95% CI: -2.47 to 2.82; p=0.90).
Figure 8. Forest plot showing postoperative Cobb angle. SD: Standard deviation; CI: Confidence interval.
Bone cement leakage rate
Bone cement leakage rate was reported in four studies, of which 16 out of 130 in the curved group and 56 out of 181 in the straight group. Figure 9 depicts that bone cement leakage rate in the curved group was lower than that in the straight group (OR=0.37, 95% CI: 0.20 to 0.69; p=0.002).
Figure 9. Forest plot showing bone cement leakage rate. CI: Confidence interval.
Other outcomes
Zhong et al.[8] reported that five and two patients developed fragile vertebral refractures at non-adjacent and adjacent levels, respectively (one patient developed adjacent level refractures twice), in the bipedicular vertebroplasty group. In contrast, none of the patients developed refractures at either non-adjacent or adjacent levels in the curved vertebroplasty group during the 36-month period. However, limited data could not be extracted for meta-analysis.
Discussion
Our meta-analysis included three RCTs and one retrospective study. All included studies were small simple size and had relatively short follow-ups. The objective of our meta-analysis was to compare the efficacy and safety of unilateral curved and bilateral straight PVA in treating OVCFs. In the current study, we found that, compared to bilateral straight PVA, unilateral curved PVA was associated with less operative time, injected bone cement volume and X-ray frequency and lower bone cement leakage rate. To the best of our knowledge, the present study is the first quantitative meta-analysis to evaluate the efficacy and safety of unilateral curved PVA in treating OVCFs.[15]
Bone cement leakage is the most frequent complication of PVA that has not been completely avoided. Previous studies have reported that the incidence of bone cement leakage ranges from 4.8 to 39%.[16] Although the majority of patients was asymptomatic, bone cement leakage may lead to neurological impairment, pulmonary embolism and even death in certain severe cases.[17] In PVA, the causes of bone cement leakage include the fracture of the perivertebral wall or endplate, injected bone cement volume and the pressure of bone cement perfusion.[18] Cheng and Liu[11] conducted a RCT which reported that unilateral percutaneous curved vertebroplasty was associated with less bone cement injection volume and bone cement leakage rate than bilateral PVP. Another randomized study led by Wang et al.[10] included 72 elderly patients with OVCF. They concluded that bone cement injection volume was lower in unilateral percutaneous curved kyphoplasty group than that in conventional bilateral PKP group. In total, 16 of 130 cases in the curved group and 56 of 181 cases in the straight group reported the occurrence of bone cement leakage. The present meta-analysis showed that unilateral curved PVA reduced the risk of bone cement leakage and injected bone cement volume compared to bilateral straight PVA. Thus, unilateral curved PVA can significantly decrease bone cement leakage rate.
In PVA, repeated fluoroscopy is mandatory and helps to confirm the needle location. Both surgeons and patients may face a risk of dermatitis, cataract, and cancer, due to significant doses of radiation exposure from repeated fluoroscopy.[19] Wang et al.[10] compared OVCF patients receiving unilateral curved PKP with traditional bipedicular PKP, and the results showed that X-ray frequency was significantly less in unilateral curved PKP group. Zhong et al.[8] in a retrospective study of 104 OVCFs treated with unilateral percutaneous curved vertebroplasty or bilateral PVP, found that percutaneous curved vertebroplasty could reduce fluoroscopy frequency during operation. In the current study, X-ray frequency and operation time were significantly lower in the curved group. The results of the present study are in line with these previous results.
The VAS score is the most commonly used tool for the evaluation of perioperative period. Although PVA was reported significant pain relief after PVA, residual back pain is not rare and greatly decreased patient satisfaction.[20] Several studies[20,21] have reported that the percentage of patients who experience unrelieved back pain after PVP ranges from 5 to 20%. In a retrospective analysis of 1,316 cases with PVP, Yang et al.[22] considered that sufficient bone cement injection with satisfactory distribution could induce a better analgesic effect. In the current study, postoperative VAS was not significantly different between the two groups. Thus, unilateral curved PVA can induce the same analgesic effect as analgesic effect as bilateral straight PVA.
Nonetheless, the limitations of present meta-analysis should be noted. First, the meta-analysis is limited to only four articles published, and the number of patients included in this meta-analysis is relatively small. Second, methodological weakness of prospective calculation of the sample size exists in non-RCTs and allocation concealment and blind method in RCTs may decrease the level of evidence. Third, postoperative height of fractured vertebrae and recurrent fractures were incomplete and we were unable to conduct a meta-analysis on these parameters.
In conclusion, compared to bilateral straight PVA, unilateral curved PVA may decrease operative time, injected bone cement volume, bone cement leakage rate, and X-ray frequency in the treatment of OVCFs. Due to the limited quality and data of the evidence currently available, more high-quality RCTs are required.
Acknowledgments.
The authors are grateful for the support by Tianjin Health Science and Technology Project (No. ZC20096 and RC20120).
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions: All authors contributed equally to the article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 2.Borgström F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, et al. Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int. 2006;17:637–650. doi: 10.1007/s00198-005-0015-8. [DOI] [PubMed] [Google Scholar]
- 3.Wang Q, Dong JF, Fang X, Chen Y. Application and modification of bone cement in vertebroplasty: A literature review. Jt Dis Relat Surg. 2022;33:467–478. doi: 10.52312/jdrs.2022.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, Yang H, Tang T. Unilateral versus bilateral balloon kyphoplasty for multilevel osteoporotic vertebral compression fractures: A prospective study. Spine (Phila Pa 1976) 2011;36:534–540. doi: 10.1097/BRS.0b013e3181f99d70. [DOI] [PubMed] [Google Scholar]
- 5.Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: Technical aspects. AJNR Am J Neuroradiol. 1997;18:1897–1904. [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang L, Liu Z, Wang J, Feng X, Yang J, Tao Y, et al. Unipedicular versus bipedicular percutaneous vertebroplasty for osteoporotic vertebral compression fractures: A prospective randomized study. BMC Musculoskelet Disord. 2015;16:145–145. doi: 10.1186/s12891-015-0590-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen B, Li Y, Xie D, Yang X, Zheng Z. Comparison of unipedicular and bipedicular kyphoplasty on the stiffness and biomechanical balance of compression fractured vertebrae. Eur Spine J. 2011;20:1272–1280. doi: 10.1007/s00586-011-1744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhong R, Liu J, Wang R, Liu Y, Chen B, Jiang W, et al. Unilateral curved versus bipedicular vertebroplasty in the treatment of osteoporotic vertebral compression fractures. BMC Surg. 2019;19:193–193. doi: 10.1186/s12893-019-0653-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brook AL, Miller TS, Fast A, Nolan T, Farinhas J, Shifteh K. Vertebral augmentation with a flexible curved needle: Preliminary results in 17 consecutive patients. J Vasc Interv Radiol. 2008;19:1785–1789. doi: 10.1016/j.jvir.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Wang C, Zhang Y, Chen W, Yan SL, Guo KJ, Feng S. Comparison of percutaneous curved kyphoplasty and bilateral percutaneous kyphoplasty in osteoporotic vertebral compression fractures: A randomized controlled trial. BMC Musculoskelet Disord. 2021;22:588–588. doi: 10.1186/s12891-021-04469-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng Y, Liu Y. Percutaneous curved vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fractures. J Int Med Res. 2019;47:2424–2433. doi: 10.1177/0300060519836917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geng Z, Zhou Q, Shang G, Ji Y, Kou H, Liu H. Short-term efficacy of the percutaneous vertebroplasty using a curved versus straight vertebroplasty needle in osteoporotic vertebral compression fractures. e131-8Orthopedics. 2021;44 doi: 10.3928/01477447-20201012-03. [DOI] [PubMed] [Google Scholar]
- 13.Handoll HH, Gillespie WJ, Gillespie LD, Madhok R. The Cochrane Collaboration: A leading role in producing reliable evidence to inform healthcare decisions in musculoskeletal trauma and disorders. Indian J Orthop. 2008;42:247–251. doi: 10.4103/0019-5413.41849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 15.Atik OŞ. Which articles do the editors prefer to publish. Jt Dis Relat Surg. 2022;33:1–2. doi: 10.52312/jdrs.2022.57903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corcos G, Dbjay J, Mastier C, Leon S, Auperin A, De Baere T, et al. Cement leakage in percutaneous vertebroplasty for spinal metastases: A retrospective evaluation of incidence and risk factors. E332-8Spine (Phila Pa 1976) 2014;39 doi: 10.1097/BRS.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 17.Savage JW, Schroeder GD, Anderson PA. Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Am Acad Orthop Surg. 2014;22:653–664. doi: 10.5435/JAAOS-22-10-653. [DOI] [PubMed] [Google Scholar]
- 18.Zhan Y, Jiang J, Liao H, Tan H, Yang K. Risk factors for cement leakage after vertebroplasty or kyphoplasty: A meta-analysis of published evidence. World Neurosurg. 2017;101:633–642. doi: 10.1016/j.wneu.2017.01.124. [DOI] [PubMed] [Google Scholar]
- 19.Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC, et al. Radiation safety and spine surgery: Systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg. 2014;82:1337–1343. doi: 10.1016/j.wneu.2014.07.041. [DOI] [PubMed] [Google Scholar]
- 20.Li Y, Yue J, Huang M, Lin J, Huang C, Chen J, et al. Risk factors for postoperative residual back pain after percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Eur Spine J. 2020;29:2568–2575. doi: 10.1007/s00586-020-06493-6. [DOI] [PubMed] [Google Scholar]
- 21.Fan X, Li S, Zeng X, Yu W, Liu X. Risk factors for thoracolumbar pain following percutaneous vertebroplasty for osteoporotic vertebral compression fractures. J Int Med Res. 2021;49:300060521989468–300060521989468. doi: 10.1177/0300060521989468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang JS, Liu JJ, Chu L, Li J, Chen C, Chen H, et al. Causes of residual back pain at early stage after percutaneous vertebroplasty: A retrospective analysis of 1,316 cases. E495-503Pain Physician. 2019;22 [PubMed] [Google Scholar]